Abstract
Treatment for cancer among adolescents is often more intense and lasts longer than treatment for older or younger patients. It typically causes pain, fatigue, and nausea and affects social and emotional well-being. This study examined the relationships among demographics, physical symptoms, perceived social support from friends and family, and affect (positive and negative) in 102 adolescents (age 13–19) with cancer using correlational analyses. Additionally, perceived social support was explored as a mediator and moderator of the relationship between physical symptoms and affect using regression. Females reported significantly lower friend support and higher negative affect compared to males. Minority participants were more likely to endorse physical symptoms and less negative affect compared to White respondents. Higher report of physical symptoms was significantly related to greater negative affect, whereas higher perceived social support from friends was related to higher positive affect. Adolescents consistently reported high levels of social support from family and friends. Additionally, adolescents tended to report average levels of positive affect and low levels of negative affect compared to healthy populations. No significant mediation or moderation effects were found. This research highlights that females and minorities, and those with greater physical symptoms, may be more vulnerable to poor adjustment to cancer during adolescence. However, overall this study lends support to the notion that adolescents with cancer are an especially resilient population, as these patients endorsed generally high levels of social support and positive affect, with low levels of negative affect.
Keywords: adolescent, oncology, social support, affect, cancer
Treatment for adolescent cancer is often more intense, longer, and associated with greater morbidities and increased risk of adverse psychological outcomes than younger patients (National Cancer Institute [NCI] & Live-STRONG, 2006). Reasons for this include the fact that adolescence is generally a time of increased mood disturbances that may be exacerbated by cancer and its treatment, especially the use of steroids, and a diagnosis of cancer during adolescence may interrupt typical adolescent developmental milestones such as individuation from parents and social and educational development (Manne & Miller, 1998; Schwartz, Kazak, & Mougianis, 2009). Although evidence suggests a relationship between cancer-related morbidities and affect in adult populations (Knotkova, Clark, Mokrejs, Padour, & Kuhl, 2004; Pinquart, Frohlich, & Silbereisen, 2007), little research has examined this relationship in adolescents with cancer. Furthermore, the relationship of social support to these variables, a critical construct for adolescents who are individuating from parents and developing intimate friendships, has not been explored.
Cancer treatments include chemotherapy, surgery, radiation therapy, hematopoeitic transplantation, and additional experimental therapies. These treatments vary in intensity, invasiveness, and severity and may cause a range of side effects (American Cancer Society, 2010). Physical side effects include hair loss, infection, pain, fatigue, vomiting, nausea, poor appetite, weight changes, seizures, and muscositis (Cavusoglu, 2000; Hockenberry, 2004; Ruland, Hamilton, & Schjodt-Osmo, 2009). Hockenberry (2004) concluded that the most distressing physical symptoms from cancer treatment in children were nausea, fatigue, and pain, which are the focus of this study. These symptoms are common among adolescent patients (Ljungman, Gordh, Sörensen, & Kreuger, 1999; Ullrich et al., 2010) and may cause further disruptions throughout treatment, including sleep disturbance (Jacob, Hesselgrave, Sambuco, & Hockenberry, 2007), failure to maintain an adequate diet during treatment (Green, Horn, & Erickson, 2010), increased distress, and diminished quality of life (Chiang, Yeh, Wang, & Yang, 2009).
Psychological difficulties reported by pediatric samples are marked by increases in negative affect (i.e., mood states), including mood changes, increased anger (Ruland et al., 2009), and anxiety (Cavusoglu, 2000) and may be related to physical symptoms. Although previous studies have demonstrated the relationship between perceived symptoms and affect in adult cancer populations (Knotkova et al., 2004; Pinquart et al., 2007), less research has focused on this relationship in pediatric patients with cancer. One study (LeBaron & Zeltzer, 1984) found that children and adolescents reported experiencing anxiety and distress prior to painful treatment procedures, and those who experienced more pain reported higher anxiety. Unfortunately, most studies have focused on negative affect, while neglecting positive affect. It has been shown that components of positive and negative affect predict overall psychological adjustment to cancer (Pinquart et al., 2007). It is important that positive affect be examined independently in adolescents with cancer given that many adjust well to diagnosis and treatment (Woodgate, 1999a, 1999b; Wallace, Harcourt, Rumsey, & Foot, 2007). Furthermore, although once thought to be opposite ends of the same spectrum, positive and negative affect have emerged as independent constructs that may coexist simultaneously and thus need to be examined separately, from a methodological standpoint (Moskowitz, Epel, & Acree, 2008).
Pediatric patients with cancer may also experience adverse social difficulties due to isolation during hospitalizations, stigma, lack of interest in friendships (Ruland et al., 2009), and frequent absences from school (Cavusoglu, 2000). Thus, not surprisingly, perceived social support has been implicated as a protective factor against negative affect in pediatric cancer populations (Manne & Miller, 1998; Varni & Katz, 1997). Social support may protect pediatric patients against the negative impact of the stressors and symptoms associated with cancer (Corey, Haase, Azzouz, & Monahan, 2008; Trask et al., 2003), especially when the relationships are particularly close (Decker, 2007). The most common reported sources of social support are the patient’s family and friends (Trask et al., 2003; Woodgate, 2006). The degree of support from parents is high across children and adolescents with cancer (Barrera, Andrews, Burnes, & Atenafu, 2007). Adolescents report better psychological adjustment to cancer treatment when they receive a higher degree of understanding and support from their parents (Williamson, Harcourt, Halliwell, Frith, & Wallace, 2010). Although support from family seems necessary toward fostering healthy adjustment to cancer, the potential for parent-child conflict in this population (Manne & Miller, 1998; Patenaude & Kupst, 2005) suggests that considering support from peers is needed as well.
Friends serve as another major source of emotional support for adolescents facing cancer (Trask et al., 2003), and adolescents rely more on social support from their friends compared to younger children (Barrera et al., 2007). Ritchie (2001) suggests that good peer relationships help an adolescent to regain normalcy in other aspects of life, which may help an adolescent feel less helpless and thus more able to manage the disease. Although peer support during an illness has positive benefits, adolescents with cancer tend to be more isolated as a result of hospitalizations and missed school, which contributes to strained relationships and inconsistent peer support throughout the duration of treatment (Cavusoglu, 2000). Moreover, patients are unable to participate in group activities, which affects the quality of their friendships and threatens their sense of normalcy (Ben-Ari, 2011). This study will examine the protective role of perceived support from friends and family in relation to physical symptoms and affect of adolescents with cancer.
In summary, cancer often relates to physical symptoms such as pain, fatigue, and nausea and may also relate to changes in affect and social well-being. Such an impact of cancer may be especially salient to adolescents who experience more cancer-related morbidity and, in general, experience more changes in mood and social networks than younger children (Fleming & Offord, 1990; NCI & LiveSTRONG, 2006; Schwartz et al., 2009). However, very little research has focused exclusively on adolescents on active cancer treatment, in general (Bellizzi et al., 2012; Ben-Ari, 2011), or on the relationships of physical symptoms, affect, and perceived social support, in particular. Additionally, the majority of studies examining psychological adjustment to cancer treatment have focused on aspects of negative affect, despite the importance of considering positive affect as a separate construct from negative affect and given its potential to be a marker of resiliency. Thus, the first aim of this study was to examine the relationships between physical symptoms, positive and negative affect, and perceived social support among adolescent patients on active treatment. It was expected that lower pain, fatigue, and nausea would be associated with higher positive affect and lower negative affect. It was also expected that higher perceived social support from friends and family would be associated with lower pain, fatigue, and nausea, higher positive affect, and lower negative affect. As a second aim, the potential role of social support as a mediator or moderator (i.e., a protective factor) between the relationship of physical symptoms and affect in adolescents with cancer was examined (see Figure 1). This analysis controlled for demographic characteristics (Draguns & Tanaka-Matsumi, 2003; Li, DiGiuseppe, & Froh, 2006), life events (Grant & Compas, 1995), and family functioning (Alderfer, Navsaria, & Kazak, 2009; Edwards & Clark, 2004; Ozono et al., 2010), if found to relate to negative or positive affect, given their demonstrated and theoretical impact on affect. The hypothesis was that higher physical symptoms would be less likely to relate to greater negative affect or lower positive affect in the presence of greater perceived social support. An exploratory aim was to examine the relationships of demographic factors and control variables with physical symptoms, perceived social support, and affect.
FIGURE 1.
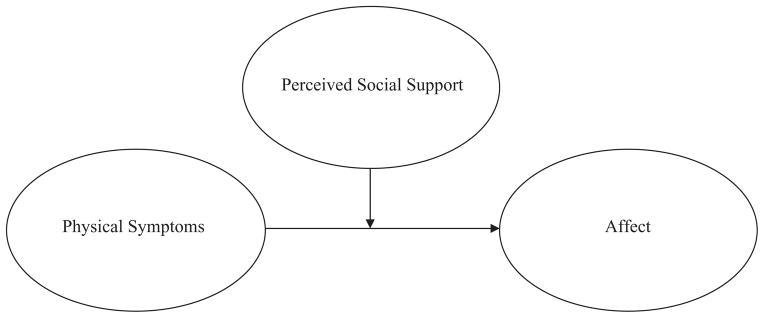
Moderation model.
METHOD
Participants
Adolescents age 13 to 19 (M = 15.59) currently undergoing cancer treatment in a large urban children’s hospital in the northeast participated in this study as part of a larger investigation on psychosocial responses to cancer treatment. Of 133 potential participants, 123 agreed to participate and completed the consent process. Complete data were obtained from 102 participants. The study excluded participants if they had significant cognitive delay as determined by the medical staff. Participants were eligible to participate in the study if they were undergoing treatment for cancer and were at least one month past diagnosis. Participants were required to read and speak English in addition to having a parent who could read and speak English sufficiently to give informed consent and complete surveys. The majority of the sample (54.9%) identified as male; 58% of the participants identified as White, 20% as African American, 6% as Asian, 6% as Hispanic, 1% as Pacific Islander, and 5% as more than one race. Participants were an average of 20.7 months since diagnosis (range 1–196 months; see Table 1) and 25.5% of the participants endorsed having at least one cancer recurrence.
TABLE 1.
Descriptive Data
| Category | Minimum | Maximum | M (SD) | Mean Log score (SD) |
|---|---|---|---|---|
| Age | 13 | 19 | 15.59 (1.80) | |
| Time since diagnosis (months) | 1 | 196 | 20.7 (37.43) | |
| Fatigue | 0 | 100 | 58.17 (28.93) | |
| Nausea | 0 | 100 | 64.80 (18.52) | |
| Pain | 0 | 100 | 56.20 (23.24) | |
| Family support | 1 | 20 | 14.46 (4.72) | .68 (.38) |
| Friend support | 1 | 20 | 15.16 (4.10) | .65 (.34) |
| Positive affect | 10 | 50 | 32.19 (8.34) | |
| Negative affect | 10 | 47 | 20.85 (7.60) | 1.29 (.15) |
| Family functioning | 1.00 | 3.42 | 1.90 (0.43) | |
| Stressful events | −95.00 | 99.00 | 29.19 (28.50) |
Note: Perceived Social Support-Family Scale and the Perceived Social Support-Friends Scale, and negative affect were transformed due to non-normal distributions.
Procedure
Potential participants were identified by the researchers through oncology clinic schedules and in-patient rosters. A research assistant or the principal investigator (LS) met with each identified family in clinic or in the hospital room to inform potential participants of the study. If they agreed to participate, the participants and parents completed informed consent and assent (for patients younger than age 18). Next, participants were asked to complete a packet of questionnaires and to return them in person or by mail using a prestamped envelope provided to them. Participants were compensated for their time. This study was approved by the hospital’s Institutional Review Board.
Measures
Demographic Measures
Parents of participants completed a demographics questionnaire that inquired about the participant’s gender, age, ethnicity, time since initial cancer diagnosis, and number of cancer recurrences.
Physical Symptoms
Physical symptoms were measured with the Pediatric Quality of Life Inventory (PedsQL) Cancer Module (Nausea and Pain subscales; Varni et al., 1998) and Multidimensional Fatigue Scale (Varni, Burwinkle, Katz, Meeske, & Dickinson, 2002). The PedsQL utilizes a 5-point Likert-type scale (0 = never a problem to 4 = Almost always a problem). Items are then reverse scored and standardized on a 100-point scale (0 = 100 to 4 = 0). Lower scores indicate more reported symptoms. The Nausea subscale consists of five items. An example from this subscale includes “I feel too sick to my stomach to eat.” The average score in the normative sample of pediatric patients with cancer was 75.81 (Varni et al., 2002). The reliability in this sample was α = .83. The Pain subscale of the PedsQL Cancer Module consists of two items. An example item from this subscale is “I hurt a lot.” The average score in the standardization sample of pediatric patients with cancer was 76.20. The reliability within this sample was α = .84. The Multidimensional Fatigue Scale is an 18-item self-report measure that assesses three domains of fatigue: general fatigue (six items; e.g., “I feel too tired to do things that I like to do”); sleep/rest fatigue (six items; e.g., “I sleep a lot”); and cognitive fatigue (six items; e.g., “It is hard for me to think quickly”). These subscales were combined to yield a total fatigue score. The average on this measure in the normative sample of pediatric oncology patients was 70.98 (Varni et al., 2002). The reliability in this sample was α = .91. The standardized total scores of pain, fatigue, and nausea were also averaged to yield one total score of physical symptoms to avoid multicolinearity (assuming these variables would be highly correlated) and maximize power in regression analyses testing the potential interaction of symptoms and social support on affect.
Perceived Social Support
Perceived social support was measured using the Perceived Social Support-Family Scale (PSS-Fa) and the Perceived Social Support-Friends Scale (PSS-Fr), which assesses perceived support received by the respondent from each social group (Procidano & Heller, 1983). Both scales consist of 20 self-report items measured on a 5-point Likert-type scale (1 = strongly disagree to 5 = strongly agree). Examples from these measures include “My family is sensitive to my personal needs,” and “My friends give me the moral support that I need.” Higher scores signify a greater level of perceived social support. The average scores on these scales in the standardization samples were 15.2 for perceived support from friends and 13.4 for perceived support from family (Procidano & Heller, 1983). The reliability of the PSS-Fa and PSS-Fr within this sample were α = .87 and α = .85, respectively.
Positive and Negative Affect
Positive and negative affect were measured using the Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988). The PANAS is a 20-item measure consisting of two subscales: positive affect (e.g., “Excited” and “Inspired”) and negative affect (e.g., “Guilty” and “Hostile/Angry”). Participants used a 5-point Likert-type scale to indicate how much a specific description is characteristic of them (1 = very slightly or not at all to 5 = extremely). High scores on the sub-scales indicate a greater experience of positive and negative affect. The average scores in the standardization sample were 32.0 and 14.0 for positive affect and negative affect, respectively (Crawford & Henry, 2004). Reliability within this sample for the positive and negative affect scales were α = .89 and α = .89, respectively.
Stressful Life Events
Stressful life events were measured with the Adolescent Perceived Events Scale (APES; Compas, Davis, Forsythe, & Wagner, 1987). The APES is a 90-item measure consisting of daily stressors and major life events, to which the respondent indicates whether it happened in the past 4 months and rates the desirability of the event on a 9-point Likert-type scale (−4 = extremely bad to 4 = extremely good). The total ratings of the desirability of events by the adolescents were used for subsequent analyses. Higher scores equate to a more desirable perception of events. Example items from this measure include “Death of a family member,” and “Doing poorly on an exam.” Compas, Howell, Phares Williams, and Giunta (1989) reported an average score of 47.2.
Family functioning
Family functioning was measured with the 12-item General Functioning Scale of the Family Assessment Device (FAD; Epstein, Baldwin, & Bishop, 1983). Items are rated on a 4-point Likert-type scale (1 = strongly agree to 4 = strongly disagree). An example item from this scale is “In times of crisis we can turn to each other for support.” Responses are coded and averaged, with higher scores indicating poorer family functioning. The average score within Kabacoff, Miller, Bishop, Epstein, and Keitner’s (1990) standardization sample was 1.8. The reliability within this sample was α = .84.
Statistical Analyses
A power analysis was conducted based on the expectation of a small to medium effect size. A priori calculations using an alpha level of .05, five predictors in the regression, a power of .80, and a medium effect size suggested that 91 participants would be needed for this study. Descriptive statistics were calculated for all variables and transformations to correct for non-normal distributions were used as needed. To determine the relationships between physical symptoms, perceived social support and affect (Aim 1), in addition to examining potential relationships between these variables and age, time since diagnosis, family functioning, and stressful life events (exploratory analyses), correlational analyses were conducted. t Tests were used to examine the relationship of gender and minority status to symptoms, affect, and social support. To test the role of perceived social support as a moderator of the relationship between physical symptoms and affect (Aim 2), a multiple regression was conducted. Demographic and potential covariates related to negative or positive affect were entered into the first step of the regression to control for these confounding factors. Perceived social support from family and friends and physical symptoms (pain, nausea, and fatigue) were centered and entered next. Interaction variables were computed by multiplying the centered predictors with the centered moderators and mediators and were entered next. A total of four regression analyses were planned: two each for negative and positive affect while accounting for perceived social support from friends and from family separately.
RESULTS
Descriptive Analyses
Mean scores are reported in Table 1. Relative to normative scores reported in prior samples, this sample demonstrated higher endorsement of physical symptoms, average levels of perceived social support, positive affect, negative affect, and family functioning, and a higher number of negative life events. Descriptive analyses revealed that perceived social support from family and friends was negatively skewed in that the majority of the sample reported a high level of social support from friends and family. Negative affect exhibited a positive skew in that the majority of the sample reported lower levels of negative affect. Therefore, a logarithmic (log10) correction was used to create a normative distribution for each variable, which were used for all subsequent analyses.
Correlations Testing the Relationships Among Physical Symptoms, Social Support, and Affect
Physical symptoms were significantly related to positive and negative affect such that adolescents who reported fewer symptoms also reported higher positive affect and lower negative affect (see Table 2). In particular, pain, fatigue, and nausea related to negative affect. Only fatigue related to positive affect. However, physical symptoms were not significantly related to perceived social support from friends or family. Perceived social support from friends was not related to negative affect but was related to positive affect, such that adolescents who reported higher friend support also reported higher positive affect. Perceived social support from family was not significantly related to positive or negative affect. As perceived social support from family was not related to affect, it was excluded from regression analyses testing the interaction of social support and symptoms on affect.
TABLE 2.
Correlations Among Physical Symptoms, Social Support, and Affect
| Pain | Fatigue | Nausea | Family Support | Friend Support | Positive Affect | Negative Affect | |
|---|---|---|---|---|---|---|---|
| Pain | — | .62** | .33** | −.14 | −.10 | .03 | −.39** |
| Fatigue | — | .47** | .04 | .02 | .26** | −.49** | |
| Nausea | — | −01 | −.03 | .03 | −.33** | ||
| Family Support | — | .28** | .10 | −.09 | |||
| Friend Support | — | **.26 | .12 | ||||
| Positive Affect | — | −.05 | |||||
| Negative Affect | — | ||||||
| Symptoms | — | — | — | −.05 | .06 | .22* | .48** |
p < .05;
p < .01.
Correlations Testing the Relationship of Demographics, Life Events, and Family Functioning with Physical Symptoms, Social Support, and Affect
There were several significant findings with regards to demographics (see Table 3). Older age was related to a higher positive affect. Females were more likely to report higher negative affect and lower perceived social support from friends. White participants were likely to report more negative affect, but less total physical symptoms and nausea relative to minorities. Negative ratings of stressful life events related to more fatigue, more perceived social support from friends, more negative affect, and less positive affect. Poorer family functioning related to higher positive affect and higher perceived social support from friends and from family.
TABLE 3.
Correlations of Demographics, Life Events, and Family Functioning with Symptoms, Social Support, and Affect
| Age r | Gender t | Minority Status t | Stressful Life Events r | Family Functioning R | |
|---|---|---|---|---|---|
| Pain | −.04 | 1.06 | −1.01 | .12 | .10 |
| Fatigue | −.11 | 1.10 | .30 | .24* | −.13 |
| Nausea | −.01 | −.31 | −2.84* | −.00 | −.00 |
| Physical symptoms | −.06 | .65 | −1.94* | −.07 | .00 |
| Family support | .19 | .88 | .98 | −.23 | .50** |
| Friend support | .09 | 2.66** | .74 | −.24** | .17* |
| Positive affect | .21* | −.50 | .03 | .25** | −.17* |
| Negative affect | .095 | −2.62** | −2.00* | −.22** | .12 |
Note: Pain, fatigue, nausea, physical symptoms, family support, friend support, and positive affect each have a positive valence; negative affect, stressful life events, and family functioning each have a negative valence.
p < .05;
p < .01.
Regressions Testing the Influence of the Interaction of Social Support and Physical Symptoms on Affect
Separate regression analyses were conducted to examine the roles of physical symptoms and perceived social support from friends, and the interaction of the two, in predicting positive and negative affect (see Table 4). The first hierarchical multiple regression analysis examined predictors of negative affect. The first step of the regression controlled for gender, minority status, and stressful life events because they were significantly correlated with negative affect. The second step of the analysis included the predictor variables of physical symptoms and perceived social support from friends. In line with Aiken and West’s (1991) guidelines for conducting moderation analyses, interaction terms for physical symptoms by perceived social support were added to the final step of the regression. Physical symptoms were a significant predictor of negative affect (p = .00) after controlling for gender, minority status, and life events. No other predictors remained significant in the model, including perceived social support from friends and the interaction term. The second hierarchical multiple regression analysis examined predictors of positive affect. The first step of the regression controlled for age, family functioning, and stressful life events because they were significantly correlated with the positive affect. The second step of the analysis included the predictor variables of physical symptoms and perceived social support from friends. The interaction term of Physical Symptoms by Social Support was added to the final step of the regression. Perceived social support from friends remained a significant predictor of positive affect after controlling for life events, age, and family functioning (p = .01). Family functioning and age were also significantly related to positive affect (p = .01 and p = .04, respectively). No other predictors, including physical symptoms or the interaction term were significant.
TABLE 4.
Regression Analyses for Positive and Negative Affect
| Regression | β | df | R2 | ΔR2 | F | p value |
|---|---|---|---|---|---|---|
| Negative affect | .05 | .05 | .18 | |||
| Step 1: Control | 99 | 1.68 | ||||
| Gender | .16 | .12 | ||||
| Minority status | .05 | .59 | ||||
| Negative events | .14 | .18 | ||||
| Step 2: Main effects | 99 | .28 | .23 | 7.20 | .00 | |
| Gender | .10 | .25 | ||||
| Minority status | .12 | .20 | ||||
| Negative events | .12 | .19 | ||||
| Friend support | −.08 | .39 | ||||
| Physical symptoms | −.47 | .00 | ||||
| Step 3: Interaction | 99 | .29 | .01 | 5.72 | .00 | |
| Gender | .10 | .28 | ||||
| Minority status | .11 | .23 | ||||
| Negative events | .11 | .23 | ||||
| Friend support | −.04 | .71 | ||||
| Physical symptoms | −.47 | .00 | ||||
| Friend Support * | .12 | .22 | ||||
| Physical Symptoms | ||||||
| Positive affect | 98 | .15 | .15 | 5.61 | .00 | |
| Step 1: Control | ||||||
| Age | .20 | .04 | ||||
| Family functioning | −.32 | .00 | ||||
| Negative events | .08 | .38 | ||||
| Step 2: Main effects | 98 | .24 | .09 | 5.71 | .00 | |
| Age | .19 | .04 | ||||
| Family functioning | −.25 | .01 | ||||
| Negative events | .09 | .34 | ||||
| Friend support | .27 | .01 | ||||
| Physical symptoms | .14 | .13 | ||||
| Step 3: Interaction | 98 | .24 | .00 | 4.76 | .00 | |
| Age | .19 | .04 | ||||
| Family functioning | −.24 | .01 | ||||
| Negative events | .09 | .32 | ||||
| Friend support | .30 | .01 | ||||
| Physical symptoms | .14 | .14 | ||||
| Friend Support * | −.05 | .61 | ||||
| Physical Symptoms |
DISCUSSION
This study illustrated the relationships among physical symptoms, perceived social support, and affect in adolescent patients on active treatment. Despite cancer-related morbidity experienced by the adolescents, they reported average levels of positive and negative affect. This indicates that adolescents on active cancer treatment are reporting that they are coping relatively well in the face of adversity. Notably, patients with a greater number of physical symptoms reported higher amounts of negative affect, which is consistent with previous findings with adult cancer patients (Knotkova et al., 2004; Pinquart et al., 2007). Contrary to previous findings (Pinquart et al., 2007), having fewer physical symptoms was not related to positive affect. This could be due to the report of high levels of positive affect across the sample, lending support to the resilience of this population (Woodgate, 1999b).
Consistent with previous literature, adolescents in this study reported high levels of social support from friends and family (Barrera et al., 2007). Surprisingly, perceived social support from the family was not related to physical symptoms or affect. This is contrary to previous findings in which low social support from families was predictive of negative affect (Corey et al., 2008). Similarly, perceived social support from friends was not related to physical symptoms. This may be due to skewed distribution in the scores, as most adolescents in the sample reported high levels of perceived support from the family and friends.
Perceived social support from friends was related to positive affect, suggesting that friends may help to foster “normalcy” and increase positive feelings. Additionally, if an individual is feeling more positive affect, he or she may be more willing to engage with peers. However, perceived social support was not directly related to negative affect, which is contrary to some previous findings (Varni & Katz, 1997), but consistent with Manne and Miller (1998). This finding could reflect the bias in the literature to report only significant results relating to negative affect. Overall, the results of this study strengthen the conclusion that perceived peer support is not related to negative affect but is related to positive affect.
There were several significant findings with respect to demographic variables examined in this study. First, two significant differences were found with gender in that female patients endorsed significantly lower perceived social support from friends and higher levels of negative affect. In general, female adolescents experience more distress due to social difficulties (Oldehinkel, Rosmalen, Veenstra, Dijkstra, & Ormel, 2007) and report higher levels of depression compared to males (Li et al., 2006). That older age was related to more positive affect may reflect greater cognitive maturity to maintain a positive attitude or find meaning in the experience, or it may also be due to greater autonomy and flexibility later in adolescence compared to early to midadolescence. Differences were also found with regards to race/ethnicity in that White participants reported greater levels of negative affect whereas minority participants reported suffering from significantly more nausea. Cultural context may influence the expression of somatic and psychological symptoms (Draguns & Tanaka-Matsumi, 2003), whereby some minorities may find it more acceptable to report physical problems compared to psychological problems. For example, Ryder et al. (2008) found that Whites were more likely to report psychological symptoms of depression whereas minorities were more likely to report physical symptoms, concluding that the same diagnosis could appear differently across cultures. Culture dictates what is “normal” versus “abnormal”; therefore, one may not endorse a specific symptom, as their culture may not consider that symptom to be abnormal (Draguns & Tanaka-Matsumi, 2003). These findings warrant further investigation of the relationship of ethnicity of adolescents with cancer to physical symptoms.
Adolescents’ perception of life events and family functioning also related to the variables of interest. The report of negative life events being related to higher report of fatigue, negative affect, and perceived social support from friends, and lower levels of positive affect indicates that other life events, in addition to cancer, may strongly affect adolescent well-being and perceived support. Poorer family functioning also was related to higher perceived social support from friends and family, indicating that another stressor could elicit the need for support.
The first regression found that physical symptoms were associated with negative affect, even after accounting for perceived social support from peers, family functioning, and stressful life events. The lack of a significant interaction indicates that social support may not protect against the detrimental effects of physical symptoms. Therefore, it is important for physical symptoms to be managed to protect an individual from experiencing negative emotional states. The second regression found that perceived social support from peers and family functioning were significant predictors of positive affect, though no other predictors including the interaction term were significant. This suggests that worse family functioning and greater support from friends relate to higher experience of positive emotions, regardless of level of physical symptoms.
Several limitations of this study should be considered when viewing the results. First, this study examined adolescents on active cancer treatment and thus may not generalize to other populations. Several variables, specifically negative affect and perceived social support from friends and family, resulted in a skewed response curve suggesting that the sample is functioning well, as there was a floor effect for negative affect (participants reported low levels of negative affect) and a ceiling effect for social support (indicating that participants overall felt well supported by their family and friends). Finally, no significant moderation interactions were found. This again may be due to the restriction in the variability of scores in the sample and resilience within the sample of adolescents included in this study.
Clinical Implications of the Study
The results of this study indicate that, overall, adolescents on active cancer treatment are functioning well psychologically, as indicated by high levels of positive affect and low levels of negative affect. However, their functioning is impacted by experience of physical symptoms and perceived social support. This study stresses the importance of managing physical symptoms and of adolescents maintaining ample peer support to reduce negative psychological symptoms and foster optimal adjustment while on active cancer treatment. When assessing these outcomes and developing interventions, it should be considered that females may be more vulnerable to more negative affect and reduced peer support, and Whites and minorities may respond differently to questions about physical and emotional symptoms. As there appears to be a bidirectional relationship between physical symptoms and affect (LeBaron & Zeltzer, 1984), it is likely that interventions aimed at either cluster of symptoms would improve both.
Contributor Information
KIMBERLY M. WESLEY, Department of Psychology, La Salle University, Philadelphia, PA, USA.
NATALIYA ZELIKOVSKY, Department of Pediatrics, The Children’s Hospital of Philadelphia, Philadelphia, PA, USA; and Department of Psychology, La Salle University, Philadelphia, PA, USA.
LISA A. SCHWARTZ, Department of Pediatrics, The University of Pennsylvania, Philadelphia, PA, USA; and Department of Pediatrics, Division of Oncology, The Children’s Hospital of Philadelphia, Philadelphia, PA, USA.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Alderfer M, Navsaria N, Kazak A. Family functioning and posttraumatic stress disorder in adolescent survivors of childhood cancer. Journal of Family Psychology. 2009;23(5):717–725. doi: 10.1037/a0015996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Cancer Society. Cancer facts and statistics. 2010 Retrieved from http://www.cancer.org/research/cancerfactsstatistics/index.
- Barrera M, Andrews S, Burnes D, Atenafu E. Age differences in perceived social support by paediatric haematopoietic progenitor cell transplant patients: A longitudinal study. Child: Care, Health, and Development. 2007;34(1):19–24. doi: 10.1111/j.1365-2214.2007.00785.x. [DOI] [PubMed] [Google Scholar]
- Bellizzi KM, Smith A, Schmidt S, Keegan THM, Zebrack B, Lynch CF, Simon M. Positive and negative psychosocial impact of being diagnosed with cancer as an adolescent or young adult. Cancer. 2012;13:1–8. doi: 10.1002/cncr.27512. [DOI] [PubMed] [Google Scholar]
- Ben-Ari E. AYAs are not alone: Confronting psychosocial challenges of cancer. National Cancer Institute Cancer Bulletin. 2011;8(15):6. [Google Scholar]
- Cavusoglu H. Problems related to the diagnosis and treatment of adolescents with leukemia. Issues in Comprehensive Pediatric Nursing. 2000;23:15–26. doi: 10.1080/014608600265183. [DOI] [PubMed] [Google Scholar]
- Chiang Y, Yeh C, Wang K, Yang C. The experience of cancer-related fatigue in Taiwanese children. European Journal of Cancer Care. 2009;18:43–49. doi: 10.1111/j.1365-2354.2007.00884.x. [DOI] [PubMed] [Google Scholar]
- Compas BE, Davis GE, Forsythe CJ, Wagner BM. Assessment of major and daily stressful events during adolescence: The Adolescents Perceived Events Scale. Journal of Consulting and Clinical Psychology. 1987;55(4):534–341. doi: 10.1037/0022-006X.55.4.534. [DOI] [PubMed] [Google Scholar]
- Compas BE, Howell DC, Phares V, Williams RA, Giunta CT. Risk factors for emotional/behavioral problems in young adolescents: A prospective analysis of adolescent and parental stress and symptoms. Journal of Consulting and Clinical Psychology. 1989;57(6):732–740. doi: 10.1037//0022-006x.57.6.732. [DOI] [PubMed] [Google Scholar]
- Corey A, Haase J, Azzouz F, Monahan P. Social support and symptom distress in adolescents/young adults with cancer. Journal of Pediatric Oncology Nursing. 2008;25(5):275–284. doi: 10.1177/1043454208321117. [DOI] [PubMed] [Google Scholar]
- Crawford JR, Henry JD. The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement, and normative data in a large non-clinical sample. British Journal of Clinical Psychology. 2004;43:245–265. doi: 10.1348/0144665031752934. [DOI] [PubMed] [Google Scholar]
- Decker C. Social support and adolescent cancer survivors: A review of the literature. Psycho-Oncology. 2007;16:1–11. doi: 10.1002/pon.1073. [DOI] [PubMed] [Google Scholar]
- Draguns JG, Tanaka-Matsumi J. Assessment of psychopathology across and within cultures: Issues and findings. Behaviour Research and Therapy. 2003;41(7):755–776. doi: 10.1016/s0005-7967(02)00190-0. [DOI] [PubMed] [Google Scholar]
- Edwards B, Clark V. The psychological impact of a cancer diagnosis on families: The influence of family functioning and patients’ illness characteristics on depression and anxiety. Psycho-Oncology. 2004;13(8):562–576. doi: 10.1002/pon.773. [DOI] [PubMed] [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. Journal of Marital and Family Therapy. 1983;9:171–180. [Google Scholar]
- Fleming JE, Offord DR. Epidemiology of childhood depressive disorders: A critical review. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29(4):571–580. doi: 10.1097/00004583-199007000-00010. [DOI] [PubMed] [Google Scholar]
- Grant K, Compas B. Stress and anxious-depressed symptoms among adolescents: Searching for mechanisms of risk. Journal of Consulting and Clinical Psychology. 1995;63(6):1015–1021. doi: 10.1037//0022-006x.63.6.1015. [DOI] [PubMed] [Google Scholar]
- Green R, Horn H, Erickson J. Eating experiences of children and adolescents with chemotherapy-related nausea and mucositis. Journal of Pediatric Oncology Nursing. 2010;27(4):209–216. doi: 10.1177/1043454209360779. [DOI] [PubMed] [Google Scholar]
- Hockenberry M. Symptom management research in children with cancer. Journal of Pediatric Oncology Nursing. 2004;21(3):132–136. doi: 10.1177/1043454204264387. [DOI] [PubMed] [Google Scholar]
- Jacob E, Hesselgrave J, Sambuco G, Hockenberry M. Variations in pain, sleep, and activity during hospitalization in children with cancer. Journal of Pediatric Oncology Nursing. 2007;24(4):208–129. doi: 10.1177/1043454207299875. [DOI] [PubMed] [Google Scholar]
- Kabacoff RI, Miller IW, Bishop DS, Epstein NB, Keitner GI. A psychometric study of the McMaster Family Assessment Device in psychiatric, medical, and nonclinical samples. Journal of Family Psychology. 1990;3:431–439. [Google Scholar]
- Knotkova H, Clark W, Mokrejs P, Padour F, Kuhl J. What do ratings on unidimensional pain and emotion scales really mean? A Multidimensional Affect and Pain Survey (MAPS) analysis of cancer patient responses. Journal of Pain and Symptom Management. 2004;28(1):19–27. doi: 10.1016/j.jpainsymman.2003.11.003. [DOI] [PubMed] [Google Scholar]
- LeBaron S, Zeltzer L. Assessment of acute pain and anxiety in children and adolescents by self-reports, observer reports, and a behavior checklist. Journal of Consulting and Clinical Psychology. 1984;52(5):729–738. doi: 10.1037//0022-006x.52.5.729. [DOI] [PubMed] [Google Scholar]
- Li CE, DiGiuseppe R, Froh J. The roles of sex, gender, and coping in adolescent depression. Adolescence. 2006;41:409–415. [PubMed] [Google Scholar]
- Ljungman G, Gordh T, Sörensen S, Kreuger A. Pain in paediatric oncology: Interviews with children, adolescents and their parents. Acta Paediatrica. 1999;88:623–630. doi: 10.1080/08035259950169279. [DOI] [PubMed] [Google Scholar]
- Manne S, Miller D. Social support, social conflict, and adjustment among adolescents with cancer. Journal of Pediatric Psychology. 1998;23(2):121–130. doi: 10.1093/jpepsy/23.2.121. [DOI] [PubMed] [Google Scholar]
- Moskowitz J, Epel E, Acree M. Positive affect uniquely predicts lower risk of mortality in people with diabetes. Health Psychology. 2008;27:73–82. doi: 10.1037/0278-6133.27.1.S73. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute & LiveSTRONG Young Adult Alliance. NIH Publication No: 06-6067. Bethesda, MD: 2006. Report of the adolescent and young adult oncology progress review group. Retrieved from http://planning.cancer.gov/library/AYAO_PRG_Report_2006_FINAL.pdf. [Google Scholar]
- Oldehinkel AJ, Rosmalen JGM, Veenstra R, Dijkstra JK, Ormel J. Being admired or being liked: Classroom social status and depressive problems in early adolescent girls and boys. Journal of Abnormal Child Psychology. 2007;35(3):417–427. doi: 10.1007/s10802-007-9100-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozono S, Saeki T, Mantani T, Ogata A, Okamura H, Nakagawa S, Yamawaki S. Psychological distress related to patterns of family functioning among Japanese childhood cancer survivors and their parents. Psychooncology. 2010;19(5):545–552. doi: 10.1002/pon.1606. [DOI] [PubMed] [Google Scholar]
- Patenaude A, Kupst M. Psychosocial functioning in pediatric cancer. Journal of Pediatric Psychology. 2005;30(1):9–27. doi: 10.1093/jpepsy/jsi012. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Frohlich C, Silbereisen R. Optimism, pessimism, and change of psychological well-being in cancer patients. Psychology, Health, and Medicine. 2007;12(4):421–432. doi: 10.1080/13548500601084271. [DOI] [PubMed] [Google Scholar]
- Procidano M, Heller K. Measures of perceived social support from friends and from family: Three validation studies. American Journal of Community Psychology. 1983;11(1):1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- Ritchie M. Psychosocial nursing care for adolescents with cancer. Issues in Comprehensive Pediatric Nursing. 2001;24:165–175. doi: 10.1080/01460860121107. [DOI] [PubMed] [Google Scholar]
- Ruland C, Hamilton G, Schjodt-Osmo B. The complexity of symptoms and problems experienced in children with cancer: A review of the literature. Journal of Pain and Symptom Management. 2009;37(3):403–418. doi: 10.1016/j.jpainsymman.2008.03.009. [DOI] [PubMed] [Google Scholar]
- Ryder AG, Yang J, Zhu X, Yao S, Yi J, Heine S, Bagby RM. The cultural shaping of depression: Somatic symptoms in China, psychological symptoms in North America? Journal of Abnormal Psychology. 2008;117(2):300–313. doi: 10.1037/0021-843X.117.2.300. [DOI] [PubMed] [Google Scholar]
- Schwartz LA, Kazak AE, Mougianis I. Cancer. In: O’Donohue W, Tolle LW, editors. Behavioral approaches to chronic disease in adolescence. New York, NY: Springer Publishing; 2009. pp. 197–217. [Google Scholar]
- Trask PC, Paterson AG, Trask CL, Bares CB, Birt J, Maan C. Parental and adolescent adjustment to pediatric cancer: Associations with coping, social support, and family function. Journal of Pediatric Oncology Nursing. 2003;20:36–47. doi: 10.1053/jpon.2003.5. [DOI] [PubMed] [Google Scholar]
- Ullrich C, Dussel V, Hilden J, Sheaffer J, Moore C, Berde C, Wolfe J. Fatigue in children with cancer at the end of life. Journal of Pain and Symptom Management. 2010;40(4):483–494. doi: 10.1016/j.jpainsymman.2010.02.020. [DOI] [PubMed] [Google Scholar]
- Varni JW, Burwinkle TM, Katz ER, Meeske K, Dickinson P. The PedsQL in paediatric cancer: Reliability and validity of the Paediatric Quality of Life Inventory generic core scales, multidimensional fatigue scale and cancer module. Cancer. 2002;94:2090–2106. doi: 10.1002/cncr.10428. [DOI] [PubMed] [Google Scholar]
- Varni J, Katz E. Stress, social support, and negative affectivity in children with newly diagnosed cancer: A prospective transactional analysis. Psycho-Oncology. 1997;6:267–278. doi: 10.1002/(SICI)1099-1611(199712)6:4<267::AID-PON277>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Varni JW, Katz ER, Seid M, Quiggins DJL, Friedman-Bender A, Castro CM. The Pediatric Cancer Quality of Life Inventory (PCQL), I: Instrument development, descriptive statistics, and cross-informant variance. Journal of Behavioral Medicine. 1998;21:179–204. doi: 10.1023/a:1018779908502. [DOI] [PubMed] [Google Scholar]
- Wallace ML, Harcourt D, Rumsey N, Foot A. Managing appearance changes resulting from cancer treatment: Resilience in adolescent females. PsychoOncology. 2007;16:1019–1027. doi: 10.1002/pon.1176. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark L, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Williamson H, Harcourt D, Halliwell E, Frith H, Wallace M. Adolescents’ and parents’ experiences of managing the psychosocial impact of appearance change during cancer treatment. Journal of Pediatric Oncology Nursing. 2010;27(3):168–175. doi: 10.1177/1043454209357923. [DOI] [PubMed] [Google Scholar]
- Woodgate RL. Conceptual understanding of resilience in the adolescent with cancer: Part I. Journal of Pediatric Oncology Nursing. 1999a;16(1):35–43. doi: 10.1177/104345429901600105. [DOI] [PubMed] [Google Scholar]
- Woodgate RL. Conceptual understanding of resilience in the adolescent with cancer: Part II. Journal of Pediatric Oncology Nursing. 1999b;16(2):78–90. doi: 10.1177/104345429901600105. [DOI] [PubMed] [Google Scholar]
- Woodgate R. The importance of being there: Perspectives of social support by adolescents with cancer. Journal of Pediatric Oncology Nursing. 2006;23:122–134. doi: 10.1177/1043454206287396. [DOI] [PubMed] [Google Scholar]


