Abstract
Knowledge of the sequences and structures of proteins produced by microbial pathogens is continuously increasing. Besides offering the possibility of unraveling the mechanisms of pathogenesis at the molecular level, structural information provides new tools for vaccine development, such as the opportunity to improve viral and bacterial vaccine candidates by rational design. Structure-based rational design of antigens can optimize the epitope repertoire in terms of accessibility, stability, and variability. In the present study, we used epitope mapping information on the well-characterized antigen of Neisseria meningitidis factor H binding protein (fHbp) to engineer its gonococcal homologue, Ghfp. Meningococcal fHbp is typically classified in three distinct antigenic variants. We introduced epitopes of fHbp variant 1 onto the surface of Ghfp, which is naturally able to protect against meningococcal strains expressing fHbp of variants 2 and 3. Heterologous epitopes were successfully transplanted, as engineered Ghfp induced functional antibodies against all three fHbp variants. These results confirm that structural vaccinology represents a successful strategy for modulating immune responses, and it is a powerful tool for investigating the extension and localization of immunodominant epitopes.
INTRODUCTION
Neisseria meningitidis is still responsible for fatal disease worldwide (1). Glycoconjugate vaccines against serogroups A, C, W, and Y have been available since the early 2000s (2), while the prevention of infection by meningococcus serogroup B (MenB) strains has to be afforded to alternative antigens due to the poor immunogenicity of the serogroup B polysaccharide and its structural similarity to human neural antigens, which has raised concerns about the risk of inducing autoreactive antibodies (3). The research of novel candidates culminated with the development of two protein-based vaccines approved for use in humans, one (Trumenba) licensed in the United States for use in individuals 10 through 25 years of age (4, 5), and the second (Bexsero) recommended in >30 countries for all age groups, including infants (6). Both vaccines contain factor H binding protein (fHbp, alternatively named rLP2086 or GNA1870), a lipoprotein expressed by a large majority of circulating strains (7), which is able to elicit a potent protective immune response against serogroup B (8–11). fHbp plays a fundamental role during meningococcal infection, providing the bacterium with a way to evade the host serum surveillance. The protein, secreted across the outer membrane, is able to bind and sequester the human complement regulator factor H on the bacterial surface. This interaction prevents the activation of the alternative complement pathway and protects meningococci from killing (12, 13).
fHbp shows a high level of genetic diversity. So far, >700 diverse fHbp peptide sequences are known, with amino acid identities ranging from about 62 to 99% (http://pubmlst.org/neisseria/fHbp/). On the basis of such variability, fHbp sequences have been classified as belonging to variant 1, 2, or 3 (8) or to subfamily A or B (9). Serological studies indicate that the genetic variability can have a profound influence on determining the ability of antibodies to kill fHbp-expressing strains, as the immune response elicited by each variant ensures poor coverage against strains expressing heterologous alleles (8, 9). The inclusion of additional antigens (11) or combinations of distant fHbp subvariants (9) are both strategies pursued to expand the vaccine coverage to virtually all circulating meningococcal strains. The fHbp subvariant 1.1, included in the Bexsero vaccine (11), represents the prototypic member of variant 1. In the past, we engineered this molecule in order to expand its coverage to variants 2 and 3. The resulting chimeric protein was able to protect mice against a panel of meningococcal strains expressing all three variants (14). Recently, the gonococcal homologue of fHbp (Ghfp) was characterized by Jongerius et al. (15) and proposed as an alternative broad-coverage vaccine candidate against meningococcal disease. Ghfp shows 60 to 94% sequence identity to fHbp and demonstrated the ability to induce in mice antibodies able to kill natural meningococcal strains expressing different fHbp variants, although the effective response against variant 1 was relatively low and limited to the subvariant 1.1. Moreover, Ghfp was unable to bind human factor H (15, 16), a desirable feature that can prevent partial masking of the protein surface to the immune system (15).
In the present work, we explored the possibility of increasing the coverage of the immune response raised by Ghfp against meningococcal strains by inserting epitopes of fHbp subvariant 1.1 on its surface.
Knowledge of the fHbp structure (17–20) provides the unique opportunity to deeply analyze the distribution and accessibility of conserved and variant-specific residues. Moreover, a considerable ensemble of epitope mapping studies have reported on fHbp. Pioneering mutagenesis studies identified critical residues for binding to bactericidal antibodies (21, 22). Subsequently, nuclear magnetic resonance (NMR) (23), hydrogen-deuterium exchange mass spectroscopy (HDX-MS) (24), and X-ray crystallographic studies (25) have allowed remarkable progress in mapping protective epitopes.
This information makes members of the fHbp family ideal candidates for rational design studies attempting to modulate their immunogenicity by the introduction of heterologous epitopes from different variants.
In order to introduce fHbp variant 1-specific epitopes onto Ghfp, we modified the gonococcal protein surface according to the information derived from the NMR epitope mapping on fHbp. We previously mapped by NMR the epitope recognized by the monoclonal antibody 502 (MAb502) specific for fHbp subvariant 1.1 (23). Here, we used the same approach to map the epitope of a second fHbp 1.1-specific monoclonal antibody called JAR5 (26). Both MAb502 and JAR5 have been reported to induce complement-mediated killing of meningococcal cells in the presence of rabbit complement (22, 26). We decided therefore to introduce onto Ghfp both the MAb502 and JAR5 epitopes. Mice immunized with the resulting chimeric proteins elicited serum able to kill a wide panel of meningococcal strains belonging to variants 1, 2, and 3. This work represents an epitope mapping-based rational design that increased the antigenicity of Ghfp and is in principle applicable to any vaccine candidate whose potential coverage is limited by sequence variability.
MATERIALS AND METHODS
Bacterial strains.
Escherichia coli strains DH5α and BL21(DE3) were purchased from Invitrogen and used as a cloning and expression strain, respectively. Ampicillin (Sigma) was used at concentration of 100 μg ml−1.
Antibody generation.
The hybridoma cell line expressing JAR5 (26) was kindly provided by D. M. Granoff (Children's Hospital Oakland Research Institute [CHORI]). The murine IgG2b isotype monoclonal antibody JAR5 and the corresponding Fab fragment were produced and purified by Areta International S.r.l. (Gerenzano, Italy).
NMR sample preparation and interaction studies.
To express recombinant 2H/15N-labeled fHbp subvariant 1.1 for NMR measurements, E. coli BL21(DE3) (pET21b-fHbp) was grown on M9 minimal medium in 80% heavy water (2H2O) with the addition of glucose and 3.0 g of 15NH4Cl (98% isotopic enrichment; Sigma-Aldrich) as the sole carbon and nitrogen source, respectively. The culture was induced at A590 of 4.0 with 1.4 mM sterile filtered isopropyl 1-thio-β-d-galactopyranoside (Sigma) for 12 h. The protein lacking the N-terminal leader peptide and the lipobox motif and containing a C-terminal 6×His tag was purified by two chromatographic steps: Ni2+ affinity (His-Trap high-performance [HP] 5-ml column; GE Healthcare), and cation exchange (HiTrap SP HP). Analytical gel filtration analysis showed that the recombinant protein was eluted as a monomer. The protein sample used for NMR experiments was subsequently dialyzed against 20 mM sodium phosphate buffer at pH 7.0. NMR samples contained 10% (vol/vol) 2H2O for NMR spectrometer lock.
The interaction between the Fab fragment of JAR5 with 2H/15N-labeled fHbp subvariant 1.1 was investigated with 1H–15N transverse relaxation-optimized spectroscopy (TROSY)-heteronuclear single quantum coherence (HSQC) experiments. All NMR measurements were performed at 298 K on a Bruker Avance 900 spectrometer, working at a 900.13-MHz frequency and equipped with a cryogenically cooled probe. Titrations were performed on 0.4 mM 2H/15N-labeled fHbp 1.1 protein samples with the unlabeled JAR5 up to an fHbp-to-JAR5 molar ratio of 1:1.5. 1H and 15N resonance assignments for the fHbp subvariant 1.1 protein were already available (27).
Cloning and expression of Ghfp mutants.
The DNA sequence of Neisseria gonorrhoeae strain FA1090 ghfp devoid of the region encoding the leader peptide and the N-terminal glycine stretch was used as starting point to generate the three chimeric proteins. The amino acid substitutions were introduced, avoiding the use of rare codons for arginine. The 3 synthetic genes were purchased from GeneArt (Invitrogen) to include NdeI and XhoI restriction sites at the 5′ and 3′ ends, respectively. Each gene was digested with NdeI/XhoI and cloned into the corresponding sites of the pET21b(+) vector (Novagen). The expression vectors were transformed into E. coli BL21(DE3). The recombinant cells were grown at 37°C to an optical density at 600 nm of ∼0.5, at which time 1 mM isopropyl-β-d-thiogalactopyranoside (IPTG) was added, and the cultures were allowed to grow for 3 h. Cells were harvested by centrifugation at 4,000 rpm for 15 min at 4°C.
Protein purification.
Bacterial pellets were resuspended in 10 ml of buffer A (50 mM NaH2PO4 [Sigma], 300 mM NaCl [Fluka], 30 mM imidazole [Merck] [pH 8.0]), sonicated, and centrifuged at 35,000 × g for 30 min. The supernatant was collected and subjected to two serial purification steps using metal affinity chromatography (IMAC) and ionic exchange chromatography with a desalting step in between. All purification steps were performed using an ÄKTAxpress chromatographic system, and the OD280 was monitored. For the IMAC purification step, filtered supernatants were automatically injected into 1-ml Ni2+-HiTrap HP columns at a flow rate of 1 ml/min, and the columns were washed with 20 column volumes (CV) of washing buffer (50 mM NaH2PO4 [Sigma], 300 mM NaCl [Fluka], 30 mM imidazole [Merck] [pH 8.0]). Next, the His tag fusion proteins were eluted with 5 CV of elution buffer (50 mM NaH2PO4, 300 mM NaCl, 500 mM imidazole [pH 8.0]) and automatically loaded on three 5-ml HiTrap (GE) desalting columns connected in series and eluted at a flow rate of 5 ml/min in 50 mM Tris-HCl (pH 8.0). For ionic exchange chromatography, the eluted proteins were automatically loaded on 1-ml HiTrap Q HP columns at a flow rate of 1 ml/min. Subsequently, the column was washed with 10 CV of 50 mM Tris-HCl (pH 8.0). The elution was set up in a linear gradient, between 50 mM Tris-HCl (pH 8.0) and 50 mM Tris-HCl and 1.0 M NaCl (pH 8.0) buffer in 10 CV, and 1-ml fractions were collected. Protein purity was >95% for all samples, as by determined by densitometry analyses of a SDS-PAGE 12% gel. Protein aggregation and apparent molecular weight were checked by analytical size exclusion chromatography (Waters Acquity ultraperformance liquid chromatography [UPLC] system equipped with a BEH200 1.7-mm column, 4.6 by 300 mm [Waters], 150 mM NaH2PO4 buffer [pH 7.0], at a flow rate of 0.4 ml/min). All protein samples were >95% in the monomeric form. A summary of the features of the purified recombinant proteins is reported in Table S1 in the supplemental material.
Surface plasmon resonance analysis.
Surface plasmon resonance (SPR) was used to analyze the binding of fHbp and chimeric proteins to MAb502 and JAR5. All SPR experiments were performed using a Biacore T200 instrument at 25°C (GE Healthcare). In brief, a carboxymethylated dextran sensor chip (CM-5; GE Healthcare) was prepared, in which high densities (∼10,000 response units [RU]) of anti-mouse antibodies from a commercially available mouse antibody capture kit (GE Healthcare) were immobilized by amine coupling. The anti-mouse IgG chip was used then to capture ∼1,000 to 1,500 RU of MAb502 and JAR5. Proteins, purified as described before, and diluted in buffer containing 10 mM HEPES, 150 mM NaCl, 3 mM EDTA, and 0.05% (vol/vol) P20 surfactant (pH 7.4) (HBS-EP) to a final concentration of 200 nM for the single-injections experiments and to a range of five consecutive injections of increasing analyte concentrations (2.5 nM to 40 nM) for the single-cycle kinetics (SCK) experiments (28) were injected over the captured antibodies. Surfaces were then regenerated with 10 mM glycine (pH 1.7). Anti-mouse antibody-coated surfaces without captured monoclonal antibody were used as the reference channel. A blank injection of buffer only was subtracted from each curve, and reference sensorgrams were subtracted from experimental sensorgrams to yield curves representing specific binding. The data are representative of at least two independent experiments. SPR data were analyzed using the Biacore T200 evaluation software (GE Healthcare). For the SCK experiments, each sensorgram was fitted with the 1:1 Langmuir binding model, including a term to account for potential mass transfer, to obtain the individual kon (association rate constant) and koff (dissociation rate constant) kinetic constants; the individual values were then combined to derive the single averaged KD (equilibrium dissociation constant) values reported.
Binding to human factor H was also analyzed in two experimental setups. First, purified full-length factor H (Calbiochem) was covalently immobilized by amine coupling on a CM5 chip to reach a density of ∼2,500 RU. Proteins at a concentration of 200 nM in phosphate-buffered saline (PBS) were injected, and binding levels were compared. Regeneration between injections was achieved by a single injection of 10 mM glycine (pH 3) in a 3 M NaCl solution. In order to assess the effect of several factor H concentrations on binding, proteins were covalently immobilized by amine coupling on a CM5 chip on different flow cells to reach a density of ∼300 to 400 RU. Full-length factor H was then injected at increasing concentrations (0.07 to 2 μM), and binding to the different surfaces was compared. Following each injection, sensor chip surfaces were regenerated with a 30-s injection of 50 mM NaOH.
Differential scanning calorimetry.
The thermal stability of the mutants was checked by differential scanning calorimetry (DSC) experiments performed with a MicroCal VP-Capillary instrument (GE Healthcare) with an integrated autosampler. The samples were dialyzed in PBS to a final protein concentration of 0.5 mg/ml. DSC scans were recorded in the temperature range of 10 to 110°C, with a thermal ramping of 200°C per hour and a 4-s filter period. The data were analyzed by subtraction of the reference data for a sample containing buffer only, using the Origin 7 software (OriginLab).
Antigen formulation.
All formulations were performed under sterile conditions under a flow hood. Each recombinant protein was adsorbed onto aluminum hydroxide at protein, aluminum (alum), and NaCl concentrations of 100 μg/ml, 3 mg/ml, and 9 mg/ml, respectively, in 10 mM histidine (pH 6.5). Water for injection and histidine buffer were premixed. Sodium chloride was added to result in a final formulation osmolality of 0.300 milliosmoles (mosmol)/kg. The addition of alum was calculated on the basis of the concentration of the alum stock to obtain a final concentration of 3 mg/ml. Antigens were added to the mix at their respective concentrations, left for 15 min under stirring at room temperature, and then stored overnight at 4°C before immunization. The final formulations were isotonic and at physiological pH. All alum formulations were characterized soon after immunization, antigen adsorption was >90%, and the adsorption profiles were similar for all antigens and adjuvants tested.
Bactericidal activity assay.
To prepare antiserum, 20 μg of protein was used to immunize 6-week-old CD1 female mice (Charles River). Eight mice per group were used. The antigens were administered intraperitoneally (i.p.), together with aluminum hydroxide (3 mg/ml), on days 0, 21, and 35. Two weeks after the third immunization, the sera were collected and pooled. Serum bactericidal antibody activity of mouse immune sera was evaluated as previously described by Borrow et al. (29) against the N. meningitidis strains listed in Table 1. Pooled baby rabbit serum was used as the complement source. Bactericidal titers in the presence of rabbit complement (rSBA) were expressed as the reciprocal of the final serum dilution step giving ≥50% killing at 60 min compared to the number of CFU at time zero.
TABLE 1.
Meningococcal strains used in this study
| Strain | Clonal complex | STa | Yr isolated | Countryb | Serogroup:serotype:serosubtypec | fHbp subvariantc |
|---|---|---|---|---|---|---|
| MC58 | 32 | 74 | 1985 | UK | B:15:P1.7,16b | 1.1 |
| M14879 | 1157 | 1157 | 2006 | USA | B:NA:P1.22,14-6 | 1.13 |
| NZ98/254 | 41/44 | 42 | 1998 | NZ | B:4:P1.4 | 1.14 |
| M01-0240660 | 269 | 269 | 2001 | UK | B:NA:P1.19,15 | 1.15 |
| M08-240104 | 35 | 35 | 2008 | UK | B:4:P1.14 | 2.16 |
| M12566 | 41/44 | 5111 | 2004 | USA | B:4,7:P1.4 | 2.19 |
| M1239 | 41/44 | 437 | 1995 | USA | B:14:P1.23,14 | 3.28 |
| M01-240988 | 213 | 213 | 2001 | UK | B:1:NA | 3.30 |
| M01-240355 | 213 | 213 | 2001 | UK | B:1:NA | 3.31 |
| LNP24551 | 32 | 34 | 2008 | FR | B:4:P1.5,2 | 3.116 |
ST, sequence type.
NZ, New Zealand; FR, France.
The fHbps are named in terms of the translated (protein) sequence, as variant class.protein ID, in accordance with the public fHbp database (http://pubmlst.org/neisseria/fHbp/), in which new protein variants are assigned a sequential numerical identifier, alongside a prefix corresponding to the Novartis variant designation (variant 1, 2, or 3). For example, fHbp 1.1 refers to Novartis subvariant 1, neisseria.org protein subvariant 1. ST, sequence type as determined by MLST. NA, not assigned.
Fluorescence-activated cell sorter analysis of fHbp expression.
The ability by mouse polyclonal anti-fHbp sera to bind the surface of meningococci was measured using a 1:100 dilution of mouse polyclonal antiserum raised by the same fHbp variant when available or by closely related alleles (25). Primary antibody binding was detected by using an anti-mouse (whole-molecule) fluorescein isothiocyanate (FITC)-conjugated antibody (Sigma) at a 1:100 dilution.
RESULTS
NMR epitope mapping.
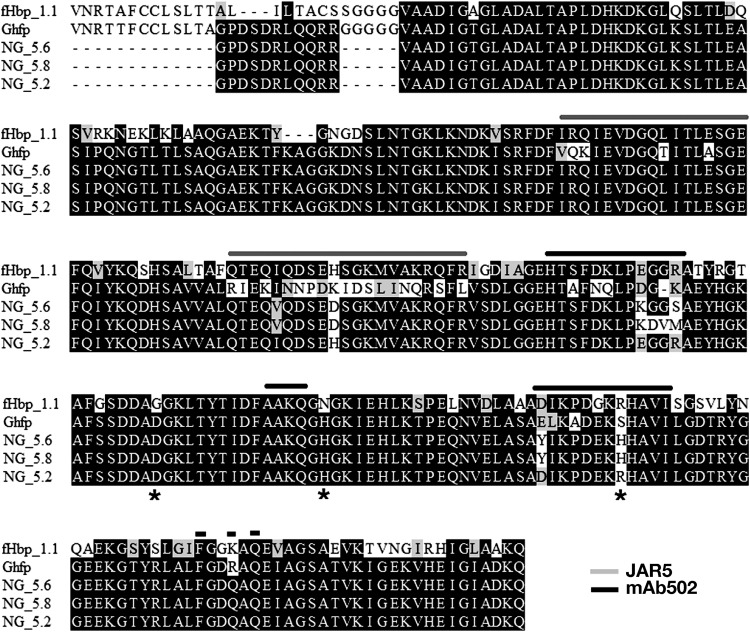
fHbp 1.1 is one of the protein subvariants more frequently found during epidemiological surveys worldwide (30, 31). For this reason, several studies have been reported describing the epitopes of this protein that are recognized by bactericidal monoclonal antibodies. In a previous study, we mapped the fHbp site recognized by MAb502 in one of the edges of the carboxyl-terminal beta barrel domain (23). Previous mutagenesis work reported by Beernink et al. (21) indicated that JAR5 targets the N-terminal domain of fHbp in a region overlapping the binding site to factor H. Such preliminary evidence suggested that MAb502 and JAR5 recognized very distinct regions of the fHbp surface and were able to cooperate in inducing a protective immune response against fHbp subvariant 1.1 (21). To identify the residues forming the JAR5 epitope, we applied the same NMR-based approach that we previously used to map MAb502 (23). Briefly, 1H,15N HSQC NMR spectra were acquired on 2H/15N-labeled fHbp in the presence and absence of the JAR5 Fab fragment. Changes in the chemical environment caused by Fab binding were expected to change the chemical shift of the backbone NH groups. The residues of fHbp experiencing chemical shift changes upon the addition of JAR5 are listed in Table S2 in the supplemental material. With the exception of Gln38, Ser39, and Asn43, all affected residues were localized on four adjacent beta strands of the N-terminal domain (Fig. 1A). Gln38, Ser39, and Asn43 were not considered a part of the JAR5 epitope, due to their distance from all the other perturbed residues. Remarkably, the epitope defined by NMR includes both Gly121 and Lys122, which were previously identified by Beernink and colleagues (21) as essential for binding to JAR5.
FIG 1.
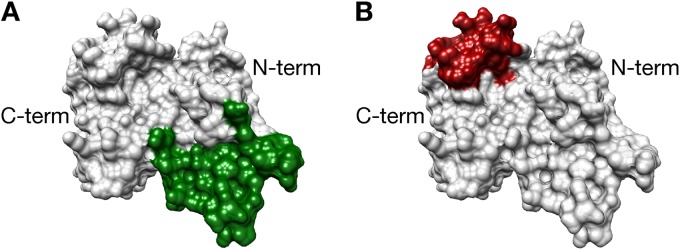
(A) NMR mapping of the epitopes recognized by JAR5 and MAb502. The residues involved in the interaction with JAR5 are depicted in green. (B) The epitope of MAb502 is colored in red and is reported according to Scarselli et al. (23). C-term, C terminus; N-term, N terminus.
The ensemble of perturbed residues formed a solvent-accessible surface of 2,860 Å2, a value exceeding the range of 900 to 2,000 Å2 typical of conformational epitopes characterized so far (32–34). We cannot, however, exclude that some perturbation effects could be ascribed to local conformational rearrangements occurring after the interaction with the antibody rather than direct contact with JAR5, leading to an overestimation of the epitope extension.
No overlap was observed between the JAR5 and MAb502 epitopes (Fig. 1B; see also Table S2 in the supplemental material), while, in line with the observation that JAR5 can inhibit the fHbp interaction with factor H (21), the JAR5 epitope largely resulted in overlapping the factor H binding site (see Table S2).
Design of chimeric Ghfp.
The aim of this work was to design a broad-coverage antigen against N. meningitidis by engineering the Ghfp surface. We selected as a scaffold the Ghfp from Neisseria gonorrhoeae strain FA1090, which encodes a fHbp homologue unable to bind human factor H and that is closely related to members of fHbp variant 3 (Fig. 2). The substitution of some surface-accessible residues of Ghfp with amino acids specifically present in fHbp variant 1 was expected to result in the creation of a chimeric molecule containing epitopes of both variants. Extension and localization of the fHbp subvariant 1.1 epitopes recognized by MAb502 and JAR5 were used to identify the portions of the Ghfp surface to be modified.
FIG 2.
Classification tree of the different fHbp alleles used in this study. Ranges of amino acid sequence identity of fHbp variants (var.) 1, 2, and 3 to Ghfp are reported in parentheses. Multiple-sequence alignment has been carried out with Clustal W (39), available at the NPS@ server. The dendrogram was obtained at Phylogeny.fr server with TreeDyn (40).
In order to produce chimeric proteins able to elicit antibodies that are cross-protective across all variant 1 subvariants, we aligned the amino acid sequences of fHbp 1.1 to 1.3, 1.14, and 1.15, the most divergent subvariants among the highly common isolates belonging to variant 1 (30) (see Fig. S3 in the supplemental material). Next, selected groups of concurrent substitutions deduced from the multiple-sequence alignment were introduced in each chimeric protein. In Fig. 3, the amino acid sequences of the wild-type gonococcal scaffold and the meningococcal allele MC58 used to elicit both JAR5 and MAb502 in mice are compared to those of the mutants. Overall, 29, 30, and 31 amino acid substitutions were made on FA1090 to generate NG_5.2, NG_5.6, and NG_5.8, respectively. The resulting three mutants, and Ghfp and the fHbp subvariants 1.1 and 3.28, were expressed in E. coli as hexahistidine-tagged proteins.
FIG 3.
Multiple-sequence alignment of the engineered proteins (NG_5.2, NG_5.6, and NG_5.8) to the wild-type Ghfp and the fHbp subvariant 1.1. The asterisk marks positions 163, 178, and 204, which are critical for MAb502 binding to fHbp subvariant 1.1.
The effects of the substitutions on the thermal stability of the proteins were investigated by DSC. In DSC experiments, a melting temperature (Tm) value is given by the peak maximum in the scanned curve. Differently from the meningococcal fHbp, which typically shows two very distinct transitions (Tm1, 70°C; Tm2, 80 to 90°C), corresponding to the N- and C-terminal domains, respectively (17), the thermal unfolding of Ghfp appeared to be much more cooperative. The DSC profile of the gonococcal protein was deconvoluted in two nearly overlapping peaks with very similar melting temperatures (Tm1, 58°C; Tm2, 67°C) and a considerably low enthalpy in the case of the second transition (Fig. 4A).
FIG 4.
DSC analysis of engineered Ghfp proteins. (A) The overlapping peaks in the melting curve of Ghfp (gray line) have been calculated by applying a non-2-state fitting model according to the Levenberg-Marquardt nonlinear least-squares method using the Origin 7 software. (B) All the mutants generated two very distinct peaks, consistent with two unfolding events. Cp, heat capacity normalized for the concentration.
All mutants showed Tm1 values similar to that of the gonococcal wild type, while Tm2 sensibly increased in NG_5.2 and NG_5.6, reaching values more in line with those observed for the C-terminal domain of meningococcal fHbp (Fig. 4B). We concluded therefore that mutations introduce to mimic the MAb502 epitope stabilized the C-terminal domain of NG_5.2 and NG_5.6, while the JAR5-related mutations left the N-terminal domain substantially unaffected.
Functional analysis of the mutants.
The interaction of each mutant with the full-length human factor H was tested by SPR in order to evaluate whether substitutions had any impact on such interaction. Differently from the strong concentration-dependent interaction observed between fHbp variant 1.1 and human fH, no binding was detectable in the case of Ghfp and all the immobilized mutants of human factor H to increasing concentrations up to 2 μM (Fig. 5). These results led us to exclude that any residue necessary to reestablish the interaction was introduced by the JAR5 epitope grafting.
FIG 5.
Interaction of immobilized engineered proteins with factor H (fH) analyzed by SPR. Biacore sensorgrams show the dose-dependent response over time (resonance units [RU]) during the binding of increasing concentrations of factor H (up to 2 μM) on immobilized recombinant fHbp, while no binding is observed with the immobilized Ghfp proteins.
In order to check the ability by the mutants to properly present the MAb502 and JAR5 epitopes, the interaction with each monoclonal antibody was also investigated by SPR (Table 2 and Fig. 6). As expected, substitutions introduced in NG_5.2 conferred to the molecule the ability to bind MAb502 with affinity comparable to that of fHbp subvariant 1.1. In NG_5.6 and NG_5.8, binding to MAb502 was compromised instead. In both of these mutants, the gonococcal serine 204 was replaced by histidine (Fig. 3), the residue naturally occurring in subvariants 1.14 and 1.15 (see Fig. S3 in the supplemental material). We hypothesize that the absence of arginine 204, previously identified as being critical for the interaction of fHbp subvariant 1.1 with MAb502 (22), prevented the binding to NG_5.6 and NG_5.8.
TABLE 2.
Summary table of SCK experiments of the monoclonal antibodies binding to the Ghfp proteins with kon, koff, and KD measurementsa
| MAb | Protein | kon (M−1 s−1) | koff (s−1) | KD (M) |
|---|---|---|---|---|
| MAb502 | fHbp | 1.93 E+06 | 0.84 E−02 | 4.34 ± 0.03 E−09 |
| MAb502 | NG 5.2 | 0.63 E+06 | 2.85 E−03 | 4.53 ± 0.01 E−09 |
| JAR5 | fHbp | 0.81 E+06 | 2.15 E−04 | 2.63 ± 0.001 E−10 |
| JAR5 | NG 5.2 | 0.58 E+06 | 2.15 E−04 | 3.71 ± 0.02 E−10 |
| JAR5 | NG 5.6 | 0.82 E+06 | 3.71 E−03 | 4.53 ± 0.09 E−09 |
| JAR5 | NG 5.8 | 0.88 E+06 | 3.86 E−03 | 4.39 ± 0.15 E−09 |
Examples of sensorgrams are reported in Fig. S5 in the supplemental material.
FIG 6.
Interaction of engineered Ghfp proteins with JAR5 (A) and MAb502 (B) analyzed by SPR. Representative Biacore sensorgrams show the response over time (resonance units [RU]) during the binding of purified recombinant proteins to immobilized MAbs.
All three mutants were able to bind JAR5 with comparable affinity, although only NG_5.2 showed the low dissociation rate characteristic of fHbp subvariant 1.1.
Overall, the SPR analysis provided a preliminary indication that surface regions corresponding to the MAb502 and JAR5 epitopes were successfully introduced on the gonococcal protein and sufficiently well exposed on the protein surface to be recognized by respective monoclonal antibodies.
The immunogenicity of NG_5.2, NG_5.6, and NG_5.8 was then evaluated by a serum bactericidal assay (SBA) on the strains reported in Table 1. To confirm fHbp accessibility to the antibodies, we first probed the meningococcal strains by fluorescence-activated cell sorting (FACS) (Fig. 7). Mouse polyclonal sera elicited by homologous or closely related fHbp subvariants were used to detect fHbp on the bacterial surface. FACS profiles revealed that fHbp was easily accessible to antibodies in all strains tested. Moreover, N. meningitidis strains with higher (MC58, M01-02400660, and M08-02400104), intermediate (M12566, M01-0240988, and M01-02400355,), or lower (M14879, NZ98/254, M1239, and LNP024551) fHbp accessibility could be distinguished, suggesting that sequence diversity and protein exposure might both have an influence on the bactericidal titers.
FIG 7.
FACS analysis of fHbp surface expression and factor H binding of N. meningitidis strains used in this study. The presence of fHbp on the meningococcal cell surface was detected by binding of mice polyclonal sera elicited by the same fHbp subvariant, when available, or by closely related alleles. In each panel, the amino acid identity between fHbp used to immunize mice and the genetic variant expressed by the strain tested is reported in parentheses. The shaded and white profiles show the reactions with preimmune and immune sera, respectively. Max, maximum; FL1-H, fluorescence intensity.
Groups of eight mice were immunized with NG_5.2, NG_5.6, or NG_5.8. Controls included animals vaccinated with Ghfp and fHbp subvariants 1.1 and 3.28. The ability of the chimeric proteins to elicit functional antibodies was evaluated by measuring the complement-mediated killing induced by the immune sera in vitro. rSBA values of <16 were considered negative, as this is the starting dilution for the experiments.
A summary of the rSBA analysis is reported in Table 3. Ghfp induced a bactericidal immune response against meningococcal strains expressing fHbp variants 2 and 3 but failed to protect mice against variant 1. Conversely, bactericidal activity against variant 1 was observed at different levels after vaccination with each of the three mutants. Complement-mediated killing of all the variant 1 isolates was induced by the sera of mice immunized with NG_5.6 and NG_5.8. Despite that fact that NG_5.2 was the only mutant able to bind MAb502 (Fig. 5B), the NG_5.2 immune sera exhibited moderate bactericidal titers of all the variant 1 strains. The loss of bactericidal activity against NZ98/254 and the low titer against M14879 might be due to the limited amount of fHbp detected on their surface (Fig. 7). To explain the relatively low titers observed against MC58, we speculated that few mismatches of surface-exposed residues, like aspartate 163 (glycine in MC58) and histidine 178 (asparagine in MC58) (Fig. 3), might have counteracted the positive effects of the epitope grafting. Alternatively, changes in the conformational equilibrium induced by the NG_5.2-specific substitutions (Fig. 4) might have indirectly influenced the variant 1 epitope presentation.
TABLE 3.
Serum bactericidal titers elicited in mice by engineered antigens against the panel of strains described in Table 1
| Strain | fHbp varianta | Titer for antigen: |
|||||
|---|---|---|---|---|---|---|---|
| NG5.6 | NG5.8 | NG5.2 | NGFA1090 | fHbp 3.28 (M1239) | fHbp 1.1 (MC58) | ||
| MC58 | 1.1 | 512 | 128 | 256 | <16 | <16 | >8,192b |
| M14879 | 1.13 | 1,024 | 1,024 | 64 | <16 | <16 | 1,024 |
| NZ98/254 | 1.14 | 256 | 512 | <16 | <16 | <16 | 128b |
| M01-240660 | 1.15 | 4,096 | 4,096 | 512 | <16 | <16 | 2,048 |
| M08-240104 | 2.16 | 2,048 | 128 | 256 | ≥8,192 | 2,048 | 16 |
| M12566 | 2.19 | 128 | 128 | 1,024 | 512 | 256 | <16 |
| M1239 | 3.28 | 64 | 16 | <16 | 256 | 2,048 | <16b |
| M01-240988 | 3.30 | 512 | 128 | 32 | 512 | 32 | <16 |
| M01-240355 | 3.31 | 256 | 256 | 128 | 2,048 | 512 | <16 |
| LNP24551 | 3.116 | 64 | 64 | <16 | 512 | <16 | <16 |
Wild-type Ghfp and fHbp subvariants 1.1 and 3.28 were also included as controls.
From reference 37.
NG_5.6 and NG_5.8 also retained the ability to kill all strains of variants 2 and 3, although a sensible decrease in bactericidal activity compared to that of the gonococcal wild type was observed, particularly against the low-fHbp-expressing strains of variant 3, M1239 and LNP24551. Bactericidal titers against variant 2 strains were also elicited by NG_5.2. This mutant was unable to promote the complement-mediated killing against M1239 and LNP24551 (Table 3), likely due to the combined effect of low fHbp abundance and sequence diversity.
DISCUSSION
Molecular grafting of functional epitopes is a promising way to improve variable antigens and realize novel proteins with prespecified functionalities. Side-chain and backbone remodeling were recently proposed as protein design strategies to stabilize and optimize protein antigens for presentation of contiguous conformational epitopes (35–37).
In a previous study, we engineered the C-terminal domain of fHbp 1.1 by introducing residues specific to variants 2 and 3 within patches of about 1,000 A2 (14). The mutagenesis was applied to the entire immunodominant carboxyl-terminal domain of the protein, whose surface was systematically explored in order to identify the region(s) able to well tolerate the epitope grafting in terms of folding and immunogenicity. In the present work, we decided to explore the possibility of modulating the immunogenicity of the gonococcal fHbp orthologue Ghfp by selectively grafting predefined meningococcal epitopes from the distantly related fHbp subvariant 1.1.
Deep structural knowledge of subvariant 1.1-specific protective epitopes allowed us to limit the mutagenesis on the regions of protein surface specifically recognized by anti-subvariant 1.1 antibodies. We previously reported the characterization of the epitope recognized by the murine monoclonal antibody MAb502 by NMR. The antibody binding site covered a surface of 1,992 Å2 entirely located on one apex of the carboxyl-terminal domain of the protein and distant from the site of interaction with factor H (23). In the present study, we mapped the epitope of a second monoclonal antibody, JAR5, previously reported to target Gly121 and Lys122 on fHbp subvariant 1.1 and able to inhibit binding to factor H (21). Such observations suggest that the region recognized by JAR5 was very distinct from the MAb502 epitope. The present results confirm this prediction. The JAR5 epitope identified by NMR was entirely located within the N-terminal domain of fHbp, excluding any overlap the region recognized by MAb502. Remarkably, the JAR5 epitope was localized in the same region where the epitopes of two murine IgG1 monoclonal antibodies (17C1 and 30G4) were previously mapped by hydrogen-deuterium exchange mass spectrometry (24). Both 17C1 and 30G4 displayed, although to different extents, synergistic bactericidal activity against strains of variant 1 when used in combination with MAb502. These results suggested that cotransplantation of the JAR5 and MAb502 epitopes in a fHbp variant 3-like environment might result in a molecule able to induce potent protective immunity against variant 1 strains.
The serum bactericidal activity assay measures the ability of immune sera to mediate killing of meningococci in vitro in the presence of an exogenous source of complement. In a previous study, Jongerius and colleagues (15) evaluated the ability by Ghfp to induce bactericidal antibodies against meningococcal strains expressing variant 1, 2, or 3. They tested a panel of seven isolates and observed comparable bactericidal activity across the three variants. A remarkable exception was the MC58 strain (fHbp subvariant 1.1), which was resistant to killing by anti-Ghfp antibodies. In the present work, we analyzed a different set of meningococcal isolates, which included four strains expressing different variant 1 subvariants. All fHbp variant 1-expressing isolates tested were not killed by anti-Ghfp serum, according to the observation that molecules of variant 3 do not induce bactericidal antibodies against variant 1 (8, 38).
Ghfp induced bactericidal antibodies against M12566 and M1239, expressing the fHbp 2.19 and 3.28 subvariants, respectively, with SBA titers comparable to those reported by Jongerius et al. (15) for the same subvariants. The M08-240104 and M01-240355 strains, expressing the fHbp 2.16 and 3.4 subvariants, respectively, showed a more pronounced sensitivity to the bactericidal activity of the anti-Ghfp immune sera. In the case of M01-240355, this might be due to the higher sequence similarity to Ghfp of the fHbp 3.4 subvariant (93.51% identity at the amino acid level) than that of all the other meningococcal strains of the panel (see Table S3 in the supplemental material). The M08-240104 sequence was 87% identical to that of Ghfp, and this cannot, however, be invoked to explain the high sensitivity of this strain to the Ghfp immune serum. It is possible that the high expression level of fHbp, together with the conservation of a small number of specific residues residing within crucial epitopes, render M08-240104 more susceptible to killing by anti-Ghfp antibodies.
Overall, the results of the bactericidal activity assay showed that the mutagenesis was able to introduce a local molecular mimicry of fHbp variant 1 sufficient to elicit antibodies that were bactericidal against a panel of natural meningococcal strains expressing different subvariants. In particular, NG5.6 and NG5.8 were both able to elicit a protective immune response against all variant 1 strains tested, including isolates expressing some of the most prevalent alleles, like 1.1 and 1.13 (7).
A general decrease in bactericidal titers against variant 3 was observed in sera elicited by the mutants compared to those obtained by immunization with the wild-type gonococcal protein. The total area including MAb502 and JAR5 epitopes accounts for about 13% of the fHbp surface, and both epitopes were localized on the predicted accessible side of the molecule. The changes introduced in the gonococcal protein reduced the surface area available to elicit variant 3-specific antibodies. This was particularly critical in the case of variant 3 strains, in which fHbp expression levels were generally lower than those in variant 1. Alternatively, the modifications might have specifically altered epitopes that are critical for variant 3. Finally, we cannot exclude that modifications in the amino acid sequence might have introduced some local conformational change of the molecule that altered the original epitope repertoire. The DSC profile of the mutants indicated that substitutions increased the thermal stability of the proteins, presumably stabilizing the overall fold. However, how this might reflect changes in immunogenicity remains unclear.
In conclusion, we enhanced the potential of Ghfp as a vaccine candidate by threading in defined portions of its surface two well-characterized heterologous functional epitopes. Although a clear correlation between the bactericidal titers obtained in mice with rabbit complement and bactericidal response in humans has not been yet defined, the positive titers reported in the present study indicate that the chimeric proteins have the potential to raise protective immunity against a wider panel of meningococcal strains than that with native Ghfp. The detailed epitope characterization obtained by NMR provided valuable information for antigen optimization, permitting us to limit the mutagenesis within restricted regions of the protein surface and minimize the changes in naturally occurring sequences. This aspect assumes particular relevance for the optimization of large proteins in which molecular dimensions and sequence variability might require the screening of a massive number of mutants.
ACKNOWLEDGMENTS
We thank Dan M. Granoff (Children's Hospital Oakland Research Institute, Oakland, CA, USA) for providing the JAR5 cell line.
This work was partially supported by Regione Toscana (grant POR CREO FESR 2007-20013) and by Instruct, part of the European Strategy Forum on Research Infrastructures (ESFRI). Specifically, we thank the EU ESFRI Instruct Core Centre CERM-Italy.
We declare no conflicts of interest.
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/CVI.00794-14.
REFERENCES
- 1.Jafri RZ, Ali A, Messonnier NE, Tevi-Benissan C, Durrheim D, Eskola J, Fermon F, Klugman KP, Ramsay M, Sow S, Zhujun S, Bhutta ZA, Abramson J. 2013. Global epidemiology of invasive meningococcal disease. Popul Health Metr 11:17. doi: 10.1186/1478-7954-11-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zimmer SM, Stephens DS. 2004. Meningococcal conjugate vaccines. Expert Opin Pharmacother 5:855–863. doi: 10.1517/14656566.5.4.855. [DOI] [PubMed] [Google Scholar]
- 3.Dull PM, McIntosh ED. 2012. Meningococcal vaccine development–from glycoconjugates against MenACWY to proteins against MenB–potential for broad protection against meningococcal disease. Vaccine 30(Suppl 2):B18–B25. doi: 10.1016/j.vaccine.2012.01.062. [DOI] [PubMed] [Google Scholar]
- 4.Marshall HS, Richmond PC, Nissen MD, Jiang Q, Anderson AS, Jansen KU, Reynolds G, Ziegler JB, Harris SL, Jones TR, Perez JL. 2012. Safety and immunogenicity of a meningococcal B bivalent rLP2086 vaccine in healthy toddlers aged 18–36 months: a phase 1 randomized-controlled clinical trial. Pediatr Infect Dis J 31:1061–1068. doi: 10.1097/INF.0b013e31826327e4. [DOI] [PubMed] [Google Scholar]
- 5.Nissen MD, Marshall HS, Richmond PC, Jiang Q, Harris SL, Jones TR, Jansen KU, Perez JL. 2013. A randomized, controlled, phase 1/2 trial of a Neisseria meningitidis serogroup B bivalent rLP2086 vaccine in healthy children and adolescents. Pediatr Infect Dis J 32:364–371. doi: 10.1097/INF.0b013e31827b0d24. [DOI] [PubMed] [Google Scholar]
- 6.Esposito S, Castellazzi L, Bosco A, Musio A, Stoddard J. 2014. Use of a multicomponent, recombinant, meningococcal serogroup B vaccine (4CMenB) for bacterial meningitis prevention. Immunotherapy 6:395–408. doi: 10.2217/imt.14.11. [DOI] [PubMed] [Google Scholar]
- 7.Lucidarme J, Tan L, Exley RM, Findlow J, Borrow R, Tang CM. 2011. Characterization of Neisseria meningitidis isolates that do not express the virulence factor and vaccine antigen factor H binding protein. Clin Vaccine Immunol 18:1002–1014. doi: 10.1128/CVI.00055-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Masignani V, Comanducci M, Giuliani MM, Bambini S, Adu-Bobie J, Arico B, Brunelli B, Pieri A, Santini L, Savino S, Serruto D, Litt D, Kroll S, Welsch JA, Granoff DM, Rappuoli R, Pizza M. 2003. Vaccination against Neisseria meningitidis using three variants of the lipoprotein GNA1870. J Exp Med 197:789–799. doi: 10.1084/jem.20021911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fletcher LD, Bernfield L, Barniak V, Farley JE, Howell A, Knauf M, Ooi P, Smith RP, Weise P, Wetherell M, Xie X, Zagursky R, Zhang Y, Zlotnick GW. 2004. Vaccine potential of the Neisseria meningitidis 2086 lipoprotein. Infect Immun 72:2088–2100. doi: 10.1128/IAI.72.4.2088-2100.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Richmond PC, Nissen MD, Marshall HS, Lambert SB, Roberton D, Gruber WC, Jones TR, Arora A. 2012. A bivalent Neisseria meningitidis recombinant lipidated factor H binding protein vaccine in young adults: results of a randomised, controlled, dose-escalation phase 1 trial. Vaccine 30:6163–6174. doi: 10.1016/j.vaccine.2012.07.065. [DOI] [PubMed] [Google Scholar]
- 11.Giuliani MM, Adu-Bobie J, Comanducci M, Arico B, Savino S, Santini L, Brunelli B, Bambini S, Biolchi A, Capecchi B, Cartocci E, Ciucchi L, Di Marcello F, Ferlicca F, Galli B, Luzzi E, Masignani V, Serruto D, Veggi D, Contorni M, Morandi M, Bartalesi A, Cinotti V, Mannucci D, Titta F, Ovidi E, Welsch JA, Granoff D, Rappuoli R, Pizza M. 2006. A universal vaccine for serogroup B meningococcus. Proc Natl Acad Sci U S A 103:10834–10839. doi: 10.1073/pnas.0603940103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Madico G, Welsch JA, Lewis LA, McNaughton A, Perlman DH, Costello CE, Ngampasutadol J, Vogel U, Granoff DM, Ram S. 2006. The meningococcal vaccine candidate GNA1870 binds the complement regulatory protein factor H and enhances serum resistance. J Immunol 177:501–510. doi: 10.4049/jimmunol.177.1.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schneider MC, Exley RM, Chan H, Feavers I, Kang YH, Sim RB, Tang CM. 2006. Functional significance of factor H binding to Neisseria meningitidis. J Immunol 176:7566–7575. doi: 10.4049/jimmunol.176.12.7566. [DOI] [PubMed] [Google Scholar]
- 14.Scarselli M, Arico B, Brunelli B, Savino S, Di Marcello F, Palumbo E, Veggi D, Ciucchi L, Cartocci E, Bottomley MJ, Malito E, Lo Surdo P, Comanducci M, Giuliani MM, Cantini F, Dragonetti S, Colaprico A, Doro F, Giannetti P, Pallaoro M, Brogioni B, Tontini M, Hilleringmann M, Nardi-Dei V, Banci L, Pizza M, Rappuoli R. 2011. Rational design of a meningococcal antigen inducing broad protective immunity. Sci Transl Med 3:91ra62. doi: 10.1126/scitranslmed.3002234. [DOI] [PubMed] [Google Scholar]
- 15.Jongerius I, Lavender H, Tan L, Ruivo N, Exley RM, Caesar JJ, Lea SM, Johnson S, Tang CM. 2013. Distinct binding and immunogenic properties of the gonococcal homologue of meningococcal factor H binding protein. PLoS Pathog 9:e1003528. doi: 10.1371/journal.ppat.1003528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Veggi D, Gentile MA, Cantini F, Lo Surdo P, Nardi-Dei V, Seib KL, Pizza M, Rappuoli R, Banci L, Savino S, Scarselli M. 2012. The factor H binding protein of Neisseria meningitidis interacts with xenosiderophores in vitro. Biochemistry 51:9384–9393. doi: 10.1021/bi301161w. [DOI] [PubMed] [Google Scholar]
- 17.Johnson S, Tan L, van der Veen S, Caesar J, Goicoechea De Jorge E, Harding RJ, Bai X, Exley RM, Ward PN, Ruivo N, Trivedi K, Cumber E, Jones R, Newham L, Staunton D, Ufret-Vincenty R, Borrow R, Pickering MC, Lea SM, Tang CM. 2012. Design and evaluation of meningococcal vaccines through structure-based modification of host and pathogen molecules. PLoS Pathog 8:e1002981. doi: 10.1371/journal.ppat.1002981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cendron L, Veggi D, Girardi E, Zanotti G. 2011. Structure of the uncomplexed Neisseria meningitidis factor H binding protein fHbp (rLP2086). Acta Crystallogr Sect F Struct Biol Cryst Commun 67:531–535. doi: 10.1107/S1744309111006154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schneider MC, Prosser BE, Caesar JJ, Kugelberg E, Li S, Zhang Q, Quoraishi S, Lovett JE, Deane JE, Sim RB, Roversi P, Johnson S, Tang CM, Lea SM. 2009. Neisseria meningitidis recruits factor H using protein mimicry of host carbohydrates. Nature 458:890–893. doi: 10.1038/nature07769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cantini F, Savino S, Scarselli M, Masignani V, Pizza M, Romagnoli G, Swennen E, Veggi D, Banci L, Rappuoli R. 2006. Solution structure of the immunodominant domain of protective antigen GNA1870 of Neisseria meningitidis. J Biol Chem 281:7220–7227. doi: 10.1074/jbc.M508595200. [DOI] [PubMed] [Google Scholar]
- 21.Beernink PT, Welsch JA, Bar-Lev M, Koeberling O, Comanducci M, Granoff DM. 2008. Fine antigenic specificity and cooperative bactericidal activity of monoclonal antibodies directed at the meningococcal vaccine candidate factor H binding protein. Infect Immun 76:4232–4240. doi: 10.1128/IAI.00367-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Giuliani MM, Santini L, Brunelli B, Biolchi A, Aricò B, Di Marcello F, Cartocci E, Comanducci M, Masignani V, Lozzi L, Savino S, Scarselli M, Rappuoli R, Pizza M. 2005. The region comprising amino acids 100 to 255 of Neisseria meningitidis lipoprotein GNA 1870 elicits bactericidal antibodies. Infect Immun 73:1151–1160. doi: 10.1128/IAI.73.2.1151-1160.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scarselli M, Cantini F, Santini L, Veggi D, Dragonetti S, Donati C, Savino S, Giuliani MM, Comanducci M, Di Marcello F, Romagnoli G, Pizza M, Banci L, Rappuoli R. 2009. Epitope mapping of a bactericidal monoclonal antibody against the factor H binding protein of Neisseria meningitidis. J Mol Biol 386:97–108. doi: 10.1016/j.jmb.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Faleri A, Santini L, Brier S, Pansegrau W, Lo Surdo P, Scarselli M, Buricchi F, Volpini G, Genovese A, van der Veen S, Lea S, Tang CM, Savino S, Pizza M, Finco O, Norais N, Masignani V. 2014. Two cross-reactive monoclonal antibodies recognize overlapping epitopes on Neisseria meningitidis factor H binding protein but have different functional properties. FASEB J 28:1644–1653. doi: 10.1096/fj.13-239012. [DOI] [PubMed] [Google Scholar]
- 25.Malito E, Faleri A, Lo Surdo P, Veggi D, Maruggi G, Grassi E, Cartocci E, Bertoldi I, Genovese A, Santini L, Romagnoli G, Borgogni E, Brier S, Lo Passo C, Domina M, Castellino F, Felici F, van der Veen S, Johnson S, Lea SM, Tang CM, Pizza M, Savino S, Norais N, Rappuoli R, Bottomley MJ, Masignani V. 2013. Defining a protective epitope on factor H binding protein, a key meningococcal virulence factor and vaccine antigen. Proc Natl Acad Sci U S A 110:3304–3309. doi: 10.1073/pnas.1222845110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Welsch JA, Rossi R, Comanducci M, Granoff DM. 2004. Protective activity of monoclonal antibodies to genome-derived neisserial antigen 1870, a Neisseria meningitidis candidate vaccine. J Immunol 172:5606–5615. doi: 10.4049/jimmunol.172.9.5606. [DOI] [PubMed] [Google Scholar]
- 27.Cantini F, Veggi D, Dragonetti S, Savino S, Scarselli M, Romagnoli G, Pizza M, Banci L, Rappuoli R. 2009. Solution structure of the factor H binding protein, a survival factor and protective antigen of Neisseria meningitidis. J Biol Chem 284:9022–9026. doi: 10.1074/jbc.C800214200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Karlsson R, Katsamba PS, Nordin H, Pol E, Myszka DG. 2006. Analyzing a kinetic titration series using affinity biosensors. Anal Biochem 349:136–147. doi: 10.1016/j.ab.2005.09.034. [DOI] [PubMed] [Google Scholar]
- 29.Borrow R, Aaberge IS, Santos GF, Eudey TL, Oster P, Glennie A, Findlow J, Høiby EA, Rosenqvist E, Balmer P, Martin D. 2005. Interlaboratory standardization of the measurement of serum bactericidal activity by using human complement against meningococcal serogroup B, strain 44/76-SL, before and after vaccination with the Norwegian MenBvac outer membrane vesicle vaccine. Clin Diagn Lab Immunol 12:970–976. doi: 10.1128/CDLI.12.8.970-976.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vogel U, Taha M-K, Vazquez JA, Findlow J, Claus H, Stefanelli P, Caugant DA, Kriz P, Abad R, Bambini S, Carannante A, Deghmane AE, Fazio C, Frosch M, Frosi G, Gilchrist S, Giuliani MM, Hong E, Ledroit M, Lovaglio PG, Lucidarme J, Musilek M, Muzzi A, Oksnes J, Rigat F, Orlandi L, Stella M, Thompson D, Pizza M, Rappuoli R, Serruto D, Comanducci M, Boccadifuoco G, Donnelly JJ, Medini D, Borrow R. 2013. Predicted strain coverage of a meningococcal multicomponent vaccine (4CMenB) in Europe: a qualitative and quantitative assessment. Lancet Infect Dis 13:416–425. doi: 10.1016/S1473-3099(13)70006-9. [DOI] [PubMed] [Google Scholar]
- 31.Bambini S, Piet J, Muzzi A, Keijzers W, Comandi S, De Tora L, Pizza M, Rappuoli R, van de Beek D, van der Ende A, Comanducci M. 2013. An analysis of the sequence variability of meningococcal fHbp, NadA and NHBA over a 50-year period in the Netherlands. PLoS One 8:e65043. doi: 10.1371/journal.pone.0065043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Davies DR, Cohen GH. 1996. Interactions of protein antigens with antibodies. Proc Natl Acad Sci U S A 93:7–12. doi: 10.1073/pnas.93.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rubinstein ND, Mayrose I, Halperin D, Yekutieli D, Gershoni JM, Pupko T. 2008. Computational characterization of B-cell epitopes. Mol Immunol 45:3477–3489. doi: 10.1016/j.molimm.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 34.Chakrabarti P, Janin J. 2002. Dissecting protein-protein recognition sites. Proteins 47:334–343. doi: 10.1002/prot.10085. [DOI] [PubMed] [Google Scholar]
- 35.Azoitei ML, Correia BE, Ban YE, Carrico C, Kalyuzhniy O, Chen L, Schroeter A, Huang PS, McLellan JS, Kwong PD, Baker D, Strong RK, Schief WR. 2011. Computation-guided backbone grafting of a discontinuous motif onto a protein scaffold. Science 334:373–376. doi: 10.1126/science.1209368. [DOI] [PubMed] [Google Scholar]
- 36.Azoitei ML, Ban YE, Julien JP, Bryson S, Schroeter A, Kalyuzhniy O, Porter JR, Adachi Y, Baker D, Pai EF, Schief WR. 2012. Computational design of high-affinity epitope scaffolds by backbone grafting of a linear epitope. J Mol Biol 415:175–192. doi: 10.1016/j.jmb.2011.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Correia BE, Ban YE, Friend DJ, Ellingson K, Xu H, Boni E, Bradley-Hewitt T, Bruhn-Johannsen JF, Stamatatos L, Strong RK, Schief WR. 2011. Computational protein design using flexible backbone remodeling and resurfacing: case studies in structure-based antigen design. J Mol Biol 405:284–297. doi: 10.1016/j.jmb.2010.09.061. [DOI] [PubMed] [Google Scholar]
- 38.Seib KL, Brunelli B, Brogioni B, Palumbo E, Bambini S, Muzzi A, DiMarcello F, Marchi S, van der Ende A, Arico B, Savino S, Scarselli M, Comanducci M, Rappuoli R, Giuliani MM, Pizza M. 2011. Characterization of diverse subvariants of the meningococcal factor H (fH) binding protein for their ability to bind fH, to mediate serum resistance, and to induce bactericidal antibodies. Infect Immun 79:970–981. doi: 10.1128/IAI.00891-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Combet C, Blanchet C, Geourjon C, Deleage G. 2000. NPS@: network protein sequence analysis. Trends Biochem Sci 25:147–150. doi: 10.1016/S0968-0004(99)01540-6. [DOI] [PubMed] [Google Scholar]
- 40.Dereeper A, Guignon V, Blanc G, Audic S, Buffet S, Chevenet F, Dufayard JF, Guindon S, Lefort V, Lescot M, Claverie JM, Gascuel O. 2008. Phylogeny.fr: robust phylogenetic analysis for the non-specialist. Nucleic Acids Res 36:W465–W469. doi: 10.1093/nar/gkn180. [DOI] [PMC free article] [PubMed] [Google Scholar]