Abstract
Three studies (N = 545) investigated the effects of social comparison on a type of heuristic called “absent-exempt” (AE; feeling exempt from future risk). Study 1 examined how comparison with an infected peer (comparison target) who was similar or non-similar in terms of sexual risk (number of partners, lack of condom use), influenced willingness and intentions to engage in sex without a condom and conditional perceived vulnerability to a sexually transmitted disease (STD). Participants generally reported lower willingness and higher conditional vulnerability if they compared with a similar-risk level target. However, high-risk students who compared with a low-risk comparison target engaged in what appeared to be AE thinking, reporting the highest willingness and lowest conditional vulnerability. Intentions to have sex without a condom were not influenced. Study 2 included a direct measure of AE thinking, and compared the impact of a low-risk comparison target with a Public Service Announcement (PSA) stating that negative outcomes (e.g., STDs) can happen even to low-risk targets. Among high-risk participants, comparing with the low-risk target led to an increase in AE thinking. As expected, the effects in Studies 1 and 2 were strongest among participants high in tendencies to socially compare. Study 3 explored whether AE thinking could be decreased by encouraging more reasoned processing. Results indicated that asking participants to think about the illogicality of AE thinking reduces AE endorsement and increases STD testing intentions. Findings suggest that comparison-based information can have a stronger influence on health cognitions than analytic-based information (e.g., most PSAs). Implications for dual-processing models of decision-making and their applicability to interventions and health messages are discussed.
Keywords: Absent-exempt, social comparison, dual-processing, health messages, prototype-willingness model
Social psychologists and medical researchers are increasingly realizing the value of using social psychological theories to explain, predict, and potentially change health cognitions and behaviors (Clark & Janevic, 2014; Klein, Shepperd, Suls, Rothman, & Croyle, 2014). One theory in particular, social comparison (Festinger, 1954), has been shown to play an important role in influencing both health cognitions and health behavior (Buunk & Gibbons, 1997; Klein & Cerully, 2007). Social comparison theory suggests that individuals are motivated to evaluate their personal attributes (e.g., risk behavior) and their situations (e.g., “how at-risk am I”) by comparing themselves with others. This is particularly true when objective standards are unavailable, as is the case with many risky health behaviors. Although individuals have some control over which comparisons they make and how they construct these comparison opportunities, the process of comparison can be automatic--simply seeing or hearing a comparison target can trigger a comparison and influence subsequent cognitions and behavior (Langer, Pirson, & Delizonna, 2010; Mussweiler & Bodenhausen, 2002).
Media and health messages often involve social comparison targets: peers suffering from a disease or some other negative health consequences (e.g., sexually transmitted disease [STD]; Rothman, Kelly, Weinstein, & O'Leary, 1999; Winterbottom, Bekker, Conner, & Mooney, 2008). Moreover, although these messages sometimes include peers who have engaged in high levels of risk behavior, they also frequently include peers who have suffered a negative consequence (e.g., contracted an STD or had an unwanted pregnancy) even though they have engaged in low levels of risk behavior (e.g., sex with just one partner; Falchuk, 2009; Gulati, 2012; Idaho Department of Health & Welfare, 2014). The assumption has been that realizing someone has experienced negative effects, in spite of low risk behavior, will scare the audience into increasing their risk perceptions and decreasing their risk behavior. But, how will participants respond to this “it only takes once” message if they have already engaged in the behavior repeatedly without any consequences (cf. Weinstein, Rothman, & Nicolich, 1998)? That is the question we examined in this research.
Social Comparison Theory, Similarity, and Risk Cognitions
When asked to think about their own risk level, individuals commonly report some kind of comparative optimism, i.e., view themselves as relatively invulnerable to negative events (Shepperd, Klein, Waters, & Weinstein, 2013). These biased perceptions of vulnerability can result in increases in risky behavior (Mayhew et al., 2014). In contrast, perceptions of vulnerability to negative health outcomes and health-protective behaviors are usually heightened when people learn that similar others have experienced misfortune (Gerend, Aiken, West, & Erchull, 2004; Rothman et al., 1999; Weinstein & Klein, 1995). For example, Rimal and Morrison (2006) manipulated similarity (e.g., age, gender, ethnicity), and found that optimistic bias for multiple risk events was highest when students compared with a dissimilar other, but was eliminated when comparing with a similar other. In another study, students watched an HIV prevention video that included HIV-positive interviewees who were similar to them in terms of age, appearance, sexual history, and sexual orientation. One month later, perceived vulnerability and condom use had increased (Fisher, Fisher, Misovich, Kimble, & Malloy, 1996). In this case, seeing a comparison target who was perceived to be similar and had experienced negative consequences due to their risk behavior appeared to have health-related benefits. Finally, Gump and Kulik (1995) found that students exposed to a HIV positive (versus negative or unknown) peer rated this individual as less similar to themselves and lowered the perceived risk of their own HIV-relevant traits. Thus, the effects of social comparison targets on perceived vulnerability depend, to a large extent, on how similar the targets are thought to be (Buunk & Ybema, 1997; Thornton, Gibbons, & Gerrard, 2002).
Absent-Exempt Endorsement
Most adolescents decrease their perceived vulnerability to risk behaviors (e.g., STDs) over time, but the amount of decrease is larger for those who are engaging in the behavior (Millstein & Halpern-Felsher, 2001; Morrell, Song, & Halpern-Felsher, 2010). For example, the more young adults drive after drinking, the lower their perceived likelihood of getting arrested for a DUI or getting in an accident (Gibbons et al., 2002). Even if the likelihood of a negative consequence is fairly low, multiple experiences with the risk behavior over time without consequence can result in even lower perceived vulnerability (Brown, 2005; Jacobs & Ganzel, 1993), and an increase in risky behavior (e.g., sex without condoms; Crosby, Yarber, & Kanu, 1998). Thus, some individuals who have engaged in risky behavior but have not (yet) experienced any negative consequences tend to believe they are immune from risk in the future. Weinstein (1982; 1987; 1989) has labeled this form of optimistic bias “absent-exempt” (AE). He suggests this perception may put these individuals at an even greater risk of suffering harmful consequences, especially for behaviors, such as sex, that they can potentially engage in repeatedly without apparent negative consequences (Albert & Steinberg, 2011; Harris, Griffin, & Murray 2008; Weinstein & Klein, 1995).
In spite of its potential significance, there have been very few studies conducted on AE endorsement. One study looked at AE in relation to breast cancer (Gerend et al., 2004). Although risk actually increases with age, older women were more likely than younger women to endorse feelings of AE (“If a woman my age has not gotten breast cancer by now, she is unlikely to in the future”) (Gerend et al., 2004). AE endorsement was also associated with lower perceived vulnerability to osteoporosis and coronary heart disease in the same sample. Moreover, similarity to others with the disease was associated with increased perceived vulnerability and decreased AE endorsement. The authors concluded that interventions should target similarities between those with the disease and intervention participants without the disease. Walsh, Stock, Peterson, and Gerrard (2013) found that AE beliefs related to skin cancer were associated with lower perceived vulnerability and less sunscreen use. In addition, older women who were given information on their UV damage and told to focus on their affective versus cognitive reactions were more likely to report AE beliefs. From a dual-processing perspective, this suggests AE thinking, similar to optimistic biases, may involve heuristic-based more than reasoned or analytic thinking. In addition, these previous studies suggest that endorsement of AE may be associated with increasing risk cognitions, including lower perceptions of vulnerability. Finally, although social comparison processes are not necessary for AE thinking to occur, we suspect they do affect the AE heuristic--just as comparisons can impact general risk perceptions.
Dual Processing, Health Decisions, and AE
Dual-processing models of decision making include two distinct types of information processing: one based more on affect and heuristics, the other more on reason and planning (Evans, 2008; Reyna & Rivers, 2008; Stanovich & Toplak, 2012). Within this context, researchers have recently begun to view social comparison as a more heuristic-based self-evaluation process (Corcoran & Mussweiler, 2009; Mussweiler, Rüter, & Epstude, 2004). However, relatively few researchers have examined social-cognitive factors that influence these two distinct routes of decision-making as they relate to health decisions (Hofmann, Friese, & Wiers, 2008; Reyna & Rivers, 2008). One modified dual-processing model that has been applied to both health decision making and social comparison is the prototype/willingness model (Gerrard, Gibbons, Houlihan, Stock, & Pomery, 2008; Gibbons, Gerrard, & Lane, 2003; Gibbons, Gerrard, Stock, & Finneran, in press).
The prototype/willingness model
The prototype/willingness model posits two pathways to health behavior. The reasoned path involves processing that is more analytic and includes behavioral intentions (intentions) as the proximal antecedent to behavior. This path reflects postulates from expectancy-value models (e.g., Theory of Planned Behavior, Ajzen, 1991) that young adults sometimes engage in risky (or health-promoting) behaviors because they have made a conscious decision ahead of time to do so. The social reaction path captures the more reactive/social element that is characteristic of many risk behaviors (Reyna & Farley, 2006). It involves more heuristic processing, and includes behavioral willingness (willingness) as the proximal antecedent. Willingness is defined as an openness to risk opportunity. A central tenet of the model is that not all health risk behaviors are intentional or reasoned; instead, they are often unplanned reactions to different circumstances. That is especially true among adolescents and young adults (cf. Reyna & Farley, 2006; Webb & Sheeran, 2006). However, while willingness to engage in a risk behavior can be impulsive and is often associated with less consideration of consequences (risk), the social reaction pathway is not necessarily automatic nor does it operate at a completely unconscious level (Gibbons, Kingsbury, & Gerrard, 2011; Gibbons et al., in press). Previous research has demonstrated that willingness (in addition to intentions) effectively predicts engagement in many risk behaviors (Blanton et al., 2001; Gerrard et al., 2006; 2008; Houlihan et al., 2008; Zimmermann, & Sieverding, 2010). Like other dual-processing models, the prototype/willingness model maintains that people engage in both analytic and heuristic processing (Boyer, 2006; Stanovich, Sá & West, 2004), sometimes simultaneously (Banks & Hope, 2014; Klaczynski, 2001; Sloman, 1996).
AE, social comparison, and willingness vs. intentions
Intentions are generally better than willingness at predicting health-promoting behaviors, such as getting tested for an STD or eating healthy, which are usually planned or premeditated (Dohnke, Steinhilber, & Fuchs, 2014; Gibbons et al., in press). Willingness, on the other hand, tends to be better at predicting health-impairing behaviors, such as substance use or risky sex (e.g., Gerrard et al., 2008; Gibbons et al., 2004; in press). Once again, that is especially true among younger people, and also those who have less experience with the behavior (Gerrard et al., 2008; Gibbons et al., 2003; Pomery, Gibbons, Reis-Bergan, & Gerrard, 2009). The model suggests that because willingness involves less reasoned, more heuristic processing, it is more likely than intentions to be altered by affect, as well as social factors, such as social influence or risk images (prototypes) and social comparison (Gibbons et al., 2004; Gibbons, Houlihan, & Gerrard, 2009; Lane, Gibbons, O'Hara, & Gerrard, 2011; Todd, Kothe, Mullan, & Monds, 2014). According to the model, both general (i.e., same age peers) and specific (i.e., exemplars or individualized comparison targets) risk images have an impact on willingness through the process of social comparison. A recent meta-analysis on constructs within the prototype/willingness model found that risk images are better predictors of health-impairing (vs. protective) behaviors and that perceived similarity to a risk engager is an important predictor of willingness (van Lettow et al., 2014). Thus, it is anticipated that the process of social comparison with a peer (e.g., someone who has experienced a negative outcome due to risk behavior) would be more likely to affect the social reaction path (willingness to engage in a health-impairing behavior) than the reasoned path (intention to engage in a health-impairing behavior) (Gibbons, et al., 2003; Lane et al., 2011). Because AE thinking is a type of heuristic and is influenced by images and affect (Gerend et al., 2004; Walsh, et al., 2013), the model provides an ideal framework for examining AE processes, especially as they pertain to risky sex behavior.
Conditional perceived vulnerability
Like most health behavior theories, the prototype/willingness model includes a perceived risk component. Most previous studies examining the impact of health messages have used absolute perceived vulnerability measures (e.g. “What is the likelihood that you will contract an STD?”). A problem with this type of measure, however, is that it confounds intentions with vulnerability: those not intending to engage in the risk behavior typically (and logically) report they are not at risk (Gibbons, Lane, Gerrard, Pomery & Lautrup, 2002; Weinstein et al., 1998). For this reason, the prototype/willingness model includes conditional perceived vulnerability measures as a precursor to willingness. These measures ask participants what their personal risk would be if they were to engage in the behavior. A negative relation between conditional vulnerability and willingness has been found in several studies: The more people think they will not suffer negative consequences, the more willing they are to engage in the risk behavior (Gerrard et al., 2008). In addition, like willingness, conditional vulnerability is influenced by social factors (Gerrard et al, 2008). However, the current study is the first to examine changes in conditional perceived vulnerability as a mediator of the relation between social factors (e.g., comparison targets) and changes in willingness to engage in a risk behavior. We propose that lower conditional vulnerability and higher willingness in response to socially-based risk information are elements of AE thinking that involve primarily the social-reaction pathway of the prototype/willingness model.
Moderation of AE Thinking: Social Comparison Orientation
The prototype/willingness model also maintains that prototypes influence behavior through a social comparison process. For example, Gibbons and Gerrard (1995) reported that risk images (prototypes) had more impact for high (frequent) social comparers than for low social comparers. This propensity to engage in social comparisons is referred to as social comparison orientation (SCO), and is assessed by the Iowa Netherlands Comparison Orientation Measure (INCOM; Gibbons & Buunk, 1999). For example, using the INCOM, Litt and colleagues found that the relation between perceived substance use norms and substance use consequences and both willingness to use and subsequent use was greater for adolescents high in SCO (Litt et al., 2012; 2014). More generally, individual differences in the tendency to compare are associated with the degree of sensitivity to the attitudes and behaviors of peers and prototypes; those with higher comparison tendencies are more influenced by comparison information or targets (Buunk, Dijkstra, Bosch, Dijkstra, & Barelds, 2012; Buunk & Gibbons, 2006; 2007). Because personal perceptions of risk (e.g., conditional vulnerability and AE endorsement) can be impacted by the process of social comparison, it should be more prevalent among those who are high in SCO.
Overview
The present studies had three goals: (a) explore the AE heuristic, specifically in relation to risky sexual behaviors; (b) examine the impact of social comparison targets on the risk cognitions (including AE thinking) of college students; and (c) expand on the role of social comparison processes in dual-processing models of health decision-making, in particular, the prototype/willingness model. As mentioned earlier, although studies have shown that comparisons play an important role in risk perceptions (e.g., Klein, 2003), researchers have rarely examined the impact of prompting the comparison process (with peer-based messages) while taking into account the past risk behavior of both the comparison target and the audience member. For the purpose of the present studies, past risk behavior is based on number of sexual partners and lack of condom use. These sexual risk behaviors are common among college students (Dermen & Thomas, 2011) and contribute to the likelihood of an STD infection (Centers for Disease Control, 2014; Mayo Clinic, 2014).
Study 1 examined how social comparison with a peer who has suffered a negative consequence (contracted an STD) after engaging in either high or low levels of previous sexual risk behavior, affects elements of AE thinking: willingness (more than intentions) to have sex without a condom and conditional vulnerability, of participants who have also engaged in either relatively high or low levels of risk behavior. Study 2 compared the impact of a low-risk target with a Public Service Announcement (PSA). This study also included a direct measure of AE thinking and an indirect measure: time spent reading information on genital herpes. The two studies also examined whether SCO moderates the anticipated interaction between the social comparison targets and the participants' own past sexual risk behavior. Finally, Study 3 explored whether AE thinking could be decreased among high-risk participants by encouraging more reasoned processing.
Study 1: Social comparison, conditional vulnerability, and risky sex willingness
Study 1 used a Condition (low-risk target vs. high-risk target) X Participant Risk level (continuous) X SCO (continuous) design. We hypothesized the following: a) Low-risk participants would report higher conditional vulnerability to STDs and lower willingness to engage in sex without a condom after comparing with a low-risk (similar) but infected target versus a high-risk (dissimilar) infected target, and b) high-risk participants who compare with the low-risk target would engage in AE thinking, reflected in reports of lower conditional vulnerability and higher willingness than high-risk participants who compare with the high-risk target. It was also expected that this condition by participant risk interaction would be moderated by SCO—i.e., be stronger among participants higher in comparison tendencies. Finally, we predicted that AE thinking would be more evident on willingness to have risky sex than intentions to do so, reflecting the fact that social (comparison) information should have more of an impact on reactions to willingness than intentions to engage in risk behavior.
Method
Participants
College students who reported in a mass pre-study data collection session that they have had unprotected sex, were not married, and had never been diagnosed with an STD were recruited for a study on health attitudes and behaviors. A total of 173 participated in the lab-based portion of the study (approximately 2-10 weeks later). The sample was 98% White; it included 68 males, the mean age was 21 (range = 18-25). For all three studies, participants were recruited through the psychology research subject pool and participated in exchange for course credit. All studies were approved by the university's Institutional Review Board.
Experimental procedure
When participants arrived at the lab, they were told that the study involved an examination of reactions to health problems and impressions of peers experiencing these problems. They were informed that they would hear another student discuss a recently diagnosed health problem. Prior to hearing the audiotape, participants completed a questionnaire about their sexual behaviors (used for the sexual risk measure) along with filler items. Next, the students were randomly assigned to hear a recording depicting a high-risk or low-risk same-sex comparison target who reported that he or she had genital herpes. In the high-risk comparison condition (n = 85), the target reported having five sexual partners and using less protection than the average student1. In the low-risk condition (n = 88), the target reported having had only one partner and using protection most of the time. To evoke general similarity, the target mentioned similar demographic characteristics as the participant (age, gender, college). Participants then read a paragraph telling them what genital herpes is and completed a questionnaire assessing conditional perceived vulnerability, willingness and intentions to engage in sex without a condom, and manipulation checks. The experimenter then probed for suspicion and debriefed the participants.
Measures
The most common measures of risky sexual behavior are total number of partners and (lack of) condom use (e.g., Devarakonda et al., 2014; Pflieger, Cook, Niccolai, & Connell, 2013). Consequently, all relevant dependent variables in Studies 1 and 2 included measures related to unprotected sex with both steady and casual partners. For all three studies, the following definitions were provided to participants: sex = vaginal or anal sexual intercourse; steady partner = committed, ongoing, dating relationship; casual partner = someone you're not exclusively dating or recently met, not a serious or steady relationship. For all studies, Time 1 (T1) refers to pre-manipulation measures and Time 2 (T2) refers to post-manipulation measures.
Social comparison orientation (T1)
SCO was assessed with the INCOM (Gibbons & Buunk, 1999), which includes 11 items (e.g., “I often compare how I am doing socially with other people” (1 = disagree strongly, 5 = agree strongly; α = .82). The scores were standardized.
Participant sexual risk (T1)
Sexual risk was assessed with two open-ended questions: “How many steady [casual] partners have you had in your lifetime?” and “How often have you used a condom in these steady [casual] relationships?” (1 = never; 7 = all the time, reverse coded). Risk was computed by multiplying the number of steady and casual partners by the frequency of condom use (Gerrard & Warner, 1994; van der Velde, van der Pligt, & Hooykaas, 1994; Wu et al., 2005). Due to the skewed number of partner reports, these scores were log transformed and standardized.
Willingness (T1, T2)
At T1, willingness to engage in sex without a condom was assessed with two items (e.g., Gibbons et al., 1998b). For a casual partner, participants were asked: “suppose you are at a party….you start talking with a man/woman whom you find very attractive and are enjoying hanging out with….but you do not have a condom with you. How willing would you be to… have sex without a condom…have sex and use withdrawal” (1 = not at all willing; 7 = very willing). At T2, willingness with a steady partner was assessed also with the following: “suppose you are on a date with your boy/girlfriend and you want to have sexual intercourse, but neither of you has a condom,” followed by the same items and scale used with casual sex. The two items at T1 (r = .72) and the four items at T2 (α = .81) were averaged.
Intentions (T1, T2)
At T1, participants indicated on a 7-point scale (1= strongly disagree; 7 = strongly agree) how much they intended to “have sex with a casual partner without a condom in the next six months.” At T2, participants were also asked whether they intended to “have sex with a steady partner without a condom in the next 6 months” (r = .43).
Conditional vulnerability (T1, T2)
The two vulnerability items were: “If you were to have sex with a [casual/steady] partner without a condom, what do you think the chances are that you would get an STD?” (1= very likely; 7 = not at all likely; T1 r = .35, T2 r = .34).
Manipulation checks (T2)
Participants were asked: “how many sexual partners did the student on the tape mention;” “how often did the student use a condom” (1 = never; 7 = all of the time); and “how risky do you believe the student's behavior to be” (1 = not at all; 7 = very).
Control variables (T1)
All analyses controlled for gender, the corresponding T1 cognitions (i.e., willingness, conditional vulnerability, and intention), and relationship status (1 = single to 7 = very serious/steady).
Results
Participants reported an average of 3.5 sexual partners (lifetime): 2 steady partners and 1.5 casual partners. Thirty-five percent reported having only one partner, whereas 20% reported having 5 or more partners; 50% reported at least 1 casual partner and 24% reported having 3 or more steady partners. Twenty-six percent reported being single; 33% reported being in a serious/steady relationship. When asked how often they had sex without a condom, participants averaged 4.5 on a 7-point scale (7 = all the time). These numbers reflect a fairly high level of risk among some of the participants, which is typical for US college students (Chandra, Mosher, & Copen, 2011; U.S. Department of Health and Human Services and CDC, 2009).
GLM ANOVAs revealed no differences between target conditions in SCO levels, or in T1 intentions, willingness, and conditional vulnerability (ps > .10). Correlations and means are presented in Table 1. As expected, willingness was negatively correlated with conditional vulnerability (p < .001). Participant risk level was positively correlated with willingness and intentions (ps < .01); and willingness and intentions were moderately correlated (rs = .42, .50). Males reported greater willingness to have sex without a condom, whereas females reported greater tendencies to socially compare (ps < .01). Participants who listened to the low-risk target tape reported that the target had more frequent condom use and lower levels of risky behavior than did participants in the high-risk target condition (both ps < .001). All participants correctly answered how many sexual partners the student mentioned.
Table 1. Study 1 Correlations and Means.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. T1 Conditional vulnerability | - | ||||||||
| 2. T1 Willingness | -.37*** | - | |||||||
| 3. T1 Intentions | -.37*** | .42*** | - | ||||||
| 4. T2 Conditional vulnerability | .56*** | -.37*** | -.19* | - | |||||
| 5. T2 Willingness | -.50*** | .43*** | .63*** | -.29*** | - | ||||
| 6. T2 Intentions | -.23** | .65*** | .58*** | -.19* | .50*** | - | |||
| 7. SCO | -0.06 | -0.01 | -0.03 | -0.11 | -0.09 | -0.13 | - | ||
| 8. Participant risk | -0.13 | .40*** | .34*** | -0.15 | .23** | .39*** | -0.04 | - | |
| 9. Gender | -.33*** | .48*** | .22** | -.31*** | .29*** | .26*** | -.20** | 0.01 | - |
|
| |||||||||
| Mean | 4.25 | 2.1 | 1.81 | 4.59 | 2.61 | 2.34 | 3.47 | 0.79 | - |
| SD | 1 | 1.21 | 1.44 | 0.88 | 1.31 | 1.32 | 0.55 | 0.44 | - |
| Range | 1.5-6.5 | 1-7 | 1-6.5 | 2.25-6.5 | 1-6.5 | 1-5.67 | 1-5 | 0-1.92 | - |
Note. N = 173;
p < .05,
p < .01,
p < .001.
Gender coded (0 = female, 1 = male). SCO indicates Social Comparison Orientation.
Effect of participant and target risk on health cognitions
To take advantage of the continuous nature of SCO and participant risk level, hierarchical multiple regression analyses were used to examine the hypothesized interaction between Participant Risk level and Condition (coded 0 = low risk target, 1 = high risk target), as well as the anticipated SCO moderation of this interaction on all risk cognitions. When an anticipated Participant Risk by Condition interaction was revealed, simple slope analyses examined the impact of Condition on the risk cognitions for low- versus high-risk (+/-1 SD) participants. In addition, when the anticipated 3-way interaction was observed, additional regression analyses were conducted separately for high and low (+/-1 SD) comparers and then simple slopes were calculated. Participant risk status was log-transformed and all continuous variables were centered in the regression models (Aiken & West, 1991). For Study 1 and 2, all regressions controlled for: gender, relationship status, and corresponding T1 cognitions. Unless significant differences were found between the steps in the regression models and otherwise noted, all statistics reported are from the final step of the specific regression model, which included all covariates, main effects, and interactions.
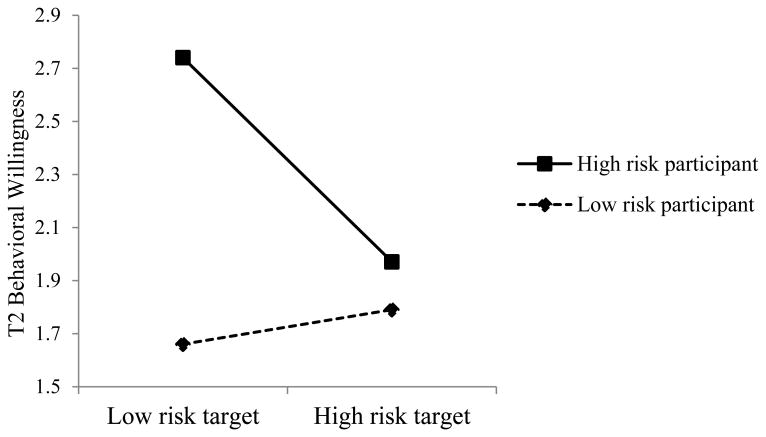
Willingness
T1 willingness was related to T2 willingness (β =.33, t = 4.56, p < .001). Nonetheless, the Participant Risk X Condition interaction was significant (β = -.20, t = -2.20, p < .03; adjusted R2 of model = .37). Simple slopes tests (participant risk +/-1 SD) revealed that target risk did not affect the willingness of low-risk participants (β = .10, t = 1.40, p = .17). However, as expected, among high-risk participants, those who heard the low-risk target reported higher willingness than those who heard the high-risk target (β = -.26, t = -2.93, p < .005). This interaction was qualified by the anticipated Participant Risk X Condition X SCO interaction (β = -.13, t = -2.02, p < .05). Decomposing this interaction revealed the Participant Risk X Condition interaction was not significant for low comparers (p > .20), but it was significant for high comparers (β = -.28, t = -2.21, p < .03; see Figure 1). Among the high comparers, simple slopes tests revealed that willingness was associated with target risk only among high-risk participants (β = -.35, t = -2.88, p < .005); participants high in comparison tendencies who compared with the low-risk target reported higher willingness to have sex without a condom than those who compared with the high-risk target. The simple slope among low-risk participants was not significant (β = .07, t = .57, p > .5).
Figure 1.
Study 1: Willingness to have sex without a condom as a function of participant risk and target risk, controlling for T1 willingness, among high comparers.
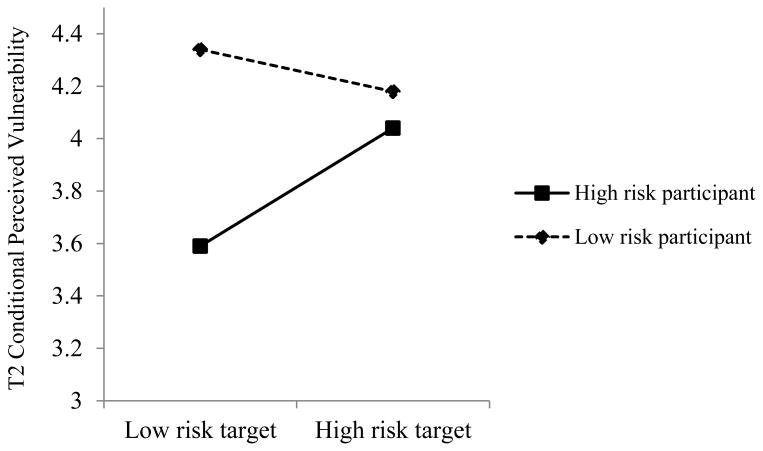
Conditional vulnerability
The stability of conditional vulnerability from T1 to T2 was strong (β = .34, t = 4.67, p < .001). High-risk participants reported lower conditional vulnerability to STDs (β = -.21, t = -2.50, p < .02; cf., Halpern-Felsher et al., 2001). High comparers also reported lower vulnerability (β= -.27, t = -3.42, p < .001), even though they did not engage in riskier past behavior. Females reported higher levels of conditional vulnerability (β = .15, p < .05; cf., Lewis et al., 1999; overall adjusted R2 = .41). The predicted Participant Risk X Condition interaction was significant (β = .19, t = 2.16, p = .03); the pattern revealed that high-risk participants who heard the low-risk target reported lower conditional vulnerability than high-risk participants who listened to the high-risk target. The slopes for risk-status were not significantly different from zero (ps > .1), but they were significantly different from each other. As seen in the willingness analyses, this 2-way interaction was qualified by the anticipated 3-way interaction (β = .13, t = 2.12, p < .04). For low comparers, the Participant Risk X Condition interaction was not significant (p > .3). However, it was significant for those who engage in high levels of social comparison (β = .26, t = 2.20, p = .03; see Figure 2). Among the high comparers, simple slopes tests revealed that conditional vulnerability was associated with target risk among the high-risk participants (β = .32, t = 2.74, p = .007); those who compared with the low-risk target reported lower vulnerability than those who compared with the high-risk target. The slope among the low-risk, high-comparing participants was not significant (β = -.03, t = -.22, p > .80).
Figure 2.
Study 1: Conditional vulnerability to STDs as a function of participant risk and target risk, controlling for T1 conditional vulnerability, among high social comparers
Mediation by conditional vulnerability
The prototype/willingness model proposes that changes in conditional vulnerability will mediate changes in willingness (Gerrard et al., 2008; Gibbons et al., in press). Thus, a mediation analysis, using the bootstrapping method (Preacher & Hayes, 2008), was performed to see if conditional vulnerability mediated the effect of Participant Risk and Condition on T2 willingness among high comparers, controlling for T1 willingness, conditional vulnerability, and gender. The bias-corrected 95% confidence interval did not contain zero (-.16, -.02); thus, change in conditional vulnerability mediated change in willingness to engage in sex without a condom.
Intentions
Stability was also high for intentions (β = .42, t = -6.07, p < .001), and high-risk participants reported greater intentions to have sex without a condom (p = .001). As anticipated, however, there was no interaction between participant risk and target risk (β = -.10, t = -.99, p = .32), and the three-way interaction was also not significant (p < .3). Thus, risk intentions (or change in intentions) were not affected by the social comparison or by SCO.2
Study 1 Discussion
Low and high risk college students reported lower willingness to engage in sex without a condom and higher conditional vulnerability to STDs if they were given an opportunity to compare with an infected peer who had a similar sexual risk level as opposed to a different level of risk. In addition, the high-risk students who heard about others their age and gender who were at lower risk, but still suffered negative consequences, engaged in what appeared to be AE thinking: they reported the highest willingness and lowest conditional vulnerability. Additionally, as the prototype/willingness model would predict, changes in conditional vulnerability mediated changes in willingness to have sex without a condom. As expected, these tendencies were stronger among high comparers. However, the process of comparing with a peer did not significantly influence intentions to engage in sex without a condom. This is consistent with a basic premise of the prototype/willingness model that intentions and willingness are correlated, but distinct constructs (Gibbons et al., 1998a; 1998b; 2004) that are affected in different ways by social factors. In short, these findings highlight: (a) how risk cognitions are differentially affected among low and high risk young adults by comparison targets and (b) the importance of past behavior in influencing this process.
Study 2: Social Comparison, Participant Risk Status, and AE Endorsement
Study 2 included a direct measure of AE. In addition, to further examine the role of social comparison, Study 2 compared the impact of a low-risk comparison target with: (a) information from a PSA that suggested negative outcomes can happen even to low-risk targets and (b) a “pure” (no information) control condition. Participants at relatively high or low risk of contracting an STD were randomly assigned to hear either the low-risk comparison target from Study 1, or the PSA, or no information. Thus, Study 2 had a Condition (low-risk target vs. PSA vs. control) X Participant Risk level (continuous) X SCO (continuous) design.
Several studies have shown that health-risk cognitions are affected more when social comparison information is included in health messages (e.g., seeing or hearing a peer discuss the health issue) than when only analytic (e.g., prevalence-based information) is presented (French, Sutton, Marteau, & Kinmonth, 2004; Klein, 1997). Since AE is assumed to involve more heuristic-based processing, it was predicted that high-risk participants who heard the message, “it only takes one time,” in a format that does not directly promote social comparison processes (i.e., a PSA), would be less likely to be affected by the information.
Similar to Study 1, we hypothesized a Condition by Participant risk interaction on the AE cognitions such that low-risk participants would report higher conditional vulnerability, lower willingness, and lower AE endorsement, especially after comparing with the low-risk target. Conversely we expected high-risk participants would report the lowest levels of vulnerability and highest willingness and AE endorsement after comparing with the low-risk target. Finally, we hypothesized that this two-way interaction would once again be stronger among participants higher in SCO, and that AE endorsement would mediate the effect. Study 2 included two additional outcome measures: time spent reading information about genital herpes, and intentions to get tested for STDs. Consistent with the defensive nature of AE (among higher risk participants) and its heuristic nature, we predicted that high-risk participants in the comparison condition would spend less time reading than would low-risk participants in this condition (Croskerry, 2009; Evans, 2008). Since there is evidence that individuals may respond to health threats in two different ways (reasoned and reactive), the current study also explored whether the anticipated pattern of heuristic processing would be replaced by more reasoned processing when participants were asked about their intentions to get tested for an STD. It has been suggested (although seldom tested) that although higher-risk individuals may report lower levels of vulnerability (especially conditional vulnerability), they may also turn to more reasoned processing and exhibit “windows of realism” for matters of importance (Taylor & Brown, 1988). For example, previous research has shown that engaging in ultraviolet (UV) risk behavior is associated with greater willingness to tan and reduced perceptions of vulnerability to skin damage, but also greater intentions to have one's skin examined by a doctor (Walsh & Stock, 2012). Thus, consistent with the dual-processing nature of the prototype/willingness model, we explored whether different effects would be found for more reactive, health-risk cognitions vs. more reasoned health-promoting cognitions.
AE Measure
AE endorsement has typically been measured with a single item: e.g., “If I haven't gotten an STD by now, I probably won't get one in the future” (Gerend et al., 2004; Weinstein, 1984). To expand this construct and further explore AE thinking, we asked 160 sexually active college students who agreed to some degree with this statement to describe why they felt exempt. Based on these responses, in addition to the typical single item, three more AE items were included in the AE construct: “If I haven't gotten an STD by now, I probably will not in the future…whether or not I use a condom….because I have good choice in sexual partners… because I am lucky” (1 = strongly disagree; 7 = strongly agree). These items were included in a mass-testing pilot survey of 464 students and all four items were found to load on a single construct (a = .82). To examine if this AE measure is related to, but distinct from, conditional vulnerability, the four AE items, along with four unprotected sex conditional vulnerability items were entered into a confirmatory factor analysis. As expected, AE and conditional vulnerability loaded onto two separate constructs (r = -.13, p < .05).
Methods
Participants
The same pre-test selection criteria and procedures were used as in Study 1. Once again, the lab-based portion took place approximately 2-10 weeks after the pre-test. A total of 222 (134 females) participated; they averaged 20.5 years of age (range = 19-26).
Experimental procedure
When participants arrived at the lab, they were told by a same-sex experimenter that the study concerned reactions to health problems and health-related information. All experimental materials were presented through MediaLab (Jarvis, 2008). Students first answered questions about their sexual behaviors. Those assigned to the comparison target condition then heard the same low-risk target tape as in Study 1. Participants in the PSA condition heard an audiotape of a same-sex health clinic employee who discussed students testing positive for herpes and mentioned “it only takes sexual contact with one person, one time, to get an STD.” Control participants did not hear a tape. Next, participants completed a second questionnaire (T2) and then read information about herpes (i.e., what is genital herpes, how is it contracted, its prevalence, and treatment/care (CDC, 2006; Mayo Clinic, 2006)). Reading time was recorded. The experimenter then probed for suspicion and debriefed the participants.
Measures
Social comparison orientation (T1)
SCO was again assessed with the INCOM (α = .76).
Participant sexual risk (T1)
Previous risk was assessed as in Study 1.
Willingness (T1, T2)
Willingness was assessed using the same scenarios and questions as at T2 in Study 1. All four items were averaged (αs = .83 & .85, at T1 and T2, respectively).
AE endorsement (T1, T2)
AE thinking was examined with the four items described above (1 = strongly disagree; 7 = strongly agree; αs = .78 & .79, respectively).
Conditional vulnerability (T1, T2)
Conditional vulnerability was assessed with the same two items as in Study 1 (T1 r = .33, T2 r = .37).
Reading time (T2)
Medialab recorded how much time participants spent reading the article on herpes, which was log transformed. Amount of time spent reading instructions was also measured, log transformed, and used as a control variable for all reading time analyses.
Intentions for STD testing (T1, T2)
Participants were asked: “Do you intend to get tested for an STD (other than HIV) in the next 6 months?” (1 = not at all, 7 = definitely).
Control variables (T1)
All analyses controlled for gender, the corresponding T1 cognition, and relationship status (0 = single, 1 = committed).
Results
Descriptives
Once again, there was a fair amount of risk behavior. Participants reported an average of 4.5 sexual partners—2.5 steady and 2 casual (range = 1-34); 23% reported having one partner, whereas 25% reported 5 or more; 66% reported at least 1 casual partner; 33.5% reported 3 or more steady partners; 65% reported currently being single. A GLM ANOVA revealed no differences between conditions in terms of SCO level, T1 willingness, or AE (all ps > .10). In the comparison target condition, high-risk participants perceived the behaviors of the comparison target as less risky than did low-risk participants (M = 2.2 vs. 3.6, F(1, 74) = 19.5, p < .001). High risk participants also reported greater willingness to have sex without a condom and more intentions to get tested (ps < .001).
Risk cognitions
Hierarchical multiple regression analyses were again used to examine the hypothesized Participant Risk by Condition interaction, as well as the anticipated moderation of this interaction by SCO. Once again, participant risk status was log-transformed and all continuous variables were centered (Aiken & West, 1991). Two planned contrasts were created for the condition variable (West, Aiken, & Krull, 1996). Because it was hypothesized that the comparison target condition would differ from both the PSA and control conditions, the first contrast compared the comparison condition with the PSA and control conditions (Contrast SC-PC; -2, 1, 1). The second contrast compared the PSA and control conditions (Contrast P-C; 0, 1, -1). When an anticipated 3-way interaction was observed, we decomposed the interaction and examined the impact of Condition and Participant Risk for high and low (+/-1 SD) comparison participants. Simple slope tests were then conducted.
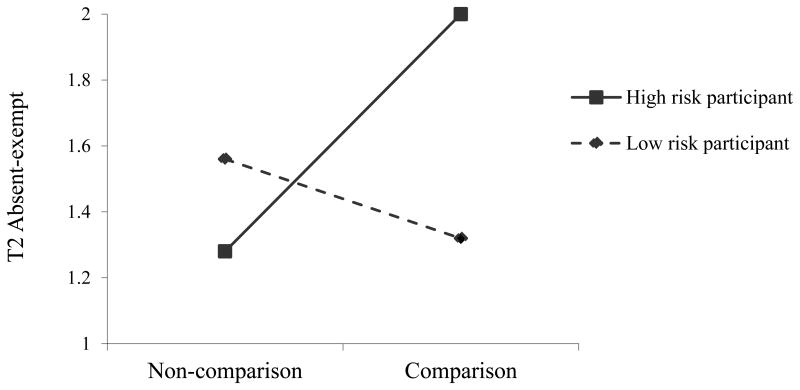
AE endorsement
Stability of AE endorsement was high (β = .53, t = 8.83, p < .001). Gender entered significantly (β = .12, t = 2.02, p < .05), as males reported higher AE endorsement, but it was non-significant once the interactions were entered (p > .30). No other main effects were significant. The 3-way and 2-way interactions with contrast P-C were not significant (ps > .13; overall R2 of model = .33). Unexpectedly, the SC-PC contrast by Participant Risk interaction was not significant (β = .04, t = .67, p = .50).3 However, the anticipated Participant Risk X SC-PC contrast X SCO was significant (β = -.16, t = -2.53, p = .01). The SC-PC contrast by Participant Risk interaction was then examined for high and low comparers (+/-1 SD) separately. The interaction was significant for high comparers (β = -.21, t = -2.53, p = .01; see Figure 3), but not for low comparers (p > .2). For high comparers, simple slopes tests revealed that the comparison (versus non-comparison) condition was associated with greater AE endorsement among high-risk participants (β = -.30, t = -2.71, p < .01), but the SC-PC contrast was not significant among low-risk participants (β = .10, t = .87, p = .39). In sum, as predicted, high-risk, high comparing participants, who compared with the low-risk target reported higher AE endorsement than those in the non-comparison conditions.
Figure 3.
Study 2: T2 AE endorsement controlling for T1 AE endorsement as a function of participant risk and condition for high social comparers.
Conditional vulnerability
T1 vulnerability predicted T2 vulnerability and being male and lower past risk behavior were associated with greater T2 vulnerability (ps < .001; overall R2 of model = .45). The P-C by Participant Risk interaction was significant (β = -.12, t = -2.21, p < .03). Breaking down this interaction revealed that among the high-risk participants, the PSA (versus control) message was associated with lower perceived vulnerability (β = -.16, t = -2.07, p = .04). However, among the low-risk participants, the PSA message was associated with marginally greater perceived vulnerability (β = .15, t = 1.83, p < .07). The SC-PC contrast by Participant Risk interaction was also significant (β = .13, t = 2.26, p < .03). Simple slopes tests revealed that high-risk participants reported lower conditional vulnerability in the comparison versus the non-comparison condition (β = .18, t = 2.36, p < .02), whereas the SC-PC (comparison versus non-comparison) contrast was non-significant among low-risk participants (β = -.09, t = -1.25, p > .2). No additional 2-way interactions nor the 3-way interaction with contrast P-C were significant (ps > .1). The anticipated 3-way interaction with contrast SC-PC was significant (β = .13, t = 2.21; p < .03). An examination of this interaction revealed, once again, the SC-PC by Participant Risk interaction was significant for high comparers (β = .30, t = 3.98, p < .001), but not for low comparers (p > .70). Simple slopes tests among high SCO participants revealed that among high-risk participants, those in the comparison condition reported lower levels of vulnerability (β = .27, t = 2.71, p < .01). However, among the low-risk participants, those in the comparison condition reported significantly higher levels of vulnerability (β = -.30, t = -2.88, p < .01).
Willingness
T1 willingness predicted T2 willingness and high-risk participants reported higher levels of willingness than did low-risk participants (ps < .001). No other main effects were significant. The anticipated SC-PC contrast by Participant Risk interaction was significant (β = .09, t = 2.17, p < .04). Simple slopes tests revealed that high-risk participants reported higher willingness in the comparison versus the non-comparison condition (β = -.13, t = -2.01, p < .05), whereas the SC-PC (comparison versus non-comparison) contrast was non-significant among low-risk participants (β = .06, t = 1.05, p > .2). The predicted 3-way interaction with the SC-PC contrast was also significant (β = -.11, t = -2.37, p = .02; overall R2 = .70), whereas, the 3-way interaction and all 2-way interactions with the P-C contrast were not (ps > .20). Once again, the SC-PC by Participant Risk interaction was not significant for low comparers (p > .60), but it was for high comparers (β = -.17, t = -2.92, p < .005). Simple slopes tests among the high comparers revealed the same pattern as AE: willingness was greatest among high-risk participants in the comparison versus the non-comparison condition (β = -.22, t = -2.83, p < .005), and there was not a significant difference in willingness by condition among low-risk participants (β = .08, t = 1.09, p = .25). In sum, similar to AE, willingness was highest among the high-risk, high comparers in the comparison condition.
Mediation by Conditional Vulnerability
The same bootstrapping method as in Study 1 was employed to examine whether the SC-PC by Participant Risk interaction on T2 willingness among high comparers was mediated by T2 conditional vulnerability (controlling for T1 willingness, conditional vulnerability, gender, and relationship status). The mediation of change in willingness by change in conditional vulnerability was significant: the bias-corrected 95% confidence interval did not contain zero (-.071, -.002).4
Reading time
All main effects and interactions with contrast P-C in the model were non-significant on reading time (ps > .1). However, the SC-PC by Participant Risk by SCO interaction was significant (β = -.16, t = -2.01, p < .05). Once again, the SC-PC by Participant Risk interaction was significant for high comparers (β = .31, t = 2.52, p < .02), but not for low comparers (β = -.06, t = -.57, p = .57). Simple slopes analyses revealed a significant SC-PC contrast effect among the high risk, high comparers (β = .36, t = 2.69, p < .01), but not the low risk, high comparers (β = -.22, t = -1.21, p < .23). The pattern was as expected: high-risk, high comparing participants in the comparison condition spent the least amount of time reading the information on STDs.
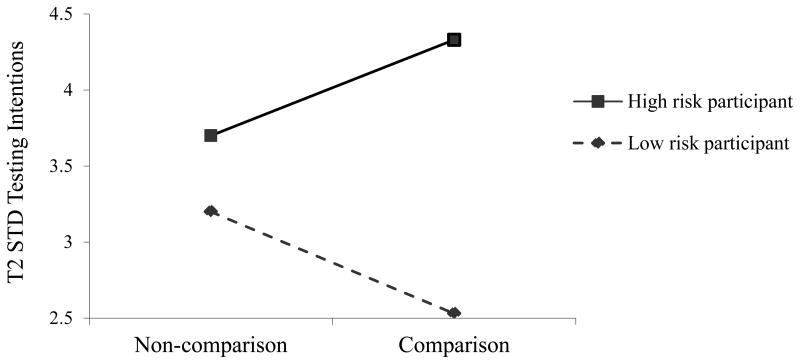
STD testing intentions
The T1 / T2 stability was high for STD testing intentions (β = .43, t = 7.28, p < .001). High-risk participants reported greater intentions to get tested (β = .22, t = 3.77, p < .001). Males and those in a committed relationship reported lower intentions (ps < .05). No significant effects were found with contrast P-C (ps > .1). The only significant interaction was the SC-PC by Participant Risk (β = -.13, t = -2.21, p < .03; see Figure 4; overall R2 of model = .45).5 Simple slopes tests revealed a pattern that was quite different than that of the other dependent variables: The SC-PC contrast was significant among the high-risk participants (β = -.17, t = -2.44, p < .02) and marginal among the low-risk participants (β = .12, t = 1.65, p = .10), but in opposite directions. The low-risk participants in the comparison condition reported the lowest intentions. However, the high-risk participants in the comparison condition -- who reported higher willingness and more AE endorsement -- also reported the greatest intentions to get tested for STDs.
Figure 4.
Study 2: T2 Intentions to get tested for STDs in the next 6 months.
Study 2 Discussion
Once again, high-risk participants who compared with a low-risk / infected target responded in an AE-consistent pattern: an increase in perceptions of being exempt from STDs in the future, a reduction in conditional vulnerability, and an increase in willingness to engage in sex without a condom. In addition, Study 2 revealed that changes in conditional vulnerability, once again, mediated the effects of comparison with the low-risk target on willingness to engage in sex without a condom. For the high-risk participants, hearing from a dissimilar target appeared to feed into their illusions of relative invulnerability. Controlling for initial reading time, these high-risk participants spent less time reading information on herpes after comparing with the low-risk target versus the non-comparison condition, suggesting that they did not believe they needed and/or did not want to pay attention to the information. These findings are consistent with previous research suggesting that individuals at high risk are motivated to process health messages more defensively and are more likely to avoid potential negative health information (e.g., Gerrard, Gibbons, & Warner, 1991; Howell & Shepperd, 2013; Kos & Clarke, 2001; Liberman & Chaiken, 1992). However, although high-risk status was associated with riskier cognitions in the comparison condition, it was also associated with greater intentions to get tested for STDs. These findings reflect the dual-pathway nature of young adult decision-making as outlined in the prototype/willingness model (Gibbons et al., 2011). In other words, high-risk individuals report lower perceived vulnerability and greater risk willingness, especially when faced with more image-based social comparison information, presumably because optimistic biases allow them to feel less threatened (e.g., Taylor & Brown, 1988). They may, however, turn to more reasoned processing and exhibit “windows of realism,” as Taylor and Brown suggest, under certain circumstances. Finally, the impact of social comparison information was again greater for those higher in SCO, demonstrating the importance of comparison processes in AE thinking in response to comparison targets.
We found only one significant result when comparing the PSA to the control message: the high-risk participants who heard the PSA (vs. control) message reported lower vulnerability. One reason for the lack of difference between the PSA and control condition may be that PSAs and health messages are fairly common and so may have been discounted by the participants. Although it is possible that the PSA could prompt thoughts about comparison targets (e.g., who are students who have herpes?), hearing a tape from an actual victim (versus a health professional) who is a peer similar in basic demographics should promote the comparison process to a greater degree (Paek, Hove, Ju Jeong, & Kim, 2011; Wood, 1989).
It is not surprising that the comparison condition had a stronger impact than the non-comparison conditions. Information that has a comparison-based element often has a stronger influence than analytic-based information (French et al., 2004; Klein, 1997). We believe it was the personal aspect in the comparison condition that resulted in a stronger overall impact on AE thinking. In short, these results were consistent with expectations, but they also raise an obvious question: Can we reduce AE thinking among high-risk engagers? This is what Study 3 was designed to explore.
Study 3: Can AE Thinking be Reduced?
To examine if AE thinking is malleable, Study 3 included only “AE-prone” participants—i.e., high-risk, sexually active college students with high SCO scores. These students heard a tape about either the low-risk or high-risk peer who had been diagnosed with genital herpes (same audios as in Study 1). Before hearing the tape, the students read an “article” on a different health behavior, sun exposure (ostensibly the first part of a 2-part study). For half of the participants, this article included a paragraph that suggested that AE thinking related to skin damage (due to sun/UV exposure) was illogical. The purpose was to see if AE endorsement among high-risk participants could be decreased after more reasoned (and less heuristic) processing was encouraged via AE information on an unrelated behavior. Thus, Study 3 was a Target Risk (low vs. high) X AE information (yes vs. no) factorial. We hypothesized a main effect for the AE information conditions: students in the AE information condition would report the lowest levels of willingness, AE endorsement, and highest conditional vulnerability. We also hypothesized an AE information by Target Risk interaction among students who heard the low-risk tape: receiving the AE information would counter AE thinking. Thus, we expected less of an increase in willingness and AE endorsement, and less of a decrease in vulnerability than that found in the first two studies. In line with the results from Studies 1 and 2, we also anticipated that casual sex intentions would not be influenced by the comparison; however, STD testing intentions would be affected and would be higher among participants in the AE information, low-risk target condition.
Methods
Participants
Undergraduates who reported in a pre-test session that they had unprotected sex in the past, had sex with at least 1 casual partner, were not married, had never had an STD, and had a SCO average score on the INCOM > 3 were recruited to participate in a lab-based study on health. The sample included 150 participants (74 males, 97% White, M age = 20.5).
Experimental procedure
Upon arriving at the lab, a same-sex experimenter told participants that the “two studies” were examining reactions to two different forms of health information, and that the first study was designed to examine reactions to written health information. Students then read a bogus article on sun exposure and skin damage. Half of them were randomly assigned to also receive information on AE thinking related to UV exposure (n = 80). After reading the article, they were told the second study involved reactions to others their age who are experiencing specific health problems, which they would hear about via an audiotape. Next, they were randomly assigned to hear the same high-risk (n = 75) or low-risk target (n = 75) used in Study 1. Finally, the students completed a questionnaire assessing AE, willingness, intentions, conditional vulnerability, and manipulation checks, and were debriefed.
Measures
AE (T1, T2)
AE was measured with the same items as in Study 2 (αs =.78, .80).
Conditional vulnerability (T1, T2)
Conditional vulnerability was assessed with two items “If you were to have sex [with a casual partner] without a condom, what do you think the chances are that you would get an STD?” (1= very likely; 7 = not at all likely; rs = .69, .58).6
Casual sex willingness (T1, T2)
The casual sex scenario from Study 1 was used followed by “… have sex without a condom…have sex and use withdrawal…go home (reverse-coded)” (1=not at all willing; 7 = very willing; T1 a = .78, T2 α = .77).
Casual sex intentions (T1, T2)
Intentions were measured with two items asking participants how much they intended to “have sex with a casual partner [without a condom] in the next six months.” (1= strongly disagree; 7 = strongly agree; T1 r = .53, T2 r = .43).
Intentions for STD testing (T2)
Testing intentions were assessed with the same item as in Study 2.
Manipulation checks (T2)
The same three manipulation check items from Study 1 were assessed. Participants also rated how similar they were to the target in terms of sexual behaviors.
Control variables (T1)
As in Studies 1 and 2, analyses controlled for gender, the corresponding T1 cognition, and relationship status (0 = single, 1 = committed).
Results
Participants reported an average of 5 sexual partners (range = 3-7); 50% reported having 3 or more casual partners; 25% reported being in a committed relationship. When asked about frequency of sex without a condom, they averaged 5 on a 7-point scale (7 = all the time). T2 AE was positively associated with T1 AE (p < .001), and negatively correlated with conditional vulnerability and testing intentions (all ps < .05; see Table 3 for correlations and means).
Table 3. Study 3 Correlations and Means.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. T1 AE | - | ||||||||
| 2. T1 Casual sex willingness | .22* | - | |||||||
| 3. T1 Casual sex intentions | 0.13 | .39*** | - | ||||||
| 4. T1 Conditional vulnerability | -.19* | -.18* | -0.05 | - | |||||
| 5. T2 AE | .43*** | .15† | -0.14 | -.27*** | - | ||||
| 6. T2 Conditional vulnerability | -.25* | -.26*** | -.17* | .46*** | -.30*** | - | |||
| 7. T2 Casual sex willingness | 0.03 | .55*** | .33*** | -.19* | 0.1 | -.33*** | - | ||
| 8. T2 Casual sex intentions | -0.03 | .33*** | .56*** | -0.07 | -0.12 | -.14† | .39*** | - | |
| 9. T2 Intentions for STD testing | -0.11 | 0.06 | 0.09 | 0.05 | -.20* | .18* | -0.11 | -0.04 | - |
| 10. Gender | 0.03 | .26*** | .14† | -0.05 | -0.02 | -.14† | .19* | 0.08 | -.24** |
|
| |||||||||
| Mean | 3.14 | 3.56 | 2.55 | 4.17 | 2.68 | 4.98 | 3.42 | 2.09 | 3.74 |
| SD | 1.29 | 1.23 | 1.48 | 1.5 | 1.08 | 0.83 | 1.24 | 1 | 1.96 |
| Range | 1-5.5 | 1-7 | 1-6 | 1-7 | 1-5 | 2.5-7 | 1-6.25 | 1-4.67 | 1-7 |
Note. N = 150;
< .10,
p < .05,
p < .01,
p < .001.
Gender coded (0 = female, 1 = male). Relationship status coded (0 = single, 1 = committed).
GLM ANOVAs on all four manipulation check items indicated that the manipulation was effective (all ps < .001). Participants in the high-risk target condition reported higher levels of similarity, in terms of sexual behaviors, than did those in the low-risk target condition (M = 4.6 vs. 3.17, p < .001). Bonferroni adjusted ANCOVAs were then conducted, controlling for gender and T1 measures, followed by regressions to examine potential mediation of the AE → willingness relation by conditional vulnerability, as found in Studies 1 and 2.
AE
Again, there was good (T1/T2) stability in the AE construct (p < .001). As anticipated, participants who learned about AE thinking reported lower AE compared to those who did not (M = 2.49 vs. M = 2.96; F (1, 140) = 8.86, p = .003). The predicted AE information by target risk interaction was also significant, F (1, 140) = 8.92, p = .003; AE thinking was highest among students in the low-risk target, no-information condition (M = 3.30, see Table 4 for means and simple main effects), whereas the lowest levels were reported in the low-risk target, AE information condition (M = 2.34). The interaction remained when controlling for T2 conditional vulnerability, F = 7.06, p < .01, indicating these constructs are measuring different aspects of risk perception.7
Table 4. Means and Standard Deviations for T2 AE, Conditional Vulnerability, Casual Sex Willingness, Casual Sex Intentions, and STD Testing Intentions by Condition (Study 3).
| Variable | No AE Information | AE Information | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Low-Risk Target (n=33) |
High-Risk Target (n=37) |
Low-Risk Target (n=42) |
High-Risk Target (n=38) |
|||||
|
|
|
|
|
|||||
| M | SE | M | SE | M | SE | M | SE | |
| Absent-exempt | 3.30a | .16 | 2.65b | .16 | 2.34b | .14 | 2.66b | .15 |
| Conditional Vulnerability | 4.70a | .14 | 4.91a,b | .14 | 5.33b | .13 | 4.94a,b | .13 |
| Casual Sex Willingness | 3.91a | .18 | 3.65a | .17 | 3.03b | 0.15 | 3.53a | .16 |
| Casual Sex Intentions | 2.38 | .13 | 2.30 | .13 | 2.21 | 0.12 | 2.38 | .12 |
| Intentions for STD testing | 3.77a,b | .34 | 3.25a | .29 | 4.40b | .32 | 3.63a,b | .31 |
Note: Means in the same row that do not share subscripts differ at p ≤ .05 level.
Conditional vulnerability
Conditional vulnerability stability was strong (p < .001); and females again reported higher conditional vulnerability (p < .05). The expected AE information main effect emerged: Participants who learned about AE thinking reported significantly higher conditional vulnerability (M = 5.14 vs. 4.81; F (1, 140) = 6.12, p < .02). The predicted AE information by target risk interaction was again significant, F (1, 140) = 4.11, p < .05. Those in the AE information, low-risk target condition reported the highest levels of conditional vulnerability (M = 5.33), whereas the lowest levels were reported by those in the low-risk target / no AE information condition (M = 4.70).
Casual sex willingness
Once again, willingness stability was high (p <.001), but the expected AE information main effect was found: participants who learned about AE thinking reported lower willingness to engage in casual sex without a condom than did those who did not (M = 3.30 vs. M = 3.79; F (1, 140) = 8.41, p = .004). The AE information by target risk interaction was also significant F (1, 142) = 4.45, p < .05; the highest levels of willingness were in the low-risk target, no information condition (M = 3.91), whereas the lowest levels were in the low-risk target, AE information condition (M = 3.03).
Mediation of willingness effects by conditional vulnerability
A bootstrapping analysis was performed among the participants exposed to the low-risk target to see if the AE information effects on T2 willingness were mediated by T2 conditional vulnerability, controlling for gender, relationship status, and T1 vulnerability and willingness. The mediation test indicated that changes in casual sex willingness were mediated by changes in conditional perceived vulnerability (95% CI = .035, .519).8
Casual sex intentions
T1 intentions to have sex without a condom were a strong predictor of T2 intentions (p < .001). There were no other significant main effects (ps > .4) and the AE information by target risk interaction was not significant F (1,143) = .17, p = .68. In fact, the means across all four cells were very similar (see Table 4).9
Intentions to get tested for STDs
Females reported higher intentions to get tested (p < .02). An AE information by target risk interaction, F (1, 142) = 4.04, p < .05, revealed that the highest intentions were reported by participants in the AE-information low-risk target condition (M = 4.40), whereas the lowest levels were reported by those in the high-risk target, no-AE information condition (M = 3.25).
Study 3 Discussion
Study 3 replicated the results from the previous two studies: when hearing from a low-risk comparison target who had been diagnosed with an STD, high-risk college students reported the highest levels of risk cognitions associated with risky sex. However, this study also showed that AE thinking (as reflected in AE endorsement, reduced conditional vulnerability, and greater willingness) is malleable. When students were given information suggesting that AE thinking was illogical before hearing from the lower-risk peer, they reported the lowest levels of risk cognitions and the greatest intentions to get tested.
General Discussion
As expected, in all three studies, perceived similarity of the comparison target (in terms of risk behavior) affected participants' reactions. Those who heard a recording depicting an STD-positive target with a similar level of risk consistently reported the least risky cognitions associated with unprotected sex. This suggests that comparison with a similar-risk target who engages in a risky behavior may have potential health-related benefits, including encouraging less willingness to engage in risk behavior, fewer feelings of being exempt from future risk, and increases in conditional perceived vulnerability. In fact, this is consistent with previous studies, which have found that perceived vulnerability is influenced by the perceived similarity of the comparison target (Klein & Weinstein, 1997; Thornton et al., 2002), and that optimistic bias declines when comparing with an individualized or single target (Price, Smith, & Lench, 2006; Lermer, Streicher, Sachs, & Frey, 2013). Very different results emerged, however, when the targets' past behavior differed from the participants.
The pattern was particularly interesting among the high-risk participants. In all three studies, comparing with a low-risk / infected comparison target led to an increase in feelings of being exempt from STDs in the future and/or a decrease in perceptions of risk, and an increase in willingness to engage in sex without a condom. These high-risk students also spent less time reading information on herpes after the comparison opportunity, suggesting they were engaging in more defensive processing, and so lowered their risk perceptions (Trumbo, 1999; 2002). Although it may not be completely illogical that feelings of being “exempt” from infection are heightened among higher-risk participants after comparing with a low-risk peer (they have, in fact, engaged in more risky behaviors than the low-risk peer without being infected), it is concerning because low risk perceptions are associated with future risky behavior and lower levels of protection (Gerrard et al., 1996; Gibbons et al., 2002; Tenkorang, 2013). Willingness was associated with higher levels of AE endorsement and lower conditional vulnerability, suggesting it may have been a reflection of the diminished perception of risk due to the comparison. In addition, among the high-risk, high-comparers, change in conditional vulnerability mediated the effect of condition on change in willingness in all three studies.
Social Comparison Processes
Our findings demonstrate how individuals' past behaviors and comparison tendencies alter the effects of comparison with peers on their risk cognitions. Specifically, students who reported engaging in comparison more often were more affected by the comparison opportunity (they reported the highest and lowest levels of AE). Although social comparison is not necessary for AE thinking to occur, the fact that AE thinking was more pronounced when comparing with an infected student versus hearing a PSA (or in the control condition), and more pronounced among those high in SCO, suggests that feelings of being exempt from future harm may be particularly impacted by social comparison opportunities. Thus, messages that employ low-risk comparison targets who have experienced negative outcomes have the potential to backfire among high-risk audience members. The moderation by SCO of risk cognitions, and AE thinking in particular, is further evidence of the important role social comparison plays in reactions to messages that involve other individuals—as they frequently do. Future research should further investigate the role of comparison processes and targets on risk perceptions and especially AE thinking.
The Prototype/willingness Model and Social Comparison Processes
The results were consistent with hypotheses regarding the two pathways of the prototype/willingness model, both reasoned and reactive, and suggest that when examining outcomes associated with social comparison targets, both pathways should be considered. These studies demonstrated once again that willingness and intentions to engage in a risk behavior are correlated (rs here ranged from .39 to .50), but they are not redundant. The two constructs also showed discriminable patterns in their relations with AE endorsement, which was consistently associated with willingness, but not intentions, to engage in risky sex. Similarly, in all three studies, social factors (social comparison, others' behavior) influenced willingness but not intentions to engage in unprotected sex. These findings are consistent with the belief that the process of social comparison should have a stronger impact on the social/reactive route of the prototype/willingness model when it comes to decision-making (Gerrard et al., 2008; Gibbons, et al., 2003; Gibbons et al., in press; Lane et al., 2011).
There is also reason for optimism in our results. First, although the high-risk participants reported the highest levels of heuristic-based responding in all three studies, including AE endorsement and willingness to engage in the risk behavior, they also reported the greatest increase from baseline to post-manipulation in intentions to get tested for an STD. This suggests that more reasoned processing regarding risk (e.g., “I should get tested”) can occur in spite of a dominance of heuristic/reactive thinking (cf., Reyna & Farley, 2006). Another possible reason for the increased intentions to get tested among this high-risk group is that this is one way for those who endorsed AE thinking to reassure themselves that they really have not yet been infected.10 The findings with STD testing intentions are very interesting and appear important. Clearly, additional research is needed to more fully understand the differences in findings between risky behavioral intentions and intentions to engage in testing.
Another reason for optimism is that the results of Study 3 demonstrated that AE thinking can be overcome fairly easily. When given information defining AE thinking prior to hearing the lower-risk comparison target, high-risk students reported lower endorsement of the health-risk cognitions. More generally, our findings add to previous research by suggesting that social comparison processes can have very different effects not only on the cognitions within the social reaction versus reasoned pathways in the prototype/willingness model, but also on intentions to engage in preventive vs. risky behaviors.
Intervention Implications
The current research has several implications for interventions intended to reduce risky behaviors. One is that they are more likely to be effective if they encourage high risk participants to compare with similar-risk others who have experienced negative consequences. Another is that comparison-based interventions may work better for those who engage in social comparison more often, especially for younger, less experienced individuals who tend to be more influenced by social comparisons (Gibbons & Buunk, 1999). The findings also have implications for dual-processing models of health behavior used in designing health interventions. Most health behavior interventions have been based on the assumption that health behavior is at least reasoned if not reasonable. Our findings, along with interventions designed with a dual-processing perspective (e.g., those incorporating the prototype/willingness model), indicate that although some risky health decisions are intentional, adolescents' and young adults' decision-making also has important heuristic and/or socially reactive elements (e.g., images of engagers, AE endorsement, affect, willingness; Gerrard et al., 2006; 2008; Reyna & Brainerd, 2011; Stanovich, Sá, & West, 2004; Webb & Sheeran, 2006). These elements, including AE cognitions, are malleable and therefore are logical cognitive targets for interventions (Gibbons et al., 2003; in press). Thus, these results suggest, once again, that intervention efforts are likely to be more successful if they take into account the dual nature of health decision-making (Gerrard et al., 2006).
Limitations and Future Directions
There are limitations with the current studies that need to be considered. First, some of the effects we found were modest in scale. They were also very consistent throughout all three studies -- while controlling for pre-manipulation cognitions, which were highly correlated with the post-manipulation cognitions. Still, replications of the effects are called for. Second, the AE measure was developed using college students. It has been shown that AE endorsement (e.g., concerning risk for skin cancer) exists and can be changed (via sun protection interventions) among at least two non-college populations: outdoor road workers and women over the age of 25 (Stock, Peterson, Gibbons, & Gerrard, 2013; Walsh et al., 2013). Nonetheless, studies employing AE measures in more diverse (e.g., racial/ethnic) populations are needed to establish external validity. Research on AE thinking also needs to be conducted on other types of risk (e.g., risky driving) behaviors and with non-college student populations—especially among older populations, who are more likely to endorse AE thinking.
More research is also needed on AE as a heuristic. First, future studies should examine how conditional perceived vulnerability and AE endorsement influence each other and how they are differentially influenced by other psychological and environmental factors over time. Second, future studies should be conducted to test the assumption that AE thinking reflects a certain kind of dual-processing (heuristic). Finally, how does AE compare with other heuristics associated with risk cognitions? It does share many characteristics with other heuristics, including being: a) influenced by social factors (e.g., social comparison), b) motivated by self-protection, and c) associated with less in-depth processing. Also, like many other heuristics, AE can have an element of veridicality—e.g., some people are in fact more immune to health problems than others. How it differs from other heuristics remains to be seen.
There are other cognitive factors that may play a role in our findings that were not examined in the present studies. For example, the degree of control or self-efficacy an individual feels they have in their sexual practices may alter the meaning and significance of the comparison process. Previous research has shown that biases in risk perceptions are increased when an individual feels he or she has more control over the risk behavior and the potential outcomes associated with it (e.g., Kos & Clark, 2001; Weinstein & Klein, 1995). Therefore, it would be interesting to examine the relation between AE endorsement and perceived control over the relevant health behaviors and outcomes.
Finally, we did not include behavior as a primary outcome measure due to the experimental design, the nature of the behavior, and our primary interest in risk cognitions, especially AE. Proximal antecedents like intentions and willingness are common outcome measures in experimental studies on risk behavior and have been shown to be predictive of future behavior (e.g., Gerrard et al., 2008; Gibbons, Etcheverry, Stock, et al., 2010; Stock, Peterson, Gibbons, & Gerrard, 2013; Todd et al., 2014; Webb & Sheeran, 2006). In addition, research has also demonstrated that risk perceptions influence future behavior (e.g., Gerrard et al., 2002; Sheeran, Harris, & Epton, 2014). Nonetheless, our findings point to a need for longitudinal research on the effectiveness of more intensive health messages and the impact of change in AE thinking over time, with sexual behaviors as a primary dependent variable. It also would be useful to investigate additional potential mediators and moderators.
Conclusion
These studies highlight the importance of social comparison and dual-processing in both the development of AE thinking and in reactions to health messages, especially those that are peer-based. Social comparison appears to be an important factor that influences risk perceptions and willingness to engage in risky behavior. This means the comparison process should be considered when designing interventions—especially if the audience includes adolescents and young adults who tend to be high in comparison tendencies (Gibbons & Buunk, 1999). Messages that use a peer to demonstrate health risks undoubtedly prompt the process of comparison. This can have positive effects—among lower risk individuals for example (as we found), or on more reasoned intentions to engage in preventive behavior. But, it can also lead to iatrogenic effects—unfortunately, among the group it was designed to affect the most, those at higher-risk. In this sense, these studies demonstrate the need to consider the risk status of both the audience and potential comparison targets employed in preventive health messages. Social comparison (in addition to other social psychological theories) has great utility for effective interventions—reflecting the fact that health promotion, and especially health risk, cognitions and behaviors are strongly influenced by the social environment.
Table 2. Study 2 Correlations and Means.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1 Willingness | - | ||||||||||
| 2. T1 AE | 0.11 | - | |||||||||
| 3. T1 Intentions for STD testing | 0.07 | -.14* | - | ||||||||
| 4. T1 Conditional Vulnerability | -.22** | -.19** | .21** | - | |||||||
| 5. T2 Willingness | .74** | -0.06 | 0.11 | -0.12 | - | ||||||
| 6. T2 AE | 0.13 | .49** | -0.05 | -.25*** | .12* | - | |||||
| 7. T2 Intentions for STD testing | 0.01 | -.13* | .57** | .16* | 0.07 | -.13* | - | ||||
| 8. T2 Conditional Vulnerability | -.32*** | -0.09 | 0.11 | .52*** | -.41*** | -.16* | 0.07 | - | |||
| 9. Reading Time | -0.04 | -0.08 | 0.08 | 0.09 | 0.02 | -0.04 | 0.13 | -0.01 | - | ||
| 10. Participant Risk | .38** | .16* | .35** | -0.01 | .52** | 0.01 | .30** | -.34*** | 0.08 | - | |
| 11. SCO | 0.08 | 0.02 | 0.05 | -0.03 | 0.11 | 0.12 | 0.07 | -0.03 | -0.04 | 0.02 | - |
| 12. Gender | .42** | 0.11 | -.18** | -.31*** | .29** | .15* | -.27** | -.43*** | 0.04 | 0.1 | -0.04 |
|
| |||||||||||
| Mean | 2.87 | 3.03 | 3.05 | 3.6 | 2.9 | 2.17 | 3.53 | 3.87 | 5.08 | 0.88 | 3.4 |
| SD | 1.37 | 1.43 | 2.14 | 0.96 | 1.38 | 1.01 | 2.26 | 0.81 | 0.11 | 0.41 | 0.67 |
| Range | 1-6.67 | 1-6.5 | 1-7 | 1-7 | 1-6.5 | 1-5 | 1-7 | 1-7 | 4.5-5.5 | 0-2.3 | 1-5 |
Notes. N = 222.
p < .05,
p ≤ .001.
Gender coded (0 = female, 1 = male). Relationship status coded (0 = single, 1 = committed).SCO indicates Social Comparison Orientation.
Acknowledgments
This research is supported by the National Institute of Drug Abuse, Grant DA021898 (PI: Frederick X. Gibbons). The authors thank members of the Health Cognitions Group for their helpful comments on this research.
Footnotes
The number of partners and condom use in the tapes were based on a different sample of college students' reports of sexual behaviors provided in a large screening survey session earlier in the year.
Study 1 also included additional measures of intentions to have sex without a condom and have sex with a casual partner. However, we chose to focus on the items that best match the willingness and conditional vulnerability items. When these intention measures were included as the outcomes in additional regressions, the pattern of results was the same as on the represented intention measure, i.e., all ps > .1.
Although the interaction was not significant, the pattern of results was consistent with the pattern found among just high comparers: high-risk participants in the comparison condition reported the highest levels of AE endorsement.
We also ran the model and included both T2 AE and T2 conditional vulnerability as potential mediators of SC-PC by Participant Risk interaction on T2 willingness among high comparers. The total mediation was significant: bias-corrected 95% confidence interval (-.109, -.014). However, only T2 conditional vulnerability was a significant mediator (CI = -.066, -.004) vs. (CI = -.072, .001 for T2 AE).
Although the 3-way interaction was not significant, the SC-PC by Participant Risk interaction was significant for high comparers (β = -.19, t = -2.51, p < .02), but not for low comparers (β = -.04, t = -.40, p > .70).
The pattern of the results does not change in Studies 1 and 2 when analyzing responses for just the casual sex partner on conditional perceived vulnerability, willingness, and intentions.
Follow-up planned comparisons on AE, willingness, and conditional vulnerability revealed that the low-risk, AE information and low-risk, no-AE information conditions were significantly different from each other on all three measures (ps < .001). In addition, for all three dependent measures, the low-risk, AE information condition means were significantly different from the other three conditions combined (ps < .01); and the low-risk target, no-AE information condition means were significantly different from the other three conditions combined (ps ≤ .02).
We also ran the mediational model and included both AE and conditional vulnerability as potential mediators. The total mediation was significant: bias-corrected 95% confidence interval (.016, .782). However, as in Study 2, only T2 conditional vulnerability was a significant mediator (CI = .019, .564) vs. (CI = -.109, .404 for T2 AE).
We also ran a GLM MANCOVA (AE information X Target Risk X Measure) on T2 casual sex willingness vs. casual sex intentions, controlling for the respective T1 cognitions and gender. Significant Measure X AE information (Wilks = 0.57, F(1,139) = 4.66, p < .05) and Measure X AE information X Target interactions were revealed (Wilks = 0.51, F(1,139) = 3.99, p < .05). These results reflect the findings from the individual ANCOVAs: casual sex intentions did not differ among conditions, however, willingness was effected by the manipulations.
We would like to acknowledge an anonymous reviewer for this suggestion.
Contributor Information
Michelle L. Stock, The George Washington University
Frederick X. Gibbons, University of Connecticut
Janine B. Beekman, The George Washington University
Meg Gerrard, University of Connecticut.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50(2):179–211. doi: 10.1080/08870446.2011.613995. [DOI] [Google Scholar]
- Albert D, Steinberg L. Judgment and decision making in adolescence. Journal of Research on Adolescence. 2011;21(1):211–224. doi: 10.1111/j.1532-7795.2010.00724.x. [DOI] [Google Scholar]
- Banks AP, Hope C. Heuristic and analytic processes in reasoning: An event-related potential study of belief bias. Psychophysiology. 2014;51(3):290–297. doi: 10.1111/psyp.12169. [DOI] [PubMed] [Google Scholar]
- Blanton H, VandenEijnden RJ, Buunk BP, Gibbons FX, Gerrard M, Bakker A. Accentuate the Negative: Social Images in the Prediction and Promotion of Condom Use. Journal of Applied Social Psychology. 2001;31(2):274–295. doi: 10.1111/j.1559-1816.2001.tb00197.x. [DOI] [Google Scholar]
- Boyer TW. The development of risk-taking: A multi-perspective review. Developmental Review. 2006;26:291–345. doi: 10.1016/j.dr.2006.05.002. [DOI] [Google Scholar]
- Brown SL. Relationships between risk-taking behavior and subsequent risk perceptions. British Journal of Psychology. 2005;96:155–164. doi: 10.1348/000712605X36703. [DOI] [PubMed] [Google Scholar]
- Buunk AP, Dijkstra P, Bosch ZA, Dijkstra A, Barelds DP. Social comparison orientation as related to two types of closeness. Journal of Research in Personality. 2012;46:279–285. doi: 10.1016/j.jrp.2012.02.008. [DOI] [Google Scholar]
- Buunk AP, Gibbons FX. Social comparison orientation: a new perspective on those who do and those who don't compare with others. In: Guimond S, editor. Social Comparison and Social Psychology; Understanding cognition, intergroup relations and culture. Cambridge: Cambridge University Press; 2006. pp. 15–33. [Google Scholar]
- Buunk AP, Gibbons FX. Social comparison: The end of a theory and the emergence of a field. Organizational Behavior and Human Decision Processes. 2007;102(1):3–21. doi: 10.1016/j.obhdp.2006.09.007. [DOI] [Google Scholar]
- Buunk BP, Gibbons FX. Health, coping, & well-being: Perspectives from social comparison theory. Mahwah, NJ: Lawrence Erlbaum; 1997. [Google Scholar]
- Buunk BP, Ybema JF. Social comparisons and occupational stress: The identification-contrast model. In: Buunk BP, Gibbons FX, editors. Health, coping, and well-being: Perspectives from social comparison theory. Mahwah, NJ US: Lawrence Erlbaum Associates Publishers; 1997. pp. 359–388. [Google Scholar]
- Centers for Disease Control and Prevention. Genital herpes – CDC fact sheet. 2006 Nov 15; Retrieved from http://www.cdc.gov/STd/herpes/STDFact-Herpes.htm.
- Centers for Disease Control and Prevention. Genital herpes – CDC fact sheet. 2014 May 15; Retrieved from http://www.cdc.gov/STd/herpes/STDFact-Herpes.htm.
- Chandra A, Mosher WD, Copen C. Sexual behavior, sexual attraction, and sexual identity in the United States: Data from the 2006-2008 National Survey of Family Growth. National Health Statistics Reports. 2011;36:1–36. [PubMed] [Google Scholar]
- Clark NM, Janevic MR. Theoretical models of health behavior change: Individual theories. In: Riekert, Ockene, Pbert, editors. The Handbook of Health Behavior Change. 4th. New York, NY: Springer; 2014. pp. 3–26. [Google Scholar]
- Corcoran K, Mussweiler T. The efficiency of social comparisons with routine standards. Social Cognition. 2009;27(6):939–948. doi: 10.1521/soco.2009.27.6.939. [DOI] [Google Scholar]
- Crosby RA, Yarber WL, Kanu A. Relationship of HIV/STD sexual risk behaviors to other health behaviors among a sample of Indiana rural youth. The Health Education Monograph Series. 1998;16(2):51–59. [Google Scholar]
- Croskerry P. A universal model of diagnostic reasoning. Academic Medicine. 2009;84(8):1022–1028. doi: 10.1097/ACM.0b013e3181ace703. [DOI] [PubMed] [Google Scholar]
- Dermen KH, Thomas SN. Randomized controlled trial of brief interventions to reduce college students' drinking and risky sex. Psychology of Addictive Behaviors. 2011;25(4):583. doi: 10.1037/a0025472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devarakonda SS, Neppalli A, Liu L, Friday E, Shi R. Risk factors and prevalence of genital HPV infection among adult females in US between 2003-2010: Data from NHANES study. Cancer Research. 2014;74(19 Supplement):278–278. [Google Scholar]
- Dohnke B, Steinhilber A, Fuchs T. Adolescents' eating behaviour in general and in the peer context: Testing the prototype-willingness model. Psychology & Health. 2014;30(4):381–399. doi: 10.1080/08870446.2014.974604. [DOI] [PubMed] [Google Scholar]
- Evans JSB. Dual-processing accounts of reasoning, judgment, and social cognition. Annual Review of Psychology. 2008;59:255–278. doi: 10.1146/annurev.psych.59.103006.093629. [DOI] [PubMed] [Google Scholar]
- Falchuk B. Falchuk B. Preggers. Hollywood, CA: Paramount Studios; 2009. Glee. [Google Scholar]
- Fisher JD, Fisher WA, Misovich SJ, Kimble DL, Malloy TE. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychology. 1996;15(2):114. doi: 10.1037/0278-6133.15.2.114. [DOI] [PubMed] [Google Scholar]
- Festinger L. A theory of social comparison processes. Human Relations. 1954;7(2):117–140. doi: 10.1177/001872675400700202. [DOI] [Google Scholar]
- French DP, Sutton SR, Marteau TM, Kinmonth AL. The impact of personal and social comparison information about health risk. British Journal of Health Psychology. 2004;9:187–200. doi: 10.1348/135910704773891041. [DOI] [PubMed] [Google Scholar]
- Gerend MA, Aiken LS, West SG, Erchull MJ. Beyond medical risk: investigating the psychological factors underlying women's perceptions of susceptibility to breast cancer, heart disease, and osteoporosis. Health Psychology. 2004;23:247–258. doi: 10.1037/0278-6133.23.3.247. [DOI] [PubMed] [Google Scholar]
- Gerrard M, Warner TD. A comparison of women Marine's and college women's HIV-relevant behaviors. Journal of Applied Social Psychology. 1994;24:959–980. doi: 10.1111/j.1559-1816.1994.tb02368.x. [DOI] [Google Scholar]
- Gerrard M, Gibbons FX, Benthin A, Hessling RM. A longitudinal study of the reciprocal nature of risk behaviors and cognitions in adolescents: What you do shapes what you think, and vice versa. Health Psychology. 1996;15:344–354. doi: 10.1037/0278-6133.15.5.344. [DOI] [PubMed] [Google Scholar]
- Gerrard M, Gibbons FX, Brody GH, Murry VM, Cleveland MJ, Wills TA. A theory-based dual-focus alcohol intervention for preadolescents: The Strong African American Families program. Psychology of Addictive Behaviors. 2006;20(2):185. doi: 10.1037/0893-164X.20.2.185. [DOI] [PubMed] [Google Scholar]
- Gerrard M, Gibbons FX, Houlihan AE, Stock ML, Pomery EA. A dual-process approach to health risk decision making: The prototype willingness model. Developmental Review. 2008;28(1):29–61. doi: 10.1016/j.dr.2007.10.001. [DOI] [Google Scholar]
- Gerrard M, Gibbons FX, Vande Lune LS, Pexa N, Gano M. Adolescents' substance-related risk perceptions: Antecedents, mediators, and consequences. Risk, Decision, and Policy. 2002;7:175–191. doi: 10.1017/S1357530902000637. [DOI] [Google Scholar]
- Gerrard M, Gibbons FX, Warner TD. Effects of reviewing risk-relevant behavior on perceived vulnerability among women Marines. Health Psychology. 1991;10:173–179. doi: 10.1037//0278-6133.10.3.173. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Buunk BP. Individual differences in social comparison: Development of a scale of social comparison orientation. Journal of Personality and Social Psychology. 1999;76:129–142. doi: 10.1037/0022-3514.76.1.129. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Etcheverry PE, Stock ML, Gerrard M, Weng CY, Kiviniemi M, O'Hara RE. Exploring the link between racial discrimination and substance use: what mediates? What buffers? Journal of Personality and Social Psychology. 2010;99(5):785. doi: 10.1037/a0019880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M. Predicting young adults' health risk behavior. Journal of Personality and Social Psychology. 1995;69:505–517. doi: 10.1037/0022-3514.69.3.505. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M, Ouellette JA, Burzette R. Cognitive antecedents to adolescent health risk: Discriminating between behavioral intention and behavior willingness. Psychology and Health. 1998a;13:319–339. doi: 10.1080/08870449808406754. [DOI] [Google Scholar]
- Gibbons FX, Gerrard M, Blanton H, Russell DW. Reasoned action and social reaction: Willingness and intention as independent predictors of health risk. Journal of Personality and Social Psychology. 1998b;74:1164–1180. doi: 10.1037/0022-3514.74.5.1164. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M, Lune LSV, Wills TA, Brody G, Conger RD. Context and cognitions: Environmental risk, social influence, and adolescent substance use. Personality and Social Psychology Bulletin. 2004;30(8):1048–1061. doi: 10.1177/0146167204264788. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Gerrard M, Lane DJ. A social reaction model of adolescent health risk. In: Suls JM, Wallston K, editors. Social Psychological Foundations of Health and Illness. Oxford, U.K: Blackwell; 2003. [DOI] [Google Scholar]
- Gibbons FX, Gerrard M, Stock ML, Finneran S. The Prototype/Willingness Model. In: Connor M, Norman P, editors. Predicting Health Behavior. in press. [Google Scholar]
- Gibbons FX, Houlihan AE, Gerrard M. Reason and reaction: The utility of a dual-focus, dual-processing perspective on promotion and prevention of adolescent health risk behaviour. British Journal of Health Psychology. 2009;14(2):231–248. doi: 10.1348/135910708X376640. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Lane DJ, Gerrard M, Pomery EA, Lautrup CL. Drinking and driving: A prospective assessment of the relation between cognitions and risk behavior. Risk Decision & Policy. 2002;7:267–283. doi: 10.1017/S1357530902000601. [DOI] [Google Scholar]
- Gibbons FX, Kingsbury JH, Gerrard M. Social-psychological theories and adolescent health risk behavior. Social and Personality Psychology Compass. 2011;10:1–14. doi: 10.1111/j.1751-9004.2011.00412.x. [DOI] [Google Scholar]
- Gulati R. What you need to know about STDs. Teen Vogue. 2012 Nov 12; Retrieved from http://www.teenvogue.com/beauty/health-fitness/2012-11/what-is-an-std-hpv-chlamydia.
- Gump B, Kulik J. The effect of a model's HIV status on self-perceptions: A self-protective similarity bias. Personality and Social Psychology Bulletin. 1995;21:827–833. doi: 10.1177/0146167295218005. [DOI] [Google Scholar]
- Halpern-Felsher BL, Millstein SG, Ellen JM, Adler NE, Tschann JM, Biehl M. The role of behavioral experience in judging risks. Health Psychology. 2001;20(2):120–126. doi: 10.1037/0278-6133.20.2.120. [DOI] [PubMed] [Google Scholar]
- Harris PR, Griffin DW, Murray S. Testing the limits of optimistic bias: Event and person moderators in a multilevel framework. Journal of Personality and Social Psychology. 2008;95:1225–1237. doi: 10.1037/a0013315. [DOI] [PubMed] [Google Scholar]
- Hofmann W, Friese M, Wiers RW. Impulsive versus reflective influences on health behavior: A theoretical framework and empirical review. Health Psychology Review. 2008;2(2):111–137. doi: 10.1080/17437190802617668. [DOI] [Google Scholar]
- Houlihan AE, Gibbons FX, Gerrard M, Yeh HC, Reimer RA, Murry VM. Sex and the self the impact of early sexual onset on the self-concept and subsequent risky behavior of African American adolescents. The Journal of Early Adolescence. 2008;28(1):70–91. doi: 10.1177/0272431607308670. [DOI] [Google Scholar]
- Howell JL, Shepperd JA. Behavioral obligation and information avoidance. Annals of Behavioral Medicine. 2013;45:258–263. doi: 10.1007/s12160-012-9451-9. [DOI] [PubMed] [Google Scholar]
- Idaho Department of Health & Welfare. The naked truth: My name is Amber. 2014 May 19; Retrieved from www.nakedtruth.idaho.gov/amber.aspx.
- Jacobs JE, Ganzel AK. Decision-making in adolescence: Are we asking the wrong question. Advances in Motivation and Achievement. 1993;8:1–31. [Google Scholar]
- Jarvis BG. MediaLab. New York, NY: Empirisoft; 2008. Computer Software. [Google Scholar]
- Klaczynski PA. Framing effects on adolescent task representations, analytic and heuristic processing, and decision making: Implications for the normative/descriptive gap. Journal of Applied Developmental Psychology. 2001;22(3):289–309. doi: 10.1016/S0193-3973(01)00085-5. [DOI] [Google Scholar]
- Klein WM. Objective standards are not enough: Affective, self-evaluative, and behavioral responses to social comparison information. Journal of Personality and Social Psychology. 1997;72:763–774. doi: 10.1037/0022-3514.72.4.763. [DOI] [PubMed] [Google Scholar]
- Klein WM. Self-prescriptive, perceived, and actual attention to comparative risk information. Psychology and Health. 2003;18(5):625–643. doi: 10.1080/0887044031000118465. [DOI] [Google Scholar]
- Klein WM, Cerully JL. Health-related risk perception and decision-making: lessons from the study of motives in social psychology. Social and Personality Psychology Compass. 2007;1(1):334–358. doi: 10.1111/j.1751-9004.2007.00023.x. [DOI] [Google Scholar]
- Klein WM, Shepperd JA, Suls J, Rothman AJ, Croyle RT. Realizing the promise of social psychology in improving public health. Personality and Social Psychology Review. 2014 doi: 10.1177/1088868314539852. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Klein WM, Weinstein ND. Social comparison and unrealistic optimism about personal risk. In: Buunk B, Gibbons F, editors. Health, Coping, and Well-being: Perspectives from Social Comparison Theory. Mahwah, New Jersey: Lawrence Erlbaum Associates; 1997. pp. 25–61. [Google Scholar]
- Kos JM, Clarke VA. Is optimistic bias influenced by control or delay? Health Education Research. 2001;16(5):533–540. doi: 10.1093/her/16.5.533. [DOI] [PubMed] [Google Scholar]
- Lane DJ, Gibbons FX, O'Hara RE, Gerrard M. Standing out from the crowd: How comparison to prototypes can decrease health-risk behavior in young adults. Basic and Applied Social Psychology. 2011;33(3):228–238. doi: 10.1080/01973533.2011.589296. [DOI] [Google Scholar]
- Langer E, Pirson M, Delizonna L. The mindlessness of social comparisons. Psychology of Aesthetics, Creativity, and the Arts. 2010;4(2):68. doi: 10.1037/a0017318. [DOI] [Google Scholar]
- Lermer E, Streicher B, Sachs R, Frey D. How risky? The impact of target person and answer format on risk assessment. Journal of Risk Research. 2013;16(7):903–919. doi: 10.1080/13669877.2012.761267. [DOI] [Google Scholar]
- Lewis LM, Rosenthal SL, Soccup PA, Stanberry LR, Bernstein DI. College students' knowledge and perceptions of genital herpes. International Journal of STD & AIDS. 1999;10:703–708. doi: 10.1258/0956462991913376. [DOI] [PubMed] [Google Scholar]
- Liberman A, Chaiken S. Defensive processing of personally relevant health messages. Personality and Social Psychology Bulletin. 1992;18:669–679. doi: 10.1177/0146167292186002. [DOI] [Google Scholar]
- Litt DM, Lewis MA, Stahlbrandt H, Firth P, Neighbors C. Social comparison as a moderator of the association between perceived norms and alcohol use and negative consequences among college students. Journal of Studies on Alcohol and Drugs. 2012;73(6):961–967. doi: 10.15288/jsad.2012.73.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litt DM, Stock ML, Gibbons FX. Adolescent alcohol use: Social comparison orientation moderates the impact of friend and sibling behavior. British Journal of Health Psychology. 2014 doi: 10.1111/bjhp.12118. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayhew A, Mullins TLK, Ding L, Rosenthal SL, Zimet GD, Morrow C, Kahn JA. Risk perceptions and subsequent sexual behaviors after HPV vaccination in adolescents. Pediatrics. 2014;133:404–411. doi: 10.1542/peds.2013-2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayo Clinic. Diseases and Conditions: Sexually Transmitted Diseases (STDs): Risk Factors. 2006 Retrieved November 2, 2006 from www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/basics/risk-factors/con-20034128.
- Mayo Clinic. Diseases and Conditions: Sexually Transmitted Diseases (STDs): Risk Factors. 2014 Retrieved June 2, 2014 from www.mayoclinic.org/diseases-conditions/sexually-transmitted-diseases-stds/basics/risk-factors/con-20034128.
- Millstein SG, Halpern-Felsher Perceptions of risk and vulnerability. Journal of Adolescent Health. 2001;31:10–27. doi: 10.1016/S1054-139X(02)00412-3. [DOI] [PubMed] [Google Scholar]
- Morrell HE, Song AV, Halpern-Felsher BL. Predicting adolescent perceptions of the risks and benefits of cigarette smoking: A longitudinal investigation. Health Psychology. 2010;29(6):610. doi: 10.1037/a0021237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mussweiler T, Bodenhausen GV. I know you are, but what am I? Self-evaluative consequences of judging in-group and out-group members. Journal of Personality and Social Psychology. 2002;82(1):19. doi: 10.1037/0022-3514.82.1.19. [DOI] [PubMed] [Google Scholar]
- Mussweiler T, Rüter K, Epstude K. The man who wasn't there: Subliminal social comparison standards influence self-evaluation. Journal of Experimental Social Psychology. 2004;40:689–696. doi: 10.1016/j.jesp.2004.01.004. [DOI] [Google Scholar]
- Paek HJ, Hove T, Ju Jeong H, Kim M. Peer or expert? The persuasive impact of YouTube public service announcement producers. International Journal of Advertising. 2011;30(1):161–188. doi: 10.2501/IJA-30-1-161-188. [DOI] [Google Scholar]
- Pflieger JC, Cook EC, Niccolai LM, Connell CM. Racial/ethnic differences in patterns of sexual risk behavior and rates of sexually transmitted infections among female young adults. American Journal of Public Health. 2013;103(5):903–909. doi: 10.2105/AJPH.2012.301005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomery EA, Gibbons FX, Reis-Bergan M, Gerrard M. From willingness to intention: Experience moderates the shift from reactive to reasoned behavior. Personality and Social Psychology Bulletin. 2009;35(7):894–908. doi: 10.1177/0146167209335166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Price PC, Smith AR, Lench HC. The effect of target group size on risk judgments and comparative optimism: The more, the riskier. Journal of Personality and Social Psychology. 2006;90(3):382. doi: 10.1037/0022-3514.90.3.382. [DOI] [PubMed] [Google Scholar]
- Reyna VF, Brainerd CJ. Dual processes in decision making and developmental neuroscience: A fuzzy-trace model. Developmental Review. 2011;31(2):180–206. doi: 10.1016/j.dr.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyna VF, Farley F. Risk and rationality in adolescent decision making: Implications for theory, practice, and public policy. Psychological Science in the Public Interest. 2006;7:1–44. doi: 10.1111/j.1529-1006.2006.00026.x. [DOI] [PubMed] [Google Scholar]
- Reyna VF, Rivers SE. Current theories of risk and rational decision making. Developmental Review. 2008;28(1):1–11. doi: 10.1016/j.dr.2008.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimal RN, Morrison D. A uniqueness to personal threat (UPT) hypothesis: How similarity affects perceptions of susceptibility and severity in risk assessment. Health Communication. 2006;20:209–219. doi: 10.1207/s15327027hc2003_1. [DOI] [PubMed] [Google Scholar]
- Rothman AJ, Kelly KM, Weinstein ND, O'Leary A. Increasing the salience of risky behavior: Promoting interest in HIV-antibody testing among heterosexually active young adults. Journal of Applied Social Psychology. 1999;29:531–551. doi: 10.1111/j.1559-1816.1999.tb01400.x. [DOI] [Google Scholar]
- Sheeran P, Harris PR, Epton T. Does heightening risk appraisals change people's intentions and behavior? A meta-analysis of experimental studies. Psychological bulletin. 2014;140(2):511–544. doi: 10.1037/a0033065. [DOI] [PubMed] [Google Scholar]
- Shepperd JA, Klein WM, Waters EA, Weinstein ND. Taking stock of unrealistic optimism. Perspectives on Psychological Science. 2013;8(4):395–411. doi: 10.1177/1745691613485247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloman SA. The empirical case for two systems of reasoning. Psychological Bulletin. 1996;119(1):3–22. doi: 10.1037/0033-2909.119.1.3. [DOI] [Google Scholar]
- Stanovich KE, Sá WC, West RF. Individual differences in thinking, reasoning, and decision making. In: Leighton JP, Sternberg RJ, editors. The Nature of Reasoning. New York, NY: Cambridge University Press; 2004. pp. 375–409. [Google Scholar]
- Stanovich KE, Toplak ME. Defining features versus incidental correlates of Type 1 and Type 2 processing. Mind & Society. 2012;11(1):3–13. doi: 10.1007/s11299-011-0093-6. [DOI] [Google Scholar]
- Stock ML, Peterson LM, Gibbons FX, Gerrard M. The effects of racial discrimination on the HIV-risk cognitions and behaviors of Black adolescents and young adults. Health Psychology. 2013;32(5):543. doi: 10.1037/a0028815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE, Brown JD. Illusion and well-being: A social psychological perspective on mental health. Psychological Bulletin. 1988;103:193–210. [PubMed] [Google Scholar]
- Tenkorang EY. A multilevel path analysis of risk perception and risky sexual behavior under the framework of the health belief model. Journal of HIV/AIDS & Social Services. 2013;12(2):125–145. doi: 10.1080/15381501.2013.764489. [DOI] [Google Scholar]
- Thornton B, Gibbons F, Gerrard M. Risk perception and prototype perception: Independent processes predicting risk behavior. Personality and Social Psychology Bulletin. 2002;28:986–999. doi: 10.1177/01467202028007011. [DOI] [Google Scholar]
- Todd J, Kothe E, Mullan B, Monds L. Reasoned versus reactive prediction of behaviour: A meta-analysis of the prototype willingness model. Health Psychology Review. 2014 doi: 10.1080/17437199.2014.922895. ahead of print. [DOI] [PubMed] [Google Scholar]
- Trumbo CW. Heuristic-systematic information processing and risk judgment. Risk Analysis. 1999;19(3):391–400. doi: 10.1111/j.1539-6924.1999.tb00415.x. [DOI] [PubMed] [Google Scholar]
- Trumbo CW. Information Processing and Risk Perception: An Adaptation of the Heuristic-Systematic Model. Journal of Communication. 2002;52(2):367–382. doi: 10.1111/j.1460-2466.2002.tb02550.x. [DOI] [Google Scholar]
- U.S. Department of Health and Human Services and Centers for Disease Control and Prevention. Sexual and reproductive health of person aged 10-24 years – United States, 2002-2007. 2009 CDC Publication No. 58. [Google Scholar]
- van der Velde F, van der Plight J, Hooykaas C. Perceiving AIDS-related risk: Accuracy as a function of difference in actual risk. Health Psychology. 1994;13:25–33. doi: 10.1037//0278-6133.13.1.25. [DOI] [PubMed] [Google Scholar]
- van Lettow B, De Vries H, Burdorf A, Van Empelen P. Quantifying the strength of the associations of prototype perceptions with behaviour, behavioural willingness, and intentions: A meta-analysis. Health Psychology Review. 2014 doi: 10.1080/17437199.2014.941997. [DOI] [PubMed] [Google Scholar]
- Walsh LA, Stock ML. Masculinity, UV photography, and college men's sun protection cognitions. Journal of Behavioral Medicine. 2012;35:431–442. doi: 10.1007/s10865-011-9372-2. [DOI] [PubMed] [Google Scholar]
- Walsh LA, Stock ML, Peterson LM, Gerrard M. Women's sun protection cognitions in response to UV photography: the role of age, cognition, and affect. Journal of Behavioral Medicine. 2013;37:553–563. doi: 10.1007/s10865-013-9512-y. [DOI] [PubMed] [Google Scholar]
- Webb TL, Sheeran P. Does changing behavioural intentions engender behavior change? A meta-analysis of the experimental evidence. Psychological Bulletin. 2006;132:249–268. doi: 10.1037/0033-2909.132.2.249. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. Unrealistic optimism about susceptibility to health problems. Journal of Behavioral Medicine. 1982;5:441–460. doi: 10.1007/BF00845372. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. Why it won't happen to me: Perceptions of risk factors and susceptibility. Health Psychology. 1984;3:431–457. doi: 10.1037/0278-6133.3.5.431.. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. Unrealistic optimism about susceptibility to health problems: Conclusions from a community-wide sample. Journal of Behavioral Medicine. 1987;10:481–500. doi: 10.1007/BF00846146. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. Optimistic biases about personal risks. Science. 1989;246:1232–1233. doi: 10.1126/science.2686031. [DOI] [PubMed] [Google Scholar]
- Weinstein ND, Klein WM. Resistance of personal risk perceptions to debiasing interventions. Health Psychology. 1995;14:132–140. doi: 10.1037/0278-6133.14.2.132. [DOI] [PubMed] [Google Scholar]
- Weinstein ND, Rothman AJ, Nicolich M. Use of correlational data to examine the effects of risk perceptions on precautionary behavior. Psychology and Health. 1998;13:479–501. doi: 10.1080/08870449808407305. [DOI] [Google Scholar]
- West SG, Aiken LS, Krull JL. Experimental personality designs: Analyzing categorical by continuous variable interactions. Journal of Personality. 1996;64(1):1–48. doi: 10.1111/j.1467-6494.1996.tb00813.x. [DOI] [PubMed] [Google Scholar]
- Winterbottom A, Bekker HL, Conner M, Mooney A. Does narrative information bias individual's decision making? A systematic review. Social Science & Medicine. 2008;67:2079–2088. doi: 10.1016/j.socscimed.2008.09.037. [DOI] [PubMed] [Google Scholar]
- Wood JV. Theory and research concerning social comparisons of personal attributes. Psychological Bulletin. 1989;106(2):231–248. doi: 10.1037/0033-2909.106.2.231. [DOI] [Google Scholar]
- Wu Y, Burns JJ, Stanton BF, Li X, Harris CV, Galbraith J, Wei L. Influence of prior sexual risk experience on response to intervention targeting multiple risk behaviors among adolescents. Journal of Adolescent Health. 2005;36:56–63. doi: 10.1016/j.jadohealth.2003.09.024. [DOI] [PubMed] [Google Scholar]
- Zimmermann F, Sieverding M. Young adults' social drinking as explained by an augmented theory of planned behaviour: The roles of prototypes, willingness, and gender. British Journal of Health Psychology. 2010;15(3):561–581. doi: 10.1348/135910709X476558. [DOI] [PubMed] [Google Scholar]