Abstract
Context:
Sport-related concussion can affect athletes' sport participation and academic success. With the recent emphasis on cognitive rest, student-athletes may benefit from academic accommodations (AA) in the classroom; however, athletic trainers' (ATs') perceived familiarity with, and use of, AA is unknown.
Objective:
To assess secondary school ATs' perceived familiarity with, attitudes and beliefs about, and incorporation of AA for student-athletes after sport-related concussion. A secondary purpose was to determine whether employment status altered familiarity and use of AA.
Design:
Cross-sectional study.
Setting:
Online survey.
Patients or Other Participants:
Of 3286 possible respondents, 851 secondary school ATs accessed the survey (response rate = 25.9%; 308 men [36.2%], 376 women [44.2%], 167 respondents [19.6%] with sex information missing; age = 37.3 ± 10.1 years).
Main Outcome Measure(s):
Participants were solicited via e-mail to complete the Beliefs, Attitudes and Knowledge Following Pediatric Athlete Concussion among Athletic Trainers employed in the secondary school setting (BAKPAC-AT) survey. The BAKPAC-AT assessed ATs' perceived familiarity, perceptions, and roles regarding 504 plans, Individualized Education Programs (IEPs), and returning student-athletes to the classroom. Independent variables were employment status (full time versus part time), employment model (direct versus outreach), years certified, and years of experience in the secondary school setting. The dependent variables were participants' responses to the AA questions. Spearman rank-correlation coefficients were used to assess relationships and Mann-Whitney U and χ2 tests (P < .05) were used to identify differences.
Results:
Respondents reported that approximately 41% of the student-athletes whose sport-related concussions they managed received AA. Respondents employed directly by the school were more familiar with 504 plans (P < .001) and IEPs (P < .001) and had a greater belief that ATs should have a role in AA. Both the number of years certified and the years of experience at the secondary school were significantly correlated with perceived familiarity regarding 504 plans and IEPs.
Conclusions:
The ATs employed directly by secondary schools and those with more experience as secondary school ATs were more familiar with AA. Understanding AA is important for all ATs because cognitive rest and “return to learn” are becoming more widely recommended in concussion management.
Key Words: adolescent sport-related concussions, concussion management, 504 plans, Individualized Education Programs
Key Points
The patients in nearly one-half of the sport-related concussion cases managed by secondary school athletic trainers received academic accommodations.
For proper management of and successful recovery from concussions, academic accommodations are often important.
Athletic trainers should become more familiar with academic accommodations to ensure that student-athletes can return successfully to the classroom.
The Centers for Disease Control and Prevention estimated that 1.6 to 3.8 million sport- and recreational-related concussions occurred annually in the United States.1 For high school athletes, an estimated 8.9% of all injuries are concussions.2 Early recognition and appropriate management of these prevalent injuries are especially important in adolescents to reduce the risk of more serious conditions and to facilitate proper recovery.3 In the secondary school setting, that recognition and management are often components of athletic training services, delivered by certified or state-licensed (or both) athletic trainers (ATs) who frequently assist with concussion management from initial evaluation through return to play. With the increased occurrence of concussions,1 it is imperative that best practices for proper management of the injuries be implemented and that those practices be consistent with expert recommendations and guidelines.
The signs and symptoms of concussion can broadly affect the student-athlete's life both in and out of athletic participation.4 After a concussion, the student-athlete may experience an array of clinical signs and symptoms. Those symptoms may include cognitive deficits,5,6 such as poor concentration and difficulty remembering, sensitivity to noise and light, dizziness, and most commonly, headaches.4,7–10 Unfortunately for the student-athlete, those signs and symptoms can be exacerbated by any activity requiring cognitive demand, such as watching TV, listening to music, reading, playing video games, and even performing school work. In fact, normal academic demands are a major source of cognitive exertion in student-athletes after sport-related concussion.
Effectively managing this complex and often-unpredictable collection of signs and symptoms can be aided through the use of individualized concussion-management plans, especially those plans that encourage a return to school in an appropriate and stepwise manner.11,12 One important component of such an individualized plan is cognitive rest. Cognitive rest is imperative for the healing process because it allows the brain time to recover without exacerbating symptoms.13 Consensus guidelines,14 expert opinion,15,16 and some evidence13 suggested that cognitive rest is beneficial in recovery. However, a common limitation of individualized concussion-management plans is that they typically omit or place less emphasis on components that are unrelated to athletics, such as limiting cognitive activity and modifying cognitive demands, specifically in academics.17 That lack is problematic because although abundant published research pertains to acute diagnosis, management, and return to play after a concussion, little research about school reintegration or return to learn has been conducted to date. Consequently, comprehensive concussion-management guidelines for student-athletes often fail to include information about both return to play and school and home functioning.7
One way of modifying cognitive demands is through academic accommodations (AA). Academic accommodations can include both informal alterations in classroom activity and formal accommodations, such as 504 plans and Individualized Education Programs (IEPs).4 One distinction between informal and formal accommodations is the temporary nature of the former. Informal accommodations allow the student-athlete to receive accommodations in school immediately after a concussion and are intended to provide temporary modifications to enhance academic performance and to aid in physical recovery.4 Informal accommodations include longer testing periods, homework extensions, lighter school days and breaks throughout the day, excused absences, relief from light and noise when necessary, excused practices or gym classes, and other arrangements.4 With selected informal AA, the student-athlete can recover and improve in the classroom over time.13,15 Section 504 plans and IEPs are formal plans that guarantee students academic assistance as well as protection from discrimination in response to an identified disability.18
Although formal accommodations are available to all high school students, including student-athletes, it is unclear how familiar ATs are with AA. Therefore, the purpose of our study was to assess the perceived familiarity with and perceptions of ATs employed in the secondary school setting (SSATs) regarding AA for adolescent student-athletes after sport-related concussion. Secondary and tertiary purposes were to determine the availability of academic-support teams in secondary schools and whether employment status altered familiarity with, and use of, AA.
METHODS
Instrumentation
Survey Development
We conducted a literature review to locate previously developed surveys that specifically addressed participants' beliefs about, attitudes toward, and perceived familiarity with AA. Because of the lack of preexisting instruments to assess ATs' familiarity with, attitudes toward, and incorporation of AA in the secondary-school clinical setting, we created a new survey instrument. With permission, we incorporated questions from the National Sports Safety in Secondary Schools Benchmark study.19 Additionally, we compiled a combination of questions based on information from content experts. The survey, titled “The Beliefs, Attitudes and Knowledge Following Pediatric Athlete Concussions among athletic trainers employed in the secondary school setting” (BAKPAC-AT), consists of 3 sections: (1) concussion management and care, (2) concussion referral, and (3) AA. Additionally, participants were asked to complete a demographic questionnaire about their educational history and job position at the end of the online instrument. Several question formats were used, including binary (yes, no), multiple choice, open ended, Likert scale, and multistep. The survey was created using an online system, Qualtrics Online Survey Software (Qualtrics LLC, Provo, UT).
Academic Accommodations Section
The focus of this article is to discuss the AA portion of the BAKPAC-AT. The AA section includes 18 questions of various formats. The first series of items assessed SSATs' beliefs about and attitudes toward AA and their perceived role regarding AA in the secondary school setting via a 4-point Likert scale. Next, the participant was asked to complete questions pertaining to the structure and personnel involved in an academic-support team at his or her school. Participants were also requested to report their perceived familiarity with 504 plans and IEPs via a 4-point Likert scale. Finally, participants were asked to respond to several demographic questions regarding any previous experience and involvement with AA for student-athletes after a sport-related concussion.
Survey Validation
Once we developed the BAKPAC-AT instrument, a panel of 3 concussion experts, consisting of a neuropsychologist, a pediatric primary-care sports medicine physician, and a concussion researcher, assessed the survey for content validity and comprehensiveness. Each expert was sent an e-mail requesting participation in the BAKPAC-AT validation process. The request was to review the survey (the URL hyperlink was provided), complete a validity rubric regarding the importance of each question, and provide comments about question phrasing and relevance. The validity rubric required each panelist to assess each survey item using a 3-point scale. A rating of 3 indicated the panelist perceived the question was good and should remain in the survey as written, a 2 indicated the question will be acceptable once revised, and a 1 was for a question that was poor and needs to be removed. If an item received a rating of 2, the panelist was asked for additional feedback. Panelists were also asked to provide feedback on the length of the survey as well as the feasibility of expanding the survey to other health care professionals. Once the completed validity rubrics were returned, we made any necessary changes.
The survey was deemed to have content validity for the assessment of SSATs' concussion management, concussion referral, and role in providing AA after a sport-related concussion. Because the style of the questions was aimed at capturing clinicians' current clinical-practice patterns, a reliability analysis to determine the internal consistency of the instrument was not warranted. However, we asked a representative sample of ATs (n = 18) to complete the BAKPAC-AT to further refine the content validity of the instrument as well as the comprehensibility of the online format.
Procedures
We obtained contact information, including names and e-mail addresses, for all members employed in the secondary school setting (n = 3286) from the National Athletic Trainers' Association via its “Survey List Request Form.” National Athletic Trainers' Association SSAT members were recruited for participation in this investigation during fall 2012. The A. T. Still University institutional review board approved this study as exempt research, and consent was implied by voluntary submission of the completed survey.
During the data-collection period, recruits were sent an introductory e-mail requesting participation in the research investigation. The e-mail included a description of the purpose and importance of the research study, the estimated survey-completion time, a URL hyperlink to the survey Web page, and a deadline date for survey completion. The e-mail also provided contact information of the primary researcher (R.M.W.) for comments, questions, or concerns about the research study or the survey instrument. Participants were given 4 weeks, between September 2012 and October 2012, to complete the survey; follow-up e-mails were sent 1 time/wk reminding those who had yet to respond. Once a participant completed the survey (indicated by clicking “submit”), a thank-you e-mail was automatically generated in Qualtrics Survey Software and immediately sent to the individual.
Data Analysis
We used IBM SPSS Statistics software (version 21.0.0; IBM Corporation, Armonk, NY) for statistical analyses. Descriptive statistics were used to calculate the means, standard deviations, and frequencies of the data. The independent variables were employment status with 2 levels (whether the AT was employed full time or part time by the school), employment model with 2 levels (direct model [working through the school] or an outreach model [working in a clinical or off-site source]), years of experience as a certified AT, and years of AT experience in the secondary school setting. The dependent variables were participants' responses to the AA questions. We calculated separate Spearman rank-correlation coefficients to assess relationships among perceived familiarity with, beliefs about, attitudes toward AAs and years of experience. The strength of the relationship was evaluated using criteria from Portney and Watkins,20 with 0.00 to 0.25 as no relationship, 0.25 to 0.50 as a fair relationship, 0.50 to 0.75 as a moderate-to-good relationship, and greater than 0.75 as a good-to-excellent relationship. Separate Mann-Whitney U tests and χ2 tests (P < .05) were used to identify differences between perceived familiarity and employment status as well as between employment models.
RESULTS
Of the convenience sample of 3286 SSATs, 851 clinicians accessed the survey, for a response rate of 25.9%. The participants were 308 men (36.2%) and 376 women (44.2%) with an average age of 37.3 ± 10.1 years. Fifty-one participants (6%) did not complete any questions and 18 participants (2%) did not practice athletic training in any capacity in the secondary school setting and were, therefore, excluded from the analysis. Thus, 782 ATs, representing all 50 states and the District of Columbia, completed at least 1 part of the survey. Participant and secondary school demographics are displayed in Tables 1 and 2, respectively.
Table 1.
Secondary School ATs' Demographics
| Characteristic |
No. (%) |
| Sex (n = 684) | |
| Male | 308 (45.0) |
| Female | 376 (55.0) |
| AT experience, y (n = 684) | |
| 0–2 | 46 (6.7) |
| 3–5 | 124 (18.1) |
| 6–10 | 137 (20.0) |
| 11–15 | 118 (17.3) |
| 16–20 | 110 (16.1) |
| 21+ | 149 (21.8) |
| Secondary school AT experience, y (n = 684) | |
| 0–2 | 75 (10.9) |
| 3–5 | 140 (20.5) |
| 6–10 | 146 (21.3) |
| 11–15 | 132 (19.3) |
| 16–20 | 88 (12.9) |
| 21+ | 103 (15.1) |
| Highest education level (n = 684) | |
| Bachelor's | 260 (38.0) |
| Master's | 417 (61.0) |
| Doctorate (PhD, EdD) | 5 (0.7) |
| Clinical doctorate (eg, DPT) | 2 (0.3) |
| Job title (n = 684) | |
| Head AT | 560 (81.9) |
| Assistant AT | 57 (8.3) |
| AT, other | 37 (5.4) |
| Associate AT | 19 (2.8) |
| School personnel | 8 (1.2) |
| Other | 3 (0.4) |
| Employment model (n = 792) | |
| Direct | 582 (73.5) |
| Outreach | 198 (25.0) |
| Other | 12 (1.5) |
Abbreviations: AT, athletic trainer; DPT, doctor of physical therapy; EdD, doctor of education; PhD, doctor of philosophy.
Table 2.
Secondary School Demographics
| Characteristic |
No. (%) |
| Type of school (n = 684) | |
| Public | 539 (78.8) |
| Public charter | 2 (0.3) |
| Private parochial | 63 (9.2) |
| Private charter | 15 (2.2) |
| Private other | 56 (8.2) |
| Other | 9 (1.3) |
| Enrollment, No. students (n = 684) | |
| <250 | 19 (2.8) |
| 250–499 | 96 (14.0) |
| 500–999 | 164 (24.0) |
| 1000–1999 | 254 (37.1) |
| 2000–2999 | 111 (16.2) |
| 3000–3999 | 31 (4.5) |
| 4000–4999 | 4 (0.6) |
| >5000 | 5 (0.7) |
| Football team (n = 684) | |
| Yes | 644 (94.2) |
| No | 40 (5.8) |
Concussions and School Performance
On average, SSATs managed 20.6 ± 17.4 (range, 0–150) student-athletes after sport-related concussions per year, and of those student-athletes, approximately 8.4 ± 13.0 (range, 0–100) received AA. The ATs who were employed directly by the school or school district managed more athletes with concussions annually (18.7 ± 18.3 versus 16.8 ± 15.5, P < .001), with a higher number of those athletes receiving AA (7.9 ± 12.9 versus 6.1 ± 11.3, P < .001).
The frequency and percentage of responses for the AA questions are presented in Table 3. Most participants either strongly agreed (92.1%, n = 644 of 699) or agreed (4.9%, n = 34 of 699) that a concussion can affect school performance, with only 3.0% (n = 21 of 699) of the participants reporting they strongly disagreed. Additionally, most respondents strongly agreed (36.3%, n = 254 of 699) or agreed (46.1%, n = 322 of 699) that student-athletes currently being managed for concussions were eligible for special considerations under the Americans with Disabilities Act, whereas 15% (n = 105 of 699) and 2.6% (n = 18 of 699) of the participants disagreed or strongly disagreed, respectively.
Table 3.
Respondents' Perceptions of Factors Related to Academic Accommodations
| Factor |
Perception, No. (%) |
|||
| Strongly Disagree |
Disagree |
Agree |
Strongly Agree |
|
| Concussions can affect school performance (n = 699) | 21 (3.0) | 0 (0) | 34 (4.9) | 644 (92.1) |
| Student-athletes with active concussions are eligible for special considerations under the Americans with Disabilities Act (n = 699) | 18 (2.6) | 105 (15.0) | 322 (46.1) | 254 (36.3) |
| An athletic trainer should be part of the team established to ensure educational accommodations for student-athletes who sustained a sport-related concussion (n = 699) | 18 (2.6) | 11 (1.6) | 167 (23.9) | 503 (71.9) |
| An athletic trainer has the ability to assist a student-athlete's return to the classroom following an absence caused by a sport-related concussion (n = 691) | 76 (10.9) | 38 (5.5) | 377 (54.6) | 200 (29.0) |
Academic Support
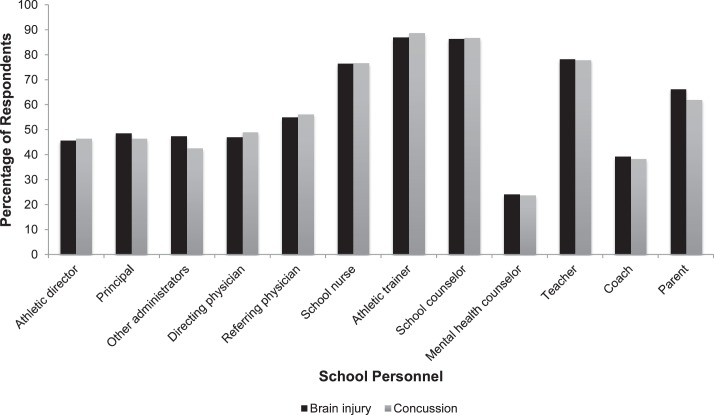
Most of those who responded strongly agreed (71.9%, n = 503 of 699) or agreed (23.9%, 167 of 699) that an AT should be a part of the academic-support team in the secondary school setting; only 1.6% (n = 11 of 699) of participants disagreed and 2.6% (n = 18 of 699) strongly disagreed. To determine whether a difference exists in school policy for those with a brain injury compared with athletes who sustained a concussion, several questions were asked about school protocols for brain injury and concussion separately. Almost half of the participants (49.2%, 344 of 699) reported that the secondary school in which they were employed had an academic-support team for student-athletes with brain injuries, and 44.3% (308 of 695) indicated the secondary school had an academic-support team for concussed student-athletes. A breakdown of the personnel involved in the secondary school academic-support teams for student-athletes with brain injuries and for student-athletes with concussions is provided in Figure 1.
Figure 1.
Personnel involved in the secondary school academic-support team for brain-injured and concussed student-athletes.
Respondents' perceived familiarity with 504 and IEP plans, according to employment model, is illustrated in Figures 2 and 3. The data suggest there is little perceived familiarity among ATs regarding 504 plans and IEPs. Of those who responded, most either agreed (54.6%, 377 of 691) or strongly agreed (29.0%, n = 200 of 691) that an AT has the ability to assist a student-athlete's return to the classroom after a sport-related concussion. Only 5.5% (n = 38 of 691) of the participants disagreed and 10.9% (n = 76 of 691) strongly disagreed with that statement.
Figure 2.
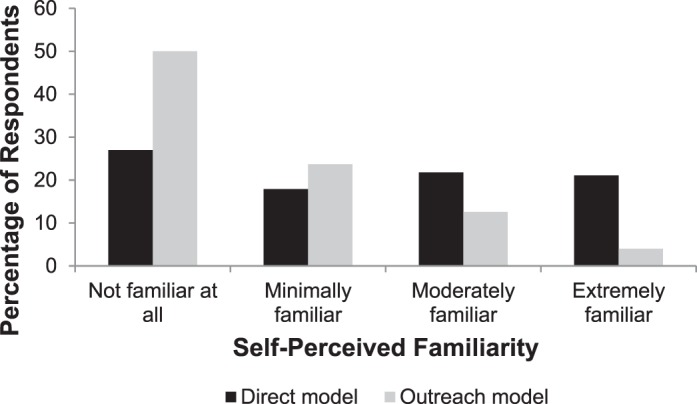
Athletic trainers' self-perceived familiarity with 504 plans by employment model.
Figure 3.
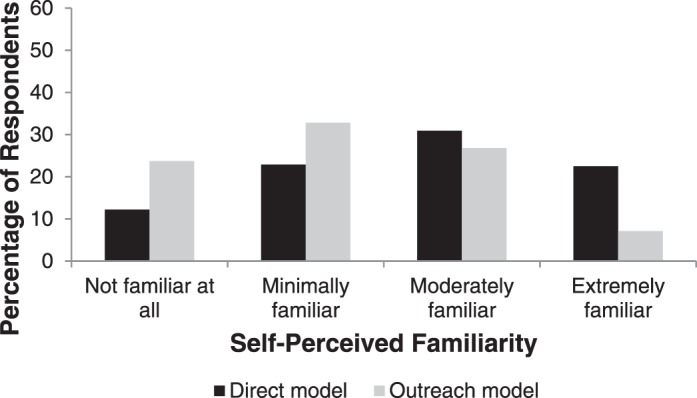
Athletic trainers' self-perceived familiarity with Individualized Education Programs by employment model.
Employment Status or Model
Compared with those ATs employed through an outreach model, respondents employed directly by a secondary school had greater familiarity with 504 plans (P < .001) and IEPs (P < .001). No differences were evident between those employed full time versus part time and their perceived familiarity with 504 plans (P = .143), IEPs (P = .856), or perceptions of ATs' role in AA (P = .219).
Years of Experience
We observed a significant, positive correlation between the number of years certified and perceived familiarity regarding 504 plans (r = 0.34, P < .001) and IEPs (r = 0.33, P < .001). A significant positive relationship also occurred between years of experience in the secondary school setting and perceived familiarity with 504 plans (r = 0.35, P < .001) and IEPs (r = 0.33, P < .001). However, no significant associations were noted between years certified (r = 0.06, P = .14) or years of secondary school experience (r = 0.001, P = .97) and perceptions of ATs' role in AA.
DISCUSSION
The purpose of our study was to determine SSATs' beliefs about, attitudes toward, and perceived familiarity with AA for student-athletes who sustain a sport-related concussion. Our main findings indicated that SSATs believed they should be part of the academic-support team, yet their perceived familiarity with formal AA was suboptimal. Additionally, both employment model and years of experience influenced an SSAT's familiarity with AA.
To ensure ATs are providing whole-person health care, which includes patients' needs, goals, and desires,21 it is important for SSATs to become more informed about the significance of AA and the processes for implementing formal accommodations. Particularly for concussed student-athletes, it is imperative that cognitive and academic struggles be considered when developing a concussion-management plan.4,11,14,22 In fact, current recommendations suggest that individuals who have sustained concussions require rest9,14,15 because both physical and cognitive activity can exacerbate symptoms.11,13,15 It is advised that physical and cognitive rest allows the brain time to heal. However, proper physical and cognitive rest for a secondary school student-athlete typically requires modification in all aspects of life, including physical activity and school. Some suggest this can be accomplished by decreasing or avoiding visually stimulating activities, such as computer work and reading, while symptoms are present.15 Consequently, to be a valuable tool for a student-athlete attempting to return to learn, a comprehensive academic-management plan must address the need for AA and should coordinate the contributions of all school personnel who may interact with that student-athlete on a regular basis.4,13,23
Informal AA are temporary accommodations in school, which assist the student-athlete in achieving optimal recovery. More-formalized AA include 504 plans and IEPs, both of which may be used for student-athletes after concussions. The 504 plans protect the rights of those with disabilities by allowing an individual the opportunity to fully participate with his or her peers.24 The 504 plans must be available to individuals with disabilities, regardless of the specific nature of the disability. To qualify for a 504 plan, an individual must display, through formal evaluation, that he or she has a physical or mental impairment that limits 1 or more major life activities.24 A major life activity consists of, but is not limited to, speaking, listening, reading, and writing. Concussed student-athletes who have continued cognitive difficulties may qualify for a 504 plan that allows accommodations, such as longer time for taking tests, homework extensions, rest periods during the day, or the use of note takers.4
The IEPs, on the other hand, are designed for people enrolled in public schools who require special education as a result of their disability. An IEP promotes collaboration of the school personnel and physicians to improve educational opportunities for individuals, often through modification of the existing curriculum.23 The IEPs are available for individuals ages 3 to 21 years who fall within 1 of the disability categories requiring special education and whose disability adversely affects his or her educational performance or the ability to benefit from general education.25
The 504 plans and IEPs provide permanent documentation in the school system that allow for the implementation of any academic changes necessary to make the student-athlete comfortable and academically successful. Both 504 plans and IEPs typically take longer to implement than temporary school accommodations; however, they are important and valuable for ensuring successful reintegration in school after a sport-related concussion.26 For concussed student-athletes, 504 plans are likely to be used more frequently than IEPs27 and carry less stigma.
Perceptions of AA
To our knowledge, the BAKPAC-AT is the first survey designed to assess the perceived familiarity with, attitudes toward, and beliefs about sport-related concussion-management practice trends and AA among SSATs. Our data suggest that SSATs agree that they should be involved in the provision of AA for a student-athlete after a sport-related concussion. This perception indicates that ATs believe that they have appropriate familiarity with AA to establish a role in their provision. It also signifies that ATs believe they are prepared to collaborate with school nurses, guidance counselors, and other school personnel who might be involved in the implementation and management of AA.
However, our findings suggest that, ironically, SSATs are not familiar with AA, and therefore, more attention should be placed on this area as part of professional education. It is important to fill the apparent gap in SSATs' perceived familiarity with AA through either postprofessional or continuing education opportunities. An increase in familiarity with AA should theoretically improve the SSAT's ability to provide concussion-management strategies necessary for return to sport as well as return to learn. Additionally, implementation of AA presents a rare opportunity for interprofessional collaboration in support of patient care. This creates the potential for better patient care and exposes the profession of athletic training to a variety of other health providers.
Familiarity with AA differed by employment model. Those employed directly through the school had greater perceived familiarity with AA compared with those employed through an outreach model. Individuals employed directly by the school were also more familiar with 504 plans and IEPs. This may be because those who are employed directly are more deeply immersed in the secondary school environment, which leads to greater familiarity with various aspects of the environment beyond athletic training. For example, those ATs may be more involved with the school and may have more frequent communication with administrative and support staff, a fact supported by research.28 Individuals employed in an outreach setting may have responsibilities to both the secondary school setting and the clinic, whereas someone employed by the secondary school directly does not share responsibility between the settings. The teaching responsibilities of the ATs involved directly with the school may also have provided them with professional development and education in teaching that can contribute to their familiarity with concerns such as disabilities.
Perceived familiarity of AA differed by the number of years certified. The number of years' experience in the secondary school setting was related to perceived familiarity with IEPs: those having more years of experience were more familiar with AA. These findings are similar to those of other studies that have shown direct relationships between years of experience and subject knowledge in health care providers.29,30 These authors looked at the general practice guidelines and consensus of all health care providers as well as the knowledge and experience of ATs. For example, Cochrane et al29 identified barriers that prevented the optimal health care delivery of knowledge transfer to patients; lack of experience and lack of knowledge were professional barriers that interfered with delivery of care. Mazerolle et al30 studied ATs' knowledge of exertional heat stroke and found that those with more experience had greater knowledge of proper management protocols. This, in part, can be correlated with advanced skills or knowledge gained through years of practice and experience with an array of patients. Currently, the new competency standards for the Commission on Accreditation of Athletic Training Education (CAATE) do not require entry-level ATs to be familiar with AA.31,32
Consequently, SSATs should enhance their knowledge base through continuing education opportunities and, when necessary, pursue postprofessional-level education to advance their skills and knowledge in the areas of concussion management and AA. The SSAT can enhance his or her familiarity with AA in a number of ways. First, the SSAT can initiate the development of a school concussion-management team, which includes the school nurse and school counselor, and set up meetings with team members to ensure everyone understands the concussion-management protocols. After a concussion, members of the team should be notified that a student-athlete may need accommodations to aid recovery. Communication among members should occur regularly as the student-athlete's concussion is managed. Lastly, the SSAT should seek continuing education opportunities and stay current with the concussion literature to learn more about AA in the management of concussion. Becoming more familiar with AA is vital to enhancing patient care after a concussion, but ATs may need to take it on themselves to increase their knowledge of and familiarity with the topic.
Limitations and Future Directions
This study had some limitations. We sent the BAKPAC-AT to individuals on the National Athletic Trainers' Association member list who were identified as ATs employed in the secondary school setting. Therefore, SSATs who were not members of the National Athletic Trainers' Association or who identified themselves in another membership category were not invited to participate. Our response rate of 25.9% was acceptable but may have limited the overall representation of ATs who provide care to secondary school student-athletes (eg, outreach). We developed the survey to evaluate the perceived familiarity of ATs employed in the secondary school setting with AA but did not formally evaluate their knowledge of AA. Therefore, it is plausible that ATs perceived themselves to be less familiar with the concepts than they actually were.
Future authors should evaluate the perceived familiarity with, attitudes toward, and beliefs about a variety of health care providers involved in the management of concussed student-athletes. Additionally, further research should be conducted to gather prospective information on AA for student-athlete's after sport-related concussion and to educate ATs on the importance of addressing academics after concussion. Investigators should also determine whether the presence of the AT in the return-to-learn process produces better outcomes for the student-athlete. This research is imperative to validate ATs' beliefs that they should be involved in this AA process.
CONCLUSIONS
Athletic trainers generally provide care for an average of 20 adolescent patients with symptoms of a concussion per year, and on average, 8 of those patients (40%) will require and receive AA. Athletic trainers employed directly by the secondary school and those with more experience as ATs employed in the secondary school setting were more familiar with AA. This may be the result of knowledge gained as members of the school staff. Understanding AA is important for all ATs because cognitive rest and return to learn are becoming more widely recommended as a part of concussion-management plans. Understanding evidence-based protocols for concussion management provides clinicians with proper and effective return-to-play guidelines and promotes the student-athlete's return to the classroom. With more familiarity and a stronger understanding of AA, ATs can ensure the proper care and facilitate the necessary steps to return to learn.
REFERENCES
- 1.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–378. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Gessel LM, Fields SK, Collins C, Dick R, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42(4):495–503. [PMC free article] [PubMed] [Google Scholar]
- 3.Bruce DA. Delayed deterioration of consciousness after trivial head injury in childhood. Br Med J (Clin Res Ed) 1984;289(6447):715–716. doi: 10.1136/bmj.289.6447.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGrath N. Supporting the student-athlete's return to classroom after a sport-related concussion. J Athl Train. 2010;45(5):492–498. doi: 10.4085/1062-6050-45.5.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Register-Mihalik J, Guskiewicz KM, Mann JD, Shields EW. The effects of headache on clinical measures of neurocognitive function. Clin J Sport Med. 2007;17(4):282–288. doi: 10.1097/JSM.0b013e31804ca68a. [DOI] [PubMed] [Google Scholar]
- 6.Cunningham J, Brison RJ, Pickett W. Concussive symptoms in emergency department patients diagnosed with minor head injury. J Emerg Med. 2011;40(3):262–266. doi: 10.1016/j.jemermed.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 7.Gioia GA, Schneider JC, Vaughan CG, Isquith PK. Which symptoms assessment approaches are uniquely appropriate for pediatric concussion? J Sports Med. 2009;43((suppl 1)):i13–i22. doi: 10.1136/bjsm.2009.058255. [DOI] [PubMed] [Google Scholar]
- 8.Alla S, Sullivan SJ, Hale L, McCrory P. Self-report scales/checklists for the measurement of concussion symptoms: a systematic review. Br J Sport Med. 2009;43((suppl 1)):i3–i12. doi: 10.1136/bjsm.2009.058339. [DOI] [PubMed] [Google Scholar]
- 9.McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport—the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sport Med. 2013;47(5):250–258. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- 10.Sady M, Vaughan C, Gioia G. School and the concussed youth—recommendations for concussion education and management. Phys Med Rehabil Clin N Am. 2001;22(4):701–719. doi: 10.1016/j.pmr.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guskiewicz KM, Bruce SL, Cantu R, et al. National Athletic Trainers' Association position statement: management of sport-related concussion. J Athl Train. 2004;39(3):280–297. [PMC free article] [PubMed] [Google Scholar]
- 12.Meehan WP, III, d'Hemecourt P, Collins CL, Comstock RD. Assessment and management of sport-related concussions in United States high schools. Am J Sport Med. 2011;39(11):2304–2310. doi: 10.1177/0363546511423503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moser RS, Glatts C, Schatz P. Efficacy of immediate and delayed cognitive and physical rest for treatment of sports-related concussion. J Pediatr. 2012;161(5):922–926. doi: 10.1016/j.jpeds.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 14.McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport. PM R. 2009;1(5):406–420. doi: 10.1016/j.pmrj.2009.03.010. the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. [DOI] [PubMed] [Google Scholar]
- 15.Moser RS, Schatz P. A case for mental and physical rest in youth sports concussion: it's never too late. Front Neurol. 2012;3:171. doi: 10.3389/fneur.2012.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. Sport Med Update. 2004;38:369–371. doi: 10.1001/jama.290.19.2556. [DOI] [PubMed] [Google Scholar]
- 17.Bey T, Ostick B. Second impact syndrome. West J Emerg Med. 2009;10(1):6–10. [PMC free article] [PubMed] [Google Scholar]
- 18.The National Center for Learning Disabilities Web site. http://www.ncld.org/ Accessed June 6, 2013. [Google Scholar]
- 19.Valovich McLeod TC, Bliven KC, Lam KC, Bay RC, Valier AR, Parsons JT. The National Sports Safety in Secondary Schools Benchmark (N4SB) Study: defining athletic training practice characteristics. J Athl Train. 2013;48(4):483–492. doi: 10.4085/1062-6050-48.4.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Portney LG, Watkins MP. In: Foundations of Clinical Research: Application to Practice. 3rd ed. Hall; Prentice., editor. Upper Saddle River, NJ: Pearson; 2009. [Google Scholar]
- 21.Duggan PS, Geller G, Cooper LA, Beach MC. The moral nature of patient-centeredness: is it “just the right thing to do”? Patient Educ Couns. 2006;62(2):271–276. doi: 10.1016/j.pec.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 22.Buzzini SR, Guskiewicz KM. Sports-related concussion in the young athlete. Curr Opin Pediatr. 2006;18(4):376–382. doi: 10.1097/01.mop.0000236385.26284.ec. [DOI] [PubMed] [Google Scholar]
- 23.Piebes SK, Gourley M. Valovich McLeod TC. Caring for student athlete following concussion. J Sch Nurs. 2009;25(4):270–281. doi: 10.1177/1059840509339782. [DOI] [PubMed] [Google Scholar]
- 24.Kaloir L. What's a 504 plan? National Center for Learning Disabilities Web site. 2013 http://www.ncld.org/learning-disability-resources/videos/video-what-is-a-504-plan. Accessed June 6. [Google Scholar]
- 25.National Center for Learning Disabilities Web site. What is an IEP. http://www.ncld.org/students-disabilities/iep-504-plan/what-is-iep. Accessed June 6, 2013. [Google Scholar]
- 26.Disabilities Rights Center Web site. Individualized education Programs (IEP) and 504 plans: what's the difference. http://www.drcnh.org/IDEA504.pdf. Updated May 2, 2008. Accessed June 6, 2013. [Google Scholar]
- 27.Kirkwood MW, Yeates KO, Wilson PW. Pediatric sport-related concussion: a review of the clinical management of an oft-neglected population. Pediatrics. 2006;117(4):1359–1371. doi: 10.1542/peds.2005-0994. [DOI] [PubMed] [Google Scholar]
- 28.Mensch J, Crews C, Mitchell M. Competing perspectives during organizational socialization on the role of certified athletic trainers in high school settings. J Athl Train. 2005;40(4):333–340. [PMC free article] [PubMed] [Google Scholar]
- 29.Cochrane LJ, Olson CA, Murray S, Dupuis M, Tooman T, Hayes S. Gaps between knowing and doing: understanding and assessing the barriers to optimal health care. J Contin Educ Health. 2007;27(2):94–102. doi: 10.1002/chp.106. [DOI] [PubMed] [Google Scholar]
- 30.Mazerolle SM, Scruggs IC, Casa DJ, et al. Current knowledge, attitudes, and practices of certified athletic trainers regarding recognition and treatment of exertional heat stroke. J Athl Train. 2010;45(2):170–180. doi: 10.4085/1062-6050-45.2.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Standards for the accreditation of professional athletic training programs. Commission on Accreditation of Athletic Training Education Web site. 2012 Updated October 31, 2013. Accessed June 6, 2013. [Google Scholar]
- 32.Athletic training education competencies. 5th edition. National Athletic Trainers' Association Web site. 20112013 http://caate.occutrain.net/wp-content/uploads/2013/04/5th-Edition-Competencies.pdf. Accessed June 6. [Google Scholar]