Abstract
Purpose
Recent policy changes in the USA have led to an increasing number of patients being placed into observation units rather than admitted directly to the hospital. Studies of administrative data that use inpatient diagnosis codes to identify cohorts, outcomes, or covariates may be affected by this change in practice. To understand the potential impact of observation stays on research using administrative healthcare data, we examine the trends of observation stays, short (≤2 days) inpatient admissions, and all inpatient admissions.
Methods
We examined a large administrative claims database of commercially insured individuals in the USA between 2002 and 2011. Observation stays were defined on the basis of the procedure codes reimbursable by Medicare or commercial insurers. We report monthly rates of observation stays and short inpatient admissions overall and by patient demographics.
Results
We identified 5 355 752 observation stays from 2002 to 2011. Over the course of study, the rate of observation stays increased, whereas the rate of short inpatient stays declined. The most common reason for observation stays was nonspecific chest pain, also the third most common reason for short inpatient stays. The increasing trend of observation stays related to circulatory diseases mirrors the decreasing trend of short inpatient stays.
Conclusions
The use of observation stays has increased in patients with commercial insurance. Failure to account for observation stays may lead to an under-ascertainment of hospitalizations in contemporary administrative healthcare data from the USA.
Keywords: observation stays, administrative claims, research methods, pharmacoepidemiology
INTRODUCTION
Administrative claims databases are increasingly used for research and to support quality improvement activities. These data provide detailed information on the use of healthcare services by entire populations of patients. However, because the data were not collected for research, the meaning of data elements is often unclear. One particular challenge confronting researchers is the identification of incident and prevalent disease.1–4 Validated algorithms have been developed for many disease conditions that require the occurrence of some combination of diagnosis codes associated with inpatient or outpatient care.2,5 Typically, diagnosis codes associated with inpatient care represent strong evidence of the presence of disease or indicate greater disease severity.5 However, the increasing use of “observation stays” over the past decade clouds the distinction between inpatient and outpatient care and may affect the identification of certain disease outcomes in administrative data.
Observation stays were intended to be used to observe patients for a short period to determine appropriateness for inpatient admission, with the determination of admission or discharge taking place within 48 h.6 There is little difference with the care a patient receives in an observation or inpatient stay, and patients have been encouraged by Medicare to ask about their stay classification if they are uncertain.7 Depending on the length, severity, and discharge status, observation stays can either be cost-saving or cost-prohibitive to patients, hospitals, and payers.8–12 Increasing numbers of Medicare patients have been placed into observation care, particularly after the introduction of the Recovery Audit Contractor program (RAC) in 2003.13 The RAC reassesses inpatient admissions to determine under and overpayments to hospitals on the basis of appropriateness of inpatient admissions. Between 2005 and 2008 and in 2011 alone, $900m and $939.3m were redistributed, respectively.13 Thus, the establishment of the RAC program gave hospitals a strong incentive to use observation stays, and recent studies have shown a sharp increase in the number of observation stays and length of these stays since the establishment of this program.8,11,14
To date, information about observation stays in the commercially insured is sparse. Use of observation stays has been observed in the Medicare population, and thus, it is likely that patients with commercial insurance are hospitalized under observation care as well.8,11,14 If not properly accounted for, patients under observation stay may represent misclassified hospitalized cases introducing bias into treatment effect estimates when hospitalization is used as part of an outcome or exposure definition. This bias may manifest itself in pharmacoepidemiologic research by a decrease in hospitalized cases associated to a drug exposure, causing the drug to appear less harmful, when exposed patients were in fact hospitalized under a different nomenclature, an observation stay. We therefore aimed to assess the extent to which observation care may be used in place of inpatient admissions among patients with commercial insurance. Specifically, we aimed to determine monthly trends in the prevalence of observation stays and the causes of the observation stays and to compare the prevalence and causes of observation stays and short inpatient admissions.
METHODS
Data source and study population
We examined 10 years of data from the Truven Health Analytics MarketScan® Commercial Claims and Encounters and Medicare Supplemental databases (2002–2011). These combined databases contain information from a large population of patients with employer-provided insurance residing in all 50 states and the District of Columbia. The MarketScan databases capture person-specific clinical utilization, expenditures, and enrollment across inpatient, outpatient, prescription drug, and carve-out services from a wide selection of employer-sponsored health plans. In 2011, the databases contained data on approximately 60 million covered lives.15
Definition of observation and short inpatient stays
To identify observation stays, we examined claims in the outpatient setting and identified observation stays on the basis of codes defined by the Centers for Medicare and Medicaid Services and publicly available policy definitions of two private insurers.6,16,17 We defined short inpatient admissions as any inpatient admission with a length of stay (LOS) of ≤2days or a difference between admission and discharge dates of ≤2 days. LOS for observation stays was determined by summing sequential days with an observation stay code. In addition, observation stays with the code 99 217 were counted as a LOS of 2 days, because of insurers not paying for a single day under this code. Additional details on applicable codes and rules are presented in Table S1.
Study variables
We used the 2014 multi-level Healthcare Cost and Utilization Project Clinical Classification Software (CCS) to group the primary diagnoses of the administrative claims into meaningful diagnostic categories.18 CCS uses International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes to create 18 Level 1 categories. The additional four levels of the CCS category are based on a hierarchical system and are similar to major diagnostic categories, totaling 728 distinct conditions. CCS Level 1 categories for “Complications of pregnancy, childbirth, and the puerperium”, “Congenital anomalies”, and “Certain conditions originating in the perinatal period” were jointly analyzed as pregnancy-related conditions. Additional variables included in our analyses were sex, region of the USA where the service occurred, employee geographic location, and age group (<18, 18–34, 35–44, 45–54, 55–64, 65 years and older).
Data analysis
The number of eligible enrollees per month was calculated as the aggregated number of enrolled person days per month using only enrollees with a valid unique identifier. Rates of observation stays, short inpatient, and all inpatient admissions are reported per 10 000 enrollees. Patients with >1 stay/admission in a month were counted as separate observations. We computed overall, yearly and monthly rates of observation stays, short inpatient admissions and inpatient admissions regardless of duration. Rates were also subset by age group, gender, and meaningful diagnostic categories.
Demographics and meaningful diagnostic categories are expressed as number (percent) or mean (standard deviation) aggregated for the entire study period unless otherwise specified. To identify the most common diagnostic categories, we report CCS Level 1 categories accounting for >5% of all stays (observation and inpatient) and subcategories accounting for >1% of all stays. Data analyses were performed with SAS 9.3 (SAS Institute, Cary, NC).
RESULTS
Overall, between 2002 and 2011, there were 5 355 752 observation stays (15.2 per 10 000 enrollees), 11 170 980 short inpatient stays (31.8 per 10 000 enrollees), and 23 837 349 inpatient stays regardless of duration (67.9 per 10 000 enrollees). Basic demographic information of patients in both observation and short inpatient stays are presented in Table I. Observation stay patients tended to be older than short inpatient stay patients, and services were rendered in different regions of the USA. Both groups were predominantly female. The mean LOS of observation stay admissions was 1.4 (0.6) days with the majority (67.6%) having a 1 day LOS. Only 3% of patients had a LOS greater than 2 days. An inpatient admission was found in the preceding 30 days for 17.6% of observation stays, 6.0% occurred on the same day as an observation stay, and 14.5% of patients were hospitalized within 30 days of observation stay discharge.
Table 1.
Basic demographics of observation and short inpatient* stays (2002–2011)
| Observation | Short inpatient | |
|---|---|---|
| N | 5 355 752 | 11 170 980 |
| Female n (%) | 3 333 211 (62.2) | 6 827 031 (61.1) |
| Region n (%) | ||
| Northeast | 475 925 (8.9) | 1 395 548 (12.5) |
| North Central | 1 749 106 (32.7) | 3 091 150 (27.7) |
| South | 2 435 459 (45.5) | 4 496 685 (40.3) |
| West | 629 998 (11.8) | 2 076 422 (18.6) |
| Unknown | 65 262 (1.2) | 111 175 (1.0) |
| Age (years) | ||
| Mean (sd) | 47.13 (21.8) | 42.53 (25.0) |
| Group n (%) | ||
| ≤17 | 490 200 (9.2) | 1 947 374 (17.4) |
| 18–34 | 1 115 000 (20.8) | 2 321 053 (20.8) |
| 35–44 | 725 886 (13.6) | 1 367 523 (12.2) |
| 45–54 | 930 353 (17.4) | 1 557 914 (14.0) |
| 55–64 | 997 458 (18.6) | 1 799 601 (16.1) |
| 65 and older | 1 096 843 (20.5) | 2 177 515 (19.5) |
| Length of stay | ||
| Mean (SD) | 1.4 (0.6) | |
| 1 day n (%) | 3 619 461 (67.6) | 5 217 215 (46.7) |
| 2 days n (%) | 1 576 232 (29.4) | 5 953 765 (53.3) |
| >2 days n (%) | 160 059 (3.0) | NA |
| Inpatient admission | 943 609 (17.6) | |
| −30 days n (%)† | ||
| Inpatient admission | 774 302 (14.5) | |
| +30 days n (%)† |
Short inpatient stays are defined as inpatient admission with length of stay ≤2 days; region: US region where service took place.
Inpatient admission occurred within ±30 days of observation stay admission or discharge.
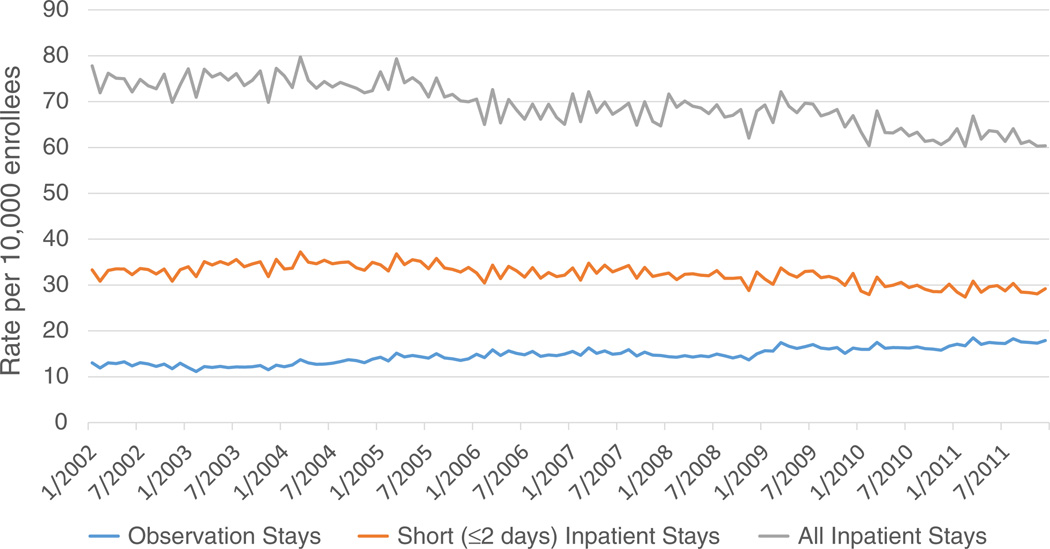
Graphical representation of monthly trends for observation, short inpatient, and all inpatient stays are presented in Figure 1. The inpatient admission rate per 10 000 enrollees decreased from 74.1 in 2002 to 60.4 in December of 2011. The short inpatient admission rate per 10 000 enrollees also decreased from 32.8 in 2002 to 29.2 in December of 2011. In contrast, the observation stay rate per 10 000 enrollees increased from 12.7 in 2002 to 17.9 in December of 2011.
Figure 1.
Trends of observation stays and inpatient admissions (2002–2011)
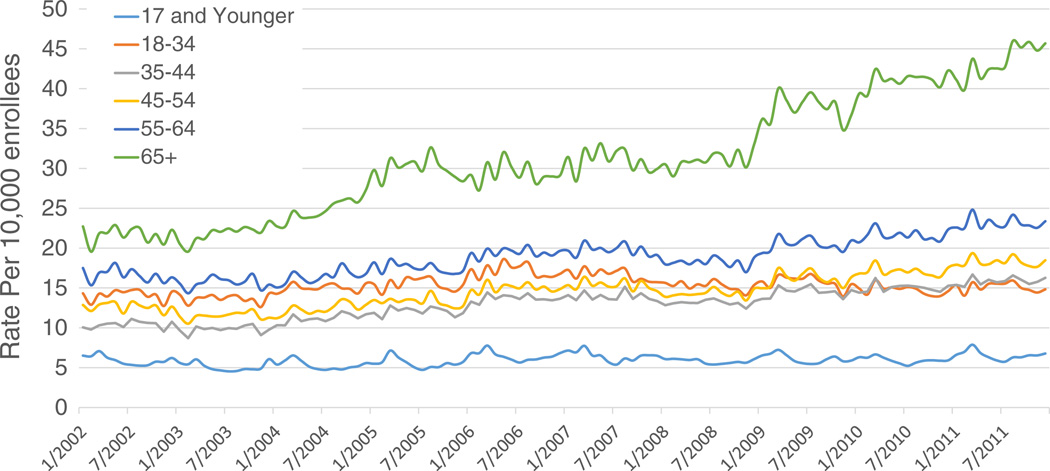
Observation stay rates by age group are presented in Figure 2, with these rates stratified by sex available in Figure S1a for women and S1b for men. The aggregate rate of observation stays per 10 000 enrollees was 15.2 (women 18.2; men 12.0) for the entire study period (2002–2011). Patients aged 65 years and older appeared to have the greatest increase in observation stay rate during the study period, particularly after 2009, with rates in all other age groups ≥35 years also appearing to increase. The rates of observation stays were generally higher for women, although the age group trends appeared similar.
Figure 2.
Trends in observation stays per 10 000 enrollees by age group (2002–2011)
Diagnostic categories based on Level 1 CCS categories representing >5% of all observation stays are presented in bold in Table II. Similar information for short inpatient stays is presented in Table III. Diseases of the circulatory system and pregnancy were the most commonly reported diagnostic categories for both observation and inpatient stays. Diseases of the digestive system were the third most common category for both types of stays. To further investigate the cause for stays, we examined the more detailed, lower level CCS categories (Tables II and III). These categories are displayed without bold emphasis and had to represent >1% of all stays for inclusion. Nonspecific chest pain was the most common category under diseases of the circulatory system for both observation stays (17.3%) and short inpatient stays (3.5%). Coronary atherosclerosis and atrial fibrillation also occurred more than 1% of the time for both observation and short inpatient stays.
Table 2.
Observation stays—most common meaningful diagnostic categories* (2002–2011)
| N | % | |
|---|---|---|
| Diseases of the circulatory system | 1 587 377 | 29.7 |
| Nonspecific chest pain | 927 647 | 17.3 |
| Coronary atherosclerosis | 123 487 | 2.3 |
| Atrial fibrillation | 60 314 | 1.1 |
| Pregnancy† | 776 319 | 14.5 |
| Diseases of the digestive system | 479 598 | 9.0 |
| Symptoms, signs, and ill-defined conditions and factors influencing health status | 477 966 | 9.0 |
| Abdominal pain | 198 388 | 3.7 |
| Syncope | 132 345 | 2.5 |
| Nausea and vomiting | 55 030 | 1.0 |
| Diseases of the genitourinary system | 315 248 | 5.9 |
| Injury and poisoning | 313 708 | 5.9 |
| Disease of the respiratory system | 307 935 | 5.8 |
| Other and unspecified lower respiratory disease | 59 568 | 1.1 |
| Also accounting for >1% of all stays | ||
| Hypovolemia | 70 700 | 1.3 |
Higher order meaningful diagnostic categories accounting for >5% of all observation stays are reported in bold; lower order meaningful diagnostic categories accounting for >1% of all observation stays are reported without bold emphasis.
ICD-9 are converted to meaningful diagnostic categories using the 2014 multi-level Healthcare cost and Utilization Project Clinical Classification Software.
Pregnancy-related conditions include meaningful diagnostic categories “Complications of pregnancy, childbirth, and the puerperium”, “Congenital anomalies”, and “Certain conditions originating in the perinatal period”.
Table 3.
| N | % | |
|---|---|---|
| Pregnancy | 3 148 084 | 28.2 |
| Diseases of the circulatory system | 1 968 707 | 17.6 |
| Nonspecific chest pain | 388 344 | 3.5 |
| Coronary atherosclerosis | 371 601 | 3.3 |
| Acute myocardial infarction | 155 461 | 1.4 |
| Atrial fibrillation | 150 087 | 1.3 |
| Disease of the digestive system | 1 029 525 | 9.2 |
| Acute appendicitis without abscess or peritonitis | 140 762 | 1.3 |
| Diseases of the genitourinary system | 749 572 | 6.7 |
| Prolapse of female genital organs | 117 461 | 1.1 |
| Diseases of the musculoskeletal system and connective tissue | 718 144 | 6.4 |
| Intervertebral disc disorders | 225 403 | 2.0 |
| Osteoarthritis; localized | 162 987 | 1.5 |
| Injury and poisoning | 669 189 | 6.0 |
| Diseases of the respiratory system | 627 785 | 5.6 |
| Pneumonia; organism unspecified | 163 594 | 1.5 |
| Neoplasms | 608 533 | 5.5 |
| Benign neoplasm of uterus | 166 871 | 1.5 |
Short inpatient stays are defined as inpatient admissions with a length of stay ≤2 days; higher order meaningful diagnostic categories accounting for >5% of all observation stays are reported in bold; lower order meaningful diagnostic categories accounting for >1% of all observation stays are reported without bold emphasis.
ICD-9 are converted to meaningful diagnostic categories using the 2014 multi-level Healthcare cost and Utilization Project Clinical Classification Software.
Pregnancy-related conditions include meaningful diagnostic categories “Complications of pregnancy, childbirth, and the puerperium”, “Congenital anomalies”, and “Certain conditions originating in the perinatal period”.
To graphically represent how the use of observation stays changed over the study period, we display rates for both observation stays and short inpatient stays of a condition which we hypothesized would not change (Pregnancy) and the three most common relevant medical conditions based on level 1 CCS categories (circulatory disorders, digestive system disorders, and ill-defined symptoms). Monthly rates are stratified by sex and presented in Figure S2. Pregnancy is presented in panel A. For both observation and short inpatient stays, there appears to be no significant change in rate of pregnancy-related stays over the entire study period. In circulatory disorders (panel B), the rate of observation stays appears to be increasing, whereas the rate of short inpatient stays are decreasing during the study period with the rate of observation stays exceeding short inpatient stays between 2009 and 2010. A convergence appears to also be replicated in digestive disorders (panel C) and ill-defined symptoms (panel D); however, observation stays did not exceed short inpatient admissions. This gradual convergence was also found when comparing three additional CCS categories (genitourinary disorders, injury and poisoning, and respiratory disease) (data not shown).
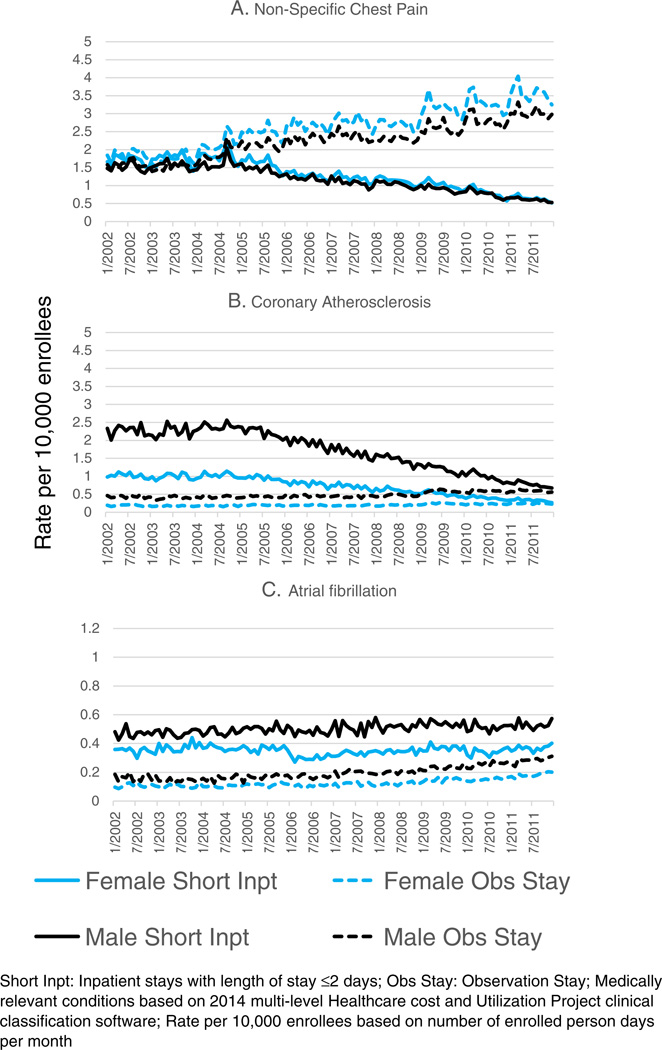
To further investigate the change and eventual predominance of observation stays in circulatory diseases, we graphically compared the three most prevalent lower level CCS categories (nonspecific chest pain, coronary atherosclerosis and atrial fibrillation), presented in Figure 3. In nonspecific chest pain (panel A), the rates of observation and inpatient stays are similar at the beginning of the study period with a sharp divergence in 2004, where the rate of observation stays increase and the rate of short inpatient stays decrease in a linear fashion. Similarly, the use of observation stays appears to be increasing for coronary atherosclerosis, whereas short inpatient stays decrease (panel B). In contrast, the rates of atrial fibrillation observation stays and short inpatient stays increased over the study period (panel C).
Figure 3.
Trends of medically relevant circulatory disorders for observation and short inpatient stays by sex (2002–2011)
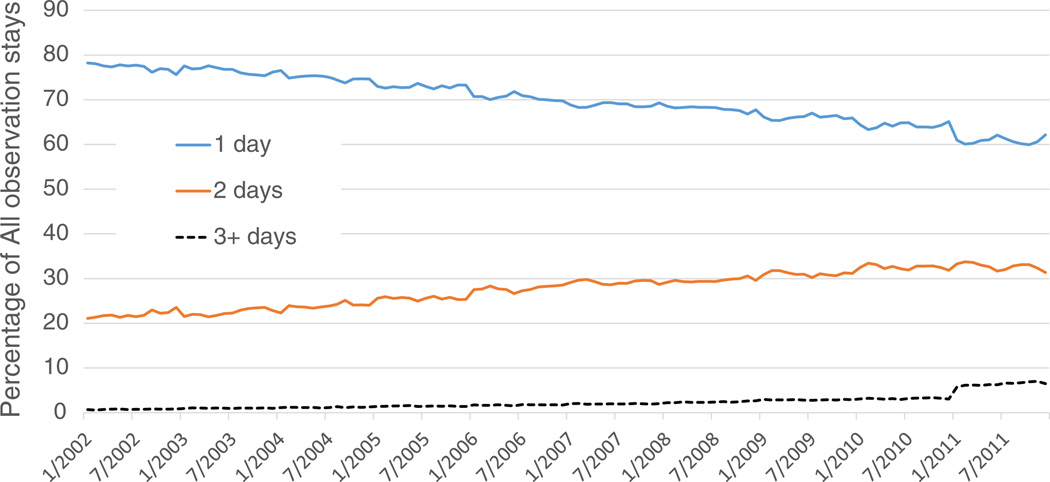
The percentage of observation stays based on LOS is presented in Figure 4. Patients with 1 day LOS appear to decrease over the study period with increases in 2 and >2 days LOS. The sharpest increase in LOS >2 days occurred in 2011 with the increase persisting for the entire year. The most common lower level diagnostic categories for subjects with observation stays >2 days were syncope (5.2%) and nausea and vomiting (4.7%) (Table S2). Using the geographic location of the health plan, the greatest percentage of all observation stays occurred in Texas (13.4%), with Illinois (7.2%), Ohio (7.1%), Michigan (6.1%), Georgia (5.4%), and California (5.2%) all also representing >5% of all observation stays (Table S3).
Figure 4.
Percentage of total observation stays by length of stay (2002–2011)
DISCUSSION
We observed an increase in the use of observation care and a corresponding decrease in the prevalence of inpatient admissions in a population of patients with commercial insurance. The rate of decrease in short inpatient stays was similar to that of the increases in observation stays. Excluding pregnancy-related conditions, the most common reasons for short inpatient and observation stays were diseases of the circulatory system. This shift from short inpatient to observation stays represents potential challenges for researchers using administrative claims data. On the basis of our data and study period and using a conventional approach to identify hospitalizations, over five million events would be missed.
The characteristics of patients in observation stays are similar to those in short inpatient admissions. Diseases of the circulatory system, pregnancy, and digestive system represented a substantial percentage of stays in both groups. Patients who were in observation stays for >2 days accounted for <10% of all observation stays, and less than 20% of all observation stays coincided with an inpatient admission in the 30 days pre-observation or post-observation stay. The possible shifting of readmissions (within 30 days of discharge) to observation stays to avoid financial penalties could not be measured by our study because our study ended before the initiation of the readmission policy but represented an area where further study is warranted.19 Our findings suggest that observation stays are becoming more prevalent, although we are unable to definitively determine if they were used to directly replace inpatient admissions.
Although not definitive, visual comparison of the rate of observation stays compared with inpatient stays indicates likely displacement of inpatient admissions, particularly short inpatient admissions, to observation stays. Further, there is a noticeable increase in the LOS for patients in observation stays. Observation stays were intended to be used for poorly defined conditions, such as nonspecific chest pain and ill-defined symptoms, which accounted for a quarter of all observation stays.6 A likely explanation for these shifts could be the introduction of the RAC, which produced similar effects in the Medicare population.8
The overall rate of observation stays was 15.2 per 10 000 enrollees per study period. This is a considerably lower rate than what has been reported in the Medicare fee-for-service population (116.9 per 1000 enrollees in 2009), but for both populations, chest pain was the primary reason for these types of stays.11,14 Observation stay use increased over the entire study period without one period of dramatic change, suggesting the RAC or other policies had a gradual effect on their use. However, in nonspecific chest pain, it appears that in August of 2004, an event caused a shift of patients with this condition to observation rather than inpatient care. In one tertiary medical center, 41% of all observation stays were in those younger than 65 years of age, and 30.3% were in patients with commercial insurance.20 Therefore, observation stays are likely more prevalent in the general populace than previously reported.
The rationale for both observation stays and short inpatient stays is similar, particularly in conditions related to the circulatory system. The growing use of observation stays with fewer inpatient stays suggest that observation stays are replacing short inpatient stays for some conditions. The changes in use of observation stays for nonspecific chest pain offer the strongest argument for this replacement. On the basis of these findings, it is our belief that many of the observation stays would have been inpatient admissions in earlier years. This shift would lead to an under-ascertainment of hospitalized cases, which is most problematic for studies that use hospitalization as an outcome or an exposure and for studies examining the prevalence of hospitalizations or hospital-acquired conditions over time. Selection bias may occur if observation stays are not appropriately accounted for, and further study should be undertaken to determine how to classify observation stays in the context of observational research. Although Marketscan is not fully nationally representative, Texas, having nearly double the number of observation stays as Illinois (the state with the second highest frequency of observation stays), likely indicates that the use of observation stays differs by geographic region. Current research has found hospital specific characteristics that increased the use of observation stays in the Medicare population, with our results suggesting that geographic location may be a contributing factor in the commercially insured population.21,22 Development of methods to account for observation stays is particularly important with the recent Centers for Medicare and Medicaid Services policy to classify all inpatient admissions fewer than 2 days as observation stays.11,23,24 One possible methodologic solution may be the utilization of sensitivity analyses in studies that use hospitalizations for case or outcome definitions.
The findings of our study should be viewed in light of its limitations and strengths. Our results are based on patients in the Marketscan databases and may not be generalizable to the entire commercially insured or general population. Our sample also only included patients with supplemental Medicare insurance. We did not have Medicare claims data on these individuals nor are these individuals representative of the entire Medicare population. It is also possible that not all observation stays were coded as such in the claims data because the rate of reimbursement for outpatient and observation stays is the same.11 However, we created a robust definition for observation stays using three publicly available definitions. We were also unable to determine the time of hospital admission and discharge, which may have led to some imprecision in our LOS calculations because we were unable to determine the number of hours spent in observation. Despite these limitations, our study provides a comprehensive look at the use and duration of observation stays for patients included in the Marketscan database and provides insight into how observation stays may affect studies using administrative claims databases.
In conclusion, we found that observation stays are increasingly used in patients with commercial insurance and supplemental Medicare insurance. Our results suggest that for patients presenting with certain conditions, observation stays may now be used in place of standard hospital admissions. This could potentially affect the ascertainment of disease conditions in studies using administrative healthcare data and introduce bias into treatment effect estimates that use hospitalization to define cases or outcomes. Further research is needed to better understand how to handle the growing use of observations stays when conducting analyses with administrative claims data.
KEY POINTS.
This is the first attempt to quantify the possible under-ascertainment of hospitalized cases in administrative claims for the commercially insured.
Greater than five million observation stays were found in the 10 years at study (2002–2011), with the rate of observation stays increasing throughout the study period, whereas the rate of inpatient stays decreased.
There was no change in the use of observation stays over time for pregnancy-related conditions. There was an increase in observation stays for circulatory disorders, specifically nonspecific chest pain.
The patient characteristics of short inpatient and observation stays are similar. The most common reason for observation stays (nonspecific chest pain) was also the third most common reason for short inpatient stays. As such, researchers should be aware of this phenomenon when analyzing administrative claims.
ACKNOWLEDGEMENTS
J. K. F. receives funding from the National Institutes of Health, Patient Centered Outcomes Research Institute, Amgen, and the Duke Endowment. M. A.B receives investigator- initiated research funding from the National Institutes of Health (R01 AG042845, R21 HD080214, and R01 AG023178) and through contracts with the Agency for Healthcare Research and Quality’s DEcIDE program and the Patient Centered Outcomes Research Institute. He has received consulting fees from RxAnte, Inc. and World Health Information Science Consultants, LLC. X. L. is a recipient of the unrestrictive Amgen Pre-doctoral Fellowship in Pharmacoepidemiology.
CONFLICT OF INTEREST
M. A. B has sat on advisory boards for Amgen, Merck, and Pfizer (honoraria received by institution).
Footnotes
ETHICS STATEMENT
This study was approved by the University of North Carolina at Chapel Hill Institutional Review Board.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Robert Overman had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Overman, Freburger, and Brookhart were responsible for the study conception and design for this paper; Overman for the acquisition of data; and Overman, Freburger, Assimon, Li, and Brookhart for the analysis and interpretation of data.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article at the publisher’s web site.
REFERENCES
- 1.Lauffenburger JC, Balasubramanian A, Farley JF, et al. Completeness of prescription information in US commercial claims databases. Pharmacoepidemiol Drug Saf. 2013;22:899–906. doi: 10.1002/pds.3458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carnahan RM, Moores KG. Mini-sentinel’s systematic reviews of validated methods for identifying health outcomes using administrative and claims data: methods and lessons learned. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):82–89. doi: 10.1002/pds.2321. [DOI] [PubMed] [Google Scholar]
- 3.Jensen PN, Johnson K, Floyd J, Heckbert SR, Carnahan R, Dublin S. A systematic review of validated methods for identifying atrial fibrillation using administrative data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):141–147. doi: 10.1002/pds.2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saczynski JS, Andrade SE, Harrold LR, et al. A systematic review of validated methods for identifying heart failure using administrative data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):129–140. doi: 10.1002/pds.2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare and Medicaid Services. Chapter 4—part B hospital (including inpatient hospital part B and OPPS) [09 December 2013];2013 Jun; Report No.: 100–04 Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c04.pdf.
- 7.Centers for Medicare and Medicaid Services. Washington DC: 2011. [18 December 2013]. Are you a hospital inpatient or outpatient? If you have Medicare—ask! Centers for Medicare and Medicaid Services. Report No.: CMS Product No. 11435 Available at: http://www.medicare.gov/Pubs/pdf/11435.pdf. [Google Scholar]
- 8.Medicare Payment Advisory Commission. A data book: health care spending and the Medicare program. Medicare Payment Advisory Commission; Washington DC: 2013. Jun, [09 December 2013]. Available at: http://www.medpac.gov/documents/Jun13DataBookEntireReport.pdf. [Google Scholar]
- 9.Baugh CW, Schuur JD. Observation care—high-value care or a cost-shifting loophole? N Engl J Med. 2013;369:302–305. doi: 10.1056/NEJMp1304493. [DOI] [PubMed] [Google Scholar]
- 10.Ross EA, Bellamy FB. Reducing patient financial liability for hospitalizations: the physician role. J Hosp Med. 2010;5:160–162. doi: 10.1002/jhm.617. [DOI] [PubMed] [Google Scholar]
- 11.Wright S. Washington DC: United States Department of Health and Human Services, Office of Inspector General; 2013. Jul 29, [09 December 2013]. Memorandum report: hospitals’ use of observation stays and short inpatient stays for Medicare beneficiaries. Report No.: OEI-02-12-00040 Available at: http://oig.hhs.gov/oei/reports/oei-02-12-00040.pdf. [Google Scholar]
- 12.Sheehy AM, Graf BK, Gangireddy S, Formisano R, Jacobs EA. “Observation status” for hospitalized patients: implications of a proposed Medicare rules change. JAMA Intern Med. 2013;173:2004–2006. doi: 10.1001/jamainternmed.2013.9382. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Medicare and Medicaid Services. Washington DC: [09 December 2013]. Recovery auditing in the Medicare and Medicaid programs for fiscal year 2011. Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/Recovery-Audit-Program/Downloads/FY2011-Report-To-Congress.pdf. [Google Scholar]
- 14.Feng Z, Wright B, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Millwood) 2012;31:1251–1259. doi: 10.1377/hlthaff.2012.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hansen L, Chang S. White paper: health research data for the real world: the Marketscan® databases. Truven Health Analytics. 2013 [Google Scholar]
- 16.United Healthcare. Observation care evaluation and management codes policy. [09 December 2013];2013 Feb; Report No.: 2013R0115A Available at: https://www.unitedhealthcareonline.com/ccmcontent/ProviderII/UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesHtml/ReimbursementPolicies/Observ_v2013A.pdf.
- 17.Cigna. Observation care. [09 December 2013];Cigna Medical Coverage Policy. 2013 Oct; Report No.: 0411, Available at: http://appealacademy.com/wp-content/uploads/2013/11/Cigna-OBS-Coverage-2013.pdf. [Google Scholar]
- 18.Elixhauser A, Steiner C, Palmer L. U.S. Agency for Healthcare Research and Quality; 2014. [09 December 2013]. Clinical classifications software (CCS) Available at: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. [Google Scholar]
- 19.Health policy brief: Medicare hospital readmissions reduction program. [04 January 2014];Health Affairs. 2013 Nov 12; Available at: http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=102. [Google Scholar]
- 20.Sheehy AM, Graf B, Gangireddy S, et al. Hospitalized but not admitted: characteristics of patients with “observation status” at an academic medical center. JAMA Intern Med. 2013 doi: 10.1001/jamainternmed.2013.8185. [epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Venkatesh AK, Geisler BP, Gibson Chambers JJ, Baugh CW, Bohan JS, Schuur JD. Use of observation care in US emergency departments, 2001 to 2008. PLoS One. 2011;6:e24326. doi: 10.1371/journal.pone.0024326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wright B, Jung HY, Feng Z, Mor V. Trends in observation care among Medicare fee-for-service beneficiaries at critical access hospitals, 2007–2009. J Rural Health. 2013;29(Suppl 1):s1–s6. doi: 10.1111/jrh.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Span P. Two kinds of hospital patients: admitted, and not. [09 December 2013];The New York Times, New Old Age. 2013 Oct 29; Available at: http://newoldage.blogs.nytimes.com/2013/10/29/two-kinds-of-hospital-patients-admitted-and-not/ [Google Scholar]
- 24.As CMS makes another policy change, policy makers distinguish between different forms of care. ED Manag. 2013;25:109–114. [PubMed] [Google Scholar]