Abstract
Background
Internal medicine residents receive limited training on how to be good stewards of health care dollars while preserving high-quality care.
Intervention
We implemented a clinical process change and an educational intervention focused on the appropriate use of preoperative diagnostic testing by residents at a Veterans Administration (VA) medical center.
Methods
The clinical process change consisted of reducing routine ordering of preoperative tests in the absence of specific indications. Residents received a short didactic session, which included algorithms for determining the appropriate use of perioperative diagnostic testing. One outcome was the average cost savings on preoperative testing for a continuous cohort of patients referred for elective knee or hip surgery. Resident knowledge and confidence prior to and after the intervention was measured by pre- and posttest.
Results
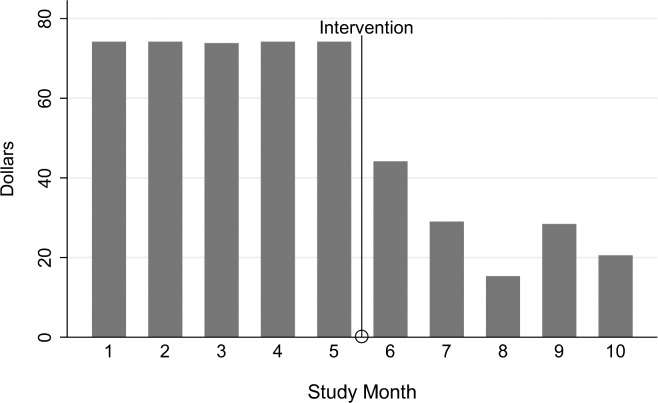
The mean cost of preoperative testing decreased from $74 to $28 per patient after the dual intervention (P < .001). The bulk of cost savings came from elimination of unnecessary blood and urine tests, as well as reduced numbers of electrocardiograms and chest radiographs. Among residents who completed the pretest and posttest, the mean score on the pretest was 54%, compared with 80% on the posttest (P = .027). Following the educational intervention, 70% of residents stated they felt “very comfortable” ordering appropriate preoperative testing (P = .006).
Conclusions
This initiative required few resources, and it simultaneously improved the educational experience for residents and reduced costs. Other institutions may be able to adopt or adapt this intervention to reduce unnecessary diagnostic expenditures.
What was known
Internal medicine residents receive limited training on how to be good stewards of health care dollars while preserving high-quality care.
What is new
A clinical process change and an educational intervention focused on the appropriate use of preoperative diagnostic testing by residents.
Limitations
Single site, single specialty study reduces ability to generalize; survey instrument did not undergo validity testing.
Bottom line
A readily implementable 2-pronged intervention achieved significant cost savings and increased resident test ordering efficacy.
Editor's Note: The online version of this article contains the instruments used in the study and modified National Institute for Health and Care Excellence guidelines on the use of routine preoperative tests for elective surgery.
Introduction
Approximately 30% of health care expenses, more than $700 billion per year, are wasted.1–3 Evidence shows that physicians have the greatest responsibility for ensuring that health care is delivered in a cost-effective manner.4 Educating physicians to be thoughtful about the costs of care is essential to achieving savings. Several medical specialties have incorporated cost-effective care into their reporting of educational Milestones as part of the Accreditation Council for Graduate Medical Education's Next Accreditation System.5,6
Preoperative evaluation is an area of practice where unnecessary expenses have been recognized.7–11 Routine ordering of preoperative tests in the absence of specific indications rarely contributes to patient care and is not cost-effective.7–12 A prior study of patients undergoing elective surgery showed that 60% of routinely ordered tests were unnecessary.12 The American College of Radiology Appropriateness Criteria for preoperative chest radiography guidelines note that only 2% of these radiographs lead to a change in management.13 In fact, many specialty societies now discourage routine preoperative testing.9,14,15
Educational research in this area is limited and, to our knowledge, no published study has aimed at reducing the cost of preoperative testing. Our goal was to alter customary preoperative ordering habits through a 2-pronged intervention that combined a simple clinical process change with a curriculum focusing on the ordering practices of residents. We hypothesized this dual intervention would help residents understand high-value care and encourage them to practice high-value care, resulting in cost savings.
Methods
Setting
The preoperative clinic at the Veterans Administration Medical Center (VAMC) in Omaha, Nebraska, provides educational opportunities to internal medicine residents from the University of Nebraska Medical Center (UNMC) and Creighton University Medical Center (CUMC). Residents from each institution rotate through the clinic monthly. Residents are paired with an attending physician from their respective institution. Patients referred to the clinic are scheduled for an elective surgery and have a least 1 medical comorbid condition.
Before our study, residents rotating through the clinic received didactic education focused solely on assessing cardiac risk. All testing was ordered by surgical nurse coordinators and performed before the clinic appointment. Testing was ordered reflexively without regard to medical history, and residents were not involved in test ordering. Results of the testing were available for review by the residents and attending at the time of the preoperative clinic appointment. Residents were responsible for interpretation of preoperative tests but were not educated on the appropriateness of testing.
Process Change
We sought the input of all medical and surgical stakeholders regarding our clinical process and education intervention. Internal medicine faculty from both institutions helped guide the development of the intervention. Letters of support were obtained from the departments of anesthesiology and orthopedics. Preoperative clinic nurses were notified of the process change during a face-to-face meeting and agreed to assist with implementation. There was no resistance to the adoption of the process change. This was likely due to relationships developed in a joint anesthesiology–internal medicine preoperative clinic and an orthopedic comanagement program at 1 of the institutions.
In June 2012, authority for ordering preoperative tests on patients scheduled for knee or hip arthroplasty transitioned from the orthopedic nurse coordinators to the residents rotating through the preoperative clinic. Under the new process, laboratory and radiographic testing was ordered by residents at the time of the visit and was reviewed by the resident and attending. Patients were notified of abnormal testing via phone or mail. An addendum was placed in the electronic health record outlining any additional or changed recommendations and routed to the orthopedic nurse coordinator and attending surgeon. Electrocardiograms (ECGs) ordered by the resident were immediately available for review.
Educational Intervention
Coinciding with the process change, residents assigned to the preoperative clinic began receiving the intervention curriculum in June 2012. The curriculum consisted of a pretest followed by a 45-minute didactic session at the beginning of the rotation and a posttest at the conclusion of the rotation. The pretest and posttest were identical evaluations of residents' knowledge and attitudes concerning preoperative medicine. The instruments were developed by the authors, who are clinician educators, without further testing, and are available as online supplemental material. The didactic session was revised to cover both risk stratification and a new section on cost-conscious preoperative testing (available from authors). Content was adapted from valid, widely accepted guidelines published by the National Institute for Health and Care Excellence (available as online supplemental material).16 The guidelines were posted in physician workrooms for reference by residents and attending physicians. Residents were advised that the guidelines would not apply in every situation and were encouraged to use clinical judgment when deciding to pursue further preoperative evaluation.
Analysis
To test our hypothesis, a prospective preintervention and postintervention cohort study was developed. The primary outcome was the average cost savings on preoperative testing for a continuous cohort of patients referred to the preoperative clinic for elective knee or hip arthroplasty. The average cost of preoperative testing was calculated from the 2012 Medicare reimbursement schedule for Nebraska. Student t test was used to compare the mean cost of preoperative testing before and after the intervention. Statistical calculation based on a review of 20 charts established that we could detect a 5% decrease in the cost of preoperative testing with an α of 0.05 and a β of 0.9 in a 2-sided t test with just 4 subjects. A sample size of 4 was considered too small to allow meaningful inferences, and we arbitrarily selected a sample size of 100 subjects, 50 in the preintervention group and 50 in the postintervention group. To measure the effect of our educational intervention, the pretest to posttest change was compared using the χ2 test. Data on surgery cancellations, hospital length of stay, and inpatient mortality for the study patients were also collected.
This study was approved by the Institutional Review Board at the Omaha VAMC. All analyses were performed using Stata software version 10.1 (StataCorp LP).
Results
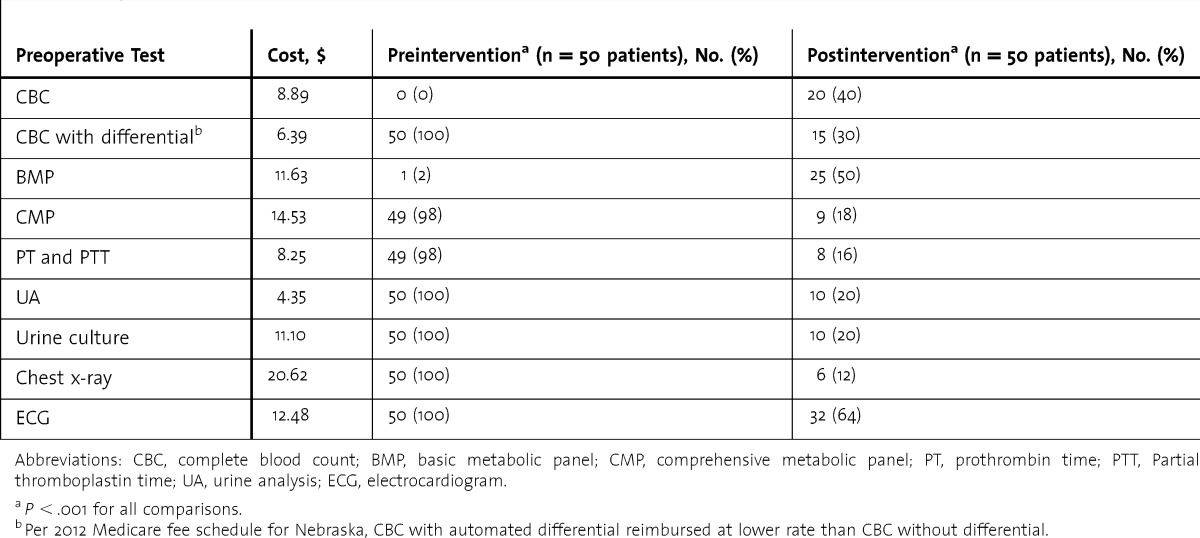
Preintervention and postintervention patients were similar in baseline demographics, indication for surgery, and medical comorbidities (table 1). A comparison of the Revised Cardiac Risk Index17 scores between the preintervention and postintervention groups revealed no significant difference. The mean cost of preoperative testing decreased from $74 to $28 per patient after initiation of the intervention (P < .001; figure). The total cost of preoperative testing for 50 patients for 6 months was reduced by $2,288. The bulk of the cost savings came from the elimination of unnecessary blood and urine tests (table 2). Another source of savings was the substitution of more precise and less expensive blood tests (eg, basic metabolic profile) in place of unnecessarily comprehensive tests (eg, comprehensive metabolic profile). Limiting ECGs to patients with symptoms or history of cardiac disease decreased costs substantially ($624 versus $399). Before the intervention, all patients within the cohort (n = 50, 100%) received urinalysis, chest radiograph, and ECG testing. After the intervention, only 4 of 50 (8%) patients received all 3 tests, and all instances occurred within the first month of the intervention.
TABLE 1.
Patient Characteristics
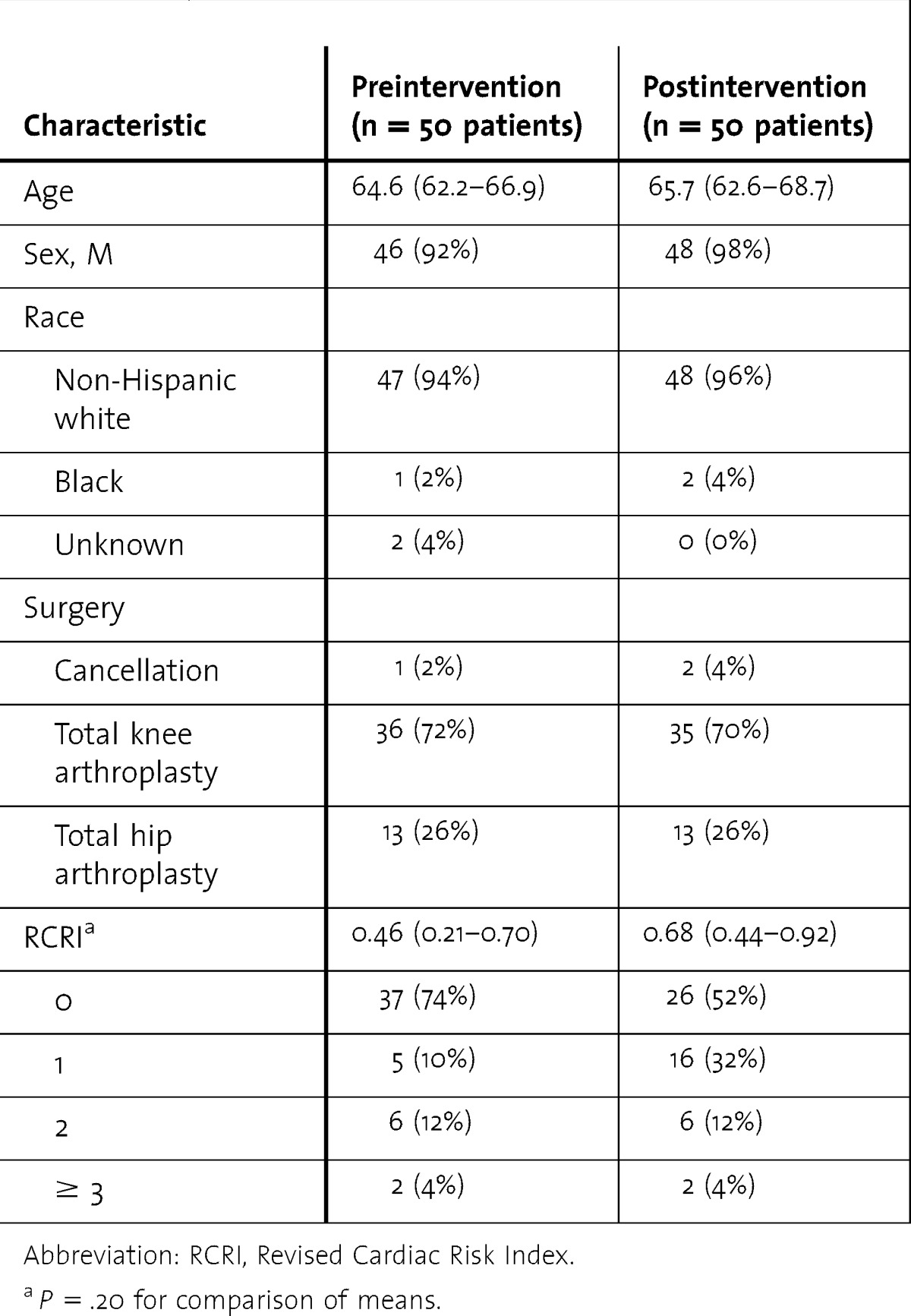
FIGURE.
Cost of Preoperative Testing Over Time
Note: Average cost per patient of all preoperative testing before and after the institution of a dual intervention. Costs are based on the 2012 Medicare Reimbursement Schedule for Nebraska.
TABLE 2.
Use of Preoperative Tests
Twenty-nine residents (20 from CUMC [69%] and 9 from UNMC [31%]) rotated through the preoperative clinic during the 5 months following initiation of the intervention. Twelve of 29 residents (41%) were in their first year of postgraduate training, 14 of 29 (48%) in their second year, and 3 of 29 (10%) in their third year. Two of the 29 residents (7%) repeated the rotation during the intervention period, and their second round of pretest and posttest scores were excluded from data analysis. Thirteen residents attended the didactic session and took the pretest, and 11 took the posttest, with 10 of 29 (35%) residents receiving the complete educational intervention including the pretest, didactic session, and posttest.
Among residents who completed both the pretest and posttest (n = 10), the mean score on the pretest was 54%, compared with 80% on the posttest (P = .027). Residents' confidence in providing cost-conscious, high-value preoperative care improved, as demonstrated by 1 of 10 residents (10%) stating they felt “very comfortable” ordering appropriate preoperative laboratory tests before the rotation, compared with 7 of 10 residents (70%) after the rotation (P = .006).
Although the study was not powered for these outcomes, the intervention did not appear to affect surgery cancellations (2% before versus 4% after intervention, P = .56), mean hospital length of stay (3.18 days before versus 3.88 days after intervention, P = .13), or inpatient mortality (2% before versus 0% after intervention, P = .32).
Time and resource use for the interventions were minimal. Development of education materials and discussions with stakeholders required a 1-time investment of approximately 15 hours. A chief resident delivered the didactic session each month and administered the pretests and posttests. Time dedicated to didactics remained the same as before the intervention. Printing costs for signage were negligible. There were no costs associated with maintaining the intervention over time.
Discussion
We demonstrated that 2 simple, parallel interventions in a resident preoperative clinic reduced costs and improved the educational experience for residents. Focused and selective preoperative testing became the norm within the clinic, despite the limited reach of the didactic sessions, particularly as the study progressed. The combination of a clinical process change and an educational intervention resulted in a cultural shift within the preoperative clinic toward cost-conscious, evidence-based care.
Several studies have demonstrated that residents can be taught to practice high-value, cost-conscious care. One study18 used chart-stimulated recall to retrospectively expose residents to the costs associated with their own ordering habits. Retrospective review of cost information, however, may not be effective at achieving real cost savings.19 In addition, that methodology does not guide residents toward the practice of evidence-based medicine.
Another study20 found that a facile cost-consciousness curriculum could alter resident behavior to reduce unnecessary inpatient imaging. Similar to ours, that educational intervention was based on published guidelines, took the form of didactic lectures targeted at residents, and incorporated reminders. In contrast to our study, their educational intervention was not accompanied by a process or systems change.
One study21 employed a dual intervention similar to ours and demonstrated a reduction in the unnecessary use of nebulized medications at a large teaching hospital. Significant cost savings were achieved by combining lectures, posted reminders, and a process change that removed nebulized medication from the computerized admission order set. Similar to our study, the process change and educational intervention occurred in parallel. As residency programs look to comply with new accreditation standards, interventions like these can provide a roadmap for the development of cost-conscious, high-value care curricula.
Although a strength, the use of a combined intervention in this study prohibits separate analysis of each of the components of the intervention. A limitation of our study is the inclusion of only patients undergoing elective hip and knee arthroplasty, and our results may not be applicable to other surgeries. Further, the predominantly non-Hispanic white and male patient population at this VAMC is not representative of the general population. The comorbid conditions of our study patients do, however, generally reflect those seen in the larger population. Additional limitations include our inability to reach all residents with the educational intervention and the lack of validity evidence for our pretest and posttest. Finally, our study design cannot rule out the possibility that the observed reduction in costs could be the result of a general increase in cost-consciousness among residents over time.
Conclusion
The US health care system needs physicians to provide high-value, cost-effective care and physicians-in-training must be taught accordingly. The combination of a clinical process change and an educational intervention to increase the awareness of cost-effective care in internal medicine residents at 2 institutions achieved significant cost savings and increased resident test ordering efficacy. Similar steps could be implemented by residency programs in all disciplines with the goal of improving the cost-effectiveness of medical care.
Footnotes
Sarah E. Richards, MD, is Assistant Professor of Medicine, University of Nebraska Medical Center; Jason F. Shiffermiller, MD, MPH, is Assistant Professor of Medicine, University of Nebraska Medical Center; Adam D.Wells, MD, is a Fellow in Pulmonary and Critical Care, University of Nebraska Medical Center; Sara M. May, MD, is a Fellow in Allergy and Immunology, Mayo Clinic; Subhankar Chakraborty, MD, is a Fellow in Gastroenterology, Mayo Clinic; Kelly J. Caverzagie, MD, is Associate Professor of Medicine and Associate Dean for Educational Strategy, University of Nebraska Medical Center; and Micah W. Beachy, DO, is Assistant Professor of Medicine, University of Nebraska Medical Center.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
References
- 1.Owens DK, Qaseem A, Chou R, Shekelle P Clinical Guidelines Committee of the American College of Physicians. High-value, cost-conscious health care: concepts for clinicians to evaluate the benefits, harms, and costs of medical interventions. Ann Intern Med. 2011;154(3):174–180. doi: 10.7326/0003-4819-154-3-201102010-00007. [DOI] [PubMed] [Google Scholar]
- 2.Smith CD Alliance for Academic Internal Medicine–American College of Physicians High Value; Cost-Conscious Care Curriculum Development Committee. Teaching high-value, cost-conscious care to residents: the Alliance for Academic Internal Medicine-American College of Physicians Curriculum. Ann Intern Med. 2012;157(4):284–286. doi: 10.7326/0003-4819-157-4-201208210-00496. [DOI] [PubMed] [Google Scholar]
- 3.Yong PL, Olsen L. Roundtable on Evidence-Based Medicine, Institute of Medicine—The Healthcare Imperative: Lowering Costs and Improving Outcomes. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- 4.Sager A, Socolar D. Health Costs Absorb One-Quarter of Economic Growth, 2000–2005. Boston, MA: Boston University School of Public Health; 2005. Data Brief No. 8 of the Health Reform Program. [Google Scholar]
- 5.Accreditation Council for Graduate Medical Education. Medical specialties. http://www.acgme.org/acgmeweb/tabid/368/ProgramandInstitutionalAccreditation/MedicalSpecialties.aspx. Accessed September 3, 2014. [Google Scholar]
- 6.Iobst W, Aagaard E, Bazari H, Brigham T, Bush RW, Caverzagie K, et al. Internal medicine milestones. J Grad Med Educ. 2013;5(1 suppl 1):14–23. doi: 10.4300/JGME-05-01s1-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lawrence VA, Kroenke K. The unproven utility of preoperative urinalysis: clinical use. Arch Intern Med. 1988;148(6):1370–1373. [PubMed] [Google Scholar]
- 8.Committee on Standards and Practice Parameters; Apfelbaum JL, Connis RT, Nickinovich DG American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Pasternak LR, et al. Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2012;116(3):522–538. doi: 10.1097/ALN.0b013e31823c1067. [DOI] [PubMed] [Google Scholar]
- 9.ABIM Foundation. Choosing wisely website. http://www.choosingwisely.org. Accessed March 12, 2014. [Google Scholar]
- 10.Johnson RK, Mortimer AJ. Routine pre-operative blood testing: is it necessary. Anaesthesia. 2002;57(9):914–917. doi: 10.1046/j.1365-2044.2002.02750.x. [DOI] [PubMed] [Google Scholar]
- 11.Qaseem A, Alguire P, Dallas P, Feinberg LE, Fitzgerald FT, Horwitch C, et al. Appropriate use of screening and diagnostic tests to foster high-value, cost-conscious care. Ann Intern Med. 2012;156(2):147–149. doi: 10.7326/0003-4819-156-2-201201170-00011. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan EB, Sheiner LB, Boeckmann AJ, Roizen MF, Beal SL, Cohen SN, et al. The usefulness of preoperative laboratory screening. JAMA. 1985;253(24):3576–3581. [PubMed] [Google Scholar]
- 13.American College of Radiology. ACR appropriateness criteria. http://www.acr.org/~/media/ACR/Documents/AppCriteria/Diagnostic/RoutineAdmissionAndPreoperativeChestRadiography.pdf. Accessed March 12, 2014. [Google Scholar]
- 14.Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof E, Fleischmann KE, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): developed in collaboration with the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation. 2007;116(17):e418–e499. doi: 10.1161/CIRCULATIONAHA.107.185699. [DOI] [PubMed] [Google Scholar]
- 15.Committee on Standards and Practice Parameters; Apfelbaum JL, Connis RT, Nickinovich DG American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Pasternak LR, et al. Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2012;116(3):522–538. doi: 10.1097/ALN.0b013e31823c1067. [DOI] [PubMed] [Google Scholar]
- 16.National Institute for Health and Care Excellence. NICE website. http://www.nice.org.uk. Accessed March 12, 2014. [Google Scholar]
- 17.Lee TH, Marcantonio ER, Mangione CM, Thomas EJ, Polanczyk CA, Cook EF, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100(10):1043–1049. doi: 10.1161/01.cir.100.10.1043. [DOI] [PubMed] [Google Scholar]
- 18.Post J, Reed D, Halvorsen AJ, Huddleston J, McDonald F. Teaching high-value, cost-conscious care: improving residents' knowledge and attitudes. Am J Med. 2013;126(9):838–842. doi: 10.1016/j.amjmed.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 19.Sommers BD, Desai N, Fiskio J, Licurse A, Thorndike M, Katz JT, et al. An educational intervention to improve cost-effective care among medicine housestaff: a randomized controlled trial. Acad Med. 2012;87(6):719–728. doi: 10.1097/ACM.0b013e31825373b3. [DOI] [PubMed] [Google Scholar]
- 20.Covington MF, Agan DL, Liu Y, Johnson JO, Shaw DJ. Teaching cost-conscious medicine: impact of a simple educational intervention on appropriate abdominal imaging at a community-based teaching hospital. J Grad Med Educ. 2013;5(2):284–288. doi: 10.4300/JGME-D-12-00117.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moriates C, Mourad M, Novelero M, Wachter RM. Development of a hospital-based program focused on improving healthcare value. J Hosp Med. 2014;9(10):671–677. doi: 10.1002/jhm.2235. [DOI] [PubMed] [Google Scholar]