Abstract
Context:
Muscle fatigue due to repetitive and prolonged overhead sports activity is considered an important factor contributing to impingement-related rotator cuff pathologic conditions in overhead athletes. The evidence on scapular and glenohumeral kinematic changes after fatigue is contradicting and prohibits conclusions about how shoulder muscle fatigue affects acromiohumeral distance.
Objective:
To investigate the effect of a fatigue protocol resembling overhead sports activity on acromiohumeral distance and 3-dimensional scapular position in overhead athletes.
Design:
Cross-sectional study.
Setting:
Institutional laboratory.
Patients or Other Participants:
A total of 29 healthy recreational overhead athletes (14 men, 15 women; age = 22.23 ± 2.82 years, height = 178.3 ± 7.8 cm, mass = 71.6 ± 9.5 kg).
Intervention(s)
The athletes were tested before and after a shoulder muscle-fatiguing protocol.
Main Outcome Measure(s)
Acromiohumeral distance was measured using ultrasound, and scapular position was determined with an electromagnetic motion-tracking system. Both measurements were performed at 3 elevation positions (0°, 45°, and 60° of abduction). We used a 3-factor mixed model for data analysis.
Results:
After fatigue, the acromiohumeral distance increased when the upper extremity was actively positioned at 45° (Δ = 0.78 ± 0.24 mm, P = .002) or 60° (Δ = 0.58 ± 0.23 mm, P = .02) of abduction. Scapular position changed after fatigue to a more externally rotated position at 45° (Δ = 4.97° ± 1.13°, P < .001) and 60° (Δ = 4.61° ± 1.90°, P = .001) of abduction, a more upwardly rotated position at 45° (Δ = 6.10° ± 1.30°, P < .001) and 60° (Δ = 7.20° ± 1.65°, P < .001) of abduction, and a more posteriorly tilted position at 0°, 45°, and 60° of abduction (Δ = 1.98° ± 0.41°, P < .001).
Conclusions:
After a fatiguing protocol, we found changes in acromiohumeral distance and scapular position that corresponded with an impingement-sparing situation.
Key Words: shoulder, subacromial impingement syndrome, injury prevention, ultrasonography
Key Points
After a fatiguing protocol, acromiohumeral distance increased, and scapular position was more upwardly and externally rotated and posteriorly tilted when the upper extremity was actively held at 45° or 60° of abduction.
The changes in acromiohumeral distance and scapular position corresponded with a protective, impingement-sparing situation that could be explained by the scapula compensating for glenohumeral shoulder-muscle fatigue.
Overhead sports activities place large-magnitude loads on the upper extremity through repetition of high-velocity overhead motion while continuously alternating between acceleration and deceleration.1 Not surprisingly, overhead athletes often present with pathologic shoulder conditions. Disorders of the rotator cuff are frequently the source of pain.2,3 Subacromial impingement plays an important role in the development of pathologic rotator cuff conditions4; it occurs when the space is inadequate for clearance of the rotator cuff tendons during elevation.5 Multiple theories exist as to why overhead athletes develop impingement-related concerns.6–8
Overhead athletes present with several adaptations that, in turn, are linked to narrowing of the subacromial space, such as glenohumeral internal-rotation deficit (GIRD) and scapular dyskinesis. Fatigue of the shoulder muscles due to repetitive and prolonged overhead sports activity also has been postulated to contribute to impingement.9 Given that the shoulder musculature plays such an important role in producing and controlling shoulder motion, impairment of these muscles could alter scapular kinematics and influence the size of the subacromial space.
No consensus exists in the literature about whether scapular upward rotation increases10–13 or decreases14,15 and what happens to external rotation and posterior tilt of the scapula after shoulder fatigue.10–15 Based on these findings, clinicians can only indirectly deduce the effect of shoulder-muscle fatigue in overhead athletes on the actual size of the subacromial space. No researchers have measured acromiohumeral distance (AHD) before and after shoulder fatigue. Moreover, many investigators10,11,14,16 have used fatiguing protocols that do not resemble overhead sports activity, such as external rotation, horizontal abduction, and elevation exercises. Therefore, the purpose of our study was to assess the effect of a fatigue protocol resembling overhead sports activity on AHD in overhead athletes through direct measurement of this space with ultrasound. In addition, we studied changes in 3-dimensional scapular position to explore the relationship between these rotations and AHD.
METHODS
Participants
A total of 29 healthy overhead athletes (14 men, 15 women; age = 22.23 ± 2.82 years, height = 178.3 ± 7.8 cm, mass = 71.6 ± 9.5 kg, body mass index = 22.47 ± 2.06, time participating in overhead sports activity = 6.5 ± 3.2 h/wk, and experience in sport = 9.17 ± 3.60 years) were recruited from recreational sports associations: volleyball (n = 20), tennis (n = 2), water polo (n = 3), squash (n = 3), and badminton (n = 1). To be included in the study, participants had to be between 18 and 30 years of age and perform overhead sports activity for at least 2 hours each week. We excluded individuals if they had experienced shoulder pain during the 6 months before the study for which they consulted a medical doctor. Given the possible influence of GIRD on scapular and glenohumeral kinematics, we excluded athletes with >20° asymmetry compared with the contralateral side.7,17,18 All participants provided written informed consent, and the Ethical Committee of Ghent University Hospital approved the study.
Data Collection
Athletes completed a questionnaire to provide information about demographics (sex, age, height, mass), their sports activities (which sport, hours of participation per week, and years of experience in this sport), and their histories of shoulder pain. Each participant underwent a clinical examination, including active movements and impingement tests (Hawkins, Neer, and Jobe tests).19 This examination was performed by the main investigator (A.M.), who had 4 years of clinical experience as a physiotherapist treating patients with shoulder conditions. If a test was painful, the athlete was excluded from the investigation.
To evaluate GIRD, internal-rotation range of motion was measured with an Acumar digital inclinometer (model ACU360; Lafayette Instrument Co, Lafayette, IN) before the investigation started. During this measurement, the participant was supine with the shoulder abducted to 90° and internally rotated until the coracoid process started moving anteriorly.20 One investigator (A.M.) checked movement of the coracoid process through palpation, and another investigator (F.D.) measured range of motion. In a previous study,21 test-retest reliability of this measurement was 0.93 (standard error of the mean = 1.6°).
We performed baseline AHD measurements in both shoulders, representing the prefatigue condition. Baseline measurements of 3-dimensional scapular kinematics were performed only on the dominant side, which was defined as the side that the participant used for overhead throwing during sport activity. Next, the dominant side was fatigued, whereas the nondominant side was not. Once the participant completed the fatigue protocol, all measurements were repeated to represent the postfatigue condition. The fatigued shoulder was tested first to limit the time to measurements and minimize muscle recovery. For the same reason, the fatiguing protocol was performed adjacent to the measurement device, and participants were instructed on quickly resuming the correct positions.
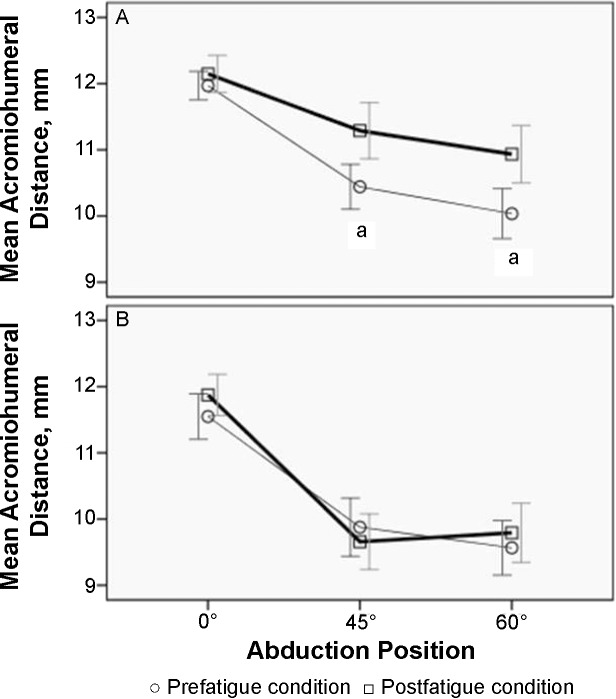
One investigator (A.M.), who specialized in shoulder ultrasonography, obtained sonographic images with a Colormaster 128 EXT-IZ device (Telemed UAB, Vilnius, Lithuania) and used a 5- to 10-MHz linear transducer (model HL9.0/40/128Z; Telemed UAB). The position of participants was standardized and corrected before the start of ultrasound scanning. Participants were seated upright without back support and with their feet flat on the ground. During AHD scanning at 0° of shoulder abduction, participants were instructed to keep their upper extremities relaxed alongside their bodies with the ulnar side of their hands supported on their thighs and thumbs pointing upward. For measurement of AHD at 45° and 60° of shoulder abduction, participants were instructed to actively keep their upper extremities in the desired position with the elbow flexed to 90° and the hand in neutral position with the thumb pointing upward. To ensure that the exact amount of abduction was maintained during measurements, a belt that was fixed to the chair and hanging around the participants' forearms was adjusted to this position, and participants were instructed to keep this belt straight without pulling at it (Figure 1).22 The amount of abduction was verified with the digital inclinometer. The transducer was positioned in the coronal plane parallel with the long axis of the humerus where the AHD was smallest.22 We collected 3-dimensional scapular kinematics at 30 Hz with the 3SPACE FASTRAK (Polhemus, Colchester, VT). This electromagnetic motion-tracking system has been used by other researchers investigating shoulder-girdle motion.11–13,23,24 The manufacturer has reported accuracy of 0.15° root mean square for orientation and 0.76 mm root mean square for position.25 It consists of a transmitter that emits the signal, 3 receivers, and a digitizing stylus, which are connected to an electronic unit. The transmitter was placed in a fixed position relative to the chair on which each participant was seated during the measurements. We chose this position because it was just posterior to the scapular sensor, and the upper extremity remained in the hemisphere during abduction. The receivers were attached to the bony landmarks with adhesive tape (Figure 2). The thoracic receiver was placed on the sternum just inferior to the sternal notch, the humeral receiver was placed on the arm just distal to the deltoid attachment on the humerus, and the scapular receiver was placed on the flat surface of the acromion. All metal and electric devices were removed from the investigation room. With the participant in a seated position, bony landmarks were palpated and digitized with the stylus (xiphoid process, most ventral point on the sternoclavicular joint, most dorsal point on the sternoclavicular joint, scapular spine triangle, inferior angle of the scapula, acromial angle of the scapula, most ventral point of the coracoid process, most caudal point on the lateral epicondyle, most caudal point on the medial epicondyle, most caudal-lateral point on the radial styloid, most caudal-medial point on the ulnar styloid).26 Given ethical considerations, the surface method was preferred over the method with sensors fixed to pins embedded in the bone. We considered the limitations of the surface method and took precautions to limit error. The low body mass index of our participants (22.47 ± 2.06) excluded potential confounding factors associated with a large amount of soft tissue, and abduction positions were restricted to much less than 120°, which is considered the limit for reliable motion tracking.27
Figure 1.
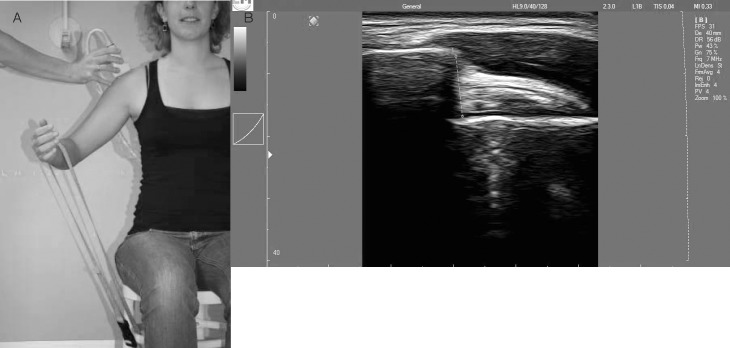
A, Participant position and probe placement during sonographic acromiohumeral distance measurements. B, Measurement of the subacromial space on ultrasonographic image.
Figure 2.

A, Receiver locations during 3-dimensional scapular position measurements. B, Coordinate axes for the local scapular reference frame.
Changes in scapular external rotation, upward rotation, and posterior tilt were quantified before and after muscle fatigue. Kinematic data were collected during each of the 3 static abduction positions of the shoulder (0°, 45°, and 60° of abduction) that corresponded with the positions in which ultrasonographic measurements were performed. Each position was held isometrically for 5 seconds, and 3 trials were conducted.
Fatiguing Protocol
To fatigue the dominant shoulder, we chose a protocol to elicit muscle fatigue that resembled overhead sport activity fatigue. The athletes had to move the upper extremity repeatedly from external to internal rotation with the shoulder abducted to 90° while holding a medium XCO-TRAINER device (XCO Sports Company BV, Leidschendam, The Netherlands; Figure 3). Resistance from the XCO-TRAINER increased the acceleration and deceleration forces so that they were similar to an overhead throwing motion. Participants knelt with the hip of the nondominant side flexed to 90° and the foot flat on the ground. This position was chosen to limit the contribution of lower extremity force during the throwing motion. No deviation of the upper extremity from the frontal plane was allowed. Speed was controlled with a metronome (model MT 50 Quarzmetronoom; Wittner GmbH & Co KG, Isny/Allgäu, Germany) set at a frequency of 144 Hz. Fatigue was defined based on both subjective and objective criteria. A Borg rating of perceived exertion scale was used to register subjective experiences of fatigue.28 This scale is a valid measure of local upper extremity exertion.29 We considered the participants to be fatigued when they reported an exertion level exceeding 14 of 20.30 A rating of 15 on the rating of perceived exertion scale corresponds with “hard/heavy work or strain and fatigue on muscles.”28 We objectively evaluated correct performance of the movement; no slowing down, no lowering of the upper extremity or deviation from the frontal plane, and no diminishing of total range of motion were allowed. When the investigator (A.M.) observed low-quality movement, she encouraged the athlete to correct the performance. Inability to do so because of muscle fatigue was the objective criterion to end the trial. The athletes were not aware of the criteria used to discontinue the fatigue protocol.
Figure 3.
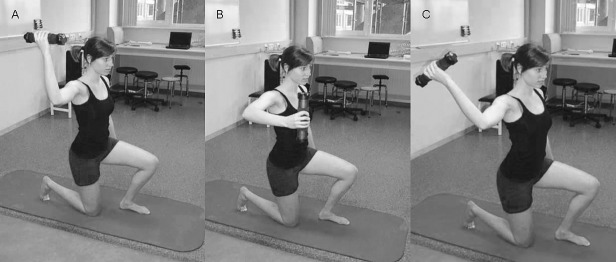
Fatigue protocol. The athlete moved repeatedly from A, external rotation, to B, internal rotation, to C, external rotation with the shoulder abducted to 90° while holding the XCO-TRAINER (XCO Sports Company BV, Leidschendam, The Netherlands).
Data Analysis
We saved all images on the sonographic unit for later AHD measurements. Echowave II software (version 1.36; Telemed UAB) was used for measuring distances. We defined AHD as the tangential distance from the most lateral part of the acromion to the humeral head (Figure 1).
Raw kinematic data of the FASTRAK were converted to anatomically defined rotations with a custom-written MATLAB program (The Mathworks, Inc, Natick, MA) and displayed with Visual 3D (C-Motion, Inc, Rockville, MD). The 3 scapular rotations were defined with an Euler axis sequence (external rotation, upward rotation, and posterior tilting).26 Means were calculated over 5 seconds, and those data again were averaged over the 3 trials.
Statistical Analysis
To determine the influence of fatiguing the dominant shoulder on AHD in both shoulders, a 3-factor mixed-model analysis was used with the factors of side (dominant, nondominant), time (prefatigue, postfatigue), and position (0°, 45°, 60°). To investigate the influence of dominant-shoulder fatigue on scapular kinematics, we used a 2-factor mixed-model analysis with the factors of time and position. Type of sports and hours of participation per week were included in both models as covariates. Post hoc analyses were adjusted with the Bonferroni correction. We used IBM SPSS software (version 19; IBM Corp, Armonk, NY) for statistical analysis. All P values were 2 tailed and considered different when less than .05.
RESULTS
Sex was distributed evenly (female to male = 15:14). The average duration of the fatigue protocol was 6 minutes, 33 seconds (minimum = 3 minutes, 19 seconds; maximum = 12 minutes, 55 seconds).
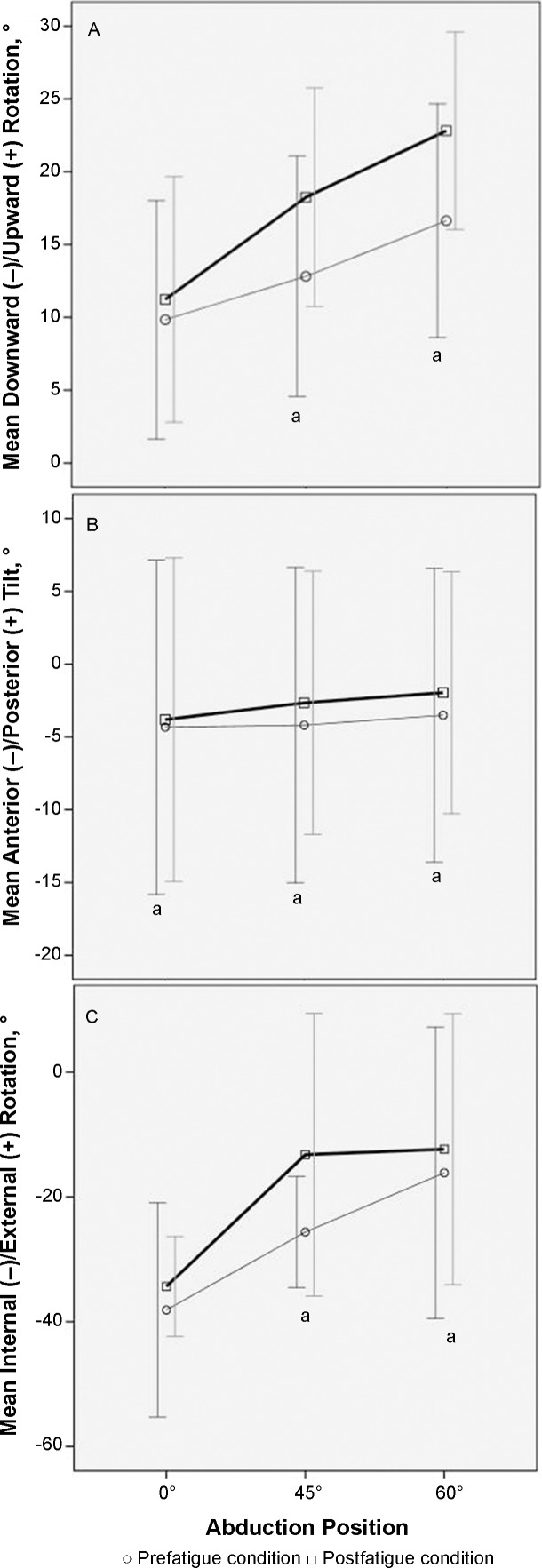
Results of sonographic AHD measurements on the dominant and nondominant sides and before and after fatiguing the dominant side are presented in the Table and Figure 4. Analysis of AHD showed an interaction effect of time × side × position (P = .048). Post hoc tests indicated that the AHD did not change postfatigue at 0° of abduction (Δ = 0.24 ± 0.16 mm, P = .15; 95% confidence interval [CI] = −0.09, 0.57 mm). On the dominant side, the AHD was larger postfatigue at 45° of abduction with an increase of 0.78 ± 0.24 mm (P = .002; 95% CI = 0.31, 1.28 mm) and at 60° of abduction with an increase of 0.58 ± 0.23 mm (P = .02; 95% CI = 0.10, 1.06 mm). Post hoc tests demonstrated no change of the AHD at any abduction position on the nondominant side, which was not fatigued (P > .05). We found no influence of type of sport or hours of participation per week.
Table.
Sonographic Acromiohumeral Distance Measurements (mm) on the Dominant and Nondominant Sides and Before and After Fatiguing the Dominant Side
| Abduction Position |
Side |
|||||
| Dominant |
Nondominant |
|||||
| Mean (Standard Error) |
Mean (Standard Error) |
|||||
| Prefatigue |
Postfatigue |
P Value for Difference |
Prefatigue |
Postfatigue |
P Value for Difference |
|
| 0° | 11.92 (0.25) | 12.15 (0.25) | .15 | 11.90 (0.30) | 11.93 (0.30) | .85 |
| 45° | 10.81 (0.34) | 11.61 (0.34) | .002a | 10.24 (0.39) | 10.03 (0.39) | .43 |
| 60° | 10.21 (0.39) | 10.79 (0.39) | .02a | 9.95 (0.36) | 10.13 (0.37) | .53 |
Indicates a difference between prefatigue and postfatigue measurements.
Figure 4.
Sonographic acromiohumeral distance measurements on the, A, dominant and, B, nondominant sides and before and after fatiguing the dominant side. The x axis displays the position of abduction at which the measurement was taken. The y axis displays the acromiohumeral distance in millimeters. Error bars indicate 95% confidence intervals. a Indicates the difference between prefatigue and postfatigue conditions.
Change in position of the dominant scapula around the 3 axes prefatigue and postfatigue is presented in Figure 5. We found a main effect of time for scapular position around the z axis (anterior-posterior tilt) with an overall change of 1.98° ± 0.41° postfatigue (P < .001; 95% CI = 1.16°, 2.79°), meaning that the scapula was in a more posteriorly tilted position postfatigue. We noted an interaction effect of time × position for scapular position around the x axis (upward-downward rotation). Post hoc tests showed that the scapula was in the same position prefatigue and postfatigue at 0° of abduction (Δ = 1.35° ± 1.07°, P = .22; 95% CI = −0.91°, 3.62°) but more upwardly rotated at 45° (Δ = 6.10° ± 1.30°, P < .001; 95% CI = 3.36°, 8.85°) and 60° (Δ = 7.20° ± 1.65°, P < .001; 95% CI = 3.72°, 10.69°) of abduction. Comparing the position of the scapula around the y axis (external-internal rotation) prefatigue and postfatigue revealed an interaction effect of time × position (P < .001). Again, we observed no change of the dominant scapular position at 0° of abduction (Δ = 1.58° ± 0.81°, P = .07; 95% CI = −3.30°, 0.13°), but at 45° (Δ = 4.97° ± 1.13°, P < .001; 95% CI = 2.58°, 7.36°) and 60° (Δ = 4.61° ± 1.90°, P = .001; 95% CI = 2.10°, 7.12°) of abduction, the scapula was in a more externally rotated position postfatigue. We found no influence of type of sport or hours of participation per week.
Figure 5.
Dominant-side scapular rotation prefatigue and postfatigue. A, Downward/upward rotation, B, Anterior/posterior tilt, C, Internal/external rotation. The x axis displays the position of abduction at which the measurement was taken. The y axis represents scapular rotation. Error bars indicate 95% confidence intervals. a Indicates difference between prefatigue and postfatigue conditions.
DISCUSSION
Based on the literature, it is not clear how muscle fatigue due to overhead sport activity affects the AHD. We wanted to measure the AHD directly by using ultrasonography before and after a protocol to elicit muscle fatigue that resembled overhead sport activity fatigue. At the same time, we wanted to determine scapular position changes. By doing this, we could link a change in AHD to changes in scapular position.
Contrary to what is believed intuitively in clinical practice, we found that the AHD increased postfatigue in the shoulder of healthy overhead athletes when the upper extremity was held actively in the 45° and 60° elevated positions. No change occurred in a relaxed position with the extremity at 0° of abduction. This coincides with the alterations in 3-dimensional scapular position seen postfatigue. The scapula was more posteriorly tilted and upwardly and externally rotated position when the upper extremity was elevated to 45° and 60°. These positions are believed to result in an increased AHD, which suggests that the increased AHD results from the scapular position changes.31,32
We are the first to directly measure the AHD before and after overhead muscle fatigue. Other researchers have investigated the influence of muscle fatigue on 3-dimensional scapular position. To put these results in the correct perspective, a distinction must be made based on fatigue protocol type.
In 4 studies10,12–14 that we found, the authors investigated changes in scapular kinematics after a fatiguing, repetitive elevation task, also called a global fatigue task. Ebaugh et al12 found increased external rotation and upward rotation along with decreased posterior tilt. McQuade et al13,14 showed less scapular motion in 1 study14 and more scapular motion after elevation fatigue in another study.13 Results of the former study,14 however, are limited by the very small sample size (N = 4). More recently, Chopp et al10 also noted increased scapular upward and external rotation and posterior tilt. These results, in general, are similar to the impingement-sparing changes that we found after fatigue. Ebaugh et al12 suggested that, after global shoulder-muscle fatigue, more compensatory scapular motion is needed to reach the requested angle of elevation, and changes in scapular kinematics must be seen as a compensatory strategy.
In addition to elevation fatigue, other researchers have investigated the influence of external-rotation fatigue, also called local shoulder fatigue. In 2 studies,11,15 investigators found less external rotation and posterior tilt of the scapula postfatigue. Upward rotation of the scapula increased after external-rotation fatigue in a study by Ebaugh et al11 but decreased in a study by Tsai et al.15 Chopp et al10 showed no change in scapular motion after the local fatigue task. The contradictory results of these studies must be seen in light of methodologic differences, such as the use of static positions versus dynamic elevation for measuring scapular position and different criteria used to determine fatigue. The only study we found in which the authors examined fatigue in overhead athletes and the study that is most comparable with ours was conducted by Joshi et al.9 Their participants performed a prone external-rotation fatiguing protocol at 90° of abduction, and the researchers found more upward rotation after the protocol during a diagonal upward movement from horizontal adduction-internal rotation to horizontal abduction-external rotation. No change was noted in external rotation and posterior tilt of the scapula.
Whereas these results are in line with ours, an important difference exists between the fatigue protocols used. By using prone external rotation at 90° of abduction, only the posterior shoulder muscles were fatigued in the study by Joshi et al.9 Our protocol fatigued both muscle groups through high-velocity concentric and eccentric contractions, similar to the way in which shoulder muscles work during overhead sport activity. We found no other studies in which the authors examined 3-dimensional scapular position changes after functional fatiguing protocols resembling overhead sport fatigue.
We did not measure muscle activity during the fatiguing protocol. However, the protocol may have elicited greater fatigue of the glenohumeral than the scapulothoracic muscles, which could explain why our athletes compensated with more scapular motion into an impingement-sparing direction. This possibility coincides with the increased AHD found during actively held abduction and suggests that humeral-head position in the dominant shoulders of our athletes either did not change or did not change enough in the superior direction to decrease the AHD. The rotator cuff muscles might not have been more fatigued than the deltoid muscle after the fatigue protocol we used.
The amount of change in scapular position postfatigue that we found was small for posterior tilt (overall 1.98° ± 0.41°), large for external rotation (4.97° ± 1.13° at 45° of abduction and 4.61° ± 1.90° at 60° of abduction), and very large for upward rotation (6.10° ± 1.30° at 45° of abduction and 7.20° ± 1.65° at 60° of abduction) compared with the studies discussed. A difference of more than 3° generally is considered the minimal clinically important change.10–12 The clinical importance of the AHD increase (0.78 ± 0.24 mm at 45° and 0.58 ± 0.23 mm at 60° of abduction) postfatigue can be questioned. However, even a small change in AHD could decrease pressure in the subacromial space. Furthermore, the absence of almost any change on the nondominant side (Δ = 0.01 ± 0.17 mm), which was not fatigued between premeasurement and postmeasurement and therefore acted as a control, strengthens the credibility of the results.
Limitations
Our study had some limitations. First, AHD measurements were performed at low-elevation angles, so no information is available on what happens at angles greater than 60°. The reason is that it was impossible to display the rotator cuff in the AHD at higher angles using ultrasonography.22 Ultrasonography was preferable because of its low cost, safety, and feasibility of examining the athletes in a seated position, which allowed free movement of the scapula. Graichen et al33 showed that the minimal AHD passes through the supraspinatus tendon at 30° and 60° of abduction, in contrast to the minimal distance at 90° of abduction that is located laterally to the suspraspinatus. This supports the relevance of lower elevation angles in view of rotator cuff tendinopathy. Moreover, in addition to impingement of the rotator cuff in the subacromial space, posterosuperior or internal impingement and coracoid impingement also might play a role.
Second, although it resembled an overhead throwing motion, the fatiguing protocol that we used differs from overhead sport activity on the field. Important differences are the kneeling position we used to limit the contribution of the lower limbs and the lack of a horizontal abduction-adduction motion and greater abduction angles. Although changing these factors would make things “easier” for the shoulder muscles, it seems unlikely that the results would be dramatically altered. Moreover, after the fatiguing protocol, our participants spontaneously mentioned that the experience of muscle fatigue resembled the feeling after heavy training or a game.
Third, our findings represent alterations that occurred immediately after the shoulder muscles were fatigued. Whether these patterns change with repeated bouts of muscle fatigue and how long these changes persist are unknown and are areas for future research.
Our results necessitate further investigation of the role of impingement in the development of pathologic rotator cuff conditions in overhead athletes because they suggest that overhead sport activity fatigue possibly does not narrow AHD but instead enlarges it. Researchers should use other measurement tools to build on our results with data collected at higher-elevation angles and in other upper extremity positions. Moreover, the correlation between sport adaptations at the shoulder and AHD needs to be elucidated. Silva et al34 found more narrowing of AHD in tennis players with scapular dyskinesis. Researchers should determine the effect of rotator cuff or scapular muscle imbalance35,36 and glenohumeral internal-rotation deficit17,18,37 on AHD to clarify their roles in impingement-related rotator cuff conditions.
CONCLUSIONS
Muscle fatigue due to repetitive and prolonged overhead sport activity is considered an important contributing factor to impingement-related pathologic rotator cuff conditions in overhead athletes. We investigated the effect of a fatigue protocol resembling overhead sport activity on the ultrasonographic AHD and 3-dimensional scapular position in overhead athletes. After a fatiguing protocol, AHD increased and the scapula was in a more upwardly and externally rotated and posteriorly tilted position when the upper extremity was actively held at 45° or 60° of abduction. This position corresponds with a protective, impingement-sparing situation and could be explained by the scapula compensating for glenohumeral shoulder-muscle fatigue.
REFERENCES
- 1.Fleisig GS, Bolt B, Fortenbaugh D, Wilk KE, Andrews JR. Biomechanical comparison of baseball pitching and long-toss: implications for training and rehabilitation. J Orthop Sports Phys Ther. 2011;41(5):296–303. doi: 10.2519/jospt.2011.3568. [DOI] [PubMed] [Google Scholar]
- 2.Blevins FT. Rotator cuff pathology in athletes. Sports Med. 1997;24(3):205–220. doi: 10.2165/00007256-199724030-00009. [DOI] [PubMed] [Google Scholar]
- 3.Wilk KE, Obma P, Simpson CD, Cain EL, Dugas JR, Andrews JR. Shoulder injuries in the overhead athlete. J Orthop Sports Phys Ther. 2009;39(2):38–54. doi: 10.2519/jospt.2009.2929. [DOI] [PubMed] [Google Scholar]
- 4.Seitz AL, McClure PW, Finucane S, Boardman ND, III, Michener LA. Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both? Clin Biomech (Bristol, Avon) 2011;26(1):1–12. doi: 10.1016/j.clinbiomech.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Neer CS., II Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am. 1972;54(1):41–50. [PubMed] [Google Scholar]
- 6.Borsa PA, Laudner KG, Sauers EL. Mobility and stability adaptations in the shoulder of the overhead athlete: a theoretical and evidence-based perspective. Sports Med. 2008;38(1):17–36. doi: 10.2165/00007256-200838010-00003. [DOI] [PubMed] [Google Scholar]
- 7.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology part I. Pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–420. doi: 10.1053/jars.2003.50128. [DOI] [PubMed] [Google Scholar]
- 8.Jobe CM, Coen MJ, Screnar P. Evaluation of impingement syndromes in the overhead-throwing athlete. J Athl Train. 2000;35(3):293–299. [PMC free article] [PubMed] [Google Scholar]
- 9.Joshi M, Thigpen CA, Bunn K, Karas SG, Padua DA. Shoulder external rotation fatigue and scapular muscle activation and kinematics in overhead athletes. J Athl Train. 2011;46(4):349–357. doi: 10.4085/1062-6050-46.4.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chopp JN, Fischer SL, Dickerson CR. The specificity of fatiguing protocols affects scapular orientation: implications for subacromial impingement. Clin Biomech (Bristol, Avon) 2011;26(1):40–45. doi: 10.1016/j.clinbiomech.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 11.Ebaugh DD, McClure PW, Karduna AR. Scapulothoracic and glenohumeral kinematics following an external rotation fatigue protocol. J Orthop Sports Phys Ther. 2006;36(8):557–571. doi: 10.2519/jospt.2006.2189. [DOI] [PubMed] [Google Scholar]
- 12.Ebaugh DD, McClure PW, Karduna AR. Effects of shoulder muscle fatigue caused by repetitive overhead activities on scapulothoracic and glenohumeral kinematics. J Electromyogr Kinesiol. 2006;16(3):224–235. doi: 10.1016/j.jelekin.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 13.McQuade KJ, Dawson J, Smidt GL. Scapulothoracic muscle fatigue associated with alterations in scapulohumeral rhythm kinematics during maximum resistive shoulder elevation. J Orthop Sports Phys Ther. 1998;28(2):74–80. doi: 10.2519/jospt.1998.28.2.74. [DOI] [PubMed] [Google Scholar]
- 14.McQuade KJ. Hwa Wei S, Smidt GL. Effects of local muscle fatigue on three-dimensional scapulohumeral rhythm. Clin Biomech (Bristol, Avon) 1995;10(3):144–148. doi: 10.1016/0268-0033(95)93704-w. [DOI] [PubMed] [Google Scholar]
- 15.Tsai NT, McClure PW, Karduna AR. Effects of muscle fatigue on 3-dimensional scapular kinematics. Arch Phys Med Rehabil. 2003;84(7):1000–1005. doi: 10.1016/s0003-9993(03)00127-8. [DOI] [PubMed] [Google Scholar]
- 16.McQuade KJ, Smidt GL. Dynamic scapulohumeral rhythm: the effects of external resistance during elevation of the arm in the scapular plane. J Orthop Sports Phys Ther. 1998;27(2):125–133. doi: 10.2519/jospt.1998.27.2.125. [DOI] [PubMed] [Google Scholar]
- 17.Laudner KG, Moline MT, Meister K. The relationship between forward scapular posture and posterior shoulder tightness among baseball players. Am J Sports Med. 2010;38(10):2106–2112. doi: 10.1177/0363546510370291. [DOI] [PubMed] [Google Scholar]
- 18.Thomas SJ, Swanik KA, Swanik CB, Kelly JD IV. Internal rotation deficits affect scapular positioning in baseball players. Clin Orthop Relat Res. 2010;468(6):1551–1557. doi: 10.1007/s11999-009-1124-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cools AM, Cambier D, Witvrouw EE. Screening the athlete's shoulder for impingement symptoms: a clinical reasoning algorithm for early detection of shoulder pathology. Br J Sports Med. 2008;42(8):628–635. doi: 10.1136/bjsm.2008.048074. [DOI] [PubMed] [Google Scholar]
- 20.Awan R, Smith J, Boon AJ. Measuring shoulder internal rotation range of motion: a comparison of 3 techniques. Arch Phys Med Rehabil. 2002;83(9):1229–1234. doi: 10.1053/apmr.2002.34815. [DOI] [PubMed] [Google Scholar]
- 21.Maenhout A, Van Eessel V, Van Dyck L, Vanraes A, Cools A. Quantifying acromiohumeral distance in overhead athletes with glenohumeral internal rotation loss and the influence of a stretching program. Am J Sports Med. 2012;40(9):2105–2112. doi: 10.1177/0363546512454530. [DOI] [PubMed] [Google Scholar]
- 22.Desmeules F, Minville L, Riederer B, Cote CH, Fremont P. Acromio-humeral distance variation measured by ultrasonography and its association with the outcome of rehabilitation for shoulder impingement syndrome. Clin J Sport Med. 2004;14(4):197–205. doi: 10.1097/00042752-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Lin JJ, Lim HK, Yang JL. Effect of shoulder tightness on glenohumeral translation, scapular kinematics, and scapulohumeral rhythm in subjects with stiff shoulders. J Orthop Res. 2006;24(5):1044–1051. doi: 10.1002/jor.20126. [DOI] [PubMed] [Google Scholar]
- 24.Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80(3):276–291. [PubMed] [Google Scholar]
- 25.3SPACE. FASTRAK User Manual, Revision F. Colchester, VT: 1993. [Google Scholar]
- 26.Wu G, van der Helm FC, Veeger HE, et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion: part II. Shoulder, elbow, wrist and hand. J Biomech. 2005;38(5):981–992. doi: 10.1016/j.jbiomech.2004.05.042. [DOI] [PubMed] [Google Scholar]
- 27.Karduna AR, McClure PW, Michener LA, Sennett B. Dynamic measurements of three-dimensional scapular kinematics: a validation study. J Biomech Eng. 2001;123(2):184–190. doi: 10.1115/1.1351892. [DOI] [PubMed] [Google Scholar]
- 28.Borg G. Borg's Perceived Exertion and Pain Scales. Champaign, IL: Human Kinetics;; 1998. [Google Scholar]
- 29.Kang J, Chaloupka EC, Mastrangelo MA, et al. Regulating exercise intensity using ratings of perceived exertion during arm and leg ergometry. Eur J Appl Physiol Occup Physiol. 1998;78(3):241–246. doi: 10.1007/s004210050414. [DOI] [PubMed] [Google Scholar]
- 30.Tripp BL, Yochem EM, Uhl TL. Functional fatigue and upper extremity sensorimotor system acuity in baseball athletes. J Athl Train. 2007;42(1):90–98. [PMC free article] [PubMed] [Google Scholar]
- 31.Atalar H, Yilmaz C, Polat O, Selek H, Uras I, Yanik B. Restricted scapular mobility during arm abduction: implications for impingement syndrome. Acta Orthop Belg. 2009;75(1):19–24. [PubMed] [Google Scholar]
- 32.Solem-Bertoft E, Thuomas KA, Westerberg CE. The influence of scapular retraction and protraction on the width of the subacromial space: an MRI study. Clin Orthop Relat Res. 1993;296:99–103. [PubMed] [Google Scholar]
- 33.Graichen H, Bonel H, Stammberger T, Englmeier KH, Reiser M, Eckstien F. Subacromial space width changes during abduction and rotation: a 3-D MR imaging study. Surg Radiol Anat. 1999;21(1):59–64. doi: 10.1007/BF01635055. [DOI] [PubMed] [Google Scholar]
- 34.Silva RT, Hartmann LG, Laurino CF, Bilo JP. Clinical and ultrasonographic correlation between scapular dyskinesia and subacromial space measurement among junior elite tennis players. Br J Sports Med. 2010;44(6):407–410. doi: 10.1136/bjsm.2008.046284. [DOI] [PubMed] [Google Scholar]
- 35.Cools AM, Witvrouw E, Declercq G, Vanderstraeten G, Cambier D. Evaluation of isokinetic force production and associated muscle activity in the scapular rotators during a protraction-retraction movement in overhead athletes with impingement symptoms. Br J Sports Med. 2004;38(1):64–68. doi: 10.1136/bjsm.2003.004952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Page P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. Int J Sports Phys Ther. 2011;6(1):51–58. [PMC free article] [PubMed] [Google Scholar]
- 37.Borich MR, Bright JM, Lorello DJ, Cieminski CJ, Buisman T, Ludewig PM. Scapular angular positioning at end range internal rotation in cases of glenohumeral internal rotation deficit. J Orthop Sports Phys Ther. 2006;36(12):926–934. doi: 10.2519/jospt.2006.2241. [DOI] [PubMed] [Google Scholar]