Abstract
Myiasis is the invasion of vertebrates' tissue by the larvae of a fly of the order Diptera. The objective of this paper is to present a rare case of secondary myiasis of ocular infestation by Chrysomya bezziana. A 55-year-old female from Sar village of Mazandaran Province, northern Iran), referred to Khatam Al-Anbia Hospital of Mashhad with extensive destruction of left orbital cavity. Existence of larvae was the major complaint in recent months. Some live larvae were removed from her destructed left eye. Primary diagnosis was myiasis of left upper lid (LUL) and suspected recurrent Basal cell carcinoma (BCC). The laboratory diagnosis was done in parasitology lab of Imam Reza Hospital of Mashhad and collected larvae were identified and confirmed to be larvae of the C. bezziana (Diptera: Calliphoridae). It is a case report of secondary ophtalmiomyiasis due to C. bezziana of a patient lives in Mazandaran Province.
Keywords: Myiasis, ophthalmomyiasis, Chrysomya bezziana
Introduction
Myiasis is the invasion of vertebrates' tissue by the larvae of a fly of the order Diptera. “Myiasis is broadly divided into obligatory, facultative and accidental myiasis depending on the biology of the fly species causing the myiasis and its likely effect” (Janovy et al. 1996, Chan et al. 2005). The condition is further categorized on the tissues that are involved. There are two types of myiasis: Primary myiasis is caused by the biontophage larvae caused primary myiasis that feed on living tissue and secondary form is caused by necrobiontophage fly larvae that feed on necrotic tissue (Raposo et al. 2012). There are more than 160000 Diptera species. However few species cause ocular injuries (Borror et al. 1989). The larvae of certain flies can invade to orbital tissue [myiasis-orbital], external ocular structures [ophthalmomyiasis externa], internal ocular structures [ophthalmomyiasis interna], and the skin of the eyelid [myiasis-dermal]. Causes of myiasis of the eyelid include Cuterebra and Dermatobia hominis (Klintworth 2012).
The C. bezziana female lays approximately 150–200 eggs at a time in wounds and mucous membranes of a live mammal and will hatch after 24 hours. The larvae invade to the tissues of the host by sharp mouth-hooks and anchoring intersegmental spines (Klintworth 2012). The first stage of larva is similar to a worm with a white color and 1.5 mm length. The measures of second and third stages larvae are 4 to 9 and 18 mm, respectively. The worm like larva is formed from eleven segmented with the anterior spiracle on the second and posterior spiracle located on the last segment. There are also compact spurs surrounding each segment of the body (Walker 1994). After being embedded in living tissue for 3–4 days the third instar larvae wriggle out of the tissues in search of a suitable substrate for pupation. However, some mature larvae die in the infested tissue. While feeding, only the posterior spiracle are visible (Cook and Zumla 2009). Larvae can invade the conjunctiva and ocular bulb, provoking conjunctivitis, corneal ulcer and destruction of the ocular bulb, eyelids and orbit, since it feeds on the surrounding tissues (Tsuda et al. 2007). The pupal stage is temperature dependent with warm weather favoring growth. Depending on the temperature, the pupal stage can last anywhere from 1 week to 2 months. The males become sexually mature after 24 hours of leaving their puparium (the hardened shell the pupae mature in), while females take about 6–7 days to become fully sexually mature. If the weather is tropical (29 °C or 84.2 °F), the entire life cycle will last about 24 days, however, at cooler temperatures (below 22 °C or 71.6 °F), the life cycle can take 2–3 months to complete (Oie committee 2008).
Case description
A fifty five-year-old female from Sar village of Mazandaran Province, northern Iran, referred to Khatam Al-Anbia Hospital with extensive destruction of left orbital cavity. She had eye pains for 4 years and the chief complaint was existence of larvae lasting months. The patient had been visited by ophthalmologist and many larvae were seen in her destructed left eye (Fig. 1). Primary diagnosis was myiasis of left upper lid (LUL) and suspected recurrent BCC (Basal cell carcinoma). The ophthalmologist referred her to the laboratory of parasitology of Imam Reza Hospital of Mashhad. Some live larvae were removed by parasitologist (Fig. 2). The collected larvae were evaluated and confirmed to be larvae of the C. bezziana by diagnosis of one pair of anterior spiracle larvae and with 4 to 6 lobes at the ends, located on the first segment, and one pair of posterior spiracles at the bottom of the third instar of the larvae (Fig. 3). The maggots placed on a dish of raw meat in a glass jar containing moist sand. The jar closed with cotton and incubated at room temperature. The maggots burrowed into the meat and stayed for some time. At last they leave meat to enter the sand in order to pupate. Then the jar examined periodically for the emergent flies (Fig. 4).
Fig. 1.

The patient with extensive destruction of left orbital cavity
Fig. 2.

Maggots of Chrysomya bezziana removed from the patient's eye
Fig. 3.

Larval spiracles of Chrysomya bezziana
Fig. 4.
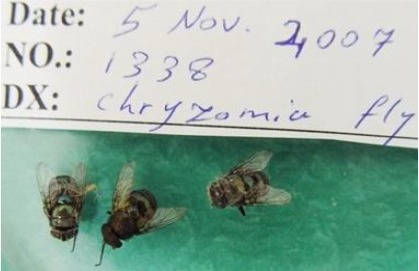
Emergent flies from pupae
Tissues from LUL and medial canthus and remaining of larvae were removed by surgery. The eye was patched. After pathological studies, revealed Basal cell carcinoma and this disease could provide an appropriate condition for larvae growth of C. bezziana and caused a secondary ophthalmomyiasis.
Discussion
Ophthalmomyias is accounts for <5% of human myiasis (Wilhelmus 1986) but the status of this disease is not clear in Iran. Immigration and traveling are two important reasons for increasing the imported cases (Langan et al. 2004). Some studies have been done on ophthalmomiyasis in our country that most known cases were caused by O. ovis and one by flesh fly (Janbakhsh et al. 1977, Razmjou et al. 2007, Yaghoubi and Heydari 2013). Dermatobia hominis and O. ovis (sheep botfly) which are endemic to tropical or subtropical areas are two major causes of ophthalmomyiasis in the world (Lagacé-Wiens et al. 2008). The first reported case of ophthalmomyiasis by O. ovis has been reported in 1977 (Janbakhsh et al. 1997).
Many parts of Iran are located in subtropical area and people are in contact with sheep, goats and many other domestic animals in rural regions. According to this information, the number of infected cases are probably more than reported (Lagacé-Wiens et al. 2008).
External ophthalmomyiasis is the most common form of ocular myasis which symptoms are like conjunctivitis (Khataminia et al. 2011). In one study on 8 farmers with external ophthalmomyiasis in Fars Province of Iran, all the larvae from the bulbar conjunctiva were removed and the symptoms resolved as soon as removal action. The number of larvae obtained from each person were about 1 to 5 and all of them were identified as O. ovis (Diptera: Oestridae) larvae (Masoodi et al. 2004).
Ophthalmomyiasis interna occurs when larvae penetrate into the eye ( Ramonas et al. 2006). Two cases of ophthalmomyiasis interna have been reported form Iran in a 70 years old woman with bilateral subretinal migration of larvae and 12 years old boy with migration of blowfly larvae (Diptera: Calliphoridae) form anterior chamber to posterior chamber after 3 days (Farahvash et al. 1998, Sharifipour et al. 2008).
This study described a case of secondry ophthalmomyiasis caused by C. bezziana. Chrysomya bezziana belongs to Calliphoridae family and suborder Brachycera (suborder Cyclorrhapha), also named as screw worm of the old world (Chemonges-Nielsen 2008). Human infestation is uncommon, but may occur with outbreaks in dogs, pigs and cattle in rural areas (Goddard 2003). Human myiasis infestation by C. bezziana has been reported from south Asia, Africa, Saudi Arabia, Indonesia Islands, Phillipines, Guinea and Persian Gulf of Iran and is well documented in India (Lane and Crosskey 1993).
Ophthalmomyiasis caused by C. bezziana is particularly damaging. There are two reported cases for orbit myiasis caused by C. bezziana in Iran. The first has described in Sina Hospital in a 90-year-old woman from Andimeshk with ocular rupturing and outpouring of hundreds of C. bezziana larvae and the second was in Imam Khomeini Hospital in Ahvaz. The patient was an 87-year-old woman with a severely necrotized left orbit and several live larvae of C. bezziana (Radmanesh et al. 2000, Khataminia et al. 2011).
A pre-existing ocular lesion such as gonococcal conjunctivitis [gonorrhea] and periocular neoplastic ulcers, endophthalmitis may predispose to ophthalmomyiasis by attracting flies. In neglected patients, fly larvae may destroy orbital tissue and cause a marked inflammation and secondary bacterial infection. Certain fly larvae can penetrate through the conjunctiva and sclera and cause internal ophthalmomyiasis of the parasitic dipterous larvae. When this occurs, a single larva usually gains access into the eye. Most affected individuals are asymptomatic, but severe visual loss may occur (Klintworth 2012). In present case predisposing factor was BCC.
Chrysomya bezziana is an obligate ectoparasite in the animals and afflicts humans especially in some conditions such as poor hygienic lifestyle, working in contaminated areas during the warm seasons (Soleimani Ahmadi et al. 2009).
Infestation in humans and livestock are often observed in the wound, normal body orifices such as eye, ear, nose and mouth. The manifestations include pruritus, pain, inflammation, redness, eosinophilia, secondary bacterial infections. It rarely results in death of the patient (Wall and Shearer 1997). In the present study, the patient lived in rural area of Mazandaran with poor sanitary conditions where there is a relationship between people and animals.
Ophthalmomyiasis caused by C. bezziana is particularly damaging and a rare case of orbital myiasis due to C. bezziana has been documented (Klintworth 2012). Periorbital tissues that have been compromised by surgery, tumors, infections or ischemia may predispose towards myiasis since the flies feed on exudates, blood, secretions and decomposing tissue (Balasubramanya et al. 2003). In this study, the patient had none diagnostic BCC which made a risk factor for internal ophthalmomyiasis.
To our knowledge this is the third case of ophthalmomyiasis caused by C. bezziana that leads to a sever destruction. In all of cases the patients were elderly with underlying disease, two with BCC and one with a type of skin cancer (Radmanesh et al. 2000, Khataminia et al. 2011).
Conclusion
Although human ophthalmomyiasis is a rare disease but it may be emerging and increasing. Besides the status of this disease is not clear in Iran but in this paper we report a rare case with ophthalmomyiasis due to C. bezziana which basal cell carcinoma could provide an appropriate condition for larvae growth of mentioned fly and caused a secondary ophthalmomyiasis.
It is considered that many metabolic diseases (diabetes mellitus) and cancers (basal or squamous cell carcinoma), as well as poor hygiene can provide a suitable ground for myiasis because of delaying in wound healing in these diseases. Dermatologist and ophthalmologist must be alert about myiasis that can affect the patients with cancerous lesion.
Acknowledgement
The authors greatly acknowledge Mr. Majid Ganjbakhsh for his kind efforts. The authors declare that there is no conflict of interests.
References
- 1. Balasubramanya R, Pushker N, Bajaj MS, Rani A. ( 2003) Massive orbital and ocular invasion in ophthalmomyiasis. Can J Ophthal. 38( 4): 297– 298. [DOI] [PubMed] [Google Scholar]
- 2. Borror DJ, Triplehorn CA, Johnson NF. ( 1989) An introduction to the study of insects. 6th ed. Saunders College Publishing, Philadelphia, p. 875. [Google Scholar]
- 3. Chemonges-Nielsen S. ( 2008) Chrysomya bezziana in pet dogs in Hong Kong: a potential threat to Australia. Aust Vet J. 81( 4): 202– 205. [DOI] [PubMed] [Google Scholar]
- 4. Chan JCM, Lee JSW, Dai DLK, Woo J. ( 2005) Unusual cases of human myiasis due to Old World screwworm fly acquired indoors in Hong Kong. Trans R Soc Trop Med Hyg. 99( 12): 914– 918. [DOI] [PubMed] [Google Scholar]
- 5. Cook GC, Zumla AI. ( 2009) Manson's Tropical Diseases. Saunders, Philadelphia. [Google Scholar]
- 6. Farahvash MS, Aalami Harandi Z. ( 1998) Bilateral ophthalmomyiasis interna posterior: report of a case with severe visual loss. Arch Iran Med. 2: 38– 41. [Google Scholar]
- 7. Goddard J. ( 2003) Physician's guide to arthropods of medical importance. CRC Press LLC, Florida. [Google Scholar]
- 8. Janovy John, Schmidt Gerald D, Roberts Larry S. ( 2012) Foundations of Parasitology: Ninth Edition. McGraw-Hill, Chicago. [Google Scholar]
- 9. Janbakhsh B, Pirouz MS, Tirgari S, Agha Mohammadi A. ( 1977) A case of ophthalmomyiasis in man by Oestrus ovis Linneaeus in Tehran (Insecta: Diptera, Oestridae). Acta Med Iran. 20( 1–2): 19– 26. [PubMed] [Google Scholar]
- 10. Khataminia G, Aghajanzadeh R, Vazirianzadeh B, Rahdar M. ( 2011) Orbital myiasis. J Ophthalmic Vis Res. 6( 3): 199– 203. [PMC free article] [PubMed] [Google Scholar]
- 11. Lagacé-Wiens PR, Dookeran R, Skinner S, Leicht R, Colwell DD, Galloway TD. ( 2008) Human ophthalmomyiasis interna caused by Hypoderma tarandi, Northern Canada. Emerg Infect Dis. 14: 64– 66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lane RP, Crosskey RW. ( 1993) Medical Insects and Arachnids. Chapman and Hall, London. [Google Scholar]
- 13. Langan SM, Dervan P, O'Loughlin S. ( 2004) A moving scalp nodule in a returning traveler. Br J Dermatol. 151( 6): 1270. [DOI] [PubMed] [Google Scholar]
- 14. Masoodi M, Hosseini K. ( 2004) External ophthalmomyiasis caused by sheep botfly (Oestrus ovis) larva: a report of 8 cases. Arch Iran Med. 7: 136– 139. [Google Scholar]
- 15. Radmanesh M, Khataminia G, Eliasi P, Korai MK, Ebrahimi A. ( 2000) Chrysomyia bezziana-infested basal cell carcinoma destroying the eye. Int J Dermatol. 39: 455– 457. [DOI] [PubMed] [Google Scholar]
- 16. Raposo AA, Schettini AP, Massone C. ( 2012) Concurrent primary and secondary myiasis on basal cell carcinoma. An Bras Dermatol. 87( 2): 292– 295. [DOI] [PubMed] [Google Scholar]
- 17. Razmjou H, Mowlavi GH, Nateghpour M, Solaymani-Mohamadi, Kia EB. ( 2007) Ophthalmomyiasis Caused by Flesh Fly (Diptera: Sarcophagidae) in a Patient with Eye Malignancy in Iran. Iran J Arthropod-Borne Dis. 1( 2): 53– 56. [Google Scholar]
- 18. Ramonas KM, Friedman AH. ( 2006) Systemic infectious and inflammatory diseases. In: Tasman W, Jaeger EA. (eds). Duane's phthalmology [CD-ROM]. Vol 5 Lippincott Williams and Wilkins, Philadelphia. [Google Scholar]
- 19. Sharifipour F, Feghhi M. ( 2008) Anterior ophthalmomyiasis interna: an ophthalmic emergency. Arch Ophthalmol. 126: 1466– 1467. [DOI] [PubMed] [Google Scholar]
- 20. Soleimani Ahmadi M, Nasirian H, Nazemi Gheshmi AM, Yaghoobi Ershadi MR. ( 2009) Human Extensive Head Skin Myiasis. Iran J Publ Health. 38( 1): 134– 138. [Google Scholar]
- 21. Tsuda S, Nagaji J, Kurose K, Miyasato M, Sasai Y, Yoneda Y. ( 2007) Furuncular Cutaneous Myiasis Caused By Dermatobia Hominis Larvae following Travel To Brazil. Int J Dermatol. 35( 2): 121– 123. [DOI] [PubMed] [Google Scholar]
- 22. Walker AR. ( 1994) Arthropods of Humans and Domestic Animals: A Guide to Preliminary Identification. Springer, New York City. [Google Scholar]
- 23. Wilhelmus KR. ( 1986) Myiasis palpebrarum. Am J ophthalmol. 101( 4): 496. [DOI] [PubMed] [Google Scholar]
- 24. World Organisation for Animal Health ( 2008) Manual of Diagnostic Tests and Vaccines for Terrestrial Animals (Mammals, Birds and Bees). 6th ed. Vol. 2 Available at: http://www.oie.int/doc/ged/D7709.PDF [Google Scholar]
- 25. Yaghoubi Gholamhossein, Heydari Behrouz. ( 2013) External Ophthalmomyiasis Presenting to an Emergency Department: Corneal Findings as a Sign of Oestrus ovis. Korean J Ophthalmol. 27( 5): 341– 344. [DOI] [PMC free article] [PubMed] [Google Scholar]


