Abstract
Although a wealth of research has examined the effects of parental mood disorders on offspring maladjustment, studies have not identified whether elevated interparental violence (IPV) may be an exacerbating influence in this pathway. This study examined levels of physical IPV perpetration and victimization in mothers with unipolar depression or Bipolar Disorder (BD) and the processes by which maternal physical IPV moderated adolescents’ physical aggression in families with maternal mood disorders. Mothers with lifetime mood disorders were predicted to have elevated IPV compared to well mothers, and maternal IPV was expected to moderate the association between lifetime mood disorders and adolescent aggression. Participants included 61 intact families with maternal depression (n = 24), BD (n = 13), or well mothers (n = 24) and two siblings (ages 10 to 18 years). Using the Conflict Tactics Scale, mothers reported on IPV perpetration and victimization, and adolescents reported on physical aggression. Mothers with BD reported significantly higher IPV perpetration, but not victimization, than depressed or well mothers. An interaction between maternal BD and IPV perpetration was a significant predictor of adolescent aggression. Main effects of maternal IPV victimization and interaction effects of maternal depression and either type of IPV on adolescent aggression were not significant. Adolescents of mothers who have BD and perpetrate IPV may be particularly vulnerable to being aggressive. Prevention and policy efforts to deter transmission of aggression in high-risk families should target families with maternal BD and intervene at the level of conflict resolution within the family.
Keywords: interparental violence, Bipolar Disorder, depression, adolescence, aggression
Adolescence provides a critical opportunity to understand how conflict management skills, an age-salient task of this period, develop in the context of the family (Hall, 1904; Laursen & Collins, 1994; Narayan, Englund, Carlson, & Egeland, 2014; Reis, Collins, & Berscheid, 2000; Selman, 1980). During adolescence, when deeper interpersonal bonds are being established and enhanced individuation is emerging, heightened interpersonal conflicts with family members may result (Erikson, 1963; Laursen, Coy, & Collins, 1998). Parents are often required to rally their available emotion regulation resources to scaffold adolescents’ burgeoning conflict resolution skills, monitor deviant conflict tactics, and mediate conflicts within the family (Dishion & Patterson, 2006; Laursen et al., 1998; Steinberg, Mounts, Lamborn, & Dornbush, 1991). However, these normative developmental changes of adolescence may be particularly challenging for parents who struggle with mood disorders and, in turn, experience higher levels of interpersonal conflict with partners and offspring (Beardslee, Versage, & Gladstone, 1998; Chang, Blasey, Steiner, & Ketter, 2001; Marmorstein & Iacono, 2004).
Interpersonal conflict is a core feature of adult mood disorders, and specifically, depression and BD, and may serve as a precipitating factor, a byproduct, or an exacerbating influence (Feldman, 2001; Garber, 2007; Golding, 1999, Miklowitz & Johnson, 2009; Prince & Jacobson, 1995). Here, the focus is on physical interpersonal conflict, and particularly, violence and aggression, as it co-occurs with mood disorders. Despite the vast literature on the deleterious effects of aggression and interparental violence (IPV) on children in families without parental psychopathology (Cappell & Heiner, 1990; Moffitt & Caspi, 1999; Narayan, Englund, & Egeland, 2013), very little research has examined how children may be at even greater risk for maladjustment when parents have mood disorders and also use IPV.
Parents who engage in physical IPV (defined here as behavior such as hitting, shoving, slapping, kicking, throwing or smashing things, threatening physical harm, or using weapons; Straus, 1979) likely serve as poor models for conflict resolution (Bandura, 1973; Kitzmann, Gaylord, Holt, & Kenny, 2003; Narayan et al., 2014). In turn, children exposed to IPV are more likely to use aggression and violence in their own relationships (Davies & Cummings, 1994; Narayan et al., 2013, 2014). Parental modeling of IPV may be particularly salient for adolescent maladjustment if it co-occurs with mood and behavioral dysregulation from parental mood disorders (Beardslee et al., 1998; Goodwin & Jamison, 1990; Muralidharan, Yoo, Ritschel, Simeonova, & Craighead, 2010). Presumably, IPV within the context of ongoing parental mood disorders may amplify conflict in the family environment and exacerbate adolescents’ interpersonal competence and well-being. To date, there is a paucity of general research on co-occurring parental mood disorders and IPV within the family context, let alone studies on whether IPV exacerbates the relations between parental mood disorders and offspring maladjustment. Thus, the following overview focuses more broadly on mood disorders and co-occurring interpersonal conflict, rather than on IPV specifically.
Co-occurrence of Mood Disorders and Interpersonal Conflict in Families
As the two major classes of mood disorders and the focus of the current study, unipolar depression and BD have estimated lifetime prevalence rates of approximately 16% and 1%, respectively (Kessler et al., 2003; Merikangas et al., 2007). Unipolar depression is characterized by two-week long depressive episodes of persistent sadness or irritability that must together be comprised of at least five symptoms, such as disruptions in appetite or sleep patterns, fatigue or loss of energy, psychomotor agitation or retardation, self-blame or hopelessness, impaired cognition, or suicidality. In addition to depressive episodes, BD includes persistent periods of elated/expansive or irritable moods accompanied by grandiosity or inflated self-esteem, reduced need for sleep, pressured speech, racing thoughts or flight of ideas, distractibility, elevated goal-directed activity or psychomotor agitation, and high-risk behavior (American Psychiatric Association, 1994). Both depression and BD contribute to interpersonal, marital, and parental impairment (Goodwin & Jamison, 1990; Prince & Jacobson, 1995; Radke-Yarrow, Martinez, Mayfield, & Ronsaville, 1998), as their associated symptoms of affective and behavioral dysregulation often take a toll on individual and interpersonal functioning (Chang et al., 2001; Goodwin & Jamison, 1990; Mathews & Reus, 2001; Miklowitz & Johnson, 2009).
Indeed, many individuals report that having depression compromises their interpersonal functioning (Ballester et al., 2012; Pollack, 1993). Couples with a depressed partner have been found to display more observed sadness, anger, and destructive behavior and report more negative interactions than couples with non-depressed partners (Kahn, Coyne, & Margolin, 1985; Prince & Jacobsen, 1995; Zlotnick, Kohn, Keitner, & Della Grotta, 2000). Depressed women also may have less stable marriages and more marital conflict than well couples (Hammen & Brennan, 2002; Heene, Buysse, & Van Oost, 2007). When a parent suffers from depression there is a heighten possibility that marital conflict will pervade the family environment and result in divorce (Beardslee et al., 1998; Radke-Yarrow et al., 1998).
Evidence also suggests that marital conflict is elevated when one or both partner(s) is diagnosed with BD. Women with BD may tend to have less stable marriages than well women (Moreno et al., 2012), and couples with a BD partner often report more marital conflict than well couples (Hoover & Fitzgerald, 1981). Additionally, in one study, up to half of the caregivers (partners or parents) of adults with BD indicated that interpersonal violence or aggression had occurred (Dore & Romans, 2001).
There are gaps, however, in the existing literature on parental IPV and mood disorders. Despite the evidence that both adult mood disorders and IPV are fairly widespread across low-income to affluent sociodemographic contexts, studies have not examined the extent to which they co-occur in marriages and families from community samples. Rates of IPV in community samples tend to range from approximately 17% to 39% (Capaldi, Knoble, Shortt, & Kim, 2012; Straus, Gelles, & Smith, 1990). Of note, contemporary research has begun to dispel historical notions on gender stereotypes of aggression (man as perpetrator, woman as victim). Recent studies have documented that in many samples, men and women are comparably likely to be both perpetrators and victims of IPV and to disclose experiencing both the perpetrator and victim roles (Ehrensaft, Moffitt, & Caspi, 2004; Moffitt et al., 1997; Narayan et al., 2013). In relationships in which IPV is present, both partners typically have taken part in perpetration (Langer, Lawrence, & Barry, 2008; Moffitt & Caspi, 1999),
Very little is known, however, about how having a mood disorder, such as depression or BD, affects the tendencies to perpetrate or be victimized by IPV within marital relationships and families with children. Although studies have found that mood disorders and IPV co-occur in community samples (Kessler, Molnar, Feurer, & Applebaum, 2001) and that female IPV perpetrators may have higher rates of mood disorders, including depression and BD, than male perpetrators (Henning, Jones, & Holdford, 2003), these findings did not pertain specifically to IPV within families. Although some studies have examined marital conflict in families with parental mood disorders (Du Rocher Schudlich, Youngstrom, Calabrese, & Findling, 2008; Emery, Weintraub, & Neale, 1982), research has not clearly identified whether parents with BD or unipolar depression are more likely to display IPV than well parents (Rowe & Morris, 2012).
Additionally, research that considers the marital relationships of individuals with mood disorders rarely restricts the samples of interest to parents or to a particular stage of parenting, such as parenting the adolescent. However, Marital strain may vary across the parenting demands of rearing infants, young children or adolescents (Weisman, Paykel, & Klerman, 1973). It may be especially high during developmental periods of high conflict, such as adolescence (Hall, 1904; Laursen & Collins, 1994).
Adolescent Maladjustment in Families with Parental Mood Disorders and IPV
Typically, parents are effective at scaffolding adolescents’ conflict management skills (Sroufe, Egeland, Carlson, & Collins, 2005; Steinberg et al., 1991); however, parental mood disorders may interfere with this process, especially in the context of IPV (Davies & Cummings, 1994; Kitzmann et al., 2003; Narayan et al., 2014). Adolescents of parents with mood disorders are already at heightened risk for elevations in behavioral problems such as physical aggression, poor conflict management, and general externalizing behavior, due to genetic and environmental factors (Beardslee et al., 1998; Birmaher et al., 2009; Chang et al., 2001; Diler et al., 2011; Downey & Coyne, 1990; Klimes-Dougan et al., 2010; Muralidharan et al., 2010; Narayan, Allen, Cullen, & Klimes-Dougan, 2013). Adolescents may be particularly vulnerable to interpersonal physical aggression if they are genetically predisposed to mood disorders and their parents also use IPV. Although a vast number of factors, including biological precursors and environmental influences may affect the risk for maladjustment in offspring of parents with mood disorders, the current study focused on a specific environmental process accounting for these risks. A central goal was to examine whether parents’ use of IPV may be an exacerbating process by which parental mood disorders predicts adolescents' elevated risk for interpersonal aggression.
It also is unknown whether the type of parental mood disorder (e.g., depression versus BD), in combination with IPV may uniquely affect adolescent interpersonal aggression. Many studies have found that marital discord in the context of parental depressive symptoms contributes to child adjustment problems (e.g., internalizing and externalizing problems, depressive symptoms, and academic difficulties) from preschool to adolescence (Davies, Dumenci, & Windle, 1999; Davies & Windle, 1997; Essex, Klein, Cho, & Kraemer, 2003; Fear et al., 2009). Family conflict and poorer communication are also evident when parents have BD versus no diagnoses (Romero, DeBello, Soutullo, Stanford, & Strakowski, 2005; Vance, Jones, Espie, Bentall, & Tai, 2008). Studies that have examined child outcomes in families with either depression or BD have found evidence that both types of mood disorders predict interparental conflict, and child behavior problems and psychopathology more strongly than other types of disorders (e.g., Schizophrenia) or well status (Emery et al., 1982; Du Rocher Schudlich et al., 2008). However, to date no studies have differentiated whether the type of mood disorder, coupled with IPV, uniquely contributes to adolescents’ physical aggression.
Finally, it also is unclear whether the risk for adolescent aggression in families with parental mood disorders and IPV changes if one or both parents has a psychological disorder and perpetrates IPV. Currently, there are mixed findings about whether heightened child risks result from psychopathology in one versus both parents (Chang et al., 2001; Du Rocher Schudlich et al., 2008). Some studies suggest that the advantages of being raised in a two-parent family may be less apparent when significant strains exist within the parental relationship (Amato, 1993; Hetherington & Clingempeel, 1992; McLanahan & Sandefur, 1994). For example, one study found that offspring were more likely to be depressed if their mother was depressed and married, rather than depressed and single, perhaps due to the combination of a mood disorder and ongoing spousal conflict (Hammen, Brennan, & Shih, 2004). An understanding of the processes by which cumulative family risks of parental psychopathology and IPV contribute to adolescents’ interpersonal aggression would inform basic and preventative research on intergenerational continuity of violence (Bella et al., 2011; Margolin, 2005; Narayan, Englund et al., 2013).
The Current Study
The current study considered whether IPV within the context of lifetime parental mood disorders (unipolar depression versus BD) contributed to adolescents’ elevated physical aggression within the family context. Mothers were the primary parents examined due to a focus on maternal mood disorders in the larger study from which the current sample was drawn. The first study aim was to extend current understanding of IPV (perpetration and victimization) within the context of parental mood disorders. It was hypothesized that the general co-occurrence of mood disorders and interpersonal conflict would extend to IPV, such that mothers with mood disorders would engage in elevated levels of IPV, compared to well mothers. There were no specific hypotheses about whether mothers with BD or depression would display higher levels of IPV, or whether heightened involvement in IPV would pertain to perpetration or victimization. The second aim was to enhance knowledge of the explanatory processes by which maternal mood disorders are associated with adolescent aggression via elevated maternal IPV. It was predicted that maternal IPV perpetration and victimization would exacerbate, or moderate, the association between maternal mood disorders and adolescents’ elevated physical aggression within the family context. A specific mood disorder was not specified for this hypothesis, and both maternal BD and depression were tested. Finally, a third exploratory aim considered if adolescent aggression was more pronounced when one or both parents had a history of psychopathology and perpetrated IPV.
Method
Participants
Participants in the current study were 61 married families with 120 adolescents (two from each family, with the exception of two families with one child). They were drawn from a larger prospective longitudinal study of 98 families with maternal mood disorders that included mothers who had experienced at least one depressive episode during their adolescents’ lifetimes, and well parents (Radke-Yarrow et al., 1998). Maternal diagnoses in the current subsample included 48 offspring of 24 mothers with depression, 24 offspring of 13 mothers with BD (two offspring did not have siblings) and 48 offspring of 24 well mothers. In the initial sample at Time 1 (T1; 1979–1981), a younger cohort (M = 2.63, years SD = .62) and an older cohort of children (M = 6.36, SD = 1.06) were identified as study participants and were assessed through early adulthood, resulting in five assessments that were spaced approximately three to four years apart. In the present study, the focus was on the T4 assessment, which took place in 1993 when the offspring were adolescents (younger cohort: M = 13.87, SD =1.71; older cohort: M = 17.68, SD =1.95). The institutional review board at the National Institute of Mental Health approved all study procedures, and parents and adolescents provided informed consent and assent for participation.
In terms of demographic characteristics and attrition rates of the larger sample, at T1 the majority of families were middle- to upper-middle class [M = 51.00, SD = 14.84 on the Hollingshead (1975) scale] and intact at T1 (94%) and T3 (76%). Most mothers from the larger sample were Caucasian (86% Caucasian, 11% African-American, 2% Asian-American, and 1% Latin-American) and had at least some college-level education (79%) at T1. Attrition rates were 9%, 12%, and 17% for mothers with depression, BD, and well mothers, respectively through T4.
At T1, the majority of families in the larger longitudinal study were composed of both biological parents and two children (95%); the remaining mothers were single (5%). However, by T4, 13% of the families with well parents, 26% of the families with depressed mothers, and 35% of the families with mothers with BD became divorced (Radke-Yarrow et al., 1998). Families were included in the current study if parents were reportedly in a marital relationship at T4, which resulted in 61 of 98 families being included, and 37 families being excluded. Compared to excluded families, included families had significantly higher SES at T1, t(1,96) = 3.27, p < . 01, significantly lower marital stress across T1 to T3, t(1,92) = 3.34, p < . 01, and mothers with significantly higher GAF scores, t(1,89) = 3.34, p < . 01, but they did not significantly differ on maternal or paternal age at T1, or on family stress across T1 to T3.
Measures
Independent and Dependent Variables
Maternal and paternal psychopathology
Maternal diagnoses were derived from the Schedule for Affective Disorders and Schizophrenia, Lifetime Version (SADS-L; Spitzer and Endicott, 1977), which was administered to mothers at T1. Diagnostic criteria at T1 enrollment adhered to the Research Diagnostic Criteria (RDC; Spitzer, Endicott, & Robins, 1978) for Bipolar Disorder (BD I or BD II), Major Depressive Disorder (MDD), or absence of any current or past psychiatric disorder. Maternal diagnoses were updated or adjusted at T3 in 1989 based on assessments from the Structured Clinical Interview, which relied on diagnostic criteria defined by the Diagnostic and Statistical Manual, Third Edition, Revised (DSM-III-R SCID; APA, 1987) and the SADS-L. The current study utilized lifetime maternal diagnoses for MDD or BD. Thus, mothers meeting criteria for either disorder at T1 could not become part of the healthy control group at T3, although healthy mothers could become diagnosed with MDD or BD at T3. All interviews were administered by clinical psychologists or psychiatric nurses who had been trained at the New York Psychiatric Institute. An independent clinician rated 10 interviews for interrater reliability, and agreement on presence and type of mood disorder was excellent (ĸ = 1.0).
Spouses of mothers were eligible to enroll as part of well families if they had no past or current psychiatric diagnoses, or as part of families with maternal mood disorders if they had a mood, anxiety, or substance use disorder. Similar to mothers, spouses were administered SADS-L and SCID interviews at T1 and T3. The primary diagnosis for the fathers in the current study was MDD (n = 21), although two fathers had an anxiety disorder (n = 2). The remaining fathers had no diagnosis (n = 38).
Interparental violence and adolescent aggression
The Conflict Tactics Scale, Form N (CTS; Straus, 1979) was administered to parents and adolescents to assess IPV and adolescent physical aggression. For the current study, only items of physically aggressive behavior from the CTS were used. This included nine items involving direct physical aggression, physical destruction of property, or threats to another person’s physical integrity (i.e., threw, smashed, hit or kicked something; threw something at someone; pushed, grabbed or shoved someone; slapped or spanked someone; kicked, bit, or hit with a fist; hit or tried to hit with something; beat up someone; threatened with a gun or knife; and used a gun or knife). According to standard procedures, respondents are asked how often they engaged in the behavior on a 0–6-point scale from Never to More than 20 times. The total physical aggression score was calculated by summing values of 0–6 across all nine items, resulting in a possible total score of 54. Mothers were asked to complete the form three times to indicate (a) which behavior they had used towards their spouses (perpetration) in the past year; (b) which behavior their spouses had used towards them (victimization) in the past year; and (c) which behavior their adolescents had used within the family in the past year. Adolescents also completed the CTS Form N about their physical aggressive behavior within the family over the past year. Adolescent reports were used for the adolescent aggression variable with the exception of 15 adolescents, who did not complete self-reports. In those cases, maternal reports were used (r = .35, p < .01 for adolescent and maternal reports of physical aggression).
Covariates
In the adolescent analyses, sex and age were included because of the age range across cohorts and the potential for sex differences in adolescent physical aggression.
Socioeconomic status
At T1, families’ socioeconomic status was classified using the Hollingshead Four-Factor Index, which is a summary score comprised of the head of households’ sex, marital status, overall level of education attained, and occupation (Hollingshead, 1975). For the current study, raw scores were transformed into T-scores.
Maternal global assessment of functioning (GAF)
As part of the structured diagnostic interviews administered to mothers at T3, clinicians also rated mothers’ overall functioning with the GAF from Axis V of the DSM-III-R (Endicott, Spitzer, Fleiss, & Cohen, 1976). To generate the GAF, a score of 1–100 is assigned to characterize the overall level of adjustment, with higher scores indicating better adjustment.
Data Analytic Plan and Missing Data
The missing data in the current study were very minimal and ranged from 0% (maternal and paternal diagnoses, maternal IPV perpetration, adolescent aggression, family SES) to 3% (maternal GAF, maternal IPV victimization); thus, analyses to compensate for missing data were not deemed necessary.
To address Hypothesis 1, which anticipated that mothers with depression and BD would display higher levels of IPV than well mothers, two separate one-way analyses of covariance (ANCOVA) tests for perpetration and victimization were conducted. The independent variable was maternal diagnosis of well, unipolar depression or BD, while family SES and maternal GAF were the covariates. For Hypothesis 1, the dependent variables, maternal IPV perpetration and victimization, were examined as raw scores in the ANCOVA tests.
To address Hypothesis 2, four binary logistic regression models with moderators were conducted (maternal depression x IPV perpetration, maternal depression x IPV victimization, maternal BD x IPV perpetration, and maternal BD x IPV victimization). The interaction terms were computed by multiplying the dichotomous maternal diagnosis (presence or absence of depression or BD) by the dichotomous IPV status (presence or absence of any IPV perpetration or any victimization). The dichotomous score of adolescent aggression was the dependent variable, with covariates (adolescent sex and age, family SES, and maternal GAF) in the first step, main effects of maternal diagnosis and IPV status in the second step, and the interaction between diagnosis and IPV in the third step. Because there were two adolescents from each family, the interclass correlations between siblings’ aggression scores were accounted for, and the p-values of the standardized coefficients in the logistic regressions were corrected to be more stringent (Hedges, 2007).
Finally, to address Hypothesis 3, two different types of analyses were conducted. The first analyses again utilized ANCOVAs. For the first ANCOVA, maternal IPV perpetration was the dependent variable, and the independent variables were maternal diagnosis, presence of any paternal psychopathology, and the interaction between maternal diagnosis and paternal psychopathology. The second ANCOVA substituted maternal IPV victimization as the dependent variable. Both ANCOVAs included SES and maternal GAF as the covariates. The second analysis utilized a cumulative risk score, which was compiled to determine whether a greater number of cumulative risks (presence of either maternal depression or BD, paternal psychopathology, maternal IPV perpetration, and maternal IPV victimization) predicted greater odds of adolescent aggression. This analysis again employed a logistic regression. Covariates included SES, maternal GAF, and adolescent age and sex.
For Hypotheses 2 and 3, maternal IPV perpetration and victimization raw scores were dichotomized into presence or absence of maternal perpetration or victimization for the regression analyses. Adolescent aggression also was dichotomized into presence or absence of aggression for all adolescent analyses. These variables were dichotomized because of significant positive skewness in the data. Specifically, 79% (n = 61) of mothers endorsed no physical aggression. Similarly, 43% (n = 51) of adolescents endorsed no physical aggression whereas 16% (n = 19) of adolescents endorsed high aggression (scores of at least 10). To account for the non-normal distributions of the CTS raw scores, analyses to address Hypothesis 1 were conducted with bootstrapping (500 samples) in SPSS version 22.
Results
Descriptive statistics are displayed in Table 1. Maternal perpetration was significantly associated with maternal victimization, r = .29, p < .05 across groups. When this association was specifically examined within each diagnosis group, maternal perpetration and victimization were only significantly associated in families with maternal depression, r = .42, p < .05 (r = .14, p = n.s., and r = .03, p = n.s. for the association between perpetration and victimization in families with well mothers or mothers with BD, respectively). Descriptive chi-square tests also revealed significant concordance between maternal diagnosis and perpetration, χ2(1, 61) = 7.20, p < . 05, but not maternal diagnosis and victimization, χ2(1, 59) = 1.96, p = n. s. (Table 2).
Table 1.
Demographic Characteristics and Descriptive Statistics by Maternal Diagnosis
| Variable | Unipolar (n = 24) |
Bipolar (n = 13) |
Well (n = 24) |
|---|---|---|---|
| Paternal diagnosis, n (%) | |||
| Psychopathology* | 13 (54%) | 9 (69%) | 1 (4%) |
| Well | 11 (46%) | 4 (31%) | 23 (96%) |
| Family diagnosis, n (%) | |||
| Control | 0 (0%) | 0 (0%) | 23 (96%) |
| One parent psychopathology | 11 (46%) | 4 (31%) | 1 (4%) |
| Two parents psychopathology | 13 (54%) | 9 (69%) | 0 (0%) |
| Family composition, n (%) | |||
| Married | 24 (100%) | 13 (100%) | 24 (100%) |
| Biological fathers† | 46 (96%) | 17 (71%) | 46 (96%) |
| Socioeconomic status at T1, M (SD) | 51.42 (14.68) | 53.08 (12.41) | 58.83 (7.90) |
| Maternal race, n (%) | |||
| Caucasian | 22 (92%) | 12 (92%) | 22 (92%) |
| African-American | 2 (8%) | 1 (8%) | 1 (4%) |
| Asian-American | 0 (0%) | 0 (0%) | 1 (4%) |
| Maternal age, M (SD) | 44.33 (5.19) | 43.96 (3.50) | 45.12 (4.19) |
| Maternal GAF at T3, M (SD) | 65.83 (9.05) | 58.69 (11.39) | 80.04 (8.48) |
| IPV-P (continuous), M (SD) | .25 (.53) | 1.31 (1.60) | .08 (.28) |
| IPV-P (binary), n (%) | 5 (21%) | 6 (46%) | 2 (8%) |
| IPV-V (continuous), M (SD) | 1.00 (1.81) | 1.83 (3.43) | .42 (.93) |
| IPV-V (binary), n (%) | 8 (33%) | 5 (38%) | 5 (21%) |
| Adolescent age, M (SD) | |||
| Younger | 13.50 (1.77) | 12.77 (1.36) | 13.42 (1.95) |
| Older | 17.04 (1.27) | 16.45 (1.75) | 16.54 (1.67) |
| Adolescent male sex, n (%) | 24 (50%) | 10 (42%) | 23 (48%) |
| Adolesc. aggression (binary), n (%) | 31 (65%) | 14 (58%) | 24 (50%) |
Note.
Paternal psychopathology consists of depressive (n = 21) and anxiety disorders (n = 2).
Numbers and percentages are doubled because they reflect the number of total adolescents. GAF = Global Adjustment Scale. IPV-P = IPV Perpetration; IPV-V = IPV Victimization.
Table 2.
Concordance Between Maternal Diagnosis and IPV Perpetration and Victimization
| IPV Perpetration | IPV Victimization* | |||
|---|---|---|---|---|
| Maternal Diagnosis | No IPV (n = 48) | IPV (N = 13) | No IPV (n = 41) | IPV (n = 18) |
| MDD (n = 24) | 19 (79%) | 5 (21%) | 15 (63%) | 8 (33%) |
| BD (n = 13) | 7 (54%) | 6 (46%) | 7 (54%) | 5 (38%) |
| Well (n = 24) | 22 (92%) | 2 (8%) | 19 (79%) | 5 (21%) |
Note. IPV = Interparental Violence; Maternal Diagnosis x IPV Perpetration: χ2(1, 61) = 7.20, p < .05; Maternal Diagnosis x IPV Victimization: χ2(1, 59) = 1.96, p = n. s.
Two families (one with maternal MDD and one with maternal BD) were missing data on maternal victimization
Aim 1
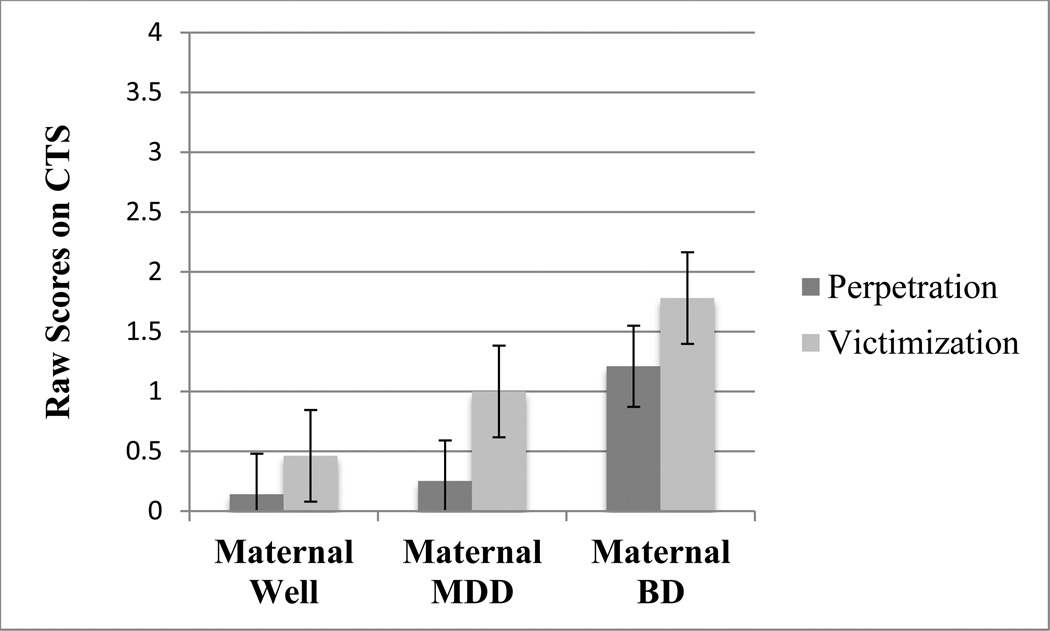
For maternal IPV perpetration, the ANCOVA of maternal diagnosis was significant, F(2, 55) = 5.77, p < .01, η2 = .17. Follow-up pairwise contrasts were conducted to examine differences among the adjusted means for maternal diagnosis, and the Bonferroni correction (α’ = .05/3 = .017) was applied across the three pairwise comparisons. Mothers with BD had significantly higher adjusted mean levels of IPV perpetration (M = 1.21, SD = .94) than mothers with unipolar depression (M = .25; SD = .88, p = .002) or well mothers (M = .14; SD = 1.01; p = .007), while the latter two groups did not significantly differ in level of perpetration. Conversely, although mean levels were in the expected direction, the ANCOVA of maternal diagnosis was not significant for maternal victimization, F(2, 55) = 3.90, p = n. s., η2 = .03 (Figure 1).
Figure 1.
Level of Maternal Interparental Violence Perpetration and Victimization by Diagnosis
Note. CTS = Conflict Tactics Scale. There was a significant effect of maternal diagnosis group on maternal IPV perpetration, F(2, 55) = 5.77, p < .01, η2 = .17, but not victimization, F(2, 55) = 3.90, p = n. s., η2 = .03. Please note that the range of possible raw scores on the CTS is zero to 54; regardless of maternal diagnostic group, very low levels of IPV perpetration and victimization were reported.
Aim 2
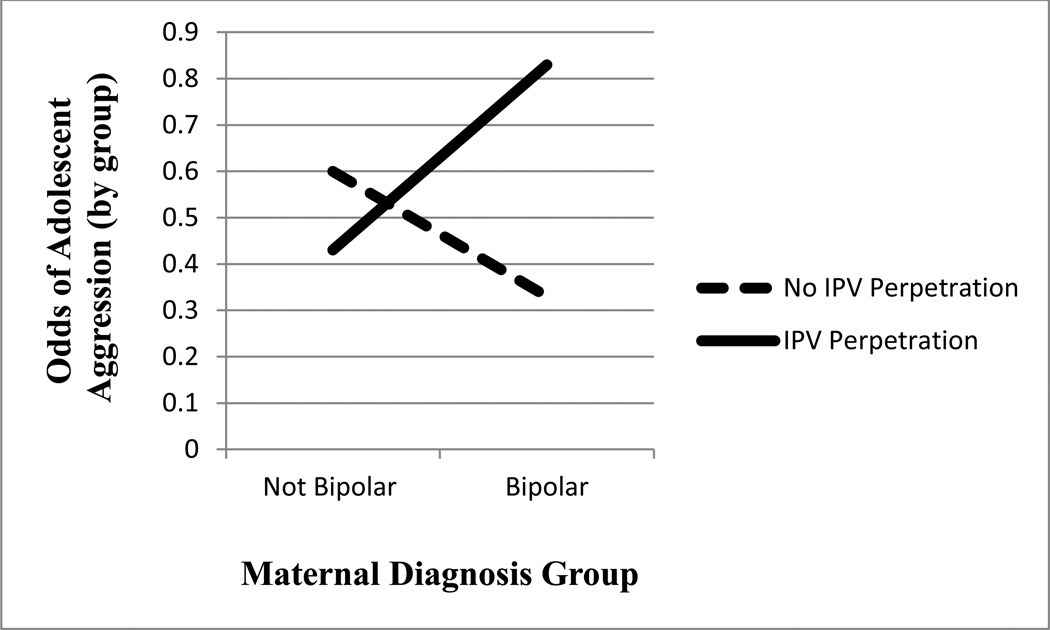
Four binary logistic regression models next examined the interactions between maternal depression or BD and IPV perpetration or victimization. In the first model, adolescent aggression was regressed onto adolescent age and sex, SES, and maternal GAF in the first step, maternal depression and presence of maternal perpetration in the second step, and the interaction between maternal depression and perpetration in the third step. Results showed that there were no significant main effects of depression or perpetration and no significant interaction between depression and perpetration for adolescent aggression. In the second model, the regression was repeated with maternal victimization substituted for perpetration. Again, there were no significant main effects or interaction. In the third model, adolescent aggression was regressed onto the covariates in the first step, maternal BD and presence of maternal perpetration in the second step, and the interaction between maternal BD and perpetration in the third step. Results showed that although the main effects were not significant, the interaction between maternal BD and perpetration was significant, ß = 2.93, SE = 1.54, p < .05, odds ratio (OR) = 18.65 (Table 3). Finally, the fourth model was repeated with maternal victimization instead of perpetration. Results indicated no significant main effects or interaction.
Table 3.
Logistic Regression of Adolescent Aggression on Maternal BD, IPV Perpetration, and the Interaction
| Step 1 | Step 2 | Step 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor | B | SE B | expB | B | SE B | expB | B | SE B | expB |
| Adolescent sex | −.81 | .40 | .45 | −.78 | .40 | .46 | −.85 | .42 | .43 |
| Adolescent age | −.14 | .09 | .87 | −.15 | .09 | .86 | −.13 | .09 | .88 |
| Family SES | −.02 | .02 | .98 | −.02 | .02 | .98 | −.03 | .02 | .97 |
| Maternal GAF | −.03 | .02 | .98 | −.03 | .02 | .97 | −.02 | .02 | .98 |
| Maternal BD | −.56 | .59 | .57 | −1.44 | .72. | .24 | |||
| Maternal IPV-P | .32 | .53 | 1.38 | −.57 | .65 | .56 | |||
| Maternal BDxIPV-P | 2.93* | 1.25 | 18.65* | ||||||
| Step χ2 | 13.53 | 1.04 | 5.98 | ||||||
| Model χ2 | 13.53 | 14.57 | 20.56 | ||||||
| Nagelkerke’s R2 | .15 | .16 | .21 | ||||||
| % Classification | 63.6 | 66.9 | 64.4 | ||||||
Note. BD = Bipolar Disorder, IPV-P = Interparental Violence Perpetration
p < .05
Further probing the interaction between maternal BD and perpetration showed that the simple slope of maternal BD status on adolescent aggression was significant when maternal IPV perpetration was present (p < .05), but not when it was absent (Figure 2). More specifically, as depicted on the graph (y-axis, “Odds of Adolescent Aggression”), if mothers had BD and perpetrated IPV, 83.3% (10/12) of adolescents in that group were physically aggressive. Converserly, when mothers had BD but did not perpetrate IPV, only 33.3% (4/12) of adolescents were physically aggressive. Moreover, when mothers did not have BD but perpetrated IPV, 42.9% (6/14) of adolescents were physically aggressive, and when mothers did not have BD or perpetrate IPV, 59.8% (49/82) of adolescents were physically aggressive (Figure 2).
Figure 2.
Effects of Maternal Diagnostic Group on Adolescent Physical Aggression by Maternal IPV Status
Note. Slope of IPV Perpetration, p < .05. Slope of No IPV Perpetration, p = .n.s.
Odds of Adolescent Aggression by group: Maternal BD, IPV Perpetration: 83.3% (10/12 adolescents in this group were aggressive); Maternal BD, No IPV Perpetration: 33.3% (4 /12); No Maternal BD, IPV Perpetration: 42.9% (6/14); No Maternal BD, No IPV Perpetration: 59.8% (49/82).
Aim 3
The final analyses examined whether the associations between maternal mood disorder diagnosis and maternal perpetration and victimization of IPV would be amplified when paternal psychopathology was also considered. Beyond the significant main effect for maternal diagnosis, F(2, 52) = 4.23, p < .05, η2 = .14, which was consistent with Aim 1, the ANCOVAs failed to show significant main effects for paternal psychopathology or interaction effects of maternal diagnosis and paternal psychopathology for maternal IPV perpetration. The second ANCOVA also indicated no significant main effects of maternal diagnosis or paternal psychopathology or interaction effects of maternal diagnosis and paternal psychopathology for maternal IPV victimization.
Finally, the effects of cumulative risk of maternal diagnosis, paternal psychopathology, and IPV perpetration and victimization on adolescent aggression were examined. Across the sample, 28.3% (n = 34) of adolescents had zero of these risks, 25.8% (n = 31) had one risk, 19.2% (n =23) had two risks, 11.7%% (n = 14) had three risks, and 11.7%% (n = 14) had all four risks [3% of adolescent (n = 4) were missing information used to compute the cumulative risk score]. The logistic regression conducted to examine the effects of cumulative risk, after controlling for adolescent age and sex, SES, and maternal GAF, indicated that the cumulative risk score was not a significant predictor of higher odds of adolescent physical aggression.
Discussion
The current study examined the relations between type of maternal mood disorder and maternal perpetration and victimization of IPV, and the moderating effects of IPV on the associations between maternal mood disorders and adolescent physical aggression. Adolescence was the focal developmental period of interest, as this is a time when the normative frequency and intensity of interpersonal conflict are typically elevated (Erikson, 1963; Hall, 1904; Laursen et al., 1998).
The first hypothesis anticipated that mothers with BD or depression would exhibit heightened levels of IPV compared to well mothers. Part of this hypothesis was supported. Findings from chi-square tests showed that there was significant concordance between maternal diagnosis and IPV perpetration, although the association between mood disorder and IPV victimization was not significant. Even though the sample and cell sizes were small, approximately twice as many mothers with BD (46%) than mothers with unipolar depression (21%) reported IPV perpetration. ANCOVA tests controlling for numerous covariates further indicated that mothers with BD reported significantly higher levels of IPV perpetration than depressed or well mothers. This finding supports past research on elevations in general aggression in individuals with BD compared to non-BD psychopathology (Ballester et al., 2012) and extends this research to include elevations in physical IPV in mothers with BD. Contrary to predictions, however, mothers with depression showed only modest prevalence of IPV perpetration (21%), yielding no significant differences compared to well mothers (8%). It is possible that these findings would have been different had other conflict tactics such as verbal conflict been examined in addition to physical IPV. It is important to note, however, that regardless of maternal diagnostic group, relatively low levels of maternal IPV perpetration or victimization were reported; thus, these results should be interpreted cautiously.
The levels of maternal IPV perpetration and victimization within families were modestly related across all groups, which supports past evidence that in relationships where IPV is present, perpetration and victimization are likely to co-occur (Langer et al., 2008; Moffitt & Caspi, 1999; Narayan, Englund et al., 2013). However, this association was driven by the highest co-occurrence of perpetration and victimization in families where mothers had unipolar depression rather than BD or no diagnosis. It is possible that in families with depressed mothers, IPV perpetration and victimization may be more reciprocal in nature. This observation aligns with past findings that couples with BD may not converge on the level of conflict used in their intimate relationships. Rather, one partner may use higher levels of IPV than the other, accounting for the low correlations between perpetration and victimization in the families with maternal BD (Hoover & Fitzgerald, 1981). Broadly, these findings also suggest there may be distinct marital profiles of IPV across different types of mood disorders. Families with maternal BD may have the highest rates of IPV perpetration, but not necessarily victimization. Conversely, while families with maternal depression may have lower levels of overall IPV than families with BD, perpetration and victimization may be more likely to co-occur between parents when the mother has unipolar depression.
The second hypothesis predicted that maternal IPV would moderate the association between parental mood disorders and elevated adolescent aggression. Adolescents were at significantly higher risk for using physical aggression if their mothers had BD and perpetrated IPV. These findings echo past research that mood disorders and elevated marital conflict may be dual risks for child adjustment (Beardslee et al., 1998; Bella et al., 2011; Chang et al., 2001). They also suggest that it may be critical to consider the type of mood disorder and type of IPV from the primary caregiver when evaluating risk factors for adolescent physical aggression within the family context. Adolescent aggression was not elevated in family contexts of maternal BD and IPV victimization, or maternal depression and either IPV perpetration or victimization. It is possible that maternal IPV victimization would have had an effect on adolescent aggression had adolescents reported on their experiences of victimization, in addition to perpetration, within their families.
Findings from the current study suggest that the risks for adolescent aggression may be interactive, rather than additive. The risks for adolescents to become physically aggressive increased by more than 18-fold, (reflected by the odds ratio for the significant interaction coefficient for maternal BD by IPV perpetration) if their mothers had BD and reported perpetrating IPV over the past year. Despite these findings, however, many other factors are likely to have contributed to elevated risks for adolescent aggression. As was evident by the interaction depicted in Figure 2, the group of adolescents with the second highest risk for aggression had mothers with neither BD nor IPV perpetration (although mothers from this group may have had depression). Taken together, these findings suggest that there are additional, unmeasured contributing factors for adolescent aggression.
Additional support for risks for adolescent aggression being interactive was evident in the observation that despite high variation of cumulative risk across the sample, the cumulative risk index, a measure of additive risks of maternal and paternal psychopathology and IPV, did not significantly predict greater odds of adolescent aggression. Taken together, these observations suggest that risks for adolescent aggression may specifically include maternal BD and IPV perpetration, rather than psychopathology and IPV in both parents more broadly. It is possible that primary caregivers who have BD and perpetrate physical aggression to solve conflict are particularly salient, yet poor, models of conflict management for adolescents (Muralidharan et al., 2010; Vance et al., 2008).
The current study did not find that maternal IPV perpetration or victimization were further amplified in the presence of paternal psychopathology in addition to maternal mood disorders. Given the small sample size and the focus on maternal psychopathology in the larger study from which the current sample was drawn, the lack of effects both for paternal psychopathology on maternal IPV perpetration or victimization, and for cumulative risk on adolescent aggression, should be interpreted with caution. It is possible that paternal psychopathology would have had a larger effect on maternal IPV or adolescent aggression in a larger sample, or if both parents had BD. However, no father in the current study had a diagnosis of BD, so this could not be tested. The best interpretation of the current findings is that adolescents may be particularly vulnerable to being aggressive if their mothers have BD and perpetrate IPV, but additional paternal effects on maternal IPV or adolescent aggression are not clearly known.
Strengths and Limitations
Very few studies have sought to understand how modeling of maladaptive conflict resolution may affect adolescent maladjustment, such as aggressive behavior, in offspring at risk for mood disorders. To our knowledge, this study was the first to examine how elevations in IPV differ across families with maternal BD, unipolar depression, and well parents and exacerbate the associations between parental mood disorders and adolescent physical aggression within the family. Given that impairments in interpersonal and marital functioning are so closely tied to mood disorders in adults (Goodwin & Jamison 1990; Mathews & Reus, 2001; Prince & Jacobson, 1995) it is critical to examine how these interpersonal risks may affect parenting of adolescents and adolescent interpersonal development. By examining IPV perpetration and victimization within distinct types of lifetime parental mood disorders, this study was able to identify particularly negative combinations of IPV and mood disorders for adolescent maladjustment. Although this study was mostly cross-sectional, a strength was that the data reflected information from multiple informants, including from mothers (for reports of IPV), clinicians (for diagnostic algorithms to assign formal mood disorder diagnoses), and adolescents (for reports of physical aggression).
The conclusions of this study are tempered by several limitations. Foremost, the sample was small, and general and group-specific rates of IPV were relatively low. There were no main effects between IPV and adolescent aggression, regardless of parental mood disorder status, that were expected given the extant literature (Davies & Cummings, 1994; Kitzmann et al., 2003). Although IPV is found to be common even in affluent samples (Ehrensaft et al., 2004; Straus, 1979), many mothers in the current sample reported no IPV. Thus, it is possible that main effects of maternal IPV and adolescent aggression were not found because of the low rates of IPV endorsed in this sample. In addition to the small sample, the current study was limited to including only intact families, as only married families completed the CTS at T4. These intact families had lower histories of marital stress, higher SES, and mothers with higher GAF scores, which suggests that excluded families, such as those who separated or divorced between T1 and T4, may have been functioning more poorly in some ways. Had the current study been able to include all families, higher variation in IPV may have been observed. The current study also was constrained to using covariates that were only available at certain data collection periods (e.g., SES at T1 and maternal GAF at T3, rather than T4). T1 and T3 were major periods of data collection for the larger longitudinal study from which this subsample was drawn. Ideally, future studies would have the ability to use covariates that were collected concurrently to the independent, dependent and moderator variables.
Additional limitations include reporter biases and sample design considerations. Mothers reported on their own IPV and fathers’ IPV, which precluded the ability to obtain IPV reports from fathers’ perspectives. Although the literature suggests that individuals within violent relationships are comparably likely to disclose experiences of victimization and perpetration (Moffitt et al., 1997; Narayan, Englund et al., 2013), the present findings would have been strengthened with fathers’ direct reports of IPV. A small subset of mothers also reported on their adolescents’ aggression because self-reports of adolescent aggression were not available. Additionally, given that recruitment for this study focused on mothers with mood disorders, all of whom were primary caregivers when adolescents were enrolled, paternal psychopathology was less inclusive. Thus, it was not possible, for example, to determine whether paternal BD and IPV perpetration also could have had potent effects on adolescent aggression. Inclusion of paternal BD specifically, as well as paternal reports of IPV also may have provided evidence for cumulative risks to adolescents of parents who both had mood disorders and engaged in IPV. Moreover, although directionality of effects between mood disorders and IPV has been documented (Golding, 1999; Pollack, 1993), the current study did not address causal pathways. This study also only addressed one of the many processes, elevations in parental IPV, by which offspring of parents with mood disorders may be at heightened risk for maladjustment. It did not consider additional processes such as genetic predispositions to behavioral dysregulation and aggression.
Finally, it is important to interpret the current findings within the historical context when this data was collected. Diagnostic data were drawn from T1 (1979–1981) and T3 (1989), and IPV data was collected at T4 (1993) using the CTS. At that time, an original version of the CTS was used, rather than the revised CTS-2. The most significant change in the updated version that could have affected the current findings was the inclusion of more items of physical assault (12 rather than nine); thereby affecting raw scores of physical aggression in the first aim of the present study. However, given the very low prevalence of physical violence in the current sample, it is unlikely that a greater repertoire of possible physically aggressive behavior would have substantially affected the findings. Furthermore, dichotomizing scores into the presence or absence of aggression, which was employed in all other study aims, is recommended for both the CTS and CTS-2 and would not have affected the current results (Straus, Hamby, Boney-McCoy, & Sugarman, 1996).
In terms of the historical context of mood disorder classification, the diagnostic criteria used here relied on RDC and DSM-III-R criteria for depression and BD. While the criteria for depression has changed minimally from then until now, major updates to the BD criteria have included specifying the duration of symptoms, which helped to distinguish BD-I from BD-II, specifying BD-Not Otherwise Specified (NOS) from BD-II (both of which were updated in the DSM-IV, APA, 1994; Dunner, 1992); and clarifying the initial gate question, such that predominant symptoms of elated/euphoric or irritable mood must be accompanied by persistent elevations in activity or energy levels (updated in the DSM-5; Angst, 2013). Although the current study included mothers who had BD-I and BD-II, thus reducing issues associated with the changes in duration criteria, it is possible that some mothers in the present study would have met criteria for BD-NOS according to the DSM-IV, or would not have met criteria for BD at all according to the DSM-5, had they not experienced elevated activity or energy levels. Generally speaking, although it is not possible to ascertain completely accurate and enduring diagnostic information, as diagnostic criteria undergoes continual revisions, it is recommended that future research replicate the current findings with the most updated versions of the DSM.
These strengths and limitations suggest numerous avenues for subsequent research. Future research should continue to examine additional processes by which maternal mood disorders may contribute to elevated risks for adolescent aggression, as the current study only examined IPV as one vulnerability process. Future studies also could examine the strength of these effects in different developmental periods besides adolescence. For example, compared to toddlers with well parents, toddlers with a parent with BD exhibited more aggression with peers (Zahn-Waxler, McKnew, Cummings, Davenport, & Radke-Yarrow, 1984). This finding suggests that maladaptive interpersonal development in children of parents with mood disorders may emerge very early. Additionally, future studies should determine whether offspring in families with parental mood disorders also show elevations in victimization of aggression, such as from their siblings or parents, or interpersonal aggression in other contexts, such as bullying peers or being victimized at school.
In conclusion, this study provides novel insight about the risks facing adolescents and parents in families with maternal mood disorders and elevated IPV. In terms of prevention and intervention efforts, programs that help to promote positive conflict resolution strategies in high-risk parents may also want to evaluate for cascading effects of effective conflict resolution strategies in adolescents. Evidence-based practices, such as family-focused treatment for BD, may be particularly effective in promoting adolescents’ psychosocial adjustment and conflict management with their parents and siblings (Miklowitz, 2010). Given that family processes are often interdependent and transactional, such efforts to promote healthy conflict resolution skills in adolescents at risk for mood disorders and interpersonal aggression may have reciprocal effects of reducing marital and parenting strain during adolescence. Continued efforts to understand the processes by which parental psychopathology contributes to adolescent risk via parental dysfunctional behavior would further illuminate how to promote parental and adolescent competence in high-risk families.
Acknowledgments and Funding Sources
Many have contributed significantly to this study, including Anne Mayfield and Gale Inoff-Germain. We want to thank the NIMH Childrearing Study participants who have shown such tremendous dedication by contributing to the understanding of mood disorders.
Funding for the first author was provided by a Graduate School Fellowship from the University of Minnesota. This study was supported by the Intramural Program of the National Institute of Mental Health (NIMH) and the Catherine T. MacArthur Foundation. It is part of a larger study of children of depressed mothers (“Study of Psychological Development of Children of Parents With and Without Affective Disorders”; protocol number NCT00001170; P.W. Gold, PI; also referred to as the “Childrearing Study”) directed for more than two decades by Marian Radke-Yarrow, Ph.D., through the Child Development Section of the NIMH, and currently led by Philip W. Gold, M.D, of the Clinical Neuroendocrinology Branch of the NIMH.
Footnotes
The authors report no conflicts of interest.
References
- Amato PR. Children’s adjustment after divorce: Theories, hypotheses, and empirical support. Journal of Marriage and Family. 1993;55:23–28. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed., rev. Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Angst J. Bipolar disorders in DSM-5: strengths, problems and perspectives. International Journal of Bipolar Disorders. 2013;1:12–14. doi: 10.1186/2194-7511-1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballester J, Goldstein T, Goldstein B, Obreja M, Axelson B, Monk K, … Birmaher B. Is bipolar disorder specifically associated with aggression? Bipolar Disorders. 2012;14:283–290. doi: 10.1111/j.1399-5618.2012.01006.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Aggression: A social learning analysis. Englewood Cliffs, NJ: Prentice Hall; 1973. [Google Scholar]
- Beardslee W, Versage EM, Gladstone TRG. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Bella T, Goldstein T, Axelson D, Obreja M, Monk K, Hickey MB, Birmaher B. Psychosocial functioning in offspring of parents with bipolar disorder. Journal of Affective Disorders. 2011;133:204–211. doi: 10.1016/j.jad.2011.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Monk K, Cal as C, Goldstein B, Hickey MB, Brent D. Lifetime psychiatric disorders in school-aged offspring of parents with bipolar disorder. Archives of General Psychiatry. 2009;66:287–296. doi: 10.1001/archgenpsychiatry.2008.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capaldi DM, Knoble NB, Shortt JW, Kim HK. A systematic review of risk factors for intimate partner violence. Partner Abuse. 2012;3:231–280. doi: 10.1891/1946-6560.3.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappell C, Heiner RB. The intergenerational transmission of family aggression. Journal of Family Violence. 1990;5:135–152. [Google Scholar]
- Chang KD, Blasey C, Ketter TA, Steiner H. Family environment of children and adolescents with bipolar disorder. Bipolar Disorder. 2001;3:73–78. doi: 10.1034/j.1399-5618.2001.030205.x. [DOI] [PubMed] [Google Scholar]
- Davies PT, Cummings EM. Marital conflict and child adjustment: An emotional security hypothesis. Psychological Bulletin. 1994;116:387–411. doi: 10.1037/0033-2909.116.3.387. [DOI] [PubMed] [Google Scholar]
- Davies PT, Dumenci L, Windle M. The interplay between maternal depressive symptoms and marital distress in the prediction of adolescent adjustment. Journal of Marriage and Family. 1999;61:238–254. [Google Scholar]
- Davies PT, Windle M. Gender-specific pathways between maternal depressive symptoms, family discord, and adolescent adjustment. Developmental Psychology. 1997;33:657–668. doi: 10.1037//0012-1649.33.4.657. [DOI] [PubMed] [Google Scholar]
- Diler RS, Birmaher B, Axelson D, Obreja M, Monk K, Hickey MB, Kupfer D. Dimensional psychopathology in offspring of parents with bipolar disorder. Bipolar Disorders. 2011;13:670–678. doi: 10.1111/j.1399-5618.2011.00966.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, Patterson GR. The development and ecology of antisocial behavior in childhood and adolescence. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology Vol. 3: Risk, disorder, and adaptation. New York: Wiley; 2006. pp. 503–541. [Google Scholar]
- Dore G, Romans SE. Impact of bipolar affective disorder on family and partners. Journal of Affective Disorders. 2001;67:147–158. doi: 10.1016/s0165-0327(01)00450-5. [DOI] [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Du Rocher Schudlich TD, Younstrom EA, Calabrese JR, Findling RF. The role of family functioning in bipolar disorder in families. Journal of Abnormal Child Psychology. 2008;36:849–863. doi: 10.1007/s10802-008-9217-9. [DOI] [PubMed] [Google Scholar]
- Dunner DL. Differential diagnosis of bipolar disorder. Journal of Clinical Psychopharmacology. 1992;12:7S–12S. doi: 10.1097/00004714-199202001-00002. [DOI] [PubMed] [Google Scholar]
- Ehrensaft MK, Moffitt TE, Caspi A. Clinically abusive relationships in an unselected birth cohort: Men’s and women’s participation and developmental antecedents. Journal of Abnormal Psychology. 2004;113:258–270. doi: 10.1037/0021-843X.113.2.258. [DOI] [PubMed] [Google Scholar]
- Emery R, Weintraub S, Neale JM. Effects of marital discord on the school behavior of children of schizophrenic, affectively ill, and normal parents. Journal of Abnormal Child Psychology. 1982;10:215–228. doi: 10.1007/BF00915942. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The global assessment scale: A procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry. 1976;33:766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- Erikson EH. Childhood and society. 2nd ed. New York: Norton; 1963. [Google Scholar]
- Essex MJ, Klein MH, Cho E, Kraemer HC. Exposure to maternal depression and marital conflict: Gender differences in children’s later mental health symptoms. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:728–737. doi: 10.1097/01.CHI.0000046849.56865.1D. [DOI] [PubMed] [Google Scholar]
- Fear JM, Champion JE, Reeslund KL, Forehand R, Colletti C, Roberts L, Compas BE. Parental depression and interparental conflict: Children and adolescents’ self-blame and coping responses. Journal of Family Psychology. 2009;23:762–766. doi: 10.1037/a0016381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman TB. Bipolar disorder and violence. Psychiatric Quarterly. 2001;72:119–129. doi: 10.1023/a:1010315509112. [DOI] [PubMed] [Google Scholar]
- Garber J. Depression in youth: A developmental psychopathology perspective. In: Masten AS, editor. Multilevel dynamics in developmental psychopathology: The Minnesota Symposia in child psychology. Vol. 34. Mahwah, NJ: Lawrence Erlbaum; 2007. pp. 181–241. [Google Scholar]
- Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. Journal of Family Violence. 1999;14:99–132. [Google Scholar]
- Goodwin FK, Jamison KR. Manic-Depressive Illness. 1st Edition. Oxford: Oxford University Press; 1990. [Google Scholar]
- Hall GS. Adolescence: Its psychology and its relations to physiology, anthropology, sociology, sex, crime, religion, and education. Vols. 1 and 2. New York: Appleton; 1904. [Google Scholar]
- Hammen C, Brennan PA. Interpersonal dysfunction in depressed women: Impairments independent of depressive symptoms. Journal of Affective Disorders. 2002;72:145–156. doi: 10.1016/s0165-0327(01)00455-4. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA, Shih JH. Family discord and stress predictors of depression and other disorders in adolescent children of depressed and nondepressed women. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:994–1002. doi: 10.1097/01.chi.0000127588.57468.f6. [DOI] [PubMed] [Google Scholar]
- Hedges LV. Effect sizes in cluster-random designs. Journal of Educational and Behavioral Statistics. 2007;32:341–370. [Google Scholar]
- Heene E, Buysse A, Van Oost P. An interpersonal perspective on depression: The role of marital adjustment, conflict communications, attributions, and attachment within a clinical sample. Family Process. 2007;46:499–514. doi: 10.1111/j.1545-5300.2007.00228.x. [DOI] [PubMed] [Google Scholar]
- Henning K, Jones A, Holdford R. Treatment needs of women arrested for domestic violence: A comparison with male offenders. Journal of Interpersonal Violence. 2003;18:839–856. doi: 10.1177/0886260503253876. [DOI] [PubMed] [Google Scholar]
- Hetherington EM, Clingempeel WG. Coping with marital transitions: A family systems perspective. Monographs of the Society for Research in Child Development. 1992;57 [Google Scholar]
- Hollingshead AB. Four-factor Index of Social Status. New Haven: Yale University Sociology Department; 1975. [Google Scholar]
- Hoover CF, Fitzgerald RG. Marital conflict of manic-depressive patients. Archives of General Psychiatry. 1981;38:65–67. doi: 10.1001/archpsyc.1981.01780260067007. [DOI] [PubMed] [Google Scholar]
- Kahn J, Coyne JC, Margolin G. Depression and marital disagreement: The social construction of despair. Journal of Social and Personal Relationships. 1985;2:447–461. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Wang PS. The epidemiology of Major Depressive Disorder: Results from the National Comorbidity Survey Replication (NCS-R) Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Molnar BE, Feurer ID, Appelbaum M. Patterns and mental health predictors of domestic violence in the United States: Results from the National Comorbidity Survey. International Journal of Law and Psychiatry. 2001;24:487–508. doi: 10.1016/s0160-2527(01)00080-2. [DOI] [PubMed] [Google Scholar]
- Kitzmann KM, Gaylord NK, Holt AR, Kenny ED. Child witness to domestic violence: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2003;71:339–352. doi: 10.1037/0022-006x.71.2.339. [DOI] [PubMed] [Google Scholar]
- Klimes-Dougan B, Long JD, Lee C-YS, Ronsaville DS, Gold PW, Martinez PE. Continuity and cascade in offspring of bipolar parents: A longitudinal study of externalizing, internalizing, and thought problems. Development and Psychopathology. 2010;22:849–866. doi: 10.1017/S0954579410000507. [DOI] [PubMed] [Google Scholar]
- Langer A, Lawrence E, Barry RA. Using a vulnerability- stress-adaptation framework to predict physical aggression trajectories in newlywed marriage. Journal of Consulting and Clinical Psychology. 2008;76:756–768. doi: 10.1037/a0013254. [DOI] [PubMed] [Google Scholar]
- Laursen B, Collins WA. Interpersonal conflict during adolescence. Psychological Bulletin. 1994;115:197–209. doi: 10.1037/0033-2909.115.2.197. [DOI] [PubMed] [Google Scholar]
- Laursen B, Coy KC, Collins WA. Reconsidering changes in parent-child conflict across adolescence: A meta-analysis. Child Development. 1998;69:817–832. [PMC free article] [PubMed] [Google Scholar]
- Margolin G. Children’s exposure to violence: Exploring developmental pathways to diverse outcomes. Journal of Interpersonal Violence. 2005;20:72–81. doi: 10.1177/0886260504268371. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG. Major depression and conduct disorder in youth: Associations with parental psychopathology and parent-child conflict. Journal of Child Psychology and Psychiatry. 2004;45:377–386. doi: 10.1111/j.1469-7610.2004.00228.x. [DOI] [PubMed] [Google Scholar]
- Mathews CA, Reus VI. Assortative mating in the affective disorders: A systematic review and meta-analysis. Comprehensive Psychiatry. 2001;42:257–262. doi: 10.1053/comp.2001.24575. [DOI] [PubMed] [Google Scholar]
- McLanahan S, Sandefur G. Growing up with a single parent. Cambridge, MA: Harvard University Press; 1994. [Google Scholar]
- Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld R, Petukhova M, Kessler RC. Lifetime and 12-month prevalence of Bipolar Spectrum Disorder in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2007;64:543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miklowitz DJ. Bipolar disorder: A family-focused treatment approach. New York: Guilford; 2010. [Google Scholar]
- Miklowitz DJ, Johnson SL. Social and familial factors in the course of bipolar disorder: Basic processes and relevant interventions. Clinical Psychology: Science and Practice. 2009;16:281–296. doi: 10.1111/j.1468-2850.2009.01166.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A. Findings about partner violence from the Dunedin Multidisciplinary Health and Development Study. Washington, DC: National Institute of Justice; 1999. [Google Scholar]
- Moffitt TE, Caspi A, Krueger RF, Magdol L, Margolin G, Silva PA, Sydney R. Do partners agree about abuse in their relationship? A psychometric evaluation of interpartner agreement. Psychological Assessment. 1997;8:47–56. [Google Scholar]
- Moreno DH, Bio DS, Petresco S, Petresco D, Gutt EK, Soeiro-de-Souza MG, Moreno RA. Burden of maternal bipolar disorder on at-risk offspring: A controlled study on family planning and maternal care. Journal of Affective Disorders. 2012;143:172–178. doi: 10.1016/j.jad.2012.05.050. [DOI] [PubMed] [Google Scholar]
- Muralidharan A, Yoo D, Ritschel LA, Simeonova DI, Craighead WE. Development of emotion regulation in children of bipolar parents: Putative contributions of socioemotional and familial risk factors. Clinical Psychology: Science and Practice. 2010;17:169–186. [Google Scholar]
- Narayan AJ, Allen TA, Cullen K, Klimes-Dougan Disturbances in reality testing in offspring of parents with bipolar disorder: A developmental psychopathology perspective. Bipolar Disorders. 2013;15:723–740. doi: 10.1111/bdi.12115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayan AJ, Englund MM, Carlson EA, Englund B. Adolescent conflict as a developmental process in the prospective pathway from exposure to interparental violence to dating violence. Journal of Abnormal Child Psychology. 2014 doi: 10.1007/s10802-013-9782-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayan AJ, Englund MM, Egeland B. Developmental timing and continuity of exposure to interparental violence and externalizing behavior as prospective predictors of dating violence. Development and Psychopathology. 2013;24:973–990. doi: 10.1017/S095457941300031X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack LE. Self-perceptions of interpersonal and sexual functioning in women with mood disorders: A preliminary report. Issues in Mental Health Nursing. 1993;14:201–218. doi: 10.3109/01612849309031617. [DOI] [PubMed] [Google Scholar]
- Prince SE, Jacobson NS. A review and evaluation of marital and family therapies for affective disorders. Journal of Marital and Family Therapy. 1995;21:377–401. [Google Scholar]
- Radke-Yarrow M, Martinez P, Mayfield A, Ronsaville D. Children of depressed mothers: From early childhood to maturity. Cambridge: Cambridge University Press; 1998. [Google Scholar]
- Reis HT, Collins WA, Berscheid E. The relationship context of human behavior and development. Psychological Bulletin. 2000;126:844–872. doi: 10.1037/0033-2909.126.6.844. [DOI] [PubMed] [Google Scholar]
- Romero S, DeBello MP, Soutullo CA, Stanford K, Strakowski SM. Family environment in families with versus families without parental bipolar disorder: A preliminary comparison study. Bipolar Disorders. 2005;7:617–622. doi: 10.1111/j.1399-5618.2005.00270.x. [DOI] [PubMed] [Google Scholar]
- Rowe LS, Morris AM. Patient and partner correlates of couple relationship functioning in bipolar disorder. Journal of Family Psychology. 2012;26:328–337. doi: 10.1037/a0027589. [DOI] [PubMed] [Google Scholar]
- Selman R. The growth of interpersonal understanding: Developmental and clinical analyses. New York: Academic Press; 1980. [Google Scholar]
- Spitzer RL, Endicott J. The schedule for affective disorders and schizophrenia: Lifetime Version. New York: New York State Psychiatric Institute, Biometrics Research; 1977. [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria. Archives of General Psychiatry. 1978;35:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Sroufe LA, Egeland B, Carlson EA, Collins WA. The development of the person. New York: Guilford; 2005. [Google Scholar]
- Steinberg L, Mounts NS, Lamborn SD, Dornbush SM. Authoritative parenting and adolescent adjustment across varied ecological niches. Journal of Research on Adolescence. 1991;1:19–36. [Google Scholar]
- Straus MA. Measuring intrafamilial conflict and violence: The Conflict Tactics (CT) Scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Straus MA, Gelles RJ, Smith C, editors. Physical violence in American families: Risk factors and adaptations to violence in 8,145 families. New Brunswick, NJ: Transaction Publishers; 1990. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised conflict tactics scales (CTS2) development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Vance YH, Jones SH, Espie J, Bentall R, Tai S. Parental communication style and family relationships in children of bipolar parents. British Journal of Clinical Psychology. 2008;37:355–359. doi: 10.1348/014466508X282824. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Paykel ES, Klerman GL. The depressed woman as a mother. Social Psychiatry. 1972;7:98–108. [Google Scholar]
- Zahn-Waxler, McKnew DH, Cummings EM, Davenport YB, Radke-Yarrow M. Problem behaviors and peer interactions of young children with a manic-depressive parent. American Journal of Psychiatry. 1984;141:236–240. doi: 10.1176/ajp.141.2.236. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Kohn R, Keitner G, Della Grotta SA. The relationship between quality of interpersonal relationships and major depressive disorder: Findings from the National Comorbidity Survey. Journal of Affective Disorders. 2000;59:205–215. doi: 10.1016/s0165-0327(99)00153-6. [DOI] [PubMed] [Google Scholar]