Abstract
Background
Readmission rates of 9.7%–15.5% after hepatectomy have been reported. These rates are difficult to interpret due to variability in the time interval used to monitor readmission. The aim of this study was to refine the definition of readmission after hepatectomy.
Study Design
A prospectively maintained database of 3041 patients who underwent hepatectomy from 1998 through 2013 was merged with the hospital registry to identify readmissions. Area under the curve (AUC) analysis was used to determine the time interval that best captured unplanned readmission.
Results
Readmission rates at 30 days, 90 days, and 1 year after discharge were 10.7% (n = 326), 17.3% (n = 526), and 31.9% (n = 971) respectively. The time interval that best accounted for unplanned readmissions was 45 days after discharge (AUC, 0.956; p < 0.001), during which 389 patients (12.8%) were readmitted (unplanned: n = 312 [10.3%]; planned: n = 77 [2.5%]). In comparison, the 30 days after surgery interval (used in the ACS-NSQIP database) omitted 65 (26.3%) unplanned readmissions. Multivariate analysis revealed the following risk factors for unplanned readmission: diabetes (odds ratio [OR], 1.6; p = 0.024), right hepatectomy (OR, 2.1; p = 0.034), bile duct resection (OR, 1.9; p = 0.034), abdominal complication (OR, 1.8; p = 0.010), and a major postoperative complication (OR, 2.4; p < 0.001). Neither index hospitalization > 7 days nor postoperative hepatobiliary complications were independently associated with readmission.
Conclusions
To accurately assess readmission after hepatectomy, patients should be monitored 45 days after discharge.
Keywords: hepatectomy, readmission, definition, time interval, rate, risk factors
INTRODUCTION
Improvements in diagnosis, multimodality therapies, surgical technique and anesthetic management have expanded the indications for hepatic resection in patients with malignant and benign disease. The rate of readmission in these patients ranges from 9.7% to 15.5%.1–7 Readmission after surgical discharge is a costly endeavor for patients, providers, and the health care system. Approximately 20% of health care costs are directly associated with hospital readmissions (U.S. estimates 2010).8 Not surprisingly, readmissions are becoming a major target for health care expense reduction.9 Beginning in fiscal year 2012, the U.S. government directed the Centers for Medicare and Medicaid Services (CMS) to track hospital readmission rates for certain high-cost conditions. Furthermore, payments may be restructured to consolidate the hospitalization and any post-discharge event care into one payment, or payments may be reduced for hospitals with high readmission rates.8
As insurers and government payers have threatened to withhold payment for readmissions, multiple groups have tried to evaluate surgical readmissions in the hopes of developing strategies to reduce the rate.5–7 However, these efforts have been impeded by variability in the definition of readmission and the time interval for assessment. For example, one-third of studies published in the literature monitor and report 30-day readmission rates after discharge, whereas the other two-thirds use 30- and 90-day rates after surgery, making comparisons difficult (Table 1).
Table 1.
Summary of Studies Reporting Readmission after Hepatectomy
| Readmission Definition | ||||||
|---|---|---|---|---|---|---|
| First author, year | n | Source | Interval, d | From | Unplanned/planned | Readmission rate, % |
| Schneider EB, 20126 | 5,311 | Medicare | 30 | Discharge | Patients admitted to acute care hospital | 14.1–15.5 |
| Kassin MT, 20122 | 124 | NSQIP (institutional) | 30 | Discharge | Institutional data used to identify unplanned | 9.7 |
| Barbas AS, 20131 | 1281 | Single institution | 90 | Surgery | All readmissions | 14.4 |
| Spolverato G, 20147 | 338 | Single institution | 30 | Discharge | All readmissions | 14.2 |
| Kelly KN, 20143 | 2555 | NSQIP | 30 | Surgery | Unplanned | 12.7 |
| Lucas DJ, 20144 | 2101 | NSQIP | 30 | Surgery | Acute care admission | 13.0 |
| Brudvik KW, 2014 | 3041 | Single institution | 45 | Discharge | Unplanned | 10.3 |
Historically, time intervals for readmission assessment have been chosen on the basis of the availability of data and not a medical rationale. For example, in the United States, the databases of the CMS and University HealthSystem Consortium (UHC) and the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) monitor readmissions in a fixed time interval, 30 days from discharge (CMS and UHC) and 30 days from surgery (ACS-NSQIP). These databases may not obtain all relevant readmissions after surgery, possibly due to unique patterns of readmission of each disease and of each surgical procedure. In addition, the databases do not accurately distinguish unplanned readmissions from planned readmissions, which in modern care of hepatobiliary tumor patients (two-stage surgery, portal vein embolization, adjuvant interventional and systemic therapy) are frequent. Last, hepatobiliary surgery is often accompanied by other visceral resections; thus, identifying the cause to which the readmission should be attributed can be difficult.2–6
There is no consensus regarding the best time interval to monitor and report readmissions after hepatectomy and reported readmission rates and factors found to be associated with readmission depends on the definition of readmission that is used. Readmission is increasingly being used as an indicator of surgical quality, thereby establishing a need for one definition with sufficient sensitivity and specificity to account for relevant events. The primary aim of the present study was to determine the optimal time interval to report readmission, with accuracy regarding planned and unplanned readmissions, after hepatic resection in a large single-center series of patients. Our secondary aim was to report clinical patterns and risk factors associated with readmission in the same cohort.
MATERIAL AND METHODS
Study population
Demographic, clinical, operative, and pathological data of 3041 patients undergoing hepatic resection between January 1998 and December 2013 were prospectively registered in an institution-approved study database. Patients who underwent an ablative procedure only (e.g., cryotherapy, radiofrequency, or ethanol ablation) or wedge biopsy without resection were excluded from the study. The subsequent data analysis focused on readmission and the retrospective analysis was approved by the Institutional Review Board of The University of Texas MD Anderson Cancer Center (IRB protocol number PA14-0281). Patients who were readmitted within 365 days of discharge after hepatic resection were identified by comparing the institutional database with the hospital admission registry; the database was retrospectively updated with each patient’s readmission date, indication, and other associated factors.
Readmissions
The index stay was defined as the hospital stay when the hepatectomy was performed. Readmissions were categorized as unplanned or planned according to the indication for readmission. Unplanned readmissions were those related or likely related to the index stay and/or the surgical procedure performed. Planned readmissions included those for resection of remaining disease (e.g., two-stage liver resection, colorectal resection in patients selected for a liver-first approach, and resection of lung, lymph node, or brain metastases), other local liver treatment (e.g., radiofrequency ablation, transarterial chemoembolization), stoma reversals, or events related to chemotherapy.
Perioperative and index stay factors
Typical management algorithms and outcomes for hepatobiliary surgery patients at our institution have been previously reported.10 In summary, preoperative evaluation included computed tomography according to hepatectomy protocol, liver function tests (aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, bilirubin, albumin, and coagulation tests), and measurements of serum tumor marker levels in all patients. Major resection was defined as resection of 3 or more Couinaud segments, and the standardized future liver remnant volume was calculated as previously described.11–13 Preoperative portal vein embolization was performed if the calculated future liver remnant was inadequate (<20%, <30% and <40% in the normal, injured, or cirrhotic liver, respectively).14–17 Intraoperative ultrasonography (Aloka Co. Ltd., Tokyo, Japan: 5- to 7.5-MHz probe) was used to detect lesions that were undetectable at preoperative imaging and to delineate anatomic relationships between tumor and vasculobiliary structures. Postoperative drains were used at the surgeon’s discretion. Any additional concomitant hepatic or extrahepatic procedure was registered. Concomitant liver procedures included wedge resection, portal lymph node dissection, en bloc diaphragmatic resection, and vascular or biliary reconstruction. Concomitant abdominal procedures included gastric, duodenal, pancreatic, bowel, uterine and adnexal, adrenal, mesenteric, kidney, and spleen resection. The majority of concomitant procedures were planned preoperatively. Cholecystectomy was widely performed and was not considered an additional procedure. Likewise, hepatic artery pump placement, ablative procedures, biopsies of the liver or peritoneum, ileostomy or colostomy reversal, and hernia repairs were not considered additional procedures.
Morbidity and mortality
Complications were categorized as minor or major according to a standardized system and as grade I and II or grade III-V.18 In addition, the time of the complication was registered as “during the index stay” or “after discharge/reason for readmission.” To evaluate the impact of different complications on readmission, we also classified the complications as being associated with the liver, abdomen (non-liver), lung, heart, or urinary tract. Liver-related complications were defined as perihepatic abscess, hemorrhage, hepatic insufficiency, and bile leak. Hepatic insufficiency was defined as a peak in serum bilirubin levels of more than 7 mg/dl at any time postoperatively, according to previously published criteria.12, 16, 19 Bile leak was defined as a bilirubin concentration in the drain fluid at least three times the serum bilirubin concentration on or after the third postoperative day or as the need for radiologic or operative intervention resulting from biliary collections or bile peritonitis.10, 20 Abdominal non-liver-associated complications included bowel obstruction or perforation, fistula, non-hepatobiliary infection, and pain without hepatobiliary explanation. Mortality was recorded but was not used as a criterion for exclusion from the study.
Statistical analysis
Given the sample size, normal distribution of continuous data was confirmed, allowing expression as the mean with standard deviation and comparison with independent t-tests. Categorical data were compared using chi-squared tests. To assess readmission rates over time, we used Pearson correlation analysis. Variables with a univariate significance at a level of p < 0.1 were included in the multivariate analysis. Multivariate analysis was performed via logistic regression. To determine the optimal time interval for identifying patients with unplanned readmission, we performed receiver-operator-characteristic (ROC) analysis. Trend lines for unplanned and planned readmissions within 90 days of discharge were assessed as logarithmic regression curves with a least squares fit. P < 0.05 was considered statistically significant. SPSS v.19.0 (SPSS Inc., IBM, Chicago, IL, USA) was used to perform the statistical analysis, and GraphPad Prism 6 (GraphPad Software Inc., La Jolla, CA, USA) was used to create figures.
RESULTS
Logistic regression and ROC curve analyses to define optimal readmission time interval
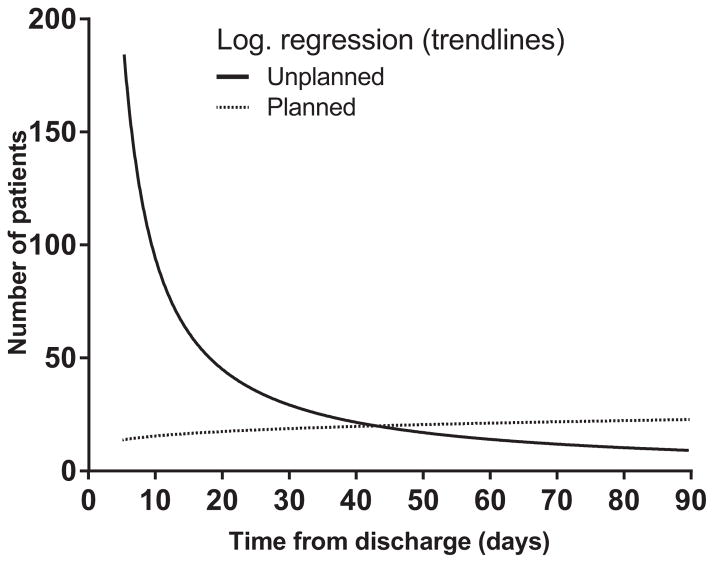
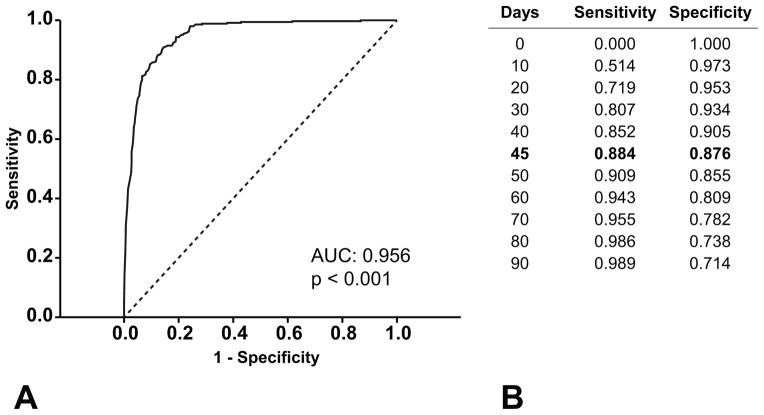
Logarithmic regression curves with least squares fit were used to evaluate trend lines for unplanned and planned readmissions occurring within 90 days after discharge (Figure 1). The trend lines of the two types of readmission crossed between 40 and 50 days, indicating that a shorter time interval would under-report unplanned readmissions, whereas a longer time interval would over-report planned readmissions. The time interval with the best combined sensitivity and specificity to identify an unplanned readmission was 45 days after discharge, as determined by ROC analysis (sensitivity, 88.4%; specificity, 87.6%; area-under-curve, 0.956 [p < 0.001]; Figure 2).
Figure 1.
Trend lines (logarithmic regression with least square fit) for readmissions occurring between 0 and 90 days after discharge (unplanned: n = 349, planned: n = 177).
Figure 2.
(A) Receiver operating characteristics (ROC) curve and (B) analysis depicting unplanned readmissions occurring within 90 days of discharge.
Capture of readmissions varies with different time interval definitions
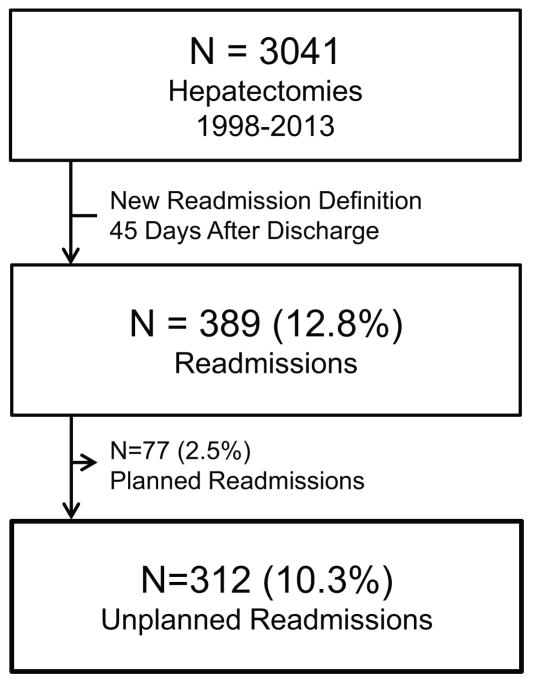
A second admission date within 1 year of discharge after hepatectomy was recorded in 971 of the 3041 (31.9%) patients. All relevant readmissions occurred within 90 days of discharge, and unplanned readmissions after this time point were attributed to medical complications and/or evolution of the primary disease. Use of the timeframe defined as 45 days after discharge identified a total of 389 readmissions (12.8%) of which 312 (10.3%) were unplanned (Figure 3). Use of the ACS-NSQIP timeframe (30 days from surgery) resulted in the identification of 288 (9.5%) readmissions of which 247 were unplanned (8.1%), omitting 65 (26.3%) unplanned readmissions. Use of the CMS and UHC timeframe (30 days from discharge) identified 326 (10.7%) readmissions of which 285 were unplanned (9.4%), omitting 27 (9.5%) unplanned readmissions. Use of the timeframe defined as 90 days from discharge identified 526 (17.3%) readmissions of which 349 (11.5%) were unplanned, adding 37 patients with unplanned readmissions of which only 12 were recorded with readmission indications that could be attributed to the index hospitalization and/or surgery.
Figure 3.
Readmissions 45 days after discharge.
Indications for readmission
Readmission indications clearly associated with the performed surgery or the index stay (abdominal fluid collection, pleural effusion, wound-related problems, biliary obstruction, cholangitis, pancreatitis, duodenitis, and hepatic insufficiency) were grouped, and their pattern of presentation after discharge (Figure 4a) was different than that of indications with more uncertain association (e.g., dehydration, gastroenteritis, urinary infection), especially when presenting after 45 days (Figure 4b). The readmission frequency time curve of patients with clearly associated readmissions declined and almost disappeared shortly after 50 days (Figure 4a), whereas the readmission frequency time curve of patients with non-hepatobiliary causes declined and disappeared around 35 days, reemerging to a low but constant level beyond 90 days, possibly reflecting a floor value of readmissions from primary disease-related conditions (Figure 4b). Indications, frequencies, and rates for unplanned readmissions within 45 days after discharge are presented in Table 2.
Figure 4.
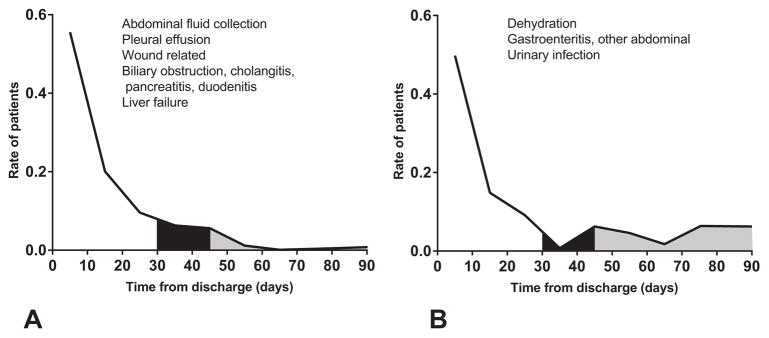
(A, B) Readmission indications classified according to pattern of presentation after discharge. The readmission rate was calculated for each indication and assessed with the time point of the readmission. The black area under curve represents patients included by extending the time interval of readmission from 30 days to 45 days, and the grey area under curve represents patients included by extending the time interval of readmission from 45 days to 90 days.
Table 2.
Indications for 45 Days Unplanned Readmission after Hepatectomy in Percent of Readmissions (n = 312) and Total (n = 3,041)
| n | % of Readmissions | % of Total | |
|---|---|---|---|
| Intraabdominal fluid collection | 141 | 45.2 | 4.6 |
| Requiring intervention (drainage, reoperation, ERCP) | 128 | 41 | 4.2 |
| Dehydration, nausea, vomiting, diarrhea, renal failure | 41 | 13.1 | 1.3 |
| Pleural effusion, pneumonia or other respiratory | 36 | 11.5 | 1.2 |
| Requiring intervention (drainage) | 26 | 8.3 | 0.9 |
| Wound infection, wound erythema, fascial dehiscence | 29 | 9.3 | 1 |
| Biliary obstruction, cholangitis, pancreatitis, duodenitis | 26 | 8.3 | 0.9 |
| Abdominal (fistula, bowel injury, bowel obstruction, GI bleeding) | 23 | 7.4 | 0.8 |
| Hepatic insufficiency and ascites | 18 | 5.8 | 0.6 |
| Pain without other finding | 12 | 3.8 | 0.4 |
| Urinary (infection, obstruction, bleeding) | 6 | 1.9 | 0.2 |
| Other cause | 27 | 8.7 | 0.9 |
| Related to index admission or disease | 22 | 7.1 | 0.7 |
ERCP: endoscopic retrograde cholangiopancreatography; GI: gastrointestinal
Characteristics and independent risk factors for unplanned readmission
Next, we identified factors associated with unplanned readmission within 45 days of discharge (Table 3). In univariate analyses, the readmitted group (n = 312, 10.3%) was characterized by a higher rate of preoperative jaundice (18.1%; p = 0.018), diabetes (13.8%; p = 0.026), right or extended right hepatectomy (14.0%; p = 0.002), bile duct resection (22.9%; p < 0.001), concomitant abdominal procedure (11.9%; p = 0.003), perioperative blood transfusion (14.9%; p = 0.001), liver-associated complications during the index stay (23.6%; p < 0.001), abdominal non-liver-associated complications during the index stay (18.8%; p < 0.001), major complications during the index stay (23.4%, p < 0.001), and a length of index stay greater than 7 days (15.6%; p < 0.001).
Table 3.
Patient Characteristics According to 45 Days Unplanned Readmission Status
| Characteristic | n | No readmission | 45-d Readmission | p Value |
|---|---|---|---|---|
| n (%) | 3,041 | 2729 (89.7) | 312 (10.3) | |
| Age, y, mean ± SD | 56.4 ± 12.8 | 56.0 ± 12.6 | 0.575 | |
| Female, n (%) | 1451 (47.7) | 1311 (90.4) | 140 (9.6) | 0.289 |
| Comorbidities, n (%) | ||||
| ASA ≥ 3 | 2002 (65.8) | 1785 (89.2) | 217 (10.8) | 0.141 |
| Hepatitis B or C | 101 (3.3) | 92 (91.1) | 9 (8.9) | 0.642 |
| Jaundice | 83 (2.7) | 68 (81.9) | 15 (18.1) | 0.018 |
| BMI ≥ 30 kg/m2 | 868 (28.5) | 773 (89.1) | 95 (10.9) | 0.406 |
| Diabetes | 297 (9.8) | 256 (86.2) | 41 (13.8) | 0.026 |
| Diagnosis, n (%) | ||||
| Primary liver or biliary tract | 450 (14.8) | 393 (87.3) | 57 (12.7) | 0.068 |
| Colorectal liver metastasis | 1767 (58.1) | 1591 (90.0) | 176 (10.0) | 0.522 |
| Other metastases | 728 (23.9) | 658 (90.4) | 70 (9.6) | 0.511 |
| Benign | 96 (3.2) | 87 (90.6) | 9 (9.4) | 0.772 |
| Multiple lesions, n (%) | 1426 (46.9) | 1277 (89.6) | 149 (10.4) | 0.963 |
| Size ≥ 30 mm, n (%) | 1331 (43.8) | 1184 (89.0) | 147 (11.0) | 0.234 |
| Perioperative, n (%) | ||||
| Right hepatectomy or extended right | 523 (17.2) | 450 (86.0) | 73 (14.0) | 0.002 |
| Left hepatectomy or extended left | 183 (6.0) | 159 (86.9) | 24 (13.1) | 0.189 |
| Bile duct resection | 153 (5.0) | 118 (77.1) | 35 (22.9) | <0.001 |
| Associated abdominal procedure | 737 (24.2) | 622 (84.4) | 115 (15.6) | <0.001 |
| Time ≥ 180 minutes | 1513 (49.8) | 1333 (88.1) | 180 (11.9) | 0.003 |
| Blood transfusion | 388 (12.8) | 330 (85.1) | 58 (14.9) | 0.001 |
| 90-days mortality | 69 (2.3) | 58 (84.1) | 11 (15.9) | 0.116 |
| Complications, n (%) | ||||
| Liver related | 225 (7.4) | 172 (76.4) | 53 (23.6) | <0.001 |
| Abdominal non liver related | 224 (7.4) | 182 (81.3) | 42 (18.8) | <0.001 |
| Cardiopulmonary or urinary | 273 (9.0) | 242 (88.6) | 31 (11.4) | 0.532 |
| Major complication (Clavien ≥ 3) | 354 (11.6) | 271 (76.6) | 83 (23.4) | <0.001 |
| Discharge, n (%) | ||||
| Length of index stay > 7 d | 965 (31.7) | 814 (84.4) | 151 (15.6) | <0.001 |
| Discharged to other than home | 200 (6.6) | 173 (86.5) | 27 (13.5) | 0.127 |
| Payer other than insurance/Medicare | 158 (5.2) | 142 (89.8) | 16 (10.2) | 0.961 |
| Discharge late period (2006–2013) | 1825 (60.0) | 1628 (89.7) | 197 (10.8) | 0.234 |
In multivariate analysis, factors independently associated with unplanned readmission were: diabetes (odds ratio [OR], 1.6; 95% confidence interval [CI], 1.1–2.3; p = 0.024), right-sided hepatectomy (OR, 2.1; 95% CI, 1.1–4.3; p = 0.034), bile duct resection (OR, 1.9; 95% CI, 1.0–3.6; p = 0.034), major complications during the index stay (OR, 2.4; 95% CI, 1.6–3.7; p < 0.001), and abdominal non-liver-associated complications (OR, 1.8; 95% CI, 1.1–2.7; p = 0.010), as shown in Table 4.
Table 4.
Multivariate Analysis of Factors Associated with 45 Days Unplanned Readmission
| OR | 95% CI | p Value | |
|---|---|---|---|
| ASA ≥ 3 | 1.2 | 0.9–1.6 | 0.303 |
| Jaundice | 0.6 | 0.3–1.4 | 0.212 |
| Diabetes | 1.6 | 1.1.2.3 | 0.024* |
| Primary liver or biliary tract | 1.2 | 0.8–1.8 | 0.27 |
| Right hepatectomy or extended right | 2.1 | 1.1–4.3 | 0.034* |
| Left hepatectomy or extended left | 1.9 | 0.9–3.8 | 0.088 |
| Bile duct resection | 1.9 | 1.0–3.6 | 0.034* |
| Associated abdominal procedure | 1.4 | 1.0–1.9 | 0.081 |
| Operation time > 180 minutes | 1 | 0.7–1.3 | 0.978 |
| Blood transfusion | 1.3 | 0.9–1.8 | 0.183 |
| Liver related complication | 1.5 | 0.9–2.5 | 0.08 |
| Abdominal non-liver related complication | 1.8 | 1.1–2.7 | 0.01* |
| Major complication (Clavien ≥ 3) | 2.4 | 1.6–3.7 | <0.001* |
| Length of index stay > 7 days | 1.2 | 0.9–1.7 | 0.223 |
| Discharged other than home | 1 | 0.6–1.6 | 0.847 |
Significant.
The incidence of both unplanned (r = 0.452, p = 0.079) and planned (r = 0.488, p = 0.055) 45 days readmission trended upwards during the study interval (1998 through 2013), likely correlating with a simultaneous trend toward more extensive surgery.
DISCUSSION
In this large, single-institution series of patients undergoing hepatectomy, the readmission time interval that best defined unplanned readmission was 45 days after discharge from the surgical hospitalization. During this time, patients are at risk for surgery-related complications and should therefore be monitored. Time intervals shorter than this did not capture up to 26.3% of unplanned readmissions, the majority of which were highly relevant to the surgery performed or the index hospitalization (abdominal fluid collection, pleural effusion, wound-related problems, biliary obstruction, cholangitis, pancreatitis, duodenitis, and hepatic insufficiency). However, monitoring beyond this time interval only tends to capture planned readmissions for subsequent treatment independent of surgical complications.
Only a small number of unplanned readmissions occurred after 45 days, with an even distribution between day 46 and day 90. More importantly, unplanned readmissions occurring after 45 days largely comprised readmissions with indications questionably related to the surgery or the index stay, especially if presenting late (dehydration, urinary tract infection, gastroenteritis). Only 12 of the 37 unplanned readmissions after 45 days could reliably be attributed to the index stay or the surgery. It is not always clear when a readmission indication becomes unrelated to the surgery or the index hospital stay—for example, urinary tract infection may or may not be related 2 months after surgery. Many of these patients have advanced cancer diagnoses and comorbid conditions; thus, some baseline medical readmissions within 90 days may be unavoidable.
Traditionally, two start points for monitoring readmissions have been used: from the date of surgery and from the date of discharge.1–7 It is clear from this analysis that the optimal data capture occurs when the time interval begins at discharge and not at the date of surgery. Several factors support this conclusion. First, our analysis and analyses by others clearly indicate that there is an association between postoperative complications and prolonged hospital stay as well as postoperative complications and readmission.1, 4, 7 Second, the decision to intervene to address complications and possibly prevent readmission is made at discharge, when the postoperative course is known. Third, when readmission is measured from the day of surgery, the patients with the most severe complications and subsequently long hospital stays are only monitored for readmission for a short time or even excluded if they stayed for more than 30 days. For example, 195 (6.4%) patients stayed for more than 15 days after surgery, leaving this cohort of patients at risk for readmission only for 15 days or fewer. Moreover, 38 of the 49 patients (78%) with a length of stay that exceeded 30 days, who would have been excluded from the 30 days from surgery definition, were readmitted within 30 days of discharge. Combined, these data indicate that readmission should be reported from discharge and not the date of surgery.
Readmission after hepatectomy and readmission after pancreas surgery should not be assessed together. First, the rate of readmission following pancreatectomy is reported to be higher (15–23%).21–23 Second, modern surgery for liver disease includes a large number of modalities requiring hospital admission (e.g., planned portal vein embolization, radiofrequency ablation, and staged resections), which explains why this cohort of patients experienced a significant number of planned readmissions occurring shortly after discharge. This is also worth noting in studies including all-cause readmissions or in studies that poorly differentiate between unplanned and planned events. After elective surgery, others have advocated that the 30 day from discharge time interval underestimates the readmission rates and suggested 90 days after discharge as the optimal time interval to monitor readmission.24 We acknowledge that the 90 days after discharge time interval would have captured more readmissions than the 45 days after discharge time interval. However, administrative databases may not be able to exclude all planned readmissions and the majority of readmissions occurring after 45 days in the current cohort were either planned or unrelated.
Multivariate analysis clearly showed that the dominant risk factor for readmission was postoperative complications. In some cases, it is difficult to determine whether the complication simply coincides with the readmission or is a preceding factor that could be used to identify patients at risk for readmission. When determining risk factors for readmission, the factors should preferably be actionable with respect to prevention, as such, post-discharge complications causing readmissions may not be optimal to include in the analyses.3 On the basis of this notion, any post-discharge complication that was the direct cause for the readmission was not included when determining risk factors. Others have discussed the timing of complications and readmissions in more detail.2–4
The current study had the following limitations. First, resection of colorectal liver metastases accounted for 58.1% of the hepatectomies. Different treatment algorithms between colorectal liver metastases and other liver lesions, including perioperative chemotherapy, may affect the rates and reasons for readmission. However, the proportion of colorectal liver metastases likely reflects current practice in most centers performing hepatectomies outside hepatitis B and C endemic areas. Second, while clinicopathologic data were collected prospectively in our institutional database, most parameters associated with readmissions were updated retrospectively and could have been subject to underreporting. Third, only readmissions to the same institution were recorded. However, we believe the number of missed readmissions was minimal, as most patients stayed geographically close for outpatient follow-up in the postoperative period or were transferred from other institutions in case of readmission. Finally, a recent report by Brown et al. indicated that readmission rates may not be an appropriate marker of quality of care.25 The authors base this conclusion on the fact that most factors associated with readmission cannot be modified, and also that high-volume centers treating the most challenging patients have higher readmission rates.25 This should not, however, dissuade attempts to lower this rate further. To achieve the best patient and economic outcomes, a balance must be struck between the use of resources associated with prolonged postoperative hospitalization of complex patients and timely discharge with low readmission rates.26
Conclusion
This analysis revealed that readmission patterns are unique to hepatobiliary surgical care and are most accurately captured within 45 days of discharge. We recommend that future quality reporting, studies related to readmission and improvement programs, and regulatory bodies moving forward with institution level comparisons adhere to this time interval. It seems the best measure to reduce readmission is to reduce severe postoperative complications occurring during hospitalization as these are closely associated with readmission after discharge.
Acknowledgments
Support: This research was supported in part by the National Institutes of Health through MD Anderson Cancer Center Support Grant, CA016672. Dr Brudvik is supported by Department of Hepato-Pancreato-Biliary Surgery, Oslo University Hospital, Norway and was awarded The Unger-Vetlesen Medical Fund for 2014.
The authors particularly thank Markeda L Wade for editing the manuscript, Madhura Biswas for providing readmission dates for the cohort, and Ruth J Haynes for secretarial assistance in the preparation of the manuscript.
Footnotes
Disclosure Information: Nothing to disclose.
Presented at the Western Surgical Association 122nd Scientific Session, Indian Wells, CA, November 2014.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Barbas AS, Turley RS, Mallipeddi MK, et al. Examining reoperation and readmission after hepatic surgery. J Am Coll Surg. 2013;216:915–923. doi: 10.1016/j.jamcollsurg.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Kassin MT, Owen RM, Perez SD, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012;215:322–330. doi: 10.1016/j.jamcollsurg.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly KN, Iannuzzi JC, Rickles AS, et al. Risk factors associated with 30-day postoperative readmissions in major gastrointestinal resections. J Gastrointest Surg. 2014;18:35–44. doi: 10.1007/s11605-013-2354-7. [DOI] [PubMed] [Google Scholar]
- 4.Lucas DJ, Sweeney JF, Pawlik TM. The timing of complications impacts risk of readmission after hepatopancreatobiliary surgery. Surgery. 2014;155:945–953. doi: 10.1016/j.surg.2013.12.034. [DOI] [PubMed] [Google Scholar]
- 5.Martin RC, Brown R, Puffer L, et al. Readmission rates after abdominal surgery: the role of surgeon, primary caregiver, home health, and subacute rehab. Ann Surg. 2011;254:591–597. doi: 10.1097/sla.0b013e3182300a38. [DOI] [PubMed] [Google Scholar]
- 6.Schneider EB, Hyder O, Wolfgang CL, et al. Patient readmission and mortality after surgery for hepato-pancreatobiliary malignancies. J Am Coll Surg. 2012;215:607–615. doi: 10.1016/j.jamcollsurg.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spolverato G, Ejaz A, Kim Y, et al. Readmission incidence and associated factors after a hepatic resection at a major hepato-pancreaticobiliary academic centre. HPB (Oxford) 2014;16:972–978. doi: 10.1111/hpb.12262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jweinat JJ. Hospital readmissions under the spotlight. J Healthc Manag. 2010;55:252–264. [PubMed] [Google Scholar]
- 9.Jencks SF. Defragmenting care. Ann Intern Med. 2010;153:757–758. doi: 10.7326/0003-4819-153-11-201012070-00010. [DOI] [PubMed] [Google Scholar]
- 10.Zimmitti G, Roses RE, Andreou A, et al. Greater complexity of liver surgery is not associated with an increased incidence of liver-related complications except for bile leak: an experience with 2,628 consecutive resections. J Gastrointest Surg. 2013;17:57–64. doi: 10.1007/s11605-012-2000-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vauthey JN, Abdalla EK, Doherty DA, et al. Body surface area and body weight predict total liver volume in Western adults. Liver Transpl. 2002;8:233–240. doi: 10.1053/jlts.2002.31654. [DOI] [PubMed] [Google Scholar]
- 12.Kishi Y, Abdalla EK, Chun YS, et al. Three hundred and one consecutive extended right hepatectomies: evaluation of outcome based on systematic liver volumetry. Ann Surg. 2009;250:540–548. doi: 10.1097/SLA.0b013e3181b674df. [DOI] [PubMed] [Google Scholar]
- 13.Chun YS, Ribero D, Abdalla EK, et al. Comparison of two methods of future liver remnant volume measurement. J Gastrointest Surg. 2008;12:123–128. doi: 10.1007/s11605-007-0323-8. [DOI] [PubMed] [Google Scholar]
- 14.Shindoh J, Tzeng CW, Aloia TA, et al. Portal vein embolization improves rate of resection of extensive colorectal liver metastases without worsening survival. Br J Surg. 2013;100:1777–1783. doi: 10.1002/bjs.9317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shindoh J, Tzeng CW, Aloia TA, et al. Safety and efficacy of portal vein embolization before planned major or extended hepatectomy: an institutional experience of 358 patients. J Gastrointest Surg. 2014;18:45–51. doi: 10.1007/s11605-013-2369-0. [DOI] [PubMed] [Google Scholar]
- 16.Shindoh J, Tzeng CW, Aloia TA, et al. Optimal future liver remnant in patients treated with extensive preoperative chemotherapy for colorectal liver metastases. Ann Surg Oncol. 2013;20:2493–2500. doi: 10.1245/s10434-012-2864-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Madoff DC, Abdalla EK, Gupta S, et al. Transhepatic ipsilateral right portal vein embolization extended to segment IV: improving hypertrophy and resection outcomes with spherical particles and coils. J Vasc Interv Radiol. 2005;16:215–225. doi: 10.1097/01.RVI.0000147067.79223.85. [DOI] [PubMed] [Google Scholar]
- 18.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mullen JT, Ribero D, Reddy SK, et al. Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg. 2007;204:854–862. doi: 10.1016/j.jamcollsurg.2006.12.032. [DOI] [PubMed] [Google Scholar]
- 20.Koch M, Garden OJ, Padbury R, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680–688. doi: 10.1016/j.surg.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 21.Sadot E, Brennan MF, Lee SY, et al. Readmission after pancreatic resection: causes and causality pattern. Ann Surg Oncol. 2014;21:4342–4350. doi: 10.1245/s10434-014-3841-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reddy DM, Townsend CM, Jr, Kuo YF, et al. Readmission after pancreatectomy for pancreatic cancer in Medicare patients. J Gastrointest Surg. 2009;13:1963–1974. doi: 10.1007/s11605-009-1006-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahmad SA, Edwards MJ, Sutton JM, et al. Factors influencing readmission after pancreaticoduodenectomy: a multi-institutional study of 1302 patients. Ann Surg. 2012;256:529–537. doi: 10.1097/SLA.0b013e318265ef0b. [DOI] [PubMed] [Google Scholar]
- 24.Fry DE, Pine M, Pine G. Ninety-day postdischarge outcomes of inpatient elective laparoscopic cholecystectomy. Surgery. 2014;156:931–936. doi: 10.1016/j.surg.2014.06.023. [DOI] [PubMed] [Google Scholar]
- 25.Brown EG, Burgess D, Li CS, et al. Hospital readmissions: necessary evil or preventable target for quality improvement. Ann Surg. 2014;260:583–591. doi: 10.1097/SLA.0000000000000923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shah BC, Ullrich F, Smith L, et al. National trends in discharge disposition after hepatic resection for malignancy. HPB (Oxford) 2011;13:96–102. doi: 10.1111/j.1477-2574.2010.00251.x. [DOI] [PMC free article] [PubMed] [Google Scholar]