Abstract
Introduction
The study details the experiences of Medicare, Medicaid and privately insured patients with diabetes in the United States by focusing on how these distinct populations perceive their disease and manage their treatment.
Methods
A national survey was fielded among a representative sample of 2,307 US adult diagnosed diabetes patients to investigate demographic, lifestyle, treatment, access to information, and socioeconomic status. This was achieved using a combination of telephone-based interviews and internet-based questionnaires administered via KnowledgePanel®, the only large-scale online panel based on a representative random sample of the US population.
Results
Patients with Medicaid-based insurance face significant differences in diagnosis, treatment and intensity of their diabetes as compared to their Medicare and privately insured counterparts. Medicaid patients develop diabetes at an earlier age with an increased level of severity, and face significant socioeconomic concerns. Medicaid patients also have different health information seeking preferences than their counterparts, impacted by technology use patterns and education preferences. All groups report challenges in paying for their diabetes care, though cost-sharing requirements are relatively low.
Conclusions
Significant variation in experience between Medicaid, Medicare, and privately insured patients can inform disease management and patient engagement strategies. Payers, clinicians and public health agencies can leverage these findings to design initiatives more effectively and understand how intergroup variability impacts program uptake and disease outcomes.
Electronic supplementary material
The online version of this article (doi:10.1007/s13300-015-0109-z) contains supplementary material, which is available to authorized users.
Keywords: Diabetes, Health insurance, Medicaid, Medicare, Patient reported outcomes, Self-management
Introduction
Diabetes mellitus is currently the seventh leading cause of mortality in the United States, and represents a significant economic and public health burden [1]. Presently, there are 21 million Americans diagnosed with diabetes, with approximately 8.1 million still undiagnosed and over 79 million with at-risk blood glucose levels [1, 2]. Diabetes is associated with a number of severe comorbidities, including visual impairment, lower extremity conditions/amputation, neuropathy, renal disease and cardiovascular disease [2].
With this rapidly growing patient base and high rates of severe comorbidities, diabetes is a major clinical and economic concern for payers and employers. In April 2013, the American Diabetes Association (ADA) released a comprehensive examination of costs in the US directly attributable to diabetes. In this report, the estimated annual cost of diabetes in the US is $245 billion, with $176 billion in direct medical costs and $69 billion in reduced productivity [3]. When examined over a 5-year period, direct medical costs of diabetes care have increased more than 30% over the rate of inflation, a number directly attributable to increased prevalence in the U.S. [3]. Previous studies have shown that this expenditure is attributable to uncontrolled diabetes, especially within the Medicare and Medicaid populations [3–5].
The United States Centers for Disease Control and Prevention (CDC) and the ADA have outlined preventative care measures for diabetes patients, including routine blood pressure screening, glycated hemoglobin (HbA1c) testing at least two times per year, blood and urine testing for nephropathy assessment, blood lipid tests, thorough foot exams, eye examinations for retinopathy at least once a year, and smoking/tobacco cessation advice and treatment [6, 7]. The ADA also recommends regular diabetes self-management education (DSME) by accredited facilities held to strict patient curriculum standards [8]. Adherence to these guidelines, particularly those concerning HbA1c and blood lipid tests, has been previously proven to contribute directly to improved long-term clinical outcomes in people with diabetes [9].
Despite these efforts, a vast discrepancy in adherence to these standards exists across different insurance types, races/ethnicities, and socioeconomic statuses (SES), resulting in many Americans with diabetes not receiving the appropriate care or education [10, 11]. For example, there is variability in access to health care providers (HCP), DSME, prescription coverage; as well as in the levels of adherence to medication across different racial groups, with black and Hispanic patients having lowest access and levels of adherence [8, 12, 13]. The discrepancies in diabetes care provision across socio-demographic groups are exacerbated by a higher disease prevalence among black and Hispanic patients than in non-Hispanic white patients: 13.2% of non-Hispanic black patients and 11.9% of Hispanic patients have diabetes, both rates significantly higher than non-Hispanic white patients at 7.1% [2]. However, racial disparities alone do not explain differential outcomes for people with diabetes. Recent studies have found that access to insurance coverage is the most powerful determinant of proper care for people with diabetes [11, 14]. Insured patients have greater access to clinicians, treatment and education generally, but little is known about the different attitudes and behaviors of people with diabetes by payer subgroup. Specifically, do Medicaid, Medicare, and privately insured people with diabetes differ significantly in their journey, access to information, use of internet education, overall patient experience of their disease, or cost burden related to their disease? As adherence and poor outcomes remains a critical issue for people with diabetes across all payer subgroups, more needs to be understood in how these populations are both consistent and differ.
It has been previously demonstrated that 33–69% of medication-based hospitalizations for people with diabetes are related to non-adherence, resulting in an annual cost of approximately $100 billion [15] with significant burden among publically insured Medicaid and Medicare patients. In 2014, the Affordable Care Act (ACA) was implemented, extending Medicaid coverage to an estimated 13.6 million currently uninsured, non-elderly adults. While this population displays better overall health, including better self-reported health status, lower overall body mass index (BMI) and lower rates of diabetes and depression than current Medicaid recipients, they also are characterized by higher rates of smoking/tobacco use and heavy alcohol consumption [16]. Understanding how these recently insured patients act in relation to other insured people with diabetes will help inform diabetes management activities targeting Medicaid patients. Additionally, looking more closely at the privately insured people with diabetes, where outcomes and adherence levels are better as compared to Medicaid and Medicare patients provides an opportunity to bring best practices to other groups.
For example, many private insurers have introduced specific programs targeting treatment adherence and self-management for people with diabetes. Digital health management solutions, utilizing both internet-connected computer and smartphone-based platforms are also being deployed to improve patient outcomes within certain payers’ populations [17–19]. Studies have shown a direct correlation between the use of information technology systems for diabetes self-management and improved metrics of overall health [20]. However, the applications available today have only been shown effective as supplementary support to traditional DSME and do not yet provide a comprehensive set of tools for self-management [21]. Furthermore, these solutions often require access to the internet and smartphones, a premise which may work fine for most privately insured patients but because elderly patients and those with lower SES have lower utilization rates, could cause access hurdles or lead to diminished use [22].
Putting these factors together, questions remain as to how differently insured populations compare to each other in terms of disease experience and types of disease management approaches that are likely to succeed within each group. This study examines Medicaid, Medicare and Privately insured populations of diabetes patients to elucidate the key differences between them and how this information could inform future program and policy making.
Methods
Patient Selection
The sample for the telephone component was generated via random digit dialing screening of c. 51,000 US households between February and May 2013. Households were qualified via the question, “Have you or has any other member of your household been told by a doctor or health professional that you or they have diabetes?” Sample for the Internet component came from GfK’s KnowledgePanel®, the only large-scale, national probability based panel that provides the highest level of accuracy and sample representativeness available in online research for measurement of public opinion, attitudes, and behaviors. Respondents were selected via address-based sampling derived from the US Postal Service’s Delivery Sequence File. Randomly selected addresses were invited to participate based on a series of bilingual mailings (English and Spanish). Panelists were pre-identified as having been diagnosed with diabetes, which was confirmed at the time of interview. Respondents from non-internet households were provided Windows-based laptops. Internet interviews were conducted in both English and Spanish.
Data Collection and Analysis
Respondents completed a 50-min interview covering demographics, diabetes treatment, blood glucose testing, diabetes self-management behaviors and attitudes, and diabetes information sources. The questionnaire was scripted in Base Professional (SPSS Data Collection Version 6.0, IPS Armonk NY, USA). Data were collected via IBM SPSS Data Collection (Version 6.0, IPS Armonk NY, USA), an online platform. Telephone interviews were entered during survey administration by the interviewers, while internet interviews were entered by independently by respondents. Data cross tabulations were produced using Quantum (Version 5.8.1, IBM Armonk NY, USA) a computer language designed for market research data analysis. Using Quantum, data were checked, validated and tabulated. Verbatim responses were reviewed and coded using Ascribe (Version 8.4, Language Logic, Cincinnati OH, USA), a comment management platform. Coded verbatim responses were imported into Quantum and integrated into the tabulations. A Quanvert respondent level data file was exported from Quantum and imported into IBM SPSS Data Collection Survey Reporter for further subgroup analysis. Statistical significance testing between analytic groups in all cases was performed at the 90% confidence level (Quantum, Version 5.8.1, IBM Armonk NY, USA).
Study results were weight adjusted to match an estimate of the U.S. diagnosed adult diabetes patient population. Data were weighted by age, gender, race, ethnicity, region, education level, income, and home internet access. Demographic weights were derived from the 2012 National Center for Health Statistics National Health Interview Survey. Weights for income and education level were derived from 2012 Behavioral Risk Factor Surveillance System (BRFSS). The home internet access weight was derived from KnowledgePanel®. Results were projected to a U.S. population of 23,152,000 diagnosed diabetes patients. This population estimate involved extrapolation of CDC’s (BRFSS) diagnosed diabetes population estimates from 1997 to 2012.
Compliance with Ethics Guidelines
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Results
The 2013 US Roper Diabetes Patient Study was conducted June 18–August 21, 2013, among 2,307 diagnosed adult (aged 18+ years) US diabetes patients. 768 interviews were completed by telephone and 1,539 were completed via the internet. The groups evaluated in this analysis are based on the self-reported health insurance source patients typically used to cover their diabetes medications and supplies. Within this analysis, 1714 patient responders were included: 791 patients with Medicare, 135 with Medicaid, and 788 with private (employer or union based) insurance. Of these patients, 3.8% had type 1 diabetes and 96.2% had type 2 diabetes.
There is widespread demographic, employment, and educational differences in the diabetes patient populations, by payer, studied (Table 1).
Table 1.
Demographic and socioeconomic breakdown of diabetes patients in study based on insurance type
| Demographics of diabetes patients | Medicaid n = 135 | Medicare n = 791 | Private n = 788 |
|---|---|---|---|
| Gender (%) | |||
| Male | 33 | 44.3 | 55.9 |
| Female | 67 | 55.7 | 44.1 |
| Age (Mean, Years) | 52.7 | 67.4 | 54.8 |
| Age at Diagnosis (Mean, Years) | 41.6 | 54.7 | 43.8 |
| Marital Status (%) | |||
| Single/Never Married | 31.8 | 12.7 | 9.7 |
| Married | 27.9 | 42.5 | 74.2 |
| Separated | 5.3 | 2.5 | 1.3 |
| Divorced | 27.5 | 19.1 | 10.3 |
| Widowed | 7.5 | 23.1 | 4.5 |
| Income (Mean, $USD) | 17,260 | 32,342 | 64,909 |
| Education Level | |||
| Graduated High School or less | 72.5 | 56.9 | 28.6 |
| Some College or more | 27.5 | 41.6 | 71.4 |
| Graduated College | 9.2 | 21.4 | 42.7 |
$USD-United states dollar
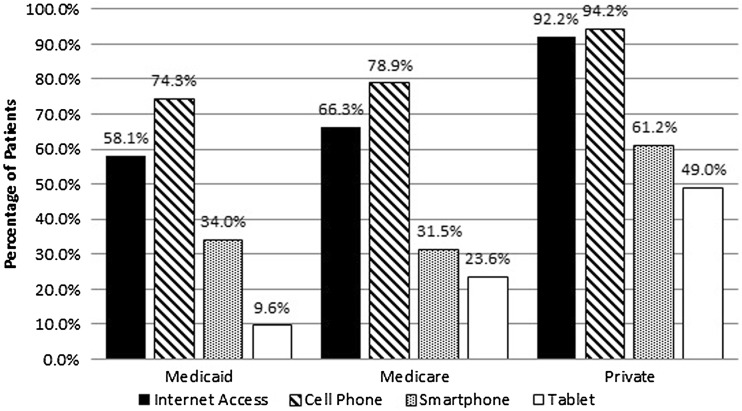
Access to Information
According to the study findings, Medicaid and Medicare patients have very different access to and use of information sources as compared to patients with private insurance. Medicaid patients have the lowest rate of internet access, either at home or at work, with 58.1% versus Medicare with 66.3% (Fig. 1). This is in contrast to privately insured patients who have near universal internet access (92.2%). As a result, the most commonly used information sources for Medicare and Medicaid patients are printed periodicals and information from friends and family, whereas privately insured patients typically get information from the internet. Medicare and Medicaid patients also had a much lower rate of cell phone ownership with 78.9% and 74.3%, respectively (private: 94.2%). Medicare and Medicaid patients also have much lower ownership of internet ready portable devices such as smartphones and tablets (Medicare: 31.5%/23.6%; Medicaid: 34.0%/9.6%; private: 61.2%/49.0%).
Fig. 1.
Reported consumer technology ownership by insurance coverage
There are also differences in whom patients go to for information related to their diabetes. Patients across all three groups exhibited equally low rates of visiting a diabetes educator in the past 12 months (Medicaid: 28.7%, Medicare: 25.4%, private: 27.3%). 21.4% of Medicaid patients strongly agree that they frequently ask their pharmacist questions pertaining to managing their diabetes at twice the rate of Medicare and privately insured patients (Medicaid: 21.4%, Medicare: 12.8%, private: 11.1%). Medicaid patients also more frequently report receiving advice about their diabetes from a social worker (11.5% versus Medicare: 4.5%, private: 1.4%). Medicaid and Medicare patients indicate that they would prefer their doctor or nurse to manage their diabetes for them more frequently than privately insured patients (Medicaid: 23.1%, Medicare: 22.3%, private: 10.9%). Privately insured patients listed the internet as their most frequent source of information related to their diabetes at twice the rate of the other two insured groups (Private: 40.8%, Medicare: 20.6%, Medicaid: 24.3%) (Supplemental Table 1).
Lifestyle and Treatment Data
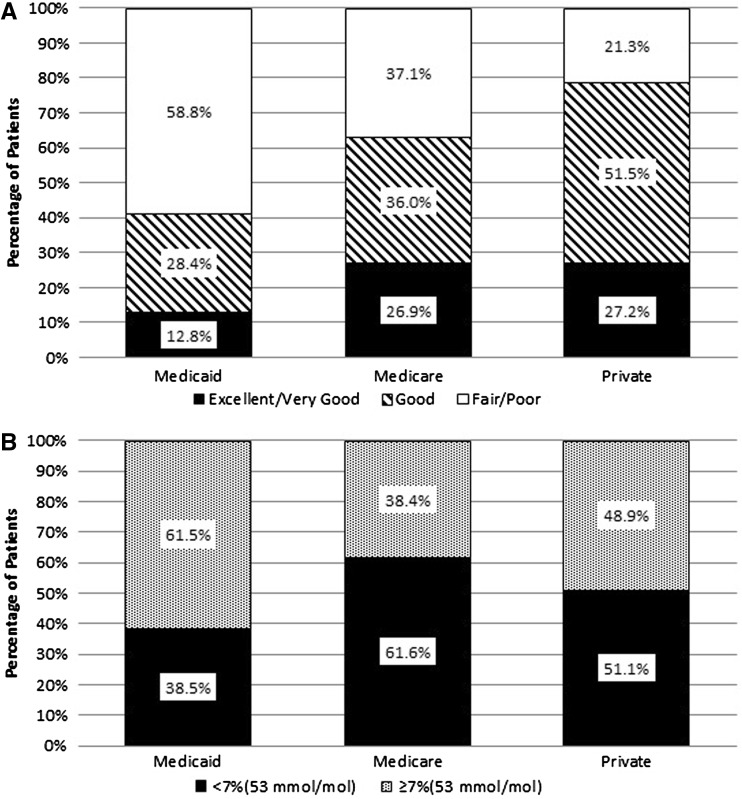
When asked to describe the status of their “Overall Health”, Medicaid patients resoundingly believed themselves to be unhealthy, with 58.8% selecting “Fair” or “Poor”, and only 12.8% selecting “Excellent” or “Very Good”. This is drastically different from Medicare and private insurance patients, who only have 37.1% and 21.3% claiming “Fair” or “Poor”, respectively, and 26.9% and 27.2% claiming “Excellent” or “Very Good”, respectively. (Figure 2a)
Fig. 2.
a Rating of overall general health by people with diabetes. b Results of most recent glycated hemoglobin test
As a result of poor general health, 48.0% of Medicaid patients claim to be out of work because of disability (Medicare: 23.4%, private: 4.7%), with 42.5% claiming to be disabled specifically because of their diabetes (Medicare: 23.7%; private: 3.5%). Similarly, 19.1% of Medicaid patients reported having “Poorly Controlled/Not at all controlled” diabetes, compared to 7.1% and 6.8% of Medicare and private insurance patients. Close to 10.0% of Medicaid patients claim to have “Severe” diabetes, twice that of Medicare and 8 times that of private insurance (Medicare: 4.0%, private: 1.1%) (Table 2). This belief is corroborated by standard HbA1c testing. When asked to report their most recent HbA1c test result, among those patients who had test results available, there is a similarly disproportionate number of Medicaid patients who have unhealthy HbA1c levels, with 61.5% reporting a score higher than or equal to 7 (Medicare: 38.4%, private: 48.9%) (Fig. 2b).
Table 2.
Patient responses to prompted opinions about the state of their diabetes
| (%) | Medicaid | Medicare | Private |
|---|---|---|---|
| (a) Out of work because of disability | 48.0 | 23.4 | 4.7 |
| (b) Disabled because of diabetes | 42.5 | 23.7 | 3.5 |
| (c) Diabetes is poorly controlled/not at all controlled | 19.1 | 7.1 | 6.8 |
| (d) Have severe diabetes | 9.3 | 4.0 | 1.1 |
| (e) I am worried about the cost of my treatment now more than ever | 44.3 | 32.0 | 36.1 |
| (f) I asked my doctor for a cheaper or generic medication | 38.8 | 36.8 | 40.2 |
| (g) I have reduced the number of visits to my HCP for economic reasons | 31.0 | 18.2 | 25.8 |
| (h) I have reduced the amount of insulin I use purely for economic reasons | 14.1 | 10.5 | 16.2 |
(a) Percentage of patients who claim to be out of work because of disability. (b) Percentage of patients who claim to be disabled because of diabetes. (c) Percentage of patients who rate their diabetes as poorly/not at all controlled. (d) Percentage of patients who rate their diabetes as severe. (e)–(h) Percentage of patients who agree with the prompted statements
HCP Health care provider
The burden of disease and associated comorbidities were significantly higher within Medicare and Medicaid than privately insured patients, reporting more than 7 other health problems in addition to diabetes on average (private: <5). Most notably, 48.3% of Medicaid patients report having depression (Medicare: 28.8%, private: 23.3%), 20.0% report a history of stroke (Medicare: 12.4%, private: 2.9%) and 55.0% report pain in hands/feet (Medicare: 39.3%, private: 27.6%). Medicare patients have the highest reported rate of congestive heart failure with 15.4% reporting a history (Medicaid: 7.4%, private: 2.5%).
Lifestyle risk factors can exacerbate diabetes and associated complications [23–25]. Medicaid patients have higher rates of lifestyle risk factors for diabetes than found in other populations. For example, the level of obesity amongst Medicaid patients is drastically higher than that of the other two groups, with an average BMI of 36.3, qualifying the average patient of this population as “morbidly obese” (Medicare: 32.3; private: 33.2). Over half (52.8%) of Medicaid patients are defined as “morbidly obese” (Medicare: 31.5%; private: 34.8%). Similarly, 13.9% of Medicaid patients have been recommended to have a surgical weight loss procedure by their HCP (Medicare: 5.6%, private: 7.7%).
Economic Data
Despite significant differences, Medicare, Medicaid and privately insured patients all share similar economic concerns when faced with treating their diabetes. When prompted with the statement, “I am worried about the cost of treating my diabetes now more than ever”, patients in all three groups had a significant number of respondents who “Agree” or “Strongly Agree” (Medicaid: 44.3%; Medicare: 32.0%; private: 36.1%). As a result, the patients were prompted with some statements to understand how they are coping with these economic issues. When prompted with the statement, “I asked my doctor for a cheaper or generic medicine”, responses were very similar across Medicare, Medicaid and private insurance patients with 36.8, 38.8 and 40.2%, respectively, responding “Agree” or “Strongly Agree” (Table 2).
Some patients showed alarming methods of saving money, with many stating that they have “reduced the number of visits to their health care provider in the past year” (Medicaid: 31.0%; Medicare: 18.2%; private: 25.8%), and some even saying that they have “reduced the amount of insulin they are taking” purely for economic reasons (Medicaid: 14.1%; Medicare: 10.5%; private: 16.2%) (Table 2).
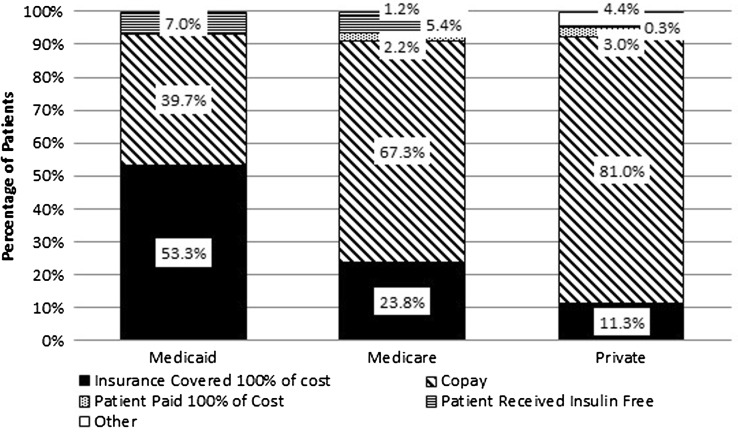
Despite all of these concerns, however, patients responded resoundingly that they were getting coverage for their diabetes medication from their insurance providers, especially in the Medicaid group. Even though 14.1% of Medicaid patients claim that they have cut back on their insulin use for financial reasons, 60.3% of Medicaid patients paid no money for their insulin (either covered completely by insurance, or received it free), with the remaining 39.7% paying only a nominal copay. This is remarkably different from the other two groups, with the majority of both Medicare and private insurance patients paying a copayment (Medicare: 67.3%, private: 81.0%) and a small population responsible for 100% of the cost of their insulin (Medicare: 2.2%; private: 3.0%) (Fig. 3). Similarly for payment of diabetes pills, more than 38.8% of Medicaid patients claim to have asked their HCP for less expensive options, however, 54.8% did not pay at all for their diabetes pills, and 39.4% had to pay only a copayment. As with insulin, the majority of Medicare and privately insured patients were required to pay a copayment for their diabetes pills (Medicare: 65.1%; private: 83.5%).
Fig. 3.
Patient responsibility for payment of Insulin based on insurance type
Discussion
Across people with diabetes studied, factors driving non-adherence were differentially represented within each insured population, with greatest burdens most frequently within the Medicaid group. Independent of insurance type, however, all patients cited economic concerns as a key driver of their adherence and treatment choices. Concerns about out-of-pocket costs associated with care were present across groups, even though most have coverage for their diabetes medicines and testing services. This is due to the fact that patients in our study were treating 2–3 comorbidities outside of their diabetes with prescription medication. Alleviating or addressing this concern, across groups, should be considered a priority as patients report the significant impact on treatment adherence and other positive health behaviors such as taking medicine or visiting their provider [9].
While people with diabetes across payer groups’ document concerns related to the cost of their disease and its management, the payers themselves are struggling to ensure their patients are better managed, adhere to treatment protocols and engage in ongoing education about their illness to support positive health behaviors. Despite providing coverage for DSME, we found that all three patient groups exhibited low utilization rates. One approach, by payers, has been to leverage digital health monitoring tools to supplement engagement and disease management of people with diabetes. These tools are becoming more available as the marketplace evolves and smartphone technologies enable wide deployment of application-based tools [17, 19, 20]. However, these and other technology based solutions may not be adopted by patients most in need; in our study those most prevalent in the Medicaid population.
Medicaid Covered Diabetes Patients
The Medicaid group report higher rates of disability, depression, and comorbidities than the other two groups. Additionally, they report having economic challenges, low use of internet-based education systems, and widespread feelings of hopelessness related to improving their disease experience. These factors drive non-adherence to treatment regimens and result in poorer outcomes. Disease management and patient engagement strategies targeting these patients, those most in need and perhaps the most complex, need to take these characteristics into account as solutions are developed. If those patients most in need have low smartphone ownership and internet use for health information, then many digital health and wellness activities targeting people with diabetes may not be reaching their target populations. Additionally, with many patients experiencing comorbidities with their diabetes, solutions will need to provide support for the whole patient experience rather than just the component associated with diabetes management.
Medicare Covered Diabetes Patients
The Medicare group is generally older, finds change more difficult, uses the internet for information sporadically, and has higher comorbidities than privately insured patients. Disease management and patient engagement strategies for this population need to leverage innovation while also communicating with patients through media they are comfortable with and most frequently utilize. Within Medicare there is likely a greater technological disparity between those baby boomers who are newer to the program, internet savvy, and are actively engaged in managing their health versus others, who may be older or less digitally connected. The latter group may require interventions that are more personal, less technology driven, and are integrated with support for other health conditions. In fact, the Medicare patients in our study that have access to internet, smartphones and tablets do not report using these tools for diabetes care and management. In this regard they are no different than the Medicaid population, and education and management programs must take this into account.
Adherence remains a major challenge among elderly people with diabetes, especially those with multiple comorbidities [9, 26]. As such, realities of Medicare patient’s lives must be better understood when designing interventions, especially those factors that drive poor adherence such as frequently changing medication regimens, forgetfulness, negative side effects, inability to access a pharmacy, economic concerns and lack of support or unstable living conditions [9].
Privately Insured Diabetes Patients
The privately insured group tends to have less severe disease, fewer comorbidities, are younger, tend to be working, and use the internet frequently to access healthcare information. As such, interventions targeting this group can leverage many technology enabled solutions, such as digital health monitors and smart phone applications. Active patient engagement models can take advantage of the perspectives documented in this study related to patients feeling more empowered to change their own disease course, generally being more hopeful and compliant. Additionally, being younger, employed, and less likely to have comorbidities allow targeted initiatives to focus on core concerns related to the disease and life experience of the patients—leveraging internet-based education models and employer support systems. While privately insured patients are likely to have more resources than their Medicaid and Medicare counterparts, they still report feelings of concern related to affording their diabetes medication and treatments.
This data should be interpreted with the following limitations in mind. This study reviews patient reported data, without examination of medical record or claims data. As a result, the accuracy of the data is limited by the patient’s memory and willingness to provide information. Additionally, this study was only performed in English and Spanish, and therefore only includes the views of patients proficient in one of those two languages.
Conclusion
While insurance status is a key determinant of diabetes outcomes, it is clear that not all insured people with diabetes are the same. The different characteristics, behaviors and beliefs demonstrated when comparing Medicaid, Medicare and privately insured patients in our study highlight the need for targeted interventions to improve diabetes care and outcomes. These differences can inform how clinicians, policy makers and the payers themselves attempt to better manage diabetes patients and provide individualized solutions that reflect patients’ experience and preferences. Additionally, as millions of otherwise uninsured or underinsured patients enter the Medicaid population as a result of the ACA, population characteristics may shift. This is also true as millions of baby boomers become Medicare beneficiaries. Understanding the impact of these shifting population dynamics within each payer population segment requires ongoing assessment of patient’s evolving perspectives, experiences and technology use. With this level of engagement, new generations of diabetes management programs are likely to be more effective.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
The authors would like to acknowledge the efforts of the GfK Roper Diabetes team for collection of data involved in this study. All aspects of this study were funded by GfK.
Conflict of interest
S. Garfield, J. Xenakis, A. Bastian and M. McBride declare that they have no competing interests.
Compliance with ethics guidelines
This article does not contain any new studies with human or animal subjects performed by any of the authors.
Author contributions
Susan Garfield conceived the overall subject matter of this study and worked on drafting the manuscript. Jason Xenakis performed analysis/interpretation of data and was responsible for drafting the manuscript. Alex Bastian performed data analysis and contributed to drafting the manuscript. Mary McBride was responsible for collection of data and contributed to drafting the manuscript.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
References
- 1.CDC National Diabetes Statistics Report (article online), 2014. Available from http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed Sep 2014.
- 2.American Diabetes Association: Statistics About Diabetes (article online), 2014. Available from http://www.diabetes.org/diabetes-basics/statistics/?loc=db-slabnav. Accessed Sep 2014.
- 3.American Diabetes Association Economic costs of diabetes in the US in 2012. Diabet Care. 2013;36:1033–1046. doi: 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim S. Burden of hospitalizations primarily due to uncontrolled diabetes. Diabet Care. 2007;30(5):1281–1282. doi: 10.2337/dc06-2070. [DOI] [PubMed] [Google Scholar]
- 5.Brown J, Pedula K, Bakst A. The progressive cost of complications in type 2 diabetes mellitus. Arch Intern Med. 1999;159(16):1873–1880. doi: 10.1001/archinte.159.16.1873. [DOI] [PubMed] [Google Scholar]
- 6.CDC Staying Healthy With Diabetes (article online), 2014. Available from http://www.cdc.gov/diabetes/living/health.html.
- 7.American Diabetes Association Standards of medical care in diabetes. Diabetes Care. 2014;37(Suppl 1):S14–S80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 8.Haas L, Maryniuk M, Beck J, Cox CE, Duker P, Edwards L, Fisher EB, Hanson L, Kent D, Kolb L, McLaughlin S, Orzeck E, Piette JD, Rhinehart AS, Rothman R, Sklaroff S, Tomky D. Youssef G; 2012 Standards Revision Task Force. National Standards for Diabetes Self-Management Education and Support. Diabetes Care. 2014;37(Suppl 1):S144–S153. doi: 10.2337/dc14-S144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Adherence to Long Term Therapies. 2003. Available from http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf?ua=1. Accessed Sep 2014.
- 10.Shaw K, Killeen M, Sullivan E, Bowman P. Disparities in diabetes self-management education for uninsured and underinsured adults. Diabet Edu. 2011;37:813. doi: 10.1177/0145721711424618. [DOI] [PubMed] [Google Scholar]
- 11.Richard P, Alexandre PK, Lara A, Akamigbo AB. Racial and ethnic disparities in the quality of diabetes care in a nationally representative sample. Prev Chronic Dis. 2011;8(6):A142. [PMC free article] [PubMed] [Google Scholar]
- 12.Agency for Healthcare Research and Quality National Healthcare Disparities Report, Chapter 10. Access to Healthcare [article online], 2013. Available from http://www.ahrq.gov/research/findings/nhqrdr/nhdr13/chap10.html. Accessed Sep 2014.
- 13.Briesacher B, Limcangco R, Gaskin D. Racial and Ethnic Disparities in prescription Coverage and Medication Use. Health Care Financ Rev Winter. 2003;25(2):63–76. [PMC free article] [PubMed] [Google Scholar]
- 14.Hu R, Shi L, Rane S, Zhu J, Chen CC. Insurance, racial/ethnic, ses-related disparities in quality of care among US adults with diabetes. J Immigrant Minor Health. 2014;16(4):565–575. doi: 10.1007/s10903-013-9966-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 16.Chang T, Davis M. Potential adult medicaid beneficiaries under the patient protection and affordable care act compared with current adult medicaid beneficiaries. Annal Family Med. 2013;11(5):406–411. doi: 10.1370/afm.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dudley B, Heiland B, Kohler-Rausch E, Kovic M. Education and technology used to improve the quality of life for people with diabetes mellitus type II. J Multidiscip Health. 2014;7:147–153. doi: 10.2147/JMDH.S52681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Reilly DJ, Bowen JM, Sebaldt RJ, et al. Evaluation of a chronic disease management system for the treatment and management of diabetes in primary health care practices in Ontario: an observational study. Ontario Health Technol Assess Ser. 2014;14(3):1–37. [PMC free article] [PubMed] [Google Scholar]
- 19.Breland J, Yeh V, Yu J. Adherence to evidence-based guidelines among diabetes self-management apps. TBM. 2013;3:227–286. doi: 10.1007/s13142-013-0205-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El-Gayar O, Timsina P, Nawar N, Eid W. A systematic review of IT for diabetes self-management: are we there yet? Int J Med Informatics. 2013;82(8):637–652. doi: 10.1016/j.ijmedinf.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 21.El-Gayar O, Timsina P, Nawar N, Eid W. Mobile applications for diabetes self-management: status and potential. J Diabet Sci Technol. 2013;7(1):247–262. doi: 10.1177/193229681300700130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pewter Internet Research Project Mobile Technology Fact Sheet (article online), 2014. Available from http://www.pewinternet.org/fact-sheets/mobile-technology-fact-sheet/. Accessed Sep 2014.
- 23.Phisitkul K, Hegazy K, Chuahirun T, Hudson C, Simoni J, Rajab H, Wesson DE. Continued smoking exacerbates but cessation ameliorates progression of early type 2 diabetic nephropathy. Am J Med Sci. 2008;335(4):284–291. doi: 10.1097/MAJ.0b013e318156b799. [DOI] [PubMed] [Google Scholar]
- 24.Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, Wedel H. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. New Eng J Med. 2004;351(26):2683–2693. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 25.Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemiö K, Tuomilehto J. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish diabetes prevention study. Lancet. 2006;368(9548):1673–1679. doi: 10.1016/S0140-6736(06)69701-8. [DOI] [PubMed] [Google Scholar]
- 26.Mulhem E, Lick D, Varughese J, Barton E, Ripley T, Haveman J. Adherence to medications after hospital discharge in the Elderly. Int J of Family Med. 2013;2013:901845. doi: 10.1155/2013/901845. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.