Abstract
Background: minor traumatic injuries among independent older people have received little attention to date, but increasingly the impact of such injuries is being recognised.
Objectives: we assessed the frequency and predictors of acute health care use, defined as return to the emergency department (ED) or hospitalisation.
Study design: national multicentre prospective observational study.
Setting: eight Canadian teaching EDs between April 2009 and April 2013.
Participants: a total of 1,568 patients aged 65–100 years, independent in basic activities of daily living, discharged from ED following a minor traumatic injury.
Methods: trained assessors measured baseline data including demographics, functional status, cognition, comorbidities, frailty and injury severity. We then conducted follow-up telephone interviews at 6 months to assess subsequent acute health care use. We used log-binomial regression analyses to identify predictors of acute health care use, and reported relative risks and 95% CIs.
Results: participants' mean age was 77.0, 66.4% female, and their injuries included contusions (43.5%), lacerations (25.1%) and fractures (25.4%). The cumulative rate of acute health care use by 6 months post-injury was 21.5% (95% CI: 19.0–24.3%). The strongest predictors of acute health care use within 6 months were cognitive impairment, RR = 1.6 (95% IC: 1.2–2.1) and the mechanism of injury including pedestrian struck or recreational injuries, RR = 1.6 (95% CI 1.2–2.2).
Conclusions: among independent community living older persons with a minor injury, cognitive impairment and mechanism of injury were independent risk factors for acute healthcare use. Future studies should look at whether tailored discharge planning can reduce the need for acute health care use.
Keywords: injuries, seniors, emergency department, services, outcomes
Introduction
In the USA, there were over 3 million emergency department (ED) visits for injuries among people 65 years and older in 2010, with 89% of these injuries were classified as ‘mild’ (not requiring admission or surgery) [1]. These ‘minor’ injuries are expected to double in the next two decades as the older population doubles [2]. Most seniors with minor injuries seek care in the (ED) [3], and 65–79% of these patients are discharged home [3, 4], whether arising from falls (75%), motor vehicle accidents (10%) or other causes. Up to 15–20% of these patients have limitations in mobility, daily activities [5], physical and social activities, which in turn is linked with functional decline, morbidity, mortality and institutionalisation [6].
ED visits have been identified as ‘sentinel events’—opportunities to prevent subsequent adverse outcomes among vulnerable older persons [7]. Unfortunately, this opportunity is often missed, and older patients experience a cascade of adverse outcomes, including mobility decline, institutionalisation and death [8, 9]. Seniors are often discharged without receiving optimal instructions or follow-up [10, 11]. Despite the central role of EDs in treating injured older people, there is currently no standard approach to discharge planning, and little is known about factors that predict subsequent acute health care use.
The primary objectives of the current study were to (i) describe acute healthcare use (return to the ED or hospitalisations) 3 to 6 months following minor injury among previously independent seniors following discharge from an ED and (ii) identify predictors of acute health care use within 6 months after minor injury.
Methods
Design and participants
This study was part of the Canadian Emergency Team Initiative (CETI) research programme, which aims to improve ED care for independent seniors with minor injuries [5]. In summary, we conducted a prospective observational cohort study between April 2009 and April 2013 in eight teaching EDs in six Canadian urban regions (Quebec City, Montreal, Ottawa, Toronto, Hamilton and Calgary). We included ED patients who were ≥65 years, could independently perform the seven basic activities of daily living (BADLs) from the Older American Adult Resources and Service (OARS) functional scale [12], and were discharged back to their home from the ED following a minor traumatic injury (i.e. lacerations, contusions, simple extremity fractures or minor head injury). Patients who were admitted to hospital (transferred to an inpatient ward) were excluded, as were those from long-term care facilities, unable to give consent, participate in telephone follow-up or to communicate in French or English.
Procedure
Recruitment occurred 24 h per day, 7 days per week. Treating physicians, research assistants or nurses identified potential participants and assessed eligibility in face-to-face interviews during the initial ED consultation or by telephone within 3 days post-visit. The 3- and 6-month follow-up could be conducted using either face-to-face or telephone interviews.
Baseline measurements
We chose the Andersen behavioural model as our theoretical framework to guide the selection of variables that predict acute healthcare use [13]. The Andersen model has been used most frequently to explore variations in healthcare use, and identifies three domains to explain variation in healthcare use. ‘Need’ factors assess the severity of an acute illness or injury, ‘predisposing’ factors represent the tendency of an individual to use health services and ‘enabling’ factors measure system characteristics that influence access to health services. McCusker adapted the Andersen model, noting that factors that ‘enable’ access to primary care may reduce ED use [14]. Baseline variables collected are described below, and classified as ‘Need’, ‘Predisposing’ or ‘Enabling’ factors.
Need factors
We included variables describing the injury severity, type and location. We also examined the mechanism of injuries, categorised as motor vehicle collisions, falls and pedestrian struck by vehicles or recreational injuries. ‘Pain severity’ was measured with self-reported pain intensity (0–10 on a Numeric Rating Scale).
Predisposing factors
‘Demographic and environmental variables’ included age, gender, education, living environment (e.g. house or apartment). The social support index (SSI) [15] was used to measure the quantity and satisfaction with available support. A SSI score ≥ 60.3 is consistent with high social support [15]. ‘Health variables’ included the number of prescribed medications and self-reported comorbidities. We also used the Identification of Seniors at Risk (ISAR) short screening tool, which includes six items: premorbid change in functional status, acute change in functional status, recent hospitalisation, impaired memory, impaired vision and number of daily medications [8]. ‘Mobility’ was measured using the Timed Up & Go test (TUG) [16], a widely validated measure of basic physical mobility. A slower TUG is considered a risk factor for functional decline in community-dwelling elders [17]. We also assessed mobility by measuring whether patients occasionally used mobility aids (cane or walker), the number of falls in the last 3 months and the number of times/week the person leaves his/her home [18]. ‘Functional status’ was measured with the Older American Adult Resources and Service functional scale [12]. It has been validated against physiotherapy and nursing assessments in the ED [18, 19]. ‘Cognitive status’ was measured using the Montreal Cognitive Assessment (MoCA) for in-person evaluations (30%) [20]. It is a sensitive and reliable measure of general cognitive functioning in the elderly. The modified Telephone Interview for Cognitive Status (TICS-m) was used for patient recruited by telephone (70%). The TICS-m can detect decline in cognitive function over time, and has been extensively validated in English and French against the MMSE [21]. We defined cognitive impairment as <23/30 on the MoCA [21, 22] and ≤31/50 on the TIC-S. ‘Frailty’ was measured using the Canadian Study of Health and Aging-Clinical Frailty Scale [23].
‘Enabling Factors’ included individuals’ access to non-emergency health care including having a Family Physician or other primary care access that potentially reduced the need for acute health care use [14]. The presence of stairs and living alone were also included as factors that might influence seeking of acute care.
Outcome measures
For our primary outcome, self-reported hospitalisations and returns to the ED in the previous 3 months were recorded either in person or during telephone interviews at 3 and 6 months.
Data analyses
Simple descriptive univariate analyses were used to describe the sample. As the prevalence of outcome was >10% [24], multivariable log-binomial regression analyses, with a Poisson distribution approach, were used to estimate relative risks (RR) with 95% confidence intervals (CI) [25]. As described above, we included the following variables for consideration in the model: ‘predisposing covariates’ (age, comorbidities, cognitive impairment, OARS score, number of medications, ISAR variables, previous ED use); ‘need covariates’ (pain severity, fracture, comorbidities); ‘enabling covariates’ (lives alone, access to Family Physician, stairs at home). As there were no statistically significant variations between hospitals for acute care use, accounting for cluster effects due to hospitals was not required. All analyses were conducted using the SAS software V 9.3. (SAS Institute, Cary, NC, USA).
Sample size, power and precision of estimate
For our primary outcome, the rate of acute health care use by 6 months, we calculated that given an actual event rate of 15 to 25%, a sample size of 1,500 would produce a confidence interval width of 2% or less. For our log-binomial regression model, we estimated that given a sample of 1,500 subjects and an event rate of 20%, we would have 300 outcomes, allowing for 30 potential predictive variables to be included in the predictive model.
Results
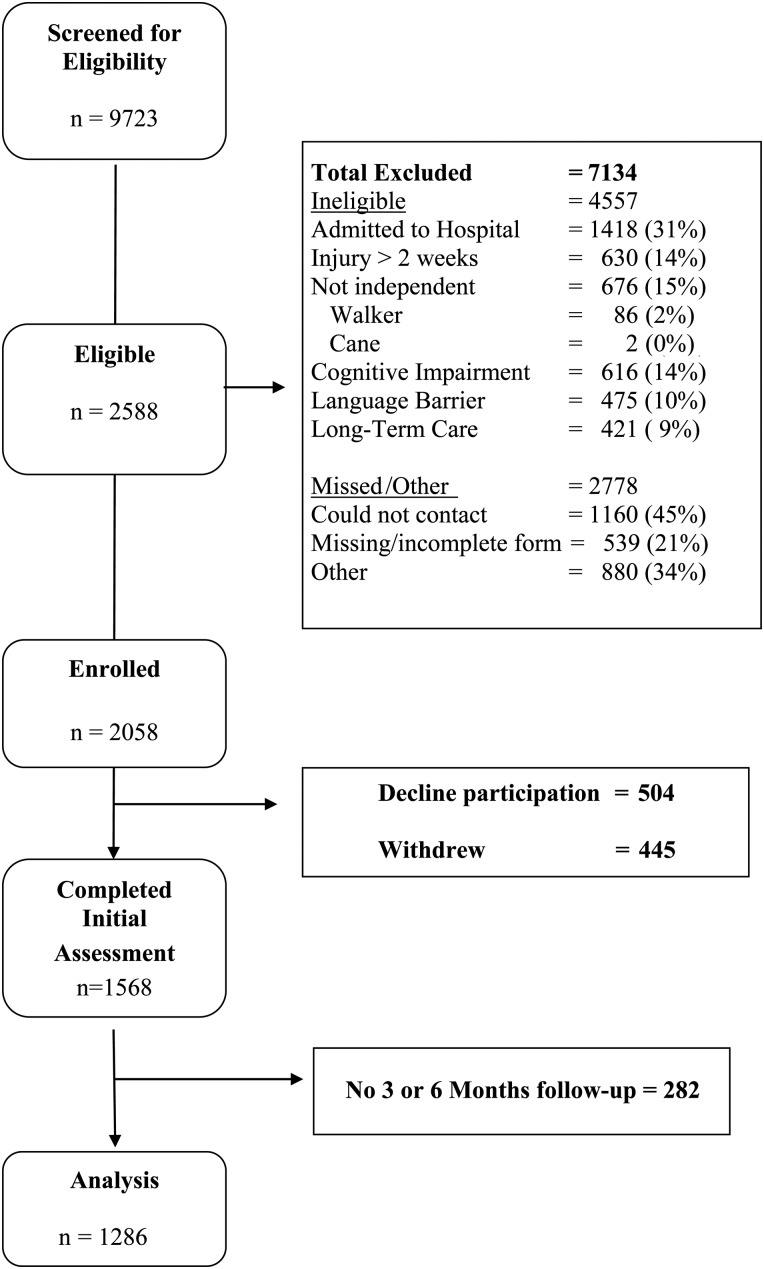
We recruited a total of 1,568 participants of whom 1,219 (77.7%) could be reached for the 3-month evaluation and an additional 67 were reached for the 6-month evaluation for a total of 1,286 subjects that were included in the analysis (see Figure 1). The 282 subjects, who were lost to follow-up were more likely to have cognitive impairment (MoCA < 23/30 or TICS < 32/50: 42.4 versus 28.3%, P < 0.001) at baseline compared with participants with complete follow-up, were less likely to complete grade 12 education (31.9 versus 43.7%, P < 0.01), were less likely to have 5 or more comorbidities (31.1 versus 43.3% P < 0.001), but were similar on a large number of other characteristics (see Supplementary data, Table S1 available in Age and Ageing online).
Figure 1.
Study flow chart.
Nearly two-thirds of patients (59.5%) presented during a day shift (08:00–16:00), 31.5% presented during an evening shift (16:00–24:00) and 9.0% at night (00:00–08:00). We enrolled 1,098 (70.0%) of the cohort using telephone interviews. Mean age of participants was 77.0 years and 34.0% were men. All participants met our definition of independence pre-injury on the OARS and Service BADL sub-scale. Baseline scores on the OARS Instrumental ADL sub-scale ranged from 4 to 14/14 (see Table 1).
Table 1.
Selected baseline characteristics of independent older participants discharged home from the emergency department following minor injuries (n = 1568)
| Characteristics of participants | na (%) |
|---|---|
| Age | |
| 65–74 | 655 (41.8%) |
| 75–84 | 637 (40.7%) |
| 85+ | 273 (17.5%) |
| Men | 526 (33.6%) |
| Number of comorbidities | |
| 0–1 | 207 (13.2%) |
| 2–4 | 711 (45.4%) |
| 5–19 | 647 (43.9%) |
| Lives alone | 574 (36.8%) |
| In the last 3 months: | |
| >3 general practitioner visits | 236 (15.1%) |
| Emergency department visits | 297 (18.9%) |
| Hospitalised | 64 (4.1%) |
| Timed-Up-Go ≥ 15 s | 251 (16.0%) |
| Identification of Seniors At Risk (ISAR) ≥ 2/6 | 451 (28.8%) |
| Cognitive impairment (MoCAb score < 23/30 or TICSc < 32/50) | 474 (30.2%) |
| Details of injury | |
| Mechanism of injury | |
| Falls from own height | 968 (63.6%) |
| Falls from higher than own height | 197 (12.6%) |
| Motor vehicle collision | 70 (4.6%) |
| Pedestrian struck, recreational injury | 286 (18.8%) |
| Type of injury | |
| Mild traumatic brain injury | 287 (18.3%) |
| Contusions | 681 (43.5%) |
| Lacerations | 393 (24.1%) |
| Sprains | 212 (13.5%) |
| Fractures | 399 (25.5%) |
| Pain level ≥ 7/10 | 224 (14.4%) |
aBecause of missing data, the number of patients does not always add to the total.
bMontréal Cognitive Assessment.
cTelephone Interview for Cognitive Status.
Acute healthcare use: return to the ED or hospitalisation
Of the 1,286 patients with 6-month follow-up, 1,008 (78.4%) had no acute care use, 182 (14.2%) had a single acute care use and 96 subjects (7.5%) had two or more encounters (range 0–10, with one individual having 8 visits and one individual with 10 visits in 6 months; see Supplementary data, Table S1 available in Age and Ageing online). Thus, 278 subjects (21.6%, 95% CI: 19.0–24.3%) had a total of 448 acute care encounters within 6 months.
Predictors of return to the ED or hospitalisation
Our multivariable analysis revealed two factors that were predictive of return visits to the ED following minor injuries: (i) cognitive impairment (relative risk, 1.6, 95% CI, 1.2–2.1); and (ii) the mechanism of injury, specifically pedestrians struck by a vehicle or recreational accidents (relative risk 1.6, 95% CI, 1.2–2.2).
Discussion
In this study, we found a total of 22% of previously independent seniors assessed in the ED for minor injuries had acute health care use within 6 months of discharge. While 92.5% of this cohort had a single or no visits, there was a minority of 96 individuals (7.5%) who required a total of 260 recurrent ED visits or hospitalisations. Thus, 7.5% of the cohort accounted for 59.0% of all the acute care encounters within 6 months. This finding that a small subsample of independent older individuals required the majority of healthcare services re-enforces the potential importance of screening for high-risk individuals who may require preventive interventions. It also suggests the hypothesis that these high-risk individuals were frailer.
The definition and measurement of frailty is controversial despite over two decades of debate in the geriatric literature [26, 27]. A recent Delphi process involving over 150 experts in frailty research found no consensus on a definition, despite consensus about the validity of frailty as a concept [27]. The discussion about the validity of frailty is less advanced within Emergency Medicine [28]. Thus, we chose the 7-point Canadian Study of Health and Aging-Clinical Frailty Scale global assessment of frailty, due to its ease of use and intrinsic face validity. Using this measure, we found a trend for patients with higher frailty to have an increased risk of acute healthcare use, although this was not statistically significant in our multivariable model (see Table 2). This finding should be explored in future studies which are specifically powered to detect the impact of frailty on acute healthcare use.
Table 2.
Adjusted relative risk of univariate association of variables with total acute health care use, plus final multivariable model
| Variables | Total acute care use Adjusted RR with 95% CI |
Reference value (Relative risk = 1.0) |
|---|---|---|
| Female | 0.88 (0.65–1.18) | Male |
| Age 75–84 years | 0.99 (0.74–1.32) | Age 65–74 |
| Age 85+ | 0.97 (0.66–1.42) | |
| 2–4 Comorbidities | 1.46 (0.91–2.34) | 0–1 |
| 5 and more comorbidities | 1.56 (0.96–2.54) | |
| Social Support Index (SSI) <63 | 1.23 (0.91–1.68) | ≥63 |
| ‘Have you needed more help than usual in the last 24 h’ Yes | 0.91 (0.69–1.22) | No |
| ‘Have you been hospitalised for one or more night during the past 6 months?’ No | 1.00 (0.63–1.57) | Yes |
| ‘In general, do you have serious problems with your vision that cannot be corrected by glasses?’ Yes | 0.93 (0.65–1.34) | No |
| ED visits in the last 3 months: No | 1.20 (0.81–1.77) | Yes |
| Frailty Score 2–3: ‘well’ to ‘well with comorbidities’ | 1.14 (0.78–1.66) | Very fit (1) |
| Frailty Score 4–6: ‘apparently vulnerable’ to ‘moderately frail’ | 1.47 (0.94–2.31) | |
| MoCA < 23 or TICS < 31: Yes | 1.58 (1.20–2.08)* | No |
| Falls efficacy scale: ≥ 9.8 | 1.04 (0.79–1.37) | <9.8 |
| No falls in the last 3 months | 0.97 (0.70–1.35) | 1 or more falls |
| Pain: <7/10 | 1.06 (0.74–1.50) | Pain ≥7/100 |
| Mechanism: falls from greater than own height | 1.01 (0.65–1.59) | Falls from own height |
| Motor vehicle collision | 1.57 (0.88–2.80) | |
| Pedestrian struck or recreational injury (e.g. skiing, cycling) | 1.56 (1.13–2.16)* | |
| Contusion: Yes | 1.01 (0.77–1.32) | No contusion |
| Sprain: Yes | 1.09 (0.74–1.60) | No sprain |
| Laceration: Yes | 0.87 (0.63–1.22) | No laceration |
| Fracture: Yes | 1.13 (0.82–1.56) | No fracture |
| Concussion: Yes | 0.97 (0.66–1.42) | No |
| Live alone: Yes | 1.12 (0.85–1.46) | Live alone: No |
| General practitioner visits in the last 3 months: ≥3 | 1.30 (0.88–1.91) | <3 Visits |
Retained in final multivariable model.
Two variables best predicted return to the ED or hospitalisation: cognitive impairment, as defined by MoCA < 23/30 or TICS-m < 32/51, and mechanism of injury, specifically pedestrians struck or recreational injuries. Of note, these two factors independently predicted acute health care use better than other factors expected to predict ED use such as comorbidities, severity of injury or previous ED use [13].
Few studies have examined the rate of acute health care use among independent older people treated for an injury. McCusker reviewed 14 studies of ED use by older adults [14]. Previous ED use, comorbidities, self-perceived poor health, depression and the ISAR screening tool were independent predictors of ED use [14]. However, cognitive impairment was not identified as a predictor of return ED visits by any previous studies in this review [14]. One possible explanation for this is the fact that cognitive impairment was frequently an exclusion criterion in previous studies. Thus, our findings suggest that patients with mild cognitive impairment, who may not have been included in previous studies, are at increased risk for acute health care use.
Hustey et al. found that only 28–38% of patients with cognitive impairment were recognised by Emergency Physicians [29]. Given this known low rate of recognition of cognitive impairment, it is likely that cognitive impairment was unrecognised by treating emergency physicians in our study as well, although this was not specifically measured. Thus, our findings highlight the potential importance of unrecognised mild cognitive impairment both clinically and in a research context.
Pedestrians struck or older people injured in recreational activities, such as cycling or skiing, were also at increased risk for acute health care use—more so than patients with falls or those injured in motor vehicle collisions. Thus, further studies should attempt to replicate our findings about the impact of these types of injuries on acute health care use.
Strengths and limitations
Major strengths of this study include its multicentre prospective design and recruitment 24 h a day, 7 days a week. Our literature review found no other multicentre studies of the consequences of minor injuries on healthcare use among older ED patients. In addition, we used the MoCA and the TICS-M to measure cognitive impairment instead of the MMSE. Studies have shown that the MoCA is a more sensitive measure of mild cognitive impairment compared with the MMSE [30]. However, we used the TICS for the 70% of patients who were enrolled by telephone. Despite the use of two different measures, cognitive impairment remained a significant predictor of repeat acute health care use. This may be explained by the fact we used previously validated cut-off scores for both the TICS and MoCA, to reduce the risk of misclassification.
The major limitation of this study was the use of patient recall to determine repeat use of ED services. Previous studies have shown that patients underestimate repeat ED use compared with objective measures and it is possible that the true acute health care use rate may be underestimated in our study.
A selection bias may have occurred in the study as patients lost to follow-up had lower cognitive levels, education and comorbidities than participants at baseline. This may have resulted in an underestimation of the true incidence of repeat use of acute care services.
Interpretation of results and clinical implications
Our findings contribute to the body of literature suggesting that clinicians need to be more vigilant in identifying older patients with mild cognitive impairment, particularly among older patients who appear fit.
Our data also suggest that patients with mild cognitive impairment or high-risk mechanisms of injury (pedestrian struck or injured in recreational activities) may benefit from targeted discharge instructions or follow-up to potential avoid acute health care use.
Conclusion
We found that among previously independent seniors, 22% of ED patients with a minor injury will return to the ED or be hospitalised within 6 months. Patients who returned to the ED were more likely to have cognitive impairment or to have been injured in recreational activities or have been a pedestrian struck by a vehicle. Whether discharge instructions have the potential to prevent return ED use in this population should be examined in future research.
Key points.
The impacts of minor traumatic injuries in independent older people, including functional decline, are increasingly being recognised.
We found that 21.6% of participants returned to the ED or were hospitalised within 6 months, and 7.5% accounted for 59% of acute healthcare use.
Participants with cognitive impairment, struck by a vehicle or injured in a recreational activity, had higher rates of acute healthcare use.
Future research should assess whether discharge instructions or management protocols can prevent return ED use in this population.
Supplementary data
Supplementary data mentioned in the text is available to subscribers in Age and Ageing online.
Funding
We acknowledge the Canadian Institutes of Health Research for funding this study through their emerging team grant in mobility in ageing (CIHR-91752).
Supplementary Material
Acknowledgements
We acknowledge all emergency and research professionals who participate in the study at the participating centres.
References
- 1.Villaveces A, Mutter R, Owens PL et al. Causes of Injuries Treated in the Emergency Department, 2010: Statistical Brief #156. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD), 2013. [PubMed]
- 2.Canada S. Population Projections for Canada, Provinces and Territories 2009 to 2036. Ottawa: Statistics Canada Demography Division, 2010. [Google Scholar]
- 3.Scott V, Pearce M, Pengelly C. Technical report: Injury resulting from falls among Canadians age 65 and over. On the analysis of data from the Canadian Community Health Survey, Cycle 2.1 as presented in Report on senior’ falls in Canada. Ottawa: Public Health Agency of Canada, 2005. [Google Scholar]
- 4.Canadian Institute for Health Information (CIHI). Pyramids of Injury in Ontario Toronto, ON. 2003. http://www.cihi.ca/cihiweb/en/downloads/bl_otrmar2003_e.pdf (16 September 2014, date last accessed).
- 5.Sirois MJ, Emond M, Ouellet MC et al. Cumulative incidence of functional decline after minor injuries in previously independent older Canadian individuals in the emergency department. J Am Geriatr Soc 2013; 61: 1661–8. [DOI] [PubMed] [Google Scholar]
- 6.Gill T, Allore H, Guo Z. Restricted activity and functional decline among community-living older persons. Arch Intern Med 2003; 163: 1317–22. [DOI] [PubMed] [Google Scholar]
- 7.Bernstein E. Repeat visits by elder emergency department patients: sentinel events. Acad Emerg Med 1997; 4: 538–9. [DOI] [PubMed] [Google Scholar]
- 8.McCusker J, Bellavance F, Cardin S et al. Detection of older people at increased risk of adverse health outcomes after an emergency visit: the ISAR screening tool. J Am Geriatr Soc 1999; 47: 1229–37. [DOI] [PubMed] [Google Scholar]
- 9.Wilber ST, Blanda M, Gerson LW. Does functional decline prompt emergency department visits and admission in older patients? Acad Emerg Med 2006; 13: 680–2. [DOI] [PubMed] [Google Scholar]
- 10.Miller E, Wightman E, Rumbolt K et al. Management of fall-related injuries in the elderly: a retrospective chart review of patients presenting to the emergency department of a community-based teaching hospital. Physiother Can 2009; 61: 26–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salter AE, Khan KM, Donaldson MG et al. Community-dwelling seniors who present to the emergency department with a fall do not receive Guideline care and their fall risk profile worsens significantly: a 6-month prospective study. Osteoporos Int 2006; 17: 672–83. [DOI] [PubMed] [Google Scholar]
- 12.George LK, Fillenbaum GG. OARS methodology. A decade of experience in geriatric assessment. J Am Geriatr Soc 1985; 33: 607–15. [DOI] [PubMed] [Google Scholar]
- 13.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 1995; 36: 1–10. [PubMed] [Google Scholar]
- 14.McCusker J, Karp I, Cardin S et al. Determinants of emergency department visits by older adults: a systematic review. Acad Emerg Med 2003; 10: 1362–70. [DOI] [PubMed] [Google Scholar]
- 15.Audet N, Lemieux M, Cardin J. Enquête sociale et de santé 1998-Cahier technique et méthodologique: Définitions et composition des indices, Montréal, Québec 2001.
- 16.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991; 39: 142–8. [DOI] [PubMed] [Google Scholar]
- 17.Stuck AE, Walthert JM, Nikolaus T et al. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med 1999; 48: 445–69. [DOI] [PubMed] [Google Scholar]
- 18.Canadian Study of Health and Aging Working Group. Canadian study of health and aging: study methods and prevalence of dementia. Can Med Assoc J 1994; 150: 899–913. [PMC free article] [PubMed] [Google Scholar]
- 19.McCusker J, Bellavance F, Cardin S et al. Validity of an activities of daily living questionnaire among older patients in the emergency department. J Clin Epidemiol 1999; 52: 1023–30. [DOI] [PubMed] [Google Scholar]
- 20.Nasreddine ZS, Phillips NA, Bedirian V et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005; 53: 695–9. [DOI] [PubMed] [Google Scholar]
- 21.Knopman DS, Roberts RO, Geda YE et al. Validation of the telephone interview for cognitive status-modified in subjects with normal cognition, mild cognitive impairment, or dementia. Neuroepidemiology 2010; 34: 34–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luis CA, Keegan AP, Mullan M. Cross validation of the Montreal Cognitive Assessment in community dwelling older adults residing in the Southeastern US. Int J Geriatric Psychiatry 2009; 24: 197–201. [DOI] [PubMed] [Google Scholar]
- 23.Rockwood K, Song X, MacKnight C et al. A global clinical measure of fitness and frailty in elderly people. Can Med Assoc J 2005; 173: 489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davies HT, Crombie IK, Tavakoli M. When can odds ratios mislead? Br Med J 1998; 316: 989–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004; 159: 702–6. [DOI] [PubMed] [Google Scholar]
- 26.Rockwood K, Fox RA, Stolee P et al. Frailty in elderly people: an evolving concept. Can Med Assoc J 1994; 150: 489–95. [PMC free article] [PubMed] [Google Scholar]
- 27.Rodriguez-Manas L, Feart C, Mann G et al. Searching for an operational definition of frailty: a Delphi method based consensus statement: the frailty operative definition-consensus conference project. J Gerontol A Biol Sci Med Sci 2013; 68: 62–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldstein JP, Andrew MK, Travers A. Frailty in older adults using pre-hospital care and the emergency department: a narrative review. Can Geriatr J 2012; 15: 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hustey FM, Meldon SW, Smith MD et al. The effect of mental status screening on the care of elderly emergency department patients. Ann Emerg Med 2003; 41: 678–84. [DOI] [PubMed] [Google Scholar]
- 30.Alagiakrishnan K, Zhao N, Mereu L et al. Montreal Cognitive Assessment is superior to Standardized Mini-Mental Status Exam in detecting mild cognitive impairment in the middle-aged and elderly patients with type 2 diabetes mellitus. BioMed Res Int 2013; 2013: 186106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.