Abstract
The community-based participatory research (CBPR) literature notes that researchers should share study results with communities. In the case of human genetic research, results may be scientifically interesting but lack clinical relevance. The goals of this study were to learn what kinds of information community members want to receive about genetic research and how such information should be conveyed. We conducted 8 focus group discussions with Yup’ik Alaska Native people in southwest Alaska (N=60) and 6 (N=61) with members of a large health maintenance organization in Seattle, Washington. Participants wanted to receive genetic information they “could do something about” and wanted clinically actionable information to be shared with their healthcare providers; they also wanted researchers to share knowledge about other topics of importance to the community. Although Alaska Native participants were generally less familiar with western scientific terms and less interested in web-based information sources, the main findings were the same in Alaska and Seattle: participants wished for ongoing dialogue, including opportunities for informal, small-group conversations and receiving information that had local relevance. Effective community dissemination is more than a matter of presenting study results in lay language. Community members should be involved in both defining culturally appropriate communication strategies and in determining which information should be shared. Reframing dissemination as a two-way dialogue, rather than a one-way broadcast, supports the twin aims of advancing scientific knowledge and achieving community benefit.
Keywords: genetic research, dissemination, communication, qualitative research, Alaska Native
INTRODUCTION
Scientific progress depends, in large part, on the timely communication of research results within the scientific community. Funding agency policies and the culture that grew up around the race to sequence the human genome arguably make rapid dissemination and data sharing a particularly salient feature of modern genetic research [NIH, 2003a; NIH, 2003b; NIH, 2007; Wellcome Trust, 2003]. At the same time, participants and communities have begun to seek a role beyond that of “subject,” [Guston, 2004; Marcus, 2011; Tabor and Lappe, 2011], and a range of approaches to engaging communities in health research have gained currency [Barkin et al., 2013; Hood et al., 2010; Isler and Corbie-Smith, 2012; Israel et al., 1998]. Although much recent work explores the issue of returning individual research results, less is known about how best to share research results with communities [Evans and Rothschild, 2012; Fabsitz et al., 2010; Henderson et al., 2014; Jarvik et al., 2014].
Human genetic research presents special challenges in this regard. The meaning or value of genetic findings – especially those that lack near-term clinical application – can be difficult to explain when non-scientists may be unfamiliar with key concepts [Bates, 2005; Condit, 2010]. Communities may lack linguistic or conceptual equivalents for technical terms such as “penetrance;” and certain words, such as “mutation,” carry negative connotations in everyday language [Condit et al., 2004]. In some cases, genetic research may simply not be a priority for the community [James and Starks, 2011] or may raise concerns over misuse or misappropriation [Foster et al., 1999; Santos, 2008].
This report presents results from the Ethics of Dissemination project, which conducted qualitative research about the return of genetic research results in two very different settings – (1) Yup’ik communities in southwest Alaska served by the Yukon-Kuskokwim Health Corporation (YKHC) and (2) Group Health Cooperative, a large health maintenance organization in Seattle, Washington – to learn about community preferences regarding dissemination. The project is a collaboration among the Center for Alaska Native Health Research at the University of Alaska Fairbanks (CANHR), the Center for Genomics and Healthcare Equality at the University of Washington (CGHE), and the Group Health Research Institute (GHRI).
MATERIALS AND METHODS
Focus Groups
We sought to recruit as broad a cross-section of each community as possible. In the Yukon-Kuskokwim Delta (YK), we recruited through posters, word of mouth, and direct approach. By cultural tradition, Yup’ik young adults are hesitant to speak when elders are present; we therefore convened younger people (age 19–36) in a separate group to promote their full participation. In Seattle, participants were identified through administrative data and stratified by age. The Group Health population is approximately 83% white; to elicit perspectives from a more racially and ethnically diverse range of individuals, we aimed for 50% enrollment of non-white and/or Hispanic participants within each of three age cohorts. Initial approach was via mail, with 3% of those contacted opting into the study. This research was approved by the UAF Institutional Review Board (IRB), the Yukon-Kuskokwim Health Corporation Human Studies Committee, and the GHRI IRB. All participants provided written informed consent, with translation as needed.
Discussions in the YK were facilitated by a team of academic researchers and community co-researchers, with Yup’ik-English interpretation as needed. Seattle discussions were co-facilitated, in English, by two academic researchers. At both sites, facilitators used a written guide to ensure consistency and coverage across groups (Table I). All sessions began with general questions aimed at participants’ views and experiences with research and progressed to more specific queries about communication and genetic research. Site-specific questions were asked in each location as noted.
Table 1.
Main Topics – Facilitator’s Guide
| Topic | Sample Questions | YK | Seattle |
|---|---|---|---|
| General views about research | When you hear the word “research,” what comes to mind? | x | x |
| Research in the community |
|
x | x |
| Desired communication (content) |
|
x | x |
| Desired communication (format) |
|
x | x |
| Language used to describe heredity, genetic concepts |
|
x | |
| Role of patients/members in research governance | Should members be involved in setting research priorities? If so, how? (with prompts and examples) | x |
Focus groups in the YK lasted approximately 90 minutes and were held in locations convenient to participants: a community center, a church, and the schoolteacher’s house, which was unoccupied at the time. YK discussions were audio-recorded and transcribed, with translation as needed. Seattle discussions lasted 2 hours and were transcribed “live” by a court reporter. We provided light refreshments at all sessions. Participants at both sites received $50 in cash at the end of the discussion. Seattle participants also received paid parking.
Community Planning Group and Ciuliat Meetings in the YK
As part of CANHR’s commitment to community-engaged research, a Community Planning Group (CPG) and Ciuliat (Yup’ik for “leaders”) group were formed for this project to assist the research team in planning data collection, performing data analysis, and clarifying the issues involved in returning genetic results to participants or the community. The CPG comprises 10 Yup’ik men and women from eight of the communities in which CANHR conducts genetic research. The Ciuliat is made up of 4 urban-dwelling, university-educated Yup’ik individuals who have pursued business, professional, or academic careers. They serve as bi-cultural liaisons between the academic partners and the CPG.
The Ethics of Dissemination team meets three times per year. Meetings are held in Bethel, the YK regional hub, and typically last 1.5 days. Meetings are audio-recorded and transcribed, with interpretation as needed. CPG and Ciuliat members receive an honorarium of $200 per day for their participation in project activities; the project pays for their travel, lodging expenses, and per diem [Hoeft et al., 2014]. The YKHC Human Studies Committee considers these meetings to be human subjects research. All members of the research team, including the CPG and the Ciuliat provided written informed consent and completed human research training as part of this project. Because the insights of the CPG and Ciuliat are key to understanding what dissemination in the YK should look like, their observations are incorporated here where appropriate.
Analysis
To engage CPG members in the interpretation of YK results, informal analysis began in the field following each focus group. These discussions were then debriefed among the academic researchers via conference call and field notes to determine how best to engage additional CPG and Ciuliat members in analysis. We then performed a qualitative content analysis [Hsieh and Shannon, 2005] to produce a descriptive summary of participants’ preferences regarding dissemination of genomic research results and to assess the degree to which views differed in the two study sites. The lead analyst read the YK and Seattle focus group transcripts several times and developed an initial coding scheme that captured the topics covered in the focus group guides (deductive codes) as well as other emergent themes that arose from the data (inductive codes). [Patton, 2002]Transcripts were uploaded into ATLAS.ti, a software application, for analysis. The lead analyst coded all the focus group transcripts, with a subset of the transcripts independently coded by two additional academic researchers. The codebook was revised as needed based on group discussion and reconciliation of coding disagreements. A fourth academic researcher coded the transcripts from team meetings in the YK, with review by 2 other members of the analytic team. Results were discussed and further interpreted at several CPG meetings.
RESULTS
We conducted 8 focus groups in two different YK communities, designated as Communities A and B to protect their privacy. We conducted 4 sessions (N = 35) in Community A in October 2011 and 4 sessions (N = 25) in Community B in January 2012 (Table II).
Table 2.
Yukon-Kuskokwim Focus Groups – Participant Characteristics
| Male | Female | Total | Age range | |
|---|---|---|---|---|
| Group A1 | 6 | 3 | 9 | 21 – 58 |
| Group A2 | 0 | 2 | 2 | 36 – 51 |
| Group A3 | 6 | 2 | 8 | 20 – 59 |
| Group A4 | 3 | 13 | 16 | 19 – 70 |
| Group B1 | 4 | 4 | 8 | 23 – 77 |
| Group B2 | 4 | 5 | 9 | 31 – 71 |
| Group B3 | 0 | 2 | 2 | 42 – 68 |
| Group B4 | 1 | 5 | 6 | 19 – 36 |
| TOTALS | 24 | 36 | 60 | – |
At Group Health, we held six focus groups (N = 61) between February and April 2012 at 2 different corporate locations (Table III).
Table 3.
Seattle Focus Groups – Participant Characteristics
| Age Distribution by Group | ||||
|---|---|---|---|---|
| Male | Female | Age range | Total | |
| Group 1A | 7 | 2 | 18 – 34 | 9 |
| Group 1B | 3 | 5 | 18 – 34 | 8 |
| Group 2A | 3 | 9 | 35 – 49 | 12 |
| Group 2B | 6 | 4 | 35 – 49 | 10 |
| Group 3A | 5 | 7 | 50+ | 12 |
| Group 3B | 6 | 4 | 50+ | 10 |
| Race and Ethnicity | ||||
|---|---|---|---|---|
| Male | Female | Unknown/not reported | Total | |
| Hispanic or Latino | 2 | 1 | 0 | 3 |
| Not Hispanic or Latino | 15 | 41 | 0 | 56 |
| Unknown | 0 | 0 | 0 | 0 |
| TOTAL | 17 | 42 | 0 | 59 |
| American Indian/Alaska Native | 1 | 2 | 0 | 3 |
| Asian | 4 | 16 | 0 | 20 |
| Native Hawaiian or Other Pacific Islander | 0 | 1 | 0 | 1 |
| Black or African American | 3 | 6 | 0 | 9 |
| White | 9 | 17 | 0 | 26 |
| More than one race | 0 | 0 | 0 | 0 |
| Unknown/not reported | 0 | 0 | 0 | 0 |
| TOTALS | 17 | 42 | 0 | 59 |
Interest in genetic information varies
We identified some differences between YK and Group Health in terms of participants’ familiarity with, and interest in, genetic information. YK participants were less conversant with scientific concepts around genetics, but most indicated interest in learning more, especially if information is provided over time and in an accessible manner. As one elder CPG member stated,
“You can’t learn about something right away. I am like someone who is sleeping towards this subject, because I’m hearing about these [things] for the first time …. Maybe in the future when we hear about them a lot more, I think we will began to understand them. I think I could possibly begin to understand them. We can’t learn about something as soon as we hear about them.”
YK participants sought to draw connections between genetic studies and other kinds of research that were more familiar. For example, kinship and relatedness are important in Yup’ik culture, and some participants described their own investigations to learn who their relatives are and where they live. Inquiries into who one’s relatives are were seen as a particular point of connection to genetic research, as in this comment from a CPG member:
“I was thinking about how my grandma used to explain to us of, you know, those people that she knew, and how we’re related. And she used to say that, you know, like this, [Yup’ik: another], the term [Yup’ik: “This world is not occupied by other people,”] and what she meant about that was that … if you look at the microscopic, you know, whatever we see on genetics of how, you know, those work, it, it kind of when you put it visually that’s how it looks, it’s like everybody is connected. So that’s why the term they say, [Yup’ik: “There are no other people living here”].“
Despite recent, highly publicized negative experiences of indigenous communities with genetic research [Couzin-Frankel, 2010; Harmon, 2010; Wiwchar, 2004], YK participants were receptive to genetic research and expressed greater sensitivity concerning other kinds of studies, such as research involving subsistence resources (e.g., related to fisheries and fishing restrictions).
In Seattle, some participants viewed genetics as an especially “cutting edge” area of research. Others noted that past abuses have given rise to misgivings about genetic research, particularly in minority communities, while also noting that not conducting research in these communities could exacerbate health disparities. One participant said,
“[M]y mother had went in to get the testing just to see if there was a genetic link in regard to why our family is continuing to get hit by this, by breast cancer and blah, blah, blah. And in the process of it, she had to keep going in for the testing, because I guess in the BRCA1 [gene] there was a definite [finding], but the BRCA2 was continually inconclusive, because I think she was only one of 17 African Americans to ever do it. So there’s this tiny little population. So what are we comparing it to?”
Most wanted: information “you can do something about”
At both sites, focus group participants expressed strong interest in information they or their healthcare providers could use to improve health. For example, one YK participant talked about wanting to learn more about how genetics might relate to her family’s hypertension: “All my grandpas and aunts and uncles have high blood pressure, and now my cousins have it, too, and I’m aware that maybe I have it too.” A participant in one of the Group Health sessions said, “Any research on preventive medicine, if I can participate or if there’s lectures or anything about the findings, then it intrigues me just to know about it so I can be aware and take care to prevent it.”
Participants wanted researchers to explain the relevance of research results to health and daily living. In the YK, a participant commented,
We get more information from the researchers on what we really didn’t know, or would like to have known. We learn more, get more input. So we get to look into what we’re actually, I mean, actually happen[s] with our body. Sometimes we learn that we can’t eat too much sugar or stuff like that, or like a diabetic. We want to learn more about what our habits are on eating or doing physical activities.
Similarly, a Group Health participant remarked,
“[S]o what? So there’s a gene. What if this gene is related? What does that mean? And what does that mean about my own knowledge of what I can do to my diet, or what I should have in my diet, or what I shouldn’t, or something else I can do that makes it so I can eat whatever I want? What does it mean for me, or what are the possibilities?”
Strong interest in community-specific research findings
Focus group participants in both sites said that they would want research results that could help to explain health phenomena specific to their communities. YK participants referred to the positive health effects of a traditional Yup’ik lifestyle, particularly subsistence activities of hunting, fishing, and gathering, and a traditional diet. In focus groups and in meetings with the CPG and Ciuliat, we have learned that many Yup’ik people wonder about the effects of kass’aq (white/non-Yup’ik) lifestyles (involving cash jobs, market foods high in saturated fats, sugar, and preservatives, and less emphasis on traditional subsistence foods and activities) on the health of the younger generation, and therefore would value research to better understand this issue. An elder CPG member explained it this way:
“Yup’ik: Our ancestors lived their lives using themselves as tools, using their bodies as weapons, as strength, to do things with. And they ate their food without adding something to it, and they ate the same food all year long. The only kass’aq food they had were coffee and tea. That is why our ancestors had very strong bodies, because they didn’t mix things into their lives. Nowadays our children do not exactly understand the way we used to live, and we cannot live the way they used to live. If we try to live as they used to live we would find it hard. I’ve been thinking about that since yesterday, thinking if CANHR continues to go forward and if they find out about it and learn it, if they don’t dissolve, if their work doesn’t dissolve, if it continues to moves forward, the way I envision it, it could possibly help those in the future after we are gone. That is what I think may happen.”
Seattle participants noted different health concerns, but they too were interested in research on issues that seem to affect the local community in particular ways. One participant remarked,
“You know, we have some issues around autism and multiple sclerosis in this area. And vitamin D issues. It would be very useful to this community, this [regional] area, even outside of Group Health, to be researching and looking into what is going on. Why do we have such high rates of multiple sclerosis here?”
Limited interest in research “progress reports”
We asked whether community members would like status updates about genetic research that has not yet produced clinically relevant results. Participants’ responses were mixed, at both sites: some wanted to know about research in their community, while others wished to hear only about results they could use to manage their health. At Group Health, one participant told us, “The kind of reporting to the participants that I think is extremely valuable is, ‘This is working, and this is the direction we see it trending,’ or ‘It’s too early to tell.’ But just to say, ‘Oh, we are still doing it’ isn’t a whole lot of help.”
In the YK, many participants told us that research as it is undertaken in NIH-funded research or western schooling is simply not part of their usual experience. As one YK participant said, “When I hear [the word ‘research’] or read about research, I only think of science, you know, and that’s what they do in school, like doing a research paper or research whatever. They assign [it to] you. Yeah. It’s hardly an everyday conversation topic.”
Participants in the Seattle focus groups were more familiar with the scientific method and health research. Some said that they valued Group Health’s engagement in research and appreciated updates; they perceived research as a sign of Group Health’s commitment to innovation and quality improvement: “I like to think where I’m getting medical care, that it’s progressive, it’s continually learning and growing and seeing what is out there.”
Face-to-face dialogue is ideal
Focus group participants in both sites valued opportunities for informal, face-to-face communication between community members and researchers. One suggestion we heard in both locations was that we “should have more group meetings like these” (i.e., the focus groups). Participants articulated a preference for an exchange of information between researchers and community members, rather than a one-way presentation at the end of the study. For example, in one of the Seattle groups, a participant said:
“So it’s not just somebody standing there and saying, “This is it. This is what happened. This is what it’s going to do to you. You’re all just going to die.” But it’s an opportunity for people to be able to say [to researchers], “This is the thing, and this happened to my family, and this is what’s going on.” And have those interactions where it’s comfortable, it’s in a place where people are familiar, it’s cozy.”
Four of the YK focus groups were held in the living room of a teacher’s house; community members and members of the research team sat informally in a circle. This was considered more conducive to communication and understanding, especially when compared to the standard setup – “more comfortable, homey” in the words of one participant.
CANHR holds community meetings to share information about research findings and progress, but attendance has been a challenge. Participants recommended that, instead of or in addition to holding a single community meeting, CANHR host several small-group discussions, using the format they were experiencing as focus group participants. CPG members suggested that combining such meetings with other social events in the community – such as bingo, movie night, or a potluck – or scheduling them to coincide with other community events could increase attendance. At Group Health, information about ongoing research is provided via a magazine for health plan enrollees, website links, and study-specific newsletters for research participants. Here too, participants suggested more active face-to-face outreach, such as working through local schools or churches, holding a monthly “tea time,” or hosting an informal “researcher Q&A” in a community venue.
Young people are an important audience
Participants in both sites noted that young people are an important audience, both for their own education and because they can explain research to their parents and elders. Participants felt that youth have likely had more formal science education than older people and are thus more familiar with relevant concepts and terminology; that their knowledge is more up to date; and that the knowledge is fresh in their minds. In the YK, some participants felt that young people may be more interested in scientific details than elders:
“And then how much information [to share] depends on two different groups again, you know. The elders will not want to know the details of the research. Younger generation already been through education, they, and then even high school, too, more details, I mean, I think cause you’re letting them know how research is done, how, why, you know cause they’re in a different, different um mind set than [the older] generation, you know?”
Seattle participants noted that sharing information with young people is especially important when language or cultural barriers may be in play: “[I]f the children are empowered, then people who have little English or no English, there’s ways that the children can empower their parents to go and get that information because of, the teacher told them to.”
In the YK, the discussion of youth brought up a number of issues that were not part of the Seattle discussions. One was a difference in vocabulary: many of the Yup’ik words that elders said they would use to describe genetics had to do with relatedness and how learning is passed down from generation to generation. Younger focus group participants (19–36 years) said they would not choose those words, though they did not disagree with the elders’ usage. One participant said, “I recognize [that word], but I don’t use it,” and another quipped, “Maybe when we grow old, we’ll start using those words.”
As small Yup’ik communities become more “westernized,” elders worry that young people may be losing touch with important traditional knowledge. Some participants and CPG members believed that these changes are having negative health effects on the younger generation. At the same time, they expressed hope that empowering youth to act as research educators could spark an exchange of scientific and traditional knowledge between youth and elders and support intergenerational learning more generally.
Researchers should communicate with affiliated healthcare providers
Unprompted by our questions, focus group participants said it was important for community-based researchers to communicate with local clinicians. Participants at both sites wanted their healthcare providers to be made aware of specific research going on in the community and to facilitate patients’ inclusion in appropriate studies. Delivering research findings to providers was viewed as essential, particularly if results could have implications for patient care.
This view was echoed by the CPG, with an additional suggestion that it is important for providers – many of whom come from the Lower 48 States – to learn how to take care of Yup’ik people, specifically. As one Ciuliat member put it, “I think there’s always some sort of distrust with doctors anyway by the people, they’re like, ‘Does this person know?’ I mean (pause), yeah, we want them to know our area and what it entails, the doctors that come in, ‘cause they’ve, they’re serving the population here.”
In Seattle, participants wanted providers to bring needs or trends reported by patients or observed in the clinic to the attention of GHRI researchers for follow up. For example, one Group Health focus group participant said,
“[I]t seems to me like, really the patients do direct the research. Right? Because you come to your doctor and you have XYZ that you are concerned about. And hopefully he or she has some sort of way to direct you to address that issue. And if not, there’s a seed that’s planted on what then needs to be investigated. We have practitioners that are gathering information from our patients, and can communicate to [GHRI], “This is what we’re really concerned about right now.”
Manner of communication
Participants at both sites expressed similar preferences about how researchers should express themselves to non-scientific audiences. “Use layman’s language” was a frequent recommendation. In the YK, we were reminded of the importance of using terms and framing that make sense in the local cultural context. For example, the CPG told us that recommendations about “exercise” make little sense in a remote community where there is no health club; but “keeping busy” or “moving around” – which could include doing household chores, walking, or engaging in subsistence activities – is understood immediately.
Focus group participants in both sites, as well as CPG members, endorsed the use of visual illustrations; YK participants suggested incorporating culturally meaningful elements or activities, such as objects associated with traditional dancing (yuraq) and subsistence hunting, fishing, and berry-picking. In research team meetings, we have learned the value of identifying culturally relevant analogies to help explain scientific concepts – for example, considering genetics in the context of breeding sled dogs and wolves; drawing a parallel between titrating a medication and assessing when enough berries have been added to akutaq, a traditional food. The CPG and Ciuliat noted that oral and visual forms of communication are more easily understood than written materials, particularly among elders; and hands-on models (e.g., a plastic cutaway model of a blood vessel) were seen as useful. Storytelling was also noted as an important means of conveying and contextualizing information.
Because many genetic research results are preliminary or not yet ready for clinical application, a Seattle participant suggested a novel solution for conveying the degree of certainty researchers have about a given result: “[c]olor coding of finished findings versus work in progress and hypotheses, so it’s really obvious to people – even if they’re skimming – that ‘This [finding] is pretty close to true’ and ‘This is, we’re just wondering still.’”
Modes of communication
Main findings are presented in Figure 1. Participants in Seattle and in the YK considered newsletters, posters, and pamphlets useful. In both sites, participants recommended making information available online through web-based reference resources and said that secure e-mail or social media (e.g., Facebook, Twitter) could be an effective means of conveying targeted information. YK participants, as well as CPG and Ciuliat members, strongly endorsed the use of videos, photovoice, and digital storytelling featuring Yup’ik people speaking their heritage language. YK participants and CPG members recommended the use of newspaper articles, radio broadcasts, and VHF radio announcements in addition to the approaches noted above. A few people in the YK suggested text messages as an effective way of communicating, particularly with youth.
FIGURE 1.
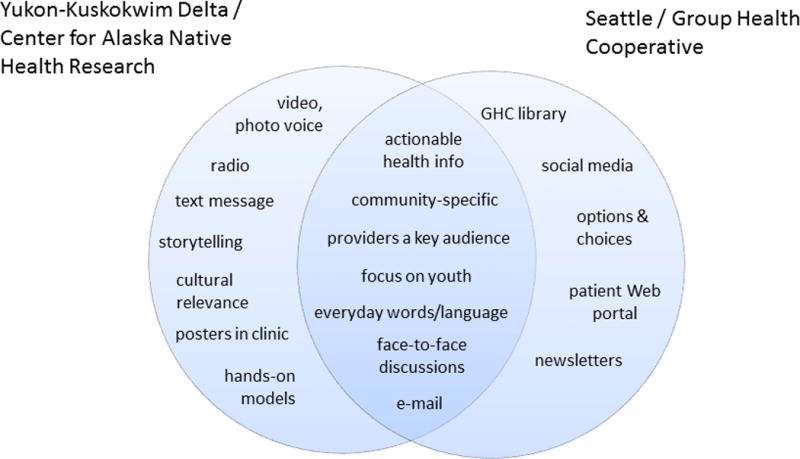
Seattle participants expressed a strong desire for “options and choices” in the way research information would be provided to them. They wanted to select topics of interest; set parameters for contact frequency; and choose modes of communications (e.g., post vs. e-mail). In the YK, by contrast, there was greater emphasis on deploying a wide range of different communication tools to reach different members of the community.
DISCUSSION
This study explored the preferences of individuals living in remote Yup’ik communities in southwest Alaska and in metropolitan Seattle for receiving information about genetic research studies conducted in their healthcare system or community. Despite significant cultural, geographical, and socioeconomic differences between the study sites, there were many points of agreement. Consistent with other studies [Rivkin et al., 2013; Yu et al., 2013a; Yu et al., 2013b], participants at both sites were most interested in information that could help them stay healthy and that was directly relevant to their health concerns and those of their family and/or community; there was less interest in results that do not yet have health or clinical applications.
Participants and community members in Seattle and the YK recommended many of the same communication tools and methods. Web-enabled tools were more strongly endorsed in Seattle than in the YK (perhaps as a consequence of differential access to Internet technology), and some communication channels (such as VHF radio) were mentioned only in the YK. But in both places, participants stressed the need to adapt communication strategies to the local context. As “team science” gains currency in academia [Disis and Slattery, 2010], genetic research can benefit from the inclusion of communication scholars and, in the case of research with culturally distinct populations, locally based bi-cultural liaisons [Allen et al., 2006; Burhansstipanov et al., 2005; Wong-Parodi and Strauss, 2014].
Participants at both sites voiced a strong preference for ongoing, face-to-face dialogue with researchers. This is a strong contrast with the conventional model of community dissemination, which typically involves a one-time, one-way broadcast of results via newsletters, websites, or community presentations. Repeatedly, participants stated that “meetings like this” (i.e., following the focus group format) would be the optimal way to share information with communities. Features that may contribute to this preference include the informal, conversational nature of discussion; the opportunity for participants to ask questions and hear others’ views; and the role of the researcher as a friendly, interested interlocutor, rather than an expert presenter. Participants recommended convening small-group discussions in familiar, comfortable settings, such as community centers and schools. At both sites, participants appreciated researchers’ sharing their expertise, including information not directly related to the study topic. Researchers’ “giving back” in this way may be especially valuable in the context of studies whose clinical usefulness is limited or longer term, and there is growing interest in effective communication as an ethical responsibility of community-based researchers [Chen et al., 2010].
As has been amply demonstrated in the clinical setting, transforming one-way communication into a two-way dialogue is a substantial undertaking; relevant lessons may be drawn from the existing literature around patient-centered communication [Elwyn et al., 2014; Phillips et al., 2014] and shared decision making [Grande et al., 2014; Politi et al., 2013; Zeuner et al., 2014]. The additional time and cost involved in such outreach may be considerable, particularly if travel to remote locations is necessary; but the potential for building trust and shared knowledge with communities in support of research suggests that these investments are worthwhile, particularly in the context of long-term partnerships [Hoeft et al., 2014].
CONCLUSION
The approach to dissemination recommended by the participants in this study implies not only a change in tactics, but also a reframing of the goals of community dissemination. Rather than a transfer of specialized knowledge from experts to non-scientists, the dialogic approach recognizes expertise on both sides of the communication, envisions an opportunity for both parties to learn from each other, and posits that information shared between partners can change the direction of the conversation. While such an approach is novel in terms of community dissemination, it is nevertheless a familiar model to scientific researchers: peer-reviewed publications and conferences support precisely this kind of interaction within the scientific community. The potential good of research is increased when the resources and knowledge of all partners are directed toward scientific advancement and community benefit.
Acknowledgments
The authors wish to thank the individuals who participated in these focus groups. We are deeply grateful to the members of the Community Planning Group and the Ciuliat for their help in this and other projects. We thank Communities A and B for hosting the focus groups in the YK Delta. Thanks also to Joseph Klejka, MD, and the Yukon-Kuskokwim Health Corporation for their support of this research; and to Phyllis Morrow, PhD, for her helpful review of this manuscript. Funding for this project was provided by the National Human Genome Research Institute under grant award 5R01HG005221 and by the National Institute of General Medical Sciences under grant award U01GM092676.
References
- Allen J, Mohatt GV, Rasmus SM, Hazel KL, Thomas L, Lindley S. The tools to understand: community as co-researcher on culture-specific protective factors for Alaska Natives. J Prev Interv Community. 2006;32:41–59. doi: 10.1300/J005v32n01_04. [DOI] [PubMed] [Google Scholar]
- Barkin S, Schlundt D, Smith P. Community-engaged research perspectives: then and now. Acad Pediatr. 2013;13:93–97. doi: 10.1016/j.acap.2012.12.006. [DOI] [PubMed] [Google Scholar]
- Bates BR. Public culture and public understanding of genetics: a focus group study. Public Underst Sci. 2005;14:47–65. doi: 10.1177/0963662505048409. [DOI] [PubMed] [Google Scholar]
- Burhansstipanov L, Christopher S, Schumacher SA. Lessons learned from community-based participatory research in Indian country. Cancer Control. 2005;12(Suppl 2):70–76. doi: 10.1177/1073274805012004s10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen PG, Diaz N, Lucas G, Rosenthal MS. Dissemination of Results in Community-Based Participatory Research. Am J Prev Med. 2010;39:372–378. doi: 10.1016/j.amepre.2010.05.021. [DOI] [PubMed] [Google Scholar]
- Condit CM. Public understandings of genetics and health. Clin Genet. 2010;77:1–9. doi: 10.1111/j.1399-0004.2009.01316.x. [DOI] [PubMed] [Google Scholar]
- Condit CM, Dubriwny T, Lynch J, Parrott R. Lay people’s understanding of and preference against the word “mutation”. Am J Med Genet A. 2004;130A:245–250. doi: 10.1002/ajmg.a.30264. [DOI] [PubMed] [Google Scholar]
- Couzin-Frankel J. Ethics. Researchers to return blood samples to the Yanomamo. Science. 2010;328:1218. doi: 10.1126/science.328.5983.1218. [DOI] [PubMed] [Google Scholar]
- Disis ML, Slattery JT. The road we must take: multidisciplinary team science. Sci Transl Med. 2010;2:22cm29. doi: 10.1126/scitranslmed.3000421. [DOI] [PubMed] [Google Scholar]
- Elwyn G, Dehlendorf C, Epstein RM, Marrin K, White J, Frosch DL. Shared decision making and motivational interviewing: achieving patient-centered care across the spectrum of health care problems. Ann Fam Med. 2014;12:270–275. doi: 10.1370/afm.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans JP, Rothschild BB. Return of results: not that complicated? Genet Med. 2012;14:358–360. doi: 10.1038/gim.2012.8. [DOI] [PubMed] [Google Scholar]
- Fabsitz RR, McGuire A, Sharp RR, Puggal M, Beskow LM, Biesecker LG, Bookman E, Burke W, Burchard EG, Church G, Clayton EW, Eckfeldt JH, Fernandez CV, Fisher R, Fullerton SM, Gabriel S, Gachupin F, James C, Jarvik GP, Kittles R, Leib JR, O’Donnell C, O’Rourke PP, Rodriguez LL, Schully SD, Shuldiner AR, Sze RK, Thakuria JV, Wolf SM, Burke GL. Ethical and practical guidelines for reporting genetic research results to study participants: updated guidelines from a National Heart, Lung, and Blood Institute working group. Circ Cardiovasc Genet. 2010;3:574–580. doi: 10.1161/CIRCGENETICS.110.958827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster MW, Sharp RR, Freeman WL, Chino M, Bernsten D, Carter TH. The role of community review in evaluating the risks of human genetic variation research. Am J Hum Genet. 1999;64:1719–1727. doi: 10.1086/302415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grande SW, Durand MA, Fisher ES, Elwyn G. Physicians as part of the solution? Community-based participatory research as a way to get shared decision making into practice. J Gen Intern Med. 2014;29:219–222. doi: 10.1007/s11606-013-2602-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guston DH. Forget politicizing science. Let’s democratize science! Issues Sci Technol. 2004;21:25–28. [Google Scholar]
- Harmon A. New York Times. New York: 2010. Indian tribe wins fight to limit research of its DNA. [Google Scholar]
- Henderson GE, Wolf SM, Kuczynski KJ, Joffe S, Sharp RR, Parsons DW, Knoppers BM, Yu JH, Appelbaum PS. The challenge of informed consent and return of results in translational genomics: empirical analysis and recommendations. J Law Med Ethics. 2014;42:344–355. doi: 10.1111/jlme.12151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeft TJ, Burke W, Hopkins SE, Charles W, Trinidad SB, James RD, Boyer BB. Building partnerships in community-based participatory research: budgetary and other cost considerations. Health Promot Pract. 2014;15:263–270. doi: 10.1177/1524839913485962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood NE, Brewer T, Jackson R, Wewers ME. Survey of community engagement in NIH-funded research. Clin Transl Sci. 2010;3:19–22. doi: 10.1111/j.1752-8062.2010.00179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Isler MR, Corbie-Smith G. Practical steps to community engaged research: from inputs to outcomes. J Law Med Ethics. 2012;40:904–914. doi: 10.1111/j.1748-720X.2012.00719.x. [DOI] [PubMed] [Google Scholar]
- Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- James R, Starks H. Bringing the “Best Science” to Bear on Youth Suicide: Why Community Perspectives Matter. In: Burke W, Edwards K, Goering S, Holland S, Trinidad SB, editors. Achieving Justice in Genomic Translation: Rethinking the Pathway to Benefit. New York: Oxford University Press; 2011. pp. 180–196. [Google Scholar]
- Jarvik GP, Amendola LM, Berg JS, Brothers K, Clayton EW, Chung W, Evans BJ, Evans JP, Fullerton SM, Gallego CJ, Garrison NA, Gray SW, Holm IA, Kullo IJ, Lehmann LS, McCarty C, Prows CA, Rehm HL, Sharp RR, Salama J, Sanderson S, Van Driest SL, Williams MS, Wolf SM, Wolf WA, Burke W. Return of genomic results to research participants: the floor, the ceiling, and the choices in between. Am J Hum Genet. 2014;94:818–826. doi: 10.1016/j.ajhg.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus AD. Wall Street Journal. New York: 2011. Citizen Scientists. [Google Scholar]
- NIH. Final NIH Statement on Sharing Research Data 2003a [Google Scholar]
- NIH. Reaffirmation and Extension of NHGRI Rapid Data Release Policies: Large-scale Sequencing and Other Community Resource Projects 2003b [Google Scholar]
- NIH. Policy for Sharing of Data Obtained in NIH-Supported or Conducted Genome-wide Association Studies (GWAS) 2007 [Google Scholar]
- Patton MQ. Qualitative Research & Evaluation Methods. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Phillips RL, Short A, Kenning A, Dugdale P, Nugus P, McGowan R, Greenfield D. Achieving patient-centred care: the potential and challenge of the patient-as-professional role Health Expect. 2014 doi: 10.1111/hex.12234. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Politi MC, Wolin KY, Legare F. Implementing clinical practice guidelines about health promotion and disease prevention through shared decision making. J Gen Intern Med. 2013;28:838–844. doi: 10.1007/s11606-012-2321-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivkin I, Trimble J, Lopez ED, Johnson S, Orr E, Allen J. Disseminating research in rural Yup’ik communities: challenges and ethical considerations in moving from discovery to intervention development. Int J Circumpolar Health. 2013;72 doi: 10.3402/ijch.v72i0.20958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos L. Genetic research in native communities. Prog Community Health Partnersh. 2008;2:321–327. doi: 10.1353/cpr.0.0046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabor HK, Lappe MD. The Autism Genetic Resource Exahange: Changing Pace, Priorities, and Roles in Discovery Science. In: Burke W, Edwards K, Goering S, Holland S, Trinidad SB, editors. Achieving Justice in Genomic Translation: Rethinking the Pathway to Benefit. New York: Oxford University Press; 2011. pp. 56–71. [Google Scholar]
- Wellcome Trust. Sharing Data from Large-scale Biological Research Projects: A System of Tripartite Responsibility. London: 2003. [Google Scholar]
- Wiwchar D. Nuu-chah-nulth blood returns to west coast. 5 Ha-Shilth-Sa: 2004. [Google Scholar]
- Wong-Parodi G, Strauss BH. Team science for science communication. Proc Natl Acad Sci U S A. 2014;111(Suppl 4):13658–13663. doi: 10.1073/pnas.1320021111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu JH, Crouch J, Jamal SM, Tabor HK, Bamshad MJ. Attitudes of African Americans toward return of results from exome and whole genome sequencing. Am J Med Genet A. 2013a;161A:1064–1072. doi: 10.1002/ajmg.a.35914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu JH, Jamal SM, Tabor HK, Bamshad MJ. Self-guided management of exome and whole-genome sequencing results: changing the results return model. Genet Med. 2013b;15:684–690. doi: 10.1038/gim.2013.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeuner R, Frosch DL, Kuzemchak MD, Politi MC. Physicians’ perceptions of shared decision-making behaviours: a qualitative study demonstrating the continued chasm between aspirations and clinical practice Health Expect. 2014 doi: 10.1111/hex.12216. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]


