Abstract
Study Objective
We evaluated shock and traumatic brain injury (TBI) patients previously enrolled in an out-of-hospital clinical trial to test the association between out-of-hospital time and outcome.
Methods
This was a secondary analysis of shock and TBI patients ≥ 15 years enrolled in a Resuscitation Outcomes Consortium out-of-hospital clinical trial by 81 EMS agencies transporting to 46 Level I and II trauma centers in 11 sites (May 2006 through May 2009). Inclusion criteria were: SBP ≤ 70 mmHg or SBP 71 - 90 mmHg with heart rate ≥ 108 beats per minute (shock cohort) and Glasgow Coma Scale score ≤ 8 (TBI cohort); patients meeting both criteria were placed in the shock cohort. Primary outcomes were 28-day mortality (shock cohort) and 6-month Glasgow Outcome Scale - Extended (GOSE) ≤ 4 (TBI cohort).
Results
There were 778 patients in the shock cohort (26% 28-day mortality) and 1,239 patients in the TBI cohort (53% 6-month GOSE ≤ 4). Out-of-hospital time > 60 minutes was not associated with worse outcomes after accounting for important confounders in the shock cohort (adjusted odds ratio [aOR] 1.42, 95% CI 0.77-2.62) or TBI cohort (aOR 0.80, 95% CI 0.52-1.21). However, shock patients requiring early critical hospital resources and arriving > 60 minutes had higher 28-day mortality (aOR 2.37, 95% CI 1.05-5.37); this finding was not observed among a similar TBI subgroup.
Conclusions
Among out-of-hospital trauma patients meeting physiologic criteria for shock and TBI, there was no association between time and outcome. However, the subgroup of shock patients requiring early critical resources arriving after 60 minutes had higher mortality.
INTRODUCTION
Background
The concept that the first 60 minutes following traumatic injury is a critical period for getting patients to a trauma center (the “golden hour”) has been deeply ingrained in trauma systems, national field triage guidelines, emergency medical services (EMS) and clinical care.1,2 While clinical experience suggests that time is critically important in certain trauma patients, there is little empiric evidence to directly support the relationship between time and outcome following injury.3 To date, identifying the subgroup of trauma patients for whom shorter time results in better outcomes has remained elusive.
Importance
There have been numerous studies exploring the relationship between out-of-hospital time and outcome following injury.4-14 While a small number of studies suggest that shorter out-of-hospital time and possibly shorter scene time are associated with improved survival,4-6 the majority of studies have failed to substantiate such a relationship.7-14 There have been many challenges and limitations in testing the time-outcome association, including: bias (e.g., longer time accrual in less seriously injured patients results in the appearance that increased time is associated with better outcomes10); unmeasured confounding; in-hospital outcomes; small or highly selected samples; retrospective study designs; and limited analytic methods. Assuming that time is an important determinant of outcome in certain trauma patients, characterizing such patients may allow EMS and trauma systems to run more efficiently, improve outcomes for certain patients, better guide out-of-hospital decision-making and minimize unnecessary risk among EMS personnel and patients.15-17
Goals of This Investigation
In this study, we analyzed two groups of patients (shock and traumatic brain injury [TBI]) previously enrolled in an out-of-hospital clinical trial18,19 to evaluate the association between total out-of-hospital time and outcome (28-day mortality in shock, 6-month neurologic function in TBI). This study was designed to address several limitations of a previous study evaluating the role of time in trauma14 by including more homogenous trauma patients, detailed in-hospital data, subgroups of patients requiring time-dependent hospital interventions and longer-term outcomes.
METHODS
Study Design
This was a secondary analysis of two cohorts of trauma patients (shock and TBI) who were enrolled in an out-of-hospital clinical trial evaluating the use of hypertonic saline and dextran (HSD) after injury.18,19
Setting
Data were collected from May 2006 to May 2009 as part of the Resuscitation Outcomes Consortium (ROC) HSD out-of-hospital clinical trial (ClinicalTrials.gov identifiers NCT00316017 and NCT00316004).18,19 The HSD study was a 3-arm, randomized, double-blind, placebo-controlled clinical trial to evaluate different types of early resuscitation fluid (0.9% saline vs. 7.5% HS vs. 7.5% HS and 6% dextran 70) among patients with field evidence of shock or TBI. This exception from informed consent study was closed early due to futility, with the results showing no outcome differences between treatment groups.18,19 The methodology and data collection used for this study have been previously detailed.20 Eligible patients were identified by 81 EMS agencies (ground and air medical) transporting to 46 Level I and II trauma hospitals in 11 sites across North America (Birmingham, AL; Dallas, TX; Memphis, TN; Milwaukee, WI; Pittsburgh, PA; Portland, OR; San Diego, CA; King County, WA; Ottawa, ON; Toronto, ON; and Vancouver, BC). Institutional Review Boards and Research Ethics Boards from the 11 sites reviewed and approved the HSD trial, which was conducted under the exception from informed consent regulations in the U.S. and Canada.
Selection of Participants
We evaluated two separate cohorts of injured adults evaluated by 9-1-1 advanced life support (ALS) EMS providers at the scene of injury: (1) patients with clinical evidence of hemorrhagic shock (systolic blood pressure [SBP] ≤ 70 mmHg or SBP 71 – 90 mmHg and heart rate ≥ 108 beats per minute at any point during out-of-hospital evaluation) and (2) patients with evidence of TBI (Glasgow Coma Scale [GCS] score ≤ 8 at any point during out-of-hospital evaluation). Patients meeting criteria for both cohorts were grouped in the shock cohort for purposes of analysis. The ROC HSD trial enrolled eligible patients ≥ 15 years (two younger patients of adult size were also enrolled based on initially incorrect ages); all enrolled patients were considered for this analysis. All patients had an intravenous line placed and study fluid initiated by EMS providers. Eligible patients had to be < 4 hours from the injury event, receive < 2 liters of crystalloid prior to enrollment and have planned transport from the scene of injury to a Level I or II trauma center. Exclusion criteria included: pregnancy, children, interhospital transfers, ongoing cardiopulmonary resuscitation, severe hypothermia, drowning, asphyxia due to hanging, burns > 20% of total body surface area, isolated penetrating injury to the head and incarceration/police custody.
We defined several a priori subgroups of patients for analysis based on plausible clinical mechanisms between time and outcome. Subgroups included: penetrating versus blunt injury, ground versus air transport and patients requiring early critical trauma resources. We defined “early critical trauma resources” as any of the following within 24 hours of emergency department (ED) arrival: packed red blood cell transfusion ≥ 6 units, major non-orthopedic surgical procedures (brain, spine, neck, thoracic, abdominal, pelvic and vascular), interventional radiology procedures or death. Patients who died within 24 hours were included to minimize survivor bias by retaining high-risk patients who may not have survived long enough to undergo critical interventions. Our definition for early critical trauma resources is similar to a recent consensus definition for patients requiring immediate care in major trauma centers.21
Methods and Measurements
The primary exposure variable was total out-of-hospital time, calculated from time of initial 9-1-1 call to time of EMS arrival at the receiving hospital ED. For patients with multiple sources of time records (e.g., dispatch, two or more patient care reports from different EMS agencies), data abstractors resolved discrepancies to produce the most accurate representation of time. There were strict quality assurance processes for data collection with the HSD trial.20 We did not evaluate sub-intervals of out-of-hospital time (e.g., response, on-scene, transport) because these intervals were not consistently captured in the trial.
We collected several additional out-of-hospital variables, including: patient demographics (age, sex), mechanism of injury (gunshot wound, stab/impalement, fall, motor vehicle occupant, motor vehicle vs. pedestrian or cyclist, motorcycle, struck, machinery or crushing injury), lowest SBP (in mmHg), initial Glasgow Coma Scale (GCS) score, highest and lowest heart rate (in beats/minute), advanced airway procedures (attempted intubation [endotracheal or nasal], supraglottic airway or cricothyrotomy), intravenous or intraosseus line placement, medication administration (paralytics, sedatives), field disposition and transport mode (ground ambulance versus helicopter).
Hospital variables included measures of injury severity (Abbreviated Injury Scale [AIS] score, Injury Severity Score [ISS]), non-orthopedic and orthopedic surgical interventions, the timing and volume of blood product transfusion, intensive care unit (ICU) duration of stay, total length of hospital stay (LOS) and in-hospital mortality.
Outcomes
We used the same primary outcomes captured in the HSD trial. For the shock cohort, the primary outcome was 28-day mortality. For the TBI cohort, the primary outcome was 6-month Glasgow Outcome Scale - Extended (GOSE). When possible, GOSE was collected directly from the patient via a structured phone interview. If the patient was unable, a family member or caregiver was allowed to provide the information. We dichotomized 6-month GOSE into poor outcome (severe disability or death, GOSE ≤ 4) versus good outcome (moderate or no disability, GOSE ≥ 5). We used mortality information to supplement the GOSE outcome, as collected from hospital records, phone follow-up and public records. For the TBI cohort, we considered 28-day mortality a secondary outcome.
Analysis
We used descriptive statistics to compare patients in each cohort by total outof-hospital time ≤ 60 versus > 60 minutes. We then used multivariable logistic regression models to test the association between out-of-hospital time and outcome in the shock and TBI patient groups, analyzed separately. The time-outcome association was evaluated using multiple configurations of the time variable in separate models to comprehensively evaluate this relationship: continuous (linear association with outcome), spline regression (continuous, non-linear association with outcome), polytomous categorical (31 – 45, 46 – 60 and > 60 minute categories with ≤ 30 minutes as the reference), and dichotomous (≤ 60 versus > 60 minutes). We considered the dichotomous time variable a direct test of the “golden hour” concept in each cohort.
Multivariable models included plausible confounders of the time-outcome association and known predictors of outcome in trauma. We considered the following variables in the models: age (linear spline with knot at 45 years), sex, ISS, penetrating injury (shock model only), head AIS (TBI model only), SBP, GCS, heart rate, advanced airway attempt, mode of transport, and ROC site (fixed effect). To reduce bias and preserve study power, we used multiple imputation to handle missing values.22 We imputed the following key variables (% missing): age (0.1%), ISS (3.1%), heart rate (0.3%), head AIS (0.7% TBI cohort), SBP category (0.8% TBI cohort), 28-day mortality (0.7% TBI cohort) and GOSE (14.9% TBI cohort). The validity of multiple imputation for imputing missing out-of-hospital values and trauma data has been demonstrated under a variety of conditions.23,24 Twenty multiply imputed datasets were generated, each analyzed independently and combined using Rubin's method to appropriately account for variance within- and between-datasets.22 We assessed model fit using the Hosmer-Lemeshow goodness of fit test and examined diagnostic plots for change in coefficients (delta-beta) when individual episodes were excluded from the analysis. Analyses were conducted using R v3.01 (R Core Team, 2013) and the following R libraries: mice v2.16 and mitools v2.2.
RESULTS
Characteristics of Study Subjects
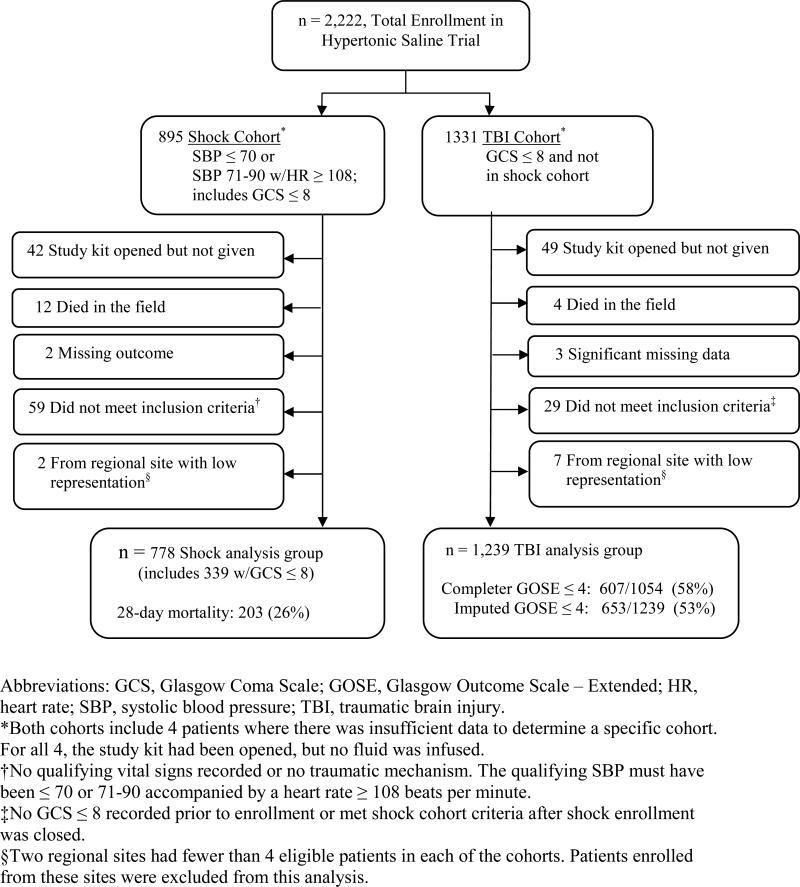
Of the 2,222 patients enrolled in the HSD trial, 2,017 met our study inclusion criteria and were retained for the primary sample. Two hundred five patients were excluded from the analysis for the following reasons: clinical trial study kit opened but not given, death in the field, missing key data, did not meet inclusion criteria and enrollment from a regional site with low representation (Figure 1). The primary sample included 778 patients in the shock cohort and 1,239 patients in the TBI cohort (Figure 1). Three hundred thirty-nine patients in the shock cohort also had an out-of-hospital GCS ≤ 8. Among patients with shock, 203 (26%) died within 28 days of injury. For the TBI cohort, 652 (53%) patients had GOSE ≤ 4 (including death) at 6 months and 304 (25%) died within 28 days. Characteristics of both cohorts, stratified by out-of-hospital time ≤ 60 versus > 60 minutes, are presented in Table 1. Shock patients with times longer than 60 minutes tended to be older, have more advanced airway interventions, air transport, blunt injury and slightly higher injury severity. TBI patients with times longer than 60 minutes tended to have more advanced airway interventions, air transport, motor vehicular mechanisms and higher injury severity.
Figure 1.
Flow diagram of patients included in the primary analysis.
Abbreviations: GCS, Glasgow Coma Scale; GOSE, Glasgow Outcome Scale – Extended; HR, heart rate; SBP, systolic blood pressure; TBI, traumatic brain injury.
*Both cohorts include 4 patients where there was insufficient data to determine a specific cohort. For all 4, the study kit had been opened, but no fluid was infused.
†No qualifying vital signs recorded or no traumatic mechanism. The qualifying SBP must have been ≤ 70 or 71-90 accompanied by a heart rate ≥ 108 beats per minute.
‡No GCS ≤ 8 recorded prior to enrollment or met shock cohort criteria after shock enrollment was closed.
§Two regional sites had fewer than 4 eligible patients in each of the cohorts. Patients enrolled from these sites were excluded from this analysis.
Table 1.
Characteristics of the two trauma patient cohorts, stratified by total out-of-hospital time.
| Shock cohort, n = 778 | TBI cohort, n = 1,239 | |||
|---|---|---|---|---|
| Out-of-hospital time ≤ 60 minutes | Out-of-hospital time > 60 minutes | Out-of-hospital time ≤ 60 minutes | Out-of-hospital time > 60 minutes | |
| n = 604 | n = 174 | n = 914 | n = 325 | |
| Demographics: | ||||
| Age in years – median (IQR) | 31 (23-45) | 38 (26-54) | 35 (24-52) | 33 (22-47) |
| Women (%) | 121 (20) | 52 (30) | 211 (23) | 84 (26) |
| Out-of-hospital physiology and procedures: | ||||
| SBP in mmHg – median (IQR) | 68 (ND**-80) | 70 (60-85) | 130 (111-150) | 130 (110-147) |
| GCS – median (IQR) | 12 (4-15) | 11 (3-15) | 4 (3-7) | 5 (3-7) |
| Heart rate in beats/minute – median (IQR) | 120 (108-132) | 120 (110-135) | 101 (86-120) | 110 (93-125) |
| Advanced airway attempt (%) | 223 (37) | 94 (54) | 521 (57) | 282 (87) |
| Air medical transport (%) | 92 (15) | 119 (68) | 242 (26) | 255 (78) |
| Mechanism of Injury: | ||||
| Gunshot wound (%) | 154 (25) | 9 (5) | 16 (2) | 2 (1) |
| Stabbing/impalement (%) | 99 (16) | 9 (5) | 2 (0) | 0 (0) |
| Other penetrating (%) | 16 (3) | 1 (1) | 0 (0) | 0 (0) |
| Motor vehicle crash (MVC) - occupant (%) | 127 (21) | 93 (53) | 300 (33) | 181 (56) |
| Motorcyclist (%) | 49 (8) | 23 (13) | 87 (10) | 38 (12) |
| MVC – Bicyclist/Pedestrian (%) | 65 (11) | 10 (6) | 161 (18) | 22 (7) |
| Fall (%) | 55 (9) | 13 (7) | 207 (23) | 39 (12) |
| Assault (%) | 21 (3) | 2 (1) | 86 (9) | 13 (4) |
| Other blunt (%) | 18 (3) | 14 (8) | 54 (6) | 30 (9) |
| Hospital measures: | ||||
| Transport to Level I (%) | 527 (87) | 160 (92) | 762 (83) | 307 (94) |
| Transport to Level II (%) | 72 (12) | 12 (7) | 140 (15) | 18 (6) |
| Injury severity: | ||||
| Median ISS (IQR) | 22 (10-34) | 25 (17-34) | 25 (14-34) | 29 (21-41) |
| ISS >= 16 (%) | 407 (67) | 137 (79) | 673 (74) | 278 (86) |
| Hospital resources within the 1st 24 hours: | ||||
| Median PRBC transfusion (IQR) | 2 (0-7) | 2 (0-6) | 0 (0-0) | 0 (0-2) |
| PRBC transfusion ≤ 1 unit (%) | 370 (61) | 101 (58) | 218 (24) | 98 (30) |
| PRBC transfusion ≤ 6 units (%) | 173 (29) | 45 (26) | 62 (7) | 31 (10) |
| Craniotomy (%) | 16 (3) | 6 (3) | 129 (14) | 41 (13) |
| Thoracic surgery (%) | 84 (14) | 17 (10) | 14 (2) | 5 (2) |
| Abdominal or pelvic surgery (%) | 179 (30) | 36 (21) | 51 (6) | 24 (7) |
| Peripheral vascular surgery (%) | 55 (9) | 7 (4) | 2 (0) | 3 (1) |
| Neck surgery (%) | 9 (1) | 1 (1) | 0 (0) | 1 (0) |
| Interventional radiology procedures (%) | 45 (7) | 11 (6) | 16 (2) | 5 (2) |
| Open fixation of fracture (%) | 69 (11) | 29 (17) | 59 (6) | 21 (6) |
| Critical resource use within 24 hours* (%) | 391 (65) | 93 (53) | 293 (32) | 109 (34) |
| Outcomes: | ||||
| Death within 1st 24 hours (%) | 127 (21) | 37 (21) | 114 (13) | 41 (13) |
| In-hospital mortality (%) | 159 (26) | 48 (28) | 226 (25) | 83 (26) |
| 28-day mortality (%) | 157 (26) | 46 (26) | 225 (25) | 78 (24) |
| 6-month GOSE ≤ 4 (%) | - - | - - | 473 (52) | 179 (55) |
Abbreviations: GCS, Glasgow Coma Scale; GOSE, Glasgow Outcome Scale-Extended; IQR, interquartile range; ISS, Injury Severity Score; PRBC, packed red blood cells; SBP, systolic blood pressure; TBI, traumatic brain injury.
Critical resource use was defined as any of the following within 24 hours of emergency department arrival: packed red blood cell transfusion ≥ 6 units, major non-orthopedic surgical procedures (brain, spine, neck, thoracic, abdominal, pelvic and vascular), interventional radiology procedures or death
ND, not detectable
Main Results
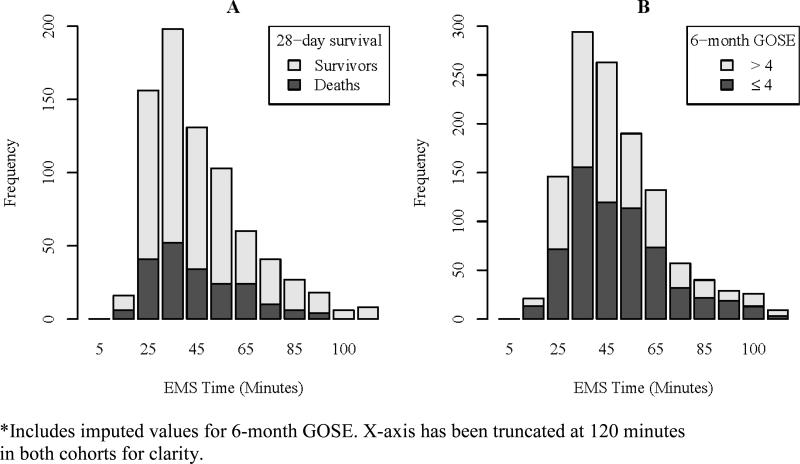
The median total out-of-hospital time was 44 minutes (IQR 33-60) for the full sample, 41 minutes (IQR 31-59) for the shock cohort and 46 minutes (IQR 35-61) for the TBI cohort. There were 174 (22%) patients with out-of-hospital time > 60 minutes in the shock cohort and 325 (26%) patients in the TBI cohort. Across the 11 sites, the shock cohort median out-of-hospital time ranged from 35 to 75 minutes and from 38 to 65 minutes for patients with TBI. The distribution of total out-of-hospital time for each cohort, including the unadjusted proportion of patients incurring primary outcomes, is illustrated in Figure 2.
Figure 2.
Total out-of-hospital time and unadjusted primary outcomes for the (A) shock cohort (n = 778) and (B) traumatic brain injury cohort (n = 1,239).*
*Includes imputed values for 6-month GOSE. X-axis has been truncated at 120 minutes in both cohorts for clarity.
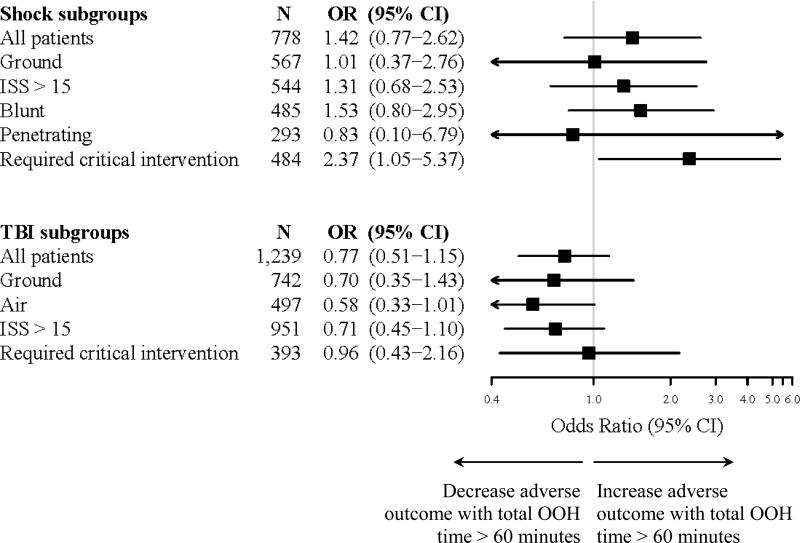
In multivariable logistic regression models for the shock cohort, total out-of-hospital time was not associated with 28-day mortality (Table 2). These results persisted using a variety of methods for modeling the time variable, including continuous, spline, dichotomous and polytomous terms (Table 3). Among subgroup analyses, only shock patients requiring early critical interventions had an adjusted association between out-of-hospital time > 60 minutes and increased mortality (OR 2.37, 95% CI 1.05, 5.37). For patients with TBI, total out-of-hospital time was not associated with neurologic outcome at 6 months or 28-day mortality (Table 4). Similarly, there was no time-outcome association among TBI patients when the time variable was modeled in different forms or evaluated in subgroups (Table 5). These results did not qualitatively change when HSD treatment arm and a dichotomous version of heart rate (≤ 110 vs. > 110 beats/minute) were included in the models (data not shown).
Table 2.
Multivariable logistic regression model evaluating the association between total out-of-hospital time and 28-day mortality among the shock cohort (n = 778).*
| Unadjusted |
Adjusted |
|||
|---|---|---|---|---|
| Modeled variables† | Odds Ratio | 95% CI | Odds Ratio | 95% CI |
| Total EMS time (minutes) | ||||
| ≤ 30 (n=172) | 1.00 | reference | 1.00 | reference |
| 30-45 (n=271) | 0.94 | (0.61, 1.45) | 0.97 | (0.52, 1.82) |
| 45-60 (n=161) | 0.85 | (0.52, 1.39) | 0.69 | (0.33, 1.46) |
| > 60 (n=174) | 0.96 | (0.59, 1.54) | 1.16 | (0.51, 2.65) |
| Age | ||||
| per 5-year increment for age < 45 | 0.96 | (0.88, 1.06) | 1.02 | (0.89, 1.16) |
| per 5-year increment for age ≥ 45 | 1.17 | (1.06, 1.29) | 1.45 | (1.25, 1.68) |
| Male | 0.86 | (0.59, 1.26) | 0.84 | (0.49, 1.46) |
| Penetrating injury | 0.60 | (0.42, 0.84) | 3.31 | (1.79, 6.12) |
| Injury severity score (ISS) | 1.06 | (1.04, 1.07) | 1.06 | (1.04, 1.07) |
| Qualifying SBP range (mmHg) | ||||
| ≤ 50 | 4.57 | (2.74, 7.61) | 6.58 | (3.06, 14.16) |
| 51-60 | 2.26 | (1.21, 4.24) | 4.55 | (1.89, 10.94) |
| 61-70 | 1.45 | (0.82, 2.55) | 3.32 | (1.48, 7.45) |
| 71-80 | 1.30 | (0.70, 2.44) | 2.61 | (1.13, 6.01) |
| 81-90 | 1.00 | reference | 1.00 | reference |
| Highest heart rate (beats/m) | ||||
| < 50 | 24.88 | (5.50, 112.45) | 6.90 | (1.16, 40.94) |
| 50-110 | 1.00 | reference | 1.00 | reference |
| > 110 | 1.15 | (0.81, 1.65) | 1.61 | (0.95, 2.72) |
| Initial GCS (per increment of 1) | 0.76 | (0.73, 0.80) | 0.83 | (0.78, 0.88) |
| Advanced airway attempted | 7.67 | (5.31, 11.07) | 5.02 | (2.58, 9.77) |
| Air transport | 1.14 | (0.80, 1.63) | 0.49 | (0.24, 0.99) |
Abbreviations: CI, confidence interval; EMS, emergency medical services; GCS, Glasgow Coma Scale; SBP, systolic blood pressure.
Site was included in the model as a fixed effects term to account for clustering.
The polytomous time variable is presented for clarity and detail across segments of time. We used multiple imputation for the following variables (counts): age (1), ISS (31), heart rate (4), and GCS (1). Partial Abbreviated Injury Scale (AIS) data were available for all patients missing ISS score. Age modeled as spline with one knot specified at 45 years.
Table 3.
The adjusted time-outcome association for the full shock cohort and shock subgroups (outcome = 28-day mortality) using different out-of-hospital time variables.*
| Total EMS time (minutes) | All patients (n=778) |
Ground (n=567) |
ISS > 15 (n=544) |
Blunt (n=485) |
Penetrating (n=293) |
Required critical intervention (n=484) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Polytomous | ||||||||||||
| ≤ 30 | 1.00 | reference | 1.00 | reference | 1.00 | reference | 1.00 | reference | 1.00 | reference | 1.00 | reference |
| 30-45 | 0.97 | (0.52, 1.82) | 0.95 | (0.47, 1.93) | 0.86 | (0.43, 1.71) | 0.64 | (0.28, 1.51) | 1.38 | (0.46, 4.13) | 1.19 | (0.56, 2.54) |
| 45-60 | 0.69 | (0.33, 1.46) | 0.81 | (0.33, 2.02) | 0.56 | (0.25, 1.29) | 0.34 | (0.13, 0.90) | 1.34 | (0.31, 5.81) | 0.97 | (0.38, 2.45) |
| > 60 | 1.16 | (0.51, 2.65) | 0.93 | (0.30, 2.88) | 0.92 | (0.37, 2.26) | 0.76 | (0.28, 2.02) | 1.09 | (0.11, 11.12) | 2.48 | (0.83, 7.43) |
| Dichotomous | ||||||||||||
| > 60 | 1.42 | (0.77, 2.62) | 1.01 | (0.37, 2.76) | 1.31 | (0.68, 2.53) | 1.53 | (0.80, 2.95) | 0.83 | (0.10, 6.79) | 2.37 | (1.05, 5.37) |
| Continuous | ||||||||||||
| per 5 min | 0.97 | (0.92, 1.03) | 0.95 | (0.88, 1.03) | 0.98 | (0.91, 1.04) | 0.97 | (0.91, 1.04) | 0.93 | (0.83, 1.06) | 1.03 | (0.95, 1.12) |
| Spline | ||||||||||||
| ≤ 30 | 0.80 | (0.45, 1.41) | 0.81 | (0.43, 1.51) | 0.83 | (0.45, 1.55) | 0.54 | (0.23, 1.24) | 1.15 | (0.37, 3.56) | 0.93 | (0.47, 1.86) |
| 30-45 | 0.99 | (0.73, 1.34) | 1.04 | (0.73, 1.48) | 0.93 | (0.67, 1.30) | 0.91 | (0.62, 1.34) | 1.00 | (0.55, 1.79) | 1.00 | (0.69, 1.44) |
| 45-60 | 1.01 | (0.75, 1.35) | 0.93 | (0.62, 1.41) | 0.99 | (0.72, 1.36) | 1.04 | (0.74, 1.46) | 1.12 | (0.48, 2.59) | 1.17 | (0.80, 1.71) |
| > 60 | 0.97 | (0.89, 1.05) | 0.94 | (0.80, 1.10) | 0.99 | (0.90, 1.09) | 0.99 | (0.91, 1.09) | 0.85 | (0.64, 1.14) | 1.01 | (0.89, 1.14) |
Abbreviations: AIS, Abbreviated Injury Scale; CI, confidence interval; EMS, emergency medical services; GCS, Glasgow Coma Scale; ISS, Injury Severity Score; OR, odds ratio; SBP, systolic blood pressure.
The following covariates were included in the model: age (spline with one knot at 45 yrs), gender, penetrating injury (except for blunt and penetrating subgroups), ISS, qualifying SBP category, heart rate category, GCS, advanced airway attempt, air transport (except for ground subgroup) and site. We used multiple imputation used for the following variables (counts): age (1), ISS (31), heart rate (4), and GCS (1). Partial AIS data were available for all patients missing ISS score. Time is modeled using four different methods: polytomous with reference category ≤ 30 minutes, dichotomous with reference category ≤ 60 minutes, continuous (per 5 minute increments), and spline (per 5 minute time difference in each range).
Table 4.
Multivariable logistic regression model evaluating the association between total out-of-hospital time and outcome among the TBI cohort (n = 1,239).*
| 6-Month GOSE ≤ 4 | 28-Day Mortality | |||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted |
Adjusted |
Unadjusted |
Adjusted |
|||||
| Modeled variables† | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI | Odds Ratio | 95% CI |
| Total EMS time (minutes) | ||||||||
| ≤ 30 (n=160) | 1.00 | reference | 1.00 | reference | 1.00 | reference | 1.00 | reference |
| 30-45 (n=431) | 0.90 | (0.63, 1.31) | 0.92 | (0.57, 1.49) | 0.80 | (0.53, 1.22) | 0.74 | (0.43, 1.27) |
| 45-60 (n=315) | 1.28 | (0.87, 1.88) | 1.23 | (0.73, 2.07) | 1.12 | (0.73, 1.72) | 1.06 | (0.58, 1.93) |
| > 60 (n=333) | 1.19 | (0.81, 1.74) | 0.83 | (0.45, 1.52) | 0.91 | (0.59, 1.40) | 0.67 | (0.34, 1.33) |
| Age | ||||||||
| per 5-year increment for age < 45 | 1.09 | (1.02, 1.16) | 1.15 | (1.06, 1.25) | 1.09 | (1.01, 1.19) | 1.15 | (1.04, 1.26) |
| per 5-year increment for age ≥ 45 | 1.31 | (1.20, 1.42) | 1.32 | (1.20, 1.47) | 1.30 | (1.21, 1.40) | 1.35 | (1.24, 1.47) |
| Male | 0.79 | (0.60, 1.04) | 0.98 | (0.68, 1.41) | 0.71 | (0.53, 0.95) | 0.91 | (0.63, 1.32) |
| Injury severity score (ISS) | 1.07 | (1.06, 1.08) | 1.07 | (1.05, 1.08) | 1.05 | (1.04, 1.06) | 1.05 | (1.04, 1.06) |
| Head AIS ≥ 3 | 4.56 | (3.41, 6.10) | 1.72 | (1.14, 2.60) | 4.25 | (2.87, 6.32) | 1.96 | (1.20, 3.19) |
| Initial SBP range (mmHg) | ||||||||
| ≤ 90 | 1.97 | (1.20, 3.25) | 1.65 | (0.88, 3.12) | 2.19 | (1.36, 3.54) | 1.61 | (0.87, 2.96) |
| 91-105 | 1.25 | (0.84, 1.86) | 1.32 | (0.80, 2.16) | 0.95 | (0.60, 1.51) | 0.79 | (0.45, 1.39) |
| 106-120 | 0.76 | (0.56, 1.04) | 0.71 | (0.48, 1.06) | 0.77 | (0.53, 1.12) | 0.73 | (0.46, 1.14) |
| 121-180 | 1.00 | reference | 1.00 | reference | 1.00 | reference | 1.00 | reference |
| > 180 | 3.80 | (2.12, 6.81) | 3.25 | (1.59, 6.68) | 2.67 | (1.68, 4.24) | 1.87 | (1.05, 3.33) |
| Heart rate (beats per min) > 110 | 1.01 | (0.80, 1.29) | 1.20 | (0.88, 1.65) | 0.98 | (0.75, 1.28) | 1.32 | (0.94, 1.85) |
| Qualifying GCS (per increment of 1) | 0.78 | (0.73, 0.83) | 0.78 | (0.72, 0.85) | 0.68 | (0.62, 0.74) | 0.67 | (0.60, 0.74) |
| Advanced airway attempted | 1.59 | (1.25, 2.03) | 0.99 | (0.64, 1.54) | 1.70 | (1.27, 2.27) | 1.50 | (0.92, 2.43) |
| Air transport | 1.53 | (1.21, 1.94) | 0.90 | (0.58, 1.39) | 1.23 | (0.94, 1.59) | 0.88 | (0.55, 1.42) |
Abbreviations: AIS, Abbreviated Injury Scale; CI, confidence interval; EMS, emergency medical services; GCS, Glasgow Coma Scale; SBP, systolic blood pressure; TBI, traumatic brain injury.
Site was included in the model as a fixed effects term to account for clustering.
The polytomous time variable is presented above for clarity and detail across segments of time. We used multiple imputation for the following variables (counts): age (1), ISS (31), head AIS (8), heart rate (2), SBP category (10) and GOSE (185). Partial Abbreviated Injury Scale (AIS) data were available for 27 of the 31 patients missing ISS score. Age modeled as spline with one knot specified at 45 years.
Table 5.
The adjusted time-outcome association for the full TBI cohort and subgroups (outcome = 6-month GOSE ≤ 4) using different out-of-hospital time variables.*
| Total EMS time (minutes) | All patients (n=1,239) |
Ground (n=742) |
Air (n=497) |
ISS > 15 (n=951) |
Required critical intervention (n=393) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Polytomous | ||||||||||
| ≤ 30 | 1.00 | reference | 1.00 | reference | 0.37 | (0.06, 2.32) | 1.00 | reference | 1.00 | reference |
| 30-45 | 0.92 | (0.57, 1.49) | 1.20 | (0.71, 2.05) | 0.51 | (0.08, 3.20) | 0.82 | (0.47, 1.44) | 1.33 | (0.51, 3.50) |
| 45-60 | 1.23 | (0.73, 2.07) | 1.58 | (0.85, 2.92) | 1.00 | reference | 1.06 | (0.58, 1.95) | 1.77 | (0.59, 5.33) |
| > 60 | 0.83 | (0.45, 1.52) | 0.90 | (0.39, 2.07) | 0.28 | (0.04, 1.74) | 0.68 | (0.34, 1.35) | 1.47 | (0.44, 4.98) |
| Dichotomous | ||||||||||
| > 60 | 0.77 | (0.51, 1.15) | 0.70 | (0.35, 1.43) | 0.58 | (0.33, 1.01) | 0.71 | (0.45, 1.10) | 0.96 | (0.43, 2.16) |
| Continuous | ||||||||||
| per 5 min | 0.98 | (0.95, 1.01) | 1.02 | (0.95, 1.09) | 0.94 | (0.91, 0.99) | 0.97 | (0.94, 1.01) | 1.01 | (0.93, 1.09) |
| Spline | ||||||||||
| ≤ 30 | 0.82 | (0.54, 1.25) | 0.96 | (0.62, 1.50) | 0.31 | (0.02, 4.84) | 0.77 | (0.45, 1.31) | 0.65 | (0.26, 1.63) |
| 30-45 | 1.11 | (0.91, 1.36) | 1.22 | (0.96, 1.55) | 1.14 | (0.71, 1.83) | 1.05 | (0.83, 1.32) | 1.13 | (0.74, 1.74) |
| 45-60 | 0.98 | (0.82, 1.17) | 0.86 | (0.65, 1.15) | 0.94 | (0.72, 1.23) | 0.98 | (0.81, 1.20) | 1.04 | (0.71, 1.50) |
| > 60 | 0.97 | (0.93, 1.01) | 1.00 | (0.85, 1.17) | 0.94 | (0.90, 0.99) | 0.97 | (0.93, 1.01) | 1.00 | (0.89, 1.11) |
Abbreviations: AIS, Abbreviated Injury Scale; CI, confidence interval; EMS, emergency medical services; GCS, Glasgow Coma Scale; GOSE, Glasgow Outcome Scale - Extended; ISS, Injury Severity Score; OR, odds ratio; SBP, systolic blood pressure.
The following covariates were included in the model: age (spline with one knot at 45 yrs), gender, ISS, head AIS, initial SBP category, heart rate category, initial GCS, advanced airway attempt, air transport (except for ground and air subgroups), and site. Multiple imputation used for the following variables (counts in parentheses): age (1), ISS (31), head AIS (8), heart rate (2), SBP (10), GCS (1), and GOSE (185). Partial AIS data were available for 27 of the 31 patients missing ISS score. Time is modeled using four different methods: polytomous with reference category ≤ 30 minutes, dichotomous with reference category ≤ 60 minutes, continuous (per 5 minute increments), and spline (per 5 minute time difference in each range).
The primary models were well-fit (Hosmer-Lemeshow goodness of fit statistic p = 0.69 for the shock cohort and p = 0.47 for the TBI cohort). There was no evidence of effect modification between time and clinical variables in the shock cohort (all interactions p > .05). In the TBI cohort, there was suggestion of effect modification in two terms: time × head AIS ≥ 3 (p = .01) and time × ISS ≥ 16 (p = .03). While these TBI interactions suggest that the association between time and outcome was modified by injury severity, the direction of effect was not clinically plausible and did not change the overall results.
Results from pre-defined subgroup analyses for multivariable models using the dichotomous time variable are presented in Figure 3. Among the shock cohort, the only subgroup with an association between longer out-of-hospital time and greater 28-day mortality was the group requiring early critical resources (aOR > 60 minutes vs. ≤ 60 minutes 2.37, 95% CI 1.05-5.37). Using different definitions of total out-of-hospital time (continuous, polytomous, spline) among the same subgroup demonstrated similar findings, though none reached statistical significance (Table 3). As a sensitivity analysis for the early critical resources subgroup, we excluded 27 patients with no signs of life upon arrival to the ED who had no procedures and were declared dead within 30 minutes of ED arrival (i.e., it is possible these patients had fatal injuries recognized by EMS personnel with longer times to reach the hospital due to field-based interventions or other factors). This analysis produced a similar point estimate, but a wider 95% CI that did not reach statistical significance (aOR > 60 minutes vs. ≤ 60 minutes 2.14, 95% CI 0.91-5.04). There were no TBI subgroups that demonstrated a statistical association between longer time (> 60 minutes) and worse 6-month neurologic outcome (all p > 0.05) or greater 28-day mortality (all p > 0.05). Subgroup analyses for the TBI cohort using different versions of the time variable in multivariable models are presented in Table 5.
Figure 3.
Subgroup analyses for shock (outcome = 28-day mortality) and traumatic brain injury (outcome = 6-month GOSE ≤ 4) cohorts using multivariable models and a dichotomous out-of-hospital time variable (> 60 minutes vs. ≤ 60 minutes).
As an additional sensitivity analysis, we conducted survival analyses for both cohorts using 28-day mortality. The lack of statistical association between out-of-hospital time (≤ 60 minutes vs. > 60 minutes) and mortality persisted in the shock cohort (hazard ratio [HR] 1.38, 95% CI .91 – 2.08) and TBI cohort (HR 0.82, 95% CI 0.59 – 1.13). Two shock subgroups demonstrated an association between longer out-of-hospital time and increased mortality: patients requiring early critical resources (HR 1.56, 95% CI 1.00 – 2.43) and patients injured by a blunt mechanism (HR 1.62, 95% CI 1.02 – 2.57). Other shock subgroups had no association. There were no TBI subgroups with an association between time and mortality in the survival analyses.
LIMITATIONS
Many factors influence out-of-hospital time, some of which may confound the association between time and outcome. Traditional injury severity measures, patient demographics, mechanism of injury, physiologic response to injury and out-of-hospital procedures may not fully account for such confounding, which creates challenges in evaluating the true influence of time on outcome. Unmeasured factors related to patient prognosis can influence EMS provider behavior (e.g., less time on scene, light-and-sirens transport and faster driving), which in turn influences time. These relationships often result in patients with the worst prognosis (and therefore poor outcomes) having shorter out-of-hospital times, as illustrated in Figure 2. In observational research, it is difficult to fully account for all factors explaining the prognostic differences between patients and resulting EMS provider behavior. Such bias and confounding can create the appearance that longer time results in better outcomes (e.g., the air medical subgroup of TBI patients in Table 5) and create difficulty in generating a completely unbiased assessment of the time-outcome association. Use of techniques such as instrumental variable analysis have been used in EMS and trauma research to account for such unmeasured confounding and bias,14,25-27 though an appropriate instrument was not available in these data.
In addition, the database used for this study provided a fixed number of patients in each cohort, including those with field times greater than 60 minutes. It is possible that a larger overall sample size or larger number of patients with prolonged out-of-hospital times would have increased the power to detect an association between time and outcome. Furthermore, this study was a secondary analysis of data from a clinical trial, rather than a study powered specifically to address the question of a time-outcome association. While the 95% confidence interval around each cohort's point estimate for the time-outcome association crosses one and we conclude that there is no association, it is possible that the true association lies within this range and may be detectable with a larger sample powered to directly address this study question.
While our results suggest that arriving within 60 minutes to a major trauma center may result in better survival for shock patients requiring early critical interventions, this finding was from a subgroup analysis. Subgroup analyses have known limitations28 and this time-outcome association did not persist using all versions of the time variable. Whether these findings reflect differences in statistical efficiency (e.g., a larger reference group in the dichotomous term) or chance is unclear. The definition used to identify this subgroup was based on expert consensus21 and was similar to resource-based definitions used in many previous trauma studies,29-36 though it is possible that a different definition for this subgroup would have produced different findings. Nonetheless, we did specify this subgroup analysis a priori and there is good biologic plausibility for the findings. However, these results require confirmation in additional studies before the relationship can be considered conclusive. The survival analysis suggested that shock patients with a blunt mechanism requiring more than 60 minutes to arrive at a trauma center also have increased mortality, though this finding was from a sensitivity analysis and did not appear in the primary results. Furthermore, the data used for the present study came from a randomized controlled trial conducted in high-functioning ALS EMS agencies with direct transport to major trauma centers; our results may not generalize to regions with different resources or non-ALS EMS systems.
Finally, out-of-hospital time represents only one portion of the time continuum following injury. We were not able to account for the time between injury and 9-1-1 call or the time from ED arrival to hospital-based definitive care (for patients requiring such care). These additional time components are also likely to be important in evaluating the role of time in determining outcome following injury. However, one distinction with outof-hospital time is that this time interval is a modifiable component of trauma systems. That is, system-level operational changes can be implemented to increase or decrease total out-of-hospital time for certain patients in an effort to further optimize trauma systems and health outcomes.
DISCUSSION
In this study, we did not find an association between longer out-of-hospital time and worse outcomes among injured patients with field-based physiologic markers of shock and TBI. However, the subgroup of shock patients requiring early critical hospital interventions and arriving at a major trauma center greater than 60 minutes from 9-1-1 call were more likely to die within 28 days. Patients with TBI did not demonstrate a similar association. While our primary findings are consistent with a large number of previous studies demonstrating no association between time and outcome following injury,6-13 the subgroup results identify a population of injured patients where time may play an important role in determining outcome.
Although the concept of the “golden hour” and expeditious trauma care is a cornerstone of trauma systems, small differences in time (e.g., minutes) are unlikely to play a crucial role in determining outcome for all trauma patients. Many patients served by EMS will have non-life threatening injuries that do not require time-dependent intervention, even when physiologic compromise is present.18-20,37 However, clinical experience suggests that time can be critical in determining outcomes for certain trauma patients. The challenge has been in identifying and defining which patients have time-dependent injuries where out-of-hospital time may have a direct impact on outcome. Pushing for the fastest possible out-of-hospital care in every trauma patient (e.g., through lights-and-siren use, rapid driving and air medical transport) can create unnecessary risks to EMS providers, patients and the nearby public,15-17 while also being a common source of tort claims against EMS agencies.38 The EMS resources needed for rapid response and transport typically require comprehensive ambulance coverage, increased EMS staffing, and air medical services, all of which are expensive to sustain. In certain regions, it may not be possible to reach a major trauma center within 60 minutes due to geography, weather, extrication delays and other factors. In seeking to further optimize trauma systems, identifying which patients have better outcomes from rapid out-of-hospital care and which patients can be safely managed without such time constraints may help improve patient outcomes, reduce EMS occupational risks, reduce system costs and increase system efficiency.
Our findings add to the existing body of literature evaluating the role of time following injury. The only clinical conditions where out-of-hospital time has been consistently linked to outcome are non-traumatic cardiac arrest (response interval)39,40 and ST-elevation myocardial infarction (total out-of-hospital time).41 Time is also closely associated with outcome in stroke,42,43 though the relationship between out-of-hospital time and outcome following stroke has not been directly evaluated. One study suggested that shorter EMS response times were linked to improved survival among a mixed sample of patients served by EMS,25 though this finding has not been replicated in other studies.44,45 Among injured patients, the majority of previous studies evaluating the association between time and outcome have demonstrated no relationship.7-14 Our primary findings were similar, despite including patients with physiologic decompensation and accounting for multiple confounders. While out-of-hospital hypotension and depressed GCS are intended to identify the highest risk trauma patients for immediate transport to major trauma centers,1,2,46,47 these physiologic measures remain relatively crude tools in identifying patients with true time-dependent illness.
Our study is unique in suggesting one plausible subgroup of trauma patients where out-of-hospital time may be linked to outcome. Shock patients who required early critical interventions had higher adjusted survival when arriving within 60 minutes to a major trauma center. However, a similar TBI subgroup did not demonstrate such findings. These results will require confirmation before influencing EMS and trauma system operations. However, if confirmed, the ability to use these results in practice will also be contingent on being able to identify this important subgroup of patients with readily available information in the field. Current field trauma triage guidelines are generally designed to identify patients with serious injuries46 and therefore are not specific enough to separate out patients with time-dependent illness from those with less time-sensitive injuries. While we did not have enough information available in these data to determine specific types of injuries or clinical conditions represented in the group of patients requiring early critical interventions, this subgroup provides a target group for whom clinical decision rules could be developed using information readily available to EMS personnel. We have recently derived preliminary field-based decision rules for identifying such high-risk patients among a larger group of hypotensive trauma patients.48
There are several potential explanations for the lack of a time-outcome association among TBI patients. First, not all patients with GCS ≤ 8 had serious TBI, illustrating the lack of precision in current out-of-hospital physiologic measures in identifying high-risk patients. Second, the management of patients with TBI is complex, with many factors affecting outcome, including the severity and type of brain injury, age, physiologic response to injury, oxygenation, comorbidities, pre-injury medication use, early resuscitative care, surgical decision-making and critical care management. That is, time is but one factor involved in a complex combination of factors affecting outcome following TBI.
CONCLUSIONS
Among out-of-hospital trauma patients meeting physiologic criteria for shock and TBI, there was no overall association between time and outcome. However, in the subgroup of shock patients requiring early critical hospital interventions, arriving at a major trauma center within 60 minutes of 9-1-1 call was associated with higher 28-day survival.
ACKNOWLEDGMENTS
We want to acknowledge and thank the many contributing EMS agencies, EMS providers, study coordinators, staff, and investigators for their willingness to participate in and support this project, and for their continued dedication to improving the EMS care and outcomes for their patients.
FUNDING
The ROC is supported by a series of cooperative agreements to multiple regional clinical centers (RCC) and one Data Coordinating Center (5U01 HL077863-University of Washington Data Coordinating Center, HL077866-Medical College of Wisconsin, HL077867-University of Washington, HL077871-University of Pittsburgh, HL077872-St. Michael's Hospital, HL077873-Oregon Health and Science University, HL077881-University of Alabama at Birmingham, HL077885-Ottawa Health Research Institute, HL077887-University of Texas SW Medical Ctr/Dallas, HL077908-University of California San Diego) from the National Heart, Lung and Blood Institute in partnership with the U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research (CIHR) - Institute of Circulatory and Respiratory Health, Defence Research and Development Canada, the Heart and Stroke Foundation of Canada, and the American Heart Association. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute or the National Institutes of Health.
Technical Appendix
Analysis Software
All analyses were conducted in R v3.01.1 Multiply imputed datasets were generated using the package mice v2.162 and results from the multiple analyses were combined using functions from the package mitools v2.2.3
Multiple Imputation
For the shock cohort, Injury Severity Score (ISS) was the only measure with any notable missingness: 31 patients (4%). Because of the potential for selection bias in doing a complete case analysis and because we had good information (partial severity score data) from which to impute ISS, we chose to employ multiple imputation in our analyses. There were three other measures with missing values (counts in parentheses): age (1), initial GCS (1), and highest heart rate (4). Several severity-related measures not in the primary analysis model were used in the imputation models to impute ISS. Table 1 shows all the measures used in the shock cohort imputation and analysis models.
For the TBI cohort, the primary outcome, 6-month Glasgow Outcome Scale – Extended (GOSE), was missing for 185 patients (15%) and ISS was missing for 31 patients (3%). In addition, the following measures had missing values (counts in parenthesis): age (1), highest heart rate (2), 28-day mortality (8), head abbreviated injury score (8), and initial systolic blood pressure (10). Several severity-related measures not in the primary analysis model were used in the imputation models to impute GOSE and ISS. The selection of measures for the imputation of GOSE was informed by recent research by Zelnick et al.4 Table 2 shows all measures used in the TBI cohort imputation and analysis models. Twenty complete datasets were generated for each cohort using multivariable imputation by chained equation (MICE),3 also known as fully conditional specification (FCS). Results from the 20 datasets were combined using the method of Rubin,5 as implemented in mitools.
Analysis Models
The columns headed “In analysis model?” in Tables 1 and 2 indicate whether the variable was included in the analysis models for the shock and TBI cohorts. We modeled the EMS time covariate four different ways in separate models: dichotomous (≤ 60 vs. > 60 minutes), polytomous (≤ 30, 30-45, 46-60, and > 60 minutes), continuous, and continuous with spline knots at 30, 45, and 60 minutes. The other covariates are modeled as described in the “Modeled as ...” column for all analysis models.
Appendix Table 1.
Shock Cohort: Characteristics in the Imputation and Analysis Models.
| The following characteristics were included in imputation models to multiply impute values for those characteristics that were missing for one or more patients. | ||||
|---|---|---|---|---|
| In analysis models? | Characteristic | Modeled as ... | # Missing | Imputation method |
| Y | 28-day mortality | Indicator | 0 | |
| Y | EMS Time (minutes)a | Categorical: ≤30, 30-45, 46-60, >60 | 0 | |
| Y | Age | Continuous, spline with knot at 45 years | 1 | PMM |
| Y | Male gender | Indicator | 0 | |
| Y | Penetrating injury | Indicator | 0 | |
| Y | ISSb | Continuous | 31 | PMM |
| Y | Qualifying SBP | Categorical: ≤50, 51-60, 61-70, 71-80, 81-90 | 0 | |
| Y | Highest heart rate (beats/minute) | Categorical: <50, 51-110, >110 | 4 | ML |
| Y | Initial GCS | Continuous | 1 | PMM |
| Y | Out-of-hospital advanced airway attempted | Indicator | 0 | |
| Y | Air transport | Indicator | 0 | |
| Y | Regional site | Categorical - fixed effect | 0 | |
| N | Required critical intervention | Indicator | 0 | |
| N | ISS disposition category | Categorical: Died < 6 hrs, other death, discharge ≥ 2 days, discharge < 2 days, discharge from ED, unknown | 1 | ML |
| N | Serious injury (AIS ≥ 3) to chest or abdomen | Indicator | 4 | LR |
| N | Serious injury (AIS ≥ 3) to extremity | Indicator | 7 | LR |
| N | Serious injury (AIS ≥ 3) to the head | Indicator | 1 | LR |
Abbreviations: AIS, Abbreviated Injury Score; ED, emergency department; GCS, Glasgow Coma Scale; ISS, Injury Severity Score; LR, logistic regression; ML, multinomial logit; PMM, predictive mean modeling; SBP, systolic blood pressure.
EMS time is also used as a continuous variable in some analysis models but not in the imputation models.
In most instances ISS is missing because one of the individual AIS scores is listed as “not otherwise specified” preventing the calculation of the ISS. However, there are other AIS scores available and this information can be used in the imputation process (see last 5 characteristics).
Appendix Table 2.
Traumatic Brain Injury Cohort: Characteristics in the Imputation and Analysis Models.
| The following characteristics were included in imputation models to multiply impute values for those characteristics that were missing for one or more patients. | ||||
|---|---|---|---|---|
| In analysis models? | Characteristic | Modeled as ... | # Missing | Imputation method |
| Y | 6-month GOSE ≤ 4 | Indicator | 185 | LR |
| Y | 28-day mortality | Indicator | 8 | LR |
| Y | EMS Time (minutes)a | Categorical: ≤30, 30-45, 46-60, >60 | 0 | |
| Y | Age | Continuous, spline with knot at 45 years | 1 | PMM |
| Y | Male gender | Indicator | 0 | |
| Y | ISSb | Continuous | 31 | PMM |
| Y | Head AIS ≥ 3 | Indicator | 8 | LR |
| Y | Initial SBP | Categorical: ≤90, 91-105, 106-120, 121-180, >180 | 10 | ML |
| Y | Highest heart rate (beats/minute) > 110 | Indicator | 2 | LR |
| Y | Qualifying GCS | Continuous | 0 | |
| Y | Out-of-hospital advanced airway attempted | Indicator | 0 | |
| Y | Air transport | Indicator | 0 | |
| Y | Regional site | Categorical - fixed effect | 0 | |
| N | Required critical intervention | Indicator | 0 | |
| N | Discharge GOSE | Continuous | 69 | PMM |
| N | Days alive and out of the hospital through day 28; death before 28 days is coded as 0. | Continuous | 13 | PMM |
| N | ISS disposition category | Categorical: Died < 6 hrs, other death, discharge ≥ 2 days, discharge < 2 days, discharge from ED, unknown | 0 | ML |
| N | Serious injury (AIS ≥ 3) to chest or abdomen | Indicator | 0 | LR |
| N | Serious injury (AIS ≥ 3) to extremity | Indicator | 0 | LR |
Abbreviations: AIS, Abbreviated Injury Score; GCS, Glasgow Coma Scale; GOSE, Glasgow Outcome Scale – Extended, ISS, Injury Severity Score; LR, logistic regression; ML, multinomial logit; PMM, predictive mean modeling; SBP, systolic blood pressure.
EMS time is also used as a continuous variable in some analysis models but not in the imputation models.
In most instances ISS is missing because one of the individual AIS scores is listed as “not otherwise specified” preventing the calculation of the ISS. However, there are other AIS scores available and this information can be used in the imputation process.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No authors had conflicts of interest with this study.
Author Contributions
CDN and KB conceived of and designed the study. ENM performed all database management and statistical analyses. All authors helped refine the study plan, interpret preliminary results, and refine the analysis. CDN drafted the manuscript and all authors participated in critical revision of the manuscript. CDN and ENM take full responsibility for the data, results and manuscript as a whole.
R Core Team (2013). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org/.
Stef van Buuren, Karin Groothuis-Oudshoorn (2011). mice: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software, 45(3), 1-67. URL http://www.jstatsoft.org/v45/i03/.
Thomas Lumley (2012). mitools: Tools for multiple imputation of missing data. R package version 2.2. http://CRAN.R-project.org/package=mitools
Zelnick LR, Morrison LJ, Devlin SM, et al. Addressing the challenges of obtaining functional outcomes in traumatic brain injury research: missing data patterns, timing of follow-up, and three prognostic models. J Neurotrauma 2014;31(11):1029-1038. doi:10.1089/neu.2013.3122.
Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons, Inc., 1987.
REFERENCES
- 1.Committee on Trauma . Resources for Optimal Care of the Injured Patient. American College of Surgeons; Chicago, Ill: 2006. [Google Scholar]
- 2.Mackersie RC. History of trauma field triage development and the American College of Surgeons criteria. Prehospital Emergency Care. 2006;10:287–294. doi: 10.1080/10903120600721636. [DOI] [PubMed] [Google Scholar]
- 3.Lerner EB, Moscati RM. The golden hour: scientific fact or medical “urban legend”? Acad Emerg Med. 2001;8:758–760. doi: 10.1111/j.1553-2712.2001.tb00201.x. [DOI] [PubMed] [Google Scholar]
- 4.Sampalis JS, Denis R, Lavoie A, et al. Trauma care regionalization: a process- outcome evaluation. J Trauma. 1999;46:565–581. doi: 10.1097/00005373-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Sampalis JS, Lavoie A, Williams JI, et al. Impact of on-site care, prehospital time, and level of in-hospital care on survival in severely injured patients. J Trauma. 1993;34:252–261. doi: 10.1097/00005373-199302000-00014. [DOI] [PubMed] [Google Scholar]
- 6.McCoy CE, Menchine M, Sampson S, Anderson C, Kahn C. Emergency medical services out-of-hospital scene and transport times and their association with mortality in trauma patients presenting to an urban Level I trauma center. Ann Emerg Med. 2013;61:167–174. doi: 10.1016/j.annemergmed.2012.08.026. [DOI] [PubMed] [Google Scholar]
- 7.Stiell IG, Nesbitt LP, Pickett W, et al. The OPALS major trauma outcome study: impact of advanced life-support on survival and morbidity. CMAJ. 2008;178:1141–1152. doi: 10.1503/cmaj.071154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pepe PE, Wyatt CH, Bickell WH, et al. The relationship between total prehospital time and outcome in hypotensive victims of penetrating injuries. Ann Emerg Med. 1987;16:293–297. doi: 10.1016/s0196-0644(87)80174-9. [DOI] [PubMed] [Google Scholar]
- 9.Petri RW, Dyer A, Lumpkin J. The effect of prehospital transport time on the mortality from traumatic injury. Prehosp Disaster Med. 1995;10:24–29. doi: 10.1017/s1049023x00041625. [DOI] [PubMed] [Google Scholar]
- 10.Lerner EB, Billittier AJ, Dorn JM, et al. Is total out-of-hospital time a significant predictor of trauma patient mortality? Acad Emerg Med. 2003;10:949–954. doi: 10.1111/j.1553-2712.2003.tb00650.x. [DOI] [PubMed] [Google Scholar]
- 11.Pons PT, Markovchick VJ. Eight minutes or less: does the ambulance response time guideline impact trauma patient outcome? J Emerg Med. 2002;23:43–48. doi: 10.1016/s0736-4679(02)00460-2. [DOI] [PubMed] [Google Scholar]
- 12.Di Bartolomeo S, Valent F, Rosolen V, et al. Are pre-hospital time and emergency department disposition time useful process indicators for trauma care in Italy? Injury. 2007;38:305–311. doi: 10.1016/j.injury.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Osterwalder JJ. Can the “Golden hour of shock” safely be extended in blunt polytrauma patients? Prehosp Disast Med. 2002;17:75–80. doi: 10.1017/s1049023x00000212. [DOI] [PubMed] [Google Scholar]
- 14.Newgard CD, Schmicker R, Hedges JR, Trickett JP, Davis DP, Bulger EM, Aufderheide TP, Minei JP, Hata JS, Gubler KD, Brown TB, Yelle JD, Bardarson B, Nichol G. Emergency medical services time intervals and survival in trauma: assessment of the “Golden Hour” in a North American prospective cohort. Annals of Emergency Medicine. 2010;55(3):235–246. doi: 10.1016/j.annemergmed.2009.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ambulance crash-related injuries among Emergency Medical Services workers – Unites States, 1991-2002. MMWR Morb Mortal Wkly Rep. 2003;52:154–156. [PubMed] [Google Scholar]
- 16.Kahn CA, Pirrallo RG, Kuhn EM. Characteristics of fatal ambulance crashes in the United States: an 11-year retrospective analysis. Prehosp Emerg Care. 2001;5:261–269. doi: 10.1080/10903120190939751. [DOI] [PubMed] [Google Scholar]
- 17.Becker LR, Zaloshnja E, Levick N, et al. Relative risk of injury and death in ambulances and other emergency vehicles. Accid Anal Prev. 2003;35:941–948. doi: 10.1016/s0001-4575(02)00102-1. [DOI] [PubMed] [Google Scholar]
- 18.Bulger EM, May S, Brasel KJ, Schreiber M, Kerby JD, Tisherman SA, Newgard C, Slutsky A, Coimbra R, Emerson S, Minei JP, Bardarson B, Kudenchuk P, Baker A, Christenson J, Idris A, Davis D, Fabian TC, Aufderheide TP, Callaway C, Williams C, Banek J, Vaillancourt C, van Heest R, Sopko G, Hata JS, Hoyt DB. ROC Investigators. Out-of-hospital hypertonic resuscitation following severe traumatic brain injury: a randomized controlled trial. JAMA. 2010;304(13):1455. doi: 10.1001/jama.2010.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bulger EM, May S, Kerby JD, Emerson S, Stiell IG, Schreiber MA, Brasel KJ, Tisherman SA, Coimbra R, Rizoli S, Minei JP, Hata JS, Sopko G, Evans DC, Hoyt DB. Out-of-hospital hypertonic resuscitation after traumatic hypovolemic shock – a randomized, placebo controlled trial. Ann Surg. 2011;253:431–441. doi: 10.1097/SLA.0b013e3181fcdb22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brasel KJ, Bulger E, Cook AJ, et al. Hypertonic resuscitation: design and implementation of a prehospital intervention trial. J Am Coll Surg. Feb. 2008;206(2):220–32. doi: 10.1016/j.jamcollsurg.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 21.Lerner EB, Willenbring B, Pirrallo RG, Brasel KJ, Cady CE, Colella MR, Cooper A, Cushman JT, Gourlay DM, Jurkovich GJ, Newgard CD, Salomone JP, Sasser SM, Shah MN, Swor RA, Wang SC. A Consensus-Based Gold Standard for Trauma Center Need. J Trauma and Acute Care Surgery. doi: 10.1097/TA.0000000000000189. In Press. [DOI] [PubMed] [Google Scholar]
- 22.Rubin DB. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons, Inc.; New York: 1987. [Google Scholar]
- 23.Newgard CD. The validity of using multiple imputation for missing prehospital data in a state trauma registry. Acad Emerg Med. 2006;13:314–324. doi: 10.1197/j.aem.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 24.Newgard CD, Haukoos J. Missing data in clinical research – part 2: Multiple imputation. Acad Emerg Med. 2007;14:669–678. doi: 10.1197/j.aem.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 25.Wilde ET. Do emergency medical system response times matter for health outcomes? Health Econ. 2013;22:790–806. doi: 10.1002/hec.2851. [DOI] [PubMed] [Google Scholar]
- 26.Pracht EE, Tepas JJ, Celso BG, et al. Survival advantage associated with treatment of injury at designated trauma centers, A bivariate probit model with instrumental variables. Med Care Res Rev. 2007;64:83–97. doi: 10.1177/1077558706296241. [DOI] [PubMed] [Google Scholar]
- 27.McConnell J, Newgard CD, Mullins RJ, et al. Mortality Benefit of Transfer to Level I vs. Level II Trauma Centers for Head-Injured Patients: Analysis using Instrumental Variables. Health Serv Res. 2005;40:435–457. doi: 10.1111/j.1475-6773.2005.00366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wears RL, Cooper RJ, Magid DJ. Subgroups, reanalyses, and other dangerous things. Ann Emerg Med. 2005;46:253–255. doi: 10.1016/j.annemergmed.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 29.Phillips JA, Buchman TG. Optimizing out of hospital triage criteria for trauma team alerts. J Trauma. 1993;34:127–32. doi: 10.1097/00005373-199301000-00024. [DOI] [PubMed] [Google Scholar]
- 30.Baxt WG, Jones G, Fortlage D. The Trauma Triage Rule: a new, resource-based approach to the out-of-hospital identification of major trauma victims. Ann Emerg Med. 1990;19:1401–1406. doi: 10.1016/s0196-0644(05)82608-3. [DOI] [PubMed] [Google Scholar]
- 31.Fries GR, McCalla G, Levitt MA, et al. A prospective comparison of paramedic judgment and the trauma triage rule in the prehospital setting. Ann Emerg Med. 1994;24:885–889. doi: 10.1016/s0196-0644(94)70207-1. [DOI] [PubMed] [Google Scholar]
- 32.Zechnich AD, Hedges JR, Spackman K, et al. Applying the trauma triage rule to blunt trauma patients. Acad Emerg Med. 1995;2:1043–1052. doi: 10.1111/j.1553-2712.1995.tb03148.x. [DOI] [PubMed] [Google Scholar]
- 33.Newgard CD, Hui J, Griffin A, et al. Prospective validation of a clinical decision rule to identify severely injured children at the scene of motor vehicle crashes. Acad Emerg Med. 2005;12:679–687. doi: 10.1197/j.aem.2005.03.526. [DOI] [PubMed] [Google Scholar]
- 34.Henry MC, Hollander JE, Alicandro JM, et al. Incremental benefit of individual American College of Surgeons trauma triage criteria. Acad Emerg Med. 1996;3:992–1000. doi: 10.1111/j.1553-2712.1996.tb03340.x. [DOI] [PubMed] [Google Scholar]
- 35.Engum SA, Mitchell MK, Scherer LR, et al. Prehospital triage in the injured pediatric patient. J Pediatr Surg. 2000;35:82–87. doi: 10.1016/s0022-3468(00)80019-6. [DOI] [PubMed] [Google Scholar]
- 36.Qazi K, Kempf JA, Christopher NC, et al. Paramedic judgment of the need for trauma team activation for pediatric patients. Acad Emerg Med. 1998;5:1002–1007. doi: 10.1111/j.1553-2712.1998.tb02780.x. [DOI] [PubMed] [Google Scholar]
- 37.Newgard CD, Rudser K, Hedges JR, Kerby JD, Stiell IG, Davis DP, Morrison LJ, Bulger E, Terndrup T, Minei JP, Bardarson B, Emerson S, the ROC Investigators A critical assessment of the out-of-hospital trauma triage guidelines for physiologic abnormality. J Trauma. 2010;68(2):452–62. doi: 10.1097/TA.0b013e3181ae20c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang HE, Faibanks RJ, Shah MN, Abo BN, Yealy DM. Tort claims and adverse events in emergency medical services. Ann Emerg Med. 2008;52:256–262. doi: 10.1016/j.annemergmed.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 39.Eisenberg MS, Bergner L, Hallstrom A. Cardiac resuscitation in the community: importance of rapid provision and implications for program planning. JAMA. 1979;241:1905–1907. doi: 10.1001/jama.241.18.1905. [DOI] [PubMed] [Google Scholar]
- 40.De Maio VJ, Stiell IG, Wells GA, et al. Optimal defibrillation response intervals for maximum out-of-hospital cardiac arrest survival rates. Ann Emerg Med. 2003;42:242–250. doi: 10.1067/mem.2003.266. [DOI] [PubMed] [Google Scholar]
- 41.Terkelsen CJ, Sorenson JT, Maeng M, Jensen LO, Tilsted H, Trautner S, Vach W, Johnsen SP, Thuesen L, Lassen JF. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–771. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- 42.The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–7. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 43.Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R. Thrombolysis with Alteplase 3 to 4.5 hours after acute ischemic stroke. NEJM. 2008;359:1317–1329. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 44.Pons PT, Haukoos JS, Bludworth W, et al. Paramedic response time: does is affect patient survival? Acad Emerg Med. 2005;12:594–600. doi: 10.1197/j.aem.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 45.Blackwell TH, Kaufman JS. Response time effectiveness: comparison of response time and survival in an urban EMS system. Acad Emerg Med. 2002;9:288–295. doi: 10.1111/j.1553-2712.2002.tb01321.x. [DOI] [PubMed] [Google Scholar]
- 46.Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, Wald MM, Jurkovich GJ, Newgard CD, Lerner EB, Cooper A, Wang SC, Henry MC, Salomone JP, Galli RL. Guidelines for Field Triage of Injured Patients: Recommendations of the National Expert Panel on Field Triage, 2011. MMWR. 2012;61:1–20. [PubMed] [Google Scholar]
- 47.Hannan EL, Farrell LS, Cooper A, et al. Physiologic trauma triage criteria in adult trauma patients: are they effective in saving lives by transporting patients to trauma centers? J Am Coll Surg. 2005;200:584–592. doi: 10.1016/j.jamcollsurg.2004.12.016. [DOI] [PubMed] [Google Scholar]
- 48.Newgard CD, Meier EN, McKnight B, Drennan IR, Richardson D, Brasel K, Schreiber M, Kerby JD, Kannas D, Austin M, Bulger EM, the ROC Investigators Understanding Traumatic Shock: Out-of-Hospital Hypotension With and Without Other Physiologic Compromise. J Trauma and Acute Care Surgery. doi: 10.1097/TA.0000000000000478. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]