Abstract
Purpose: we evaluated mortality risk in relation to social vulnerability across levels of frailty among a cohort of older Japanese-American men.
Methods: in secondary analysis of the Honolulu-Asia Aging Study (HAAS), participants (n = 3,271) were aged 72–93 years at baseline. A frailty index (FI) created using 58 potential health deficits to quantify participants' frailty level at baseline, with four frailty strata: 0.0 < FI ≤ 0.1 (n = 1,074); 0.1 < FI ≤ 0.20 (n = 1,549); 0.2 < FI ≤ 0.30 (n = 472); FI > 0.3 (n = 176). Similarly, a social vulnerability index was created using 19 self-reported social deficits. Cox proportional hazard modelling was employed to estimate the impact of social vulnerability across the four levels of frailty, accounting for age, smoking, alcohol use and variation in health deficits within each frailty level.
Results: for the fittest participants, social vulnerability was associated with mortality (hazards ratio (HR) = 1.04, 95% confidence interval (CI) = 1.01, 1.07; P value = 0.008). Similarly, for those considered at risk for frailty, each social deficit was associated with a 5% increased risk of mortality. For frail individuals, the Cox regression analyses indicated that social vulnerability was not significantly associated with mortality (0.2 < FI ≤ 0.3: HR = 1.016, 95% CI = 0.98, 1.06; P value = 0.442; FI > 0.3: HR = 0.98, 95% CI = 0.93, 1.04).
Conclusions: for the fittest and at-risk HAAS participants, the accumulation of social deficits was associated with significant increases in mortality risk. For frail individuals (FI > 0.20), the estimation of mortality risk may depend more so on intrinsic factors related to their health.
Keywords: social vulnerability, frailty, frailty index, aged
Introduction
Frailty is a state of increased vulnerability for people of the same age, so that frail older adults are less able to tolerate stressors and are at increased risk for adverse outcomes, including falls, delirium and death [1]. The accumulation of deficits frailty index (FI) quantifies the health states of individuals, which can range from fitness to severe frailty [2]. It has been validated in several cohort studies and has been demonstrated to estimate mortality risk in older population-based and clinical samples [3–8].
Social risk factors can also impact health outcomes of older adults, including socioeconomic status, social supports, social engagement and mastery. Although these factors are often considered independently, prior studies have illustrated their cumulative effects [9]. Canadian studies have shown that a general measure of social vulnerability, one that combines a variety of factors into a single measure, can predict negative health outcomes including cognitive decline [10, 11] and mortality [12, 13]. While social vulnerability can distinguish levels of mortality risk in healthy older adults [13], it is unclear how social vulnerability impacts survival across degrees of frailty; it is conceivable that the effect of social vulnerability on risk of mortality may attenuate as frailty levels increase. Similar attenuation of effects with increases in frailty have also been found for metformin for older adults with type 2 diabetes [14] and when examining cardiovascular adaptations related to exercise [15].
Here, our objective is to examine the impact of social vulnerability across the continuum of fitness to frailty in data collected from the Honolulu-Asia Aging Study. In particular, we were interested to know whether social vulnerability conferred risk across all grades of frailty.
Methods
The sample of 3,271 older men was derived from the Honolulu-Asia Aging Study (HAAS). HAAS evolved from the Honolulu Heart Program that began in 1965 and follows men of Japanese descent born between 1900 and 1919 inclusive. In 1991, investigators began the HAAS focussing on conditions of ageing. A detailed overview of the methods for HAAS and Honolulu Heart Program is provided elsewhere [16].
Frailty and social vulnerability measures were developed using data from the baseline wave. The approach to developing a social vulnerability index (SVI) has been described previously [12]. For the current study, 19 items cover domains such as marital status, living situation, social supports and social engagement. Each variable was dichotomised with values of ‘1’ representing the presence of a social deficit and ‘0’ marking the absence. For each participant, the sum of social deficits was calculated and divided by the number of social deficits considered. This provides each individual with <20% missing data with a SVI score between 0 and 1, with higher scores representing higher social vulnerability. Any participant with missing values for >20% of the social deficits was assigned a null value and was excluded from the analyses. SVI Items can be found in Supplementary data, Appendix S1 available in Age and Ageing online.
An FI was developed using the standard procedure outlined in Searle and colleagues [17]. Fifty-eight variables were selected as health deficits if they were associated with health status, accumulate with age, and have prevalence >1% but <80% in the sample. Each variable was dichotomised (0 for absent; 1 for present), summed and divided by the total number of deficits considered, providing an FI score between 0 and 1. FI items can be found in Supplementary data, Appendix S2 available in Age and Ageing online.
To examine social vulnerability and mortality across levels of frailty, the HAAS participants were grouped using the following frailty groups: 0.0 < FI ≤ 0.1 (fittest; n = 1,074); 0.1 < FI ≤ 0.20 (at risk; n = 1,549); 0.2 < FI ≤ 0.30 (frail; n = 472); FI > 0.3 (frailest; n = 176). Data on date of death have been collected on 90.9% of the sample, with the longest lived individuals surviving up to 21 years from baseline.
Standard protocol approvals, registrations and patients' consents
Data collection was approved by the Kuakini Medical Center IRB, with informed consent provided by all participants. Approval for the secondary analyses came from the Research Ethics Committee of the Capital District Health Authority, Halifax, Nova Scotia, Canada.
Analyses
Descriptive analyses examined the properties of the SVI, demographic variables and lifestyle factors across the four levels of frailty at the baseline wave in 1991. To estimate the impact of social vulnerability on time to death, separate Cox regression models were developed for each grouping of frailty. Each model contained social vulnerability deficit count, health deficit count, age in years, number of pack years (cigarette smoking) and alcohol use (oz/month). Analyses were performed in the IBM SPSS Statistics 20 statistical package.
Results
At baseline, the mean age of the sample was 77.9 years (SD = 4.7; range of 72–93). The SVI mean was 0.27 (SD = 0.13) and ranged from 0 to 0.89. The distribution was skewed (skewness statistic = 0.89) with a long right tail (kurtosis statistic = 1.52). The mean FI was 0.15 (SD = 0.08; range of 0–0.57). With increasing levels of the FI, participants had greater social vulnerability, on average (Table 1) and tended to be older, have diminished cognition and report greater smoking rates and alcohol use, with lower amounts of physical exercise on average.
Table 1.
Baseline demographic and lifestyle factors stratified by FI level. Averages and standard deviations (SD)
| Fittest 0.0 < FI ≤ 0.1 (n = 1,074) |
At risk 0.1 < FI ≤ 0.20 (n = 1,549) |
Frail 0.2 < FI ≤ 0.30 (n = 472) |
Frailest FI > 0.3 (n = 176) |
|
|---|---|---|---|---|
| Age | 76.7 (4.2) | 77.5 (4.3) | 77.7 (4.4) | 79.0 (4.8) |
| Education (years) | 10.9 (3.2) | 10.6 (3.2) | 10.8 (3.2) | 10.3 (3.2) |
| SVI | 0.25 (0.13) | 0.27 (0.13) | 0.29 (0.13) | 0.33 (0.14) |
| Smoking: average pack years | 21.7 (31.0) | 26.0 (35.1) | 32.2 (35.5) | 36.7 (41.0) |
| Alcohol: average oz/month (SD) | 16.1 (32.0) | 18.5 (40.8) | 22.5 (47.5) | 21.2 (44.4) |
| Average time to death (years) | 12.6 (5.6) | 10.9 (5.7) | 9.4 (5.8) | 6.6 (4.7) |
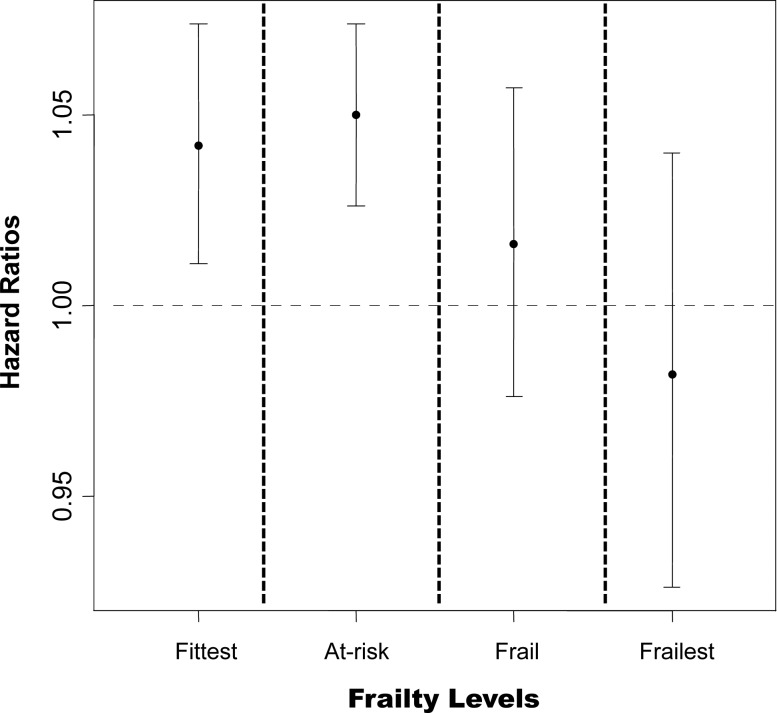
For each level of frailty, the hazard ratios (HR) for time to death from the adjusted Cox regression models are illustrated in Figure 1. After controlling for the age, smoking, alcohol use and deficit count, social vulnerability was significantly associated with mortality for the fittest participants (FI ≤ 0.10: HR = 1.04, 95% confidence interval (CI) = 1.01, 1.07; P value = 0.008) and at-risk participants (0.10 < FI ≤ 0.20: HR = 1.05, 95% CI = 1.03, 1.07; P value < 0.001). For these participants, each additional social vulnerability deficit was associated with a 5% increased risk of death after accounting for age and frailty (variation of health deficits within each frailty group). Thus, compared with a non-frail individual with no social deficits, a man with similar characteristics in age and frailty but with five additional social deficits would have a 25% higher risk of mortality. With increasing frailty, social vulnerability was not significantly associated with mortality in the adjusted models (0.2 < FI ≤ 0.3: HR = 1.016, 95% CI = 0.98, 1.06; P value = 0.370; FI > 0.3: HR = 0.98, 95% CI = 0.93, 1.04).
Figure 1.
For each level of frailty, survival curves were generated for a categorised SVI, controlling for age, health deficit count, smoking and alcohol use. Fittest: 0.0 < FI ≤ 0.1; At risk: 0.1 < FI ≤ 0.20; Frail: 0.2 < FI ≤ 0.30; Frailest: FI > 0.3.
Discussion
We found that the impact of the social vulnerability on mortality differed across frailty groups. For the fittest participants, social vulnerability was significantly associated with mortality. Each additional social deficit was associated with a 5% increased risk of death. This is in keeping with a report from the Canadian Study of Health and Aging [13] in which social vulnerability differentiated mortality risk among the fittest individuals. The outcomes of the healthiest older individuals are of considerable interest as they may provide insights into how extrinsic factors impact health and ageing. Social vulnerability was also able to discriminate mortality risk among the at-risk group (0.1 < FI ≤ 0.2), further demonstrating the impact of social deficits on health outcomes in older adults. For the frail men in the HAAS (FI > 0.20), social vulnerability was not a significant predictor of time to death. The Cox regression model indicated that the accumulation of social risk factors does not provide reliable information on mortality risk for older frail adults beyond age and degree of frailty. These findings do not discount the importance of social vulnerability in frail older adults. They do however imply that once an individual is frail, the estimation of mortality risk may depend more so on intrinsic factors related to their health.
The distribution of the SVI in the HAAS baseline wave was skewed with a long right tail. In previous population-based studies, the distribution of the SVI was a closer fit to a normal distribution [12]. This difference may be due to the fact that the HAAS consisted only of men. Previous studies using the SVI found on average lower scores for men compared with those found for women [12, 13]. This sex difference may explain the shifted and slightly skewed distribution. Sex differences in SV may also have impacted our finding that the SVI did not independently predict mortality in the frail men represented here; the importance of social vulnerability across grades of frailty can be different in women [18]. This warrants further investigation.
Our results should be interpreted with caution. The HAAS collected information using a self-report approach which can be less accurate than data retrieved clinically or through laboratory tests. Second, there were a limited number of social risk factors that could be extracted from the baseline wave. This restricted the number of variables that could be included in the SVI and may have led to a less robust measure of social vulnerability. For example, we do not have data on social support service which can reduce feelings of social isolation [19] and protect against elder abuse [20, 21]. Finally, 8.9% of participants were excluded in the analyses due to missing data. Those who were missing these indices were older and closer to death, and their exclusion from our analyses may have impacted the estimates.
Key points.
Changes in the health of individuals result from both intrinsic and extrinsic factors, such as social vulnerability.
The impact of social vulnerability on mortality differed across frailty groups.
For frail individuals, intrinsic factors influenced mortality risk more than extrinsic factors.
Conflicts of interest
None declared.
Funding
J.A. is supported by a post-doctoral fellowship award from the Alzheimer Society of Canada. A.M. is supported by an operating grant from the Canadian Institutes of Health Research. K.R. was supported by the Dalhousie Medical Research Foundation who provides career funding as the Kathryn Allen Weldon Professor of Alzheimer Research Chair. Funding bodies played no role in the design, execution, analysis, interpretation of data or writing of the study.
Supplementary data
Supplementary data mentioned in the text are available to subscribers in Age and Ageing online.
References
- 1.Clegg A, Young J, Iliffe S, Rikkert M, Rockwood K. Frailty in elderly people. Lancet (London, England) 2013; 381: 752–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Geront A-Bio Sci 2007; 62: 722–7. [DOI] [PubMed] [Google Scholar]
- 3.Mitnitski A, Song X, Skoog I, et al. Relative fitness and frailty of elderly men and women in developed countries and their relationship with mortality. J Am Geriatr Soc 2005; 53: 2184–9. [DOI] [PubMed] [Google Scholar]
- 4.Yashin AI, Arbeev KG, Kulminski A, Akushevich I, Akushevich L, Ukraintseva SV. Cumulative index of elderly disorders and its dynamic contribution to mortality and longevity. Rejuvenation Res 2007; 10: 75–86. [DOI] [PubMed] [Google Scholar]
- 5.Kulminski A, Ukraintseva S, Kulminskaya I, Arbeev KL, Yashin A. Cumulative deficits better characterize susceptibility to death in elderly people than phenotypic frailty: lessons From the cardiovascular Health Study. J Am Geriatr Soc 2008; 56: 898–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dent E, Chapman I, Howell S, Piantadosi C, Visvanathan R. Frailty and functional decline indices predict poor outcomes in hospitalised older people. Age Ageing 2014; 43: 477–84. [DOI] [PubMed] [Google Scholar]
- 7.Evans S, Sayers M, Mitnitski A, Rockwood K. The risk of adverse outcomes in hospitalized older patients in relation to a frailty index based on a comprehensive geriatric assessment. Age Ageing 2014; 43: 127–32. [DOI] [PubMed] [Google Scholar]
- 8.Krishnan M, Beck S, Havelock W, Eeles E, Hubbard R, Johansen A. Predicting outcome after hip fracture: using a frailty index to integrate comprehensive geriatric assessment results. Age Ageing 2014; 43: 122–6. [DOI] [PubMed] [Google Scholar]
- 9.Andrew M, Keefe J. Social vulnerability from a social ecology perspective: a cohort study of older adults from the National Population Health Survey of Canada. BMC Geriatrics 2014; 14: 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andrew M, Rockwood K. Social vulnerability predicts cognitive decline in a prospective cohort of older Canadians. Alzheimers Dement 2010; 6: 319,325.e1. [DOI] [PubMed] [Google Scholar]
- 11.Andrew M, Fisk J, Rockwood K. Social vulnerability and prefrontal cortical function in elderly people: a report from the Canadian study of health and aging. Int Psychogeriatr 2011; 23: 450–8. [DOI] [PubMed] [Google Scholar]
- 12.Andrew M, Mitnitski A, Rockwood K, von Elm E. Social vulnerability, frailty and mortality in elderly people. PLoS ONE 2008; 3: e2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andrew M, Mitnitski A, Kirkland S, Rockwood K. The impact of social vulnerability on the survival of the fittest older adults. Age Ageing 2012; 41: 161–5. [DOI] [PubMed] [Google Scholar]
- 14.Wang C-P, Lorenzo C, Espinoza SE. Frailty attenuates the impact of metformin on reducing mortality in older adults with type 2 diabetes. J Endocrinol Diabetes Obes 2014; 2: 1031. [PMC free article] [PubMed] [Google Scholar]
- 15.Ehsani A, Spina R, Peterson L, et al. Attenuation of cardiovascular adaptations to exercise in frail octogenarians. J Appl Physiol 2003; 95: 1781–8. [DOI] [PubMed] [Google Scholar]
- 16.White L, Petrovitch H, Ross W, et al. Prevalence of dementia in older Japanese-American men in Hawaii: the Honolulu-Asia Aging Study. J Am Med Assoc 1996; 276: 955–60. [PubMed] [Google Scholar]
- 17.Searle S, Mitnitski A, Gahbauer E, Gill T, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatrics 2008; 8: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kendig H, Browning C, Pedlow R, Wells Y, Thomas S. Health, social and lifestyle factors in entry to residential aged care: an Australian longitudinal analysis. Age Ageing 2010; 39: 342–9. [DOI] [PubMed] [Google Scholar]
- 19.Nguyen VP, Sarkari F, Macneil K, Cowan L, Rankin J. The role of support services in promoting social inclusion for the disadvantaged urban-dwelling elderly. Canad Geriatr J 2013; 16: 156–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johannesen M, LoGiudice D. Elder abuse: a systematic review of risk factors in community-dwelling elders. Age Ageing 2013; 42: 292–8. [DOI] [PubMed] [Google Scholar]
- 21.Naughton C, Drennan J, Lyons I, et al. Elder abuse and neglect in Ireland: results from a national prevalence survey. Age Ageing 2012; 41: 98–103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.