Abstract
BACKGROUND
The prevalence of overweight children has reached epidemic proportions, and affects Latinos youth more than other subgroups in the United States. Given the prevalence of obesity and its economic consequences, community health initiatives have shifted toward primary prevention at younger ages.
METHODS
Data representing all levels of the ecological systems theory were collected using diverse methods. Participants were children enrolled in K-2nd grade and their parents.
RESULTS
Overweight children were less active compared to normal weight children. The parents of overweight children provided less instrumental support to engage in activity and set fewer limits on their child’s activities. Similarly, parents of overweight children were less likely to control, but more likely to set limits on their child’s diet compared to parents of normal weight children. Parents who rated their health more positively and were less acculturated were more likely to have children who were overweight. School and community level variables were not significantly correlated with children’s weight. Adjusting for the aforementioned variables, parents’ weight status was positively associated with children’s weight.
CONCLUSIONS
Social and structural environments in which Hispanic children are reared may play an important role in determining their risk for obesity and related behaviors. Parents’ weight was among the strongest correlate of child weight; however, the extent to which this influence functions primarily through biological or social/structural influences is not entirely clear. The role of school and community factors on child’s health practices and body mass index needs to be further examined.
Keywords: nutrition, diet, physical fitness, sport, chronic diseases, community health
Trends in US children’s overweight and obesity have accelerated in recent years, including marked increases in racial and ethnic disparities.1 Over the past 3 decades, the childhood obesity rate has more than doubled for children aged 2–5 years and adolescents aged 12–19 years, and it has more than tripled for children aged 6–11 years. Recent national data indicate that an estimated 14.5% of low income preschool children are overweight.2 Latino adults and children have been particularly affected by overweight and obesity.3 In 2008, 18.5% of Latino children were overweight.
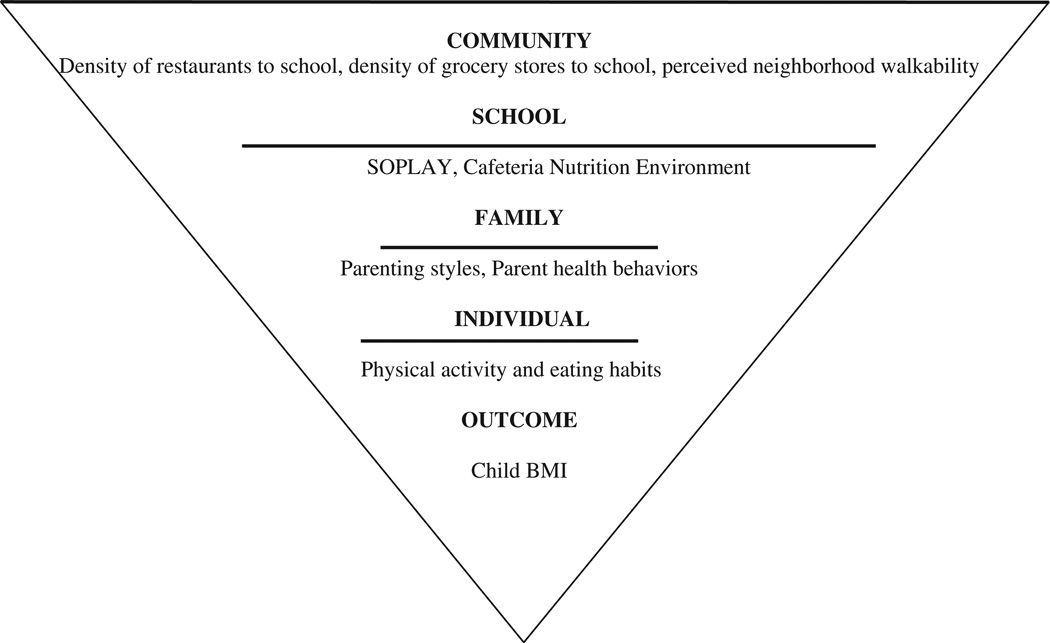
According to the ecological systems theory (EST), childhood overweight is influenced by individual, family, and community factors.4,5 Children who are sedentary and consume high amounts of sugar-sweetened beverages have a higher prevalence of overweight and obesity.6–8 Studies also show that family characteristics and parenting styles shape children’s activity patterns, dietary intake, and obesity risk. Children of parents who use “controlling strategies” (eg, demanding, rigid) are less likely to eat healthy.9 In contrast, monitoring of children’s eating and reinforcing healthy eating encourage healthy eating.10,11 Although the relationship between parenting styles and children’s physical activity (PA) is not fully understood, research suggests that parents who encourage their children to engage in PA have more active children.12 Family characteristics such as parents’ income level are related to children’s weight status, healthy eating, and PA.13,14 Among Hispanics, studies have been inconsistent in showing an association between parental acculturation and children’s body mass index (BMI).15–17 Investigators finding such a relationship note that the process of parental acculturation likely influences the consumption of unhealthy foods, which places Hispanic families at risk for obesity.18 However, acculturation also has been associated with the adoption of PA which complicates the relation between acculturation and weight status.19 Among the strongest predictors of children’s BMI is parents’ BMI.20
School-related factors also impact children’s risk for obesity. Studies have shown that verbal encouragement by school cafeteria staff is positively related to children’s fruit and vegetable consumption.21 Students in schools that facilitate PA by maintaining their activity grounds and providing physical education classes are more active and less likely to be overweight. Veugelers and Fitzgerald22 found that schools offering at least 2 physical education classes per week had fewer overweight children than schools offering fewer classes. The neighborhood environment is also hypothesized to influence childhood obesity risk, but the evidence for this is mixed.23–25 When considering PA opportunities, Saelens and colleagues26 found that a walkable neighborhood environment (as assessed by residential density, mixed land use, street connectivity, aesthetics, and safety) was associated with higher PA and lower overweight among adults.
Most studies examining correlates of children’s weight status have failed to simultaneously consider the relative impact of multiple levels of EST on Latino children’s weight status. As suggested by EST, the proposed study examines 4 levels of influence: child characteristics (eg, gender) and child risk factors (eg, dietary behavior); parenting and parents’ sociodemographic characteristics; school and community related characteristics; and parents’ BMI. Findings from this study can inform future interventions that target modifiable factors with the greatest promise to change the current upward trend in childhood obesity rates.
METHODS
Aventuras Para Niños (“Adventures for Kids”) was a randomized community trial designed to test an environmentally based intervention to prevent childhood obesity.27 Following baseline assessment, schools were randomly assigned to 1 of 3 intervention conditions or a control condition: micro (family environment), macro (school and community), and micro + macro (family environment, school and community). Data for the present study were collected at baseline using multiple methods: measured data (anthropometric), self-reported, observed and geographically coded data. These data were selected to represent multiple levels of influence consistent with EST,4 as presented in Figure 1.
Figure 1.
Ecological Systems Theory as Applied to the Present Study
Subjects
Elementary schools within 3 school districts in south San Diego County were invited to participate in the study if they (1) had Hispanic enrollment of at least 70%, (2) agreed to be randomized into intervention or control conditions, (3) did not have any other obesity-related programs or special physical education training28 within the past 4 years, and (4) had defined attendance boundaries (as opposed to charter or magnet schools that draw students from a broad region). A total of 13 public elementary schools from the 3 school districts that met these criteria were successfully recruited.
Hispanic children entering kindergarten, first or second grade were eligible to participate in the study if they lived within the school attendance boundaries. Additional eligibility criteria included planning on living in the target area for the next year, parents’ ability to read in English or Spanish, and willingness to be randomized into one of the experimental conditions. If the family had more than one eligible child, the youngest was selected. Children on a medically prescribed restricted diet or with a condition that limited their PA were excluded. Families were ineligible to participate if they anticipated moving out of the San Diego area during the study period. A total of 812 parent-child dyads were enrolled in the study. Following completion of the parent survey and anthropometric measurements, parent-child dyads were given a $20 incentive.
Procedure
Data for the present study were collected at baseline between August 2003 and January 2004 and employed 4 modalities. Measured child and parent weight and height were obtained by trained evaluation assistants (EAs) using portable scales and stadiometers, respectively. Twenty percent of the anthropometric measurements were randomly selected for reliability testing yielding inter-rater reliability estimates between 97% and 99%. To obtain self-report data, a self-administered, 22-page questionnaire (available in English or Spanish) was given to the parents of each eligible child. Bilingual/bicultural EAs were available to assist with the questionnaire. Observed data were collected by trained research assistants. Geographically coded data were collected by a trained GIS master’s level student. Base GIS data was obtained from SanGIS (San Diego Geographic Information Source, an agency of the city and county of San Diego). Data licensed was the South County Landbase, updated quarterly during the period of July 2003–July 2004. Layers included were municipal (city) boundaries, road centerlines (roads, major roads and minor highways, and freeways), parcels, and control monuments. The data dictionary was uploaded to a GPS unit and field visits were made to the areas previously classified as commercial to confirm the accuracy of the list.
Instruments
Body mass index (BMI) was the primary outcome variable. Individual, family/home, school and community level influences on BMI were captured using the following variables consistent with EST: (1) individual: children’s demographic characteristics, history of having been breastfed, and health behaviors (PA and diet); (2) family: parents’ characteristics and parenting styles; (3) school: environmental influences that prompt and support children to eat healthy and engage in PA; (4) community: environmental influences on PA and diet; and (5) parent BMI.
Child and Parent Body Mass Index
Weight was measured to the nearest pound using a Health-o-Meter standard scale with the participant standing without shoes and heavy objects removed from pockets. Height was measured to the nearest 1/4 inch, using a standard portable stadiometer with shoes and head wear removed. Measures were all taken in the clothing worn by the participant on the day of measurement. Participants were asked to remove their jackets for weight measures. These measures were converted into metric equivalents to calculate BMI. BMI was calculated using the Quetelet index (kg/m2). Child BMI percentiles and z-scores were calculated to standardize the data to national samples (adjusted for age and gender) using the Centers for Disease Control and Prevention (CDC) 2000 growth charts. Similar to the child anthropometric data collection procedures, adult weight (lbs) and height (in) were measured and categorized using CDC guidelines.
Child Characteristics and Health Behaviors
Child Food Frequency Questionnaire (Parent Report)
Child diet was assessed using a food frequency questionnaire, with food items identified from focus groups involving the target population.29 With input from an anthropologist and our research team, items that were known to be obesogenic for Latinos were added. Parents were asked to rate how often their child consumed each food item using 4 response categories: (1) never, (2) at least once a month, (3) at least once a week, and (4) every day. Food items were categorized by 3 independent reviewers as to their contribution to obesity risk and a summary score was computed to reflect daily consumption. The foods included: (1) fruits and vegetables, (2) savory snacks, (3) sugar-sweetened beverages, and (4) plain water.
Child PA (Parent Report)
Parents were asked, “in comparison to other children, how active is your child?” Response options ranged from “1 = much less than others” to “5 = much more than others.”
Characteristics
Parents also reported on their child’s gender, ethnicity, place of birth, familial relationship to the child, and breastfeeding history.
Family Characteristics (Parents’ Sociodemographic Characteristics and Parenting Styles)
Encouragement of PA, Participation in PA, Instrumental Support for PA (Parent Report)
Parents were asked how often during a typical week they encouraged their child to participate in PA, participated in PA with child, and provided transportation where the child can be physically active. Response options ranged from 1 to 7 days a week.
Behavioral Strategies to Reduce Fat and Increase Fiber (Parent Report)
This 30-item scale was developed in a previous study30 and based, in part, on Kristal’s work31,32 in dietary behavioral strategies to reduce dietary fat and increase fiber. This scale was developed for Latinos and has demonstrated construct and predictive validity. The scale has been used with Latinos living in California and North Carolina.33 The Cronbach coefficient alpha for the fat subscale (19 items) was α = .73 and for the fiber subscale (11 items) α = .76.
Parenting Styles for Healthy Eating and PA (Parent Report)
This scale assessed parenting styles associated with children’s dietary and activity behaviors. The 26-item scale (14 for diet and 12 for activity) was developed for this project using qualitative and quantitative methods.34 Concurrent validity was established with the child feeding questionnaire35 and predictive validity was established with child BMI.36 Response options ranged from “1 = never” to “5 = always.” A mean score for each subscale was calculated. The alpha coefficient for each subscale ranged from .73–.87.
Frequency of Eating Away From Home (Parent Report)
Parents noted how frequently their families ate at fast food restaurants. Due to the distribution of the responses, responses specific to each setting were dichotomized as less than versus once a week or more.
Parent Characteristics
Sociodemographic Characteristics
Demographic information such as country of formal education, household size, employment status, type of residential dwelling, homeownership, age, history of breastfeeding, education, marital status, income, and dominant language were collected from parents.
Self-Rated Health (Parent Report)
Parents were asked, “compared to other people of your age, would you say your health is. … ” Response options ranged from “5 = excellent” to “1 = poor.”
Parent Acculturation (Parent Report)
Acculturation was measured using the acculturation rating scale for Mexican Americans (ARSMA-II).37 Elements included (1) language familiarity and usage, (2) ethnic pride and identity, (3) ethnic interaction, (4) cultural heritage, and (5) generational proximity. Parents received an acculturation score reflecting greater acculturation to the Anglo culture with a higher/less negative score (α = .72).
Adult PA (Parent Report)
The short version of the self-administered international PA questionnaire (IPAQ) assessed the frequency and duration of walking, moderate intensity, and vigorous intensity PA for occupational purposes, house and yard work, transportation, and leisure during the last 7 days.38 The IPAQ has previously been used with Latinos.38
School Characteristics
School Nutrition Environment (Observed)
A scan of the school environment was conducted on 3 different days by 2 research staff to ascertain the number of visual and verbal prompts for healthy eating. Any verbal prompt by the teacher, cafeteria aid worker, a volunteer or any adult in the lunch area to eat more fruit and/or vegetable was coded. Prompts were recorded during two 5-minute intervals. The average number of verbal prompts from the 3 days of observation was used as an independent variable in the model.
System for Observing Play and Leisure Activity in Youth (Observed)
System for observing play and leisure activity in youth (SOPLAY) is an observational method to determine level of PA among individuals observed within a given target area. PA target areas at the schools were identified and assessed (N = 137; mean per school = 10.5; SD = 2.8). Trained assessors conducted SOPLAY observations before school, during recess, and at lunch time in the 13 elementary schools over an 18-month period and on at least 5 days at each school. During an observation in a target area, each child was coded as sedentary (ie, lying down, sitting, or standing), walking, or engaged in vigorous activity using specialized counters. Activity counts were summarized as the percentage of children engaging in different levels of activity. Assessors also coded area characteristics (eg, accessibility, usability; and presence of supervision, loose equipment, and organized activities). Presence of PA equipment and percent of children involved in sedentary activity were included in the analyses.
Community Characteristics
Perceived Neighborhood Safety/Aesthetics (Parent Report)
A modified version of the US Department of Transportation, Partnership for a Walkable America, Pedestrian and Bicycle Information Center, and the United States Environmental Protection Agency’s Walkability Checklist was used. Six questions assessed perceived neighborhood safety/aesthetics, including the presence of crime, lights, and vehicle exhaust in the neighborhood. The final model included a summarized score assessing perceived neighborhood safety/aesthetics (6 items; α = .60).
Restaurant and Grocery Store Density Within a Mile of Participants’ School (Geo-Coded)
The number of restaurants and grocery stores within a 1-mile radius of the school was included in the analyses.
DATA ANALYSIS
Data were examined for normality and intraclass correlation (ICC) assessed for independence. The ICC for BMI was zero and preliminary models adjusting for school as a random effect showed no influence on the regression coefficients or standard errors of the predictor variables. This suggested no school clustering and appropriate use of multiple linear regression as the analytic approach. Percentages were calculated for categorical data and measures of central tendency for continuous data. Child BMI z scores were used as the outcome variable for the final regression models to adjust for differences by age and gender. Eight hundred and twelve families were recruited and completed baseline assessment; however, only 745 biological mothers were included in the current study, given interest in examining the relationship between biological parent weight and child weight. Because there were few fathers (N = 23), these cases were also deleted. In addition, due to missing data on acculturation (N = 91) and income (N = 48), 44 additional cases were omitted from the analysis. Grocery store and restaurant density was calculated using GIS software (ESRI® ArcMap™ 9.2). Density was defined as the total number of stores or restaurants within a 1-mile radius from each participant’s school address.
A series of hierarchical regression analyses were performed to examine the effects of each theoretically derived correlate on child BMI. To examine the impact that each EST level had on the amount of variance that explained child BMI, the R2 change was evaluated. In the first block, child characteristics were regressed on child BMI. In the second block, child and parenting characteristics were regressed on child BMI. In the third block, child, parenting, and family characteristics were regressed on child BMI. In the fourth block, the aforementioned variables were entered in addition to school characteristics. The fifth block included community characteristics and the sixth and final block included parent BMI.
RESULTS
Child and Parent Sociodemographic Characteristics
Table 1 presents the general demographic, anthropometric and other characteristics of the children and their parents. The mean age of the children was nearly 6 years old and 86% of the children were born in the United States, contrasted to 28% of their parents. Participating families were generally very poor, with fully 35.2% being at or below the 100% federal poverty level of $1,720/month for a family of 4. Three-fourths of the families rented their homes.
Table 1.
Child and Parent Demographics and Anthropometrics (N = 745)
| Child | |
|---|---|
| Mean age (SD) | 5.97 (.943) |
| % Girls | 50.0 |
| % Children born in United States | 86.2 |
| % Body mass index ≤ 85th percentile [N] | |
| Girls | 53.9 [152] |
| Boys | 53.1 [154] |
| % Body mass index ≥ 85th & <95th percentile—At risk of overweight | |
| Girls | 17.0 [48] |
| Boys | 16.9 [49] |
| % Body mass index ≥ 95th percentile—Overweight | |
| Girls | 29.1 [82] |
| Boys | 30.0 [87] |
| Mean activity compared to other children (SD) | 3.01 (0.87) |
| Mean child acculturation (SD) | 1.77 (0.67) |
| Parent | |
| Mean age (SD) | 33.54 (6.59) |
| % Did you breast feed child? | 80.50 |
| % Female | 95.60 |
| % Married or living as married | 71.80 |
| % Poverty in terms of monthly income (<$1,720/family of 4) | 35.30 |
| % Completed high school or less | 67.00 |
| % Country of formal education | |
| Mexico or other country | 62.50 |
| United States | 37.60 |
| % Employed outside the home (vs homemaker) | 3 8 .90 |
| % Born outside of United States | 71.80 |
| If born outside United States, mean years in the United States (SD) | 12.48 (9.96) |
| Median household size (range) | 5.00 (2 –13) |
| % Rent (vs own) | 74.60 |
| % live in a house (vs apartment or condominium) | 42.00 |
| Mean body mass index (SD) | 29.70 (6.67) |
| % Adult BMI categories | |
| Under weight | 1.10 |
| Normal | 23.80 |
| Overweight (not obese) | 33.80 |
| Obese | 41.30 |
| % Self-rated health | |
| Excellent | 11.0 |
| Good to very good | 63.7 |
| Fair to poor | 25.3 |
| Mean acculturation score (SD) | −1.36 (1.13) |
Nearly one half of the children were at risk for being overweight (ie, >85th percentile for their age and gender; see Table 1). The average age of the parent was 34 years, and nearly 70 percent were married or living as married. The mean BMI for the parent was 29.7, with over one third of them being overweight and over 40 percent being obese. Three fourths of the parents reported their health to be in good, very good or excellent condition. In terms of the acculturation measures, parents generally indicated being very Mexican-oriented and only somewhat Anglo-oriented. Descriptive statistics on school and community environment characteristics are provided in Table 2.
Table 2.
Descriptive Statistics on School and Community Environment Characteristics (N = 13)
| School Characteristics | |
|---|---|
| Median number of visual prompts promoting F&V (range) | 2.00 (0 –9) |
| Median number of verbal prompts promoting F&V | 2.00 |
| Percent of sedentary children | 44.04 |
| Percent of children walking | 32.71 |
| Percent of very active children | 23.25 |
| Community Characteristics | |
| Mean perceived walkability of their neighborhood (SD)* | 3.47 (3.27) |
| Mean number of restaurants w/in 1 mile from school (SD) | 43 (23) |
| Mean number of grocery stores w/in 1 mile from school (SD) | 18 (5) |
Maximum score is 18. Lower score denotes greater perceived walkability.
Child Characteristics and Risk Factors
Table 3 presents the regressions on z scores of child BMI. Gender was associated with weight status. (Boys were significantly more overweight compared to girls.) Children who were overweight were significantly less likely to be physically active compared to normal weight children (Adj R2 = .03).
Table 3.
Correlates of z Score Child BMI (N = 606)
| Block 1 (Std beta) |
Block 2 (Std beta) |
Block 3 (Std beta) |
Block 4 (Std beta) |
Block 5 (Std beta) |
Block 6 (Std beta) |
|
|---|---|---|---|---|---|---|
| Child characteristics | ||||||
| Fruits and vegetables per day | −.009 | −.006 | .004 | .013 | .011 | .006 |
| Sweet and savory snacks per day | −.007 | −.005 | −.016 | −.020 | −.022 | −.011 |
| Sugar-sweetened beverages per day | .027 | .050 | .043 | .041 | .041 | .029 |
| Water drinking per day | .024 | .014 | .015 | .014 | .010 | −.006 |
| Child PA compared to other children | −.187*** | −.163*** | −.142** | −.142** | −.139** | −.118** |
| Age of child | −.017 | −.012 | −.020 | −.027 | −.024 | −.047 |
| Child gender† | −.084* | −.076* | −.075* | −.079* | −.083* | −.073* |
| Child breast fed‡ | −.014 | −.014 | −.026 | −.025 | −.028 | −.020 |
| Home characteristics | ||||||
| Parenting | ||||||
| Encouragement for PA | −.038 | −.036 | −.043 | −.040 | −.033 | |
| Participate in PA | .031 | .028 | .039 | .036 | .039 | |
| Instrumental support for PA | −.093* | −.087* | −.082* | −.085* | −.091* | |
| Behavioral strategies for fat | .035 | .066 | .064 | .064 | .071 | |
| Behavioral strategies for fiber | −.041 | −.062 | −.063 | −.052 | −.056 | |
| PS monitoring for diet | .022 | .012 | .014 | .012 | .002 | |
| PS discipline for diet | .046 | .049 | .044 | .049 | .056 | |
| PS control for diet | −.259*** | −.267*** | −.262*** | −.264*** | −.235*** | |
| PS limit for diet | .154** | .158*** | .150** | .147** | .135** | |
| PS reinforcement for diet | −.024 | −.022 | −.019 | −.016 | −.018 | |
| PS monitoring for activity | .055 | .066 | .072 | .074 | .065 | |
| PS discipline for activity | −.044 | −.040 | −.035 | −.039 | −.041 | |
| PS control for activity | .020 | .011 | .017 | .018 | .016 | |
| PS limit for activity | −.100* | −.095* | −.098* | −.101* | −.083* | |
| PS reinforcement for activity | .061 | .060 | .059 | .052 | .063 | |
| Eating out fast food§ | .049 | .060 | .066 | .068 | .041 | |
| Parent characteristics | ||||||
| Employment║ | −.032 | −.042 | −.045 | −.046 | ||
| Years of education¶ | .011 | .016 | .017 | .017 | ||
| Marital status# | −.015 | −.009 | −.013 | −.007 | ||
| Monthly income†† | −.068 | −.076 | −.068 | −.063 | ||
| Household size | .043 | .050 | .054 | .026 | ||
| Self-rated health | .124** | .129*** | .125** | .086* | ||
| Adult acculturation | −.121* | −.077* | −.084* | −.097* | ||
| Adult total per week MVPA | .056 | .053 | .052 | .042 | ||
| School characteristics | ||||||
| Median number of visual prompts promoting F&V | −.056 | −.036 | −.075 | |||
| Median number of verbal prompts promoting F&V | −.035 | −.037 | −.022 | |||
| PA equipment | −.048 | .000 | −.017 | |||
| Percent of sedentary children | −.005 | .015 | −.017 | |||
| Community characteristics | ||||||
| Walkability | .046 | .026 | ||||
| Number of restaurants w/in 1 mile from school | .099 | .048 | ||||
| Number of grocery stores w/in 1 mile from school | −.067 | −.051 | ||||
| Parent BMI | .227*** |
p < .05;
p < .01;
p < .001.
1 = male; 2 = female.
0 = no; 1 = yes.
0 = once/week; 1 = greater than once/week.
0 = employed; 1 = home maker or stay at home.
0 = completed less than high school; 1 = completed high school or more.
0 = otherwise; 1 = married.
0 = less than $1,500; 1 = equal or greater than $1,500.
BMI, body mass index; MVPA, moderate-to-vigorous physical activity; PA, physical activity.
Family Environment (Parenting and Parent Characteristics)
The parents of overweight versus normal weight children provided less instrumental support to engage in activity and set fewer limits on their child’s activities. Similarly, parents of overweight versus normal weight children did not control their child’s diet and yet set more limits on their child’s diet (Adj R2 = .10). Parents who rated their health more positively were more likely to have children who were overweight, as were parents who were less acculturated (Adj R2 = .12).
School and Community Environment
School and community level variables were not significantly correlated with children’s weight (Adj R2 = .12).
Parent BMI
Adjusting for the aforementioned variables, parents’ weight status was positively associated with children’s weight (Adj R2 = .16).
DISCUSSION
The EST was used to examine the influence of individual, family, school, and community level factors on children’s BMI. Specifically, microenvironmental influences more proximal to the child’s health behaviors and his or her daily life were examined, gradually moving toward macroenvironmental or more distal influences of the family and home environment, the school environment, and the community and neighborhood environment. As expected, the contributions of proximal individual and family levels were generally stronger for predicting child’s BMI than the more distal school and community variables. The BMI of the adult caregiver (in almost all cases the child’s biological parent) was one of the strongest of all individual correlates with the child’s BMI.
Family-level variables were significant correlates of child BMI. However, several of the associations between parenting styles and children’s weight status were in the unexpected direction. Our results suggest that parents’ limit setting for dietary intake was positively associated with children’s weight status. Also, parents who reported using few controlling strategies had more children who were overweight. Previous studies have shown that children with controlling parents are less likely to consume healthy foods, and are more likely to consume unhealthy foods34 as well as more food overall than children of parents who do not engage in controlling strategies. One possible explanation for these findings is that the adverse impact of parent controlling strategies on children’s weight status may not be evident until later in the developmental process. Another reason may be that Hispanic parents who have normal weight children as defined by US standards consider their children to be underweight. As Kimbro and colleagues39 point out, Hispanic parents may be more likely to hold the cultural belief that heavier children are healthier which could lead them, in turn, to provide more food and to pressure their children to eat more. Third, as we are neither able to discern causal links nor direction if such a connection does exist, it could be that parents who notice their children getting heavier are more likely to adopt controlling strategies. Prospective studies are needed to establish causal effects.
Consistent with the latter finding, our results suggest that less acculturated (ie, traditionally Mexican) parents were significantly more likely to have children who were overweight. These findings held even after adjusting for parents’ socioeconomic factors. Also, Hispanic parents who rated their health as “good to excellent” had children who were heavier than parents who rated their health as “fair to poor.” Surprisingly, we found no association between parents’ SES and children’s weight status. This is in contrast to past results which showed that parents with lower incomes had children who were heavier due in part to the lack of affordability of healthy foods.40 As with the influence of parenting styles, one explanation for the null findings may be that the effects of parents’ SES on children’s weight becomes manifest in later developmental years.
One of the strongest correlates of children’s BMI was parents’ BMI. The contribution of maternal BMI to the prediction of the child’s BMI could stem from a variety of factors that are difficult to disaggregate. Genetic and prenatal factors may predispose a child to obesity. Also, the parents’ eating patterns would contribute directly to what and how frequently the child ate, as this behavior will not only be imitated by the child, but will result in the structuring of the environment that certain foods would be more or less available. Future research should continue to examine the interactions of Hispanic and other caregivers with their children to determine the individual contributions of their various behaviors (as well perhaps as any genetic predisposition) to the child’s obesity. Such research will contribute greatly to deriving interventions for the early prevention of obesity.
Aspects of the school and larger community were, at best, marginally related to children’s weight status. This weak relationship may be the result of the developmental stage of the children studied. Young children’s behaviors are largely influenced by parental factors and the amount of time these young children spend in the school environment may be limited. It is also the case that measurement techniques are more sensitive to child-parent relationships and other “microenvironmental” indices than they are to the relationship between the “macroenvironment” (eg, school, community structures) and child weight status. Future studies should continue to assess socio-ecological influences at various levels, with special attention to refining and expanding assessments of broader environments.
Limitations and Strengths
Limitations of this study included its cross-sectional design, which precluded the inference of causality. Additionally, because many of the correlates of children’s weight status were collected through self-report, they are subject to self-report biases. Furthermore, the lack of association between participants’ SES and children’s weight status may be due to the lack of variance in SES; this sample was fairly homogenous in SES. The lack of association between community level variables and children’s weight status may have been due to the lack of variability in the community level variables (N = 13 schools). Also, because some of the constructs were assessed with one item measures (eg, PA), measurement of this construct is limited. Further, because we involved a convenience sample of Latinos living in the southwestern region of the United States, the generalizability of our findings is limited. Moreover, the total variance accounted by our measures is small, suggesting that there may be number of other factors that were not assessed that may predict weight status in children.
Strengths of the study included its examination of parenting practices of a large number of Hispanic families living in a border community, a population at substantial risk for obesity and related morbidity. Moreover, we were able to concurrently evaluate the potential impact of individual, family, school, and neighborhood on children’s weight status, informing both future research and prevention efforts. Previous studies have primarily focused on one level of influence.
Conclusion
Children in the present study were still very young, and it is logical that the parents might exert a stronger influence on the child’s eating, activity and physical status compared to school or community environments. Future research should continue to examine these more distal environments. They may especially be relevant not only to children as they mature but also to the parents’ own eating and PA, which in turn may contribute to the child’s BMI.
IMPLICATIONS FOR SCHOOL HEALTH
Schools provide a unique opportunity for preventing and treating child obesity. Children spend a large percent of their time in schools, a setting in which parents and children can receive information about nutrition and PA. Although changes in body weight rarely have been observed in community trials, school-based interventions have been found to contribute to healthful lifestyle choices among children. For example, findings from a school-based randomized controlled trial suggest a significant reduction in the percentage of energy from fat among school age children.41 School-based interventions targeting children’s PA have also shown to be effective (eg, SPARK). Findings from such studies suggest that lifestyle changes among children may be achieved by training and supporting PA instructors and food service staff.
Footnotes
This protocol was approved by the San Diego State University Institutional Review Board to ensure the protection of human participants.
Indicates CHES and Nursing continuing education hours are available. Also available at: http://www.ashaweb.org/continuing_education.html
REFERENCES
- 1.Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology, and demographics. Pediatrics. 1998;101(3):497–504. [PubMed] [Google Scholar]
- 2.MMWR. Obesity Prevalence Among Low-Income, Preschool-Aged Children—United States, 1998–2008. Vol. 58. United States Government Printing Office; 2009. [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 4.Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996;10(4):282–298. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- 5.Davison KK, Birch LL. Childhood overweight: a contextual model and recommendations for future research. Obes Rev. 2001;2:159–171. doi: 10.1046/j.1467-789x.2001.00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Brien M, Nader PR, Houts RM, et al. The ecology of childhood overweight: a 12-year longitudinal analysis. Int J Obes. 2007;31(9):1469–1478. doi: 10.1038/sj.ijo.0803611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gillis LJ, Bar-Or O. Food away from home, sugar-sweetened drink consumption and juvenile obesity. J Am Coll Nutr. 2003;22(6):539–545. doi: 10.1080/07315724.2003.10719333. [DOI] [PubMed] [Google Scholar]
- 8.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet. 2001;357(9255):505–508. doi: 10.1016/S0140-6736(00)04041-1. [DOI] [PubMed] [Google Scholar]
- 9.Costanzo PR, Woody EZ. Domain-specific parenting styles and their impact on the child’s development of particular deviance: the example of obesity proneness. J Soc Clin Psychol. 1985;3(4):425–445. [Google Scholar]
- 10.Stark LJ, Collins FL, Jr, Osnes PG, Stokes TF. Using reinforcement and cueing to increase healthy snack food choices in preschoolers. J Appl Behav Anal. 1986;19(4):367–379. doi: 10.1901/jaba.1986.19-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Faith MS, Berkowitz RI, Stallings VA, Kerns J, Storey M, Stunkard AJ. Parental feeding attitudes and styles and child body mass index: prospective analysis of a gene-environment interaction. Pediatrics. 2004;114(4):e429–e436. doi: 10.1542/peds.2003-1075-L. [DOI] [PubMed] [Google Scholar]
- 12.Sallis J, Prochaska J, Taylor W. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32(5):963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Anderson R, Crespo C, Bartlett S, Cheskin L, Pratt M. Relationship of physical activity and television watching with body weight and level of fatness among children. JAMA. 1998;279(12):938–942. doi: 10.1001/jama.279.12.938. [DOI] [PubMed] [Google Scholar]
- 14.Mei Z, Scanlon K, Grummer-Stawn L, Freedman D, Yip R, Trowbridge F. Increasing prevalence of overweight among US low income preschool children: the Centers for Disease Control and Prevention Pediatric Nutrition Surveillance 1983–1995. Pediatrics. 1998;101(1):103–105. doi: 10.1542/peds.101.1.e12. [DOI] [PubMed] [Google Scholar]
- 15.Kaiser L, Melgar-Quinonez H, Lamp C, Johns M, Harwood J. Acculturation of Mexican-American mothers influences child feeding strategies. J Am Diet Assoc. 2001;101(5):542–547. doi: 10.1016/S0002-8223(01)00136-5. [DOI] [PubMed] [Google Scholar]
- 16.Olvera N, Suminski R, Power T. Intergenerational perceptions of body image in Hispanics: role of BMI, gender, and acculturation. Obes Res. 2005;13:1970–1979. doi: 10.1038/oby.2005.242. [DOI] [PubMed] [Google Scholar]
- 17.Ariza A, Chen E, Binns H, Christoffel K. Risk factors for overweight in five-to six-year old Hispanic-American children: a pilot study. J Urban Health. 2004;81(1):150–161. doi: 10.1093/jurban/jth091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neuhouser ML, Thompson B, Coronado GD, Solomon CC. Higher fat intake and lower fruit and vegetables intakes are associated with greater acculturation among Mexicans living in Washington State. J Am Diet Assoc. 2004;104(1):51–57. doi: 10.1016/j.jada.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 19.Evenson KR, Sarmiento OL, Ayala GX. Acculturation and physical activity among North Carolina Latina immigrants. Soc Sci Med. 2004;59(12):2509–2522. doi: 10.1016/j.socscimed.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 20.Lin B, Huang C, French S. Factors associated with women’s and children’s body mass indices by income status. Int J Obes. 2004;28:536–542. doi: 10.1038/sj.ijo.0802604. [DOI] [PubMed] [Google Scholar]
- 21.Perry C, Bishop DB, Taylor GL, et al. A randomized school trial of environmental strategies to encourage fruit and vegetable consumption among children. Health Educ Behav. 2004;31(1):65–76. doi: 10.1177/1090198103255530. [DOI] [PubMed] [Google Scholar]
- 22.Veugelers P, Fitzgerald A. Prevalence of and risk factors for childhood overweight and obesity. Can Med Assoc J. 2005;173(6):607–613. doi: 10.1503/cmaj.050445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maddock J. The relationship between obesity and the prevalence of fast food restaurants: state-level analysis. Am J Health Promot. 2004;19(2):137. doi: 10.4278/0890-1171-19.2.137. [DOI] [PubMed] [Google Scholar]
- 24.Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: relationships to overweight in low-income preschool children. Prev Med. 2004;38(1):57–63. doi: 10.1016/j.ypmed.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 25.Jeffery RW, Baxter J, McGuire M, Linde J. Are fast food restaurants an environmental risk factor for obesity? Int J Behav Nutr Phys Act. 2006;3:2. doi: 10.1186/1479-5868-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saelens B, Sallis J, Black J, Chen D. Neighborhood-based differences in physical activity: an environment scale evaluation. Am J Public Health. 2003;93(9):1552–1558. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duerksen SC, Campbell NR, Arredondo EM, Ayala GX, Baquero B, Elder JP. Aventuras para niños. Obesity prevention in the homes, schools, and neighborhoods of Mexican American children. In: Brettschneider WD, Naul R, editors. Obesity in Europe. Frankfurt: Peter Lang; 2007. pp. 135–152. [Google Scholar]
- 28.Dowda MC, Sallis JF, McKenzie TL, Rosengard PR, Kohl HW. Evaluating the sustainability of SPARK physical education: a case study of translating research into practice. Res Q Exerc Sport. 2005;76:11–19. doi: 10.1080/02701367.2005.10599257. [DOI] [PubMed] [Google Scholar]
- 29.Zive MM, Frank-Spohrer GC, Sallis JF, et al. Determinants of dietary intake in a sample of White and Mexican-American Children. J Am Diet Assoc. 1998;98(11):1282–1289. doi: 10.1016/S0002-8223(98)00288-0. [DOI] [PubMed] [Google Scholar]
- 30.Ayala GX, Elder JP. Measuring the behaviors: food purchasing, food preparation, and food consumption. Pub Health Ass. 2000 Nov 13; [Google Scholar]
- 31.Kristal A, Shattuck AL, Patterson RE. Differences in fat-related dietary patterns between black, Hispanic and White women: results from the Women’s Health Trial Feasibility Study in Minority Populations. Public Health Nutr. 1999;2(3):253–262. doi: 10.1017/s1368980099000348. [DOI] [PubMed] [Google Scholar]
- 32.Kristal AR, Shattuck AL, Henry HJ. Patterns of dietary behavior associated with selecting diets low in fat: reliability and validity of a behavioral approach to dietary assessment. J Am Diet Assoc. 1990;90(2):214–220. [PubMed] [Google Scholar]
- 33.Elder JP, Ayala GX, Slymen DJ, Arredondo EM, Campbell NR. Evaluating psychosocial and behavioral mechanisms of change in a tailored communication intervention. Health Educ Behav. 2009;36(2):366. doi: 10.1177/1090198107308373. [DOI] [PubMed] [Google Scholar]
- 34.Arredondo EM, Elder JP, Ayala GX, Campbell N, Baquero B, Duerksen S. Is parenting style related to children’s healthy eating and physical activity in Latino families? Health Educ Res. 2006;21(6):862. doi: 10.1093/her/cyl110. [DOI] [PubMed] [Google Scholar]
- 35.Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the Child Feeding Questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36(3):201–210. doi: 10.1006/appe.2001.0398. [DOI] [PubMed] [Google Scholar]
- 36.Larios S, Ayala GX, Arredondo EM, Baquero B, Elder JP. Development and validation of a scale to measure Latino parenting strategies related to children’s obesigenic behaviors: the Parenting strategies for Eating and Activity Scale (PEAS) Appetite. 2009;52(1):166–172. doi: 10.1016/j.appet.2008.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cuellar I, Arnold B, Maldonado R. Acculturation rating scale for Mexican Americans-II: a revision of the original ARSMA scale. Hisp J Behav Sci. 1995;(17):275–304. [Google Scholar]
- 38.Craig CL, Marshall AL, Sastram M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 39.Kimbro RT, Brooks-Gunn J, McLanahan S. Racial and ethnic differentials in overweight and obesity among 3-year-old children. Am J Public Health. 2007;97(2):298–305. doi: 10.2105/AJPH.2005.080812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 41.Caballero B, Clay T, Davis SM, et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78(5):1030–1038. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]