Abstract
Background
Regular physical activity plays an important role in the amelioration of several mental health disorders; however, its relationship with burnout has not yet been clarified.
Objective
To determine the association between achievement of national physical activity guidelines and burnout in internal medicine resident physicians.
Methods
A Web-based survey of internal medicine resident physicians at the University of Minnesota and Hennepin County Medical Center was conducted from September to October 2012. Survey measures included the Maslach Burnout Inventory-Human Services Survey and the International Physical Activity Questionnaire.
Results
Of 149 eligible residents, 76 (51.0%) completed surveys, which were used in the analysis. Burnout prevalence, determined by the Maslach Burnout Inventory, was 53.9% (41 of 76). Prevalence of failure to achieve US Department of Health and Human Services physical activity guidelines was 40.8% (31 of 76), and 78.9% (60 of 76) of residents reported that their level of physical activity has decreased since they began medical training. Residents who were able to meet physical activity guidelines were less likely to be burned out than their fellow residents (OR, 0.38, 95% CI 0.147–0.99).
Conclusions
Among internal medicine resident physicians, achievement of national physical activity guidelines appears to be inversely associated with burnout. Given the high national prevalence of burnout and inactivity, additional investigation of this relationship appears warranted.
What was known
Regular physical activity may be important in reducing the risk for burnout, though this relationship has not been formally studied.
What is new
A sizable percentage of internal medicine residents did not meet guidelines for adequate physical activity, while residents who met guidelines were less likely to meet criteria for burnout.
Limitations
Survey study with self-reporting; single specialty study reduces generalizability.
Bottom line
The protective properties of physical activity merit further study and should be communicated to residents in an effort to reduce burnout.
Editor's Note: The online version of this article contains tables of demographics by burnout status and items pertaining to residency and physical activity by burnout status.
Introduction
The practice of medicine is changing: Work pressure has increased, autonomy is diminishing, and the elevated status physicians have historically enjoyed is eroding.1 A consequence of these changes is burnout—defined as a syndrome of emotional exhaustion and depersonalization accompanied by a decreased sense of personal accomplishment in those who work closely with people.2,3
Burnout is highly prevalent in medical professionals.1,4–6 Residency training presents a particular burden due to long hours, sleep deprivation, irregular schedules, intense emotional demands, as well as the pressure to master a large body of clinical knowledge.5,7,8 Added to this are other issues common during medical residency, including work/home conflicts, loan debt, limited emotional support, fatigue, and lack of confidence in one's own skill.9–13
Prevalence of burnout varies by specialty, and estimates for internal medicine residents range from 55% to 76%.4,5,8,13–18 The consequences of burnout are potentially quite serious and include deterioration of the quality of care provided by the resident, turnover, absenteeism, and low job satisfaction and morale.2,19,20 Additionally, rates of depression as well as suicidal ideation, plans, and attempts have been linked to burnout status.8,17,21,22 Self-reported medical errors as well as suboptimal patient care are disproportionately reported in persons who meet criteria for burnout.4,18,23
Health benefits from sustained, regular physical activity are broad, including the important role it plays in the amelioration of several mental health disorders, specifically depression and anxiety.24–27 Physicians, in general, enjoy healthier lifestyles and lower mortality than the general public.28,29 However, there is evidence that resident physicians are less likely to engage in regular physical activity than medical students or attending physicians.30,31
Despite the potentially serious consequences of burnout, an understanding of its relationship with physical activity in resident physicians is lacking. We sought to investigate the burnout status and physical activity level of resident physicians. We hypothesized that achievement of national physical activity guidelines would be inversely associated with burnout status.
Methods
Participants
The internal medicine residency programs at the University of Minnesota and Hennepin County Medical Center were selected to participate in this study. Hennepin County Medical Center matches approximately 20 residents to their program annually, and the University of Minnesota has 30 residents per year. All residents were eligible for participation in this study.
Data Collection
We surveyed the residents using a single, self-administered questionnaire distributed electronically through a popular online survey tool (SurveyMonkey). A link to the survey was e-mailed to each program director, who forwarded it to their residents. After gaining consent, participants were asked to complete the questionnaire online. Data were collected from September to October 2012.
Survey Measures
The questionnaire incorporated the instruments described below. We collected basic demographic information and information regarding call schedule, work hours, sleep, and perceptions concerning residency and physical activity. Age, sex, and postgraduate year were gathered from each training program for all residents potentially sampled.
Job burnout was measured using the self-administered Maslach Burnout Inventory-Human Services Survey (MBI-HSS), which has been validated in multiple populations and is widely considered the gold standard for assessing burnout.2,6 The survey includes 22 questions in 3 domains. Using norms for medical professionals, burnout was detected based on threshold scores for emotional exhaustion (≥ 27), depersonalization (≥ 10), and personal accomplishment (≤ 33).2
To aid in comparability with other studies, results were converted into a 1-dimension construct, defining respondents with high subscores in emotional exhaustion or depersonalization as “burned out.” Personal accomplishment was not used, as previous research has suggested that it may measure a somewhat distinct quality from the other 2 domains.2–4
We used the International Physical Activity Questionnaire Short Form (IPAQ-SF) to quantify respondents' physical activity level. Research indicates that it is valid and reliable for assessing physical activity, although it has not been formally tested in resident physicians or individuals with burnout.32–35 Completion of this tool required answering 7 brief questions assessing the frequency and time spent performing vigorous and moderate physical activity as well as walking.36
Current US Department of Health and Human Services (DHHS) guidelines indicate that there are substantial health benefits when adults participate in at least 150 minutes per week of moderate intensity physical activity, 75 minutes per week of vigorous intensity physical activity, or an equivalent combination of the 2.37 These criteria were used to classify respondents. The DHHS guidelines classify walking at a brisk pace as moderate physical activity. However, the IPAQ-SF does not differentiate casual walking from brisk walking, and we used a more stringent definition of the volume of moderate activity achieved that did not include time spent walking.
The study received approval from the University of Minnesota's and Hennepin County Medical Center's institutional review boards.
Statistical Analysis
Data for analysis were obtained after collection and analyzed using SAS version 9.3 (SAS Institute Inc). Descriptive summary statistics using frequency and mean procedures were generated. Bivariate tables were created for variables of interest, and hypothesis testing using Student t test, χ2, or Fisher exact test were done. Two-sided alpha levels of P values < .05 were considered statistically significant. Logistic regression procedures were used to determine effect measures in the form of odds ratios (ORs) and 95% CIs were also determined.
Results
Of the 149 residents in both programs, 78 completed both the IPAQ-SF and the MBI-HSS. One survey was excluded as the participant had completed it twice, and another was excluded as the participant was not an internal medicine resident. The 76 completed surveys represent a 51% response rate.
Participant Demographics
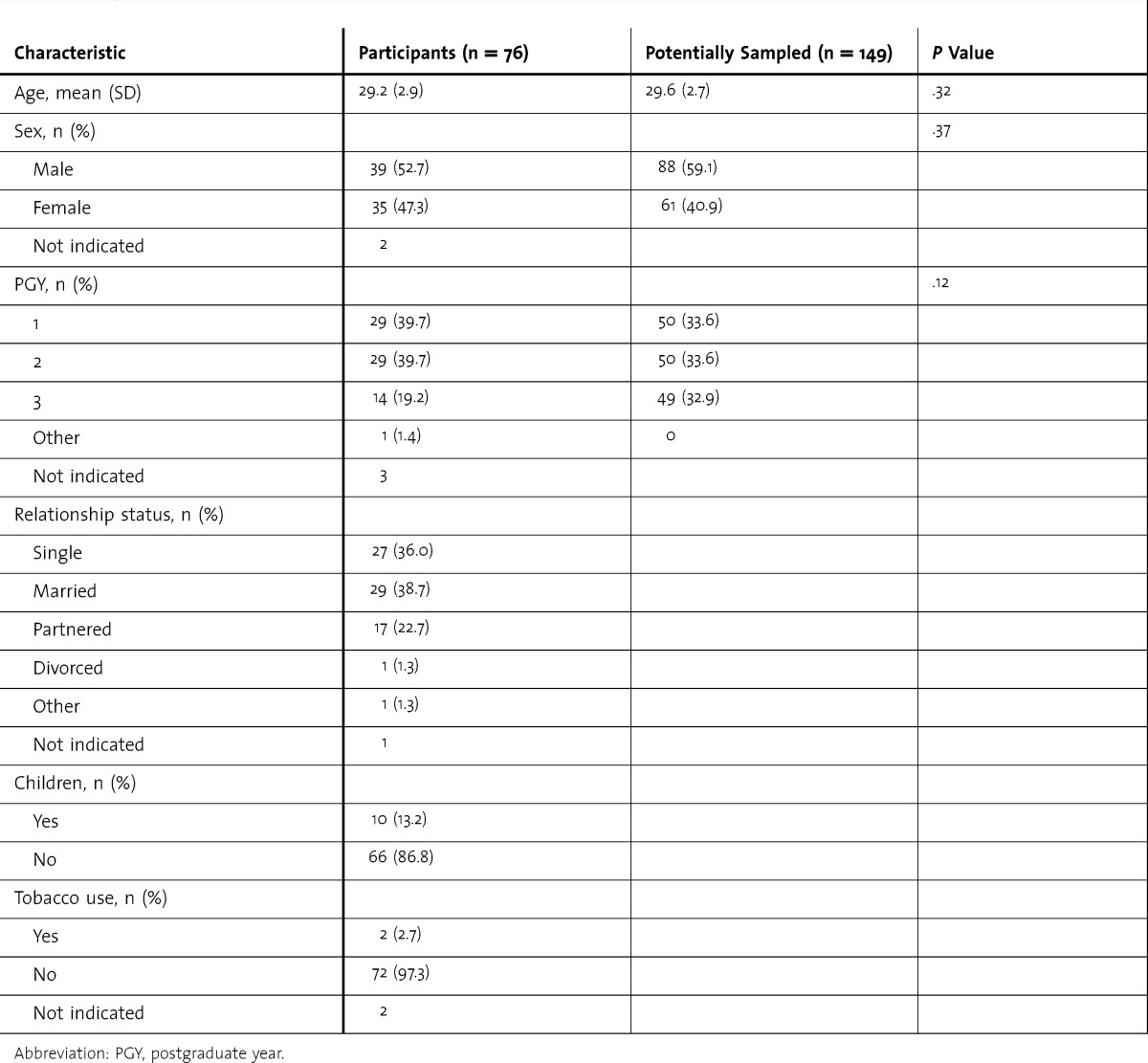
Around half (52.7%) of the respondents were men, with the average age less than 30. Response rate was proportional between postgraduate year (PGY)-1 and 2. PGY-3 was less well represented in this sample, though this did not reach the threshold for statistical significance. Most respondents were married or partnered, did not have children, and were nonsmokers (table 1).
TABLE 1.
Demographics of Participants and Potentially Sampled Population
Association Between Physical Activity and Burnout
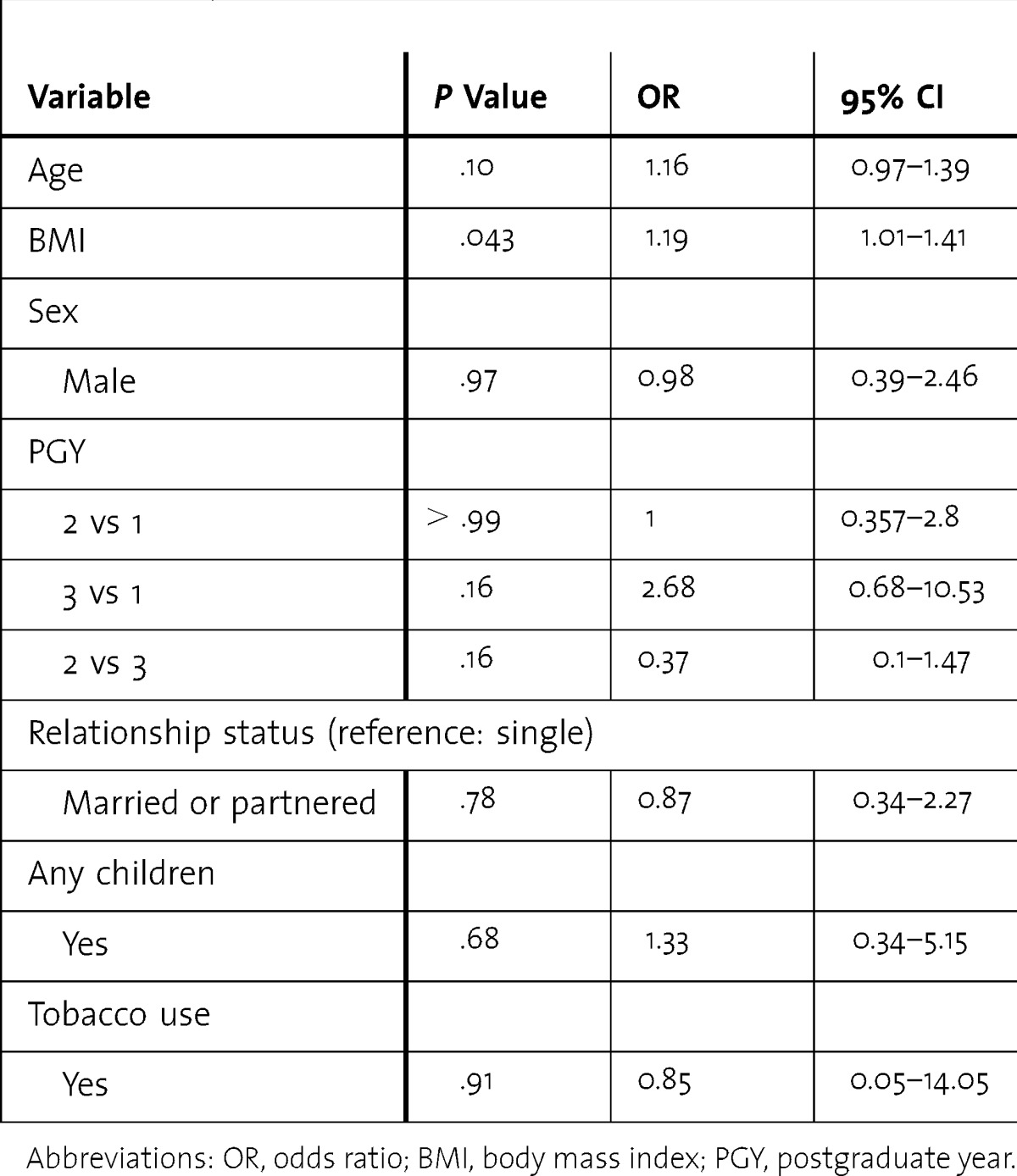
Of the 76 residents who completed the survey, 41 (53.9%) met the criteria for burnout. Increased body mass index was associated with higher odds of burnout (OR = 1.19, 95% CI 1.01–1.41). A statistically significant association was not detected between burnout and age, sex, PGY, relationship status, having children, or tobacco use (table 2).
TABLE 2.
Odds of Burnout and 95% CI by Demographic Categories
Of the 76 respondents, 31 (40.8%) failed to achieve DHHS physical activity guidelines. Residents who were able to meet physical activity guidelines were less likely to be burned out than their fellow residents (OR, 0.38; 95% CI 0.147–0.99; table 3). Sixty respondents (78.9%) reported that their level of physical activity has decreased since beginning medical training, although there was not a significant association with burnout. No association was found between burnout and regular physical activity prior to beginning medical training (table 4).
TABLE 3.
Odds of Burnout and 95% CI by Achievement of DHHS Guidelines
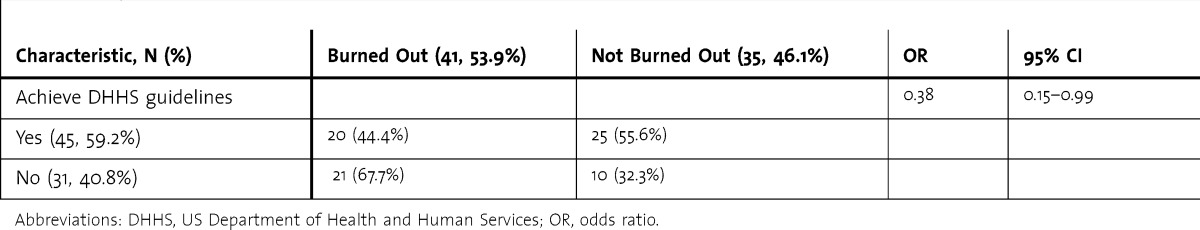
TABLE 4.
Odds of Burnout and 95% CI by Perceived Barriers and Physical Activity Categories

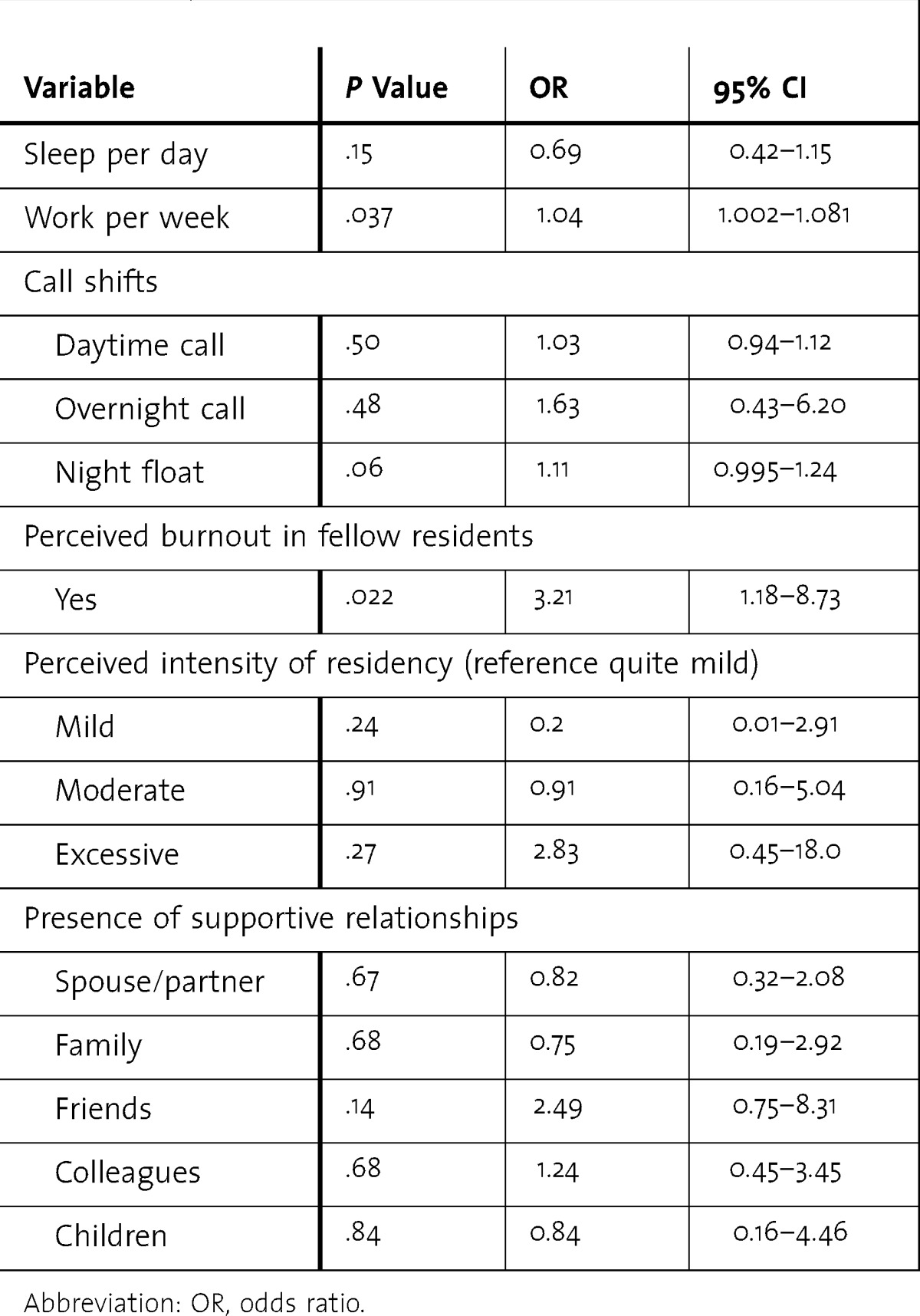
Barriers to regular physical activity were assessed, and “lack of time” (100% of burned-out residents, OR incalculable, Fisher exact test used to estimate P < .005) and “lack of energy” (88% of burned-out residents, OR, 3.29, 95% CI 1.02–10.7) were significantly associated with burnout. Residents were also asked about whether they believed they would be capable of maintaining regular physical activity, if given the chance. Burnout was inversely associated with the belief that they would be capable of maintaining regular activity (OR, 0.24; 95% CI 0.076–0.73; table 4).
Residents who reported that they thought their fellow residents were burned out were more likely to meet criteria for burnout themselves (OR, 3.21, 95% CI 1.18–8.73). Additionally, a higher average number of hours worked per week (OR, 1.04, 95% CI 1.01–1.41) was associated with burnout, though no significant association was found with sleep. No association was found between burnout and the report of presence of various supportive relationships (table 5).
TABLE 5.
Odds of Burnout and 95% CI by Work and Relationship Categories
Discussion
To the authors' knowledge this is the first study specifically assessing the association between physical activity and burnout in resident physicians. Nearly 41% of internal medicine resident physicians failed to meet DHHS guidelines, and 79% reported that their level of physical activity had decreased since beginning their medical training. This is similar to the findings of another cross-sectional web-based study investigating physical activity level in physicians, which found that 27% of residents and 32% of fellows failed to achieve DHHS guidelines.30
Residents who met physical activity guidelines were significantly less likely to be burned out than their fellow residents. Numerous mechanisms have been suggested to explain the beneficial effects of exercise on mental health disorders; a conclusive model remains elusive, though it likely involves a complex interaction of psychological and neurobiological mechanisms.25
Our findings also indicate that perceptions of residency and physical activity may be involved in the relationship between physical activity and burnout. This is suggested by the disproportionate reporting of the barriers “lack of energy” and “lack of time” in burned-out residents, as well as the significant difference in the proportion who indicated that they were capable of maintaining regular physical activity if given the chance, and that were more likely to identify their fellow residents as burned out.
This study has several limitations. As with any self-reported survey, there is a potential for misclassification bias. Our response rate was modest at around 50%. The IPAQ-SF requires participants to recall and properly input a representation of their physical activity in the previous week, rather than relying on more direct measures of activity. Some participants with a sufficient quantity of brisk walking may have been misclassified because we excluded walking as moderate physical activity.
Given the high national prevalence of burnout and inactivity, additional investigation of the relationship between physical activity and burnout appears warranted. This should include clarifying the temporal nature of burnout and physical activity as well as other covariates that appear to be related, assessing if regular physical activity is preventive and/or palliative of burnout, if inability to achieve physical activity guidelines is a result of symptoms of burnout itself or due to something else causing both burnout and diminished physical activity.
Conclusion
We found that nearly 41% of a sample of internal medicine residents from 2 programs failed to achieve DHHS physical activity guidelines and that residents who met these guidelines were less likely to be burned out. Residents also reported that their level of physical activity had decreased since beginning medical training. The potential protective properties of adequate physical activity merit further study.
Footnotes
Shawn M. Olson, MD, MPH, is Assistant Residency Director, HealthPartners/ University of Minnesota Occupational and Environmental Medicine Residency; Nnaemeka U. Odo, MD, MPH, is a Doctoral Candidate, Division of Environmental Health Sciences, University of Minnesota School of Public Health; Alisa M. Duran, MD, FACP, is Program Director, Internal Medicine Residency Program, University of Minnesota; Anne G. Pereira, MD, MPH, FACP, is Assistant Dean for Clinical Education, University of Minnesota Medical School; and Jeffrey H. Mandel, MD, MPH, is Associate Professor, Division of Environmental Health Sciences, University of Minnesota School of Public Health.
Funding: This work was supported, in part, by HealthPartners Institute for Education and Research, as well as the Midwest Center for Occupational Health and Safety Education and Research Center, through funding from the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention, Department of Health and Human Services (T42-OH008434).
Conflict of interest: The authors declare they have no competing interests.
The contents of this effort are solely the responsibility of the authors and do not necessarily represent the official view of the Centers for Disease Control and Prevention, HealthPartners, or other associated entities.
References
- 1.Linzer M, Visser MR, Oort FJ, Smets EM, McMurray JE, de Haes HC, et al. Predicting and preventing physician burnout: results from the United States and the Netherlands. Am J Med. 2001;111(2):170–175. doi: 10.1016/s0002-9343(01)00814-2. [DOI] [PubMed] [Google Scholar]
- 2.Maslach C, Jackson S. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: CPP; 1996. [Google Scholar]
- 3.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 5.Thomas NK. Resident burnout. JAMA. 2004;292(23):2880–2889. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- 6.Ishak WW, Lederer S, Mandili C, Nikravesh R, Seligman L, Vasa M, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236–242. doi: 10.4300/JGME-D-09-00054.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goitein L, Shanafelt TD, Wipf JE, Slatore CG, Back AL. The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Arch Intern Med. 2005;165(22):2601–2606. doi: 10.1001/archinte.165.22.2601. [DOI] [PubMed] [Google Scholar]
- 8.Gopal R, Glasheen JJ, Miyoshi TJ, Prochazka AV. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005;165(22):2595–2600. doi: 10.1001/archinte.165.22.2595. [DOI] [PubMed] [Google Scholar]
- 9.Eckleberry-Hunt J, Lick D, Boura J, Hunt R, Balasubramaniam M, Mulhem E, et al. An exploratory study of resident burnout and wellness. Acad Med. 2009;84(2):269–277. doi: 10.1097/ACM.0b013e3181938a45. [DOI] [PubMed] [Google Scholar]
- 10.McManus IC, Keeling A, Paice E. Stress, burnout and doctors' attitudes to work are determined by personality and learning style: a twelve year longitudinal study of UK medical graduates. BMC Med. 2004;2:29. doi: 10.1186/1741-7015-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prins JT, Gazendam-Donofrio SM, Tubben BJ, van der Heijden FM, van de Wiel HB, Hoekstra-Weebers JE. Burnout in medical residents: a review. Med Educ. 2007;41(8):788–800. doi: 10.1111/j.1365-2923.2007.02797.x. [DOI] [PubMed] [Google Scholar]
- 12.Prins JT, Hoekstra-Weebers JE, Gazendam-Donofrio SM, Van De Wiel HB, Sprangers F, Jaspers FC, et al. The role of social support in burnout among Dutch medical residents. Psychol Health Med. 2007;12(1):1–6. doi: 10.1080/13548500600782214. [DOI] [PubMed] [Google Scholar]
- 13.Ripp J, Fallar R, Babyatsky M, David R, Reich L, Korenstein D. Prevalence of resident burnout at the start of training. Teach Learn Med. 2010;22(3):172–175. doi: 10.1080/10401334.2010.488194. [DOI] [PubMed] [Google Scholar]
- 14.Legassie J, Zibrowski EM, Goldszmidt MA. Measuring resident well-being: impostorism and burnout syndrome in residency. J Gen Intern Med. 2008;23(7):1090–1094. doi: 10.1007/s11606-008-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martini S, Arfken CL, Churchill A, Balon R. Burnout comparison among residents in different medical specialties. Acad Psychiatry. 2004;28(3):240–242. doi: 10.1176/appi.ap.28.3.240. [DOI] [PubMed] [Google Scholar]
- 16.West CP, Shanafelt TD, Kolars JC. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306(9):952–960. doi: 10.1001/jama.2011.1247. [DOI] [PubMed] [Google Scholar]
- 17.Rosen IM, Gimotty PA, Shea JA, Bellini LM. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81(1):82–85. doi: 10.1097/00001888-200601000-00020. [DOI] [PubMed] [Google Scholar]
- 18.West CP, Tan AD, Habermann TM, Sloan JA, Shanafelt TD. Association of resident fatigue and distress with perceived medical errors. JAMA. 2009;302(12):1294–1300. doi: 10.1001/jama.2009.1389. [DOI] [PubMed] [Google Scholar]
- 19.Goldberg R, Boss RW, Chan L, Goldberg J, Mallon WK, Moradzadeh D, et al. Burnout and its correlates in emergency physicians: four years' experience with a wellness booth. Acad Emerg Med. 1996;3(12):1156–1164. doi: 10.1111/j.1553-2712.1996.tb03379.x. [DOI] [PubMed] [Google Scholar]
- 20.Michie S, Williams S. Reducing work related psychological ill health and sickness absence: a systematic literature review. Occup Environ Med. 2003;60(1):3–9. doi: 10.1136/oem.60.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin F, Poyen D, Bouderlique E, Gouvernet J, Rivet B, Disdier P, et al. Depression and burnout in hospital health care professionals. Int J Occup Environ Health. 1997;3(3):204–209. doi: 10.1179/oeh.1997.3.3.204. [DOI] [PubMed] [Google Scholar]
- 22.Dyrbye LN, Thomas MR, Massie FS, Power DV, Eacker A, Harper W, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334–341. doi: 10.7326/0003-4819-149-5-200809020-00008. [DOI] [PubMed] [Google Scholar]
- 23.Prins JT, van der Heijden FM, Hoekstra-Weebers JE, Bakker AB, van de Wiel HB, Jacobs B, et al. Burnout, engagement and resident physicians' self-reported errors. Psychol Health Med. 2009;14(6):654–666. doi: 10.1080/13548500903311554. [DOI] [PubMed] [Google Scholar]
- 24.Paluska SA, Schwenk TL. Physical activity and mental health: current concepts. Sports Med. 2000;29(3):167–180. doi: 10.2165/00007256-200029030-00003. [DOI] [PubMed] [Google Scholar]
- 25.Ströhle A. Physical activity, exercise, depression and anxiety disorders. J Neural Transm. 2009;116(6):777–784. doi: 10.1007/s00702-008-0092-x. [DOI] [PubMed] [Google Scholar]
- 26.Wolff E, Gaudlitz K, von Lindenberger BL, Plag J, Heinz A, Ströhle A. Exercise and physical activity in mental disorders. Eur Arch Psychiatry Clin Neurosci. 2011;261(suppl 2):186–191. doi: 10.1007/s00406-011-0254-y. [DOI] [PubMed] [Google Scholar]
- 27.Vuori I. Does physical activity enhance health. Patient Educ Couns. 1998;33(suppl 1):95–103. doi: 10.1016/s0738-3991(98)00014-7. [DOI] [PubMed] [Google Scholar]
- 28.Frank E, Brogan DJ, Mokdad AH, Simoes EJ, Kahn HS, Greenberg RS. Health-related behaviors of women physicians vs other women in the United States. Arch Intern Med. 1998;158(4):342–348. doi: 10.1001/archinte.158.4.342. [DOI] [PubMed] [Google Scholar]
- 29.Frank E, Biola H, Burnett CA. Mortality rates and causes among U.S. physicians. Am J Prev Med. 2000;19(3):155–159. doi: 10.1016/s0749-3797(00)00201-4. [DOI] [PubMed] [Google Scholar]
- 30.Stanford FC, Durkin MW, Blair SN, Powell CK, Poston MB, Stallworth JR. Determining levels of physical activity in attending physicians, resident and fellow physicians and medical students in the USA. Br J Sports Med. 2012;46(5):360–364. doi: 10.1136/bjsports-2011-090299. [DOI] [PubMed] [Google Scholar]
- 31.Rye PL, Reeson ME, Pekrul CM, Asfour NA, Kundapur R, Wilson MP, et al. Comparing health behaviours of internal medicine residents and medical students: an observational study. Clin Invest Med. 2012;35(1):e40–e44. doi: 10.25011/cim.v35i1.16105. [DOI] [PubMed] [Google Scholar]
- 32.Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 33.Mäder U, Martin BW, Schutz Y, Marti B. Validity of four short physical activity questionnaires in middle-aged persons. Med Sci Sports Exerc. 2006;38(7):1255–1266. doi: 10.1249/01.mss.0000227310.18902.28. [DOI] [PubMed] [Google Scholar]
- 34.Papathanasiou G, Georgoudis G, Papandreou M, Spyropoulos P, Georgakopoulos D, Kalfakakou V, et al. Reliability measures of the short International Physical Activity Questionnaire (IPAQ) in Greek young adults. Hellenic J Cardiol. 2009;50(4):283–294. [PubMed] [Google Scholar]
- 35.Faulkner G, Cohn T, Remington G. Validation of a physical activity assessment tool for individuals with schizophrenia. Schizophr Res. 2006;82(2–3):225–231. doi: 10.1016/j.schres.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 36.Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ) 2005. http://www.ipaq.ki.se/scoring.pdf. Accessed October 10, 2014. [PubMed] [Google Scholar]
- 37.Services UDoHaH. Physical Activity Guidelines for Americans. 2008. http://www.health.gov/paguidelines/pdf/paguide.pdf. Accessed October 10, 2014. [Google Scholar]


