Abstract
Background:
Due to various climatic conditions in different parts of Iran, presenting of various kinds of human myiasis is expected. Despite of a few case series, most papers related to myiasis are case reports originated from various parts of Iran. This study discusses on different clinical features of myiasis in Iran and description of one case from Tehran as a representative to nosocomial infection in Iran.
Methods:
The information needed for this descriptive study was derived mainly from the digital library of Tehran University of Medical Sciences. The larvae have been identified with observing on posterior spiracles, spines of their body and anal tubercles.
Results:
Total number of reported myiasis cases from Iran is 77 which can be categorized clinically as furuncular, wound, ophthalmic, auricular, nasopharyngeal, oral, intestinal and genitourinary. Based on parasitological features, all myiasis agents in Iran are belonging to Calliphoridae, Sarcophagidae, Oestridae and Syrphidae flies. The case which is reporting in this paper can be mentioned as representative of nosocomial myiasis which it seems to be underreported because of some medicolegal reasons.
Conclusion:
Low number of investigations on various aspects of human myiasis, as well as incuriosity to report of the cases in disease reporting system of health minister, made the myiasis as a neglected disease.
Keywords: Myiasis, Diptera, Nosocomial, Hospital, Iran
Introduction
The parasitic relation which is induced with dipteran true fly larvae including feeding on ingested food, body materials and living/dead tissues of their hosts has been defined as myiasis disease (Zumpt 1965). Various species of true flies can cause myiasis disease around the world (John and Petri 2006). This kind of infestation in human is more spread in humid and warm geographical conditions (Maturo et al. 2007). Thus various kinds of the human myiasis are expected to be found in most parts of Iran due to their climatic conditions.
There is one fruncular myiasis from Iran in literature. That was an imported case on thighs of an Iranian 40 yr old man who came back from Africa after finishing his business trip. Presence of larvae made red pruritic lesions on his body (Mostafavizadeh et al. 2003).
Various cases of wound myiasis have been reported from various parts of Iran which occurred in different clinical settings such as head skin (Talari et al. 2004, Davami et al. 2005), scalp (Soleimani-Ahmadi et al. 2009), and basal cell carcinoma of head (Asilian and Andalib 2012) as well as the wound around pharyngostomy operation (Soleimani-Ahmadi et al. 2013). Lucilia sericata (Diptera: Calliphoridae) and Chrysomyia bezziana (Diptera: Calliphoridae) were identified as agents of wound myiasis in Iran.
Aalam described some cases of ophthalmomyiasis in his PhD thesis (Ghassemi 1989). Ophthalmomyiasis is infestation of human eyes and orbits tissues with larvae of myiasis agents which usually cause by the botfly Oestrus ovis (Diptera: Oestridae) (Akbarzadeh 2012). This kind of myiasis has been reported from various parts of Iran (Minar 1976, Ferdowsi and Rostami 2007, Soleymani et al. 2012, Akbarzadeh 2012).
Auricular myiasis is another kind of the disease which infects human ears. There are a few cases of auricular myiasis in Iran which were occurred by Ch. bezziana (Talari et al. 2002, Yaghoobi et al. 2005) and Lu. sericata (Akbarzadeh 2012).
Majority of myiasis cases reported in the literature from Iran were nasal myiasis originated from various parts. The agents of these cases were Ch. bezziana, Lu. sericata and Erystalis tenax (Diptera: Syrphidae) (Tirgari et al. 2003, Salimi et al. 2010a,b, Ghafori et al. 2011, Babamahmoodi et al. 2012, Youssefi et al. 2012).
Oral/gingival myiases also have been reported from various parts of Iran which affect on jaws or on mucosal tissues in oral cavities. The agents of these disease were obligatory myiasis producing flies, Oe. ovis (Diptera: Oestridae) and Wohlfahrtia magnifica (Diptera: Sarcophagidae) (Athari and Fallah 1993, Pour Eslami and Fallah 1996, Hakimi and Yazdi 2002, Mohammadzadeh et al. 2008, Moshref et al. 2008, Tamizi et al. 2008, Faramarzi et al. 2009).
The pharyngeal manifestation with larvae of Oe. ovis is more prevalent among shepherds and ranchers of Fars Province (Akbarzadeh 2012). There is only one comprehensive study on treatment of 33 cases of respiratory and non-respiratory manifestations of human pharyngeal myiasis in Fars Province (Masoodi and Hosseini 2003).
Intestinal myiasis or accidental myiasis is due to eating of food contaminated with egg or larvae of true flies (Mandell et al. 2010). This kind of myiasis is very rare in Iran and has the only two reports. Sarcophaga haemorrhoidalis (Diptera: Sarcophagidae) and Er. tenax cleared as responsible for these two cases (Khalili et al. 2007, Youssefi et al. 2010).
Urogenital myiasis is also not common and there are two case reports from Iran. Larvae of obligatory myiasis agents, Ch. bezziana and Wo. magnifica were observed in these two cases (Jdalayer et al. 1978, Salimi et al. 2010b).
In addition to their medical importance as mechanical vectors of parasitic disease agents (Kassiri et al. 2012) dipteran true flies can make myiasis in hospital environment called nosocomial myiasis (Nazni et al. 2011). Despite of low environmental sanitation in few hospitals, there are some features to make hospitalized patients easily accessed for flies (Franza et al. 2006). All of the nosocomial myiasis infections in Iran were nasal myiasis which occurred by facultative myiasis agents, Lu. sericata (Diptera: Calliphoridae) and Wohlfahrtia nuba (Diptera: Sarcophagidae) (Mowlavi et al. 2011, Maleki et al. 2012).
After occurring of fatal nosocomial myiasis in one case in a hospital in Tehran, this study was conducted to describe this case as a representative for this indifferent nosocomial infection. On the other hand all documented reports related with different kinds of myiasis disease in Iran have been collected and analyzed with the aim of declaring the status of this dangerous disease and showing the research gap in this issue.
Materials and Methods
The information needed for this study including papers, case reports, case series and student dissertations were derived mainly from the digital library of Tehran University of Medical Sciences. Regardless of number of papers or scientifically reports, all reported cases of various kinds of myiasis from Iran were counted and stratified in two ways, based on anatomical and parasitological features. The data was analyzed based on the number of cases, age grouping, gender, percent of death and of nosocomial infection, and spatial distribution of cases.
A case of nosocomial myiasis infection from one hospital in Tehran has been described as a representative sample of more underreported cases of such disease in hospitals. The larvae which originated from this case were sent to the Dipterology Laboratory, Department of Medical Entomology and Vector Control in Tehran University of Medical Sciences. Some of the larvae has preserved in 70% Ethanol and remained alive. Live larvae placed in the jar on a piece of fresh cow meat to complete the larval cycle and emerge the adults for confirming identification of samples. Identification of larvae has been done using the key of Zumpt (1965).
Results
Total number of myiasis cases in all published documents from Iran was 77. Based on the clinical/anatomical features, it is cleared that majority of cases (52%) were oral myiasis (Fig. 1).
Fig. 1.
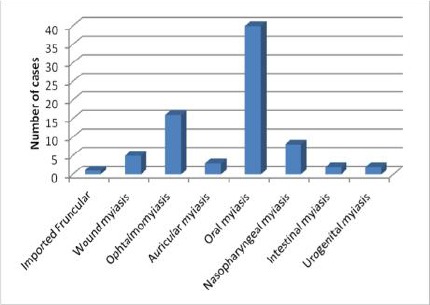
Number of reported cases in Iran divided by anatomical features
Categorizing of age groups of reported cases shows that there are two peaks (Fig. 2). i.e. most of the patients were between 21–40 years old (41.2%), while another peak indicates people with more than 61 years old.
Fig. 2.
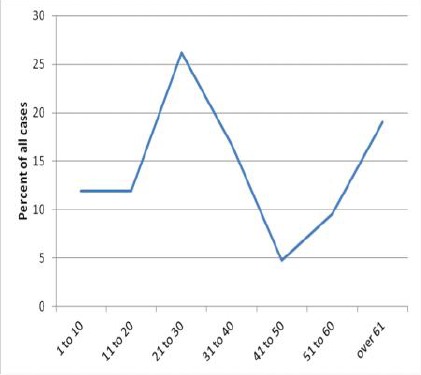
Age groups of reported myiasis cases in Iran
Despite of near 6.5% of non-identified/ not-reported agents, majority of the myiasis cases were due to Oe. ovis (Diptera: Oestridae) (65%) (Fig. 3).
Fig. 3.
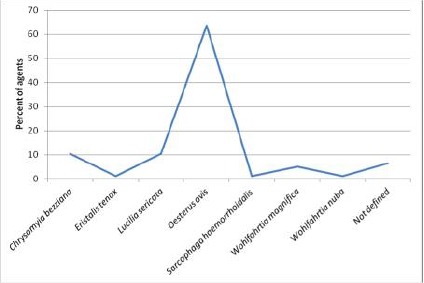
Dipteran species which have reported as myiasis agents in Iran
Human myiasis reports have been documented from 16 out of 31 provinces of Iran. It is cleared that more than 62% of all cases are reported from Fars Province (Fig. 4).
Fig. 4.
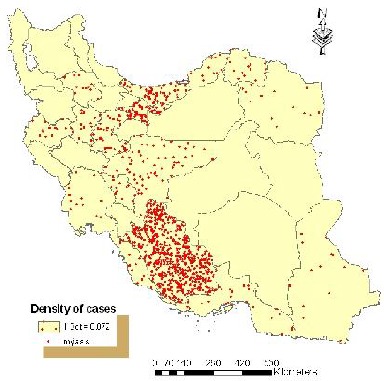
Spatial distribution of documented myiasis cases in provinces of Iran
Analysis of the documented cases based on gender showed 80.5% were male and 19.5% were female. About 3.9% of all cases were nosocomial infections in which one case (1.3%) has been reported as fatal nosocomial myiasis.
Case presentation
A 36 year old woman from Zanjan Province was referred to Baharloo Hospital in Tehran with fever, weakness, general body pain, vomiting and vaginal secretions at the end of 2012. She remarked that the symptoms have started since 6 weeks ago. She had IUD but few days before admission in hospital, it had been removed. In physical examination, pale conjunctiva was observed and systolic heart murmur was auscultated. Severe mitral regurgitation without vegetation was reported in her echocardiography. Other significant paraclinical results were: Hb: 8, WBC: 14000, CRP: 93 and ESR: 84. After a few days of starting empirical antibiotic therapy for covering both SBE/PID (Sub Acute Bacterial Endocarditis/Pelvic Inflammatory Disease), and while complementary diagnostic process was planning, she started to clinical improvement and fever was discontinued. In order to correcting of anemia, she received packed cell and several hours later, she fell down in progressive respiratory distress and then respiratory arrest occurred (probably due to pulmonary edema or transfusion related acute lung injury), therefore CPR was performed and after intubation she transferred to ICU. After one month of admission, while she was in comatose state and she had sepsis with hospital acquired gram negative organisms, during suction process, crawling fly larvae were observed from pharynx and tracheal trunk. She died one day later. The larvae were sent to the Department of Medical Parasitology, Tehran University of Medical Sciences, for further investigations and identification.
The agent of this case was Lu. sericata (Diptera: Calliphoridae). Some of the basic characters which have been obvious in the sampled larvae were completed perithremal ring, absence of accessory oral sclerite on cephalopharyngeal skeleton, absence of short process on dorsal and lateral surface on the larval body (Zumpt 1965).
Discussions
Clinically, myiasis may be categorized as based on the involved tissues or cavitites of body organs (Mandell et al. 2010). Literature review showed that except of furuncular myiasis, all clinical forms of the disease have reported to be originated from various parts of Iran.
Myiasis agents can be categorized as obligatory, facultative and accidental forms (Mullen and Durden 2002). All parasitological kinds of myiasis disease have been reported from Iran.
Nosocomial myiasis is not common even in endemic areas (Sinclair et al. 2011) but most of these rare cases will not report officially because of some reasons (Joo and Kim 2001). Based on this study the rates for nosocomial myiasis infections in Iran are about 4% and the proved mortality rate is 1.3%.
Most of hospital originated myiasis cases were due to facultative and accidental myiasis (Joo and Kim 2001). The agent of the case of this study was Lu. sericata which is a facultative myiasis fly. However it is proved that nosocomial myiasis caused by facultative agents can be fatal (Mowlavi et al. 2011).
A questionnaire based study in Fars Province cleared that more than 88% of the target community who are involved in sheep and goat breading industries were infected at least one time with oral myiasis (Akbarzadeh et al. 2012a). Based on high number of people involving with these industries, it cleared that total oral myiasis cases in Iran would be more than the 77 reported cases in literature.
Oestrus ovis is usually known as the agent of oral myiasis. About 65% of all reported cases in Iran were produced by this species. It can be resulted that this fly can be mentioned as the common human myiasis agent in the country.
Various climatic condition in different parts of Iran has provided suitable conditions for presence of various potentially myiasis agents. More than 62% of all myiasis reports were from Fars Province. This issue may be due to comprehensive studies with actively search for this disease and its agents (Akbarzadeh et al. 2012a, b, Akbarzadeh 2012) as well as a valuable study on treatment of 33 oral myiasis cases (Masoosdi and Hosseini 2003) in this province. Conducting synchronized studies in various parts of Iran may change the features of geographical distribution of myiasis cases in Iran.
Neither human nor animal myiasis diseases have been defined in governmental reporting systems of Iran. Therefore the exact status of both diseases, their distribution in the country and their causative agents remain obscure (Akbarzadeh et al. 2012a, Akbarzadeh 2012). A few reasons can be mentioned for this gap even in scientific literature of Iran. There are no more emphasizing on definition of myiasis diseases and identifications on their causative agents in medical colleges. Due to high volume of basic knowledge which should be learnt by medical students, the basic information about myiasis disease remained unconsidered. Identification of myiasis agents (dipteran larvae) are more difficult especially for the larvae of Sarcophagidae (Except of Wo. magnifica and Wo. nuba) as well as some species of Muscidae (Amendt et al. 2010, Pinto et al. 2011). Temporary rearing is essential for precise identification of the myiasis agents. This process is not possible in pathological laboratories and need subdivision cooperation between them and entomological laboratories in medical universities which is not occur in most cases.
Conclusion
Results of this review will provide useful information about distribution of myiasis agents in Iran for preventing the disease in man and animals. Improving new vision to this disease, conducting new efforts for situation analysis and providing suitable programs for control and treatment of the disease is highly recommended.
Acknowledgement
The authors wish to thanks to Ms Neda Mirsepahi for her kind cooperation and also want to make gratitude to lab technicians and nurses who helped us in accomplishing this work. The authors also wish to thanks Dr AA Hanafi-Bojd for kindly editing of the manuscript. The authors declared that there is no conflict of interest.
References
- 1. Akbarzadeh k. ( 2012) Estimation of geographical distribution, biodiversity and species richness of myiasis inducing flies in Fars Province. [PhD dissertation]. School of Public Health Tehran University of Medical Sciences, Iran. [Google Scholar]
- 2. Akbarzadeh K, Rafinejad J, Alipour H, Biglarian A. ( 2012a) Human myiasis in Fras Province, Iran. Southeast Asian J Trop Med Public Health. 43( 5): 1205– 1211. [PubMed] [Google Scholar]
- 3. Akbarzadeh K, Rafinejad J, Nozari J, Rassi Y, Sedaghat MM, Hosseini M. ( 2012b) A Modified Trap for Adult Sampling of Medically Important Flies (Insecta: Diptera). J Arthropod-Borne Dis. 6( 2): 119– 128. [PMC free article] [PubMed] [Google Scholar]
- 4. Amendt J, Lee Goff M, Campobasso CP, Grassberger M. ( 2010) Current Concepts in Forensic Entomology. Springer, Dordrecht: Chapt 16. p. 355. [Google Scholar]
- 5. Asilian A, Andalib F. ( 2012) Scalp Myiasis Associated with Advanced Basal Cell Carcinoma. J Isfahan Med Sch, Special Issue (Skin Diseases and Leishmaniasis). 29( 173): 3109– 3112. [Google Scholar]
- 6. Athari A, Fallah T. ( 1993) Dental cavity myiasis due to Wohlfahrtia magnifica. Med J IR Iran. 7( 3): 209– 210. [Google Scholar]
- 7. Babamahmoudi F, Rafinejhad J, Enayati A. ( 2012) Nasal myiasis due to Lucilia sericata (Meigen 1826) from Iran: A case report. Trop Biomed. 29( 1): 175– 179. [PubMed] [Google Scholar]
- 8. Davami M H, Kiani A, Salimi M, Farhadi E. ( 2005) Head skin myiasis due to Chrysomyia bezziana: A case report (in Persian). Skin Dis. 8( 4): 311– 315. [Google Scholar]
- 9. Faramarzi A, Rasekhi AR, Kalantari M, Hatam GR. ( 2009) Chrysomya bezziana as a Causative Agent of Human Myiasis in Fars Province, Southern Iran. Iran J Arthropod-Borne Dis. 3( 1): 60– 63. [PMC free article] [PubMed] [Google Scholar]
- 10. Ferdowsi A, Rostami A. ( 2007) Ophtalmomyiasis with expanded destruction on carcinoma of squamal cells of orbit. Bina J Ophthalmol. 13( 2): 273– 274. [Google Scholar]
- 11. Franza R, Leo L, Minerva T, Sanapo F. ( 2006) Myiasis of the tracheostomy wound: case report. Acta Otorhinolaryngol Ital. 26: 222– 224 [PMC free article] [PubMed] [Google Scholar]
- 12. Ghafori M, Samizadeh M, Rezaee A. ( 2011) Nasopharyngeal myiasis in a ICU hospitalized 52 years old woman (in Persian). J North Khorasan Univ Med Sci. 3( 2): 61– 64. [Google Scholar]
- 13. Ghassemi MJ. ( 1989) Identification of further cases of human myiasis and their distribution in Iran. [MSPH thesis]. School of Public Health, Tehran University of Medical Sciences. [Google Scholar]
- 14. Hakimi R, Yazdi I. ( 2002) Oral mucosa myiasis caused by Oestrus ovis. Arch Iranian Med. 5( 3): 194– 196. [Google Scholar]
- 15. Jdalayer T, Maleki M, Moghtaderi M. ( 1978) Human urogenital myiasis caused by Chrysomyia bezziana. Iranian J Publ Health. 7( 3): 116– 117. [Google Scholar]
- 16. John DT, Petri WA. ( 2006) Markell and Voge's Medical Parasitology. 9th ed. Saunders: Elsevier. [Google Scholar]
- 17. Joo CY, Kim JB. ( 2001) Nosocomial submandibular infections with dipterous fly larvae. Korean J Parasitol. 39( 3): 255– 260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kassiri H, Akbarzadeh K, Ghaderi A. ( 2012) Isolation of Pathogenic Bacteria on the House Fly, Musca domestica L. (Diptera: Muscidae), Body Surface in Ahwaz Hospitals, Southwestern Iran. Asian Pac J Trop Biomed. S1116– S1119 [Google Scholar]
- 19. Khalili B, Ebrahimi M, Khoobdel M. ( 2007) A case of intestinal myiasis due to Sarcophaga hemorrhoidalis from Chahar Mahal and Bakhtiari Province. J Shahrekord Univ Med Sci. 9( 2): 85– 88. [Google Scholar]
- 20. Maleki Ravasan N, Shayeghi M, Najibi B, Oshaghi MA. ( 2012) Infantile Nosocomial Myiasis in Iran. J Arthropod-Borne Dis. 6( 2): 156– 163. [PMC free article] [PubMed] [Google Scholar]
- 21. Mandell GL, Bennett JE, Dolin R. (eds) ( 2010) Principles and Practice of Infectious Diseases. Vol. 2 Elsevier Churchill Livingstone, Philadelphia. [Google Scholar]
- 22. Masoodi M, Hosseini K. ( 2003) The respiratory and allergic manifestations of human myiasis caused by larvae of the sheep bot fly ( Oestrus ovis) a report of 33 pharyngeal cases from southern Iran. Ann Trop Med Parasitol. 97( 1): 75– 81. [DOI] [PubMed] [Google Scholar]
- 23. Maturo S, Michaelson PG, Brennan J. ( 2007) Auricular myiasis. Otolaryngol Head Neck Surg. 136: 668– 669. [DOI] [PubMed] [Google Scholar]
- 24. Minar J. ( 1976) A case of eye myiasis in man caused by first instar larvae of Oestrus ovis L (Diptera: Oestridae) in Iran. Folia Parasitol (Praha). 23: 283– 284. [PubMed] [Google Scholar]
- 25. Mohammadzadeh T, Hadadzadeh R, Esfandiari F, Sadjjadi SM. ( 2008) A Case of Gingival Myiasis Caused by Wohlfahrtia magnifica. Iran J Arthropod-Borne Dis. 2( 1): 53– 56. [Google Scholar]
- 26. Moshref M, Ansari G, Lotfi A. ( 2008) Oral gingival myiasis: A case report. Int J Trop Med. 3( 4): 97– 100. [Google Scholar]
- 27. Mostafavizadeh K, Emami Naeini AR, Moradi S. ( 2003) Cutaneous Myiasis. Iran J Med Sci. 28( 1): 46– 47. [Google Scholar]
- 28. Mowlavi Gh, Nateghpour M, Teimoori S, Amin A, Noohi F, Kargar F. ( 2011) Fatal nosocomial myiasis caused by Lucilia sericata. J Hosp Infect. 78: 335– 339. [DOI] [PubMed] [Google Scholar]
- 29. Mullen GR, Durden LA. ( 2002) Medical and Veterinary Entomology. Academic Press/Elsevier Science, San Diego. [Google Scholar]
- 30. Nazni WA, Jeffery J, Lee HL, Lailatul A, Chew WK, Heo CC, Sadiyah I, Khairlasuad M, Heah SK, Mohd Hisham H. ( 2011) Nosocomial nasal myiasis in an intensive care unit. Malaysian J Pathol. 33( 1): 53– 56. [PubMed] [Google Scholar]
- 31. Pinto e Vairo K, de Mello-Patiu CA, de Carvalho CJB. ( 2011) Pictorial identification key for species of Sarcophagidae (Diptera) of potential forensic importance in southern Brazil Rev Bras Entomol. 55( 3): 333– 347. [Google Scholar]
- 32. Pour Eslami H, Fallah T. ( 1996) Dental myiasis due to Wohlfahrtia magnifica. J Dent. 8( 1): 85– 90. [Google Scholar]
- 33. Salimi M, Edalat H, Jourabchi A, Oshaghi MA. ( 2010a) First Report of Human Nasal Myiasis Caused by Eristalis tenax in Iran (Diptera: Syrphidae). Iran J Arthropod-Borne Dis. 4( 1): 77– 80. [PMC free article] [PubMed] [Google Scholar]
- 34. Salimi M, Goodarzi D, Karimfar MH, Edalat H. ( 2010b) Human Urogenital Myiasis Caused by Lucilia sericata (Diptera: Calliphoridae) and Wohlfahrtia magnifica (Diptera: Sarcophagidae) in Markazi Province of Iran. Iran J Arthropod-Borne Dis. 4( 1): 72– 76. [PMC free article] [PubMed] [Google Scholar]
- 35. Sinclair BJ, Gill BD, McCarthy AE. ( 2011) Nosocomial myiasis in a Canadian intensive care unit. Can Med Assoc J. 177( 7): 719– 720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Soleimani-Ahmadi M, Nasirian H, Nazemi Gheshmi AM, Yaghoobi Ershadi MR. ( 2009) Human Extensive Head Skin Myiasis. Iran J Publ Health. 38( 1): 134– 138. [Google Scholar]
- 37. Soleimani-Ahmadi M, Vatandoost H, Hanafi-Bojd AA, Poorahmad-Garbandi F, Zare M, Hosseini SMV. ( 2013) First Report of Pharyngostomy Wound Myiasis Caused by Chrysomya bezziana (Diptera: Calliphoridae) in Iran. J Arthropod-Borne Dis. 7( 2): 194– 198. [PMC free article] [PubMed] [Google Scholar]
- 38. Soleymani A, Tayebi E, Omidbakhsh S. ( 2012) A Case Report of External Ophthalmomyiasis. J Mazandaran Univ Med Sci. 22( 92): 104– 107 (Persian). [Google Scholar]
- 39. Talari SA, Yeganeh-Moghadam A, Dehghani R. ( 2002) Chrysomyia bezziana infestation. Arch Iran Med. 5( 1): 56– 58. [Google Scholar]
- 40. Talari SA, Sadr F, Doroodgar A, Talari MR, Gharabagh AS. ( 2004) Wound myiasis caused by Lucilia sericata. Arch Iranian Med. 7( 2): 128– 129. [Google Scholar]
- 41. Tamizi M, Najafi MH, Sargolzaee N. ( 2008) Gingival myiasis: A case report. J Dent Tehran Univ Med Sci. 5( 1): 42– 45. [Google Scholar]
- 42. Tirgari S, Nateghpour M, Jahanian AH, Akbarzadeh K. ( 2003) Case report: First Record of Human Myiasis caused by Chrysomia bezziana (Villeneuve) in Iran (Diptera, Calliphoridae). Iran J Publ Health. 32( 3): 68– 70. [Google Scholar]
- 43. Wilhelmus K. ( 1986) Myiasis palpebrarum. Am J Ophthalmol. 101: 496– 498. [DOI] [PubMed] [Google Scholar]
- 44. Yaghoobi R, Tirgari S, Sina N. ( 2005) Human auricular myiasis caused by Lucilia sericata: clinical and parasitological considerations. Acta Med Iran. 43( 2): 155– 157. [Google Scholar]
- 45. Youssefi MR, Sefidgar SAA, Abouhosseini Tabari M. ( 2010) First Report of Intestinal Myiasis Due To Eristalis tenax in Iran. Iran J Parasitol. 5( 2): 77– 79. [PMC free article] [PubMed] [Google Scholar]
- 46. Youssefi MR, Rahimi MT, Marhaba Z. ( 2012) Occurrence of Nasal Nosocomial Myiasis by Lucilia sericata (Diptera: Calliphoridae) In North of Iran. Iran J Parasitol. 7( 1): 104– 108. [PMC free article] [PubMed] [Google Scholar]
- 47. Zumpt F. ( 1965) Myiasis in man and animals in the Old World. Butterworth's, London. [Google Scholar]


