Abstract
Objective:
To present the case of 2 adolescent high school student-athletes who developed postconcussion syndrome with protracted and limiting visual complaints that markedly affected academic, social, and athletic activity for a year after the onset of symptoms. Both had significant improvement soon after a unique intervention was administered.
Background:
A 14-year-old female soccer and softball player sustained 2 concussions in the same week. She had persistent symptoms for a year that affected her grades and precluded athletic participation. A 15-year-old male football player sustained a concussion during an altercation with 2 other male adolescents. He continued to have symptoms 1 year later, with a marked decrease in academic performance and restriction from athletics. Both adolescents reported blurry vision, photophobia, and associated headache as significant components of the postconcussion syndrome.
Differential Diagnosis:
Concussion, postconcussion syndrome, skull fracture, subdural hematoma, epidural hematoma, second-impact syndrome, and visually sensitive migraine.
Treatment:
Both patients were advised to obtain computer gaming glasses to use throughout the day. The female patient was diligent in her use of the glasses, with marked lessening of symptoms. The male patient was less accepting of the glasses but did report lessening of symptoms when using the glasses.
Uniqueness:
We hypothesized that postconcussion syndrome with marked visual complaints would respond to and improve with decreased stimulation of the visual system. This was attempted with the addition of computer gaming glasses. Both adolescent athletes responded well to the filtering of visual stimuli by off-the-shelf computer gaming glasses.
Conclusions:
Postconcussion syndrome is a persistent condition with a myriad of symptoms. Two young athletes developed postconcussion syndrome with prominent visual symptoms that lasted a year. The addition of computer gaming glasses markedly lessened symptoms in both patients.
Key Words: traumatic brain injuries, computer glasses, gaming glasses
A concussion is a traumatically induced alteration in brain function1–4 that can be summarized as a disorder of information processing. Concussions are brain injuries that are considered functional and diffuse in nature, rather than structural, as in mild traumatic brain injuries (mTBIs). Concussions occur frequently within the sporting arena, with the incidence varying among sports.5
These patients have a wide array of symptoms: headaches, dizziness and vertigo, difficulty concentrating, amnesia, difficulty sleeping, light sensitivity, depression, irritability, word-finding difficulty, and impulsiveness.6,7 Feeling slowed down or foggy and having difficulty concentrating are often prominent symptoms during the first week after a concussion.6 The assortment of clinical symptoms that occur in individuals with concussion or postconcussion syndrome has not correlated well with the mechanism of injury or the cellular pathophysiology.
Symptoms generally resolve within 21 days, with the majority of concussions resolving in 7 to 10 days.8,9 High school athletes are thought to require a longer recovery time than collegiate athletes.9–11 Treatment options are limited, with mainstream recommendations emphasizing physical and cognitive rest,9 but there is even some question as to the efficacy or necessity of the prescribed rest.11,12
A significant percentage of patients diagnosed with concussions have persistent symptoms.8,13 Ten percent to 20% of concussed patients have symptoms that last longer than 2 weeks, whereas approximately 2% have symptoms that last weeks to months.14,15 The incidence may be higher in emergency room patients presenting with concussion.16
The purpose of this article is to report on a novel intervention using computer gaming glasses with 2 adolescents who had postconcussion syndrome.
CASE REPORT
Patient 1
A 14-year-old female soccer goalie in the regional Olympic Development Program sustained 2 concussions in the same week. The first occurred on October 17, 2011, while she was attempting a diving save. The ball struck low on the upright and rebounded against her head. She immediately felt dizzy with vertigo that lasted a couple of minutes. The initial assessment was performed by her pediatrician, who diagnosed a mild concussion. She had a normal physical examination. She was held from participation. She tried naproxen and ibuprofen for the headache, but symptoms did not abate. On October 21, 2011, she underwent Immediate Post-Concussion Assessment and Cognitive Testing ([ImPACT]; test version 2.1, ImPACT Applications, Inc, Pittsburgh, PA), which indicated a significant deficit (Table 1A).
Table 1A.
Patient 1's Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) Results
| Cognitive Function |
October 21, 2011 |
Percentile Score |
November 10, 2011 |
Percentile Score |
| Memory–verbal | 58 | <1 | 53 | <1 |
| Memory–visual | 53 | 5 | 56 | 7 |
| Visual motor speed | 32.45 | 17 | 31.55 | 16 |
| Reaction time | 0.59 | 48 | 0.64 | 26 |
| Impulse control | 9 | 9 | ||
| Total symptom score | 15 | 20 |
On October 22, while spectating at a softball game, she was struck in the back of the head by a poorly thrown softball. She had an immediate escalation of symptoms, which included diplopia, photophobia, nausea, and confusion that lasted a couple of minutes. The headache and photophobia persisted. A magnetic resonance imaging scan was obtained by the pediatrician on November 4, 2011, to rule out subdural hematoma, epidural hematoma, and skull fracture. The only significant finding was a small benign cyst. Rest was the initial treatment, but symptoms continued to escalate. She was started on cyproheptadine (Periactin, Merck & Co Inc, White House Station, NJ) by her pediatrician on November 8, 2011, at a dose of 4 mg 3 times per day. This first-generation antihistamine was tried because the headache history was suggestive of migraines. She was seen by a neurologist on November 9, 2011, with another assessment of a normal physical examination. She was given the diagnoses of postconcussion headache and a benign pineal cyst. A second ImPACT test was obtained the following day and showed a continued deficit (Table 1A).
Due to the persistent headaches, she was seen by a pediatric neurologist on November 28, 2011. Photophobia, daily headaches that worsened with reading, and trouble concentrating were noted at this visit. The physical examination remained normal. Topiramate (Topamax, Janssen Pharmaceuticals Inc, Titusville, NJ) was started at 25 mg each evening for 1 week, with an increase to 50 mg each evening thereafter. Topiramate was developed as an anticonvulsant but is also used in the treatment of migraine and as a mood stabilizer in bipolar disorder. Decreased vision has been reported as an adverse effect. A follow-up examination on February 20, 2012, reported no improvement in headaches, with continuing photophobia. The patient reported that blurred vision and dizziness often increased within a few hours of taking the topiramate. Continued lack of improvement was noted on April 4, 2012, so topiramate was discontinued.
Amitryptiline (Elavil, AstraZeneca Pharmaceuticals, London, UK) was substituted at 10 mg each morning and 20 mg each evening. Amitryptiline is a tricyclic antidepressant that has also been used with success in several chronic neurologic conditions. At follow-up examination on June 15, 2012, the patient reported a lack of improvement in symptoms. Neurologic examination demonstrated an inability to recite the months backward and remember 1 of 3 items at 5 minutes. The headaches were prominent enough to warrant the addition of Fioricet (Actavis Pharma, Inc, Parsippany, NJ) on an as-needed basis. Amitryptiline was titrated to 25 mg twice a day at the subsequent follow-up appointment on August 15, 2012. Daily symptoms continued, however, so amitryptiline was discontinued on September 15, 2012. No medications were substituted.
The patient's school attendance suffered during this time frame. Due to continued headaches and photophobia, she started attending school (8th grade) only for the initial half of the day in January 2012. She remained on half days through June 2012, missing an additional 26 mornings due to symptoms and 9 for physician appointments. She returned to full days of school in August 2012 primarily because she was entering high school. She continued to have daily symptoms and would have to lie down for extended periods once arriving home in the afternoon. She missed 3 half days and 3 full days of school from late August through October 2012, with an additional 4 half days for physician appointments.
The athletic trainer and senior author (S.S.G.) was introduced to the patient approximately 1 year after the injury. Her symptoms were unrelenting and incessant. She was having persistent academic and social difficulties. She reported that the older classrooms with fluorescent lights, some computer monitors, and iPad screens increased her symptoms.
On a cursory Internet search, the senior author uncovered some brief reports of patient improvement with changes in light bulb types or the use of tinted lenses. There were also reports of similar modifications to treat migraines and epilepsy. The athletic trainer reasoned that a similar modification could be helpful with the visual symptoms occurring in this patient, but a change of lighting could not be accomplished in the school setting. An alternate solution was to add filtering at the eye, given that all other available treatments had been exhausted.
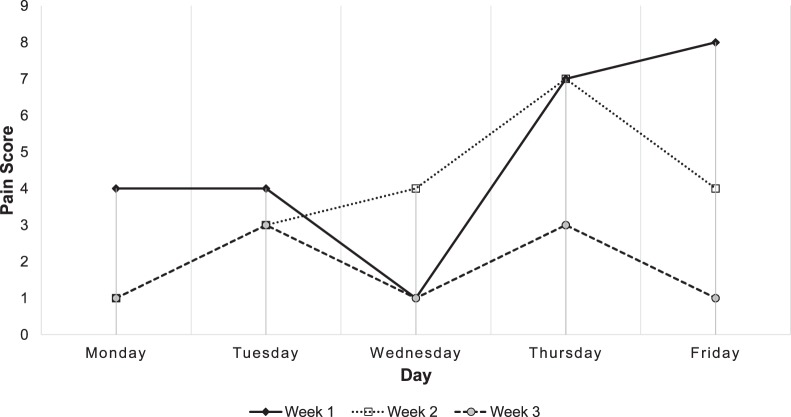
Computer gaming glasses (Gunnar Optiks, Rancho Santa Fe, CA) were added to the patient's treatment regimen approximately 1 year postinjury in an attempt to lessen cortical stimulation. She ordered and received the glasses via mail in early October 2012. She used them sporadically over 1 weekend and noticed some lessening of photophobia and headaches. She began wearing the glasses full time on October 15, 2012. The glasses reduced her symptoms, as evidenced by the self-report symptom survey completed daily over a 3-week period (Figure 1). Her school attendance improved and she remained on full-day attendance, with 14 half days missed and 5 physician appointments over the next 5 months. Her academic performance also strengthened.
Figure 1.
Three-week symptom self-report survey using gaming glasses. Note: glasses were not worn on Thursdays as an internal control. Pain Score Scale range = 1–10.
She was seen by a sports-trained neurologist on December 13, 2012. Occasional sensitivity to light and mild daily headaches were still reported, but symptoms were noted to be significantly improved. The neurologist commented that the patient credited the use of computer gaming glasses for improvement. The physical examination was normal. A diagnosis of postconcussion syndrome was given and the restriction from activity was continued. Repeat magnetic resonance imaging was obtained on December 18, 2012; a pineal cyst was the only diagnosis. At a follow-up visit with the sports neurologist on January 17, 2013, continued improvement was reported. The athlete had started playing tennis on her own and was symptom free while doing so.
Six months after the addition of the computer gaming glasses, she was released by the neurologist to begin batting and running for softball. She is doing well in school. She continues to have episodes of photosensitivity with bright stadium lights but is able to play when she wears sunglasses.
Patient 2
A 15-year-old male football player was involved in an altercation with 2 other male adolescents during September 2011. He received numerous blows to the head during the mugging. His persistent headache, eye fatigue, and difficulty reading caused a great deal of trouble with academics. He was prescribed several different medications to reduce symptoms during the initial months, but each was discontinued due to adverse effects. He was eventually relegated to remedial classes for the school period starting in January 2012.
In the summer of 2012, he transferred to a new school. He joined the football team without reporting the injury history or the ongoing symptoms. Two weeks into the practice season, the senior author (S.S.G.) interacted with the young man and obtained the injury history. He was held from participation and an ImPACT test was obtained (Table 1B). He obtained a pair of computer gaming glasses (Gunnar Optiks) in November 2012 but wore them sporadically during the school day due to the distinctive appearance of the glasses. He was not taking any medications when the gaming glasses were introduced. He reported wearing the glasses frequently on weekends because they improved his symptoms. He had increasing resolution of symptoms and was cleared by his physician to return to football participation in August 2013.
Table 1B.
Patient 2's Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) Results
| Cognitive Function |
August 15, 2012 |
Percentile Score |
| Memory–verbal | 63 | 3 |
| Memory–visual | 48 | 2 |
| Visual motor speed | 26.38 | 2 |
| Reaction time | 0.62 | 31 |
| Impulse control | 6 | |
| Total symptom score | 35 |
DISCUSSION
Cerebral concussions involve a cascade of metabolic changes that occur at the cellular level.17 The initial injury causes a change in membrane permeability, resulting in abnormal distribution of ions across the axon and excessive excitatory neurotransmitter release. The restoration of normal ion and neurotransmitter distribution and concentration requires a great deal of cellular energy from adenosine triphosphate to power the sodium-potassium pump. This requires increased glucose metabolism to support the accelerated energy demand.17
Other cell components begin to malfunction later in the cascade. Increased intracellular calcium concentration results in mitochondrial dysfunction, worsening the energy crisis. The calcium increase also disrupts neurofilaments and microtubules, impairing neural connectivity.17 The altered cellular homeostasis accompanies the energy imbalance.8 As clinical symptoms resolve, it is presumed that homeostasis is re-established at the cellular level. Failure to restore homeostasis may cause postconcussion syndrome.
A large assortment of symptoms can occur with postconcussion syndrome. However, it seems a limited range of symptoms are prognostic for it. Amnesia seems only to be predictive of prolonged postconcussion sequelae in athletes.16,18 The presence of dizziness is a significant on-field predictor of protracted recovery in high school football players.19 Athletes who develop postconcussion syndrome typically have increased symptoms early in the episode that continue throughout the duration of the concussion.14,18
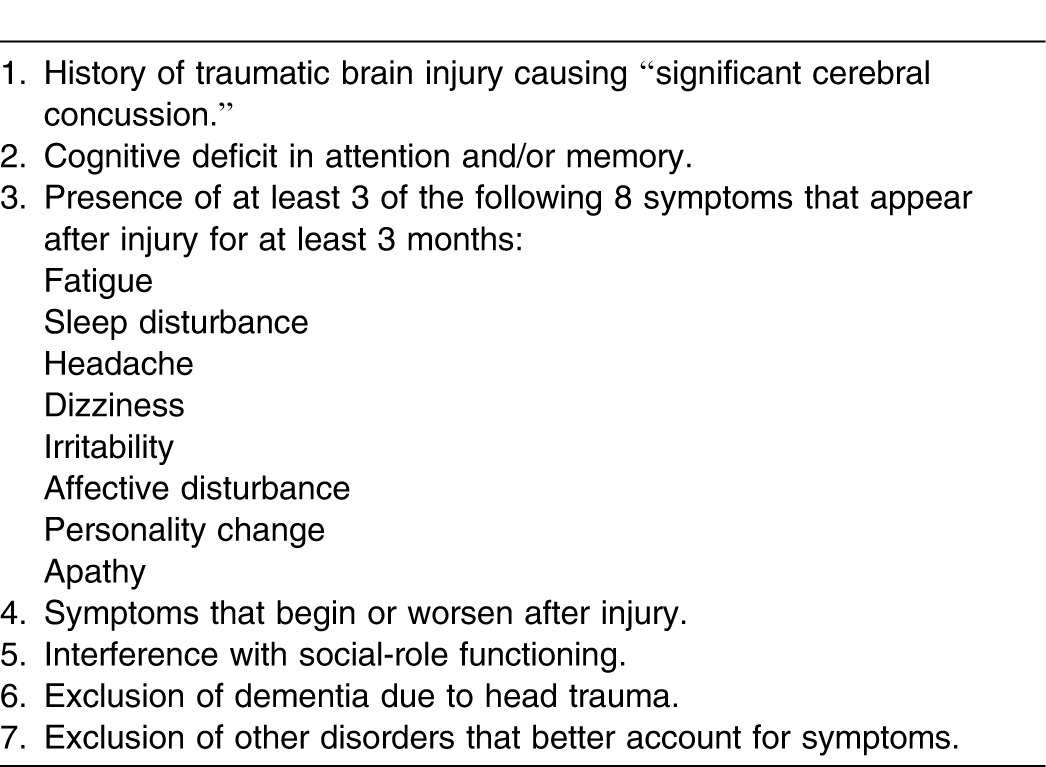
Diagnostic criteria for postconcussion syndrome have been established in both the International Statistical Classification of Diseases, 10th Revision (ICD-10)20 and the Diagnostic and Statistical Manual of Mental Disorders (4th edition) (DSM-IV)21 (Tables 2 and 3). The use of the ICD-10 criteria will result in the diagnosis of more postconcussion syndrome cases.22
Table 2.
Clinical Criteria for Postconcussion Syndrome According to the International Statistical Classification of Diseases, 10th Revision20
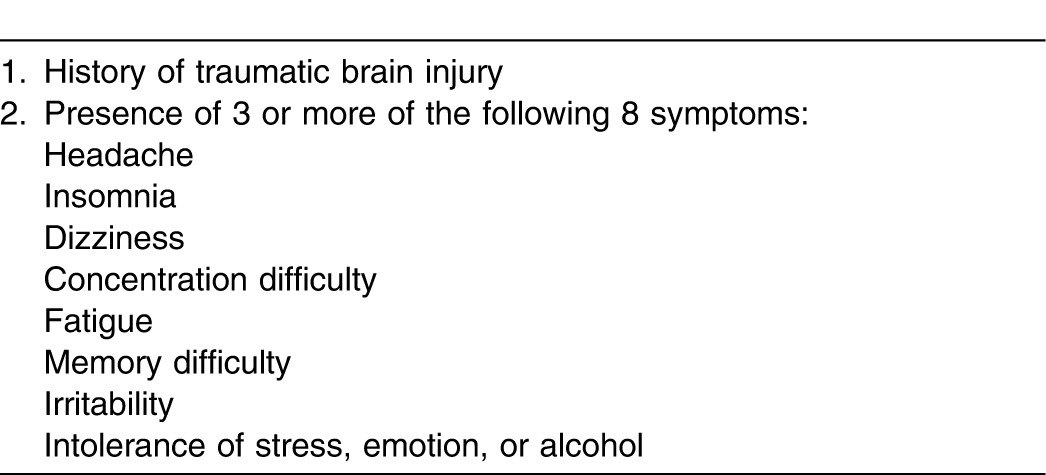
Table 3.
Criteria for Postconcussion Syndrome According to the Diagnostic and Statistical Manual of Mental Disorders21
The wide array of symptoms in concussion and postconcussion syndromes has sparked consideration of subtypes in both conditions and prompted attempts to group symptoms.7,23–25 These subtypes are most commonly grouped into some version of 3 categories: cognitive, somatic, and emotional/behavioral symptoms.7,23,24 Subsequent treatment may be tailored to the particular classification or symptom complex an individual patient is experiencing. We believe the treatment of visual symptoms will be 1 of these differentiations.
Visual Symptoms in Concussion
Both of these patients had visual symptoms as a strong component of the postconcussion syndrome. Visual changes, including increased photosensitivity and photophobia, have been reported in concussion patients.26–31 Visual symptoms are included in 1 of the 3 categories often used to describe proposed subtypes of concussion, though visual symptoms may be placed in the cognitive or somatic category.26–31
Patients with closed-head injuries were less tolerant of luminance (brightness) than control participants at 1366 lux (a measure of lumens per square meter; 1 foot candle = 11 lux) versus 1783 lux.26 In a study using resting-state functional magnetic resonance imaging in patients with closed-head injuries and matched controls, a cluster of increased functional connectivity in the right frontoparietal network was noted in the injured group. This may cause increased awareness of the external environment, resulting in cognitive fatigue with headache and increased sensitivity to noise and light.32
Visual dysfunction has also been documented in soldiers with mTBI during the subacute stage after blast injuries.30 Forty soldiers were matched and evaluated, with 20 having sustained mTBI after a blast injury. All 40 soldiers had normal high-contrast visual acuity, color vision, and overall ocular health. However, soldiers with mTBI showed oculomotor deficits in vergence, version, and accommodation (alignment, tracking, and focusing). They also displayed deficits in reading speed and comprehension when compared with the matched controls.30 The authors suggested that patients with mTBI receive functional vision examinations with an emphasis on near oculomotor function. This assessment includes the components of near lateral and vertical phorias (misalignment) and saccades. Photosensitivity was thought to be particularly important.30
Vertical heterophoria has been documented in some postconcussion patients.31 This is a misalignment in which the line of sight of 1 eye is higher than the other when at physiologic rest, causing diplopia.31 Patients with vertical heterophoria excessively use the levator and depressor extraocular muscles to realign the line of sight and maintain a fused image, avoiding diplopia.31 The muscle fatigue that occurs contributes to symptoms. The utricle and brainstem are likely areas of involvement for the faulty alignment signal.31 Treatment of this condition involves the use of prismatic lenses.31
Visuospatial attention deficits are demonstrable in some patients with concussion.27,33 Visuospatial attention can be separated into alerting, orienting, and executive components. The alerting component functions to maintain vigilance throughout performance of a continuous task—a new stimulus appears in a region of the visual field. The orienting component facilitates shifts of attentional resources to a desired spatial location to allow increased speed of perception of targets appearing in that space—a stimulus is followed through the visual field. The executive component involves the capacity to efficiently switch between tasks and resolve conflict. Deficits in both the orienting and executive components were found early (at 24–48 hours) and late (at 1–2 months) in patients postconcussion.27,33 The deficits in the orienting component were mild, but the executive component was substantially affected.27 The orienting deficit implies that regions of the superior parietal lobule, intraparietal sulcus of the posterior parietal cortex, and cingulate gyrus may be involved in the injury. The deficit in the executive component suggests involvement of the anterior cingulate cortex.27,33
Eye-movement function also has been found to be impaired in postconcussion patients at 3 to 5 months after injury.29 Saccades are small movements of the eyes to fix the target object onto the fovea, allowing detailed visual assessment. The worsened eye-movement performance was associated with increased symptoms. Several of the eye-movement deficits are not under conscious control, indicating subcortical involvement. The poor results on self-paced saccades suggest visuospatial attention deficits, consistent with the findings of Halterman et al.27 The high number of directional errors indicates poor function in the prefrontal cortical areas, consistent with the results of neuropsychological testing.29 The use of the increasingly popular King-Devick test in concussion assessment is predicated upon deleterious effects on saccadic eye movement.34–36
Brain pathways for saccades are widely distributed through the frontal eye fields, dorsolateral prefrontal cortex (DLPFC), parietal lobes, and the brainstem. The DLPFC has been suggested as the highest cortical area responsible for motor planning and working memory, indicating a common link between the eye-movement symptoms and memory-related deficits in patients with concussion.35 In particular, the DLPFC has been linked with anticipatory saccades, a type of eye movement necessary in rapid number-naming tasks such as the King-Devick test. That test requires saccades, as well as concentration and language function, for successful performance.36
Computer Vision Syndrome
Computer vision syndrome is thought to occur in 75% of computer workers who view a video display for 6 to 9 hours per day.37 The syndrome comprises ocular complaints that include eye fatigue, burning, redness, blurred vision, and dry eyes, as well as nonocular symptoms, such as headache, neck pain, and shoulder pain.37
Most people blink 10 to 15 times per minute. The blink rate while using a computer is significantly reduced. This causes poor tear-film quality that results in stress for the cornea and possibly some of the subsequent symptoms of computer vision syndrome.37
Prolonged use of a video display can cause a transient deviation of phoria (visual alignment), transient myopia, and a diminished power of accommodation.37 Screen resolution and refresh rates of the video display affect the incidence of computer vision syndrome. Low refresh rates of 8 to 14 Hz can induce epileptogenic seizures. Flicker of the video display can be evident with refresh rates less than 30 to 50 Hz. Therefore, minimum refresh rates are recommended to be above 75 Hz.37 Refresh rates at 300 Hz or above shortened blink time, lengthened blink duration, and improved accommodation and saccadic accuracy.37,38 Computer glasses decreased symptoms in those with computer vision syndrome37 and have improved worker productivity.37,39,40
Photosensitive Epilepsy
Approximately 5% of patients with epilepsy are photosensitive. Four percent to 8% of the general population is photosensitive without having epilepsy—a phenomenon termed photoparoxysmal responsiveness—with the peak incidence at puberty. Strong photic stimulation may cause seizures in these patients, but they will not go on to develop epilepsy.41 Perhaps the most famous example is the December 1997 television episode of the cartoon “Pokémon” that caused seizures in 103 patients.42
Two pathophysiologic mechanisms are involved in the photoparoxysmal response. The first is a wavelength-dependent mechanism. The response is elicited with a flashing red light greater than ∼700 nm, which activates only L cones.41 The other mechanism is independent of the wavelength and depends only on the quantity of flashing light. Optical filters have been shown to reduce the incidence of both photoparoxysmal responses41 and photosensitive epileptic seizures.41,43
Visually Sensitive Migraine
Approximately 8% of adults experience migraine headaches.44 Photophobia accompanies most migraine attacks, perhaps as many as 90%, in patients with and without aura.45 Various visual stimuli can trigger an attack. The most common visual trigger is pattern glare (ie, certain patterns of stripes). It is unclear how many migraine patients have visual abnormalities.45 Several studies43–45 have suggested visual deficits, but not all are considered reliable. These studies43–45 have supported cortical hyperexcitability. Tinted lenses decreased the incidence of migraine, though with marginal statistical significance.44,45 It has been postulated that the colored lenses redistribute the cortical excitation that results from visual processes, particularly when the excitation is strong, such as in pattern glare.45
A Unique Intervention
As we delved into the medical literature, it became apparent that subcortical mechanisms are involved in several pathologic entities affecting the visual system, as described in the previous section. This lent support to the original hypothesis that filtering visual stimuli could provide relief in patients with postconcussion syndrome who had prominent visual complaints.
Computer gaming glasses are popular appliances used by enthusiasts of the increasingly popular massive multiplayer role games (eg, Halo, Worlds of Warcraft) and by workers who use computers on a continuous basis. An Amazon (www.amazon.com) search in December 2013 displayed several hundred options for computer gaming glasses. These glasses weigh between 14 and 18 ounces (397 and 510 grams), depending on the frame style. All use lenses with tinting, ultraviolet protection, or polarization to narrow the spectrum of light entering the eye. Various frame styles are available, but the lens is the critical component for the desired effects on the visual system. Although authors37,39,40 have investigated the effects of the glasses on clinical symptoms and worker productivity, to our knowledge, no one has described the neural mechanism for these effects.
The brand of glasses (Gunnar Optiks) we chose seemed to have the highest quality with the best pricing (Figure 2). The frame style was left to each patient's preference to increase the likelihood of use. This brand of computer gaming glasses has a patented amber tint that filters from nearly 100% of blue light at 400 nm to 45% of blue light in the 450-nm wavelength. Blue light in the 400- to 450-nm–wavelength range activates S cones in the retina. The focal area has a flatter and wider midpoint, lessening the need for accommodation (focusing) at a distance of 20 to 24 in (51 to 61 cm), the typical viewing distance for a computer monitor.
Figure 2.

Computer gaming glasses (Gunnar Optiks, Rancho Santa Fe, CA).
The current recommendations for treatment of concussion involve physical and cognitive rest on the presumption that decreased stimuli will allow restoration of cellular homeostasis within the neural tissue. We suggest that adding computer gaming glasses to the treatment of postconcussion syndrome in individuals with prominent visual symptoms follows this line of reasoning. The literature documents visual dysfunction at the subcortical level in patients with concussion and postconcussion syndrome. Decreasing the stimulation of these tissues may allow successful restoration of homeostasis within the system. The filtering of blue light may lessen the stimulation of the visual cortex by decreasing activation of the S cones.
CONCLUSIONS
The human visual system processes a great deal of information. It responds to a cacophony of color while assessing the external surroundings, interpreting a wide variety of lines, shapes, and movements to construct a valid interpretation of the environment. Concussions can be considered a disorder of information processing. Visual symptoms are a common occurrence in concussion, but some patients have significantly more visual complaints.
Patients with concussion and postconcussion syndrome have a wide variety of symptoms. The symptom complex may vary among individuals because the injury forces have unique vectors that traverse different parts of the brain. The visual system is located throughout the brain, from the retina and optic chiasm anteriorly to the posterior occipital cortex. As a result, injury forces associated with mTBI and concussion are likely to affect some of the structures of the visual system.
Classically, concussions have been assessed via tests of cognitive function. The various neuropsychological tests are composed of scales that assess the function of different areas of the brain. For example, the Balance Error Scoring System is a popular assessment of concussion, focusing on the ability to balance through motor function.46 The increasingly popular King-Devick test uses a simple timed test to assess visual saccades as well as concentration and language function in patients with concussions. The wide variety of symptoms and natural history of concussions are likely to be due in part to the large number of brain structures that can be affected by the injury forces.
We propose that patients with postconcussion syndrome who have notable visual symptoms can benefit from using gaming glasses to reduce the stimuli reaching the visual cortex. However, our small case series is in no way a definitive investigation. We believe the success of this simple intervention in our 2 young athletes warrants further investigation by additional researchers on a larger scale. Patients with concussions should be investigated for a variety of oculomotor deficits to establish the incidence, prevalence, and timing of such visual signs. A subset of patients may be identified who can benefit from the addition of these specialized and readily available lenses.
REFERENCES
- 1.Giza CC, Kutcher JS, Ashwal S, et al. Summary of evidence-based guideline update: evaluation and management of concussion in sports: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2013;80(24):2250–2257. doi: 10.1212/WNL.0b013e31828d57dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harmon KG, Drezner JA, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47(1):15–26. doi: 10.1136/bjsports-2012-091941. [DOI] [PubMed] [Google Scholar]
- 3.McCrory P, Meeuwisse W, Aubry M, et al. Consensus statement on concussion in sport—the 4th International Conference on Concussion in Sport held in Zurich, November 2012. Clin J Sport Med. 2013;23(2):89–117. doi: 10.1097/JSM.0b013e31828b67cf. [DOI] [PubMed] [Google Scholar]
- 4.Halstead ME, Walter KD. Council on Sports Medicine and Fitness; American Academy of Pediatrics. Clinical report: sport-related concussion in children and adolescents. Pediatrics. 2010;126(3):597–615. doi: 10.1542/peds.2010-2005. [DOI] [PubMed] [Google Scholar]
- 5.Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among United States high school athletes in 20 sports. Am J Sports Med. 2012;40(4):747–755. doi: 10.1177/0363546511435626. [DOI] [PubMed] [Google Scholar]
- 6.Kontos AP, Elbin RJ, Shatz P, et al. A revised factor structure for the Post-Concussion Symptom Scale: baseline and postconcussion factors. Am J Sports Med. 2012;40(10):2375–2384. doi: 10.1177/0363546512455400. [DOI] [PubMed] [Google Scholar]
- 7.DeKosky ST, Ikonomovic MD, Gandy S. Traumatic brain injury: football, warfare, and long-term effects. N Engl J Med. 2010;363(14):1293–1296. doi: 10.1056/NEJMp1007051. [DOI] [PubMed] [Google Scholar]
- 8.McCrory P, Meeuwisse WH, Echemendia RJ, Iversen GL, Dvorak J, Kutcher JS. What is the lowest threshold to make a diagnosis of concussion? Br J Sports Med. 2013;47(5):268–271. doi: 10.1136/bjsports-2013-092247. [DOI] [PubMed] [Google Scholar]
- 9.Moser RS, Glatts C, Schatz P. Efficacy of immediate and delayed cognitive and physical rest for treatment of sports-related concussion. J Pediatr. 2012;161(5):922–926. doi: 10.1016/j.jpeds.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 10.Field M, Collins MW, Lovell MR, Maroon J. Does age play a role in recovery from sports-related concussion? A comparison of high school and collegiate athletes. J Pediatr. 2003;142(5):546–553. doi: 10.1067/mpd.2003.190. [DOI] [PubMed] [Google Scholar]
- 11.Majerske CW, Mihalik JP, Ren D, et al. Concussion in sports: postconcussive activity levels, symptoms, and neurocognitive performance. J Athl Train. 2008;43(3):265–274. doi: 10.4085/1062-6050-43.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kirkwood MW, Randolph C, Yeates KO. Sport-related concussion: a call for evidence and perspective amidst the alarms. Clin J Sport Med. 2012;22(5):383–384. doi: 10.1097/JSM.0b013e31826396fc. [DOI] [PubMed] [Google Scholar]
- 13.Bohnen N, Twijnstra A, Jolles J. Persistence of postconcussional symptoms in uncomplicated mildly head-injured patients: a prospective cohort study. Neuropsychiatry Neuropsychol Behav Neurol. 1993;6(3):193–200. [Google Scholar]
- 14.McCrea M, Guskiewicz K, Randolph C, et al. Incidence, clinical course, and predictors of prolonged recovery time following sport-related concussion in high school and college athletes. J Int Neuropsychol Soc. 2013;19(1):22–33. doi: 10.1017/S1355617712000872. [DOI] [PubMed] [Google Scholar]
- 15.Makdissi M, Darby D, Maruff P, Ugoni A, Brukner P, McCrory PR. Natural history of concussion in sport: markers of severity and implications for management. Am J Sports Med. 2010;38(3):464–471. doi: 10.1177/0363546509349491. [DOI] [PubMed] [Google Scholar]
- 16.Bazarian JJ, Wong T, Harris M, Leahey N, Mookerjee S, Dombovy M. Epidemiology and predictors of post-concussive syndrome after minor head injury in an emergency population. Brain Inj. 1999;13(3):173–189. doi: 10.1080/026990599121692. [DOI] [PubMed] [Google Scholar]
- 17.Giza CC, Hovda DA. The neurometabolic cascade of concussion. J Athl Train. 2001;36(3):228–235. [PMC free article] [PubMed] [Google Scholar]
- 18.Collins MW, Iverson GL, Lovell MR, McKeag DB, Norwig J, Maroon J. On-field predictors of neuropsychological and symptom deficit following sports-related concussion. Clin J Sport Med. 2003;13(4):222–229. doi: 10.1097/00042752-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 19.Lau BC, Kontos AP, Collins MW, Mucha A, Lovell MR. Which on-field signs/symptoms predict protracted recovery from sport-related concussion among high school football players? Am J Sports Med. 2011;39(11):2311–2318. doi: 10.1177/0363546511410655. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva, Switzerland: World Health Organization;; 1992. [Google Scholar]
- 21.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association;; 1994. [Google Scholar]
- 22.Boake C, McCauley SR, Levin HS, et al. Diagnostic criteria for postconcussional syndrome after mild to moderate traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2005;17(3):350–356. doi: 10.1176/jnp.17.3.350. [DOI] [PubMed] [Google Scholar]
- 23.Piland SG, Motl RW, Guskiewicz KM, McCrea M, Ferrara MS. Structural validity of a self-report concussion-related symptom scale. Med Sci Sports Exerc. 2006;38(1):27–32. doi: 10.1249/01.mss.0000183186.98212.d5. [DOI] [PubMed] [Google Scholar]
- 24.Potter S, Leigh E, Wade D, Fleminger S. The Rivermead Post Concussion Symptoms Questionnaire: a confirmatory factor analysis. J Neurol. 2006;253(12):1603–1614. doi: 10.1007/s00415-006-0275-z. [DOI] [PubMed] [Google Scholar]
- 25.Cicerone KD, Kalmar K. Persistent postconcussion syndrome: the structure of subjective complaints after mild traumatic brain injury. J Head Trauma Rehabil. 1995;10(3):1–17. [Google Scholar]
- 26.Waddell PA, Gronwall DM. Sensitivity to light and sound following minor head injury. Acta Neurol Scand. 1984;69(5):270–276. doi: 10.1111/j.1600-0404.1984.tb07812.x. [DOI] [PubMed] [Google Scholar]
- 27.Halterman CI, Langan J, Drew A, et al. Tracking the recovery of visuospatial attention deficits in mild traumatic brain injury. Brain. 2006;129((pt 3)):747–753. doi: 10.1093/brain/awh705. [DOI] [PubMed] [Google Scholar]
- 28.Stovner LJ, Schrader H, Mickeviciene D, Surkiene D, Sand T. Headache after concussion. Eur J Neurol. 2009;16(1):112–120. doi: 10.1111/j.1468-1331.2008.02363.x. [DOI] [PubMed] [Google Scholar]
- 29.Heitger MH, Jones RD, Macleod AD, Snell DL, Frampton CM, Anderson TJ. Impaired eye movements in post-concussion syndrome indicate suboptimal brain function beyond the influence of depression, malingering or intellectual ability. Brain. 2009;132((pt 10)):2850–2870. doi: 10.1093/brain/awp181. [DOI] [PubMed] [Google Scholar]
- 30.Capó-Aponte JE, Urosevich TG, Temme LA, Tarbett AK, Sanghera NK. Visual dysfunctions and symptoms during the subacute stage of blast-induced mild traumatic brain injury. Mil Med. 2012;177(7):804–813. doi: 10.7205/milmed-d-12-00061. [DOI] [PubMed] [Google Scholar]
- 31.Doble JE, Feinberg DL, Rosner MS, Rosner AJ. Identification of binocular vision dysfunction (vertical heterophoria) in traumatic brain injury patients and effects of individualized prismatic spectacle lenses in the treatment of postconcussive symptoms: a retrospective analysis. PM R. 2010;2(4):244–253. doi: 10.1016/j.pmrj.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 32.Shumskaya E, Andriessen TM, Norris DG, Vos PE. Abnormal whole-brain functional networks in homogeneous acute mild traumatic brain injury. Neurology. 2012;79(2):175–182. doi: 10.1212/WNL.0b013e31825f04fb. [DOI] [PubMed] [Google Scholar]
- 33.Howell D, Osternig L, Van Donkelaar P, Mayr U, Chou LS. Effects of concussion on attention and executive function in adolescents. Med Sci Sports Exerc. 2013;45(6):1030–1037. doi: 10.1249/MSS.0b013e3182814595. [DOI] [PubMed] [Google Scholar]
- 34.Galetta KM, Barret J, Allen M, et al. The King-Devick test as a determinant of head trauma and concussion in boxers and MMA fighters. Neurology. 2011;76(17):1456–1462. doi: 10.1212/WNL.0b013e31821184c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Galetta KM, Brandes LE, Maki K, et al. The King-Devick test and sports-related concussion: study of a rapid visual screening tool in a collegiate cohort. J Neurol Sci. 2011;309((1–2)):34–39. doi: 10.1016/j.jns.2011.07.039. [DOI] [PubMed] [Google Scholar]
- 36.Galetta MS, Galetta KM, McCrossin J, et al. Saccades and memory: baseline associations of the King-Devick and SCAT2 SAC tests in professional ice hockey players. J Neurol Sci. 2013;328((1–2)):28–31. doi: 10.1016/j.jns.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 37.Blehm C, Vishnu S, Khattak A, Mitra S, Yee RW. Computer vision syndrome: a review. Surv Ophthalmol. 2005;50(3):253–262. doi: 10.1016/j.survophthal.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 38.Gunnar Optiks Digital Performance Eyewear Market Test. 2012 Gunnar Web site. http://www.gunnars.com/b2b/gunnar-optiks-digital-performance-eyewear-market-test/. Published December 11. Accessed February 21, 2014. [Google Scholar]
- 39.Worker productivity and computer vision. 2012 Gunnar Web site. http://www.gunnars.com/b2b/worker-productivity-computer-vision/. Published December 3. Accessed February 21, 2014. [Google Scholar]
- 40.Daum KM, Clore KA, Simms SS, et al. Productivity associated with visual status of computer users. Optometry. 2004;75(1):33–47. doi: 10.1016/s1529-1839(04)70009-3. [DOI] [PubMed] [Google Scholar]
- 41.Takahashi Y, Sato T, Goto K, et al. Optical filters inhibiting television-induced photosensitive seizures. Neurology. 2001;57(10):1767–1773. doi: 10.1212/wnl.57.10.1767. [DOI] [PubMed] [Google Scholar]
- 42.Okumura A, Watanabe K, Ishikawa T. Five years after the “Pocket Monster” seizures. N Engl J Med. 2004;351(4):403–404. doi: 10.1056/NEJM200407223510424. [DOI] [PubMed] [Google Scholar]
- 43.Wilkins AJ, Baker A, Amin D, et al. Treatment of photosensitive epilepsy using coloured glasses. Seizure. 1999;8(8):444–449. doi: 10.1053/seiz.1999.0337. [DOI] [PubMed] [Google Scholar]
- 44.Evans BJ, Patel R, Wilkins AJ. Optometric function in visually sensitive migraine before and after treatment with tinted spectacles. Ophthalmic Physiol Opt. 2002;22(2):130–142. doi: 10.1046/j.1475-1313.2002.00017.x. [DOI] [PubMed] [Google Scholar]
- 45.Wilkins AJ, Patel R, Adjamian P, Evans BJ. Tinted spectacles and visually sensitive migraine. Cephalalgia. 2002;22(9):711–719. doi: 10.1046/j.1468-2982.2002.00362.x. [DOI] [PubMed] [Google Scholar]
- 46.Riemann BL, Guskiewicz KM. Effects of mild head injury on postural stability as measured through clinical balance testing. J Athl Train. 2000;35(1):19–25. [PMC free article] [PubMed] [Google Scholar]