Abstract
Background:
The conventional technique of ilioinguinal and iliohypogastric nerve block may be associated with drug toxicity, block failure and needs large drug volume. The ultrasound-guided (USG) nerve block enables accurate needle positioning that may reduce the chances of drug toxicity, drug dose and block failure.
Aim:
In this study, we compared the onset and duration of the motor and sensory nerve block, the drug volume required and time to rescue analgesic between USG and conventional technique.
Settings and Design:
Sixty male patients aged between 18 and 60 years, belonging to American society of Anesthesiology I-II, scheduled for inguinal hernia repair were enrolled in this prospective study and were randomly allocated into two groups of thirty each by computerized method.
Materials and Methods:
Group A patients received hernia block by conventional method using 0.75% ropivacaine 15 ml, and Group B patients were given the block guided by ultrasound using 0.75% ropivacaine, till the nerves were surrounded on all sides by the drug.
Statistical Analysis:
The data were analyzed using two independent sample t-tests for demographic and hemodynamic parameters. Nonparametric test (Mann-Whitney U-test) was used to find the significance between visual analog scale.
Results:
There was significantly early onset of sensory block in Group B 14.03 ± 2.82 min as compared to Group A 15.57 ± 1.52 min (P = 0.047). The onset of motor block was also earlier in Group B 19.40 ± 2.85 min as compared to Group A 20.67 ± 1.90 min. The time to rescue analgesia was more in Group B 7.22 ± 0.97 h as compared to Group A 6.80 ± 0.70 h (P = 0.062). The volume of drug required was less with ultrasound guided block.
Conclusions:
Ultrasound-guided hernia block thus has the advantage of early onset, less dose requirement and increase in time to rescue analgesia.
Keywords: Iliohypogastric, ilioinguinal, nerve block, ropivacaine, ultrasonography
INTRODUCTION
Ilioinguinal and iliohypogastric blocks have been routinely used as anesthetic technique for surgeries at the inguinal region like inguinal hernia and encysted hydrocoele and for lower abdominal surgeries. These blocks also help in the postoperative analgesia for cesarean section and lower abdominal surgeries.[1,2] The nerve block involves the blocking of ilioinguinal and iliohypogastric nerves in the plane between the transverses abdominis and internal oblique.
In the conventional block technique, the plane mentioned above is reached by the standard “click” felt while inserting the needle at this point. Since this is a blind technique, the plane between the transverses abdominis and internal oblique is often missed, and hence the drug can often enter in the wrong plane leading to inadequate action. Moreover, chance of bowel perforation and femoral block is high with the blind technique.
Ultrasonographic guided nerve blocks help by visually identifying the nerves to be blocked. The visual confirmation helps in accurately placing the drug and as the nerves are visualized the drug required is less.
Ultrasonographic guided ilioinguinal and iliohypogastric nerve blocks are of moderate level difficulty. It needs expertization in technique and accurate visualization of the nerves. The drug is placed by out-of-plane approach till the nerves are seen to be surrounded completely by the drug.
In this study, we compared the onset of sensory and motor block, the drug volume required and the duration of the block in both the above mentioned techniques in adult patients posted for elective hernia surgeries.
MATERIALS AND METHODS
After the approval of the Institutional Ethical Committee, this randomized prospective study was conducted in 60 male patients. Written informed and valid consent were taken. The patients were allocated randomly by computerized method into two groups of 30 each.
Inclusion criteria were male patients aged between 18 and 60 years, American Society of Anesthesiology I-II, scheduled for elective uncomplicated unilateral inguinal hernia repair.
Exclusion criteria were, patients who did not consent to the study, age ≤18 years and ≥60 years, large and irreducible hernia, body mass index ≥40 kg/m2, skin infection at the puncture site, allergy to local anesthetic agents, chronic hepatic or renal failure and preoperative opioid or nonsteroidal anti-inflammatory drug treatment for chronic pain.
All routine investigations were carried out, and fitness was confirmed. On the preoperative night, each patient received ranitidine tablet 150 mg, metoclopramide 10 mg tablet, diazepam 10 mg tablet orally. On the operative day, after confirming the nil by mouth status the patient was taken to operation theatre and intravenous (i.v.) fluid started. Necessary monitors were attached. All patients were premedicated with injection ondansetron 4 mg, injection midazolam 0.02 mg/kg and injection pentazocin 0.3 mg/kg i.v.
Conventional technique
All patients in Group A received ilioinguinal and iliohypogastric nerve blocks by conventional method using injection ropivacaine 0.75% 15 ml. The patient was placed supine on the operation table. The inguinal region was painted and draped. Then a 22G blunt 1.5 inch needle was inserted at 2 cm medially and 2 cm caudally to the anterior superior iliac spine (ASIS)[3] perpendicularly till a loss of resistance was felt. Then 5cc of injection ropivacaine 0.75% was infiltrated. After that needle was withdrawn till the skin and reinserted at 45° angle medially till loss of resistance was again felt and another 5cc injection ropivacaine was infiltrated at this plane. This procedure was repeated laterally. Thus, the total volume of 15 ml 0.75% of injection ropivacaine was used. The onset of motor and sensory block and the duration of block was recorded.
Ultrasound-guided technique
All patients in Group B received ilioinguinal and iliohypogastric block using ultrasonographic guidance. The patient was placed supine on the operation table, after preparation of the inguinal region sterile linear high frequency probe was placed between the iliac crest and costal margin (more cephalad than the usual location for ilioinguinal block). In this location, the ilioinguinal and iliohypogastric nerves in between the transverses abdominus and internal oblique are well defined Figure 1.[4] After visualization, a 22G 1.5 inch needle was used in out-of-plane approach to reach the nerves. After aspiration, 0.75% injection ropivacaine was injected till the nerves were surrounded on all sides by the drug (kayak sign). The volume required was recorded. The onset of motor and sensory block and the duration of block was recorded.
Figure 1.
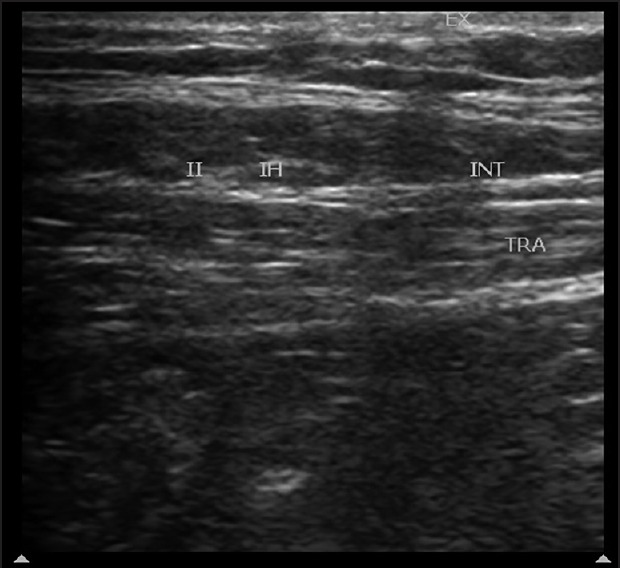
Ultrasonographic view of abdominal wall for ilioinguinal and iliohypogastric nerve block. II: Ilioinguinal nerve; IH: Iliohypogastric nerve; EX: External oblique muscle; INT: Internal oblique muscle; TRA: Transvesus abdominus
Patients of both the groups were given local skin infiltration and infiltration around the cord with injection ropivacaine up to 5 ml intraoperatively.
Motor and sensory blockade were assessed every 5 min till the onset of action that involves relaxation of lower abdominal muscles and sensory block by pin — prick. The duration of the block was assessed. Vitals were monitored every 15 min till the end of surgery. The visual analogue scale (VAS) recorded at 1st, 2nd, 4th, 6th, 8th h postoperatively for rescue analgesia.[5] Time to rescue analgesia was noted. At VAS score III when patient complained of first time pain postoperatively, we gave intramuscular injection diclofenac 1 mg/kg as rescue analgesia.
Visual analogue scale score:
Grade 0 (0-1): Good analgesia.
Grade I (1-4): Moderate analgesia.
Grade II (4-7): Mild analgesia.
Grade III (7-10): No analgesia.
RESULTS
Sixty male patients were studied as two groups of 30 each. Group A was given conventional and Group B was given ultrasound-guided (USG) ilioinguinal and iliohypogastric nerve block.
Two patients in Group A and one patient in Group B had inadequate action and had to be given general anesthesia.
The age of patients in Group A (42.03 ± 11.68) was comparable with that in Group B patients (40.07 ± 11.07, P = NS). As shown in Figure 2, mean basal values of systolic blood pressure (SBP) in both groups were comparable throughout the study except at 10th min. After block, where the difference in the SBP (P < 0.05) was statistically significant, but clinically not of much consequence.
Figure 2.
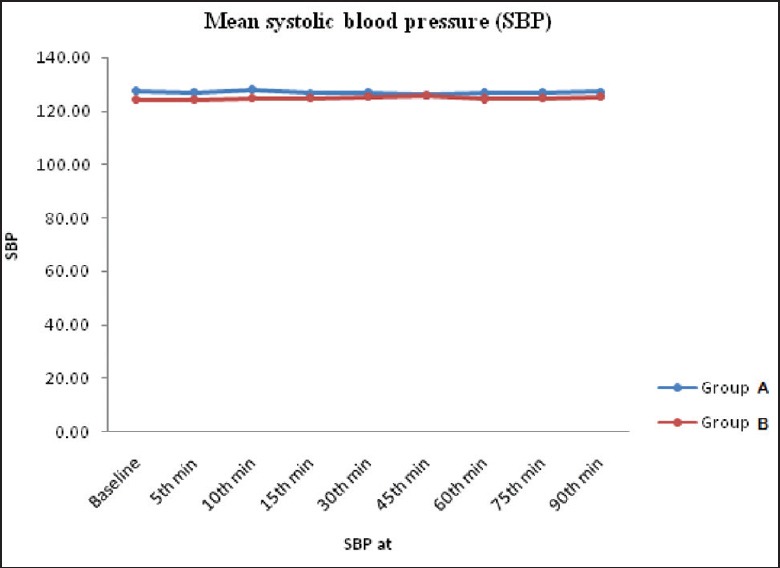
Comparison of systolic blood pressure
The diastolic blood pressure (DBP) and the pulse rate (PR) were comparable in both the groups throughout (P = NS).
We noted that in Group B patients required mean volume of 12.66 ± 1.24 ml of ropivacaine for adequate nerve surrounding and action. Thus, up to mean of 12.66 ml of drug was sufficient for block with the USG technique as compared to the conventional method that required more volume.
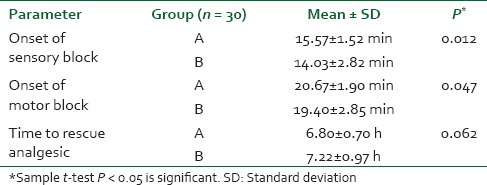
As shown in Table 1, there was significantly early onset of sensory block in Group B 14.03 ± 2.82 min as compared to Group A 15.57 ± 1.52 min (P = 0.047). The onset of motor block was also earlier in Group B 19.40 ± 2.85 min as compared to Group A 20.67 ± 1.90 min. The time to rescue analgesia was more in Group B 7.22 ± 0.97 h as compared to Group A 6.80 ± 0.70 h (P = 0.062).
Table 1.
Comparison of block profile
As shown in Figure 3, VAS score were comparable in both the groups. VAS score III at 6 h was noted in 12 patients of Group A and 6 patients in Group B. At VAS III, we gave rescue analgesia. We noted the time to rescue analgesia that was more in Group B 7.22 ± 0.97 h as compared to Group A 6.80 ± 0.70 h (P = 0.062).
Figure 3.
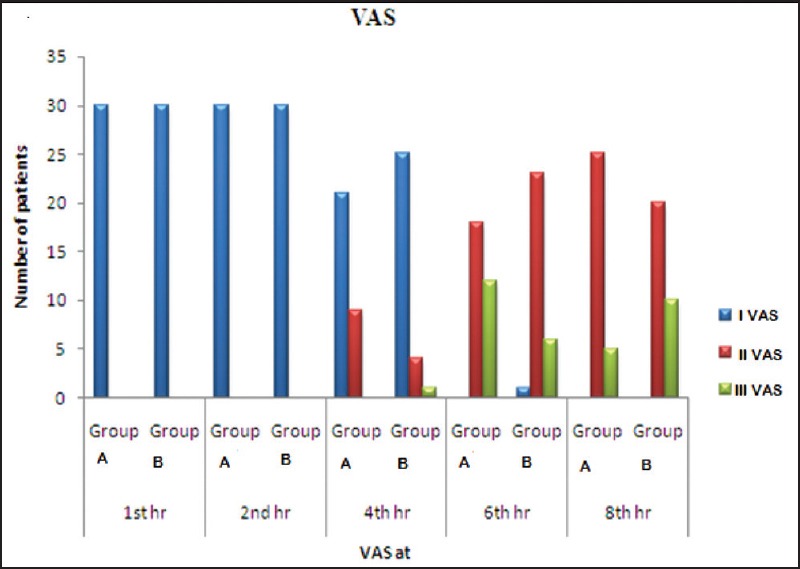
Comparison of visual analogue scale score
Power analysis
The study was conducted between March and August 2012. The population of surgery over this period was 150 patients. The sample size of the patients was calculated using population based formula. By exclusion and inclusion criteria and loss to follow-up, we divided the patients using simple computerized randomization in two independent groups. Power of the test for the onset of motor block is 0.74. Power of the test for the onset of sensory block is 0.83.
Statistical analysis
Data analysis was done using SPSS (Statistical Package for Social Science) version 17.0 (SPSS inc, Chicago, II, USA). We have used two independent sample t-tests to find the significance between two groups for age, onset of sensory, onset of motor block, time to rescue analgesia, PR, SBP and DBP.
Nonparametric test (Mann-Whitney U-test) was used to find the significance between VAS with respect to Group A and Group B. The statistical test was used at 5% level of significance. The P <0.05 was considered as significant.
DISCUSSION
An ilioinguinal and iliohypogastric nerve block seems to be a simple and straight forward technique based on surface anatomy and visible skin landmarks. But anatomic variation can be a source of frustration when nerve stimulation or surface landmarks are used for regional block. Several descriptions of the conventional technique have been published all of which are based on the subjective feeling of a “fascial click” when the needle pierces the deep fascia of the external oblique muscle. There is no agreement, however, about where the needle should be placed. One expert recommends starting 2 cm medial and 2 cm cephalad to the ASIS;[6] another recommends that the needle be inserted 2 in medial and 2 in inferior to the ASIS.[3] This inconclusiveness of recommendations about the block technique, somewhere medial from the ASIS, merely confirms the ambiguity in the nerve pathway. Conversely, the nerve passes consistently between the internal oblique and transverse muscles above the ASIS. Such a deep needle insertion seems dangerous for a routine peripheral nerve block because of the proximity to the abdominal cavity and intestines.
In reality, the courses of both the ilioinguinal and iliohypogastric nerves are consistent with those described in anatomy texts in only 41.8% of patients. The absence of one or both is estimated as high as 12.5%, whereas the rate of occurrence of an accessory ilioinguinal or iliohypogastric nerve is approximately 5%.[7]
Although the anatomic deviation could be overcome by giving a large-volume local anesthetic drug in a “fanlike” manner, visualization of applied anatomy seems to be more feasible, predictable, and safe. Ultrasonography is the only routinely available tool for real-time soft tissue imaging. Using an USG block technique, anatomical variations can be detected and accordingly the approach to block can be modified. It is important to develop the skill to accurately identify anomalies and understand their clinical implications.
In our study, we compared the conventional technique of ilioinguinal and iliohypogastric nerve block with ultrasonographic guided nerve block in 60 patients, with 30 in each group. We used injection ropivacaine 0.75% for the blocks. We compared the quality of the block, the onset of action, the drug volume required and the duration of the block in both the above mentioned techniques in adult patients posted for elective hernia surgeries.
We noted that in Group B patients required mean volume of 12.66 ± 1.24 ml of ropivacaine for surrounding the nerve. This volume was sufficient for block with the USG technique as compared to the conventional method that required more volume. We recorded the drug volume required to surround the nerves by directly visualizing under ultrasonography. So the drug toxicity by high volume used in a conventional technique was avoided. But the patient who receives lesser volume may require early rescue analgesia and chances of failure can be higher. In our study, one out of four patients in Group B who received 11 ml of drug had inadequate analgesia that may be because of less volume. It could also be due to the learning curve.
Recently, an unselective USG technique for ilioinguinal and iliohypogastric nerve blocks in children just medial to the ASIS was described by Willschke et al.[8] The authors could significantly reduce the volume of local anesthetic to achieve an appropriate block and the intra- and post-operative requirements for additional analgesics was significantly lower in the USG nerve block group compared with the traditional “blind” fascia click method.
The pharmacokinetic data indicate faster absorption and higher maximal plasma concentration of local anesthetic drug when ultrasound was used as a guidance technique for ilioinguinal nerve block (INB) compared with the landmark-based technique. Thus, a reduction of the volume of local anesthetic should be considered when using an USG technique for INB.[9]
In our study, we found the onset of sensory block in Group B was earlier 14.03 ± 2.28 min as compared to Group A 15.57 ± 1.52 min (P = 0.012). The onset of motor block was also earlier in Group B 19.40 ± 2.85 min than Group A 20.67 ± 1.90 min (P = 0.047).
We noted the time to rescue analgesia that was more in Group B 7.22 ± 0.97 h as compared to Group A 6.80 ± 0.70 h. VAS score III, at 6 h was noted in 12 patients of Group A and 6 patients in Group B. At VAS score III postoperatively we gave intramuscular injection diclofenac 1 mg/kg as rescue analgesia.
Recently Aveline et al.,[10] have compared USG transversus abdominis plane (TAP) block and conventional ilioinguinal/iliohypogastric nerve block in day care open hernia repair in 273 patients. They found that patients who received TAP block expressed significantly less pain at rest on VAS score at 4, 12 and 24 h. The postoperative morphine requirement in first 24 h was also less in TAP group.
No complications were seen in our study, but there are chances of complications like extension of the block to the femoral nerve,[11] trauma to blood vessels,[12] urinary retention or puncture of intraperitoneal viscera.[13,14] The use of ultrasound may also reduce these risks. Overall, the block action was inadequate in three patients.
Limitations
More number of patients need to be given USG hernia blocks to improve our expertise and get more appropriate results. Availability of the ultrasound machine itself could be a problem.
CONCLUSION
Ultrasound-guided ilioinguinal and iliohypogastric nerve block was found to have early onset of sensory and motor block with less dose requirement. The time to rescue analgesia was also prolonged as compared to the conventional method. This technique could be a boon in patients where neuraxial block is detrimental, like those with heart disease and a poor cardiopulmonary status.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.McDonnell JG, Curley G, Carney J, Benton A, Costello J, Maharaj CH, et al. The analgesic efficacy of transverses abdominis plane block after caesarean delivery: A randomized controlled trial. Anesth Analg. 2008;106:186–91. doi: 10.1213/01.ane.0000290294.64090.f3. [DOI] [PubMed] [Google Scholar]
- 2.Gofeld M, Christakis M. Sonographically guided ilioinguinal nerve block. J Ultrasound Med. 2006;25:1571–5. doi: 10.7863/jum.2006.25.12.1571. [DOI] [PubMed] [Google Scholar]
- 3.Waldman SD. 2nd ed. Philadelphia: WB Saunders Co; 2000. Atlas of Pain Management Injection Techniques. [Google Scholar]
- 4.Eichenberger U, Greher M, Kirchmair L, Curatolo M, Moriggl B. Ultrasound-guided blocks of the ilioinguinal and iliohypogastric nerve: Accuracy of a selective new technique confirmed by anatomical dissection. Br J Anaesth. 2006;97:238–43. doi: 10.1093/bja/ael103. [DOI] [PubMed] [Google Scholar]
- 5.Sivapurapu V, Vasudevan A, Gupta S, Badhe AS. Comparison of analgesic efficacy of transversus abdominis plane block with direct infiltration of local anesthetic into surgical incision in lower abdominal gynecological surgeries. J Anaesthesiol Clin Pharmacol. 2013;29:71–5. doi: 10.4103/0970-9185.105807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reynolds L, Kedlaya D. 2nd ed. Philadelphia: WB Saunders Co; 2001. Interventional Pain Management; pp. 508–11. [Google Scholar]
- 7.Al-Dabbagh AK. Anatomical variations of the inguinal nerves and risks of injury in 110 hernia repairs. Surg Radiol Anat. 2002;24:102–7. doi: 10.1007/s00276-002-0006-9. [DOI] [PubMed] [Google Scholar]
- 8.Willschke H, Marhofer P, Bösenberg A, Johnston S, Wanzel O, Cox SG, et al. Ultrasonography for ilioinguinal/iliohypogastric nerve blocks in children. Br J Anaesth. 2005;95:226–30. doi: 10.1093/bja/aei157. [DOI] [PubMed] [Google Scholar]
- 9.Weintraud M, Lundblad M, Kettner SC, Willschke H, Kapral S, Lönnqvist PA, et al. Ultrasound versus landmark-based technique for ilioinguinal-iliohypogastric nerve blockade in children: The implications on plasma levels of ropivacaine. Anesth Analg. 2009;108:1488–92. doi: 10.1213/ane.0b013e31819cb1f3. [DOI] [PubMed] [Google Scholar]
- 10.Aveline C, Le Hetet H, Le Roux A, Vautier P, Cognet F, Vinet E, et al. Comparison between ultrasound-guided transversus abdominis plane and conventional ilioinguinal/iliohypogastric nerve blocks for day-case open inguinal hernia repair. Br J Anaesth. 2011;106:380–6. doi: 10.1093/bja/aeq363. [DOI] [PubMed] [Google Scholar]
- 11.Lipp AK, Woodcock J, Hensman B, Wilkinson K. Leg weakness is a complication of ilio-inguinal nerve block in children. Br J Anaesth. 2004;92:273–4. doi: 10.1093/bja/aeh045. [DOI] [PubMed] [Google Scholar]
- 12.Vaisman J. Pelvic hematoma after an ilioinguinal nerve block for orchialgia. Anesth Analg. 2001;92:1048–9. doi: 10.1097/00000539-200104000-00045. [DOI] [PubMed] [Google Scholar]
- 13.Jöhr M, Sossai R. Colonic puncture during ilioinguinal nerve block in a child. Anesth Analg. 1999;88:1051–2. doi: 10.1097/00000539-199905000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Amory C, Mariscal A, Guyot E, Chauvet P, Leon A, Poli-Merol ML. Is ilioinguinal/iliohypogastric nerve block always totally safe in children? Paediatr Anaesth. 2003;13:164–6. doi: 10.1046/j.1460-9592.2003.01005.x. [DOI] [PubMed] [Google Scholar]


