Abstract
OBJECTIVES
Diabetes may raise dementia risk. However, the pattern of cognitive change over time in non-demented older adults with diabetes, including the onset of cognitive decline, is unclear. We examined the association of diabetes and cognitive functioning at baseline and cognitive change over time in a large, ethnically diverse sample of older adults.
DESIGN
Prospective cohort study.
SETTING
Washington Heights-Inwood Columbia Aging Project (WHICAP), a community-based, prospective study of risk factors for dementia.
PARTICIPANTS
1,493 met both inclusion and exclusion criteria for this study.
MEASUREMENTS
Participants underwent baseline and follow-up cognitive and health assessments approximately every 18 months. Generalized estimating equations were used to examine the longitudinal association between diabetes and cognition.
RESULTS
Diabetes was associated with poorer baseline cognitive performance in memory, language, processing speed/executive functioning, and visuospatial abilities. After adjusting for age, education, sex, race/ethnicity, and apolipoprotein-ε4, participants with diabetes performed significantly worse at baseline relative to those without diabetes in language and visuospatial abilities. There were no differences between those with and without diabetes in terms of rate of cognitive change over a mean follow-up time of six years.
CONCLUSION
The rate of cognitive change in elderly persons with and without diabetes is similar, although cognitive performance is lower in persons with diabetes. Our findings suggest that cognitive changes may occur early during the diabetes process and highlight the need for studies to follow participants beginning at least in midlife, prior to the typical later-life onset of dementia.
Keywords: Diabetes, cognition, aging, vascular risk factors
INTRODUCTION
Approximately 27% of adults aged 65 years or older in the United States are estimated to have type-2 diabetes. If pre-diabetes is also considered, the estimated prevalence rate increases to 50%1. It seems clear that diabetes is associated with a higher risk of clinical dementia including vascular dementia and Alzheimer’s disease (AD)2–4, but the mechanisms remain unclear. Diabetes is related to a higher risk of cerebral infarcts5,6, but evidence for its association with AD neuropathology (i.e., amyloid plaques and neurofibrillary tangles [NFT]) is conflicting 5–9. It remains unclear whether diabetes increases risk for AD neuropathology or solely lowers the threshold to manifest dementia through cerebrovascular disease2,10.
There is growing interest in the role of vascular risk factors such as diabetes in cognitive decline short of dementia. Several cross-sectional studies have reported that older adults with diabetes show decrements across a variety of cognitive domains including memory, language, processing speed, executive functioning, and visuospatial abilities11–17. Less is known about how these cognitive changes evolve over time. Results from longitudinal studies have been mixed with some studies showing that cognitive decline among older adults with diabetes exceeds the effects of normal aging18–22 whereas other studies have not found evidence of accelerated cognitive decline in diabetes23–25. Notably, many of these longitudinal studies have used very limited testing and included global cognitive screening measures18,21,22, which have been criticized for poor sensitivity26,27.
We addressed the question of how diabetes affects cognitive trajectories by examining the cross sectional and longitudinal association of diabetes with cognition in an ethnically diverse, well-characterized sample with comprehensive neuropsychological data. Given that previous studies suggest that diabetes is associated with increased risk of mild cognitive impairment28 and dementia4, we hypothesized that diabetes is associated with steeper decline in performance in all cognitive domains.
METHODS
Participants
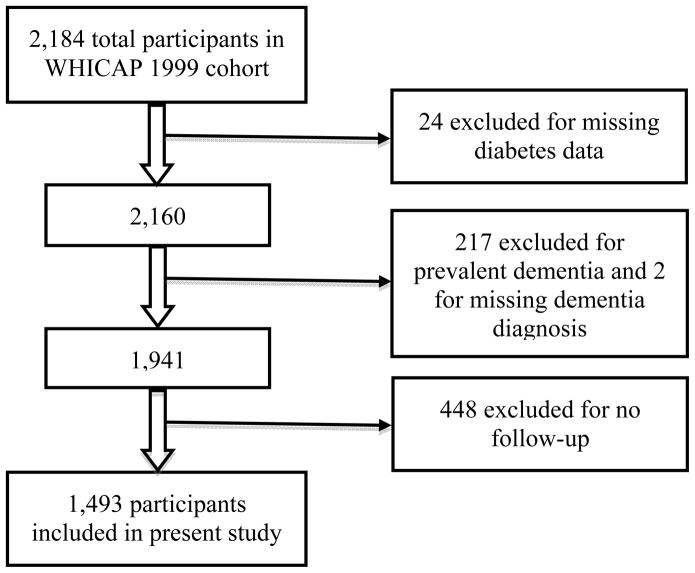
Participants for these analyses were from the Washington Heights-Inwood Columbia Aging Project (WHICAP) cohort recruited between 1999 and 2001. WHICAP is a community-based, prospective study designed to identify dementia predictors. A sample of non-demented Medicare recipients aged 65 years or older from three contiguous ZIP codes in northern New York City were invited to participate29–31. Briefly, invitations were mailed to 7,120 individuals from households with known telephone numbers. Among these, 265 (3.7%) had died, 1,541 (21.6%) no longer lived in the area, 662 (9.3%) were ineligible, and 2,810 (39.5%) refused participation. Individuals who reported a dementia diagnosis were excluded. The sample recruited included 2,184 individuals, with a recruitment rate among eligible individuals of approximately 40%. Among these 2,184 participants, we excluded those with missing diabetes information (n = 24), prevalent dementia (n = 217 including 159 individuals [73.3%] without diabetes and 58 individuals [26.7%] with diabetes) or missing dementia diagnosis information (n = 2), and no follow-up (n = 448). Reasons for no follow-up included refusal (n=136, 30.4%), unable to contact (n=104, 23.2%), death (n=97, 21.7%), move (n=43, 9.6%), and unable to schedule (n=68, 15.2%). The final analytic sample comprised 1,493 participants (Figure 1). This study was approved by the New York Psychiatric Institute Institutional Review Board. All participants provided written informed consent.
Figure 1.
Flow chart showing participant selection process
Assessment Procedures
Participants underwent baseline and follow-up interviews including medical and psychiatric history; physical examination; phlebotomy; and comprehensive neuropsychological assessments32. Follow-up interviews occurred approximately every 18 months. The mean follow-up time across the entire sample was 6.05 years (standard deviation=3.02; range=1.14–12.09). Follow-up data up to 2012 were included in these analyses.
Diabetes and Demographic and Vascular Risk Covariates
Demographic variables including age, education, and race/ethnicity using the format of the 1990 census were determined by self-report. Diabetes was identified by self-report or by use of diabetes medications at baseline or during follow-up. History of stroke, hypertension, and smoking, were determined by self-report or clinical history. Plasma total cholesterol level was obtained using standard enzymatic techniques. High density lipoprotein (HDL) cholesterol was determined after precipitation of apolipoprotein B-containing lipoproteins with phosphotungstic acid33. Non-HDL cholesterol was calculated as the difference between total cholesterol and HDL. High-sensitivity C-reactive protein (CRP) level was measured using an ultra-sensitive enzyme-linked immunosorbent assay. Apolipoprotein E (APOE) genotyping was obtained using a polymerase chain reaction based method. Participants were classified as APOE-ε4 carriers if they had at least one ε4 allele.
Neuropsychological Assessment
The neuropsychological battery was designed to assess a broad range of cognitive abilities including memory, language, processing speed/executive functioning, and visuospatial abilities32. Specific tests included for each domain were: memory (Selective Reminding Test [SRT] total recall, delayed recall, and delayed recognition), language (modified 15-item Boston Naming Test total score, Letter Fluency total, Category Fluency total, Similarities subtest of the Wechsler Adult Intelligence Scale – Revised, Boston Diagnostic Aphasia Evaluation Repetition and Comprehension subtests), processing speed/executive functioning (Color Trails 1 and 2), and visuospatial abilities (Benton Visual Retention Test [BVRT] recognition and matching tests, Rosen Drawing Test, Identities and Oddities subtest of the Mattis Dementia Rating Scale). Table 2 presents possible ranges and descriptive statistics (means and standard deviations for those with and without diabetes separately) as well as results from linear regression examining the association between diabetes and cognitive performance for these individual measures. Participants were tested in either English or Spanish depending on their preferred language.
Table 2.
Descriptive statistics and linear regression results for association between diabetes and performance on individual neuropsychological measures at baseline and final follow-up
| Baseline | Follow-up | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Possible Range | Non-diabetes mean (± SD) |
Diabetes mean (± SD) |
B | SE | Cohen’s d | p | Non-diabetes mean (± SD) |
Diabetes mean (± SD) |
B | SE | Cohen’s d | p |
| N | 1115 | 378 | 1115 | 378 | |||||||||
| Memory | |||||||||||||
| SRT-total recall | 0–72 | 38.24 (±10.45) | 36.87 (±9.83) | −1.36 | 0.62 | 0.13 | .028 | 34.28 (±11.55) | 32.87 (±11.27) | −1.42 | 0.76 | 0.12 | .061 |
| SRT-delayed recall | 0–12 | 5.56 (±2.63) | 5.38 (±2.42) | −0.17 | 0.16 | 0.07 | .275 | 4.46 (±2.89) | 4.25 (±2.62) | −.023 | 0.19 | 0.07 | .255 |
| SRT-delayed recognition | 0–12 | 11.14 (±1.44) | 11.06 (±1.37) | −0.07 | 0.09 | 0.06 | .390 | 10.16 (±2.37) | 10.17 (±2.11) | <.001 | 0.15 | 0.01 | .998 |
| Language | |||||||||||||
| Naming total | 0–15 | 13.66 (±1.73) | 13.37 (±1.78) | −0.29 | 0.11 | 0.17 | .007 | 13.47 (±1.94) | 13.39 (±1.98) | −0.09 | 0.13 | 0.04 | .504 |
| Letter fluency mean (# of words) | 0+* | 10.07 (±4.42) | 8.66 (±4.02) | −1.41 | 0.26 | 0.33 | <.001 | 9.77 (±6.13) | 8.67 (±6.19) | −1.11 | 0.41 | 0.18 | .007 |
| Category fluency mean (# of words) | 0+* | 14.78 (±4.29) | 13.77 (±4.05) | −1.01 | 0.26 | 0.24 | <.001 | 13.03 (±4.43) | 12.25 (±4.10) | −0.77 | 0.29 | 0.18 | .007 |
| Similarities | 0–28 | 11.98 (±7.32) | 9.53 (±7.08) | −2.48 | 0.43 | 0.34 | <.001 | 11.81 (±7.63) | 9.58 (±7.18) | −2.25 | 0.49 | 0.30 | <.001 |
| Repetition | 0–8 | 7.68 (±0.69) | 7.59 (±0.76) | −0.09 | 0.04 | 0.13 | .031 | 7.37 (±1.11) | 7.33 (±1.11) | −0.04 | 0.07 | 0.04 | .560 |
| Comprehension | 0–6 | 5.28 (±1.07) | 5.07 (±1.20) | −0.21 | 0.07 | 0.19 | .002 | 5.05 (±1.25) | 4.75 (±1.39) | −0.30 | 0.09 | 0.23 | <.001 |
| Visual-spatial | |||||||||||||
| BVRT recognition | 0–10 | 7.04 (±2.17) | 6.60 (±2.23) | −0.45 | 0.13 | 0.20 | .001 | 6.80 (±2.26) | 6.29 (±2.31) | −0.52 | 0.16 | 0.22 | .001 |
| BVRT matching | 0–10 | 8.69 (±1.81) | 8.35 (±1.99) | −0.35 | 0.11 | 0.18 | .002 | 8.51 (±1.84) | 8.04 (±1.99) | −0.47 | 0.13 | 0.25 | <.001 |
| Rosen | 0–5 | 2.66 (±0.95) | 2.38 (±1.09) | −0.27 | 0.06 | 0.28 | <.001 | 2.41 (±1.11) | 2.25 (±1.15) | −0.16 | 0.08 | 0.14 | .032 |
| Identities/Oddities | 0–16 | 14.52 (±1.75) | 14.15 (±1.91) | −0.38 | 0.11 | 0.21 | .001 | 14.54 (±1.83) | 14.23 (±2.00) | −0.30 | 0.13 | 0.17 | .020 |
| Processing speed | |||||||||||||
| CTT 1 (seconds) | <360┼ | 94.60 (±46.85) | 105.38 (±52.94) | 10.67 | 3.57 | 0.22 | .003 | 108.85 (±62.54) | 123.17 (±67.10) | 14.30 | 4.69 | 0.22 | .002 |
| CTT 2 (seconds) | <360┼ | 158.18 (±52.00) | 169.19 (±54.82) | 10.87 | 4.04 | 0.21 | .007 | 182.85 (±73.94) | 209.17 (±80.19) | 26.21 | 6.03 | 0.35 | <.001 |
SRT = Selective Reminding Test; BVRT = Benton Visual Retention Test
B, standard error, and p values are from linear regressions with diabetes as the predictor variable and cognitive score as the dependent variable. B (unstandardized coefficient) is equal to the difference in mean scores between those with and without diabetes. Cohen’s d of 0.2, 0.5, and 0.8 are considered small, moderate, and large effect sizes, respectively35. Hierarchical linear regression models demonstrated that, after adjusting for age and education, diabetes was associated with significantly poorer baseline performance on measures of language (Letter Fluency: B ± SE = −.89 ± .22, p < .001; Category Fluency: B ± SE = −.61± .22, p = .007; Similarities: B ± SE = −1.26 ± .33, p < .001) and visuospatial abilities (Rosen: B ± SE = −.19 ± .06, p = .001; Identities/Oddities: B ± SE = −.22 ± .10, p = .029) with trends toward poorer performance on executive functioning/processing speed (Color Trails 1: B ± SE = 5.74 ± 3.12, p = .066; Color Trails 2: B ± SE = 6.34 ± 3.57, p = .076). After adjusting for age and education, diabetes was associated with poorer follow-up performance on measures of language (Similarities: B ± SE = −1.02 ± .39, p = .009) and executive functioning/processing speed (Color Trails 1: B ± SE = 9.30 ± 4.41, p = .035; Color Trails 2: B ± SE = 20.55 ± 5.69, p < .001) with trends toward poorer performance on additional measures of language (Category Fluency mean: B ± SE = −.44 ± .26, p = .082; Comprehension: B ± SE = −.15 ± .08, p = .052); and visuospatial abilities (Benton Matching: B ± SE = −.20 ± .12, p = .089).
Participants are asked to generate as many words as they can that begin with each letter or category (e.g., animals) in 60 seconds (within specific guidelines). Mean number of correct words named across the three letters or categories are displayed.
The Color Trails test (CTT) requires participants to connect numbers (CTT 1) or numbers alternating in the same color (CTT 2) in the correct order as quickly as possible. Higher scores indicate slower speeds (i.e., worse performance).
For this study we examined a composite score developed for the WHICAP sample constructed for each cognitive domain using factor analysis34. Methods used to create the composite scores used in the current study have been previously described34. Briefly, to identify the underlying factor structure, exploratory factor analysis (EFA) using principal axis factoring and oblique rotation was conducted on the 15 cognitive measures in the English speaking sample only. The number of factors to retain was determined by several methods including visual inspection of the scree plot, adherence to the Kaiser eigenvalue >1 rule, and inspection of the factor solution to ensure that the factors were interpretable and consistent with prior research in different samples. Four factors were derived from the EFA: memory, language, processing speed, and visuospatial ability. The model from the EFA was then converted to a confirmatory factor analysis (CFA) in which each variable loaded only on the factor with the highest loading. CFA demonstrated that the four-factor model fit the data well in the English and Spanish samples and across the entire sample. The fit of three- and five-factor models across the English speakers, Spanish speakers, and entire sample demonstrated the four-factor model was the best-fitting model within each sample. For all factor scores, a higher score reflects better performance.
Invariance analyses are statistical tools that allow researchers to assess whether variables of interest represent the same theoretical constructs across groups. The establishment of measurement invariance indicates that test scores measure the same psychological constructs across diverse groups. It is crucial to establish equivalence of neuropsychological constructs used to characterize cognitive decline and dementia across diverse cultural and linguistic groups. A previously published report applying invariance analyses to the WHICAP sample indicated that scores on the neuropsychological tests are assessing similar constructs across English and Spanish speakers34.
Statistical Analyses
We conducted 3 types of analyses. First, we conducted bivariate analyses comparing baseline participant characteristics between those with and without diabetes. Second, we compared the baseline scores and follow-up scores on individual cognitive measures that comprised the composite cognitive scores between participants with and without diabetes. Third, we related diabetes status to changes in the composite z scores during follow-up using repeated measures analyses.
For the bivariate analyses, analysis of variance (ANOVA) for continuous variables, χ2 tests for categorical variables, and a Mann-Whitney U test for CRP were performed to compare participants with and without diabetes in terms of demographic, vascular risk, and cognitive variables. Tukey’s post-hoc tests were conducted for comparison of the participants with and without diabetes in terms of racial/ethnic group.
For the analyses relating diabetes status to the individual components of the composite cognitive scores, we used linear regression to estimate the difference between the means for participants with and without diabetes. We also calculated Cohen’s d in order to provide an estimate of effect size35. Cohen’s d of 0.2, 0.5, and 0.8 are considered small, moderate, and large effect sizes, respectively35.
For the repeated measures analyses relating diabetes status to changes in the composite cognitive scores generalized estimating equations36 (GEE) were used to model the relationship over time of participant group (with versus without diabetes) and cognitive performance. GEE is a statistical method that allows the examination of repeated correlated data across individuals, in this case, repeated cognitive scores. This type of analysis is different from that in which there is a single outcome measure per individual (e.g., when examining mortality or dementia onset). Our data had multiple repeated cognitive outcome measures per individual that are not independent of each other, and GEE takes this into account. The variables of interest from a GEE model output include time (years from baseline), group (with versus without diabetes) and the time x group interaction. A significant group effect indicates a difference between the groups at the baseline evaluation, with a negative regression coefficient indicating that those with diabetes had poorer cognitive performance than those without diabetes. A significant time effect indicates a change of test scores over time, with a negative regression coefficient indicating worsening scores over time regardless of diabetes status. A significant group × time regression coefficient indicates that the change in scores over time is different for the two groups. A negative regression coefficient indicates that individuals with diabetes had a relative decline compared with those without diabetes.
We performed GEE analyses using three sets of models: 1) unadjusted model with no covariates; 2) adjusted model with demographic and genetic variables that are risk factors for cognitive decline in the WHICAP cohort including age at baseline, years of education, sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic), and APOE-ε4 genotype as covariates; and 3) adjusted model with the risk factors for cognitive decline from the second model and vascular risk factors that co-occur with diabetes and predict cognitive impairment37,38 as covariates. These vascular risk factors included stroke, hypertension, HDL and non-HDL cholesterol levels, CRP, and current smoking, all predictors of cognitive impairment in our sample37–39. Because these vascular factors may share the causal pathway between diabetes and cognitive impairment, attenuation of associations after the addition of these covariates should be interpreted as evidence of mediation, not confounding. This third model was run in order to examine whether the association of diabetes with cognitive impairment was independent of vascular mechanisms. Significance levels of 0.05 were used for all tests. All analyses were performed using SPSS (version 19).
RESULTS
We excluded 691 participants from the analytic sample due to missing diabetes information, prevalent dementia, or no follow-up. Compared to participants in the analytic sample, those excluded were older at baseline (mean age of 78.95 ± 7.85 versus 76.04 ± 6.46 years); less educated (8.89 ± 4.81 versus 10.88 ± 4.76 years of education); were more likely to be Black, Hispanic, and APOE-ε4 carriers; and had lower memory, language, processing speed/executive functioning, and visuospatial composite scores. There was no difference between the sample participants and those who attended the baseline exam but were excluded from the present study in terms of prevalence of diabetes (Supplemental Table S1).
Compared to those without diabetes, individuals with diabetes were younger; less educated; less likely to be white and APOE-ε4 carriers; and more likely to have hypertension, stroke, higher CRP levels, and lower HDL and non-HDL cholesterol levels (Table 1). Participants with diabetes had significantly lower composite scores of language, processing speed/executive functioning, and visuospatial abilities at baseline relative to those without diabetes. Participants with diabetes also had lower composite memory scores at baseline compared to those without diabetes but this difference was not statistically significant (p = 0.10). There was no difference between those with and without diabetes in terms of length of follow-up.
Table 1.
Baseline participant characteristics by diabetes status
| Non-diabetes mean (± SD) |
Diabetes mean (± SD) |
F, χ2, or U | p╬ | |
|---|---|---|---|---|
| N | 1115 | 378 | ||
| Age (years) | 76.3 (± 6.7) | 75.4 (± 5.8) | 5.01 | 0.03 |
| Education (years) | 11.2 (± 4.7) | 9.9 (± 4.8) | 21.88 | <0.001 |
| Sex (% women) | 67.5 | 66.6 | 0.10 | 0.76 |
| Ethnic group (%) | <0.0001 | |||
| Non-Hispanic white | 36.4 | 22.2 | ||
| Non-Hispanic black | 31.4 | 34.4 | 13.93 | <0.001 (vs. white) |
| Hispanic | 31.0 | 39.9 | 23.84 | <0.001 (vs. white) |
| Other | 1.2 | 3.4 | 17.46 | <0.001 (vs. white) |
| APOE genotype (% ε4 carrier) | 27.4 | 20.7 | 5.61 | 0.02 |
| Current smoker (%) | 10.5 | 10.1 | 0.04 | 0.84 |
| Hypertension history (%) | 73.7 | 85.2 | 14.60 | <0.001 |
| Stroke history (%) | 13.7 | 21.3 | 8.73 | 0.003 |
| CRP, median (interquartile) mg/L† | 5.0 (2.7–13.4) | 7.4 (3.8–19.3) | U=88973.00 Z=−3.19 |
<0.001 |
| HDL* | 49.5 (± 14.9) | 45.0 (± 13.1) | 19.80 | <0.001 |
| Non-HDL cholesterol* | 152.1(± 36.8) | 146.6 (± 37.4) | 4.54 | 0.03 |
| Baseline memory Z score | 0.31 (± 0.71) | 0.24 (± 0.65) | 2.67 | 0.10 |
| Baseline language Z score | 0.36 (± 0.62) | 0.15 (± 0.61) | 32.33 | <0.001 |
| Baseline speed/executive function Z score | 0.43 (± 0.79) | 0.22 (± 0.89) | 11.69 | 0.001 |
| Baseline visuospatial Z score | 0.36 (± 0.56) | 0.19 (± 0.62) | 24.61 | <0.001 |
| Follow-up time (years) | 6.05 (± 3.02) | 6.05 (± 3.06) | <.0001 | 0.99 |
SD = standard deviation; APOE = apolipoprotein E; CRP = C-reactive protein; HDL = high-density lipoprotein
Based on 1135 participants. 358 participants were excluded from the analysis due to missing data on lipids information.
Based on 1060 participants. 433 participants were excluded from the analysis due to missing CRP data.
P-values from Chi-squared test for categorical variables, from Mann-Whitney U test for CRP, and from analysis of variance (ANOVA) for all other continuous variables.
When the 15 individual cognitive measures included in the composite scores were examined separately with linear regression, diabetes was associated with significantly poorer baseline performance on 13 of the 15 measures including measures of memory, language, processing speed/executive functioning, and visuospatial abilities (Table 2). At each participant’s final follow-up (a mean of approximately 6 years after baseline), diabetes was associated with significantly poorer performance on 10 of the 15 cognitive measures including measures of language, processing speed/executive functioning, and visuospatial abilities. In general, the magnitude of differences in mean scores between those with and without diabetes at baseline and follow-up was generally small (Cohen’s d values, which are an effect size measure indicating the difference in means in standard deviation units, ranged from .01 to .35).
Unadjusted GEE models demonstrated that participants with diabetes performed significantly worse at baseline relative to those without diabetes in memory, language abilities, processing speed/executive functioning, and visuospatial abilities (Table 3). After adjusting for risk factors for cognitive decline including age at baseline, years of education, sex, race/ethnicity, and APOE-ε4 genotype (Model 2), participants with diabetes performed significantly worse at baseline relative to those without diabetes in terms of language and visuospatial abilities with a trend toward poorer performance on processing speed/executive functioning. After adjusting for additional vascular risk factors (stroke, hypertension, HDL and non-HDL cholesterol levels, CRP level, and smoking), results remained qualitatively and statistically similar to Model 2, which adjusted for demographic and genetic risk factors.
Table 3.
GEE models of cognitive performance at baseline and over time as a function of diabetes status
| Memory | Language | Processing speed/executive functioning | Visuospatial | |||||
|---|---|---|---|---|---|---|---|---|
| Model 1: Unadjusted | B | p | B | p | B | p | B | p |
| Diabetes (Yes vs. No) | −0.094 | 0.031 | −0.205 | <0.001 | −0.170 | 0.003 | −0.165 | <0.001 |
| Time (year) | −0.022 | <0.001 | −0.001 | 0.738 | −0.032 | <.001 | 0.001 | 0.830 |
| Diabetes X Time | 0.004 | 0.634 | 0.006 | 0.386 | −0.023 | 0.095 | 0.002 | 0.741 |
| Model 2: Adjusted for age, education, sex, ethnicity, and APOE genotype | B | p | B | p | B | p | B | p |
| Diabetes (Yes vs. No) | −0.020 | 0.603 | −0.090 | 0.004 | −0.087 | 0.102 | −0.080 | 0.004 |
| Time (year) | 0.002 | 0.626 | 0.008 | 0.015 | −0.021 | 0.001 | 0.006 | 0.056 |
| Diabetes X Time | 0.010 | 0.217 | 0.010 | 0.098 | −0.011 | 0.383 | 0.008 | 0.164 |
| Model 3: Adjusted for age, education, sex, ethnicity, APOE genotype, and vascular risk factors* | B | p | B | p | B | p | B | p |
| Diabetes (Yes vs. No) | −0.052 | 0.276 | −0.077 | 0.046 | −0.130 | 0.052 | −0.084 | 0.015 |
| Time (year) | 0.002 | 0.657 | 0.008 | 0.037 | −0.022 | 0.006 | 0.005 | 0.171 |
| Diabetes X Time | 0.015 | 0.129 | 0.013 | 0.079 | −0.008 | 0.617 | 0.009 | 0.177 |
All predictors were simultaneously included in each GEE model.
APOE = apolipoprotein E
Model adjusted for age, education, sex, ethnicity, APOE genotype (APOE ε4 carrier versus noncarriers), vascular risk factors (history of stroke, hypertension, high density lipoprotein [HDL] and non-HDL cholesterol levels, and smoking) and C-reactive protein level
Across the entire sample of participants with and without diabetes, there was significant decline in memory and processing speed/executive functioning over time using unadjusted models. Both adjusted models showed decline in processing speed/executive functioning but improvement in language abilities over time. See Table 3.
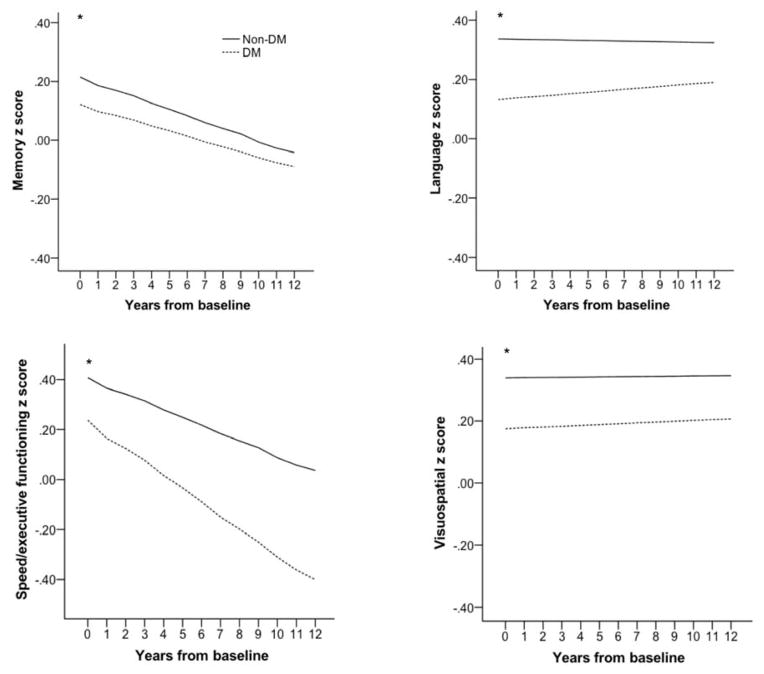
When the interaction between time and diabetes status was assessed, there was no significant difference between participants with and without diabetes in terms of rate of change in any of the cognitive abilities assessed as indicated by a non-significant interaction term for diabetes and time across all models (Table 3). However, although the rates (slopes) of change in memory, language, speed/executive functioning, and visuospatial abilities were similar for persons with and without diabetes, persons with diabetes performed consistently worse over time such that the slope of performance for persons with diabetes was similar in rate but lower in performance than for those without diabetes (Figure 2, Table 3).
Figure 2.
Regression (GEE predicted z scores from adjusted models) of change in performance in memory, language, processing speed/executive functioning, and visuospatial abilities by diabetes mellitus status from unadjusted models.
* Older adults with diabetes performed significantly more poorly at baseline relative to those without diabetes (p < .05).
We conducted secondary GEE analyses among those without incident dementia examining the association of diabetes with cognitive change to ensure that the results were not biased by the inability of persons with dementia to undergo proper neuropsychological testing. These analyses showed results similar to those described above (Supplementary Table S2).
DISCUSSION
Diabetes was associated with worse baseline cognitive performance on all cognitive domains including memory, language, processing speed/executive functioning, and visuospatial abilities. In general, the sizes of the differences were small. After adjusting for demographic variables and APOE-ε4 genotype, diabetes was significantly associated with worse baseline language and visuospatial performance, and an association with poorer processing speed/executive functioning that was close to statistical significance. After adjusting for vascular predictors of cognitive impairment, findings remaining qualitatively and statistically similar, suggesting that results were not mediated by vascular disease. However, diabetes was not associated with rate of change in any cognitive domain. These findings are contrary to our hypothesis that diabetes is associated with steeper cognitive decline. Potential explanations for the finding of poorer performance but equal rates of change include that separation of slopes occurred earlier in life (e.g., during middle age), that diabetes causes an insult or a state that causes lower cognitive performance without accelerated decline, that a third factor related to diabetes such as lower cognitive reserve explains this finding, or that diabetes and cognitive decline are somehow co-occurring but are not causally related.
Our findings are consistent with evidence from previous studies of older adults showing that diabetes is associated with worse cognitive performance but not accelerated cognitive decline23–25,40. Studies in middle-aged adults diagnosed with diabetes suggest that cognitive decrements likely begin during the pre-diabetic stages and progress slowly17,25,41,42. Neuroimaging studies show that diabetes is associated with lower brain volumes but not brain atrophy43, paralleling the findings for cognitive performance. Although several studies suggest that the cognitive trajectories of most older adults with diabetes do not substantially differ from those seen in normal aging 44, other studies have shown accelerated cognitive aging in diabetes 18–22.
Diabetes is associated with higher dementia risk3,4, but the underlying mechanisms remain uncertain. Diabetes increases the risk of cerebral infarcts5,6, but its association with AD neuropathology is less clear and studies are conflicting6–9,5. Evidence from autopsy studies suggests that vascular and AD pathologies may have an additive effect on cognitive impairment 10,45 raising the possibility that those with diabetes who may be at risk for vascular pathologies require less AD pathology to reach a threshold where cognitive impairment manifests itself clinically. It is possible that diabetes may lead to lower resilience to AD pathology due to increased cerebrovascular burden, increasing the risk of clinical diagnosis of AD or other dementia. In addition, individuals with diabetes have lower educational attainment that may be related to lower cognitive reserve46 that may further decrease resilience to AD pathology in addition to cerebrovascular disease. Our results suggest that the association of diabetes with cognitive performance is at least partially independent of cerebrovascular factors, and this association could be accounted for by less cognitive reserve, neurodegenerative mechanisms, or other unknown mechanisms.
The onset of cognitive changes related to diabetes is not clear. One view proposes that there are two crucial periods of life during which diabetes-related cognitive decrements occur: early in life during brain development and later in life when age-related neurodegenerative changes occur, often at age 65 or older47. However, middle age may also be a critical time point, when the prevalence of diabetes and prediabetes increases. It is possible that our elderly sample did not provide the opportunity to detect the point when the separation of slopes of change in cognitive performance between persons with and without diabetes occurred, and that the study of younger cohorts is necessary for this purpose.
The finding that slopes of cognitive change are similar in persons with and without diabetes is not inconsistent with previous findings of increased incident MCI48 and dementia4,31,37. Although we show that the slopes of cognitive decline are similar for persons with and without diabetes, cognitive performance is consistently lower for persons with diabetes, explaining how persons with diabetes reach thresholds for MCI and dementia diagnoses sooner than persons without diabetes. Our current finding that diabetes is related to lower performance in all cognitive domains is also consistent with our previous findings relating diabetes to both amnestic and non-amnestic cognitive syndromes, including amnestic and non-amnestic MCI,48 and Alzheimer’s and vascular dementia4,31,37.
The primary strengths of the present study include the detailed longitudinal cognitive assessment and the large, ethnically diverse sample. The latter is particularly important in light of evidence that prevalence of cognitive impairment and dementia attributable to diabetes is higher in blacks and Hispanics than in whites49. However, the present study has limitations that include ascertainment of diabetes and other vascular risk factors (e.g., hypertension) by self-report and/or medication use. As a result, we may not have captured individuals with undiagnosed pre-diabetes, diabetes or hypertension, which may underestimate the effects of these conditions on cognition. In addition, we cannot rule out practice effects, regression to the mean, or unmeasured or residual confounding that may have influenced the observed pattern of results. Given that individuals with diabetes had significantly less education relative to those without diabetes, it is possible that they had less experience with test-taking and strategies for maximizing test performance. These individuals may have the most to gain from practicing the cognitive tests50. However, notably, a recent study demonstrated that retest effects do not differ by vascular risk burden in the WHICAP sample50. Also, there is potential selection bias due to attrition related to diabetes morbidity and mortality. Furthermore, we did not assess the course or severity of diabetes and did not examine diabetes treatment or complications.
Findings from the present study and previous studies suggest that cognitive changes occur relatively early during the diabetes process. As the global prevalence of diabetes continues to increase, the number of dementia cases attributable to diabetes is also expected to increase. Given that interventions that treat or prevent diabetes could serve as potential interventions to prevent or postpone the development of cognitive decline and dementia, a better understanding of the evolution of cognitive changes associated with diabetes is necessary.
CONCLUSION
In the present study diabetes was associated with significantly worse baseline cognitive performance on all cognitive domains we studied including memory, language, processing speed/executive functioning, and visuospatial abilities in a sample of ethnically diverse older adults. However, there were no significant differences between those with and without diabetes in terms of rate of change in any of these domains. Future longitudinal studies need to examine younger age groups with ascertainment of pre-diabetes and continuous measures of glycemia such as HbA1c incorporating clinical, genetic, and neuroimaging data in order to better understand the mechanisms by which diabetes and pre-diabetes affect cognitive decline.
Supplementary Material
Acknowledgments
Funding sources: This study was funded by the National Institute on Aging (AG026413, AG037212, AG030995, K99AG042483), National Institute on Mental Health (T32 MH 19934-17), and National Institute on Minority Health and Health Disparities (P60 MD000206)
K. Bangen, Y. Gu, N. Schupf, R. Mayuex, J. Manly, and J. Luchsinger receive funding from the National Institutes of Health. fThis study was funded by the following grants: National Institute on Aging (AG026413, AG037212, AG030995, K99AG042483), National Institute on Mental Health (T32 MH 19934-17), and National Institute on Minority Health and Health Disparities (P60 MD000206). In addition, J. Luchsinger is a consultant to Nutricia, Inc and has received royalties from Springer Publishing for the book he edited entitled “Diabetes and the Brain.”
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
There are no other conflicts to report.
Sponsor’s Role: The sponsors had no role in the design, methods, subject recruitment, data collections, analysis, or preparation of the paper.
Author Contributions: K. Bangen: primary responsibility for analysis and interpretation of data and drafting of the manuscript with J. Luchsinger, study conception and design. Y. Gu: primary responsibility for data analyses, assisted K. Bangen and J. Luchsinger with drafting of the manuscript. A. Gross, B. Schneider, J. Skinner, A. Benitez, B. Sachs, R. Shih, S. Sisco: study conception and design, critical revision of the manuscript for important intellectual content. N. Schupf and R. Mayeux: study funding, study conception and design, acquisition of the data, critical revision of the manuscript for important intellectual content. J. Manly: study funding, acquisition of the data, critical revision of the manuscript for important intellectual content primary responsibility for the development, use, and interpretation of neuropsychological variables. J. Luchsinger: study funding, primary responsibility for study conception and design analysis and interpretation of data, drafting of the manuscript, critical revision of the manuscript for important intellectual content. All authors approved the final version of the submitted manuscript.
References
- 1.Center, for, Disease, Control, and, Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States. Atlanta, Georgia: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 2.Vagelatos NT, Eslick GD. Type 2 diabetes as a risk factor for Alzheimer’s disease: The confounders, interactions, and neuropathology associated with this relationship. Epidemiol Rev. 2013 Jan 21; doi: 10.1093/epirev/mxs012. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 3.Biessels GJ, Staekenborg S, Brunner E, et al. Risk of dementia in diabetes mellitus: A systematic review. Lancet Neurol. 2006;5:64–74. doi: 10.1016/S1474-4422(05)70284-2. [DOI] [PubMed] [Google Scholar]
- 4.Luchsinger JA, Tang MX, Stern Y, et al. Diabetes mellitus and risk of Alzheimer’s disease and dementia with stroke in a multiethnic cohort. Am J Epidemiol. 2001;154:635–641. doi: 10.1093/aje/154.7.635. [DOI] [PubMed] [Google Scholar]
- 5.Arvanitakis Z, Schneider JA, Wilson RS, et al. Diabetes is related to cerebral infarction but not to AD pathology in older persons. Neurology. 2006;67:1960–1965. doi: 10.1212/01.wnl.0000247053.45483.4e. [DOI] [PubMed] [Google Scholar]
- 6.Peila R, Rodriguez BL, Launer LJ. Honolulu-Asia Aging S. Type 2 diabetes, APOE gene, and the risk for dementia and related pathologies: The Honolulu-Asia Aging Study. Diabetes. 2002;51:1256–1262. doi: 10.2337/diabetes.51.4.1256. [DOI] [PubMed] [Google Scholar]
- 7.Malek-Ahmadi M, Beach T, Obradov A, et al. Increased Alzheimer’s disease neuropathology is associated with type 2 diabetes and ApoE epsilon.4 carrier status. Curr Alzheimer Res. 2013;10:654–659. doi: 10.2174/15672050113109990006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahtiluoto S, Polvikoski T, Peltonen M, et al. Diabetes, Alzheimer disease, and vascular dementia: A population-based neuropathologic study. Neurology. 2010;75:1195–1202. doi: 10.1212/WNL.0b013e3181f4d7f8. [DOI] [PubMed] [Google Scholar]
- 9.Beeri MS, Silverman JM, Davis KL, et al. Type 2 diabetes is negatively associated with Alzheimer’s disease neuropathology. J Gerontol A Biol Sci Med Sci. 2005;60:471–475. doi: 10.1093/gerona/60.4.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chui HC, Zheng L, Reed BR, et al. Vascular risk factors and Alzheimer’s disease: Are these risk factors for plaques and tangles or for concomitant vascular pathology that increases the likelihood of dementia? An evidence-based review. Alzheimers Res Ther. 2012;4:1. doi: 10.1186/alzrt98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reijmer YD, van den Berg E, van Sonsbeek S, et al. Dementia risk score predicts cognitive impairment after a period of 15 years in a nondemented population. Dement Geriatr Cogn Disord. 2011;31:152–157. doi: 10.1159/000324437. [DOI] [PubMed] [Google Scholar]
- 12.Reaven GM, Thompson LW, Nahum D, et al. Relationship between hyperglycemia and cognitive function in older NIDDM patients. Diabetes Care. 1990;13:16–21. doi: 10.2337/diacare.13.1.16. [DOI] [PubMed] [Google Scholar]
- 13.Brands AM, Van den Berg E, Manschot SM, et al. A detailed profile of cognitive dysfunction and its relation to psychological distress in patients with type 2 diabetes mellitus. J Int Neuropsychol Soc. 2007;13:288–297. doi: 10.1017/S1355617707070312. [DOI] [PubMed] [Google Scholar]
- 14.van Harten B, Oosterman J, Muslimovic D, et al. Cognitive impairment and MRI correlates in the elderly patients with type 2 diabetes mellitus. Age Ageing. 2007;36:164–170. doi: 10.1093/ageing/afl180. [DOI] [PubMed] [Google Scholar]
- 15.Bangen KJ, Beiser A, Delano-Wood L, et al. APOE genotype modifies the relationship between midlife vascular risk factors and later cognitive decline. J Stroke Cerebrovasc Dis. 2013;22:1361–1369. doi: 10.1016/j.jstrokecerebrovasdis.2013.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arvanitakis Z, Wilson RS, Bienias JL, et al. Diabetes mellitus and risk of Alzheimer disease and decline in cognitive function. Arch Neurol. 2004;61:661–666. doi: 10.1001/archneur.61.5.661. [DOI] [PubMed] [Google Scholar]
- 17.Reijmer YD, van den Berg E, Ruis C, et al. Cognitive dysfunction in patients with type 2 diabetes. Diabetes Metab Res Rev. 2010;26:507–519. doi: 10.1002/dmrr.1112. [DOI] [PubMed] [Google Scholar]
- 18.Gregg EW, Yaffe K, Cauley JA, et al. Is diabetes associated with cognitive impairment and cognitive decline among older women? Study of Osteoporotic Fractures Research Group. Arch Intern Med. 2000;160:174–180. doi: 10.1001/archinte.160.2.174. [DOI] [PubMed] [Google Scholar]
- 19.Fontbonne A, Berr C, Ducimetiere P, et al. Changes in cognitive abilities over a 4-year period are unfavorably affected in elderly diabetic subjects: Results of the Epidemiology of Vascular Aging Study. Diabetes Care. 2001;24:366–370. doi: 10.2337/diacare.24.2.366. [DOI] [PubMed] [Google Scholar]
- 20.Hassing LB, Grant MD, Hofer SM, et al. Type 2 diabetes mellitus contributes to cognitive decline in old age: A longitudinal population-based study. J Int Neuropsychol Soc. 2004;10:599–607. doi: 10.1017/S1355617704104165. [DOI] [PubMed] [Google Scholar]
- 21.Kanaya AM, Barrett-Connor E, Gildengorin G, et al. Change in cognitive function by glucose tolerance status in older adults: A 4-year prospective study of the Rancho Bernardo study cohort. Arch Intern Med. 2004;164:1327–1333. doi: 10.1001/archinte.164.12.1327. [DOI] [PubMed] [Google Scholar]
- 22.Yaffe K, Falvey C, Hamilton N, et al. Diabetes, glucose control, and 9-year cognitive decline among older adults without dementia. Arch Neurol. 2012;69:1170–1175. doi: 10.1001/archneurol.2012.1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fischer AL, de Frias CM, Yeung SE, et al. Short-term longitudinal trends in cognitive performance in older adults with type 2 diabetes. J Clin Exp Neuropsychol. 2009;31:809–822. doi: 10.1080/13803390802537636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu JH, Haan MN, Liang J, et al. Impact of diabetes on cognitive function among older Latinos: A population-based cohort study. J Clin Epidemiol. 2003;56:686–693. doi: 10.1016/s0895-4356(03)00077-5. [DOI] [PubMed] [Google Scholar]
- 25.van den Berg E, Reijmer YD, de Bresser J, et al. A 4 year follow-up study of cognitive functioning in patients with type 2 diabetes mellitus. Diabetologia. 2010;53:58–65. doi: 10.1007/s00125-009-1571-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Jager CA, Schrijnemaekers AC, Honey TE, et al. Detection of MCI in the clinic: Evaluation of the sensitivity and specificity of a computerised test battery, the Hopkins Verbal Learning Test and the MMSE. Age Ageing. 2009;38:455–460. doi: 10.1093/ageing/afp068. [DOI] [PubMed] [Google Scholar]
- 27.Ostrosky-Solis F, Lopez-Arango G, Ardila A. Sensitivity and specificity of the Mini-Mental State Examination in a Spanish-speaking population. Appl Neuropsychol. 2000;7:25–31. doi: 10.1207/S15324826AN0701_4. [DOI] [PubMed] [Google Scholar]
- 28.Luchsinger JA, Reitz C, Patel B, et al. Relation of diabetes to mild cognitive impairment. Arch Neurol. 2007;64:570–575. doi: 10.1001/archneur.64.4.570. [DOI] [PubMed] [Google Scholar]
- 29.Tang MX, Stern Y, Marder K, et al. The APOE-epsilon4 allele and the risk of Alzheimer disease among African Americans, whites, and Hispanics. JAMA. 1998;279:751–755. doi: 10.1001/jama.279.10.751. [DOI] [PubMed] [Google Scholar]
- 30.Manly JJ, Bell-McGinty S, Tang MX, et al. Implementing diagnostic criteria and estimating frequency of mild cognitive impairment in an urban community. Arch Neurol. 2005;62:1739–1746. doi: 10.1001/archneur.62.11.1739. [DOI] [PubMed] [Google Scholar]
- 31.Cheng D, Noble J, Tang MX, et al. Type 2 diabetes and late-onset Alzheimer’s disease. Dement Geriatr Cogn Disord. 2011;31:424–430. doi: 10.1159/000324134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stern Y, Andrews H, Pittman J, et al. Diagnosis of dementia in a heterogeneous population. Development of a neuropsychological paradigm-based diagnosis of dementia and quantified correction for the effects of education. Arch Neurol. 1992;49:453–460. doi: 10.1001/archneur.1992.00530290035009. [DOI] [PubMed] [Google Scholar]
- 33.Lopes-Virella MF, Stone P, Ellis S, et al. Cholesterol determination in high-density lipoproteins separated by three different methods. Clin Chem. 1977;23:882–884. [PubMed] [Google Scholar]
- 34.Siedlecki KL, Manly JJ, Brickman AM, et al. Do neuropsychological tests have the same meaning in Spanish speakers as they do in English speakers? Neuropsychology. 2010;24:402–411. doi: 10.1037/a0017515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 36.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: A generalized estimating equation approach. Biometrics. 1988;44:1049–1060. [PubMed] [Google Scholar]
- 37.Luchsinger JA, Reitz C, Honig LS, et al. Aggregation of vascular risk factors and risk of incident Alzheimer disease. Neurology. 2005;65:545–551. doi: 10.1212/01.wnl.0000172914.08967.dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Noble JM, Manly JJ, Schupf N, et al. Association of C-reactive protein with cognitive impairment. Arch Neurol. 2010;67:87–92. doi: 10.1001/archneurol.2009.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reitz C, Tang MX, Schupf N, et al. Association of higher levels of high-density lipoprotein cholesterol in elderly individuals and lower risk of late-onset Alzheimer disease. Arch Neurol. 2010;67:1491–1497. doi: 10.1001/archneurol.2010.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schneider BC, Gross AL, Bangen KJ, et al. Association of vascular risk factors with cognition in a multiethnic sample. J Gerontol B Psychol Sci Soc Sci. 2014 May 12; doi: 10.1093/geronb/gbu040. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Euser SM, Sattar N, Witteman JC, et al. A prospective analysis of elevated fasting glucose levels and cognitive function in older people: Results from PROSPER and the Rotterdam Study. Diabetes. 2010;59:1601–1607. doi: 10.2337/db09-0568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Knopman D, Boland LL, Mosley T, et al. Cardiovascular risk factors and cognitive decline in middle-aged adults. Neurology. 2001;56:42–48. doi: 10.1212/wnl.56.1.42. [DOI] [PubMed] [Google Scholar]
- 43.de Bresser J, Tiehuis AM, van den Berg E, et al. Progression of cerebral atrophy and white matter hyperintensities in patients with type 2 diabetes. Diabetes Care. 2010;33:1309–1314. doi: 10.2337/dc09-1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Biessels GJ. Intensive glucose lowering and cognition in type 2 diabetes. Lancet Neurol. 2011;10:949–950. doi: 10.1016/S1474-4422(11)70199-5. [DOI] [PubMed] [Google Scholar]
- 45.Bangen KJ, Nation DA, Delano-Wood L, et al. Aggregate effects of vascular risk factors on cerebrovascular changes in autopsy-confirmed Alzheimer’s disease. Alzheimers Dement. 2014 Jul 8; doi: 10.1016/j.jalz.2013.12.025. pii: S1552-5260(14)00119-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc. 2002;8:448–460. [PubMed] [Google Scholar]
- 47.Biessels GJ, Deary IJ, Ryan CM. Cognition and diabetes: a lifespan perspective. Lancet Neurol. 2008;7:184–190. doi: 10.1016/S1474-4422(08)70021-8. [DOI] [PubMed] [Google Scholar]
- 48.Luchsinger JA, Reitz C, Patel B, et al. Relation of diabetes to mild cognitive impairment. Arch Neurol. 2007;64:570–575. doi: 10.1001/archneur.64.4.570. [DOI] [PubMed] [Google Scholar]
- 49.Noble JM, Manly JJ, Schupf N, et al. Type 2 diabetes and ethnic disparities in cognitive impairment. Ethn Dis. 2012;22:38–44. [PMC free article] [PubMed] [Google Scholar]
- 50.Gross AL, Benitez A, Shih R, et al. Predictors of retest effects in a longitudinal study of cognitive aging in a diverse community-based sample. doi: 10.1017/S1355617715000508. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.