Abstract
Cervical cancer continues to be a major public health problem in India in the absence of wide spread organised cervical screening programs. Visual inspection of the cervix with acetic acid (VIA) is an effective, inexpensive screening test that can be combined with simple treatment procedures for early cervical lesions, provided by trained health workers. We report 7 years experience in early detection of cervical cancer and pre-cancers using the VIA test in a community-based program in rural Andhra Pradesh, India where there are no existing organised cervical screening programs.
Materials and Methods:
Eligible women aged between 26 and 60 were opportunistically screened by trained health wor kers using the VIA test. Women who tested positive were further evaluated and those with cervical lesions were treated either by cryotherapy in the screening clinic or referred to a higher center.
Results:
A total of 18,869 women were screened by a single round of VIA testing with a positive rate of 10.75%. Biopsy proven high-grade squamous intraepithelials (HSILs) were 90 (0.48%) and low-grade squamous intraepithelials (LSILs) were 43 (0.28%). The overall prevalence of cervical intraepithelial neoplasia (CIN) 2+ lesion rate is 1.05%. A total of 312 (1.65%) cryotherapies were done and 49 women underwent hysterectomy.
Conclusions:
VIA by trained female health workers is a safe, acceptable, and effective test that can save lives from cervical cancer even in remote areas with few resources. These results have important implications for efficient service delivery in cervical screening programs in low-resourced settings.
Keywords: Cervical cancer screening, cervical screening in low resource settings, early detection of cervical cancer, screen and treat, visual inspection with acetic acid (VIA)
Introduction
Cervical cancer continues to be a major public health problem in India with an incidence of 134,420 cases and mortality of 72,825 cases in the year 2008.(1) Only a few organized cervical screening programs exist in India, even though the disease burden is high. Many studies now provide evidence of the feasibility and cost-effectiveness of screening and treatment approaches for cervical cancer prevention. These can be easily adopted for various settings.(2,3,4,5,6,7,8) A significant reduction in cervical cancer mortality was shown following a single round of screening with HPV testing or VIA screening in a randomized trial in India.(9,10) Studies have also shown the safety, feasibility, and efficacy of conservative treatments for pre-cancers.(11,12)
Visual inspection with acetic acid (VIA) is a simple, inexpensive test with moderate sensitivity and specificity for screening that can be combined with simple treatment procedures for early cervical lesions.(13) Health workers or nurses can be trained as test providers; the results are available immediately. VIA is feasible in many low-resource areas where it is difficult to sustain high-quality cytology programs.
An expert group also recommended to the Government of India the use of VIA as the primary screening test to be performed by trained nurses or health workers in primary healthcare.(14) Scaling up and inclusion of VIA-based programs into national programs is already taking place in many low- and middle-income countries.(15,16,17) The evaluation of its impact on the service delivery will largely determine the success of the program when introduced into routine healthcare. We report 7 years experience of VIA testing in the early detection of cervical cancer and pre-cancers in a rural south Indian population where there are no organized cervical screening programs.
Materials and Methods
VIA-based cervical screening as a community outreach program was started by the Institute for Rural health Studies, Hyderabad in the rural areas of Mahabubnagar district of Andhra Pradesh, India from January 2006 onwards by trained female health workers (ANMs) hired locally. Data on the performance of VIA test in a programmatic manner was analyzed until December 2012, i. e., the last 7 years. Mahabubnagar district is one of the most backward districts of Andhra Pradesh state with lowest female literacy rate in India at 27.8%.
Eligible women aged between 26-60 years were invited for cervical screening conducted either in the fixed cancer screening clinic based in the district hospital or in the makeshift mobile cervical cancer screening clinics organized in 66 villages of Mahbubnagar district. Women who were not pregnant, with intact uterus, and no previous history of CIN or cancer who were willing to undergo screening were asked to participate. Trained female health workers (ANMs) conducted prior health education activities on cervical screening in the villages through group meetings and discussions involving local village leaders and women's self-help groups. Mobile screening camps were organized in village schools or community centers on mutually convenient dates. Informed consent was taken after complete explanation of test and treatment procedures. A basic proforma with identification numbers and general information is collected for each woman. The screening tests were performed by the ANMs and the diagnostic investigations were carried out by a medical officer in the same visit. After insertion of a sterile Cusco's self-retaining vaginal speculum, the ANM performs VIA test by applying freshly prepared 4% acetic acid to the cervix. The results are recorded after 1 minute using a halogen lamp to provide good illumination. The test results are scored as positive when a well-defined, dense acetowhite area with regular margins appears attached to the squamo columnar junction. The test is reported as either positive if an acetowhite area is seen in the transformation zone or negative if no change is observed or suspicious for invasive cancer, i. e., if a growth or ulcerative lesion is observed. Colposcopy was carried out with a binocular portable field colposcope (Ascon India) using 10 X magnification on all screen positive women in the same visit itself after applying 4% acetic acid and Lugol's iodine and followed by guided cervical punch biopsies. These specimen were transported to the Pathology department for histopathological confirmation as normal, squamous metaplasia, chronic cervicitis or probable low-grade (LSIL)/high-grade squamous intraepithelial (HSIL) lesion, invasive cancers, or inconclusive for lesions. These results were obtained within 3-4 weeks.
Treatment
In the initial 2 year period, those women with VIA-positive lesions were treated with cryotherapy by the health workers immediately after cervical biopsy as “screen and treat method.” After reviewing the protocol due to logistic issues of cryo gas supply, only women with biopsy confirmed precancerous lesions were recalled and treated ensuring compliance for the treatment as a “screen, test, and treat method.” Colposcopically or histologically confirmed LSIL or HSIL lesions occupying <3 quadrants of cervix not extending into endocervical canal or vaginal fornices and without any evidence of invasive cancer were treated by cryotherapy using nitrous oxide gas with the standard double freeze technique. A course of presumptive antibiotics was given after treatment. Those women requiring treatment for HSIL other than cryotherapy or with invasive cancer were referred to a higher center for appropriate treatment. Post-treatment advice was give to the women with a follow-up visit after 1 year.
Training and quality maintenance
Four female health workers were recruited and trained to run this program. The ANMs were trained on cervical screening methods and cryotherapy using the International Agency for Research on Cancer (IARC) manual(18) for 4 days through didactic lectures, practical training sessions, and using digital manuals. Following this, hands-on experience under supervision for two subsequent weeks allowed them to screen independently in the community. Periodic reorientation sessions were conducted to improve quality assurance. The medical officer was trained in performing colposcopy and followed the steps described in the IARC manual on colposcopy.(19)
Results
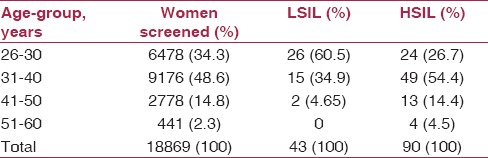
A total of 18,869 women were screened offering a single round of VIA test of which 2030 women were screen positive with VIA test positivity rate of 10.75% [Table 1]. Around 108 (0.57%) women with suspicious growths, or with invasive cancer, were referred to Mehdi Nawaz Jung (MNJ) Institute of Oncology & RCC, Hyderabad, and were treated free of cost through the state government insurance scheme. Overall, nearly half of the women screened were in the age group 31-40 years [Table 2]. Correspondingly 54.4% high-grade lesions were in this age-group. Around 60% of low-grade lesions were in the younger age-group of <30 years. Colposcopy was done on the 1922 screen-positive women in the same visit and directed cervical punch biopsy were done on 1722 women (9.1%). Biopsy proven HSILs were 90 (0.48%) and LSILs were 43 (0.28%). The overall prevalence of CIN 2 + lesion rate is 1.05%.
Table 1.
Results of VIA screening program
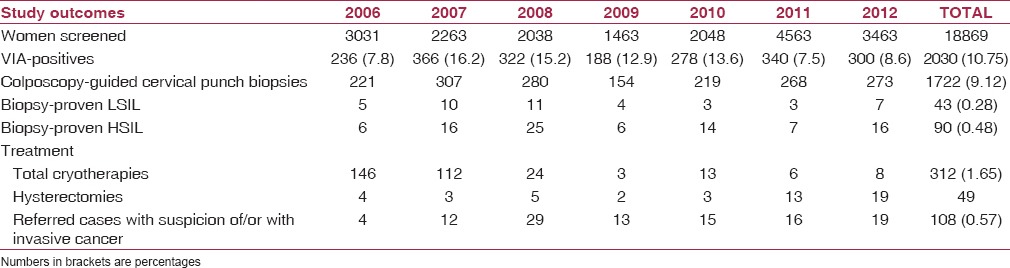
Table 2.
Age distribution by age and lesion category
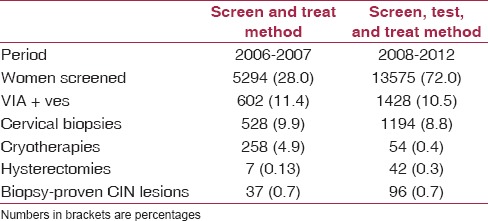
During 2006-2007 about 258 VIA-positive women underwent cryotherapy immediately after cervical punch biopsy as single-visit approach. From the year 2008 onwards, only women with biopsy-proven lesions were treated [Table 3]. A total of 312 (1.65%) cryotherapies were done and 49 women underwent hysterectomy. There were no serious adverse events recorded.
Table 3.
Comparison of screen and treat versus screen, test, and treat methodologies
Discussion
This study reports the experiences of implementing VIA-based cervical screening method in a remote, rural setting where medical facilities are limited. VIA is a simple and affordable screening test with acceptable sensitivity and specificity in the range 50-88.6% and 66.7-89.7%, respectively, in a research setting.(20) Our experience has shown that rural women accepted VIA test performed by female health workers even though these women had never been screened nor had any awareness of cervical cancer. The screening clinics were held in the villages within walking distance for most of the women and the service was provided free of cost.
The results show that adequately trained health workers under medical supervision can effectively perform cervical screening, cryotherapy, and follow-up care even with few resources. The screen positivity was 10.75% and the detection rate of CIN 2+ lesions in this program was 1.05%. This is comparable with other research studies on VIA where positivity ranged from 6.6% to 27.4%.(7,21) The average sensitivity of VIA in various studies from low resource settings is 50% (range 14-95) with a specificity of 85% (range 14-98). This wide range is due to variation in age of the women, type of provider, and their training.(20,22) Majority of the cervical abnormalities (85%) in our study were detected in women <40 years age [Table 2] indicating that VIA is effective in pre-menopausal age. Since the results are immediately available, diagnostic tests and treatment can be done in the same visit ensuring good compliance for screen positive women.(23) In our program, around 85% of screen-positive women had diagnostic confirmation in the same visit. Linkage of the screen-positives to the diagnosis and treatment is also an integral part of the program. Cryotherapy is widely considered to be an effective and appropriate means of treating pre-cancerous cervical lesions. Cryotherapy has been advocated as a safe option for treating women with screen-positive lesions in low resource settings.(24) Cryotherapy was provided for women screened by VIA by nurses in field clinics in Dindigul district, India. A high cure rate of 81% was reported in women with CIN 1 lesions and 71% in those with CIN 2-3 lesions.(11,12) Women in our program also have accepted and tolerated this procedure in the mobile camps as well without any adverse side effects. During the first 2 years of the program, even though the over-treatment rate is 7 times more, it ensured better compliance for treatment as a single visit approach. Colposcopy-directed biopsy, taken just before cryotherapy, has given an opportunity to get a histological proof of lesions treated and exclusion of any occult invasive cervical cancers among those who received treatment with cryotherapy.
The “screen, test, and treat method” that was followed from the year 2008 onwards also suggests that it is equally effective, provided great care is taken to get the women with lesions for treatment. This will avoid overtreatment and reduce the logistic difficulties with cryo gas availability. But the rate of hysterectomy for HSIL is more as these women insist on definitive treatment methods after biopsy confirmation. A single round of screening would still offer good benefits for these women in reducing the incidence and mortality from cervical cancer. The RCT in Dindigul district in south India found there was a reduction in cervical cancer incidence and mortality by 25% and 35%, respectively, with a single visit VIA followed by cryotherapy done by mid-level providers.(10) As recommended by Alliance for Cervical Cancer Prevention (ACCP) and Global Guidance for Cervical Cancer Prevention by FIGO, VIA plus cryotherapy programs using local physicians, nurses, midwives, and paramedical personnel could still result in a significant programmatic impact until affordable HPV deoxyribonucleic acid (DNA) tests become available.(25)
Our program proves that this cervical screening model can be easily adopted anywhere in order to reduce the burden of this disease. We conclude that VIA by trained female health workers is a safe, acceptable, and effective test that can save lives from cervical cancer even in remote areas with few resources. The experience from our program suggests that the performance of this test can be improved with good quality training and supervision as quality assurance is essential for a successful VIA-based program. These results have important implications for efficient service delivery in cervical screening programs in low-resource settings or even in integrating into primary care services.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Lyon: International Agency for Research on Cancer; 2010. [Last accessed on 2011 Nov 20]. GLOBOCAN 2008 v1.2, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No. 10. Available from: http://globocan.iarc.fr . [Google Scholar]
- 2.Shastri SS, Dinshaw K, Amin G, Goswami S, Patil S, Chinoy R, et al. Concurrent evaluation of visual, cytological and HPV testing as screening methods for the early detection of cervical neoplasia in Mumbai, India. Bull World Health Organ. 2005;83:186–94. [PMC free article] [PubMed] [Google Scholar]
- 3.Sankaranarayanan R, Wesley R, Thara S, Dhakad N, Chandralekha B, Sebastian P, et al. Test characteristics of visual inspection with 4% acetic acid (VIA) and Lugol's iodine (VILI) in cervical cancer screening in Kerala, India. Int J Cancer. 2003;106:404–8. doi: 10.1002/ijc.11245. [DOI] [PubMed] [Google Scholar]
- 4.Bhatla N, Gulati A, Mathur SR, Rani S, Anand K, Muwonge R, et al. Evaluation of cervical screening in rural North India. Int J Gynaecol Obstet. 2009;105:145–9. doi: 10.1016/j.ijgo.2008.12.010. [DOI] [PubMed] [Google Scholar]
- 5.Sankaranarayanan R, Nessa A, Esmy PO, Dangou JM. Visual inspection methods for cervical cancer prevention. Best Pract Res Clin Obstet Gynaecol. 2012;26:221–32. doi: 10.1016/j.bpobgyn.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 6.Ghosh P, Gandhi G, Kochhar PK, Zutshi V, Batra S. Visual inspection of cervix with Lugol´s iodine for early detection of premalignant and malignant lesions of cervix. Indian J Med Res. 2012;136:265–71. [PMC free article] [PubMed] [Google Scholar]
- 7.Sankaranarayanan R, Basu P, Wesley R, Mahe C, Keita N, Mbalawa CC, et al. IARC Multicentre Study Group on Cervical Cancer Early Detection. Accuracy of visual screening for cervical neoplasia: Results from an IARC multicentre study in India and Africa. Int J Cancer. 2004;110:907–13. doi: 10.1002/ijc.20190. [DOI] [PubMed] [Google Scholar]
- 8.Arbyn M, Sankaranarayanan R, Muwonge R, Keita N, Dolo A, Mbalawa CG, et al. Pooled analysis of the accuracy of five cervical cancer screening tests assessed in eleven studies in Africa and India. Int J Cancer. 2008;123:153–60. doi: 10.1002/ijc.23489. [DOI] [PubMed] [Google Scholar]
- 9.Sankaranarayanan R, Nene BM, Shastri SS, Jayant K, Muwonge R, Budukh AM, et al. HPV screening for cervical cancer in rural India. N Engl J Med. 2009;360:1385–94. doi: 10.1056/NEJMoa0808516. [DOI] [PubMed] [Google Scholar]
- 10.Sankaranarayanan R, Esmy PO, Rajkumar R, Muwonge R, Swaminathan R, Shanthakumari S, et al. Effect of visual screening on cervical cancer incidence and mortality in Tamil Nadu, India: A cluster randomized trial. Lancet. 2007;370:398–406. doi: 10.1016/S0140-6736(07)61195-7. [DOI] [PubMed] [Google Scholar]
- 11.Sankaranarayanan R, Rajkumar R, Esmy PO, Fayette JM, Shanthakumary S, Frappart L, et al. Effectiveness, safety and acceptability of ‘see and treat’ with cryotherapy by nurses in a cervical screening study in India. Br J Cancer. 2007;96:738–43. doi: 10.1038/sj.bjc.6603633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nene BM, Hiremath PS, Kane S, Fayette JM, Shastri SS, Sankaranarayanan R. Effectiveness, safety, and acceptability of cryotherapy by midwives for cervical intraepithelial neoplasia in Maharashtra, India. Int J Gynaecol Obstet. 2008;103:232–6. doi: 10.1016/j.ijgo.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 13.Alliance for Cervical Cancer Prevention. New evidence on the impact of cervical cancer screening and treatment using HPV DNA tests, visual inspection, or cytology. Cervical Cancer Prevention Fact Sheet. 2009 [Google Scholar]
- 14.Government of India and World Health Organization. Guidelines for cervical cancer screening program. Recommendation of the Expert Group Meeting held on 18-19 Nov 2005. 2006 [Google Scholar]
- 15. [Last accessed on 2012 Mar 18]. Available form: http://www.cervicalcanceraction.org/comments/map-slideshow-via.php .
- 16.Nessa A, Hussain MA, Rahman JN, Rashid MH, Muwonge R, Sankaranarayanan R. Screening for cervical neoplasia in Bangladesh using visual inspection with acetic acid. Int J Gynaecol Obstet. 2010;111:115–8. doi: 10.1016/j.ijgo.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 17.Tamil Nadu Health Systems Project. [Last accessed on 2013 March 29]. Available from: http://www.tnhsp.org/screening-cervical-cancer-and-breast-cancer .
- 18.Sankaranarayanan R, Wesley RS. Lyon: IARC Press; 2003. A Practical Manual on Visual Screening for Cervical Neoplasia. IARC Technical Publication, 41. [Google Scholar]
- 19.Sellors JW, Sankaranarayanan R. Lyon: IACR; 2003. Colposcopy and treatment of cervical intraepithelial neoplasia: A beginners’ manual. [Google Scholar]
- 20.Visual inspection with acetic acid for cervical cancer screening: Test qualities in a primary-care setting. University of Zimbabwe/JHPIEGO Cervical Cancer Project. Lancet. 1999;353:869–73. [PubMed] [Google Scholar]
- 21.Basu PS, Sankaranarayanan R, Mandal R, Roy C, Das P, Choudhury D, et al. Calcutta Cervical Cancer Early Detection Group. Visual inspection with acetic acid and cytology in the early detection of cervical neoplasia in Kolkata, India. Int J Gynecol Cancer. 2003;13:626–32. doi: 10.1046/j.1525-1438.2003.13394.x. [DOI] [PubMed] [Google Scholar]
- 22.Sauvaget C, Fayette JM, Muwonge R, Wesley R, Sankaranarayanan R. Accuracy of visual inspection with acetic acid for cervical cancer screening. Int J Gynaecol Obstet. 2011;113:14–24. doi: 10.1016/j.ijgo.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 23.Gaffikin L, Blumenthal PD, Emerson M, Limpaphayom K. Royal Thai College of Obstetricians and Gynaecologists (RTCOG)/JHPIEGO Corporation Cervical Cancer Prevention Group (corrected). Safety, acceptability, and feasibility of a single-visit approach to cervical-cancer prevention in rural Thailand: A demonstration project. Lancet. 2003;361:814–20. doi: 10.1016/s0140-6736(03)12707-9. [DOI] [PubMed] [Google Scholar]
- 24.Geneva, Switzerland: WHO Press; 2006. World Health Organization (WHO). Comprehensive Cervical Cancer Control: A Guide to Essential Practice. [PubMed] [Google Scholar]
- 25.Global Guidance for Cervical Cancer Prevention and Control. International Federation of Gynecology and Obstetrics (FIGO) 2009 [Google Scholar]


