Abstract
AIMS
There is limited longitudinal research examining incarceration and subsequent changes in drug use among people who inject drugs (PWID) in the US. The objective of the current study was to characterize the frequency of incarceration and estimate the association between incarceration and subsequent injection drug use among current and former PWIDs in one US city.
DESIGN
ALIVE (AIDS Linked to the Intravenous Experience) is a prospective cohort study of current and former PWIDs, with semi-annual follow-up occurring since 1988.
SETTING
Baltimore, Maryland, USA
PARTICIPANTS
A total of 3,245 participants with 48,738 study visits were included. Participants enrolled from 1988 through 2012 with a median of 13 follow-up visits per participant (interquartile range: 7–25).
MEASUREMENTS
Incarcerations were defined as any self-reported jail or prison stays in the previous six months that were 7 days or longer. The primary outcome was defined as any self-reported injection drug use in the previous six months.
FINDINGS
At baseline, 29% were female, 90% African-American, and 33% HIV-positive. Fifty-seven percent of participants experienced at least one incarceration episode. After adjusting for confounders, there was a positive association between incarceration and subsequent injection drug use (AOR=1.48, 95% CI:1.37–1.59),; however stratified analysis showed that the effect was restricted to those who were not injecting at the time of incarceration (AOR=2.11, 95% CI: 1.88–2.37).
CONCLUSIONS
In the United States, incarceration of people who had previously stopped injecting drugs appears to be associated with an increased risk of subsequent injecting.
INTRODUCTION
The United Nations Office on Drugs and Crime estimated that there were 14 million (11.2 to 22.0 million) people who inject drugs (PWID) worldwide in 2013. Globally incarceration is widely employed as a strategy for addressing drug use. The United States has the highest incarceration rate in the world. Since the 1980s in the US, law enforcement approaches have been the mainstay of policies designed to control substance use. However, evidence to support incarceration as a public health policy effective at reducing drug use behaviors, drug dependence, and eventual disease transmission, is non-existent, particularly among high-risk PWID. Indeed, incarceration rates have skyrocketed in the previous three decades without clear linkage to reductions in drug use (1), resulting in a disproportionate and growing number of non-violent drug users behind bars. In 2011, nearly half of inmates in federal prisons were serving time for drug offenses (2). In Maryland over 40% of all prison admissions statewide are for drug-related offenses (3).
A number of studies have demonstrated an association between high-risk behaviors for the transmission of HIV and blood borne viral infections and a history of incarceration (4,5). However, the directionality of this association remains unclear. On the one hand, the behaviors that place individuals at highest risk for HIV also often place individuals at high risk for incarceration, meaning any observed association may reflect a convergence of risk factors. On the other hand, jails and prisons may create opportunities for high-risk social networks to interact, making the time during and following incarceration a time of increased risk (6,7). Moreover, incarceration may interrupt access to resources aimed at reducing drug use or the harms associated with drug use.
A key challenge in teasing out the directionality of these relationships is the lack of longitudinal data examining changes in drug use behaviors before and after periods of incarceration. A recent research study from Canada suggested that syringe sharing increased among PWID following incarceration, but there was no effect on other drug use behaviors (8). Other studies have shown that the immediate weeks post-release are a time of high risk for overdose among drug users (9,10). While these studies demonstrate that the post-incarceration period may be associated with increased risk, it is unclear how incarceration changes drug use behaviors over time.
The current study objectives are therefore to: 1) characterize the frequency of incarceration in a longitudinal cohort of injection drug users in Baltimore, Maryland, and 2) to determine the association of incarceration with subsequent drug use behaviors while controlling for factors known to be associated with injection drug use in this cohort.
METHODS
Study Population
The ALIVE (AIDS Linked to the IntraVenous Experience) study is a prospective cohort study of PWID in Baltimore, Maryland that has been described in detail elsewhere (11). Briefly, initial recruitment occurred during 1988–1989 using street outreach. Individuals had to be 18 years of age or older with a history of drug injection. Additional enrollment periods occurred in 1994–5, 1997–8, and most recently in 2005–8. For the purposes of this analysis, the sample was followed from study enrollment (occurring between 1988–2012) through December 2012, or censoring at death or when lost-to-follow-up. From the initial 3923 participants in the sample, we excluded 678 PWIDs who had fewer than two study visits with information regarding incarceration. The final sample included 3,245 participants with 48,738 study visits of observation, with a median of 13 study visits per participant (interquartile range (IQR): 7–25 visits), with a median of 6.75 years in follow-up. The median time between visits was 6 months (IQR: 5.9–6.6 months).
Measures
Data collected at semi-annual study visits via interviewer-administered and audio computer-assisted self-interview (ACASI) included information on demographic characteristics, drug use and sexual behaviors, medical history and utilization of health care, and information about recent incarceration episodes. For the purposes of this analysis, our main exposure of interest was incarceration, defined as any self-reported jail or prison stays in the six months prior to the study visit that were seven days or longer in length. Specifically, participants answered the following question: “Have you been incarcerated or in jail for at least a week at any time in the last 6 months? (By incarcerated, we mean where you were sentenced, not including overnight jail stays).” In the US jails are most often run by local jurisdictions and serve as a holding area for individuals awaiting trial or those serving short sentences, while prisons are state and federal institutions for individuals convicted of crimes. The primary outcome was defined as any self-reported injection drug use in the six months prior to the study visit. We also examined the impact of incarceration on behaviors related to sharing injection equipment, restricted to active injectors. Potential confounders were based on the literature and included: socio-demographic factors (i.e., age, sex, race, educational attainment, marital status, employment, income, homelessness, health insurance coverage), HIV status, recent drug treatment, use of methadone maintenance therapy, recent detoxification, alcohol and non-injection drug use (i.e., cigarette, crack, marijuana), type of drug injected (i.e., heroin, cocaine, both heroin and cocaine) and frequency (i.e., none, less than daily, daily or more frequently), and risk behaviors for HIV transmission (i.e., sharing syringes, sexual activity, sexual activity with an injector).
Statistical Analysis
Standard descriptive statistics were used to describe the sample and to characterize incarceration within the cohort. Socio-demographic and behavioral characteristics were examined at baseline. We also estimated the percentage of visits with incarceration over the course of follow-up by characteristics of interest. Logistic regression with generalized estimating equations (GEE) was used to examine the impact of incarceration on subsequent drug use accounting for repeated measures among individuals over time. Incarceration and all potential time-varying confounders were lagged one study visit to ensure temporality. The covariates for inclusion in the final model were selected with a combination of backwards and forwards stepwise regression, with inclusion based on statistical significance (p≤0.05) in the adjusted model. Basic demographic characteristics (i.e., age, sex, race, and HIV status) and year of study visit (to account for secular changes over time) were included regardless of statistical significance. In addition we excluded any covariates that were collinear with the outcome (e.g., injection drug use) or our main exposure (e.g., incarceration).
To further understand the association between incarceration and injection drug use, we examined whether the association between incarceration and injection drug use differed by the amount of time incarcerated; we compared shorter (e.g., 30 days or fewer) vs. longer (e.g., 31 days or more) amounts of time incarcerated in a subset of participants with information regarding length of time (n=34,332 observations from 2,607 participants). Next, we examined whether the association between incarceration and subsequent injection drug use differed by whether or not the participant was injecting at the time of incarceration (prior visit), with both an interaction model and stratified analysis. In particular, we were interested in whether incarceration was associated with relapse into injection among those who were not actively injecting prior to incarceration.
RESULTS
Table 1 presents the baseline socio-demographic and behavioral characteristics of the study sample. At baseline, the median age of the sample was 37 years, 29% were female, 90% African-American, 33% HIV-positive, 63% never married, and 43% had achieved at least a high school education. In the six months prior to the baseline visit, 15% were not actively injecting, while 66% reported injecting cocaine and heroin, 10% injecting heroin only, and 9% injecting cocaine only. Approximately one-third reported non-injection crack use in the prior six months, while 77% reported any use of alcohol. Over ninety-percent reported smoking cigarettes in the six months prior to the first follow-up visit, with 48% reporting 1 pack or more daily. Nearly half of the sample reported sharing needles or other injection equipment and 45% reported sex with an IDU partner in the six months prior to the first follow-up visit.
Table 1.
Socio-demographic and behavioral characteristics at baseline, by history of incarceration, and percentage of study visits where incarceration was reported by each characteristic among 3,245 current and former injectors from the ALIVE cohort study (1988–2012)
| Characteristic | N=3245 % | Never incarcerated N=1383 |
Ever incarcerated N=1862 |
% visits where incarceration was reported |
|---|---|---|---|---|
| Median age in years (IQR) | 37 (31–43) | 39 (34–46) | 35 (30 –41) | |
| Sex | ||||
| Female | 29 | 38 | 22 | 8 |
| Male | 71 | 62 | 78 | 13 |
| Race | ||||
| African-American | 90 | 88 | 91 | 11 |
| Other | 10 | 12 | 9 | 14 |
| HIV status | ||||
| HIV-positive | 33 | 36 | 31 | 13 |
| HIV-negative | 67 | 64 | 69 | 11 |
| Educational attainment | ||||
| Less than high school education | 57 | 55 | 58 | 12 |
| High school education or more | 43 | 45 | 42 | 11 |
| Marital status | ||||
| Ever married | 37 | 42 | 33 | 10 |
| Never married | 63 | 58 | 67 | 12 |
| Income | ||||
| Less than $5,000 | 55 | 54 | 55 | 13 |
| Greater than $5,000 | 45 | 46 | 45 | 6 |
| Employment | ||||
| Employed | 14 | 12 | 16 | 6 |
| Unemployed | 86 | 88 | 84 | 13 |
| Frequency of injection* | ||||
| None | 15 | 19 | 12 | 8 |
| Less than daily | 37 | 37 | 37 | 15 |
| Daily or more often | 48 | 43 | 52 | 14 |
| Type of drug injected* | ||||
| None | 15 | 20 | 12 | 8 |
| Heroin only | 10 | 13 | 7 | 12 |
| Cocaine only | 9 | 9 | 9 | 12 |
| Both heroin and cocaine | 66 | 59 | 71 | 16 |
| Used non-injection crack* | ||||
| No | 70 | 71 | 70 | 11 |
| Yes | 30 | 29 | 30 | 13 |
| Alcohol use* | ||||
| None | 23 | 27 | 21 | 10 |
| Less than daily | 59 | 58 | 59 | 13 |
| Daily or more often | 18 | 15 | 20 | 13 |
| Cigarette use* | ||||
| None | 9 | 10 | 9 | 8 |
| Less than 1 pack daily | 43 | 42 | 43 | 12 |
| 1 pack or more daily | 48 | 48 | 49 | 13 |
| Used marijuana* | ||||
| No | 56 | 60 | 54 | 11 |
| Yes | 44 | 40 | 46 | 12 |
| Homelessness*a | ||||
| No | 71 | 77 | 67 | 10 |
| Yes | 29 | 23 | 33 | 22 |
| Methadone maintenance therapy* | ||||
| No | 88 | 83 | 91 | 13 |
| Yes | 12 | 17 | 9 | 5 |
| Health insurance* | ||||
| None | 39 | 31 | 46 | 20 |
| Any | 61 | 69 | 54 | 8 |
| Any alcohol or drug treatment* | ||||
| No | 66 | 63 | 68 | 13 |
| Yes | 34 | 37 | 32 | 9 |
| Detoxification* | ||||
| No | 85 | 87 | 85 | 12 |
| Yes | 15 | 13 | 15 | 11 |
| Sexual activity* | ||||
| None | 17 | 21 | 15 | 13 |
| Sex with non-IDU partner | 38 | 37 | 38 | 10 |
| Sex with IDU partner | 45 | 42 | 47 | 13 |
| Sharing needles* | ||||
| No injection drug use | 15 | 19 | 12 | 8 |
| Injection, no sharing | 36 | 37 | 35 | 14 |
| Injection, sharing | 49 | 44 | 53 | 16 |
Numbers reflect % of sample unless otherwise noted;
Baseline percentages reflect the six months prior to the first follow-up visit with information regarding incarceration;
Homelessness is missing for 37%; percentage of homelessness reflect the proportion among those with information on homelessness.
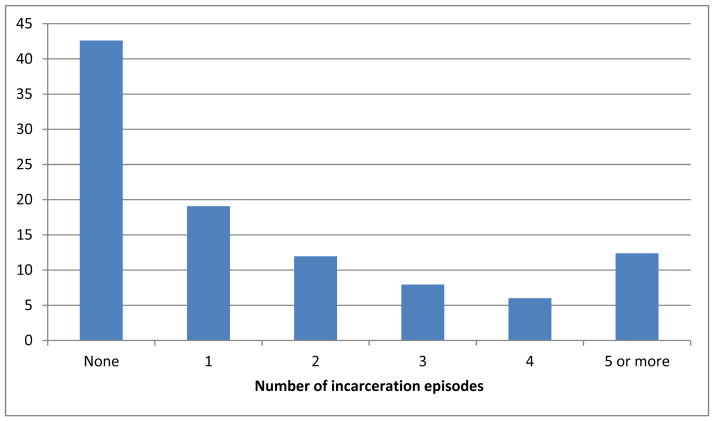
Fifty-seven percent of the sample was incarcerated at least once over the course of study follow-up. Among those who reported any incarceration, the median number of incarceration episodes was 2 (IQR: 2–4, range 1–22). Nineteen percent were incarcerated once, 26% had between 2 and 4 incarcerations, while the remaining 12% were incarcerated 5 or more times (Figure 1). Incarceration in the previous six months was reported at 11.6% of visits overall. Incarceration was more common during periods of active injection, with those not injecting reporting incarceration at 8% of visits, while those who injected less than daily and more than daily reported incarceration at 15% and 14% of visits, respectively. Also of note is that 22% of visits where homelessness was reported also had an incarceration episode reported compared to 10% of those visits where homelessness was not reported. Among visits with information regarding the amount of time incarcerated in the prior six months (n=3446), 24% reported incarcerated time of 30 days or less, while 76% reported 31 days or longer. The median amount of time incarcerated in the prior six months was 86 days (IQR: 33–152).
Figure 1.
Proportion of participants with number of incarceration episodes during study follow-up in the ALIVE study, 1988–2012.
Table 2 presents the crude and adjusted odds ratios with 95% confidence intervals examining the association of incarceration and other factors with subsequent injection drug use. In univariate analysis, being incarcerated for 7 days or longer in the prior six months was associated with a 59% increase in the odds of injection drug use at the next study visit (Odds ratio (OR) = 1.59, 95% CI: 1.51, 1.67). Current daily or less than daily injection (vs. none), injection of cocaine (vs. none), injection of cocaine (vs. none), injection of heroin and cocaine (vs. none), low income (<$5,000) (vs. ≥$5,000), non-injection crack use (vs. none), daily or less frequent alcohol use (vs. none), smoking (vs. none), marijuana use (vs. none), homelessness, detoxification, sex with an injecting or non-injecting partner (vs. none), and sharing injecting equipment (vs. not sharing) were associated with increased odds of subsequent injection drug use. Increasing age, being female (vs. male), HIV-positive (vs. HIV-negative), employment (vs. none), methadone maintenance therapy (vs. none), health insurance (vs. none), and any alcohol or drug treatment (vs. none) were associated with decreased odds of subsequent injection drug use.
Table 2.
Unadjusted (OR) and adjusted odds ratios (AOR) and 95% confidence intervals (95% CI) examining the impact of incarceration in the prior six months and socio-demographic and behavioral factors on subsequent injection drug use among 3,245 current and former injectors from the ALIVE cohort study (1988–2012).
| Characteristic | OR (95% CI) | AOR (95%CI) |
|---|---|---|
| Incarceration (vs. none) | 1.59 (1.51, 1.68) | 1.48 (1.37, 1.59) |
| Previous incarceration history (vs. none) | -- | 0.99 (0.97, 1.01) |
| Age per 5 years | 0.56 (0.55, 0.57) | 0.92 (0.89, 0.94) |
| Female (vs. male) | 0.76 (0.69, 0.84) | 0.85 (0.78, 0.94) |
| African-American (vs. other race) | 1.04 (0.88, 1.21) | 0.93 (0.80, 1.08) |
| HIV-positive (vs. HIV-negative)* | 0.55 (0.51, 0.59) | 0.83 (0.77, 0.90) |
| High school education or more (vs. less than high school) | 0.93 (0.84, 1.01) | -- |
| Never married (vs. ever married) | 1.09 (0.99, 1.20) | -- |
| Income | ||
| Greater than $5,000 | 1.00 | 1.00 |
| Less than $5,000 | 1.86 (1.77, 1.95) | 1.16 (1.08, 1.24) |
| Missing | 2.13 (1.20, 2.29) | 1.08 (0.95, 1.23) |
| Employed* (vs. unemployed) | 0.75 (0.72, 0.79) | 0.85 (0.80, 0.90) |
| Frequency of injection* | ||
| None | 1.00 | 1.00 |
| Less than daily | 7.99 (7.58, 8.42) | 5.33 (5.02, 5.66) |
| Daily or more often | 14.9 (14.1, 15.81) | 8.75 (8.19, 9.35) |
| Type of drug injected* | ||
| None | 1.00 | -- |
| Cocaine only | 2.44 (2.30, 2.59) | |
| Heroin only | 2.60 (2.45, 2.75) | |
| Heroin and cocaine | 2.80 (2.63, 2.98) | |
| Used crack* (vs. none) | 1.66 (1.58, 1.74) | -- |
| Alcohol use* | ||
| None | 1.00 | 1.00 |
| Less than daily | 2.46 (2.37, 2.57) | 1.34 (1.27, 1.42) |
| Daily or more often | 3.23 (3.03, 3.44) | 1.34 (1.22, 1.46) |
| Cigarette use* | ||
| None | 1.00 | 1.00 |
| Less than 1 pack daily | 2.14 (2.00, 2.29) | 1.34 (1.23, 1.47) |
| 1 pack or more daily | 2.97 (2.77, 3.18) | 1.30 (1.19, 1.43) |
| Used marijuana* (vs. none) | 2.00 (1.91, 2.08) | 1.10 (1.03, 1.17) |
| Homeless* (vs. not homeless) | 1.56 (1.48, 1.64) | -- |
| Methadone maintenance therapy* (vs. none) | 0.56 (0.53, 0.59) | -- |
| Health insurance* (vs. none) | 0.65 (0.62, 0.67) | 0.85 (0.81, 0.90) |
| Alcohol or drug treatment (vs. none) | 0.86 (0.83, 0.89) | 0.82 (0.81, 0.91) |
| Detoxification* (vs. none) | 1.62 (1.52, 1.72) | -- |
| Sexual activity* | ||
| None | 1.00 | 1.00 |
| Sex with non-IDU partner | 1.18 (1.13, 1.23) | 0.86 (0.81, 0.91) |
| Sex with IDU partner | 2.05 (1.95, 2.15) | 1.11 (1.03, 1.18) |
| Sharing needles* | ||
| Injection, no sharing | 1.00 | -- |
| Injection, sharing | 1.11 (1.04, 1.18) | |
Refers to prior six months; Adjusted model includes all covariates in table unless blank (--), plus year of current study visit. Type of drug injected was excluded from the final model due to collinearity with frequency of injection.
Table 2 also presents the adjusted odds ratios and 95% confidence intervals of the association between incarceration and subsequent injection drug use. The positive association between incarceration and subsequent injection drug use persisted (adjusted odds ratio (AOR) = 1.48, 95% CI: 1.37, 1.59) after adjusting for socio-demographic characteristics and recent HIV status, income, employment, frequency of injection, alcohol use, cigarette use, health insurance status, sexual activity, number of prior incarceration episodes, and year of study visit. Older age, female sex, HIV-positive status, employment, health insurance, alcohol or drug treatment, and sex with a non-IDU partner were all associated with decreased odds of injection drug use in adjusted models, while income less than $5,000, any alcohol use, any cigarette use, marijuana, injection and sex with an IDU partner at the previous visit were associated with increased likelihood of injection drug use at the current visit. Any earlier history of incarceration was not related to injection at the next study visit after accounting for incarceration in the prior six months (AOR = 0.99, 95% CI: 0.97, 1.01).
We also examined whether the association between incarceration and subsequent drug injection differed by whether the participant reported injecting at the visit where they reported incarceration (Table 3). Among persons who were not injecting at the time of incarceration, those who were incarcerated were more than two times more likely to report injection at the next study visit (OR = 2.60, 95% CI: 2.36, 2.88), an association that persisted after adjusting for confounders (AOR = 2.11, 95% CI: 1.88, 2.37). While overall, those who reported injecting at the time of incarceration were more likely to report subsequent injection, the likelihood of subsequent injection did not vary substantially by whether an individual was incarcerated. Results from the interaction model demonstrated that those who reported injecting at the time of incarceration were 6 times more likely to report injection at the next visit, regardless of whether they were incarcerated (OR = 6.27, 95% CI: 5.67, 6.93, and OR = 6.93, 95% CI: 6.06, 95% CI: 5.69, 6.45, respectively, data not shown), compared with those who were not injecting or incarcerated. In stratified analysis (Table 3), incarceration was associated with only a marginal increased likelihood of subsequent injecting among those who reported injecting at the time of incarceration (OR = 1.10, 95% CI: 1.02, 1.20). Moreover, this association was no longer statistically significant after adjusting for confounders (AOR = 1.07, 95% CI: 0.98, 1.18).
Table 3.
Unadjusted (OR) and adjusted odds ratios (AOR) of the effect of incarceration on subsequent injection drug use, stratified by injection status at the time of incarceration.
| Injecting at time of incarceration | OR (95% CI) | AOR (95% CI) |
|---|---|---|
| Yes | 1.10 (1.01, 1.20) | 1.07 (0.98, 1.18) |
| No | 2.60 (2.36, 2.88) | 2.11 (1.88, 2.37) |
Adjusted models included age, sex, African-American (vs. other), and the following characteristics in the prior six months: incarceration, previous history of incarceration, HIV status, income, employment, alcohol use, cigarette use, marijuana use, health insurance status, alcohol/drug treatment, sexual activity, and year of study visit.
When restricting to those who reported injecting at the visit following incarceration, there was no association between incarceration and sharing behaviors (AOR = 0.95, 95% CI: 0.88, 1.02) after controlling for demographic characteristics, non-injection drug use, previous history of incarceration, and all factors included in the final adjusted model (data not shown).
We further examined the impact of short (between 7 and 30 days) and long (greater than 30 days) incarceration time on injection drug use in the next study visit. While both short and long stays were associated with a nearly two-fold increase in injection drug use in unadjusted models (OR = 1.69, 95% CI: 1.50, 1.90 and OR = 1.74, 95% CI: 1.61, 1.86, respectively), these differences did not hold after controlling for demographic characteristics, non-injection drug use, previous history of incarceration and all factors included in the final adjusted model; in adjusted models, only longer incarceration episodes were statistically associated with increased injection drug use at the next study visit (AOR = 1.70, 95% CI: 1.55, 1.86).
DISCUSSION
Among current and former injectors enrolled in a community-based study in Baltimore, incarceration was commonly reported. Over half of the sample reported at least one jail or prison stay across a median of nearly 7 years of follow-up, with the majority of those who were incarcerated reporting multiple episodes over time. The frequency of incarceration observed in our sample is not necessarily surprising and is comparable to what has been observed in other samples of PWID (4).
While incarceration and injection drug use have been linked for some time (6), it is not entirely clear whether this relationship reflects that PWID are more likely to be incarcerated or whether incarceration itself has an independent negative impact on drug use. We observed both that incarceration was more common among persons who were actively injecting and that incarceration was associated with increases in injection drug use after release, specifically among those who did not report injecting prior to imprisonment. It appeared that not only did time in jail or prison not curtail injection drug use, but that longer periods of incarceration were associated with increases in injection among former injectors. These results support earlier work in this cohort and others suggesting that history of incarceration, as well as recent incarceration, are negatively associated with patterns of injection cessation and long-term injection cessation (5,12,13).
Additional research is needed to understand the mechanisms by which incarceration increases the risk of injection and relapse among drug users in the US, as well as to design and implement interventions designed to address the period of high-risk surrounding incarceration among this population. Research suggests that incarceration may impact continued injection drug use in two ways: 1) by limiting access to resources and factors helpful for promoting injection cessation during the period of incarceration, such as drug treatment and social networks of those who have stopped injecting, and 2) by increasing exposure to risk networks and behaviors during the time incarcerated.
Interestingly, despite the association between incarceration and relapse in this study, we did not observe an association between incarceration and subsequent needle sharing. These findings were encouraging given the associated risk of HIV and hepatitis C virus infection, however our findings support the idea that the period following incarceration is one of high risk for former injectors. However, research from other regions in North America has suggested that injection and high-risk sharing behaviors occur frequently during incarceration (4,14,15) and that lending and borrowing of syringes among injectors increase following incarceration episodes (8,16). Recent studies from Australia have also demonstrated that the immediate weeks post-release from prison represent a time of increased risk for overdose and mortality among those with drug-related offenses (10). Similar findings have also been observed in the US, comparing those released from prison to the general population (9). Thus despite the lack of an association between incarceration and needle sharing in our study, these data collectively suggest that the period following incarceration is one of high risk for PWID.
Interestingly in this study, African-American PWIDs were less likely to be incarcerated and there was no impact of race on subsequent injection risk. Nationwide in the US, the magnitude of incarceration is disproportionately borne by minority communities, with African-American men more likely to be arrested and prosecuted for drug use than White men, despite lower rates of use among African-Americans overall (1). While not investigated in this study, incarceration may have profound implications that extend beyond the individual drug user and his or her drug use to the wider community. For example, those who have been incarcerated may have difficulty finding employment post-release and face disruptions in their families (17).
Our study bears several limitations. First, both incarceration and drug use in the current analysis were based on self-report. While bias due to social desirability has been shown to be limited in this cohort (18), data regarding incarceration from objective sources such as administrative data would be preferable and would limit recall bias. Estimates of incarceration based on self-report may be lower than estimates based on administrative data. We have no information regarding the nature of the charges that resulted in the incarceration episode of interest. In addition we have limited information regarding the use of any drugs or access to drug treatment or methadone maintenance therapy during incarceration. The results of this study may be limited in terms of generalizability since they are based on a predominantly African-American cohort of current and former injectors in Baltimore.
From a public health perspective incarcerating non-violent drug offenders represents a missed opportunity to intervene and provide access to proven effective interventions to improve the health and well-being of PWID, such as drug treatment, methadone programs, access to health insurance, employment, and other social programs (19,20). A recent report from the Justice Policy Institute highlighted that the provision of drug treatment was more cost-effective than incarceration, reduced substance abuse, and decreased recidivism among those arrested for drug charges (21). Alternative approaches are needed to replace the role of imprisonment in handling substance use offenses.
At the very least, PWIDs should be linked to services while in jails and prisons and upon release. A recent study from Australia demonstrated decreased mortality following incarceration among those receiving opioid substitution therapy during prison and post-release (22). Unfortunately the provision of opioid substitution therapy during incarceration and referrals for treatment upon release in the US is infrequent (23,24). Releasing those with a history of injection drug use without appropriate connections to services and resources, such as drug treatment, stable housing and employment may exacerbate a time of increased risk for relapse.
In summary, a majority of PWIDs in Baltimore City reported having been incarcerated and most had been incarcerated repeatedly. After controlling extensively for socio-demographic and behavioral characteristics associated with injection drug use, incarceration increased the likelihood of subsequent active injection following release by around 50%. Additional research is needed to understand the mechanisms through which incarceration impacts injection drug use. Alternative approaches to imprisonment are urgently needed in urban centers of the United States.
Acknowledgments
This research was funded by the National Institute on Drug Abuse at the National Institutes of Health (Grant nos.: R01DA012568 and 1U01DA036297). We would like to thank the participants and staff of the ALIVE study.
Footnotes
Declarations of interest: The authors have no conflicts of interest to report.
References
- 1.Moore LD, Elkavich A. Who’s using and who’s doing time: incarceration, the war on drugs, and public health. Am J Public Health. 2008;98:782–6. doi: 10.2105/AJPH.2007.126284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carson EA, Sabol WJ. Prisoners in 2011. Washington, D.C: U.S. Department of Justice, Bureau of Justice Statistics; 2012. [Google Scholar]
- 3.Schiraldi V, Ziedenberg J. Race and Incarceration in Maryland. Washington, D.C: Justice Policy Insitute; 2003. [Google Scholar]
- 4.Milloy MJ, Wood E, Small W, Tyndall M, Lai C, Montaner J, et al. Incarceration experiences in a cohort of active injection drug users. Drug Alcohol Rev. 2008;27:693–9. doi: 10.1080/09595230801956157. [DOI] [PubMed] [Google Scholar]
- 5.Galai N, Safaeian M, Vlahov D, Bolotin A, Celentano DD. Longitudinal patterns of drug injection behavior in the ALIVE Study cohort, 1988–2000: description and determinants. Am J Epidemiol. 2003;158:695–704. doi: 10.1093/aje/kwg209. [DOI] [PubMed] [Google Scholar]
- 6.Alcabes P, Vlahov D, Anthony JC. Characteristics of intravenous drug users by history of arrest and treatment for drug use. J Nerv Ment Dis. 1992;180:48–54. doi: 10.1097/00005053-199201000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Sheu M, Hogan J, Allsworth J, Stein M, Vlahov D, Schoenbaum EE, et al. Continuity of medical care and risk of incarceration in HIV-positive and high-risk HIV-negative women. J Womens Health (Larchmt) 2002;11:743–50. doi: 10.1089/15409990260363698. [DOI] [PubMed] [Google Scholar]
- 8.Milloy MJ, Buxton J, Wood E, Li K, Montaner JS, Kerr T. Elevated HIV risk behaviour among recently incarcerated injection drug users in a Canadian setting: a longitudinal analysis. BMC Public Health. 2009;9:156. doi: 10.1186/1471-2458-9-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013;159(9):592–600. doi: 10.7326/0003-4819-159-9-201311050-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merrall EL, Kariminia A, Binswanger IA, et al. Meta-analysis of drug-related deaths soon after release from prison. Addiction. 2010;105(9):1545–1554. doi: 10.1111/j.1360-0443.2010.02990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vlahov D, Anthony JC, Munoz A, Margolick J, Nelson KE, Celentano DD, et al. The ALIVE study, a longitudinal study of HIV-1 infection in intravenous drug users: description of methods and characteristics of participants. NIDA Res Monogr. 1991;109:75–100. [PubMed] [Google Scholar]
- 12.Genberg BL, Gange SJ, Go VF, Celentano DD, Kirk GD, Latkin CA, et al. The effect of neighborhood deprivation and residential relocation on long-term injection cessation among injection drug users (IDUs) in Baltimore, Maryland. Addiction. 2011;106:1966–74. doi: 10.1111/j.1360-0443.2011.03501.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeBeck K, Kerr T, Li K, Milloy MJ, Montaner J, Wood E. Incarceration and drug use patterns among a cohort of injection drug users. Addiction. 2009;104:69–76. doi: 10.1111/j.1360-0443.2008.02387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pollini RA, Alvelais J, Gallardo M, Vera A, Lozada R, Magis-Rodriquez C, et al. The harm inside: injection during incarceration among male injection drug users in Tijuana, Mexico. Drug Alcohol Depend. 2009;103:52–8. doi: 10.1016/j.drugalcdep.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kang SY, Deren S, Andia J, Colon HM, Robles R, Oliver-Velez D. HIV transmission behaviors in jail/prison among Puerto Rican drug injectors in New York and Puerto Rico. AIDS Behav. 2005;9:377–86. doi: 10.1007/s10461-005-9011-4. [DOI] [PubMed] [Google Scholar]
- 16.Wood E, Li K, Small W, Montaner JS, Schechter MT, Kerr T. Recent incarceration independently associated with syringe sharing by injection drug users. Public Health Rep. 2005;120:150–6. doi: 10.1177/003335490512000208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Freudenberg N, Daniels J, Crum M, Perkins T, Richie BE. Coming home from jail: the social and health consequences of community reentry for women, male adolescents, and their families and communities. Am J Public Health. 2005;95:1725–36. doi: 10.2105/AJPH.2004.056325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Latkin CA, Vlahov D, Anthony JC. Socially desirable responding and self-reported HIV infection risk behaviors among intravenous drug users. Addiction. 1993;88:517–26. doi: 10.1111/j.1360-0443.1993.tb02058.x. [DOI] [PubMed] [Google Scholar]
- 19.Rich JD, McKenzie M, Shield DC, Wolf FA, Key RG, Poshkus M, et al. Linkage with methadone treatment upon release from incarceration: a promising opportunity. J Addict Dis. 2005;24:49–59. doi: 10.1300/J069v24n03_04. [DOI] [PubMed] [Google Scholar]
- 20.Rich JD, Holmes L, Salas C, Macalino G, Davis D, Ryczek J, et al. Successful linkage of medical care and community services for HIV-positive offenders being released from prison. J Urban Health. 2001;78:279–89. doi: 10.1093/jurban/78.2.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McVay D, Schiraldi V, Ziedenberg J. National and State Findings on the Efficacy and Cost Savings of Drug Treatment Versus Imprisonment. Washington, DC: Justice Policy Institute; 2004. Treatment or Incarceration? [Google Scholar]
- 22.Degenhardt L, Larney S, Kimber J, et al. The impact of opioid substitution therapy on mortality post-release from prison: retrospective data linkage study. Addiction. 2014;109:1306–1317. doi: 10.1111/add.12536. [DOI] [PubMed] [Google Scholar]
- 23.Cropsey KL, Binswanger IA, Clark CB, Taxman FS. The unmet medical needs of correctional populations in the United States. J Natl Med Assoc. 2012;104:487–492. doi: 10.1016/s0027-9684(15)30214-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nunn A, Zaller N, Dickman S, Trimbur C, Nijhawan A, Rich JD. Methadone and buprenorphine prescribing and referral practices in US prison systems: results from a nationwide survey. Drug Alcohol Depend. 2009;105:83–88. doi: 10.1016/j.drugalcdep.2009.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]