Abstract
BACKGROUND
As part of a randomized controlled trial, problem drinkers who recently initiated natural recovery on their own were offered access to an Interactive Voice Response (IVR) self-monitoring (SM) system as a sobriety maintenance tool during early recovery when relapse risk is high. Because observed IVR utilization was variable, predictors of utilization were evaluated to inform knowledge of populations likely to access and use IVR services.
METHODS
Participants were 87 untreated community-dwelling adults who recently initiated sobriety following longstanding high-risk drinking practices and alcohol-related problems (M = 16.58 years, SD = 10.95). Baseline interviews assessed pre-resolution drinking practices and problems, and behavioral economic (BE) measures of reward preferences (delay discounting, pre-resolution monetary allocation). Participants had IVR access for 24 weeks to report daily drinking and to hear weekly recovery-focused messages.
RESULTS
IVR use ranged from 0 to 100%. Frequent (n = 28), infrequent (n = 42), and non-caller (n = 17) groups were identified. Non-callers tended to be younger and to report heavier pre-resolution drinking. Frequent callers (≥ 70% of IVR days) tended to be older, male non-smokers with higher/stable socio-economic status and lower delay discounting compared to infrequent callers. Premature drop-out typically occurred fairly abruptly and was related to extended binge drinking.
CONCLUSIONS
Characteristics common in the untreated problem drinker population were associated with higher IVR utilization. This large under-served population segment can be targeted for lower intensity alcohol interventions using an IVR platform.
Keywords: natural recovery, interactive voice response, alcohol, utilization, behavioral economics
1. Background
Most problem drinkers do not seek professional alcohol treatment (Klingemann and Sobell, 2007). The minority who do tend to have more severe problems and to seek help late in problem development when health and daily functioning have been impaired (Simpson and Tucker, 2002; Sobell et al., 1996). Lower threshold interventions not requiring health care system entry are needed to expand services for drinkers who find formal treatment and mutual help groups such as Alcoholics Anonymous (AA) unappealing (Tucker and Simpson, 2011).
Interactive Voice Response (IVR) systems are a computerized telecommunications platform that can extend the reach of care from the clinic into the community (Abu-Hasaballah et al., 2007; Tucker and Grimley, 2011). They allow callers to report quickly and privately on health behaviors, including alcohol use (e.g., Helzer et al., 2008) and related contextual variables (e.g., Ayer et al., 2011), and can be made available over long intervals for cost-effective risk monitoring, relapse prevention, and rapid treatment re-entry when needed (Tucker and Simpson, 2011). Although generally well accepted, IVR systems are not universally appealing, and utilization varies (e.g., Helzer et al., 2008; Mundt et al., 2006). Furthermore, most studies have evaluated IVR applications delivered in conjunction with professional alcohol treatment (e.g., for post-treatment relapse prevention), but not as a stand-alone aid to natural resolution. In either case, understanding which segments of drinkers find IVR systems appealing is essential to realizing their potential as stand-alone interventions for otherwise untreated high-risk drinkers or as clinical treatment add-ons.
Data analyzed in the present study are from an evaluation of IVR self-monitoring (SM) as a tool for stabilizing natural recoveries (Tucker et al., 2011). IVR SM had beneficial effects on drinking outcomes for selected subgroups of the non-treatment-seeking sample, but only if it was used. The present study investigated predictors of observed IVR utilization among problem drinkers who had recently initiated sobriety on their own, either abstinence or low-risk drinking without problems, following longstanding high-risk drinking practices and alcohol-related problems. IVR access was presented as a low-intensity recovery support option that did not require entering formal alcohol treatment, which is unappealing to many persons with alcohol-related problems. Shortly after initiating sobriety, when relapse risk was high, participants received 24 weeks of IVR access to report daily drinking and contextual variables and to hear recovery-support messages. Prior to IVR access, baseline interviews assessed established drinking outcome predictors including demographics, pre-resolution drinking practices and problems, and behavioral economic (BE) measures of impulsive choice and preference for short-term rewards such as drinking (i.e., delay discounting, pre-resolution discretionary spending on alcohol versus saving for the future; Tucker et al., 2009).
Three sets of hypotheses were evaluated using data from participants randomized to the IVR intervention condition. First, consistent with past research, IVR utilization was predicted to vary across participants, with greater utilization associated with older age and higher or more stable socio-economic status (SES; e.g., Horvath et al., 2007). Second, BE measures of impulsive choice shown to predict addictive behavior change (e.g., Bickel and Marsch, 2001; Tucker et al., 2009) were investigated in relation to IVR utilization. Persons with addictive disorders tend to make choices that favor shorter- over longer-term rewards and to organize present behavior accordingly. Consistent engagement in IVR SM was hypothesized to be associated with less impulsive baseline behavior patterns, i.e., lower discounting of delayed rewards and relatively greater pre-resolution year monetary allocation to saving for the future than purchasing alcohol. Third, premature IVR drop-out was hypothesized to vary with drinking practices reported earlier during the SM interval. Conventional wisdom suggested that IVR dropout would be preceded by relapse, particularly extended binge drinking. An alternative possibility was that IVR dropout would be preceded by stable abstinence making continued SM less useful for behavioral regulation.
2. Methods
2.1. Sample Characteristics
The sample consisted of the subset of 87 participants in the larger trial who were randomized to the IVR SM intervention designed to support initial recovery without formal alcohol treatment from a qualified provider or program (e.g., professional counseling, physician supervised pharmacotherapy, residential/outpatient treatment) or extensive participation in AA or other mutual help groups (Tucker et al., 2011). The assessment-only control group did not provide IVR data and were excluded from the present analyses. The research received Institutional Review Board approval and a federal Certificate of Confidentiality.
Advertisements recruited adults in Alabama, Georgia, and Mississippi, who were screened using the Michigan Alcoholism Screening Test (MAST; Selzer, 1971), Alcohol Dependence Scale (ADS; Skinner and Horn, 1984), and Drinking Problems Scale (DPS; Cahalan, 1970). Eligibility criteria were: (1) legal drinking age (≥ 21 years), (2) high-risk drinking practices and alcohol-related problems ≥ 2 years, (3) no current other drug misuse (except nicotine) based on participants’ reports of current use of other drugs at initial assessment, and (4) problem drinking cessation in the past 3-16 weeks without alcohol-focused interventions (M = 2.30 months resolved, SD = 0.99). Resolution onset was defined as the most recent date participants began abstaining or drinking in a non-problem manner without further high-risk drinking (Sobell et al., 1996). Non-problem drinking was defined as (a) no dependence symptoms on the ADS; (b) no alcohol-related negative consequences on the DPS; and (c) no risky drinking days (≥ 5 standard drinks/day for men, ≥ 4 drinks/day for women; National Institute on Alcohol Abuse and Alcoholism, 2005). Problem drinking was defined as drinking that exceeded these limitations on any screening criterion. Limited earlier help-seeking was not an exclusion criterion if it occurred ≥ 2 years before the current resolution and was limited to medication, religious/pastoral counseling, or lifetime attendance of ≤ 9 AA meetings.
Table 1 presents the sample baseline characteristics as a function of subsequent IVR utilization patterns. Problem histories were consistent with moderate alcohol dependence typical of outpatient treatment samples (Miller and Munoz, 2005). Although not required, participants met diagnostic criteria for alcohol dependence (American Psychiatric Association, 1994).
Table 1.
Sample characteristics at initial assessment as a function of IVR caller group
| Non-callers (n = 17) |
Infrequent callers (n = 42) |
Frequent callers (n = 28) |
Test Statistic | p value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | (SD) | % | M | (SD) | % | M | (SD) | % | |||
| Demographic characteristics | |||||||||||
| Male | 82.4 | 47.6 | 75.0 | χ2(2) = 8.74 | .013 | ||||||
| Female | 17.6 | 52.4 | 25.0 | ||||||||
| White | 41.2 | 47.6 | 57.1 | χ2(2) = 1.18 | ns | ||||||
| Other race/ethnicity | 58.8 | 52.4 | 42.9 | ||||||||
| Married/partnered | 47.1 | 28.6 | 51.8 | χ2(2) = 4.23 | ns | ||||||
| Employed full- or part-time | 52.9 | 45.2 | 48.1 | χ2(2) = 0.29 | ns | ||||||
| Age (years) | 40.82 | (15.21) | 44.64 | (9.47) | 52.82 | (10.36) | F(2. 84) = 7.40 | .001 | |||
| Years of education | 13.35 | (1.84) | 13.60 | (2.70) | 15.09 | (3.50) | F(2, 83) = 2.88 | .062 | |||
| Drinking history | |||||||||||
| Problem duration (years) | 11.44 | (8.39) | 17.40 | (10.62) | 18.66 | (12.20) | F(2, 80) = 2.55 | .084 | |||
| Alcohol Dependence Scale | 18.81 | (9.23) | 18.48 | (8.15) | 17.61 | (11.33) | F(2, 83) = 0.10 | ns | |||
| Michigan Alcoholism Screening Test | 13.41 | (3.97) | 13.05 | (3.38) | 11.93 | (4.22) | F(2, 83) = 1.05 | ns | |||
| Drinking Practices Scale | 20.06 | (9.74) | 17.98 | (8.33) | 16.50 | (10.23) | F(2, 83) = 0.78 | ns | |||
| Resolved abstinent (initial status) | 64.7 | 83.3 | 85.7 | χ2(2) = 3.40 | ns | ||||||
| Resolved non-abstinent | 35.3 | 16.7 | 14.3 | ||||||||
| Pre-resolution year drinking practices (TLFB) | |||||||||||
| % heavy drinking days | 75.75 | (30.41) | 56.03 | (40.12) | 43.98 | (37.79) | F(2, 84) = 3.76 | .028 | |||
| Quantity/drinking day (ml ethanol) | 243.40 | (155.72) | 184.39 | (108.99) | 175.02 | (126.41) | F(2, 84) = 1.78 | ns | |||
| Current tobacco use | 76.9 | 74.19 | 35.0 | χ2(2) = 9.42 | .009 | ||||||
| Behavioral economic measures | |||||||||||
| Discounting rate (log k) | −5.15 | (2.34) | −4.60 | (1.86) | −5.75 | (2.52) | F(2, 81) = 2.27 | .110 | |||
| Total income (dollars) | 41,971 | (27,652) | 32,646 | (30,807) | 77,597 | (81,673) | F(2, 84) = 6.35 | .003 | |||
| Discretionary expenditures (DE) | 18,224 | (12,926) | 11,556 | (7,755) | 16,945 | (13,710) | F(2, 84) = 3.15 | .048 | |||
| Proportion DE on alcohol (A/DE) | 0.25 | (0.17) | 0.29 | (0.25) | 0.26 | (0.27) | F(2, 84) = 0.17 | ns | |||
| Proportion DE on savings (S/DE) | 0.06 | (0.15) | 0.01 | (0.04) | 0.07 | (0.16) | F(2, 84) = 2.62 | .079 | |||
| ASDE index | 0.19 | (0.27) | 0.28 | (0.26) | 0.19 | (0.35) | F(2, 84) = 0.95 | ns | |||
Note. Reward k-parameters and total income log-transformed for analysis. P-values are from one-way analyses of variance or chi-square tests comparing the three IVR utilization groups; ns = non-significant with p > .10. TLFB = Timeline Followback interview. DE = sum of dollars spent in pre-resolution year on discretionary commodities (e.g., entertainment, alcoholic beverages, tobacco, gifts, savings; see text); the proportion of DE spent on alcoholic beverages (A/DE) or put into savings (S/DE) could vary from 0 (no spending) to 1.0 (all discretionary spending allocated to either alcohol or savings). ASDE = Alcohol/Savings Discretionary Expenditure index computed as [(A/DE) – (S/DE)]. Values could range from 1.0 to −1.0 (1.0 = all DE for alcoholic beverages and −1.0 = all DE were for saving money; 0 = equal proportions of DE for alcohol and savings).
2.2 Procedures
Procedures summarized here are similar to those detailed in earlier publications (e.g., Tucker et al., 2007, 2009, 2011), including selection of validated measures and establishment of interview reliability and validity. All procedures described here are specific to the current study; selected procedures relevant only to the parent study are published elsewhere (Tucker et al., 2011). In baseline sessions, participants were consented, with sobriety verified by breathalyzer. Drinking practices and monetary allocation during the pre-resolution year were assessed using an expanded Timeline Followback (TLFB) interview (Sobell and Sobell, 1992; Vuchinich and Tucker, 1996). Participants were administered a computerized delay discounting task (Rachlin et al., 1991), received IVR training, and given IVR access for 24 weeks. Compensation was via university-issued gift cards or checks ($50 per interview).
Drinking practices and money spent on alcohol
Participants reported past year consumption of beer, wine, or liquor consumed (in oz.), converted to ml of 190-proof ethanol for analysis. They also reported daily spending on alcohol, regardless of whether the alcohol was consumed.
Monetary allocation
Participants reported income and expenditures for the same period using U.S. federal consumer expenditure commodity classes (Vuchinich and Tucker, 1996). Income in dollars was reported by source (e.g., wages, loans). Expenditures were reported in three general categories, each with subcategories, including housing (e.g., mortgage, utilities), consumable goods (e.g., food, alcohol), and other (e.g., entertainment, voluntary savings). Transactions were summed to obtain category totals for analysis.
Pre-resolution year expenditures were separated into obligatory and discretionary categories (Tucker et al., 2009). Obligatory expenditures were for essential, largely fixed costs of living (e.g., housing, transportation). Discretionary expenditures were for less essential, intermittently purchased commodities (e.g., recreation, alcohol, elective savings). An Alcohol-Savings Discretionary Expenditure (ASDE) index was computed for analysis as the proportion of pre-resolution discretionary expenditures spent on alcohol minus the proportion put voluntarily into savings. ASDE values ranged from 1.0 to – 1.0; higher scores indicated proportionally more money spent on alcohol and less toward savings.
Delay discounting task
Participants repeatedly chose between hypothetical monetary rewards of smaller amounts now versus a larger amount later (e.g., “$500 now or $1000 in 6 months?”) across a series of delays (Rachlin et al., 1991). A titration procedure determined an equivalence point at each delay, at which the values of the larger later and the smaller immediate amounts were rated as equally preferred. Equivalence points were fit to Mazur's (1987) discounting equation to determine a discount rate (k-parameter) for each participant: v = Ai/(1 + k Di), with v, Ai and Di representing the equivalent present value (e.g., $500), the fixed delayed amount (e.g., $1,000), and delay in weeks to the reward, respectively. The k-parameter is an individual difference variable, generally ranging from 0 to 1, that is proportional to rate of reward discounting. Higher k-parameters indicate higher discounting and stronger preference for more immediate rewards. Because k-parameters tend to cluster at the lower end of the possible range, analyses used the natural logarithm of k.
IVR intervention
Detailed description is available in Tucker et al. (2011). After training, participants accessed the toll-free IVR system, programmed using commercial software (SmartQ-Version 5(5.0.141), Telesage, Chapel Hill, NC). Daily questions assessed ounces of beer, wine, and liquor consumed; use of other drugs to “get high;” and dollars spent on alcohol and other drugs during the 24-hour period midnight-to-midnight yesterday. Questions about other activities on the preceding day balanced call duration when no substance use was reported.
Additional questions asked once a week varied day-to-day on Monday through Thursday (e.g., strategies used to avoid/limit drinking, activities paired with drinking). On Mondays, participants received verbal feedback concerning last week's drinking goals and set goals for the coming week. On Fridays, they could listen to 1-2 minute IVR-delivered education modules patterned after guided self-change materials (e.g., goal-setting, relapse prevention) (Sobell and Sobell, 1993). Daily and weekly surveys averaged 4.6 and 2.3 minutes, respectively.
Points for daily calls were awarded and modestly reimbursed via an “electronic bank” (Searles et al., 1995), a commonly used procedure to encourage daily calls. Participants received $0.50 minimum for each daily call and $1.00 after 7 consecutive calls; bonus payments stopped when a call was missed, were reinstated after another 7 consecutive calls, and so forth. Among those who called at least once, mean earnings were $33.79 (SD = 52.56).
Data quality checks
Participant reports of help-seeking, resolution status, and drinking practices were verified using brief collateral phone interviews scheduled after participants’ initial interview and annually thereafter; 82% of participants nominated collaterals, and one or more collateral interviews were completed for 43% of participants with collaterals. Data from one participant were excluded due to inconsistent reporting of help-seeking. As a further reliability check, TLFB and IVR drinking reports were compared for the 30 participants who provided ≥ 10 days of time-matched reports. Reports of drinking practices did not differ significantly across measures, which correlated 0.854 for percentage of drinking days during the IVR interval and 0.656 for mean quantities consumed per drinking day (ps < .0001). These results support that participants gave reliable reports of study eligibility criteria and drinking behavior (Sobell and Sobell, 1992).
2. 3 Statistical Analysis
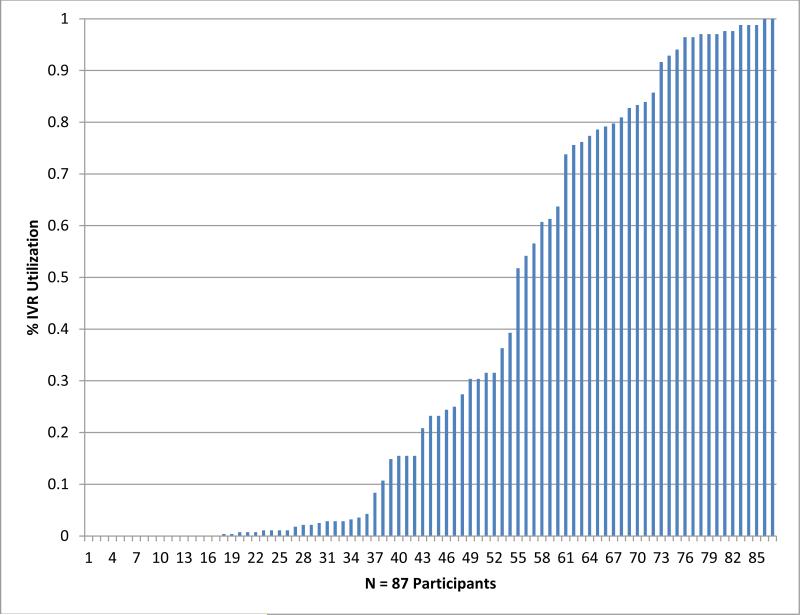
Participants were categorized as either (1) callers (n = 70) or non-callers (n = 17), depending on whether they ever called the IVR system; and (2) among callers, whether they were frequent (n = 28) or infrequent (n = 42) callers based on whether they did or did not complete ≥ 70% of scheduled daily calls, respectively. As Figure 1 shows, two notable factures were observed in the cumulative percentage of IVR calls around 70% and 50%. The 70% cut-point was used for analysis given our interest in promoting IVR utilization.
Figure 1.
Percentage of scheduled calls made to the IVR system over the 168 day self-monitoring interval. The x-axis represents each of the 87 participants, and the y-axis is the percentage of their daily calls (0 to 100%).
As summarized in Table 1, baseline variables were screened as potential candidate predictors of IVR utilization in preliminary univariate analyses of variance or chi-square tests that compared the three IVR utilization groups. Variables that were significant (p < .05) or approached significance (p < .10) in these overall tests were then evaluated in two sets of logistic regression analyses that separately compared callers vs. non-callers (N = 87) and infrequent vs. frequent callers, excluding non-callers (n = 70). Non-callers were the referent group in the set of analyses concerned with IVR engagement. Infrequent callers were the referent group in the set of analyses concerned with IVR utilization among callers.
Univariate logistic regression models included one candidate predictor of IVR utilization from among those identified per Table 1. Variables that were significant or approached significance in the single variable models or were relevant to the hypotheses were then evaluated in multivariate logistic regression models that included two or three predictors and examined the relative utility of predictors at the p < .05 significance level. Odds ratios (ORs) based on a one standard deviation change in the predictor variable and associated 95% confidence intervals (CI) are reported for continuous variables to allow for direct comparisons. Dichotomous variables were not z-transformed.
Cox proportional hazards survival analyses were conducted to evaluate the third study hypothesis concerning whether quitting calling was related to drinking patterns reported earlier during the IVR interval. The to-be-predicted event was the last call day before no further calls were made up to the final week of IVR availability (week 24). Participants who made at least 1 call during the final week were right-censored cases (n = 29 of 70 callers). Four time-dependent variables were examined in separate survival analyses: cumulative heavy drinking calls and cumulative abstinent calls prior to the last call day, summed over the IVR participation interval; and cumulative consecutive heavy drinking call days and cumulative consecutive abstinent call days, which reflected the extent of multiple day runs of heavy drinking or abstinence calls across the IVR participation interval. The possibility that IVR drop-out was related to relapse was examined in models that included either cumulative or cumulative consecutive heavy drinking calls, whereas the alternative possibility that stable abstinence predicted IVR drop-out was examined in the models that included either cumulative or cumulative consecutive abstinent calls. Time-invariant predictors were age, log k, and current smoking status (based on the logistic regression results).
3.0 Results
3.1 IVR Utilization
Figure 1 presents the percentage of days that each of the 87 participants made scheduled IVR calls over the 168-day reporting interval. Call frequency ranged from 0 to 100%. For the whole sample (70 callers, 17 non-callers), the mean percentage of IVR call days was 37.77% (SD = 38.98), and the median was 23%. For callers only, the mean was 46.95% (SD = 38.17), and the median was 34%.
3.2 Predictors of IVR Utilization
Table 2 summarizes results of the single variable logistic regressions that compared caller and non-callers (N = 87) or infrequent and frequent callers, excluding non-callers (n = 70). Because only age showed significant univariate effects in both contrasts, the 2-variable logistic regression models included age and one other candidate predictor. These findings are presented next for each contrast.
Table 2.
Logistic regression results using one baseline variable to predict IVR utilization
| Callers (n = 70) vs. Non-callers (n = 17) |
Frequent (n = 28) vs. Infrequent callers (n = 42) |
|||||
|---|---|---|---|---|---|---|
| Baseline variable | OR | 95% CI | p | OR | 95% CI | p |
| Demographic characteristics | ||||||
| Age | 1.934 | 1.06, 3.53 | .031 | 2.670 | 1.41, 5.05 | .003 |
| Gender | 0.303 | 0.08, 1.15 | .080 | 3.300 | 1.16, 9.41 | .026 |
| Married | 0.689 | 0.24, 2.01 | ns | 2.724 | 0.99, 7.48 | .052 |
| Years of education | 1.430 | 0.74, 2.76 | ns | 1.617 | 0.97, 2.69 | .063 |
| Substance use | ||||||
| Drinking problem duration (years) | 2.150 | 1.10, 4.22 | .026 | 1.097 | 0.70, 1.73 | ns |
| % pre-resolution heavy drinking days | 0.487 | 0.26, 0.91 | .025 | 0.733 | 0.45, 1.19 | ns |
| Quantity/drinking day (ml ethanol) | 0.641 | 0.39, 1.05 | .076 | 0.913 | 0.54, 1.55 | ns |
| Current tobacco use | 0.572 | 0.15, 2.15 | ns | 0.171 | 0.05, 0.53 | .002 |
| Behavioral economic variables | ||||||
| Discount rate (log k) | 1.068 | 0.63, 1.81 | ns | 0.549 | 0.32, 0.95 | .031 |
| Pre-resolution year income (log scale) | 0.749 | 0.37, 1.52 | ns | 2.327 | 1.13, 4.80 | .022 |
| Proportion DE on alcohol (A/DE) | 1.102 | 0.63, 1.92 | ns | 0.898 | 0.57, 1.42 | ns |
| Proportion DE on savings (S/DE) | 0.841 | 0.53, 1.33 | ns | 2.332 | 0.94, 5.76 | .066 |
| ASDE index | 1.175 | 0.68, 2.02 | ns | 0.733 | 0.45, 1.21 | ns |
Note. Reference groups were non-callers or infrequent callers (< 70% of IVR days). Continuous predictor variables were z-transformed to allow direct comparisons among odds ratios (OR) adjusted to indicate a one standard deviation change in the predictor variable; dichotomous variables were not z-transformed. P-values are for the associated 95% confidence intervals (CI). DE = sum of dollars spent in pre-resolution year on discretionary commodities (e.g., entertainment, alcoholic beverages, tobacco, gifts, savings); the proportion of DE spent on alcoholic beverages (A/DE) or put into savings (S/DE) could vary from 0 (no spending) to 1.0 (all discretionary spending allocated to alcohol or savings). ASDE = Alcohol/Savings Discretionary Expenditure index computed as [(A/DE) – (S/DE)]. Values could range from 1.0 to −1.0 (1.0 = all DE for alcoholic beverages and −1.0 = all DE were for saving money; 0 = equal proportions of DE for alcohol and savings).
3.2.1 Callers versus non-callers
In models with one predictor of whether participants started the IVR, significant ORs were observed for age (p = .031), drinking problem duration (p < .026), and percentage of pre-resolution heavy drinking days (p = .025). One standard deviation increases in age and problem duration, respectively, were associated with 1.93- and 2.15-fold increases in the odds of calling the IVR system, whereas a one standard deviation increase in heavy drinking days was associated with a 2.05-fold decrease in the odds of calling. BE measures had no predictive utility in distinguishing callers from non-callers.
A second set of logistic regression models included age and one other predictor from among those with effects at p < .10 in the single variable models. As Table 2 shows, age remained significant in all models except when paired with problem duration, perhaps because the two variables were significantly correlated (r = .436, p < .001). Percentage of heavy drinking days remained significant when paired with age (p = .036). Thus, younger age was a robust predictor of failure to engage the IVR task when paired with all other predictors.
3.2.2 Frequent versus infrequent callers
Older age (p = .003) and male gender (p = .026) predicted call frequency among callers. However, male gender was associated with higher call frequency. Males tended to not call the IVR at all or to call more frequently compared to females. Females were more likely to be infrequent callers.
Significant ORs also were found for log k (p = .031), income (p = .022), and current tobacco use (p = .002). One standard deviation decreases in log k (indicating lower delay discounting) and current tobacco use, respectively, were associated with a 1.82-fold and a 5.85-fold increase in the odds of being a frequent IVR caller. A one standard deviation increase in income was associated with a 2.33-fold increase in the odds of being a frequent caller.
A second set of logistic regression models included either age or log k with one other predictor from among those with effects at p < .10 (per Table 2) in the single variable models (excluding problem duration given redundancy with age). Age was included because it was an empirically robust predictor, and log k was included because of its conceptual significance in BE addictive behaviors research. As Table 3 summarizes, both variables were significant when included in the same model. When age was paired with one other predictor, male gender (p = .035) and current tobacco use (p = .009) remained significant. When log k was paired with one other predictor, current tobacco use was a significant predictor (p = .006). The predictive utility of log k was somewhat attenuated in the two-variable models except when paired with age and marital status.
Table 3.
Logistic regression results using age or delay discounting and one other baseline variable to predict IVR call frequency (frequent or infrequent)
| Age |
BV |
Discounting (log k) |
BV |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline variable (BV) | r | OR | 95% C | p | OR | 95% C | p | r | OR | 95% CI | p | OR | 95% CI | p |
| Male gender | .063 | 2.668 | 1.39, 5.14 | .003 | 3.363 | 1.09, 10.38 | .035 | −.217 | 0.629 | 0.37, 1.08 | .095 | 2.586 | 0.86, 7.76 | .090 |
| Married | .363 | 2.427 | 1.25, 4.71 | .009 | 1.732 | 0.57, 5.24 | ns | −.190 | 0.569 | 0.33, 0.97 | .039 | 2.628 | 0.92, 7.54 | .072 |
| Current tobacco use | −.271 | 2.584 | 1.27, 5.25 | .009 | 0.182 | 0.05, 0.65 | .009 | .236 | 0.599 | 0.34, 1.07 | .082 | 0.190 | 0.06, 0.62 | .006 |
| Pre-resolution income | .099 | 2.459 | 1.28, 4.71 | .007 | 1.989 | 0.95, 4.16 | .068 | −.150 | 0.612 | 0.35, 1.07 | .084 | 1.998 | 0.95, 4.18 | .066 |
| Proportion DE on savings | .063 | 2.485 | 1.28, 4.81 | .007 | 2.133 | 0.83, 5.49 | ns | −.168 | 0.058 | 0.33, 1.00 | .050 | 2.298 | 0.87, 6.04 | .092 |
| Discounting rate (log k) | −.035 | 2.683 | 1.42, 5.07 | .002 | 0.520 | 0.29, 0.94 | .030 | -------------------------------------------------------------------------- | ||||||
Note. Reference group was infrequent callers (< 70% of IVR days). Continuous predictor variables were z-transformed to allow direct comparisons among adds ratios (OR) adjusted to indicate a one standard deviation change in the predictor variable; dichotomous variables were not z-transformed. P-values are for the associated 95% confidence intervals (CI). DE = sum of dollars spent in pre-resolution year on discretionary commodities (e.g., entertainment, alcoholic beverages, tobacco, gifts, savings; see text); the proportion of DE spent on alcoholic beverages (A/DE) or put into savings (S/DE) could vary from 0 (no spending) to 1.0 (all discretionary spending allocated to either alcohol or savings).
As a final step, select 3-variable models included age, log k, and a third significant predictor in the 2-variable models (i.e., gender, marital status, current tobacco use, income). Age was significant in all four 3-variable models, log k was significant or near significant in all models, and only current tobacco use had further predictive utility when paired with age and log k. In the model with these three variables together, the ORs for age, log k, and current tobacco use were 2.640 (CI = 1.30, 5.36, p = .007), 0.555 (CI = 0.30, 1.04, p = 0.067), and 0.202 (CI = 0.05, 0.76, p = .018), respectively. Older non-smokers with lower discounting rates were more likely to be frequent callers.
3.3 Attrition Patterns among IVR Callers
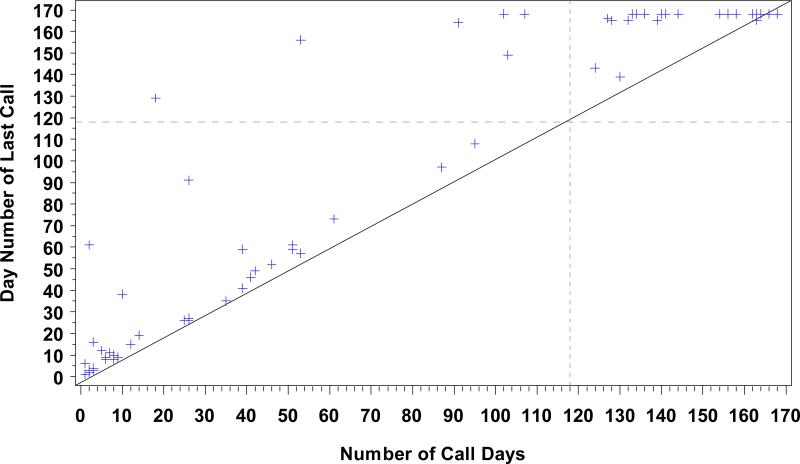
To examine call pattern variability across the IVR interval, the total number of call days was plotted against the day number of the last call for each caller. This reflects the duration of the IVR participation interval regardless of call frequency. The two measures were highly correlated (r = .940, p < .0001), with means of 78.87 (SD = 64.13) and 96.06 (SD = 69.91) days for frequency and duration, respectively, among callers. As Figure 2 shows, call frequency and duration had similar values for most callers, indicating daily calling with few missed days until abrupt cessation of calling. A minority called relatively infrequently with interspersed intervals of consecutive missed days over longer IVR participation periods.
Figure 2.
IVR call frequency versus days until the last call for each of 70 callers. The x-axis shows the total number of call days (168-days maximum), and the y-axis shows the final call day. The dashed lines at Day 118 represent 70% call compliance, the cut-point for categorizing callers into frequent and infrequent groups for analysis. The diagonal solid line represents consecutive daily calling until participants abruptly stopped calling. The area above the diagonal line represents daily calling with missed days. The distance from the diagonal line reflects the number of missed days.
Cox proportional hazards models to predict when participants stopped using the IVR revealed significant or near significant effects for all time invariant predictors (age, log k, tobacco use), consistent with the logistic regression results. Cumulative consecutive heavy drinking calls was the only time-varying predictor that approached significance (hazard ratio = 1.311, p = .073). Each consecutive heavy drinking day increased the probability of IVR drop-out by 31%, suggesting a trend for extended relapses to increase risk for stopping IVR use.
4. Discussion
Consistent with past research, most participants called the IVR system at least once, but a minority never called. Compared to callers, non-callers were younger, had shorter problem histories, and reported heavier pre-resolution drinking practices. Younger age was the most robust predictor of failure to engage in the IVR task when paired with all other potential predictors. BE variables had no predictive utility in distinguishing callers from non-callers, despite their association in prior research with younger age and risk-taking (Read, 2004).
Among callers, findings supported the hypothesis that frequent callers would be relatively older and have greater socio-economic stability and lower reward discount rates. Consistent with observed associations between smoking status and discount rates, frequent callers also were more likely to be non-smokers (Bickel and Marsch, 2001). The ASDE index did not predict call frequency. The single model that best predicted high call frequency included older age, no current tobacco use, and lower delay discounting.
The results advance understanding about how to develop appealing IVR-based interventions for the large under-served population of persons with alcohol-related problems who do not seek help from treatment or mutual aid groups. First, even though we did not have well established relationships with callers, IVR engagement and retention among our natural resolution sample were similar to patterns observed when IVR was offered as a treatment adjunct or aftercare option (e.g., Aharonovich et al., 2006; cf. Abu-Hasaballah et al., 2007). Results supported use of IVR systems to monitor and support change over intervals that extend beyond time-limited treatments.
Second, drinker characteristics that predicted higher IVR utilization (e.g., older, higher SES, non-smokers with longer time horizons) also are good prognostic indicators of stable recovery. They are common characteristics among untreated problem drinkers with less severe problems for whom lower intensity interventions are appropriate (Tucker and Simpson, 2011). Third, the finding that recovering problem drinkers with lower discount rates engaged IVR SM with higher frequency is consistent with the possibility that IVR SM functioned as behavioral chaining, in which a series of short-term discrete acts of daily SM assisted in building and making salient an emerging pattern of longer term rewarding behaviors, i.e., sobriety and its benefits (Rachlin, 1995).
A question remains whether IVR SM is enough to support longer term positive change and the relative influence of different components of the IVR system on outcomes. For example, participants were provided access to daily IVR SM, and they also had access to IVR-delivered educational modules (e.g., goal setting, relapse prevention) and received monthly feedback letters highlighting the behaviors they reported via IVR SM. Results from the larger RCT reported elsewhere (Tucker et al., 2011) suggested that IVR SM selectively supported moderation if it was used, which underscores why it is important to investigate and promote IVR utilization. While not the focus of the present study, understanding the relative contributions to behavior change of components such as IVR SM, feedback letters, and weekly surveys is an important question for future studies.
Fourth, attrition among IVR callers suggested that the great majority who quit calling did so fairly abruptly after calling consistently. A minority made infrequent calls over long intervals. These results raise questions about attrition predictors and handling of missed calls. Tentative evidence from the survival analyses suggested that consecutive heavy drinking days (binges) contributed to premature IVR drop-out, even though heavy drinking per se did not, nor did cumulative or cumulative consecutive abstinent days. These findings suggest drop-out intervention points for providers using IVR technology.
How best to promote IVR utilization merits further research. Although we sought to promote utilization using an electronic bank with modest payments for daily calls, we did not aggressively call participants who stopped calling except for making two reminder calls. This decision was based on Mundt et al.'s (2006) finding that repeated reminder calls tended to undermine further IVR participation. We did not elect to make automated reminder calls using the IVR system given potential participant confidentiality risks. In applied settings where monetary payment is not feasible, lottery or voucher systems similar to those used successfully in contingency management programs (Lussier et al, 2006) may be a good option.
The variable utilization rates observed in the study supported use of an IVR-based, low-intensity telehealth intervention for a specific segment of problem drinkers who were attempting to quit problem drinking on their own. Phone access is near universal, and continuing advances in technology provide opportunities to combine the individualization of clinical care with public health dissemination strategies to reach more problem drinkers in community settings (Tucker and Grimley, 2011). Advancing this health services agenda depends on continued development of IVR-based approaches and understanding how IVR utilization interacts with drinker characteristics and contexts to support behavior change.
Acknowledgments
Role of Funding Source
Funding for this study was provided by NIAAA Grant 2 R01 AA008972 and NIAAA ARRA supplement 3 R01 AA008972-16S1; the NIAAA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Authors Tucker and Simpson designed the study and wrote the protocol. Authors Simpson and Tucker managed the literature searches and summaries of previous related work. Authors Huang and Roth undertook the statistical analysis, authors Simpson and Tucker wrote the first draft of the manuscript, and authors Simpson, Huang, Roth, Chandler, and Tucker participated in writing subsequent drafts. All authors contributed to and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
References
- Abu-Hasaballah K, James A, Aseltine RH., Jr. Lessons and pitfalls of interactive voice response in medical research. Contemp. Clin. Trials. 2007;28:593–602. doi: 10.1016/j.cct.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Aharonovich E, Hatzenbuehlerm ML, Johnston B, O'Leary A, Morgenstern J, Wainberg ML, Yao P, Helzer JE, Hasin DS. A low-cost, sustainable intervention for drinking reduction in the HIV primary care setting. AIDS Care. 2006;18:561–568. doi: 10.1080/09540120500264134. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; Washington, D.C.: 1994. [Google Scholar]
- Ayer LA, Harder VS, Rose GL, Helzer JE. Drinking and stress: an examination of sex and stressor differences using IVR-based daily data. Drug Alcohol Depend. 2011;115:205–212. doi: 10.1016/j.drugalcdep.2010.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA. Toward a behavioral economic understanding of drug dependence: delay discounting processes. Addiction. 2001;96:73–86. doi: 10.1046/j.1360-0443.2001.961736.x. [DOI] [PubMed] [Google Scholar]
- Calahan D. Problem Drinkers: A National Survey. Jossey-Bass; San Francisco: 1970. [Google Scholar]
- Helzer JE, Rose GL, Badger GJ, Searles JS, Colleen ST, Lindberg SA, Guth S. Using interactive voice response to enhance brief alcohol intervention in primary care settings. J. Stud. Alcohol Drugs. 2008;69:251–258. doi: 10.15288/jsad.2008.69.251. [DOI] [PubMed] [Google Scholar]
- Horvath KJ, Beadnell B, Brown AM. A daily web diary of the sexual experiences of men who have sex with men: comparisons with a recall survey. AIDS Behav. 2007;11:537–548. doi: 10.1007/s10461-007-9206-y. [DOI] [PubMed] [Google Scholar]
- Klingemann H, Sobell LC, editors. Promoting Self-change from Addictive Behaviors: Practical Implications for Policy, Prevention, and Treatment. Springer; New York: 2007. [Google Scholar]
- Little RJ, Yau LHY. Statistical techniques for analyzing data from prevention trials: treatment of no-shows using Rubin's causal model. Psychol. Methods. 1998;3:147–159. [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Mahoney DF, Tarlow BJ, Jones RN. Effects of an automated telephone support system on caregiver burden and anxiety: Findings from the REACH TLC study. Gerontologist. 2003;43:556–67. doi: 10.1093/geront/43.4.556. [DOI] [PubMed] [Google Scholar]
- Mazur J. An adjusting procedure for studying delayed reinforcement. In: Commons M, Mazur J, Nevin JA, Rachlin H, editors. Quantitative Analysis of Behavior (Vol. 5): The Effect of Delay and of Intervention Events on Reinforcement Value. Lawrence Erlbaum Associates; Hillsdale, NJ: 1987. [Google Scholar]
- Miller WR, Munoz RF. Controlling Your Drinking: Tools to Make Moderation Work for You. Guilford; New York: 2005. [Google Scholar]
- Mundt JC, Moore HK, Bean P. An interactive voice response program to reduce drinking relapse: a feasibility study. J. Subst. Abuse Treat. 2006;30:21–29. doi: 10.1016/j.jsat.2005.08.010. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism . Helping Patients Who Drink Too Much: A Clinician's Guide. NIAAA/National Institutes of Health/U.S. Department of Health and Human Services; Rockville, MD: 2005. [Google Scholar]
- Rachlin H. Self-control: beyond commitment. Behav. Brain Sci. 1995;18:109–159. [Google Scholar]
- Rachlin H, Raineri A, Cross D. Subjective probability and delay. J. Exp. Anal. Behav. 1991;55:233–244. doi: 10.1901/jeab.1991.55-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read D. Time discounting over the lifespan. Organ Behav. Hum. Decis. Process. 2004;94:22–32. [Google Scholar]
- Searles JS, Perrine MW, Mundt JC, Helzer JE. Self-report of drinking using touch-tone telephone: extending the limits of reliable daily contact. J. Stud. Alcohol. 1995;56:375–382. doi: 10.15288/jsa.1995.56.375. [DOI] [PubMed] [Google Scholar]
- Selzer ML. The Michigan Alcoholism Screening Test: the quest for a new diagnostic instrument. Am. J. Psychiatry. 1971;127:1653–1658. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- Simpson CA, Tucker JA. Temporal sequencing of alcohol-related problems, problem recognition, and help-seeking episodes. Addict. Behav. 2002;27:659–674. doi: 10.1016/s0306-4603(01)00200-3. [DOI] [PubMed] [Google Scholar]
- Skinner HA, Horn JL. Alcohol Dependence Scales (ADS) User's Guide. Addiction Research Foundation; Toronto: 1984. [Google Scholar]
- Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am. J. Public Health. 1996;86:966–972. doi: 10.2105/ajph.86.7.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback: a technique for assessing self-reported alcohol consumption. In: Litten R, Allen J, editors. Measuring Alcohol Consumption. Humana Press; Totowa, N.J.: 1992. pp. 41–72. [Google Scholar]
- Sobell MB, Sobell LC. Problem Drinkers: Guided Self-Change Treatment. Guilford Press; New York: 1993. [Google Scholar]
- Tucker JA, Foushee HR, Black BC, Roth DL. Agreement between prospective IVR self-monitoring and structured retrospective reports of drinking and contextual variables during natural resolution attempts. J. Stud. Alcohol Drugs. 2007;68:538–542. doi: 10.15288/jsad.2007.68.538. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Grimley DM. Public health tools for practicing psychologists. In: Wedding D, Beutler L, Freedland KE, Sobell LC, Wolfe DA, editors. Advances in Psychotherapy — Evidence-based Practice (Vol. 20) Hogrefe and Huber; Cambridge, MA: 2011. [Google Scholar]
- Tucker JA, Roth DL, Huang J, Crawford MS, Simpson CA. Effects of IVR self-monitoring on drinking problems depend on IVR utilization and behavioral economic factors. J. Stud. Alcohol Drugs. doi: 10.15288/jsad.2012.73.686. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JA, Roth DL, Vignolo M, Westfall AO. A behavioral economic reward index predicts drinking resolutions: moderation re-visited and compared with other outcomes. J. Consult. Clin. Psychol. 2009;77:219–228. doi: 10.1037/a0014968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JA, Simpson CA. The recovery spectrum: from self-change to seeking treatment. Alcohol Res. Health. 2011;33:371–379. [PMC free article] [PubMed] [Google Scholar]
- Vuchinich RE, Tucker JA. The molar context of alcohol abuse. In: Green L, Kagel JH, editors. Advances in Behavioral Economics (Vol. 3): Substance use and abuse. Ablex Publishing Co.; 1996. [Google Scholar]