Abstract
Background
Traditional “batched” bedside clinical care rounds, where rounds for all patients precede clinical tasks, may delay clinical care and reduce resident work efficiency.
Innovation
Using Lean concepts, we developed a novel “Rounding-in-Flow” approach, with the patient care team completing all tasks for a single patient before initiating any tasks for the next patient. Outcome measures included timely patient discharge and intern work hours.
Methods
We performed a retrospective cohort study with historic and contemporaneous control groups, with time series adjustment for underlying temporal trends at a single medical center. Primary outcomes were timely patient discharge orders and resident duty hours. Participants were 17 376 consecutive hospital inpatients between January 1, 2011, and June 30, 2012, and medical ward rounding teams of interns, residents, and attending hospitalists.
Results
Timely discharge orders, defined as written by 9:00 am, improved from 8.6% to 26.6% (OR, 1.55; 95% CI 1.17–2.06; P = .003). Time of actual patient discharge was unchanged. Resident duty hour violations, defined as less than 10 hours between clinical duties, decreased from 2.96 to 0.98 per intern per rotation (difference, 1.98; 95% CI 1.09–2.87; P < .001). Average daily intern work hours decreased from 12.3 to 11.9 hours (difference, 0.4 hours; 95% CI 0.16–0.69; P = .002).
Conclusions
Compared with batched rounding, Lean Rounding-in-Flow using “1-piece flow” principles was associated with more discharge orders written before 9:00 am and fewer violations in the 10-hour break rule, with minimal changes to intern total work hours and actual patient discharge time.
What was known
Traditional inpatient rounding has inherent inefficiencies that may affect patient care and resident duty hours.
What is new
Application of Toyota Lean 1-piece flow principles to bedside rounding in an internal medicine inpatient unit.
Limitations
Single specialty, single institution study limits generalizability.
Bottom line
Lean “Rounding-in-Flow” was associated with earlier writing of discharge orders and improved compliance with the requirement for a 10-hour rest period.
Introduction
Resident patient rounds form the cornerstone of resident education and patient care for hospitalized patients. However, there is pressure to improve the efficiency of rounds, both to facilitate early patient discharge and to limit resident duty hours. In addition, recent evidence suggests that clinical care is changing, with resident and attending physicians increasingly making clinical decisions away from the patient bedside.1
To improve intern inpatient rounds on our hospitalist service, we applied Lean principles,2–4 adapted from the Toyota Production System.5,6 A major principal of Lean is the concept of 1-piece flow,5,6 whereby all work for a single production unit is completed before initiation of work on the next unit. One-piece flow contrasts with batching, whereby a single portion of the work for all units is completed before moving to a different task. The advantages of 1-piece flow include less waiting, information reacquisition, information decay, and travel, with overall improvement in production timeliness.2,4–6
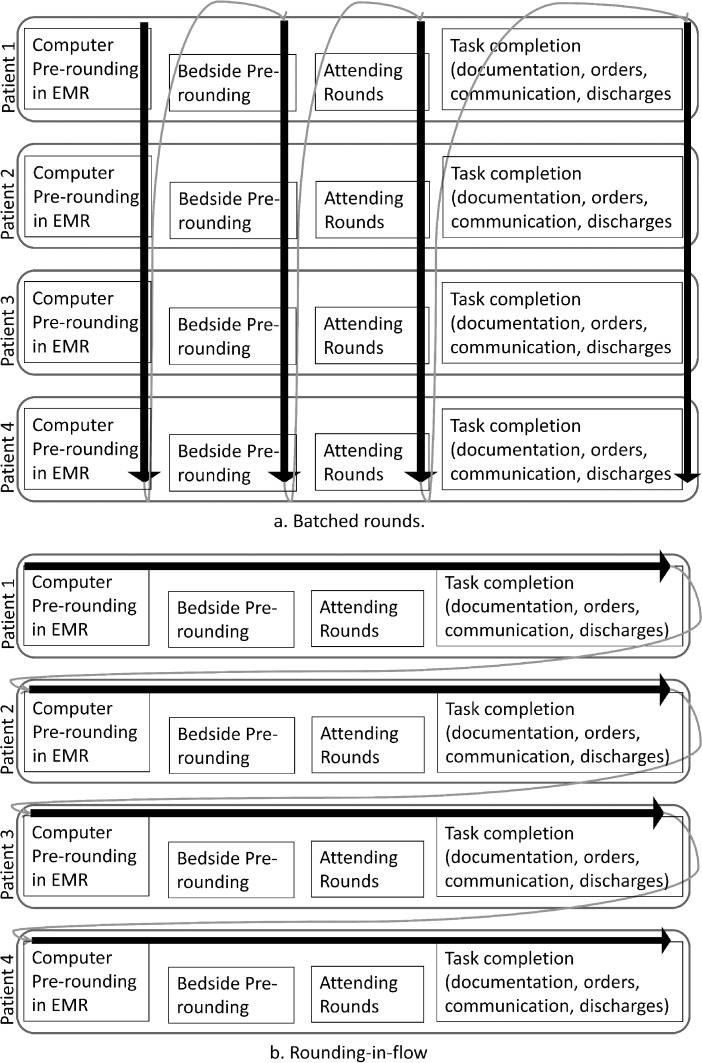
Although institutions differ, the standard process historically for inpatient intern rounds was a batched process.7 The first batch was intern electronic health record prerounds consisting of laboratory data review. The second batch was clinical prerounds, with intern-patient interviews and physical examinations. The third batch was attending rounds, with intern bedside presentations and team formulation of the clinical plan. Finally, the fourth batch, after attending rounds, was intern documentation, order entry, consult requests, and discharge preparation (figure 1a). This historic batch processing potentially disrupted workflow, increasing workload.8 We applied Lean 1-piece flow to inpatient rounds, an approach that, to our knowledge, has not been reported previously in the medical literature. This new “Rounding-in-Flow” involved completing all tasks for a single patient before initiating care for the next patient (figure 1b), with the potential to improve quality and efficiency. We measured the effectiveness of this effort on patient care through timely order writing and timely discharge, and on the interns, through duty hour violations.
FIGURE 1.
Batched Rounds Versus Rounding-in-Flow; (a) Under Traditional Rounding, a Single Task Is Completed For All Patients Before Initiating The Next Task; (b) In Contrast, Under Rounding in Flow, All Tasks Are Completed for a Patient Before Initiating Any Tasks for the Next Patient
Methods
The setting was a 336-bed hospital in Seattle, Washington, with 17 000 annual inpatient admissions. The internal medicine residency program included categorical, 3-year internal medicine residents (10 per year) and preliminary interns (17 per year). The resident calendar consisted of 13 four-week rotations, each with 8 interns on inpatient service. Ward teams were composed of 1 senior resident, 2 interns, and 1 hospitalist attending.
Planning the Intervention
To improve the quality and efficiency of our intern rounding, we undertook a 5-day Rapid Process Improvement Workshop (RPIW) in October 2011.9 The RPIW team included interns, residents, hospitalist attendings, nurses, administration staff, and social workers. Areas of waste identified from batching included, for the interns: (1) reacquisition of patient information multiple times: on computer prerounds, before attending rounds, at attending rounds, and before writing orders; (2) decreased recall of physical examination and care plan details over time; and (3) the need to travel to see patients multiple times.
The Rounding-in-Flow Intervention
To reduce those inefficiencies, the RPIW team developed Rounding-in-Flow. Instead of batching tasks, the intern performed prerounds and immediately saw the first patient. Next was intern bedside presentation to the senior resident and attending and bedside teaching. After bedside care planning, the intern completed the documentation and order writing “in-flow.” The senior resident and attending would also complete all of their documentation and billing tasks, thus completing the entire rounding process for that patient before starting with the next patient. While the hospitalist attending and resident were staffing with 1 intern, the other intern was prerounding and seeing their first patient, enabling the attending and resident to “toggle” between 2 interns. Intrinsic to the system was that the team senior resident determined the rounding order through a computer prescreen to identify potentially unstable patients.
Intervention Evaluation
We performed a retrospective before and after cohort study with interrupted time series and difference in difference analysis, taking advantage of a natural experiment in having patients in the same hospital cared for by 3 different attending groups: (1) intervention hospitalists, (2) control hospitalists who are not part of the residency program, and (3) surgical nonhospitalists. Although not identical to the intervention group at baseline, we used the control groups to adjust for underlying trends in outcome variables not attributable to our intervention, thereby strengthening the evidence of causation. Use of control hospitalists allowed adjustment for coincident changes in patient care, and use of surgical attendings allowed adjustment for concurrent changes in graduate medical education.
Outcomes identified related to patient care: timeliness of discharge order writing (before 9:00 am), timeliness of discharge (by noon), and intern work (average duty hours and violations). Those outcomes were institutional priorities selected a priori to motivate the quality improvement intervention. The study sample was 22 604 consecutive patients admitted and discharged by intervention or control physicians between January 1, 2011, and July 31, 2012. Excluded were patients who expired (842, 3.7%), were discharged to a setting other than home or hospice (4105, 18.2%), were under age 18 (19, 0.1%), or had 24 hours or more between discharge order writing and actual discharge (262, 1.2%), leaving 17 376 for analysis.
Duty hour violations (any break < 10 hours) were determined from the required intern weekly self-report into a web-based duty hour system. To avoid confounding by resident experience, we compared the 6 rotations preintervention (June 2011–October 2011) to the same 6 rotations after the intervention (June 2012–October 2012).
An Institutional Review Board waiver was granted for this quality improvement project.
Analysis
Initial analysis was before and after the intervention date of November 1, 2011, using a χ2 test. To adjust for underlying temporal changes, we used an interrupted time series with segmented logistic regression. We also used the difference in difference approach to adjust for institutional trends identified in the control groups. Finally, to assess implementation, we compared before and after at the physician level. Duty hour violations were compared with a t test. Statistical analyses were performed using Stata version 12 software (StataCorp LP).
Results
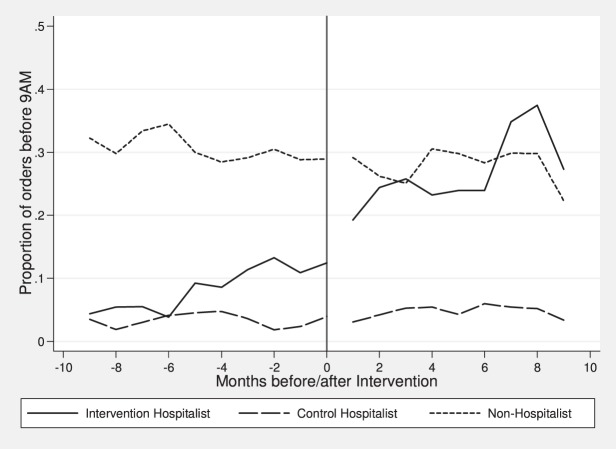
Details of the intervention and control cohorts are provided in table 1. In the intervention cohort, there was substantial improvement in discharge orders by 9:00 am (8.6% to 26.6%; difference, 18.0 percentage points; 95% CI 16.1–19.9; P < .001), with the mean time improving from 12:26 pm to 11:27 am (improvement, 59 minutes, P < .001) and in discharge by noon (16.1% to 23.0%; difference, 6.9 percentage points; 95% CI 4.8–8.9; P < .001), with the mean time improving from 2:40 pm to 2:15 pm (improvement, 25 minutes; P < .001; table 2; figure 2). Because we identified significant improvement in the intervention group that was temporally independent of the intervention, we adjusted the analyses using segmented regression, for an adjusted odds ratio (OR) for timely discharge orders of 1.55 (95% CI 1.17–2.06, P = .003). However, after adjustment, differences in timely patient discharge were not statistically significant (OR, 1.03; 95% CI 0.80–1.33; P = .82).
TABLE 1.
Study Sample and Patient Demographics (January 1, 2011, to June 30, 2012)
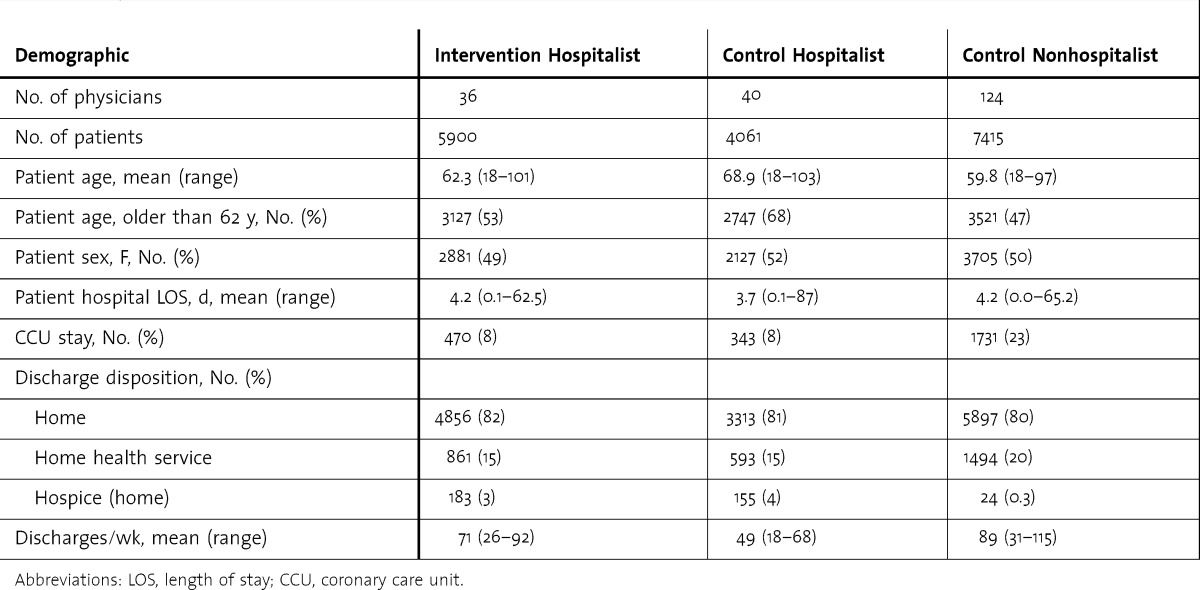
TABLE 2.
Discharge Orders Before 9:00 am and Patient Discharge Before Noon for Intervention and Control Cohortsa
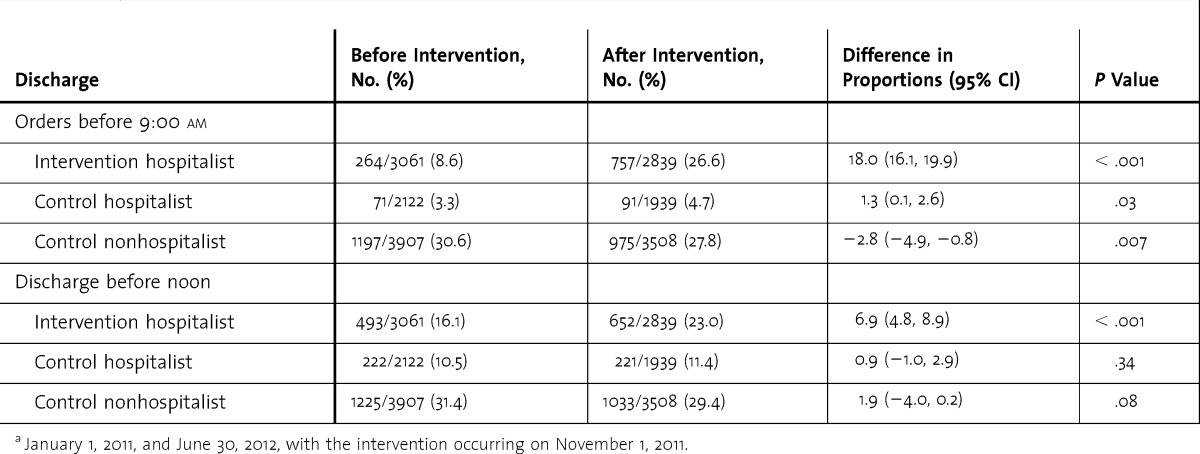
FIGURE 2.
Proportion of Discharge Orders Before 9:00 am, Before and After Rounding-in-Flow Intervention (Middle Line)
For timely discharge orders in the controls, a small improvement in the hospitalist controls (3.3% to 4.7%; difference, 1.3 percentage points; 95% CI 0.1–2.6; P = .028) contrasted with a small decrease in the nonhospitalist controls (30.6% to 27.8%; difference, –2.8 percentage points; 95% CI –0.8 to –4.9; P = .007; table 2). No significant changes were seen in either control group in timely patient discharge. Because there was no consistent background trend for the control group, we did not use the difference in difference model in the final regression.
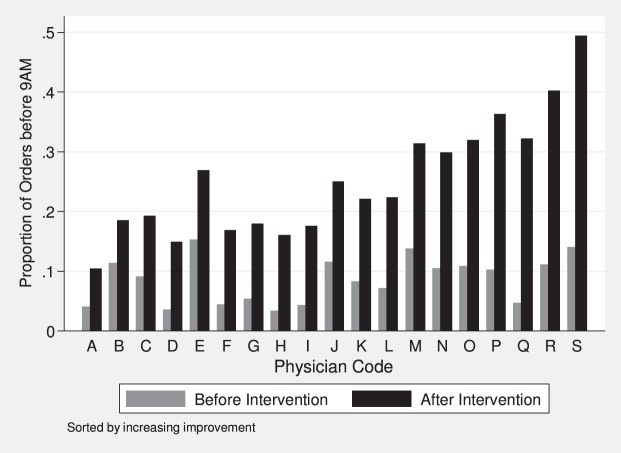
Implementation was broadly successful, with statistically significant improvement in 18 of 19 (95%) intervention hospitalists (figure 3).
FIGURE 3.
Timely Discharge Orders by Attending Hospitalists in Intervention Groupa
a More than 25 discharges before the intervention and 25 discharges after the intervention (total N = 5210 discharges for 19 hospitalists, mean = 274, range = 139–453). All differences were significant (P < .05), except physician B (P = .13).
There were 46 intern rotations preintervention and 47 intern rotations postintervention. Following the Rounding-in-Flow intervention, the average number of 10-hour duty hours violations per intern per rotation decreased from 2.96 to 0.98 (difference, 1.98; 95% CI 1.09–2.87; P < .001). The average number of hours worked per day by interns decreased from 12.3 to 11.9 (difference, 0.4 hours; 95% CI 0.16–0.69; P = .002).
Discussion
After applying Lean concepts to inpatient rounding on an internal medicine service, we found improvements in timely patient discharge order writing and intern duty hour violations in association with Rounding-in-Flow when compared with batched rounding. We found no difference in adjusted patient discharge time, possibly because actual discharge is dependent on patient factors beyond our control. Rounding-in-Flow was feasible in our setting, with no increase in resources and appeared to be acceptable to interns.
Other rounding innovations in the literature include rounding with handheld computers to facilitate real-time order writing and evidence review10; geographically consolidating patients; multidisciplinary rounds including nurses, pharmacists, and other providers11; and family-centered rounds, directly involving family members with ward rounding teams.12 Our Rounding-in-Flow intervention is not necessarily exclusive of those other approaches, and mobile computers were available to our Rounding-in-Flow interns about half of the time. The relationship between different innovations in rounding would require further research.
Other potential effects of the intervention that we could not measure directly would benefit from further study. First, intern education was potentially affected. Interns lose the ability to learn from each other's patients but may gain more time to learn from their own patients and to learn about more efficient patient care. Anecdotally, our interns reported high satisfaction with the new system and more time to spend in direct patient care activities. In addition, Rounding-in-Flow permits attendings to review intern patient care in real time, providing a more immediate safety check. Rounding-in-Flow also potentially decreased the accumulation of incomplete tasks, decreasing the work intensity experienced by interns.13 In addition, medical students are not routinely part of our medical ward teams, and the effect of Rounding-in-Flow on them would require further study. We expect no effect on nursing time, although we were not able to measure that. Finally, we were unable to directly assess patient satisfaction.
Our implementation was heavily dependent on our institutional adoption of Lean,3,4 because working in flow, Lean tools, and workflow redesign3,14,15 were already familiar to faculty. In our model, rounding subsumes all inpatient clinical work, and rounding itself may take longer. Overall, however, clinical care was completed earlier. Hence, our model may not work where attendings have responsibilities beyond inpatient care.
Our intervention has limitations. As a quality improvement project, it was, by necessity, a single institution, retrospective, before and after cohort study. To avoid bias, we adjusted for underlying trends driving change independent of the intervention with an interrupted time series and 2 distinct control groups, and we also seasonally matched resident months to avoid potential bias in the duty hours from interns gaining experience as the year progresses. Duty hours for participants were self-reported with the potential for recall bias. We also excluded the approximately 20% of patients who were not discharged to home, and logistical issues may have affected the ability to discharge those patients.
Conclusion
Rounding-in-Flow proved to be feasible and acceptable in our program, with prior faculty education and support. Through this intervention, we improved the timeliness of patient discharge while decreasing violations in the intern 10-hour free rule. Dissemination of this model will require evaluation of the effect of Rounding-in-Flow on education and quality of patient care.
Footnotes
All authors are at Virginia Mason Medical Center. Alvin S. Calderon, MD, PhD, FACP, is Program Director, Internal Medicine Residency Program; C. Craig Blackmore, MD, MPH, is Director, Center for Health Services Research; Barbara L. Williams, PhD, is Research Scientist, Center for Health Services Research; Kavita P. Chawla, MD, MHA, is Internal Medicine Resident; Dana L. Nelson-Peterson, DNP, MN, RN, is Administrative Director, Ambulatory Care Nursing; Michael D. Ingraham, MD, is Section Head, Hospital Medicine; Donna L. Smith, MD, is Hospital Medical Director; and Gary S. Kaplan, MD, is Chairman and CEO.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
References
- 1.Gonzalo JD, Chuang CH, Huang G, Smith C. The return of bedside rounds: an educational intervention. J Gen Intern Med. 2010;25(8):792–798. doi: 10.1007/s11606-010-1344-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bush RW. Reducing waste in US health care systems. JAMA. 2007;297(8):871–874. doi: 10.1001/jama.297.8.871. [DOI] [PubMed] [Google Scholar]
- 3.Kenney C. Transforming Health Care: Virginia Mason Medical Center's Pursuit of the Perfect Patient Experience. New York, NY: Productivity Press–Taylor & Francis Group; 2011. [Google Scholar]
- 4.Kaplan GS. Waste not: the management imperative for healthcare. J Healthc Manag. 2012;57(3):160–166. [PubMed] [Google Scholar]
- 5.Ohno T. Toyota Production System: Beyond Large-Scale Production. New York, NY: Productivity Press; 1998. [Google Scholar]
- 6.Womack JP, Jones DT. Lean Thinking: Banish Waste and Create Wealth in Your Corporation. Vol. 2003. New York, NY: New York Free Press; p. 396. [Google Scholar]
- 7.Payson HE, Barchas JD. A time study of medical teaching rounds. N Engl J Med. 1965;273(27):1468–1471. doi: 10.1056/NEJM196512302732706. [DOI] [PubMed] [Google Scholar]
- 8.Weigl M, Mueller A, Vincent C, Angerer P, Sevdalis N. The association of workflow interruptions and hospital doctors' workload: a prospective observational study. BMJ Qual Saf. 2012;21(5):399–407. doi: 10.1136/bmjqs-2011-000188. [DOI] [PubMed] [Google Scholar]
- 9.Nelson-Peterson DL, Leppa CJ. Creating an environment of caring using Lean principles of the Virginia Mason Production System. J Nurs Adm. 2007;37(6):287–294. doi: 10.1097/01.NNA.0000277717.34134.a9. [DOI] [PubMed] [Google Scholar]
- 10.Phua J, See KC, Khalizah HJ, Low SP, Lim TK. Utility of the electronic information resource UpToDate for clinical decision making at bedside rounds. Singapore Med J. 2012;53(2):116–120. [PubMed] [Google Scholar]
- 11.Siegel J, Whalen L, Burgess E, Joyner BL, Jr, Purdy A, Saunders R, et al. Successful implementation of standardized multidisciplinary bedside rounds, including daily goals, in a pediatric ICU. Jt Comm J Qual Patient Saf. 2014;40(2):83–90. doi: 10.1016/s1553-7250(14)40010-2. [DOI] [PubMed] [Google Scholar]
- 12.Sandhu AK, Amin HJ, McLaughlin K, Lockyer J. Leading educationally effective family-centered bedside rounds. J Grad Med Educ. 2013;5(4):594–599. doi: 10.4300/JGME-D-13-00036.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Szymczak JE, Bosk CL. Training for efficiency: work, time, and systems-based practice in medical residency. J Health Soc Behav. 2012;53(3):344–358. doi: 10.1177/0022146512451130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blackmore CC, Edwards JW, Searles C, Wechter D, Mecklenburg RS, Kaplan GS. Nurse practitioner-staffed clinic at Virginia Mason improved care and lowers costs for women with benign breast conditions. Health Aff (Millwood) 2013;32(1):20–26. doi: 10.1377/hlthaff.2012.0006. [DOI] [PubMed] [Google Scholar]
- 15.Ching J, Long C, Williams B, Blackmore CC. Using Lean to improve medication administration safety: in search of the “perfect dose.”. Jt Comm J Qual Saf. 2013;39(5):195–204. doi: 10.1016/s1553-7250(13)39026-6. [DOI] [PubMed] [Google Scholar]