Abstract
Objectives
With ever increasing mandates to reduce costs and increase the quality of pain management, health care institutions are faced with the challenge of adopting innovative technologies and shifting workflows to provide value-based care. Transaction cost economic analysis can provide comparative evaluation of the consequences of these changes in the delivery of care. The aim of this study was to establish proof-of-concept using transaction cost analysis to examine chronic pain management in-clinic and through telehealth.
Methods
Participating health care providers were asked to identify and describe two comparable completed transactions for patients with chronic pain: one consultation between patient and specialist in-clinic and the other a telehealth presentation of a patient’s case by the primary care provider to a team of pain medicine specialists. Each provider completed two on-site interviews. Focus was on the time, value of time, and labor costs per transaction. Number of steps, time, and costs for providers and patients were identified.
Results
Forty-six discrete steps were taken for the in-clinic transaction, and 27 steps were taken for the telehealth transaction. Although similar in costs per patient ($332.89 in-clinic vs. $376.48 telehealth), the costs accrued over 153 business days in-clinic and 4 business days for telehealth. Time elapsed between referral and completion of initial consultation was 72 days in-clinic, 4 days for telehealth.
Conclusions
U.S. health care is moving toward the use of more technologies and practices, and the information provided by transaction cost analyses of care delivery for pain management will be important to determine actual cost savings and benefits.
Keywords: Telehealth, Chronic pain, Economics, Transaction cost, Triple aim, Cost-benefit
Introduction
Chronic pain poses unique challenges to the health care system, including ever-escalating costs, unintentional poisonings and deaths from overdoses of painkillers, and incalculable suffering for patients as well as their families. According to a recent report from the Institute of Medicine, approximately 100 million adults in the United States are affected by chronic pain, with treatment costs and losses in productivity totaling $635 billion annually [1]. Symptoms of pain are the leading reason patients visit health care providers [2]. At the level of the community-based primary care provider, especially in rural areas of the United States, there is often not enough capacity to manage complex chronic pain cases, often due to lack of access to specialty pain care [3, 4]. However, it is this rural and underserved population in particular that is the most vulnerable to the impact of chronic pain.
Compared with the population in urban areas, the rural population is associated with several factors contributing to chronic pain, such as older age, poorer overall health, more chronic illnesses and disabilities, and greater likelihood of being uninsured or underinsured and of living in poverty [5]. Even in urban areas, lack of access to care due to being uninsured or underinsured is prevalent [6]. More accessible and cost-effective methods of care delivery are warranted to more effectively manage the challenge of chronic pain.
Several initiatives have recently been introduced to ensure accessible, high-quality, and affordable health care to Americans. These include initiatives at the federal level such as the Affordable Care Act (ACA) for reforms to the health care system in general [7], as well as state-level initiatives such as Washington State’s Substitute House Bill 2876 on chronic pain management guidelines [8]. Building on this legislative framework, specific models of care emphasizing a collaborative, interdisciplinary approach to chronic pain have been proposed [1, 9].
One innovative approach to providing access to high-quality interdisciplinary pain care uses telehealth consultations. A unique approach based on provider-to-provider consultation, this model allows community-based providers to present complex chronic pain cases to an interdisciplinary panel of pain specialists (both board-certified pain medicine specialists and other specialties with expertise in pain management), through a videoconferencing infrastructure that also incorporates longitudinal outcomes tracking to monitor patient progress. Project Extension for Community Health Outcomes (ECHO) is an example of a telehealth program that provides chronic pain management education and consultation to health care providers in rural and underserved communities [10, 11]. While this innovative model of health care delivery has been rapidly expanding throughout the United States over the last several years [12–14], and has shown improvements in providers’ self-reported knowledge, skills, and practice [10], it is not known what effect this type of program has on the costs of pain care delivery. This study introduces a unique methodology to begin building a body of evidence for this telehealth model based on the economic theory and analysis of transaction costs.
The theory of transaction cost developed from the observation that our structures for governing transactions— the ways in which we organize, manage, support, and carry out exchange—have economic consequences [15–18]. Though prices matter, this theory recognizes that prices can and do deviate from the cost of production and do not include the cost of transacting [15, 19]. Setting aside neoclassical economic conceptions of price, output, demand, and supply, the transaction becomes the unit of analysis [16, 17]. In transactions, there are typically two parties engaging in the exchange of goods or services, and both exert effort to carry out the transaction, spending time, and incurring costs in the hope or with the expectation of realizing benefits. Some ways of structuring or supporting a given transaction, such as consultation or treatment for a patient from a health care provider, may be more efficient than others. Analysis examines the actual costs incurred and related consequences experienced by the parties as transactions were carried out over time, with the hypothesis that efficiency results from the discriminating alignment of transactions with alternative, more efficient structures of governance [20].
The theory of transaction cost gains predictive content by naming the key ways in which transactions differ, describing the economic properties of alternative structures of governance, and measuring the costs that parties experienced as they carried out transactions [21]. Originally applied to the “make or buy” decision in infrastructure and commodity markets [22, 23], the theory and its practical implications extend to the public sector [24, 25] and to virtually any situation in which two or more different arrangements may be used to govern the same transaction and research may be designed to determine which arrangement, ceteris paribus, is more efficient. If we realize that health care delivery comprised the complex sequences of transactions, between patients, providers, and other stakeholders, then we can see that transaction costs can exist, “at every juncture over which information flows, at every hand-off in the process of care, and in all aspects of organizing how care is arranged, by whom (and where) it is provided, and how it is reimbursed.” [26]
With ever increasing mandates to reduce the cost and increase the quality of pain management, health care institutions are faced with the challenge of demonstrating that new technologies, such as the networked systems of telehealth, provide value while maintaining or even improving the quality of care [27]. When new technologies such as telehealth are adopted, they are accompanied by changes in work flow intended to capture value and, in the process, these technologies inspire alternative ways of organizing or governing the economic activity of health care. As a theory and methodology, transaction cost economics is designed to compare evidence of the cost-effectiveness of alternative organizational arrangements [28]. This approach may be particularly useful to health care providers interested in determining the relative costs and consequences of adopting telehealth technology.
Transaction costs in the United States comprise an estimated 25% of health insurance premiums [29]. These costs are not simply a function of the contractual mechanisms managed by insurance companies, they also emerge from the choices made by providers of care; coordination, organization, and the adoption of technologies influence costs as well as patient outcomes [26, 30], and although it may be common for transaction cost methodologies to rely on qualitative descriptions of cost [31, 32], the 2009 Nobel Prize Winner for transaction cost economics, Oliver Williamson, operationalized the theory by calling for the comparative analysis of actual costs—the sum of production and transaction costs—as they accrue ex post, after contracts are signed [17]. Furthermore, Williamson provides a framework for interpreting the comparative efficiency of alternative organizational arrangements for delivering health care using micro-data from real transactions, consisting of quantitative measures of labor, capital, and technology [33]. The promise of analysis with such rich datasets potentially equips health care providers and administrators with assessments that will illuminate the actual costs attached to minute organizational changes, “with a view to understanding what kind of efficacious interventions are possible in a complex, evolving system, involving unforeseen outcomes.” [30]
Transactions in telehealth models of care can be substantially different from their in-clinic counterparts, posing methodological complications for health care economists. While clinical consultations with patients may use the services of one or two medical specialists and require the presence of the patient for an interview and physical examination, as is the practice at the University of Washington (UW) Center for Pain Relief, the UW TelePain model of care uses the patient’s primary care physician in an online presentation of the patient’s case to six medical specialists, thus providing access to specialized consultation for the patient without demanding that the patient travel to a specialty clinic. To address issues of access to care as well as the cost-effective provision of care, economic analysis would have to incorporate the comparative costs to the patient as well as providers in delivering these services. Transaction cost analysis may prove more suitable than traditional approaches because this method examines the costs experienced by both parties to the transaction—the patient and the provider—as the tasks required to execute the transaction are carried out (i.e., [34, 35]).
Health care managers using activity-based costing or time-driven activity-based costing [36, 37], will find transaction cost measures useful for empirically validating the estimates used to calculate capacity and cost-efficiency. Importantly, transaction cost analysis should be designed to follow patients (with particular conditions) and providers (with particular resources engaged in providing services to those patients), through the complete sequence and duration of the transaction. In doing so, it will provide types of information, such as the duration between tasks for the patient, desired in the broader effort to account for “the total costs of all the resources used by the patient as she or he traverses the system” [38] and couple these costs with patient outcomes [39].
To observe the suitability of a transaction cost method of analysis to the goal of achieving value for patients [40], research would begin by controlling for health outcomes and examining the time and costs experienced by patients and providers as comparable transactions take place under alternative models of service. The smallest possible sample size would be a single pair of transactions, delivered two different ways [17]. When scaling up, increases in sample size would then allow analyses to vary patient condition and outcome, and expand across multiple models for structuring the delivery of care. In doing so, analysis may also need to expand longitudinally, to “encompass all services or activities that jointly determine success in meeting a set of patient needs” [40].
The aim of this study was to conduct a proof-of-concept transaction cost analysis of telehealth-based chronic pain management, based on the UW TelePain program, compared with traditional in-clinic consultation with a pain medicine specialist, based on work flow at the UW Center for Pain Relief. To examine proof-of-concept in the application of transaction cost microanalytics, a comparative analysis was performed on key variables that included the number and duration of steps in the clinical work flow, the real labor costs to the provider, and estimated time incurred for the patient at each step of the clinical work flow for each of these two care delivery models.
Methods
Participants
This study was approved by the Institutional Review Board of the UW. Health care services participating in this study included the UW Center for Pain Relief and the UW TelePain program. The Center for Pain Relief is an outpatient multispecialty consultation and treatment clinic that uses the assembled expertise and skills of physicians and other medical team providers to assist in diagnosis and care for chronic pain, for example, for people with painful disorders that have persisted beyond expected duration for recovery from injury or surgery, or for those with medical conditions that have persistent uncontrolled pain despite appropriate treatment for the underlying disorder. The clinic also offers pain consultation and treatment for a variety of new-onset or acute problems that may benefit from selective anesthetic procedures, such as nerve blocks or spinal nerve root decompression.
The TelePain program serves primarily rural community-based providers in the Washington, Wyoming, Alaska, Montana, and Idaho region [12]. These community providers include primary care physicians, physician assistants, and nurse practitioners. The community providers have access to weekly videoconferences with both other community providers and university-based pain and symptom management experts. During videoconferences, providers manage cases, engage in evidence-based practice activities, and receive peer support. Throughout the process, community providers are responsible for direct patient care, and they act on recommendations of the interdisciplinary panel consulting through TelePain. Another unique feature of this model of care delivery is an introductory didactic session on varying chronic pain care topics, which allows participating community providers to obtain Continuing Medical Education credits and improve their knowledge in managing patients with chronic pain.
The two care delivery models discussed above provided this study with two comparative arrangements for delivering the same transaction: traditional in-clinic consultation at Center for Pain Relief; telehealth case consultation through TelePain. It should be noted that in both cases, the referral for specialty consultation was generated by the referring primary care provider. As such, the baseline steps required to generate a consult at the primary care level are assumed to be equivalent, and the transaction for each scenario (in-clinic and telehealth) begin at the point of referral requested by the primary care provider.
Clinical care teams for each service provided two onsite interviews documenting clinical work flow and processes (i.e., the steps in the transaction). For the in-clinic transaction, members of the clinical care team interviewed included a nurse care coordinator, pain medicine specialist, medical assistant, patient outcomes assessment coordinator, nurse triage manager, patient support services supervisor, and financial authorization specialist. For the TelePain transaction, team members interviewed included a nurse care coordinator, two pain medicine specialists, and an information technology specialist.
Procedures
Structured interviews and site visits with the clinical care teams were used to identify and describe two comparable completed transactions for two patients with chronic pain. Members of the clinical care teams selected one transaction from each model of service that was typical of the characteristics of patients and services provided, for which the care could be said to represent the routines and norms of their health care organization. The pair of transactions was carried out with patients of the same gender, similar age, and similar health characteristics. With team members, researchers observed a telehealth session and led a walk-through of the clinic to recall the discrete tasks involved in both transactions.
The following were the protocols of the analysis:
Individual steps, or discrete tasks, within each transaction (in-clinic versus TelePain), differentiated for purpose, cost, or disposition of the patient, provider, or medical record, were identified and itemized in detail.
Details included a description of each task, the person(s) engaged, the duration of engagement of each person in minutes, the information accrued to the patient’s medical record, the technologies used, and the locations where tasks were conducted and information was transmitted or stored.
The date and time, and therefore, duration in business days, that accumulated with each step in the transaction was tracked.
The costs of each step were identified and estimated for each transaction. Analysis focused on the primary costs in health care: the value of people’s time, limited to labor costs in-clinic and among telehealth personnel, and proxies for the value of time, with estimates of time for the patient.
Costs were estimated as a function of time spent per task and per patient and the actual wage, including benefits, of personnel engaged in the transaction.
Data Analysis
To confirm case selection, personal identifiable information was redacted from each patient’s medical record, and the records were reviewed for comparability as well as for norms and routines of care for the clinic and telehealth organizations. The characteristics of the two patients were similar. Both were first-time patients to their respective organizations, and were referred by their primary care providers for specialized care. The reasons for seeking care and report of conditions potentially related to chronic pain were similar. Both transactions resulted in a consultation recommending referral for additional specialized care or treatment. Patient conditions and care exemplified norms and routines for the organizations.
To determine the ways in which organizational arrangements and technologies differed, observations of the clinical and telehealth environments, and structured interviews of participants in the transaction were conducted. Two work flows, one in-clinic and one telehealth, were developed by documenting actual tasks undertaken during the transactions. Interview results included participants’ perceptions of the rationales (regulatory, economic, care-related, etc.) for the tasks undertaken. The interviews were intended to offer insight into the origin and evolution of the technological and organizational arrangements that governed each transaction. The location of the city or town of each patient’s residence was noted, as was the relative distance and estimated travel time between the city or town and the specialized services of the clinic or office locations of the telehealth specialists. The nature of the activities undertaken by the patient in each transaction was added to the work flows.
In follow-up interviews, the work flow was presented to participants for review and comment, which resulted in a complete itemized list of dates, personnel, and time spent per person on discrete steps or tasks. Wage rates were collected for each participant, along with estimates of time per task and a proxy of value of time was set for the patient at $30 per hour, consistent with revealed preference studies of the value of time in travel to scheduled appointments [41]. Elapsed time in calendar days and business days per task and in total per transaction were calculated, as were labor costs and proxies for patient costs per task and in total. The equation expressing the cost per transaction is as follows, where the total cost of the transaction (CT) is the sum of the costs of each discrete task (ki) in the transaction, measured per participant (x, y, z…) on the task, as the product of time (t) and wage rate (w), or in the case of the patient (x, y, z…), a proxy for the value of time (w) and estimated time (t).
The telehealth transaction included a didactic session, introductions to the numerous primary care providers participating in the session, and presentation of not only the study transaction but also two additional cases for consultation. This is consistent with the UW TelePain model of care, where three patient cases for consultation are presented per session. Therefore, an adjusted cost model for telehealth was conducted to estimate potential costs unique to the patient of interest. Tables and graphs expressing the steps, with cost accrual over time and in sum, were developed and compared for each transaction, to each other, and with respect to participants’ rationales for the tasks in each transaction. All data referring to participants in the transaction were anonymized; references to names, specific titles, exact wage amounts, and dates of record were removed.
Results
Each transaction began from the point of initial referral from a community provider and concluded with the completion of referral (i.e., the treatment plan or recommendations transmitted back from the clinic or telehealth session to the referring provider, and the scheduling of any follow-up consults, if routine or within the norms of the organization). For both types of consultation, the characteristics of the patient population from which our cases were drawn from were on average 47 years of age, more likely to be female, reporting a mean duration of pain of 8.5 years, and a majority (78%) being treated with chronic opioid therapy [42, 43].
In total, 46 discrete steps were taken for the typical in-clinic transaction at the Center for Pain Relief (one patient case, reviewed by two pain medicine specialists) versus 27 steps for the typical TelePain transaction (three patient cases, reviewed by six pain medicine specialists). Tables 1 and 2 detail each step of the transaction for the in-clinic and TelePain transactions, respectively. The greater number and types of administrative steps taken to schedule, execute, and follow-up the in-clinic consultation resulted in greater duration of time between receipt of initial referral request and completion of the initial consultation with the pain medicine specialists. A total of 153 business days (213 calendar days) elapsed between referral and the completion for the patient through the entire in-clinic transaction, versus 4 business days (4 calendar days) to conclude the TelePain transaction. Importantly, for the transaction at the Center for Pain Relief, 72 business days transpired before consultation concluded with a referral for the patient’s record (step 34); the same conclusion was reached for TelePain in 4 days (step 27).
Table 1.
Individual Steps for the In-Clinic Transaction
| Steps | Tasks | Days Elapsed |
|---|---|---|
| 1 | NCC reviews patient referral history | 1 |
| 2 | NCC checks with PCP about plan for referral | 28 |
| 3 | NCC consults PS, requests referral from PCP | 32 |
| 4 | PCP enters referral information into GDB | 32 |
| 5 | PS notes patient is referred | 32 |
| 6 | PS triages referral, checks insurance, mails letter about completing PQ before first appointment | 33 |
| 7 | PS notes referring clinic, edits referral | 33 |
| 8 | PS receives call from patient and gives PQ instructions | 35 |
| 9 | PS (in PQ database) provides user ID and password, documents in EMR | 35 |
| 10 | NCC checks referral status, waits for patient response to calls/letter | 36 |
| 11 | Patient logs in and completes PQ | 37 |
| 12 | NCC notes completed PQ, reviews referral, marks “in process,” and puts in scheduling queue | 38 |
| 13 | PS leaves voice mail with patient to call back and schedule with MDA per NCC | 38 |
| 14 | NCC reviews patient’s case notes and progress notes, enters data, starts goals | 38 |
| 15 | NCC reviews GDB, checks on appointment, calls patient for follow-up | 42 |
| 16 | PS (in call with patient) schedules patient for appointment, makes changes to GDB | 44 |
| 17 | PS assembles 6 forms for new patient packet, sends to patient | 44 |
| 18 | Patient completes forms, returns them to clinic | 44 |
| 19 | MA makes two changes to GDB for patient | 67 |
| 20 | Patient travels to clinic | 68 |
| 21 | Patient checks in at front desk with PS, provides ID, insurance, and file | 68 |
| 22 | Patient fills in another PQ in waiting area, provides medication and allergy list | 68 |
| 23 | PS prepares chart, queries multiple databases | 68 |
| 24 | MA prepares a room | 68 |
| 25 | MA directs patient from waiting area to room, takes vitals | 68 |
| 26 | MDA, MDF, and NCC see patient in room | 68 |
| 27 | MDA, MDF, and NCC exit room to consult | 68 |
| 28 | MDA, MDF, and NCC return to room with suggestion of referral | 68 |
| 29 | Paper record deposited in inbox in provider area | 68 |
| 30 | Patient returns to front desk, completes visit, makes follow-up appointment | 68 |
| 31 | Paper record from MDA taken from inbox, entered into GDB | 68 |
| 32 | NCC sends MDF’s plan to patient and PCP | 69 |
| 33 | Batch Scheduler accesses patient’s GDB note | 70 |
| 34 | PS enters two referrals into GDB, places in work queue for insurance authorization by FC | 72 |
| 35 | Two referrals, one approved and one denied by FC | 74 |
| 36 | PS leaves voice mail for patient to call back to schedule, sends letter | 74 |
| 37 | NCC discusses treatment plan with patient by phone and e-mail | 77 |
| 38 | PQ coordinator makes change in GDB for patient | 77 |
| 39 | NCC reviews GDB record, leaves voice mail with patient, sends message to PCP in GDB | 89 |
| 40 | PCP replies to NCC’s note | 90 |
| 41 | PS reschedules follow-up for patient with MDA | 96 |
| 42 | Patient cancels follow-up; PS reschedules follow-up | 97 |
| 43 | Patient cancels rescheduled follow-up | 103 |
| 44 | NCC reviews measures, calls patient for update and to schedule appointment | 138 |
| 45 | NCC calls and e-mails patient to facilitate follow-up | 140 |
| 46 | NCC e-mails patient | 153 |
Abbreviations: EMR, electronic medical record; FC, financial coordinator; GDB, global databases and Web-based EMR functionality; MA, medical assistant; MDA, attending MD (Pain Specialist); MDF, pain fellow; NCC, nurse care coordinator; PCP, primary care provider/community provider; PQ, patient questionnaire (background and history, outcomes assessment); PS, patient support services.
Table 2.
Individual Steps for the Telehealth Transaction
| Steps | Tasks | Days Elapsed |
|---|---|---|
| 1 | PCP prepares for TM participation with equipment | 1 |
| 2 | NCC and IT work with PCP to prepare for participation | 1 |
| 3 | NCC instructs PCPs to enter case to TM queue (email day 1) | 1 |
| 4 | PCP prints the PQ | 1 |
| 5 | PCP completes PQ on behalf of patient | 2 |
| 6 | PCP faxes signed and completed PQ to NCC | 2 |
| 7 | NCC moves fax to NCC inbox | 3 |
| 8 | NCC picks up faxes from inbox (day 3) | 3 |
| 9 | NCC receives fax and case, enters to TM queue | 3 |
| 10 | NCC reviews completeness of submission | 3 |
| 11 | NCC redacts patient identifying information | 3 |
| 12 | NCC selects (FIFO) cases for weekly TM event | 3 |
| 13 | NCC gives PCP’s patient an alphanumeric identifier | 3 |
| 14 | NCC emails PCP to confirm upcoming TM presentation | 3 |
| 15 | NCC confirms agenda with MD | 3 |
| 16 | NCC makes folder for case presentation to TM | 3 |
| 17 | NCC prepares 6 copies of documents from the folder | 3 |
| 18 | NCC sets out nameplates and docs for TM event | 3 |
| 19 | TM event begins with video connections (6 MDs, NCC, TM, +) | 3 |
| 20 | TM part one is introductions of people on video | 3 |
| 21 | TM part two is lecture | 3 |
| 22 | TM part four is presentation of patient’s case by PCP | 3 |
| 23 | All 6 MDs speak about the patient’s case | 3 |
| 24 | TM part five is presentation of two additional patient cases after the first patient | 3 |
| 25 | NCC emails recommendations with survey on patient to PCP | 3 |
| 26 | NCC duplicates files to second laptop | 3 |
| 27 | PCP receives recommendations and survey | 4 |
Abbreviations: EMR, electronic medical record; FIFO, First-In, First-Out process for cases; IT, information technology specialist; MD, consulting MD (pain specialists); NCC, nurse care coordinator; PCP, primary care provider/community provider; PQ, patient questionnaire (background and history, outcomes assessment); TM, telemedicine event; +, additional PCPs, observers, and listeners on the video and phone conference lines, or in the room of the TM provider
Table 3 summarizes the results of the transaction cost analysis per patient for each setting. The TelePain consultation was organized around a panel of six specialists, while the in-clinic visits involved two specialists. The overall costs, per patient, associated with preparing for and then completing each consultation were similar, at $332.89 for the in-clinic consultation versus $376.48 for the TelePain consultation. However, it should be noted that the total cost per patient for the in-clinic consultation included components of costs accrued by both the health care clinic ($225.89) and the patient (estimated at $107.00). Patients were not asked to attend the telehealth sessions. TelePain consultations, as provider-to-provider case consultations, accrue costs only to the health care providers. In total, the TelePain transaction served a total of three patients for $763.80 while the in-clinic transaction served one patient for $332.89. Figures 1 and 2 summarize the accrual of costs as the steps in the work flow were completed, per patient and transaction.
Table 3.
Summary of Results from the Transaction Cost Analysis
| Cost Component | In-Clinic Cost* | Telehealth Cost† |
|---|---|---|
| Total number of steps in work flow | 46 | 27 |
| Business days elapsed to complete patient record with consultation | 72 days | 4 days |
| Total business days elapsed | 153 days | 4 days |
| Actual labor costs accrued by health care system | $225.89 (1 pt.,2MDs) | $763.80 (3pts.,6MDs) |
| Estimated costs accrued by patient | $107.00 | $0 |
| Total cost | $332.89 | $763.80 |
| Estimated cost per patient | $332.89 (1 pt.,2MDs) | $376.48 (1 pt.,6MDs) |
In-clinic costs calculated for the University of Washington Center for Pain Relief.
Telehealth costs calculated for the University of Washington’s TelePain program.
Figure 1.

Total cost as a function of number of steps in the in-clinic transaction.
Figure 2.
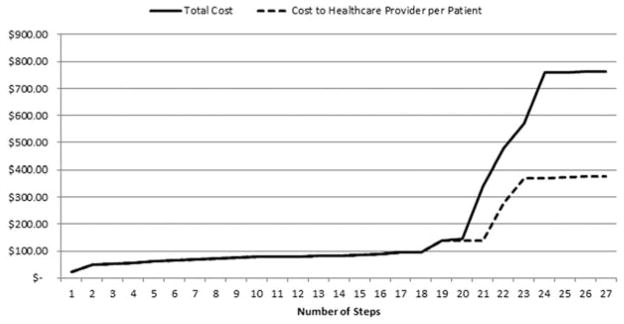
Total cost as a function of number of steps in the telehealth transaction.
Discussion
This study provides results that demonstrate the meaningful role transaction cost economic analysis can play in comparative analysis of delivery models for chronic pain management. In particular, results suggest a role for transaction cost analysis in building a body of evidence for the cost-benefit of telehealth delivery models. Despite similar costs per patient accrued over the clinical work flow in-clinic and telehealth consultations, telehealth provides rapid access to interdisciplinary and collaborative consultation, in ways that are likely to minimize the burden for patients. These results are promising for future expansion of the telehealth model for several reasons.
Rapid access to specialty consultation in as little as 4 business days stands in stark contrast to typical wait times for in-clinic chronic pain management consultations, which were reported to be between 2 and 3 months in a 1994 review [44]. In this study, the elapsed time of 68 business days before the patient was seen in-clinic and approximately 153 days before the follow-up was scheduled (thus starting a new transaction), suggests that not much has changed in the past 2 decades. However, the wait times reported in this study reflect possible capacity and workflow factors in one pain service within an academic medical center. Given the variability in capacity and resources of pain management clinics, it can be reasonably expected that this wait time may not be typical across practices in the United States. Further research using this proof of concept for transaction cost analysis may be able to yield a more accurate estimate of typical wait times for consultation. Despite this possible variability in wait times encountered by patients, it should be noted that the telehealth model also minimizes the costs accrued by the patient in terms of time spent making an appointment, traveling to the specialty clinic, and waiting for the next follow-up.
Access to a panel of interdisciplinary specialists via telehealth is also a boon. The specialists consulted on the telehealth case in this study represented pain medicine specialists as well as specialists in internal medicine, physiatry, psychiatry, addictions, and integrative medicine who have expertise in pain management. Although the total costs per patient case for in-clinic versus telehealth transactions were similar, the latter provided a greater depth of interdisciplinary specialty consultation. Similar breadth of consultation in conventional in-clinic visits would typically require multiplying the transaction three times, to visit separate providers, regardless of colocation of services, thus potentially increasing costs and wait times. Furthermore, an added benefit of this particular telehealth model is the educational component for community providers. By participating in a community of practice that provides case presentations and didactic instruction, community providers increase their skills and knowledge to manage complex chronic pain patients in the future [12, 45].
At a time when U.S. health care is moving toward the use of more innovative technologies and practices, comparative transaction cost analyses of telehealth-based pain management with other models of delivery offers important evidence toward determining the actual cost savings, benefits, and vulnerabilities of these practices. Transaction cost analyses in other sectors of critical infrastructure, such as energy [46], water [47], transportation [48, 49], and communications [34, 50], have developed richness and definitiveness for their subject matter over time, allowing theory and empirical evidence to become the basis for strategic guidance for public and private decision makers [51]. In each sector, research began with the meticulous identification of variables from small samples of cases, was coupled with analytical models emanating from the behavioral assumptions of transaction cost economic theory, and was then followed by larger representative samples with formal mathematical modeling [21]. In health care as in other sectors, transaction cost economics can show the economic consequences of the technological and organizational change experienced by producers of goods and services and their customers.
The purpose of this study was to provide proof of concept for the application of transaction cost economic analysis in accounting for the costs and timeliness of in-clinic and telehealth consultations for chronic pain management. This is an early-stage study on clinical care with a complex work flow, and several limitations are noteworthy for discussion within the context of future research.
First, the costs documented in this study focused only on the value of people’s time (labor costs, patients’ time) as encountered or estimated at each step of the transaction. Personnel time is one of the most costly factors in health care [52]. Costs for facilities and equipment per patient case would require analyses of capital outlay, operation, and maintenance, allocated across the population of patients whose care has benefited and will presumably benefit from those outlays. Future research will need to broaden the scope of transaction cost analysis by accounting for details of facility costs, as well as any relevant capital outlays for equipment and technology.
Second, this is a study of one pairwise sample, selected to examine two extremely different organizational arrangements for delivering care. One pairwise sample may suffice to demonstrate the concept of transaction cost analysis, but the possibility that these particular transactions are less than representative for patients and providers, and the need to measure and understand variation in time, cost, and duration across the patient population served by these models provides the impetus for additional research. For instance, future studies should provide adequate sample size to determine the range, mean values, and standard deviation of the times and costs accrued to a representative sample of transactions between patients and providers. Future research will also expand sample size and selection to account for activities in the full cycle of care, more variation in models of delivering care, and the technological supports they depend on. The latter is particularly noteworthy as variations in adoption of electronic health records at both primary care and specialty clinics may impact the work flow and thus influence the latency between a requested referral and completion of a consultation.
Importantly, this study does not yet take into account patient outcomes when comparing the two models of health care delivery. However, it should be noted that this study is part of a broader federally funded research program to investigate the impact of telehealth delivery on a broad set of patient outcomes, including patient-reported outcomes on health-related metrics, as well as a comprehensive account of patients’ health care utilization and associated costs. Further investigation is warranted to determine if the telehealth model, in addition to reducing costs and wait times for access to interdisciplinary specialty consultation, would also improve patient outcomes and their satisfaction with treatment as well as reduce further health care utilization. For example, other established models for reducing wait times and improving patient outcomes, such as group-based preclinic education sessions [53], would be a valuable comparative analysis against the telehealth model. Other innovative variations of the electronic consultation (e-consultation [54]) model of care delivery (of which telehealth is one type) have demonstrated preliminary evidence for improved patient satisfaction with treatment, provider satisfaction with the consult process, reduced wait times, and reduced health care utilization; however, reimbursement models for e-consultation are still lacking [55, 56]. It is hoped that a broader application of the transaction cost model to study these innovative e-consultation models, such as provider-to-provider telehealth consultation, would facilitate a paradigm shift in health care delivery.
Finally, it should be noted that this study does not intend to make the case for replacing in-clinic consultations with telehealth consultations. In-clinic visits will always be an important component of chronic pain management, especially for interventional pain procedures. However, explaining the economic cost-benefit to stakeholders in the health care system can help to expand chronic pain care. The onset of chronic pain can present a substantial barrier to patients who might otherwise prefer a visit, in person, to the clinic. Furthermore, specialty clinics are not as well distributed geographically as are primary care facilities [57], and the necessary travel and costs of in-clinic visits can impose on patients with chronic pain difficulties that, for some, may prove insurmountable. The patient in this study’s in-clinic case was estimated to spend 45 minutes in travel, from door to door. The patient in the TelePain case would have traveled more than 2 hours for the same model of care. Without the comparative patient experience, cost-benefit analyses of new models of care will miss fundamental aspects of patient-centered care. The key first step will be to convince payors of the benefits of the provider-to-provider model of consultation as described in the TelePain program. Therefore, future research should provide a comparison of transaction costs of this study’s telehealth model (provider-to-provider) to the costs of currently reimbursed provider-to-patient telemedicine consultations [58], to determine value and sustainability.
Conclusion
Telehealth models of pain management, such as practiced at UW TelePain, hold promise to improve access to specialty consultation by reducing wait times, and reducing some of the costs for access to this consultation. Ultimately, the survival of such programs will be dependent not only on demonstrating cost-effectiveness in terms of patient health outcomes, but also on demonstrating sustainability and cost-benefit to the health care system and its various stakeholders. These include community providers, pain medicine specialists, and federal, state, and private payors. This study, therefore, shows how transaction cost analysis can become an important part of a broader program to build evidence for long-term sustainability of telehealth programs for chronic pain management.
Acknowledgments
Funding sources: This work was supported by a grant from the US Department of Homeland Security, supplemental to the NSF (National Science Foundation) DUE (Division of Undergraduate Education) Federal Cyber Service: Scholarship for Service (SFS) under Grant No. 0912109 (Endicott-Popovsky—PI, Whittington—Co-PI,).
Research reported in this article was also supported by the National Institute of Nursing Research of the National Institutes of Health under award number #R01NR012450 and the National Cancer Institute of the National Institutes of Health under award number #R42 CA141875.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the US Department of Homeland Security, National Science Foundation, or National Institutes of Health. We would like to acknowledge generous assistance in data collection and project management from Mike Simon, Ginger Armbruster, and Michael Schweiger.
Footnotes
Conflict of Interest/Disclosure: None
References
- 1.Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: Institute of Medicine; 2011. [Google Scholar]
- 2.Hing E, Cherry DK, Woodwell DA. National Ambulatory Medical Care Survey: 2004 Summary. Hyattsville, MD: National Center of Health Statistics; Jun, 2006. Advance data from vital and health statistics. [PubMed] [Google Scholar]
- 3.Jukkala AM, Henly SJ, Lindeke LL. Rural perceptions of continuing professional education. J Contin Educ Nurs. 2008;39(12):555–563. doi: 10.3928/00220124-20081201-08. [DOI] [PubMed] [Google Scholar]
- 4.Baldwin LM, Patanian MM, Larson EH, et al. Modelling the mental health workforce in Washington State: Using state licensing data to examine provider supply in rural and urban areas. J Rural Health. 2006;22(1):50–58. doi: 10.1111/j.1748-0361.2006.00003.x. [DOI] [PubMed] [Google Scholar]
- 5.Rosenthal TC, Fox C. Access to health care for the rural elderly. JAMA. 2000;284(16):2034–2036. doi: 10.1001/jama.284.16.2034. [DOI] [PubMed] [Google Scholar]
- 6.Wilper AP, Woolhandler S, Lasser KE, et al. A national study of chronic disease prevalence and access to care in uninsured U.S. adults. Ann Intern Med. 2008;149(3):170–76. doi: 10.7326/0003-4819-149-3-200808050-00006. [DOI] [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Services. Report to Congress: National Strategy for Quality Improvement in Health Care. Washington, DC: U.S. Department of Health and Human Services; 2011. [Google Scholar]
- 8.Agency Medical Directors’ Group. Interagency guideline on opioid dosing for chronic non-cancer pain: An educational aid to improve care and safety with opioid therapy. Olympia, WA: Agency Medical Directors’ Group; 2010. [accessed 18 December 2014]. p. 59. [Internet] update. Available at: http://www.agencymeddirectors.wa.gov/Files/OpioidGdline.pdf. [Google Scholar]
- 9.Cahana A, Dansie EJ, Theodore BR, Wilson HD, Turk DC. Redesigning delivery of opioids to optimize pain management, improve outcomes, and contain costs. Pain Med. 2013;14(1):36–42. doi: 10.1111/pme.12013. [DOI] [PubMed] [Google Scholar]
- 10.Katzman JG, Comerci G, Boyle JF, et al. Innovative telementoring for pain management: Project ECHO pain. J Contin Educ Health. 2014;34(1):68–75. doi: 10.1002/chp.21210. [DOI] [PubMed] [Google Scholar]
- 11.Scott JD, Unruh KT, Catlin MC, et al. Project ECHO: A model for complex, chronic care in the Pacific Northwest region of the United States. J Telemed Telecare. 2012;18(8):481–484. doi: 10.1258/jtt.2012.GTH113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tauben D, Towle C, Gordon DB, Theodore BR, Doorenbos AZ. TelePain: A platform for concurrent education, clinical care, and research. Pain Med. 2013;14(4):560. [Google Scholar]
- 13.Mchaourab AS, Ober S, Gaudino CP. Innovation in specialty care delivery to rural areas. Pain Med. 2013;14(4):576. [Google Scholar]
- 14.Haozous E, Doorenbos AZ, Demiris G, et al. Role of Telehealth/videoconferencing in managing cancer pain in rural American Indian communities. Psychooncology. 2012;21:219–223. doi: 10.1002/pon.1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coase R. The nature of the firm. Economica. 1937;4(16):386–405. [Google Scholar]
- 16.Williamson OE. Markets and Hierarchies: Analysis and Antitrust Implications. New York: The Free Press; 1975. [Google Scholar]
- 17.Williamson OE. The Economic Institutions of Capitalism. New York: The Free Press; 1985. [Google Scholar]
- 18.Williamson OE. Comparative economic organization: the analysis of discrete structural alternatives. Adm Sci Q. 1991;36(2):269–296. [Google Scholar]
- 19.Coase R. The problem of social cost. J Law Econ. 1960;3:1–44. [Google Scholar]
- 20.Williamson OE. The theory of the firm as governance structure: from choice to contract. J Econ Perspect. 2002;16(3):171–195. [Google Scholar]
- 21.Tadelis S, Williamson OE. Transaction cost economics. In: Gibbons R, Roberts J, editors. Handbook of Organizational Economics. Princeton, New Jersey: Princeton University Press; 2012. pp. 159–91. [Google Scholar]
- 22.Shelanski H, Klein P. Empirical research in transaction cost economics: A review and assessment. J Law Econ Organ. 1995;11:335–61. [Google Scholar]
- 23.LaFontaine F, Slade M. Vertical integration and firm boundaries: The evidence. J Econ Lit. 2007;45(3):629–685. [Google Scholar]
- 24.Williamson OE. Public and private bureaucracies. J Law Econ Organ. 1999;15(1):306–342. [Google Scholar]
- 25.Spiller P. An Institutional Theory of Public Contracts: Regulatory Implications. Cambridge, MA: National Bureau of Economic Research; 2008. [Google Scholar]
- 26.Stiles RA, Mick SS, Wise CG. The logic of transaction cost economics in health care organization theory. Health Care Manage Rev. 2001;26(2):85–92. doi: 10.1097/00004010-200104000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Harries D, Yellowlees PM. Cyberterrorism: Is the U.S. healthcare system safe? Telemed J E Health. 2013;19(1):61–66. doi: 10.1089/tmj.2012.0022. [DOI] [PubMed] [Google Scholar]
- 28.Williamson OE. The new institutional economics: Taking stock, looking ahead. J Econ Lit. 2000;38(3):595–613. [Google Scholar]
- 29.Hsiao WC. Abnormal economics in the health sector. Health Policy. 1995;32(1–3):125–139. doi: 10.1016/0168-8510(95)00731-7. [DOI] [PubMed] [Google Scholar]
- 30.Hodgson GM. An institutional and evolutionary perspective on health economics. Cambridge J Econ. 2008;32(2):235–256. [Google Scholar]
- 31.Donato R. Extending transaction cost economics: Towards a synthesized approach for analysing contracting in health care markets with experience from the Australian private sector. Soc Sci Med. 2010;71(11):1989–1996. doi: 10.1016/j.socscimed.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 32.Ashton T. Contracting for health services in New Zealand: A transaction cost analysis. Soc Sci Med. 1998;46(3):357–367. doi: 10.1016/s0277-9536(97)00164-0. [DOI] [PubMed] [Google Scholar]
- 33.Yu K. Thesis (PhD) University of British Columbia; Saarbucken, Germany: VDM Verlag; 2010. Essays on the Theory and Practice of Index Numbers: The Making of Macroeconomics Data. 2003. [Google Scholar]
- 34.Williamson OE. Franchise bidding for natural monopolies—In general and with respect to CATV. Bell J Econ. 1976;7(1):73–104. [Google Scholar]
- 35.Klein B, Crawford RG, Alchian AA. Vertical integration, appropriable rents and the competitive contracting process. J Law Econ. 1978;21(2):297–326. [Google Scholar]
- 36.Kaplan RS, Anderson SR. Time-driven activity based costing. Harvard Bus Rev. 2004;82(11):131–138. [PubMed] [Google Scholar]
- 37.Demeere N, Stouthuysen K, Roodhooft F. Time-driven activity-based costing in an outpatient clinic environment: Development, relevance and managerial impact. Health Policy. 2009;92:296–304. doi: 10.1016/j.healthpol.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 38.Kaplan RS, Porter ME. How to solve the cost crisis in health care. Harvard Bus Rev. 2011;89(9):46–64. [PubMed] [Google Scholar]
- 39.Porter ME, Lee TH. The strategy that will fix health care. Harvard Bus Rev. 2013;91(10):50–70. [Google Scholar]
- 40.Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–2481. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 41.Brownstone D, Small KA. Valuing time and reliability: Assessing the evidence from road pricing demonstrations. Trans Res A Policy Pract. 2005;39:279– 293. [Google Scholar]
- 42.Theodore BR, Wilson HD, Cahana A, Turk DC. Patients’ perspectives on non-invasive versus invasive treatment modalities: a preliminary baseline profile report from a comprehensive pain registry. Pain Pract. 2012;12(s1):109. [Google Scholar]
- 43.Cahana A, Theodore BR, Wilson HD, et al. Characteristics of patients prescribed opioids versus non-opioid medication: Preliminary observations from a comprehensive patient registry. Proceedings of the 13th World Congress on Pain; 2010 Aug 30–Sept 2; Montreal: [accessed 31 January 2014]. [Internet] Available at: http://www.iasp-pain.org/AM/Template.cfm?Section=IASP_Press_Books2&Template=/CM/HTMLDisplay.cfm&ContentID=12983. [Google Scholar]
- 44.Davies HT, Crombie IK, Macrae WA. Waiting in pain. Delays between referral and consultation in outpatient pain clinics. Anaesthesia. 1994;49(8):661–665. doi: 10.1111/j.1365-2044.1994.tb04392.x. [DOI] [PubMed] [Google Scholar]
- 45.Doorenbos AZ, Demiris G, Towle C, et al. Developing the native people for cancer control telehealth network. Telemed J Econ Health. 2011;17:30–34. doi: 10.1089/tmj.2010.0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Joskow PL. Vertical integration and long-term contracts: the case of coal-burning electric generating plants. J Law Econ Organ. 1985;1(1):33–80. [Google Scholar]
- 47.Saussier S, Staropoli C, Yvrande-Billon A. Public-private agreements, institutions, and competition: When economic theory meets facts. Rev Ind Organ. 2009;35:1–18. [Google Scholar]
- 48.Bajari P, McMillan R, Tadelis S. Auctions versus negotiations in procurement: An empirical analysis. J Law Econ Organ. 2008;25(2):372–399. [Google Scholar]
- 49.Whittington J. When to partner for public infrastructure? J Am Plann Assoc. 2012;78(30):269– 285. [Google Scholar]
- 50.Levy B, Spiller P. The institutional foundations of regulatory commitment: A comparative analysis of telecommunications regulation. J Law Econ Organ. 1994;10:201–246. [Google Scholar]
- 51.Guasch JL. Studies in Development Series. Washington, DC: World Bank Institute; 2004. Granting and Negotiating Infrastructure Concessions. [Google Scholar]
- 52.Bove VM. Health care costs tied to many issues. Physician Exec. 1992;18(5):23–29. [PubMed] [Google Scholar]
- 53.Davies S, Quintner J, Parsons R, et al. Preclinic group education sessions reduce waiting times and costs at public pain medicine units. Pain Med. 2011;12(1):59–71. doi: 10.1111/j.1526-4637.2010.01001.x. [DOI] [PubMed] [Google Scholar]
- 54.Liddy C1, Maranger J, Afkham A, Keely E. Ten steps to establishing an e-consultation service to improve access to specialist care. Telemed J Econ Health. 2013;19(12):982–990. doi: 10.1089/tmj.2013.0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Horner K, Wagner E, Tufano J. Electronic consultations between primary and specialty care clinicians: Early insights. Issue Brief (Commonw Fund) 2011;23:1–14. [PubMed] [Google Scholar]
- 56.Liddy C, Rowan MS, Afkham A, Maranger J, Keely E. Building access to specialist care through e-consultation. Open Med. 2013;7(1):e1–e8. [PMC free article] [PubMed] [Google Scholar]
- 57.Baldwin LM, Hollow WB, Casey S, et al. Access to specialty health care for rural American Indians in two states. J Rural Health. 2008;24(3):269–278. doi: 10.1111/j.1748-0361.2008.00168.x. [DOI] [PubMed] [Google Scholar]
- 58.U.S. Department of Health and Human Services. Rural health fact sheet series. Washington, DC: U.S. Department of Health and Human Services; 2012. [accessed 18 December 2014]. Telehealth Services [Internet] Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/telehealthsrvcsfctsht.pdf. [Google Scholar]


