Abstract
Background
Carbapenem resistant Enterobacteriaceae (CRE) is increasingly reported worldwide. A similar increase is seen in Singapore since identification of its first case in 2008. The aim of this study was to identify local risk factors for carriage of CRE in patients from an acute tertiary care hospital in Singapore.
Method
A matched case-control study was conducted on inpatients treated from January 1, 2011 till December 31, 2013. Two hundred and three cases of CRE infection or colonization were matched with 203 controls. CRE types were identified by PCR. Statistical analysis of data including a multivariate logistic regression analysis was done using SPSS 21.0.
Results
CREs were commonly seen in Klebsiella pneumoniae (42.2 %), Escherichia coli (24.3 %) and Enterobacter cloacae complex (17.2 %) in the 268 isolates. NDM-1 was the commonest CRE type seen (44.4 %), followed by KPC (39.9 %) whilst OXA-48 only constituted (7.8 %). Univariate analysis identified key risk factors associated with CRE as history of previous overseas hospitalization (OR: 33.667; 95 % CI: 4.539-259.700), admission to ICU (OR: 11.899; 95 % CI: 4.986-28.399) and HD/ICA (OR: 6.557; 95 % CI: 4.057-10.596); whilst a multivariate analysis revealed exposure to antibiotics penicillin (OR: 4.640; 95 % CI: 1.529-14.079] and glycopeptide (OR: 5.162; 95 % CI: 1.377-19.346) and presence of central line device (OR: 3.117; 95 % CI: 1.167-8.330) as significant independent predictors.
Conclusions
The identification of risk factors amongst our local population helped to refine the criteria used for target active surveillance screening for CRE amongst inpatients at time of hospital admission.
Keywords: Enterobacteriaceae, Carbapenem resistant, Risk factors, Epidemiology
Introduction
Carbapenem resistant Enterobacteriaceae (CRE) is increasingly reported worldwide with increasing awareness of the global problem and improved methods of laboratory identification. Following the report of the emergence of the New Delhi metallo-β-lactamase-1 (NDM-1) in India, Pakistan, and the United Kingdom in 2010, there has also been much worldwide interest and concern of its increased epidemiology and potential impact on patient care. In Asia, Klebsiella pneumoniae Carbapenemase (KPC) was first detected in China in 2004 [1], and subsequently in South Korea and Taiwan [2, 3]. In Singapore, KPC was first reported in 2012 [4] where two of the four patients had strains closely related to the Chinese strain but the other two patients were non-Chinese with no travel history. The authors suggested possible community dissemination of KPC.
Shortly after the first discovery of the first NDM-1 patient at the Singapore General Hospital (SGH) in 2008, we noticed a steady gradual rise in the number of CRE patients in the subsequent years [5, 6]. This has significant implication on care of some of our patients requiring intermediate long term care (ILTC) management as some ILTCs were reluctant to receive CRE patients due to limited isolation facilities. Healthcare associated infections associated with multidrug resistant Gram negative bacilli have been shown to incur higher financial costs; although a significant proportion of which are subsidized by public funding in the form of governmental subvention in Singapore [7]. Moreover, there is also the risk of potential nosocomial CRE outbreaks arising from environmental contamination or lapses in infection control practices [8–11]. In light of these challenges and the fact that there are limited therapeutic options for the management of patients with CRE infections, we conducted a case-control study with the main objectives of identifying risk factors for carriage of CRE in our patients and enhancing existing strategies in controlling the spread of CRE amongst inpatients at our hospital.
Methods
Study design and population
We conducted a matched case-control study to identify risk factors associated with the acquisition of CRE amongst inpatients treated at SGH, a 1700-bed tertiary acute care hospital in Singapore. Cases were adults over age 18 years, whom CRE were isolated from clinical cultures from any source between January 1, 2011 and December 31, 2013. For each CRE patient, one control was randomly selected from adult inpatients admitted within the study period matched for gender, age, without CRE isolates. Subjects with CRE isolated from multiple sites or on multiple dates were counted only once where information from first event was collected as a case.
Data collection
Data were extracted from the patients’ medical records and from hospital computerized databases according to a pre-prepared questionnaire. Variables analyzed as possible predictors included demographics (age, gender, ethnic group, ward class), specific co-morbid conditions (cardiovascular, renal, diabetes mellitus, malignancy, transplantation, etc.), length of stay, history of admission from overseas hospital in the past one year, history of admission in the past one year, history of overseas travel in the past one year, admissions to intensive care unit (ICU), high dependency or intermediate care area (HD or ICA), invasive procedures, surgical procedures, presence of other multidrug resistant organisms (MDROs), invasive devices (within one month prior to CRE) and exposure (≥1 day(s)) to antimicrobials (imipenem, meropenem, ertapenem, doripenem, ciprofloxacin, vancomycin, cephalosporins, piperacillin-tazobacatam, metronidazole), and radiation therapy (deep x-ray therapy DXT) (within one month prior to CRE identification).
Microbiological methods
Carbapenem susceptibility was determined using disk diffusion and interpreted in accordance to the 2009 Clinical and Laboratory Standards Institute guidelines as per hospital’s clinical microbiology laboratory protocol. Carbapenemase-producing CRE were then identified using the modified Hodge test and the Roscoe test. Their CRE types were confirmed by the National Public Health Laboratory using the polymerase chain reaction (PCR) method.
Data analysis
The association of categorical variables with CRE patients was first examined using Χ2or Fisher exact test and Odds ratio (ORs) analysis with corresponding 95 % confidence intervals (CIs) computed. For continuous data, Student t tests and Mann-Whitney U tests were applied appropriately. A multivariate logistic regression analysis evaluated the independent contribution of the variables if p < 0.1, adjusted for total length of hospital stay. Statistical significance was considered when p was less than 0.05. Statistical analyses were performed using SPSS 21.0(SPSS, Chicago, IL, USA).
Results
Demographic data
Two hundred and three cases of CRE infection or colonization were identified between 1 January 2011–31 December 2013 and matched with 203 controls. The distributions of age, race, gender and ward classes are shown in Table 1.
Table 1.
Demographic details of CRE patients and control patients
| Demographic | CP-CRE patients | Control | Standards | X-value |
|---|---|---|---|---|
| (N = 203) | (N = 203) | (p-value) | ||
| n (%) | n (%) | n (%) | (case vs. standards) | |
| Mean age ± SD (years) | 64.3 ± 16.0 | 64.0 ± 15.7 | - | - |
| (mean years 95 % confidence interval) | (62.1–66.5) | (61.9–66.2) | ||
| Gender | ||||
| Male | 113 (55.7 %) | 113 (55.7 %) | 1,891,500 (49.2 %)[a] | 3.331 |
| Female | 90 (44.3 %) | 90 (44.3 %) | 1,953,200 (50.8 %)[a] | (0.068) |
| Paying class | ||||
| (based on collection ward) | ||||
| Class A | 16 (7.9 %) | 26 (12.8 %) | 5696 (7.2 %)[b] | |
| Class B1/B1+ | 20 (9.9 %) | 15 (7.4 %) | 9050 (11.5 %)[b] | 9.086 |
| Class B2 | 86 (42.4 %) | 77 (37.9 %) | 32,048 (40.8 %)[b] | (0.028)* |
| Class C | 81 (39.9 %) | 85 (41.9 %) | 24,028 (30.6 %)[b] | |
| Ethnic group | ||||
| Chinese | 134 (66.0 %) | 133 (72.7 %) | 2,853,800 (74.2 %)[a] | |
| Malay | 29 (14.3 %) | 32 (17.5 %) | 512,800 (13.3 %)[a] | 5.437 |
| Indian | 16 (7.9 %) | 16 (8.7 %) | 351,700 (9.1 %)[a] | (0.142) |
| Others (Singaporean) | 1 (0.5 %) | 2 (1.1 %) | 126,500 (3.3 %)[a] | |
| Others: Bangladeshi | 7 (3.4 %) | 1 (0.5 %) | - | - |
| Others: Burmese | 1 (0.5 %) | 1 (0.5 %) | - | - |
| Others: Chinese | 1 (0.5 %) | 4 (1.9 %) | - | - |
| Others: Indian | 2 (1.0 %) | 2 (1.0 %) | - | - |
| Others: Indonesian | 4 (1.9 %) | 4 (1.9 %) | - | - |
| Others: Malaysian | 2 (1.0 %) | 0 (0 %) | ||
| Others: Oman | 1 (0.5 %) | 0 (0 %) | ||
| Others: Pakistani | 2 (1.0 %) | 0 (0 %) | ||
| Others: Qatar | 0 (0 %) | 1 (0.5 %) | - | - |
| Others: Thai | 0 (0 %) | 1 (0.5 %) | - | - |
| Others: UAE | 0 (0 %) | 2 (1.0 %) | ||
| Others: Vietnamese | 3 (1.5 %) | 3 (1.5 %) | - | - |
*p < 0.05 (Significance of association; 2-tailed)
aDepartment of Statistics Singapore, 2013, Population Trends 2013
bSGH Bulletin Beds in Service by Ward and Bed Class (2013)
The common CRE isolated from 203 patients were Klebsiella pneumoniae (42.2 %), Escherichia coli (24.3 %) and Enterobacter cloacae complex (17.2 %). The cases were non-gender bias in the 32–96 years old age group with distribution as Chinese (66.0 %), Malay (14.3 %), Indian (7.9 %) and others (11.8 %). Average length of stay before the patient was identified with CRE was 21.1 ± 40.5 days.
Isolation sites and types of CRE
The distribution of isolation sites of the 268 isolates are shown in Fig. 1. CRE was commonly isolated from stool/rectal swab (61.6 %), urine (13.1 %) and other clinical sites (25.3 %). NDM-1 was the commonest CRE type seen (44.4 %), followed by KPC (39.9 %) whilst OXA-48 only constituted 7.8 % (Fig. 2).
Fig. 1.
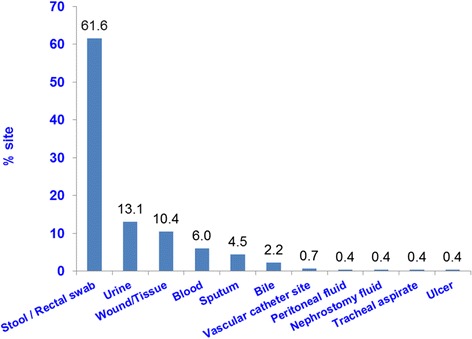
Distribution of CRE by isolation sites
Fig. 2.
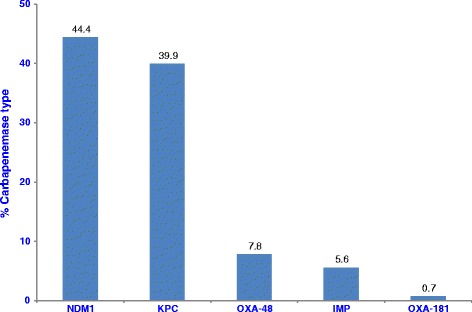
Carbapenemase types isolated
Risk factor analysis
The mean total length of hospital stay is significantly longer in CRE cases than controls (48.0 vs 3.9 days, p < 0.001). Significant risk factors of the univariate analysis were summarized in Table 2. Higher proportions of CRE cases had an exposure to health care with history of previous overseas hospitalization (OR: 33.667; 95 % CI: 4.539–259.700), admission to ICU (OR: 11.899; 95 % CI: 4.986–28.399) and HD/ICA (OR: 6.557; 95 % CI: 4.057–10.596), with need for urinary catheter (OR: 4.239; 95 % CI: 2.630–6.831), drains (OR: 3.146; 95 % CI: 1.534–6.450) and enteral feeding (OR: 5.554; 95 % CI: 2.793–11.044). CRE cases were less likely to be ambulant upon arrival (OR: 0.337; 95 % CI: 0.221–0.513), and more likely to have comorbidities such as cardiovascular disease (OR: 1.868; 95 % CI: 1.256–2.778) and hematology conditions (OR: 4.328; 95 % CI: 1.592–11.769). They were also exposed to immunosuppressive treatments of DXT (OR: 2.230; 95 % CI: 1.057–4.706) and steroid (OR: 3.202; 95 % CI: 1.606–6.384). CRE cases were also exposed to a variety of antibiotics classes which included β-lactam/β-lactamase inhibitor combinations (OR: 3.676; 95 % CI: 2.432–5.557) and fluoroquinolones (OR: 2.018; 95 % CI: 1.111–3.663). In addition, CRE cases harbored other MDROs: MRSA (OR: 2.051; 95 % CI: 1.213–3.468) and VRE (OR: 7.411; 95 % CI: 2.825–19.441) and were exposed to invasive procedures of bronchoscopy (OR: 6.047; 95 % CI: 2.045–17.881).
Table 2.
Univariate analysis of risk factors associated with CRE carriage
| Risk factors | CP-CRE patients | Control | X = value/Mann-Whitney U | Odds Ratio |
|---|---|---|---|---|
| (N = 203) | (N = 203) | (p-value/Fisher Exact) | [95 % Cl] | |
| n (%) | n (%) | |||
| Total length of stay ± SD | 48.0 ± 59.5 | 3.9 ± 3 8 | U: 3223 | 1.266 [1.197–1.340] |
| (days) | (39.8–56.3) | (3.4–4.5) | (<0.001) | (<0.001) |
| (moan days 95 % confidence interval) | ||||
| History of previous overseas hospitalisation | 29 (14.3 %) | 1 (0.5 %) | 28.218 (<0.001)** | 33.667 [4.539–259.700] |
| History of travelling in past 90 days | 29 (14.3 %) | 15 7.4 %) | 4.996 (0.025)* | 2.089 [10.83.4.028] |
| Ambulant on arrival | 103 (50.7 %) | 153 (75.4 %) | 26.432 (<0.001)** | 0.337 [0.221–0.513] |
| Admission to CU | 54 (26.6 %) | 6 (3.0 %) | 45.059 (<0.001)** | 11.899 [4.986–28.399] |
| Mean ICU stay ± SD, day | 9.6 ± 12.2 | 1.2 ± 1.0 | U: 46.0 (<0.004)** | - |
| (mean days 95 % confidence interval) | (6.3—13.0) | (0.1—2.2) | ||
| Admission to HD/ICA | 106 (52.2 %) | 29 (14.3 %) | 65.797 (<0.001)** | 6.557 [4.057–10.596] |
| Mean HD/ICA stay ± SD, day | 5.3 ± 6.1 | 2.0 ± 1.7 | 9.0 (0.372) | - |
| (mean days 95 % confidence interval) | (4.1–6.5) | (1.4–2.7) | ||
| Cardiovascular disease comorbidity | 105 (51.7 %) | 74 (36.5 %) | 9.602 (0.002)** | 1.868 [1.256–2.778] |
| Diabetes mellitus comorbidity | 67 (33.0 %) | 58 (28.6 %) | 0.936 (0.333) | 1.232 [0.807–1.870] |
| Malignancy cormorbidity | 57 (28.1 %) | 41 (20.2 %) | 3.443 (0.064) | 1.543 [0.974–2.442] |
| Immunodeficiency comorbidity | 10 (4.9 %) | 2 (1.0 %) | 5.496 (0.019)* | 5.207 [1.126–24.072] |
| Haematology comorbidity | 20 (9.9 %) | 5 (2.5 %) | 9.591 (0.002)** | 4.328 [1.592–11.769] |
| Exposure to DXT | 23 (11.3 %) | 11 (5.4 %) | 4.622 (0.032)* | 2.230 [1.057–4.706] |
| Exposure to steroid | 34 (16.7 %) | 12 (5.9 %) | 11.866 (0.001)** | 3.202 [1.606–6.384] |
| Exposure to chemotherapy | 15 (7.4 %) | 16 (7.9 %) | 0.035 (0.852) | 0.933 [0.448–1.941] |
| Exposure to penicillin antibiotics | 33 (16 3 %) | 7 (3.4 %) | 18.747 (<0.001)** | 5.435 [2.344–12.604] |
| Exposure to β-lactam/β-lactamase inhibitor combinations antibiotics | 122 (60.1 %) | 59 (29.1 %) | 39.568 (<0.001)** | 3.676 [2.432–5.557] |
| Exposure to cephalosporin antibiotics | 65 (32.0 %) | 43 (21.2 %) | 6.106 (0.013)* | 1.753 [1.120–2.742] |
| Exposure to carbapenems antibiotics | 62 (30.5 %) | 5 (2.5 %) | 58.077 (<0.001)** | 17.413 [6.826–44.417] |
| Exposure to fluoroquinolones antibiotics | 35 (17.2 %) | 19 (9.4 %) | 5.468 (0.019)* | 2.018 [1.111–3.663] |
| Exposure to glycopeptide antibiotics | 69 (34.0 %) | 4 (2.0 %) | 70.564 (<0001)** | 25.618 [9.132–71.865] |
| Exposure to metronidazole antibiotics | 36 (17.7 %) | 15 (7.4 %) | 9.889 (0.002)** | 2.702 [1.428–5.110] |
| Exposure to aminoglycosides antibiotics | 17 (8.4 %) | 1 (0.5 %) | 14.882 (<0.001)** | 18.462 [2433–140,097] |
| Presence of central line device | 80 (39.4 %) | 11 (5.4 %) | 67.433 (<0.001)** | 11.353 [5.811–22.179] |
| Presence of urinary catheter device | 86 (42.4 %) | 30 (14.8 %) | 37.842 (<0.001)** | 4.239 [2.630–6.831] |
| Presence of ETT device | 42 (20.7 %) | 6 (3.0 %) | 30.620 (<0.001)** | 8.565 [3.55 1–20.658] |
| Presence of intra-arterial line device | 24 (11.8 %) | 5 (2.5 %) | 13.406 (<0.001)** | 5.309 [1.984–14.2 11] |
| Presence of drains device | 31 (15.3 %) | 11 (5.4 %) | 10.623 (0.001)** | 3.146 [1.534–6.450] |
| Presence of enteral feeding device | 49 (24.1 %) | 11 (5.4 %) | 28.240 (<0.001)** | 5.554 [2.793–11.044] |
| Presence of additional MRSA | 47 (23.2 %) | 26 (12.8 %) | 7.365 (0.007)** | 2.051 [1.213–3.468] |
| Presence of additional VRE | 32 (15.8 %) | 5 (2.5 %) | 21.678 (<0.001)** | 7.411 [2.825-19.441] |
| Exposure to bronchoscopy procedure | 22 (10.8 %) | 4 (2.0 %) | 13.314 (<0.001)** | 6.047 [2.045–17.881] |
| Exposure to gastroscopy procedure | 18 (8.9 %) | 10 (4.9 %) | 2.455 (0.117) | 1.878 [0.845–4.175] |
| Exposure to colonoscopy procedure | 4 (2.0 %) | 6 (3.0 %) | 0.410 (0.522) | 0.660 [0.183–2.375] |
| Exposure to angiogram procedure | 9 (4.4 %) | 6 (3.0 %) | 0.623 (0.430) | 1.523 [0.532–4361] |
| Underwent surgery | 141 (69.5 %) | 146 (71.9 %) | 0.297 (0.586) | 1.126 [0.734–1.727] |
*p < 0.05 (Significance of association; 2-tailed), **p < 0.01 (Significance of association; 2-tailed)
The results for the multivariate analysis were presented in Table 3. Upon adjustment for total length of hospital stay, exposure to antibiotics penicillin (OR: 4.640; 95 % CI: 1.529–14.079] and glycopeptide (OR: 5.162; 95 % CI: 1.377–19.346) and presence of central line device (OR: 3.117; 95 % CI: 1.167–8.330) emerged as significant independent predictors associated with CRE.
Table 3.
Multivariate analysis of risk factors
| Risk factor (Multivariable model) | Adjusted Odds Ratio |
|---|---|
| [95 % Confidence Interval] | |
| (Sig) | |
| Exposure to antibiotics penicillin | 4.640 [1.529–14.079] (0.007)* |
| Exposure to antibiotics glycopeptides | 5.162 [1.377–19.346] (0.015)** |
| Presence of central line device | 3.117 [1.167–8.330] (0.023)** |
*p < 0.01; **p < 0.05 (Significance of association; 2-tailed)
Outcomes
There were 37 (18.2 %) mortalities amongst the CRE cases. CRE cases had ~3.5 times odds of fatality adjusted for length of hospital stay (adjusted OR: 3.532; 95 % CI: 1.281–9.741; p: 0.015) compared to controls. No outbreak was noted during the study period.
Discussion
Interestingly, the results of our case-control study revealed different risk factors from other investigators. Twenty-nine of our 203 cases (85.7 %) had no history of overseas travel in the past 90 days before admission and had no previous overseas hospitalization. Hence, it is likely that CRE is already in our community setting.
Our study identified similar risk factors that other investigators have highlighted-exposure to antimicrobials, especially carbapenems and fluoroquinolones [12–15], admission to ICU [16]; presence of indwelling devices [17] e.g. central line, urinary catheter, endotracheal tube and the enteral feeding tube. In addition, our study identified unique risk factors viz. hematology patients and those with immunodeficiency. This may be explained by the recurring admissions and discharges as well as a relatively longer length of stay in this patient population exposing them to greater risk than the general patient population.
Our multivariate analysis showed similar findings with other investigators [18, 19] that antimicrobial usage, increased risk for CRE colonization. Penicillin use was associated with increased risk for CRE colonization among patients admitted to the hospital, as in our study. From 2011 to 2013, there were 11 patients with CP-CRE bacteraemia; four of these (36.3 %) had a central venous pressure (CVP) line. Indwelling devices are recognised risk factors for healthcare-associated infections [20, 21]. Hence, it is not surprising to see the presence of a CVP line as an independent risk factor for CRE infection. This highlights the importance of safe patient care practices especially in the care of devices as well as the significance of an antimicrobial stewardship program in the strategy for the prevention of CRE infections.
We conducted a preliminary data analysis for risk factors from the 2011–2012 data and identified criteria for active surveillance for CRE as part of an effort to reduce the incidence of CRE. From January 2013, the criteria used were history of overseas travel in the past one year, transfers from overseas hospital and history of admissions to private hospitals in Singapore in past one year. This was modified to include admissions to ICU, high dependency units and intermediate care units (October 2013); renal (March 2014), haematology (April 2014), oncology (June 2014). Since then, our healthcare-associated CRE has stabilized to 0.28 per 1000 patient days (2014) from previous rates of 0.03 and 0.26 respectively (2012, 2013). We were able to institute prompt isolation and control measures upon knowing the active surveillance screening results. This helped to prevent horizontal transmission between patients in our general wards, where most patients are housed in open wards with 4–8 beds in a cubicle.
Our study has several limitations. Firstly, CRE was identified from clinical specimens submitted to the Microbiology Laboratory. Active surveillance for CRE carriage was not done during 2011–2012 and the CRE carriage rate could have been higher than found. Secondly, because active surveillance for CRE was not done at admission, we were not able to determine if the patients had acquired it during their inpatient stay. A case control study involving multiple centers or over a longer period may help to overcome the problem of small sample size. Our study is underpowered at 47.4 % (α: 0.05) as we only had 203 patients in each arm. For power to be at 80 %, we would need 855 patients in each arm [22]. This study investigated the risk factors for being colonized with CRE in our patient population. Acquisition was not studied as exit swabs were not done for those who had entry screening swabs done. Hence, it will not be possible to correlate the link between the risk factors and acquisition.
Conclusions
The global increase in CRE in many healthcare facilities poses challenges to infection control and infectious disease professionals. Risk-based screening is one strategy that has been used to limit the spread of CRE in healthcare settings [18, 19, 23]. We have demonstrated the value of understanding local epidemiology to help modify our risk-based screening as a strategy to limit the spread of CRE. Hence, we recommend targeted screening strategies to identify patients colonized with CRE at the time of admission to a healthcare institution as a component of a CRE reduction program.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MLL conceptualized the project, performed literature search, analysed data, responded to reviewers and wrote the first and revised drafts of the manuscript; YMT, SGT, IMA, KBH, KYT and LCL collected data and analysed data; IMA conducted the data analyses interpretation of data and contributed to response to reviewers and revision of the drafts. All authors read and approved the final manuscript.
Contributor Information
Moi Lin Ling, Email: ling.moi.lin@sgh.com.sg.
Yong Ming Tee, Email: tee.yong.ming@sgh.com.sg.
Soong Geck Tan, Email: tan.soong.geck@sgh.com.sg.
Ismawati M. Amin, Email: ismawati.mohd.amin@sgh.com.sg
Kue Bien How, Email: molly.how.k.b@sgh.com.sg.
Kwee Yuen Tan, Email: tan.kwee.yuen@sgh.com.sg.
Lai Chee Lee, Email: lee.lai.chee@sgh.com.sg.
References
- 1.Wei ZQ, Du XX, Yu YS, et al. Plasmid-mediated KPC-2 in a Klebsiella pneumoniae isolate from China. Antimicrob Agents Chemother. 2007;51:763–5. doi: 10.1128/AAC.01053-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rhee JY, Park YK, Shin JY, et al. KPC-producing extreme drug-resistant Klebsiella pneumoniae isolate from a patient with diabetes mellitus and chronic renal failure on hemodialysis in South Korea. Antimicrob Agents Chemother. 2010;54:2278–9. doi: 10.1128/AAC.00011-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chia JH, Su LH, Lee MH, et al. Development of high-level carbapenem resistance in Klebsiella pneumoniae among patients with prolonged hospitalization and carbapenem exposure. Microb Drug Resist. 2010;16:317–25. doi: 10.1089/mdr.2009.0048. [DOI] [PubMed] [Google Scholar]
- 4.Balm MN, Ngan G, Jureen R, Lin RT, Teo J. Molecular characterization of newly emerged blaKPC-2-producing Klebsiella pneumoniae in Singapore. J Clin Microbiol. 2012;50:475–6. doi: 10.1128/JCM.05914-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yong D, Toleman MA, Giske CG, et al. Characterisation of a new metallo- β -lactamase gene, bla NDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob Agents Chemother. 2009;53:5046–54. doi: 10.1128/AAC.00774-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chien JM, Koh TH, Chan KS, et al. Successful treatment of NDM-1 Klebsiella pneumoniae bacteraemia in a neutropenic patient. Scand J Infect Dis. 2012;44:312–4. doi: 10.3109/00365548.2011.633549. [DOI] [PubMed] [Google Scholar]
- 7.Ng E, Earnest A, Lye DC, et al. The excess financial burden of multidrug resistance in severe gram-negative infections in Singaporean hospitals. Ann Acad Med Singapore. 2012;41:189–93. [PubMed] [Google Scholar]
- 8.Ben-David D, Maor Y, Keller N, et al. Potential role of active surveillance in the control of a hospital-wide outbreak of carbapenem-resistant Klebsiella pneumoniae infection. Infect Control Hosp Epidemiol. 2010;31:620–6. doi: 10.1086/652528. [DOI] [PubMed] [Google Scholar]
- 9.Munoz-Price LS, Cuesta CDL, Adams S, et al. Successful eradication of a monoclonal strain of Klebsiella pneumoniae during a K. pneumoniae carbapenemase-producing K. pneumoniae outbreak in a surgical intensive care unit in Miami, Florida. Infect Control Hosp Epidemiol. 2010;31:1074–7. doi: 10.1086/656243. [DOI] [PubMed] [Google Scholar]
- 10.Lerner A, Abu-Hanna K, Meitus I, et al. Environmental contamination by carbapenem-resistant Enterobacteriaceae. J Clin Microbiol. 2013;51:177–81. doi: 10.1128/JCM.01992-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kotsanas D, Wijesooriay WR, Korman TM, et al. “Down the drain”: carbapenem-resistant bacteria in intensive care unit patients and handwashing sinks. Med J Aust. 2013;198:267–9. doi: 10.5694/mja12.11757. [DOI] [PubMed] [Google Scholar]
- 12.Kritsotakis EI, Tsioutis C, Roumbelaki M, et al. Antibiotic use and the risk of carbapenem-resistant extended spectrum-β-lactamase-producing Klebsiella pneumoniae infection in hospitalized patients: results of a double case–control study. J Antimicrob Chemother. 2011;66:1383–91. doi: 10.1093/jac/dkr116. [DOI] [PubMed] [Google Scholar]
- 13.Schechner V, Kotlovsky T, Tarabeia J, et al. Predictors of rectal carriage of carbapenem-resistant Enterobacteriaceae (CRE) among patients with known CRE carriage at their next hospital encounter. Infect Control Hosp Epidemiol. 2011;32:497–503. doi: 10.1086/659762. [DOI] [PubMed] [Google Scholar]
- 14.Patel N, Harrington S, Dihmess A, et al. Clinical epidemiology of carbapenem-intermediate or –resistant Enterobacteriaceae. J Antimicrob Chemother. 2011;66:1600–8. doi: 10.1093/jac/dkr156. [DOI] [PubMed] [Google Scholar]
- 15.Liu S, Chang H, Chia J, et al. Outcomes and characteristics of ertapenem non-susceptible Klebsiella pneumoniae bacteremia at a university hospital in Northern Taiwan: a matched case-control study. J Microbiol Immunol Infect. 2012;45:113–9. doi: 10.1016/j.jmii.2011.09.026. [DOI] [PubMed] [Google Scholar]
- 16.Lee GC, Lawson KA, Burgess DS. Clinical epidemiology of carbapenem-resistant Enterobacteriaceae in community hospitals: a case-case-control study. Ann Pharmacother. 2013;47:1115–21. doi: 10.1177/1060028013503120. [DOI] [PubMed] [Google Scholar]
- 17.Bhargava A, Hayakawa K, Silverman E, et al. Risk factors for colonization due to carbapenem-resistant Enterobacteriaceae among patients exposed to long-term acute care and acute care facilities. Infect Control Hosp Epidemiol. 2014;35:398–405. doi: 10.1086/675614. [DOI] [PubMed] [Google Scholar]
- 18.Borer A, Saidel-Odes L, Eskira S, et al. Risk factors for developing clinical infection with carbapenem-resistant Klebsiella pneumoniae in hospital patients initially only colonized with carbapenem-resistant K pneumoniae. Am J Infect Control. 2012;40:421–5. doi: 10.1016/j.ajic.2011.05.022. [DOI] [PubMed] [Google Scholar]
- 19.Falagas ME, Rafailidis PI, Kofteridis D, et al. Risk factors of carbapenem-resistant Klebsiella pneumoniae infections: a matched case control study. J Antimicrob Chemother. 2007;60:1124–30. doi: 10.1093/jac/dkm356. [DOI] [PubMed] [Google Scholar]
- 20.Rosenthal VD, Maki DG, Salomao R, et al. Device-associated nosocomial infections in 55 intensive care units of 8 developing countries. Ann Intern Med. 2006;145:582–91. doi: 10.7326/0003-4819-145-8-200610170-00007. [DOI] [PubMed] [Google Scholar]
- 21.Moreno CA, Rosenthal VD, Olarte N, et al. Device-associated infection rate and mortality in intensive care units of 9 Colombian hospitals: findings of the International Nosocomial Infection Control Consortium. Infect Control Hosp Epidemiol. 2006;27:349–56. doi: 10.1086/503341. [DOI] [PubMed] [Google Scholar]
- 22.Whitley E, Ball J. Statistics Review 4. Sample size calculations. Crit Care. 2002;6:335–41. doi: 10.1186/cc1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chitnis AS, Caruthers PS, Rao AK, et al. Outbreak of carbapenem-resistant Enterobacteriaceae at a long-term acute care hospital: sustained reductions in transmission through active surveillance and targeted interventions. Infect Control Hosp Epidemiol. 2012;33:984–92. doi: 10.1086/667738. [DOI] [PubMed] [Google Scholar]


