Abstract
Objective
To determine surgical risk in nursing home residents undergoing major abdominal surgery.
Summary Background Data
Recent studies suggest that surgery can be performed safely in the very old. Surgical risk in nursing home residents is poorly understood.
Methods
We used national Medicare claims and the nursing home Minimum Data Set (1999–2006) to identify nursing home residents undergoing surgery (surgery for bleeding duodenal ulcer, cholecystectomy, appendectomy, and colectomy, n=70,719). We compared operative mortality and use of invasive interventions (mechanical ventilation, intravascular hemodynamic monitoring, feeding tube placement, tracheostomy, and vena cava filters) among nursing home residents to rates among non-institutionalized Medicare enrollees age 65 and older undergoing the same procedures. (n=1,060,389). We adjusted for patient characteristics using logistic regression.
Results
Operative mortality among nursing home residents was substantially higher than among non-institutionalized Medicare enrollees for all procedures (surgery for bleeding duodenal ulcer, 42% v. 26%, adjusted odds ratio (AOR) 1.79; colectomy, 32% v. 13%, AOR 2.06; appendectomy, 12% v. 2%, AOR 3.27; cholecystectomy, 11% v. 3%, AOR 2.65; p<0.001 for all comparisons). Overall, invasive interventions were more common among nursing home residents than controls (ranging from 18% and 5%, respectively, for cholecystectomy to 55% and 43%, respectively, for surgery for bleeding duodenal ulcer, p<0.0001 for all comparisons).
Conclusions
Nursing home residents experience substantially higher rates of mortality and invasive interventions after major surgery than other Medicare beneficiaries that are independent of age and measured comorbidities. Our data suggest that the risks of major surgery are substantially higher in nursing home residents and this information should inform decisions of physicians and patients and their families.
Introduction
Published studies suggest that major surgery can be performed safely in the very old.1,2 Single center case series report outcomes after surgery in older patients similar to that observed in younger patients.3,4 While these data show that surgery can be performed safely and with low mortality rates among selected very old persons, it is unknown whether these favorable outcomes apply widely because there is limited population-based evidence about surgical outcomes in the elderly. Recent population-based evidence from Washington State found that 90-day mortality after major abdominal surgery rose markedly with age, from 2.5% in those age 65–69 years to 16.7% in those age 90 years or older.5 These studies, however, did not specifically address risk in the most vulnerable old -- nursing home residents.
Nursing home residents are a large and vulnerable population. They represent approximately 5% of people age 65 years and older at any time and it is estimated that more than one third of people age 70 years and older will spend some time in a nursing home before they die.6 Nonetheless, morbidity and mortality after major surgery for common surgical diseases in nursing home residents have not been studied. It is difficult, therefore, for physicians, patients, and their families to make informed decisions when faced with a diagnosis for which surgery is generally recommended for younger, healthier patients. Population-based data about operative risk is essential to provide realistic expectations for surgical outcomes. Such data also could prompt providers to consider less invasive therapeutic options such as antibiotic therapy alone for acute appendicitis.
To evaluate outcomes after major surgery among elderly nursing home residents, we determined operative mortality and the rates of use of secondary invasive interventions after major surgery among all Medicare beneficiaries age 65 years or older. We then compared outcomes among nursing home residents to outcomes for other Medicare beneficiaries undergoing the same procedures, adjusting for patient characteristics.
Methods
Study Population
We used ICD-9 procedure and diagnosis codes in the Medicare Inpatient Files to identify all Medicare beneficiaries age 65 years or older who underwent surgery from 1999–2006 for bleeding duodenal ulcer, colectomy for benign colon diseases (e.g diverticulitis, volvulus, ischemic colitis), cholecystectomy for benign biliary disease, and appendectomy for appendicitis. These procedures were selected because they were frequently performed in nursing home residents (over 1000 performed over the study period) and are associated with substantial morbidity and mortality in the elderly. To increase the homogeneity of our cohort, we included only patients undergoing surgery for benign disease, excluding patients with a diagnosis code for cancer (e.g. patients undergoing colectomy with a diagnosis code for cancer were excluded). Beneficiaries were classified as long-term nursing home residents if they underwent 2 consecutive assessments for the Minimum Data Set for Nursing Homes (MDS) within 6 months prior to surgery. The MDS is a standardized assessment administered quarterly for all residents of nursing homes participating in Medicare or Medicaid programs. Beneficiaries were classified as not nursing home residents if they did not undergo any MDS assessment before their surgery. Patient demographic data were obtained from the Medicare Denominator File. Using methods described by Elixhauser et al., we identified patient comorbidities in the MEDPAR file from the index admission.7
Assessement of Outcomes
Our primary outcome measure was operative mortality. We defined operative mortality as the percentage of patients experiencing either death within 30 days of surgery (including patients discharged alive before 30 days who subsequently died within 30 days of the index surgery) or death during the hospitalization in which the index surgery was performed (even if more than 30 days post-operatively). Death after hospital discharge was ascertained from the Medicare Denominator File for nursing home residents and the non-institutionalized Medicare population. Secondary invasive interventions – mechanical ventilation, bronchoscopy, placement of feeding tubes and tracheostomies, intravascular hemodynamic monitoring, and vena cava filter placement – were identified using ICD-9 codes in the Medicare Inpatient File.
Statistical Analysis
To assess the impact of nursing home resident status on operative outcomes, we used logistic regression techniques to determine risk ratios of operative mortality and the use of invasive in-hospital interventions among nursing home residents and in the non-institutionalized Medicare population, adjusting for age, sex, race (black and non-black), admission acuity (elective or urgent/emergent), year of hospital admission, and patient comorbidities. We then explored the impact of age and comorbidity on operative mortality by stratifying mortality by age and comorbidity for each procedure for nursing home residents and the general Medicare population.
To further control for potential unmeasured confounders associated with operative mortality, we performed a propensity score-stratified analysis. Using stepwise logistic regression analyses, we identified patient characteristics associated with nursing home residence. We constructed a propensity score predicting nursing home residence based on age, gender, race, admission acuity, and comorbidity. The predictive ability of the final model as measured by the c statistic ranged from 0.66 for the bleeding duodenal ulcer surgery cohort to 0.79 for appendectomy cohort. We then created a study cohort containing each nursing home resident undergoing a procedure of interest matched to one non-institutionalized elders undergoing the same procedure based on propensity score. With this cohort, we used logistic regression to assess the impact of nursing home residency on outcomes.
All statistical tests were two-tailed and p<0.05 was considered statistically significant. Statistical analysis was performed using SAS software (SAS Institute, Cary, North Carolina). The Institutional Review Board at the University of California, San Francisco approved this study protocol.
Results
Patient characteristics
Between 1999 and 2006, 70,719 nursing home residents and 1,060,389 patients in the non-institutionalized Medicare population aged 65 and older underwent one of the four procedures examined. The mean age of nursing home patients undergoing surgery was over age 80 – substantially higher than other Medicare beneficiaries undergoing the same procedures (Table 1). The majority of patients undergoing surgery in both groups were admitted urgently or emergently. Nursing home residents were much more likely than other Medicare beneficiaries to have multiple medical comorbidities.
Table 1.
Characteristics of Patients Undergoing Surgery
| Procedure | Nursing home resident | Non-institutionalized elderly Medicare enrollees | p-value |
|---|---|---|---|
| Surgery for bleeding ulcer | n=2344 | n=19455 | |
| Age (mean, SD) | 82.8 (7.9) | 78.7 (7.8) | <0.001 |
| Sex (%/nmale) | 30.3% (710) | 44.4% (8636) | <0.001 |
| Race (% black) | 5.7% (133) | 5.7% (1111) | 0.943 |
| Comorbidity count 2+ (%/n) | 75.2% (1762) | 68.6% (13354) | <0.001 |
| Urgent/emergent (%/n) | 93.4% (2190) | 94.2% (18323) | 0.145 |
| Cholecystectomy | n=41412 | n=697644 | |
| Age (mean, SD) | 80.7 (7.9) | 75.8 (7.1) | <0.001 |
| Sex (%/n male) | 34.2% (14170) | 42.5% (296641) | <0.001 |
| Race (%/n black) | 9.5% (3943) | 6.2% (43143) | <0.001 |
| Comorbidity count 2+ (%/n) | 77.4% (32066) | 53.1% (370544) | <0.001 |
| Urgent/emergent (%/n) | 79.5% (32902) | 70.0% (488210) | <0.001 |
| Appendectomy | n=2105 | n=94154 | |
| Age (mean, SD) | 80.7 (8.3) | 73.8 (6.6) | <0.001 |
| Sex (%/n male) | 42.0% (884) | 51.1% (48113) | <0.001 |
| Race (%/n black) | 7.3% (153) | 4.0% (3779) | <0.001 |
| Comorbidity count 2+ (%/n) | 75.0% (1579) | 42.0% (39515) | <0.001 |
| Urgent/emergent (%/n) | 91.1% (1917) | 89.4% (84175) | 0.014 |
| Colectomy | n=24858 | n=249136 | |
| Age (mean, SD) | 80.7 (7.6) | 76.0 (7.1) | <0.001 |
| Sex (%/n male) | 32.3% (8023) | 38.1% (94825) | <0.001 |
| Race (%/n black) | 11.7% (2895) | 7.1% (17565) | <0.001 |
| Comorbidity count 2+ (%/n) | 74.4% (18492) | 55.8% (139044) | <0.001 |
| Urgent/emergent (%/n) | 91.1% (1917) | 89.4% (84175) | 0.01 |
Operative mortality
Figure 1 shows unadjusted rates of operative mortality in nursing home residents and non-institutionalized elderly Medicare enrollees. For procedures with very low mortality risk in non-institutionalized Medicare enrollees, cholecystectomy and appendectomy, operative mortality was high in the nursing home population – 11% after cholecystectomy (v. 3%, adjusted odds ratio (AOR) 2.65, 95% confidence interval (CI) 2.56–2.75) and 12% after appendectomy (v. 2%, AOR 3.27, 95% CI 2.81–3.81). Among nursing home residents undergoing surgery for benign colon disease, operative mortality was nearly 3-fold higher than among non-institutionalized elderly Medicare enrollees – 32% v. 13%, respectively (AOR 2.06, 95% CI 1.99–2.12). Operative mortality after surgery for bleeding duodenal ulcer was very high in nursing home residents – 42% (versus 26% among non-institutionalized Medicare enrollees, AOR 1.79, 95%, 1.63–1.96).
Figure 1.
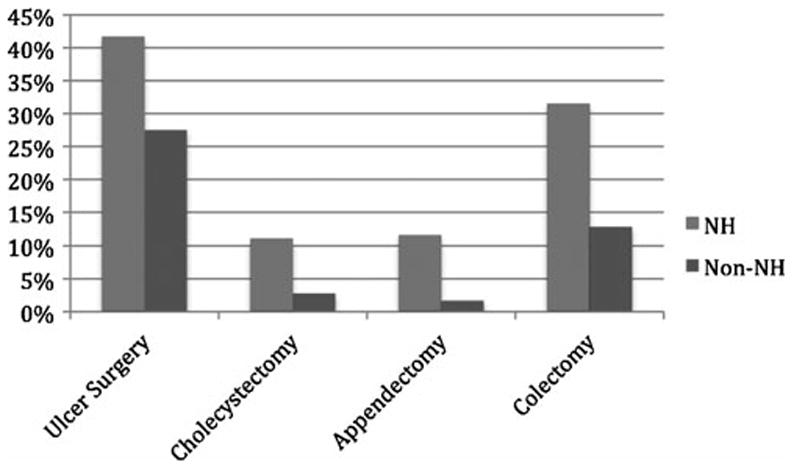
Operative Mortality Among Nursing Home Residents and Non-Institutionalized Elderly Medicare Enrollees, By Procedure Type.
Operative mortality varied widely by age and comorbidity count for all four procedures (Table 2). Nonetheless, for nearly every age-comorbidity stratum, mortality was significantly higher (P<0.01) for nursing home residents than for non-institutionalized elders. In the propensity score analysis, operative mortality among nursing home residents was substantially higher than among matched non-institutionalized Medicare enrollees for all 4 procedures (Table 3). For cholecystectomy and appendectomy, operative mortality in nursing home residents was more than double that of non-institutionalized Medicare patients (11% v. 5%, p>0.0001). While operative mortality was high among matched community dwelling elders after colectomy (18%) and surgery for bleeding duodenal ulcer (30%), it was still significantly lower that mortality rates observed in the nursing home population (32% and 42%, respectively, p>0.0001 for both comparisons).
Table 2.
Operative Mortality, by Procedure Type, Age and Comorbidity
| Nursing home residents | Non-institutionalized elderly Medicare enrollees | Nursing home residents | Non-institutionalized elderly Medicare enrollees | Nursing home residents | Non-institutionalized elderly Medicare enrollees | Nursing home residents | Non-institutionalized elderly Medicare enrollees | |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 0–1 Comorbidities | 2 Comorbidities | 3 Comorbidities | 4+ Comorobidities | |||||
|
| ||||||||
| Procedure | Operative Mortality % (total n) | Operative Mortality % (total n) | Operative Mortality % (total n) | Operative Mortality % (total n) | Operative Mortality % (total n) | Operative Mortality % (total n) | Operative Mortality % (total n) | Operative Mortality % (total n) |
| Surgery for bleeding ulcer | ||||||||
| Age category | ||||||||
| 65–74 | 28.9%(83) | 13.4%(2030) | 35.7%(98) | 19.5%(1817) | 35.6%(87) | 22.7%(1417) | 33.0%†(115) | 26.8%†(1070) |
| 75–84 | 40.2%(214) | 21.0%(2625) | 42.6%(265) | 24.7%(2494) | 43.8%(219) | 26.2%(1920) | 40.1%*(192) | 31.0%*(1302) |
| 85+ | 42.1%(285) | 32.7%(1446) | 47.7%(331) | 35.6%(1488) | 44.0%*(257) | 37.2%*(1139) | 43.4%†(198) | 37.1%(707) |
| Cholecystectomy | ||||||||
| Age category | ||||||||
| 65–74 | 7.5%(1729) | 0.8%(165362) | 8.6%(2307) | 1.7%(85930) | 7.7%(2561) | 2.7%(48633) | 7.9%(2825) | 4.2%(27571) |
| 75–84 | 9.8%(4002) | 1.8%(126315) | 10.0%(4988) | 3.1%(80338) | 10.1%(4777) | 4.2%(48259) | 10.6%(4079) | 5.6%(26864) |
| 85+ | 13.1%(3615) | 5.0%(35423) | 13.7%(4152) | 7.4%(26134) | 14.4%(3736) | 8.6%(17152) | 15.7%(2641) | 10.8%(9663) |
| Appendectomy | ||||||||
| Age category | ||||||||
| 65–74 | 5.2%(115) | 0.5%(34873) | 8.0%(150) | 1.2%(12499) | 10.9%(128) | 1.7%(5770) | 7.4%(136) | 3.1%(2663) |
| 75–84 | 8.7%(184) | 1.2%(16617) | 9.1%(242) | 2.3%(8227) | 10.6%(217) | 3.6%(4255) | 7.3%†(179) | 5.1%†(2097) |
| 85+ | 15.4%(227) | 4.1%(3149) | 16.7%(221) | 7.2%(2104) | 20.6%(175) | 9.4%(1193) | 13.0%†(131) | 9.3%(707) |
| Colectomy | ||||||||
| Age category | ||||||||
| 65–74 | 26.8%(1271) | 5.3%(55441) | 28.3%(1464) | 9.0%(30587) | 29.1%(1359) | 11.0%(17911) | 26.4%(1229) | 14.1%(9555) |
| 75–84 | 30.2%(2890) | 11.3%(42802) | 30.2%(3423) | 14.7%(30094) | 29.1%(2873) | 16.1%(19281) | 26.9%(2108) | 18.7%(10178) |
| 85+ | 40.9%(2205) | 24.1%(11849) | 37.5%(2489) | 26.2%(10364) | 36.0%(2087) | 26.9%(7057) | 32.1%(1460) | 28.0%(4017) |
All differences in mortality between Nursing Home Residents and Non-institutionalized elderly were significant at p<0.01 except:
p=0.05–0.01 and
p >0.05.
Table 3.
Operative Mortality, by Procedure Type: Propensity Score Analysis
| Procedure | Nursing Home Resident | Non-institutionalized elderly Medicare enrollees |
|---|---|---|
| Surgery for bleeding ulcer | ||
| Total number of patients | 2337 | 2337 |
| Operative mortality % (n) | 41.6% (972) | 29.8% (696) |
| Cholecystectomy | ||
| Total number of patients | 41405 | 41405 |
| Operative mortality % (n) | 11.0% (4544) | 4.7% (1963) |
| Appendectomy | ||
| Total number of patients | 2099 | 2099 |
| Operative mortality % (n) | 11.4% (240) | 4.5% (94) |
| Colectomy | ||
| Total number of patients | 24851 | 24851 |
| Operative mortality % (n) | 31.5% (7835) | 18.3% (4552) |
Secondary invasive interventions
Patients admitted from nursing homes were significantly more likely to undergo secondary invasive interventions during their surgical hospitalization than non-institutionalized Medicare patients (Table 4). Rates of invasive interventions among nursing home resident ranged from 18% after cholecystectomy to 55% after surgery for bleeding duodenal ulcer. Among non-institutionalized Medicare patients, invasive interventions were less frequent – ranging from 5% after cholecystectomy to 43% after surgery for bleeding duodenal ulcer. In general, rates of invasive interventions were very high among patients who died – over 40% for most procedures in both nursing home residents and non-institutionalized Medicare patients. Among nursing home residents who survived surgery, rates of secondary invasive interventions were nearly threefold higher for cholecystectomy (15% v. 5%; AOR 2.84, 95% CI 2.75–2.93) and appendectomy (18% v. 6%; AOR 2.48, 95% CI 2.19–2.82) and over 50% higher for colectomy 41% v. 22% (AOR 1.77, 95% CI 1.71–1.83) and bleeding duodenal ulcer surgery (49% v. 36%; AOR 1.56, 95% CI 1.43–1.84) compared to non-institutionalized Medicare patients.
Table 4.
Operative Mortality and Invasive Interventions in Nursing Home Residents and Non-institutionalized Elderly Medicare Enrollees, by Procedure Type
| Procedure | Nursing Home Resident Unadjusted Rates % (n) | Non-institutionalized elderly Medicare enrollees Unadjusted Rates % (n) | Adjusted OR (95% CI)* |
|---|---|---|---|
| Surgery for bleeding ulcer | |||
| Operative mortality | 41.7% (977) | 25.7% (4994) | 1.79 (1.63–1.96) |
| Invasive interventions | |||
| Mechanical ventilation > 96 hr (%) | 13.4% (315) | 9.6% (1866) | 1.49 (1.30–1.69) |
| Tracheostomy (%) | 1.5% (36) | 1.5% (300) | 1.22 (0.86–1.74) |
| Feeding tube placement (%) | 17.8% (416) | 11.7% (2274) | 1.52 (1.35–1.71) |
| IVC filter placement (%) | 1.5% (34) | 0.8% (153) | 1.91 (1.30–2.80) |
| Bronchoscopy (%) | 2.0% (46) | 2.0% (383) | 1.06 (0.77–1.45) |
| Central venous catheterization (%) | 32.5% (762) | 26.6% (5172) | 1.26 (1.15–1.38) |
| Pulmonary artery catheterization (%) | 4.1% (95) | 2.8% (553) | 1.34 (1.06–1.68) |
| Any invasive intervention | 55.0% (1289) | 42.6% (8285) | 1.56 (1.43–1.70) |
| Survivors | 49.2% (673) | 36.2% (5229) | 1.64 (1.46–1.84) |
| Deaths | 63.0% (616) | 61.2% (3056) | 1.08 (0.94–1.25) |
| Cholecystectomy | |||
| Operative mortality | 11.0% (4546) | 2.8% (19717) | 2.65 (2.56–2.75) |
| Invasive interventions | |||
| Mechanical ventilation > 96 hr (%) | 2.1% (864) | 0.7% (4564) | 2.57 (2.38–2.78) |
| Tracheostomy (%) | 0.2% (87) | 0.08% (524) | 2.47 (1.95–3.13) |
| Feeding tube placement (%) | 3.1% (1261) | 0.5% (3144) | 4.86 (4.53–5.21) |
| IVC filter placement (%) | 0.5% (188) | 0.1% (925) | 2.82 (2.40–3.32) |
| Bronchoscopy (%) | 0.8% (330) | 0.3% (1948) | 2.43 (2.16–2.75) |
| Central venous catheterization (%) | 13.4% (5559) | 4.1% (28783) | 2.63 (2.55–2.72) |
| Pulmonary artery catheterization (%) | 0.8% (319) | 0.4% (2687) | 1.54 (1.37–1.74) |
| Any invasive intervention | 17.8% (7380) | 5.4% (37546) | 2.82 (2.74–2.90) |
| Survivors | 15.0% (5528) | 4.5% (30443) | 2.84 (2.75–2.93) |
| Deaths | 40.7% (1852) | 36.0% (7103) | 1.23 (1.15–1.32) |
| Appendectomy | |||
| Operative mortality | 11.5% (241) | 1.7% (1604) | 3.27 (2.81–3.81) |
| Invasive interventions | |||
| Mechanical ventilation > 96 hr (%) | 2.6% (55) | 0.8% (709) | 2.01 (1.50–2.68) |
| Tracheostomy (%) | 0.4% (8) | 0.1% (130) | 2.03 (0.97–4.23) |
| Feeding tube placement (%) | 3.0% (63) | 0.3% (283) | 5.50 (4.08–7.40) |
| IVC filter placement (%) | 0.5% (10) | 0.09% (85) | 3.59 (1.81–7.11) |
| Bronchoscopy (%) | 0.6% (13) | 0.3% (254) | 1.39 (0.78–2.46) |
| Central venous catheterization (%) | 16.7% (351) | 5.1% (4828) | 2.34 (2.07–2.64) |
| Pulmonary artery catheterization (%) | 1.1% (23) | 0.3% (321) | 1.84 (1.19–2.85) |
| Any invasive intervention | 20.8% (438) | 6.1% (5764) | 2.50 (2.23–2.80) |
| Survivors | 18.3% (341) | 5.5% (5071) | 2.48 (2.19–2.82) |
| Deaths | 40.3% (97) | 43.2% (693) | 0.92 (0.70–1.23) |
| Colectomy | |||
| Operative mortality | 31.5% (7839) | 12.8% (31804) | 2.06 (1.99–2.12) |
| Invasive interventions | |||
| Mechanical ventilation > 96 hr (%) | 9.4% (2344) | 4.1% (10078) | 1.89 (1.80–1.98) |
| Tracheostomy (%) | 1.5% (377) | 0.8% (2031) | 1.62 (1.44–1.82) |
| Feeding tube placement (%) | 9.4% (2347) | 3.3% (8238) | 2.25 (2.14–2.37) |
| IVC filter placement (%) | 1.4% (342) | 0.6% (1604) | 1.75 (1.55–1.97) |
| Bronchoscopy (%) | 1.7% (427) | 0.9% (2115) | 1.67 (1.50–1.86) |
| Central venous catheterization (%) | 31.2% (7761) | 19.9% (49651) | 1.39 (1.35–1.43) |
| Pulmonary artery catheterization (%) | 2.5% (613) | 1.5% (3612) | 1.27 (1.16–1.39) |
| Any invasive intervention | 45.8% (11387) | 26.5% (66115) | 1.73 (1.68–1.78) |
| Survivors | 40.7% (6932) | 22.4% (48759) | 1.77 (1.71–1.83) |
| Deaths | 56.8% (4455) | 54.6% (17356) | 1.09 (1.04–1.15) |
Adjusted for age, sex, race, admission acuity, year of hospital admission, comorbidities
Life sustaining interventions were much more frequent in nursing home residents than in the general Medicare population. Compared to the non-institutionalized Medicare population, nursing home residents were approximately twice as likely to undergo prolonged mechanical ventilation (>96 hours) for all 4 conditions examined – 13% v 10% (AOR 1.49, 95% CI 1.30–1.69) for surgery for bleeding duodenal ulcer; 9% v. 4% (AOR 1.89, 95%CI 1.80–1.98) for colectomy; 3% v 0.8% (AOR 2.01, 95%CI 1.50–2.68) for appendectomy; and 2% v. 0.7% (AOR 2.57, 95%CI 2.38–2.78) for cholecystectomy. Operative and percutaneous placement of feeding tubes was substantially higher among nursing home residents. Feeding tubes were used most frequently in nursing home residents undergoing surgery for bleeding duodenal ulcer (18%) and benign colon conditions (9%) (versus 12% (AOR 1.52, 95%CI 1.35–1.71) and 3% (AOR 2.25, 95%CI 2.14–2.37) among non-institutionalized elderly Medicare enrollees). Although feeding tubes were used in only 3% of nursing home residents undergoing appendectomy and cholecystectomy, they were used more frequently than among non-institutionalized Medicare enrollees undergoing the same procedures (0.3% (AOR 5.50, 95% CI 4.08–7.40) and 0.5% (AOR 4.86, 95% CI 4.53–5.21), respectively). Tracheostomy placement after surgery was relatively infrequent – less than 2% in both populations for all 4 procedures.
Rates of other invasive interventions were generally low. Fewer than 2% of nursing home residents underwent inferior vena cava (IVC) filter placement for all 4 procedures examined (Table 4). IVC filters, however, were less frequently used among non-institutionalized elderly Medicare enrollees undergoing the same procedures, ranging from 0.1% for appendectomy (AOR 3.59, 95% CI 1.81–7.11) and 0.8% for surgery for bleeding duodenal ulcer (AOR 1.91, 95% CI 1.30–2.80).
Nursing home resident status was associated with increased use of invasive hemodynamic monitoring. Over 30% of nursing home residents undergoing duodenal ulcer surgery and colectomy underwent central venous catheterization (Table 4). Central venous catheterization was used in 13% of nursing home residents undergoing cholecystectomy and 17% of nursing home residents undergoing appendectomy (versus 4% (AOR 2.63, 95% CI 2.55–2.72) and 5% (AOR 2.34, 95%CI 2.07–2.64) among non-institutionalized elderly Medicare enrollees, respectively). Although rates of pulmonary artery catheter insertion were low in all patients, they were used more frequently in nursing home residents than among non-institutionalized Medicare enrollees.
Discussion
In this national study of surgical outcomes for elderly nursing home patients, we found that operative mortality among nursing home residents is substantially higher than observed among non-institutionalized elderly Medicare enrollees, even after correcting for traditional risk factors such as age and comorbidity. Even for typically ‘low risk’ procedures such as appendectomy and cholecystectomy, more than 1 in 10 nursing home residents die postoperatively. For most procedures examined, a 65 year old patient admitted from a nursing home had an operative mortality risk similar to that of an 85 year old admitted from the community. Moreover, while stepwise increases in operative mortality with increasing comorbidity burden were observed in the non-institutionalized elderly Medicare population, comorbidity was not prognostic in nursing home residents. These data suggest that surgical risk calculations should be very different for nursing home patients than for non-institutionalized elders.
We also found that nursing home residents were more likely than non-institutionalized Medicare enrollees to undergo additional invasive life-sustaining interventions during their surgical hospitalization. The use of life sustaining interventions – prolonged mechanical ventilation and feeding tube placement – was substantially higher in nursing home residents than among non-institutionalized elderly Medicare enrollees. Differences in intervention rates were most dramatic among patients who survived surgery, indicating that nursing home residents require far more ‘rescue procedures’ than non-institutionalized Medicare to survive surgery.
To our knowledge, this is the first population-based study to examining surgical risk in nursing home residents. Small studies have examined surgical outcomes in long stay nursing home residents. Zenilman et al performed a study of surgical interventions in a cohort of 153 nursing home patients undergoing general and vascular surgery.8 Morbidity and 30 day mortality for this cohort were high, 18% and 10%, respectively. This analysis, however, was limited to patients at a single institution. Moreover, the majority of interventions (66%) were minor procedures (incisional biopsy, debridement of pressure ulcers). We found that mortality rates after major surgery are substantially higher than have been previously reported in the elders in published case series. Single center studies have suggested that surgery is safe in the very old. For instance, in a study of operative mortality after cholecystectomy, Annamaneni RK et al. report zero mortality among octogenarians (without describing the percentage who were nursing home residents).9 A recent single center series examining operative mortality in multi-morbid elders undergoing appendectomy found no association between comorbidity burden and operative mortality, but again results for nursing home residents were not reported.3 However, single center case series may be more likely to be submitted and published if observed mortality is low. For this reason, we believe that our population-based analysis provides more realistic risk estimates for elders undergoing gastrointestinal surgery. Our findings are consistent with previously published population-based analyses that have reported high morbidity and mortality after major surgery in very old patients, 10,11,12 but suggest that even nursing home patients in the 65–74 age range may do as poorly as the very elderly.
This study has several limitations. Although we used standard approaches to risk adjustment with administrative data, administrative data may not include sufficient clinical detail to fully account for differences in patient characteristics. For this reason, we may have underestimated the contribution of patient comorbidity to the observed high mortality. Furthermore, it is difficult to determine severity of illness using claims data. In this study, however, we found that comorbidity predicted operative mortality in non-institutionalized patients. In addition, a propensity score analysis to control for propensity for nursing home residence yielded similar results. Our analysis includes outcomes for common diseases that most often present for urgent or emergent surgery. Our observed mortality rates in both populations studied are likely to be substantially higher than for elective surgery. For this reason, caution should be used when extrapolating our results to elderly undergoing less risky, elective surgery. Finally, because we were limited to Medicare claims data for the non-institutionalized patients, we were unable to assess other outcomes that are important in elders such as functional status.
Our study has important implications for the delivery of surgical care in the growing population of elders. High surgical risk in nursing home residents raises questions about the optimal treatment of ‘surgical diseases’ in nursing home residents. For truly life-threatening conditions, surgical risk observed in our study is not high enough to suggest that surgery is futile–over half of nursing home residents age 85 and older survive major surgery. There is evidence that patients with limited life expectancy are willing to undergo high risk procedures if there is a chance of an eventual return to baseline functioning.13 Use of less invasive therapies, however, may improve outcomes after treatment for these conditions in this population. For example, antibiotic therapy may be a safer treatment for appendicitis in multimorbid patients --an approach commonly used outside the United States. 14, 15 Percutaneous aspiration or cholecystostomy tube placement may be preferable options for patients with acute cholecystitis and high surgical risk. Aggressive endoscopic treatment or embolization of bleeding duodenal ulcers in this population may be a more appropriate approach than operative therapy. Similarly, selective use of endoluminal stents for large bowel obstruction may be an effective option in a patient with limited life expectancy. These interventions, however, have not been well studied in the elderly and further research is needed to determine whether less invasive interventions will result in improved outcomes in this population. Information about mortality risk and the likelihood of secondary invasive interventions after surgery will also help patients and caregivers set realistic expectations for surgical outcomes. Knowledge of expected outcomes can help patients and physicians anticipate and prepare for difficult care decisions about life sustaining interventions after surgery.
In conclusion, operative mortality and rates of secondary interventions are much higher among nursing home residents undergoing major surgery in the United States than reported in previous studies of surgical outcomes among the elderly. Moreover, unlike non-institutionalized elderly patients, observed differences in surgical risk cannot be entirely explained by advanced age and comorbidity burden. These data should be used to inform clinical decision-making about surgical versus non-surgical approaches to treating the conditions studied and to focus efforts on improving outcomes in this vulnerable population.
Acknowledgments
Funding/Support: Work on this study was funded in part by a National Institute on Aging/Paul B. Beeson Clinical Scientist Development Award in Aging (5K08AG028965). Dr. Dudley’s work was supported by an Investigator Award in Health Policy from the Robert Wood Johnson Foundation.
Work on this study was funded by a National Institute on Aging/Paul B. Beeson Clinical Scientist Development Award in Aging (5K08AG028965). Dr. Dudley’s work was supported by an Investigator Award in Health Policy from the Robert Wood Johnson Foundation.
Footnotes
Reprints will not be available from the authors
The authors have no other financial disclosures.
References
- 1.Ibis C, Albayrak D, Hatipoglu AR, et al. The amount of comorbidities as a single parameter has no effect in predicting the outcome in appendicitis patients older than 60 years. South Med J. 2010;103(3):202–6. doi: 10.1097/SMJ.0b013e3181ce0e20. [DOI] [PubMed] [Google Scholar]
- 2.Majeski J. Laparoscopic cholecystectomy in geriatric patients. Am J Surg. 2004;187:747–750. doi: 10.1016/j.amjsurg.2003.11.031. [DOI] [PubMed] [Google Scholar]
- 3.Reissman p, Agachan F, Wexner Outcome of laparoscopic colorectal surgery in older patients. Am Surg. 1996;62(12):1060–3. [PubMed] [Google Scholar]
- 4.Gurevitch AJ, Davidovitch B, Kashtan H. Outcome of right colectomy for cancer in octogenarians. J Gastrointest Surg. 2009;13(1):100–4. doi: 10.1007/s11605-008-0643-3. [DOI] [PubMed] [Google Scholar]
- 5.Massarweh NN, Legner VJ, Symons RG, et al. Impact of advancing age on abdominal surgical outcomes. Arch Surg. 2009;144(12):1108–1114. doi: 10.1001/archsurg.2009.204. [DOI] [PubMed] [Google Scholar]
- 6.Murtaugh CM, Kemper P, Spillman BC, et al. The amount, distribution, and timing of lifetime nursing home use. Med Care. 1997;35(3):204–218. doi: 10.1097/00005650-199703000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Zenilman ME, Bender JS, Magnuson TH, et al. General surgical care in the nursing home patient: results of a dedicated geriatric surgery consult service. J Am Coll Surg. 1996;183:361–370. [PubMed] [Google Scholar]
- 9.Annamaneni RK, Moraitis D, Cayten CG, et al. Laparoscopic cholecystectomy in the elderly. JSLS. 2005;9(4):408–10. [PMC free article] [PubMed] [Google Scholar]
- 10.Finlayson E, Fan Z, Birkmeyer JD. Outcomes in octogenarians undergoing high-risk cancer operation: a national study. J Am Coll Surg. 2007;205(6):729–734. doi: 10.1016/j.jamcollsurg.2007.06.307. [DOI] [PubMed] [Google Scholar]
- 11.Finlayson EV, Birkmeyer JD. Operative mortality with elective surgery in older adults. Eff Clin Pract. 2001;4(4):172–177. [PubMed] [Google Scholar]
- 12.Hamel MB, Henderson WG, Khuri SF, et al. Surgical outcomes for patients aged 80 and older: morbidity and mortality from major noncardiac surgery. J Am Geriatr Soc. 2005;53(3):424–9. doi: 10.1111/j.1532-5415.2005.53159.x. [DOI] [PubMed] [Google Scholar]
- 13.Fried TR, Bradley EH, Towle VR, et al. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346(14):1061–6. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 14.Hansson J, Körner U, Khorram-Manesh A, et al. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009;96(5):473–81. doi: 10.1002/bjs.6482. [DOI] [PubMed] [Google Scholar]
- 15.Malik AA, Bari SU. Conservative management of acute appendicitis. J Gastrointest Surg. 2009;13(5):966–70. doi: 10.1007/s11605-009-0835-5. [DOI] [PubMed] [Google Scholar]


