Abstract
Objective
The aim of this study was to identify biomarkers with prognostic value in the setting of surgically treated endometrial cancer.
Methods
Medical data for 282 patients with surgically treated endometrial cancer were reviewed retrospectively. Preoperative concentrations of six serum biomarkers (CA125, CA15-3, C-reactive protein [CRP], D-dimer [D-D], platelet-to-lymphocyte ratio [PLR], and neutrophil-to-lymphocyte ratio [NLR]) were analysed to determine potential associations with clinicopathologic characteristics and to assess prognostic values separately via Kaplan-Meier method and multivariate Cox regression.
Results
In univariate analyses, the 5-year overall survival (OS) rate was 86.5% for a maximum follow-up period of 75 months. High concentrations of CA125, CA15-3, CRP, D-D, PLR, and NLR each proved significantly predictive of poor survival (log-rank test, P<0.01). CRP and D-D were identified as independent prognosticators, using a Cox regression model. Study patients were then stratified (based on combined independent risk factors) into three tiers (P<0.001), marked by 5-year OS rates of 92.1%, 78.4%, and 33.3%.
Conclusions
All serum biomarkers assessed (CA125, CA15-3, CRP, D-D, PLR, and NLR) proved to be valid prognostic indices of surgically treated endometrial cancer. A novel prognostic grouping system, incorporating independent risk factors (CRP and D-D Concentrations), may have merit in assessing these patients preoperatively, providing a biologic basis for improved clinical staging.
Introduction
Endometrial carcinoma is the most common gynaecologic malignancy [1, 2], accounting for approximately 288,000 new diagnoses and 50,327 deaths worldwide each year [3]. A clinical staging system developed by the International Federation of Gynecology and Obstetrics (FIGO) is currently used to guide surgical management and to predict outcome among patients with endometrial cancer. However, same-stage patients often experience substantially different clinical courses [1, 4]. To address this discrepancy, many investigators have pursued multivariate analysis of tumour attributes to delineate prognostic factors, such as pelvic lymph node metastases (LNM), tumour size (TS), cervical stromal invasion, lymphatic vascular space involvement (LVSI), histologic subtypes, and more [4–6]. Unfortunately, preoperative evaluations generally call for fractional curettage, transvaginal sonography, magnetic resonance imaging, or hysteroscopic assessment, which are invasive, costly, and time-consuming [1, 7–9].
Recently, novel biomarkers (especially those circulating in blood) have been increasingly targeted to predict the course of endometrial cancer. The latter include serum tumour markers (e.g., CA125, HE4, CA15-3) [10, 11], indices of systemic inflammation (e.g., C-reactive protein [CRP], neutrophil-to-lymphocyte ratio [NLR], and platelet-to-lymphocyte ratio [PLR]) [12, 13], and factors implicated in venous thromboembolism (VTE) (e.g., thrombin-antithrombin III complex and D-dimer [D-D]) [14]. Such markers are readily monitored through relatively noninvasive means.
For this study, predictive values of six circulating biomarkers (CA125, CA15-3, CRP, D-D, PLR, and NLR) were addressed via Kaplan-Meier method and multivariate Cox regression. We then used two independent risk factors to develop a prognostic grouping system, thus identifying meaningful prognostic subsets of the study population (as opposed to clinical staging).
Materials and Methods
Patients
A retrospective review was conducted, analysing data on 282 patients (age range, 21–76 years; median, 53 years) subjected to surgery at Sun Yat-Sen University Cancer Center (SYSUCC; Guangzhou, China) as primary treatment of endometrial cancer between September 2007 and June 2009. Insufficient data, non-surgical treatment, secondary malignancies, and haematologic diseases were grounds for exclusion.
Each diagnosis of endometrial cancer was based on curetted tissue. Classified by differences in histology and molecular characteristics, endometrial carcinoma has been generally distinguished as Types I (mainly endometrioid) and II (non-endometrioid) as suggested by Bokhman and subsequent researchers.[15–18] For histologic grading of tumours, WHO classification was used. All patients were clinically staged according to FIGO guidelines (2009). Patients underwent total abdominal hysterectomy only (195 cases), or total abdominal hysterectomy plus total abdominal hysterectomy bilateral salpingoo-ophorectomy, and systemic pelvic lymphadenectomy (87 cases); among these 282 surgeries, 110 cases were with and 172 cases withoutpara-aortic lymph node dissection. Radical hysterectomy was performed in instances of suspected cervical stromal involvement. Both common iliac and obturator nodes (above obturator nerve) were included in pelvic lymphadenectomies. Adjuvant chemotherapy was administered postoperatively at the discretion of gynaecologic oncologists overseeing patients with lymph node metastases, parametrial invasion, and positive or close surgical margins. Information about the expression of serum biomarkers is stratified according to endometrial cancer stage, grade, type and patient's age, shown in Table 1.
Table 1. The relationship between clinicopathological characteristics and serum biomarkers concentrations.
(Mean and 95% CI).
| n | CA125 | P v | CA15-3 | P v | CRP | P v | D-D | P v | PLR | P v | NLR | P v | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (U/ml) | (U/ml) | (mg/l) | (mg/l) | |||||||||||
| Age | ||||||||||||||
| <50 | 98 | 23.82 | 0.491 | 12.92 | 0.336 | 1.13 | 0.002 | 0.55 | 0.286 | 147.64 | 0.001 | 2 | 0.257 | |
| (14.08–46.81) | (9.14–19.89) | (0.46–2.89) | (0.40–0.90) | (113.36–208.92) | (1.52–2.74) | |||||||||
| ≥50 | 184 | 21.11 | 12.19 | 2.17 | 0.6 | 125.1 | 1.83 | |||||||
| (14.07–39.90) | (8.88–17.71) | (0.72–6.19) | (0.40–1.00) | (99.13–165.96) | (1.38–2.69) | |||||||||
| Type | ||||||||||||||
| Ⅰ | 254 | 132.18 | 0.708 | 21.67 | 0.787 | 6.42 | <0.001 | 1.34 | 0.349 | 148.87 | 0.008 | 2.29 | <0.001 | |
| (41.11–223.23) | (14.04–29.31) | (3.59–9.34) | (0.45–2.23) | (140.15–157.96) | (2.11–2.46) | |||||||||
| Ⅱ | 28 | 79.55 | 24.91 | 33.62 | 2.65 | 191.45 | 3.88 | |||||||
| (35.68–123.28) | (7.81–42.01) | (13.79–53.46) | (1.22–4.08) | (137.34–245.57) | (2.51–5.25) | |||||||||
| FiGO | ||||||||||||||
| Ⅰ | 152 | 18.73 | <0.001 | 10.97 | <0.001 | 1.33 | 0.003 | 0.5 | <0.001 | 126.47 | 0.365 | 1.8 | 0.054 | |
| (13.31–25.62) | (7.80–15.59) | (0.54–4.20) | (0.30–0.73) | (106.33–167.91) | (1.37–2.46) | |||||||||
| Ⅱ | 58 | 25.53 | 12.37 | 1.33 | 0.6 | 129.33 | 1.9 | |||||||
| (15.93–46.99) | (9.37–19.35) | (0.58–4.70) | (0.45–0.90) | (99.03–200.59) | (1.46–2.88) | |||||||||
| Ⅲ | 61 | 44.41 | 15.99 | 3.07 | 0.9 | 139.07 | 2.08 | |||||||
| (20.65–72.30) | (10.84–29.3) | (0.82–10.43) | (0.50–1.70) | (104.76–185.46) | (1.52–3.47) | |||||||||
| Ⅳ | 11 | 93.19 | 27.93 | 3.17 | 1.4 | 155 | 2.84 | |||||||
| (57.93–386.90) | (10.27–43.3) | (2.28–29.68) | (0.65–2.45) | (111.20–255.14) | (1.60–3.20) | |||||||||
| Grade | ||||||||||||||
| G1 | 69 | 17.75 | 0.001 | 11.16 | 0.003 | 1.11 | 0.011 | 0.5 | <0.001 | 145 | 0.124 | 2.1 | 0.126 | |
| (13.22–23.01) | (7.45–15.21) | (0.45–3.27) | (0.30–0.90) | (114.94–195.72) | (1.30–2.55) | |||||||||
| G2 | 145 | 25.08 | 13.07 | 1.7 | 0.55 | 129.5 | 1.76 | |||||||
| (13.73–44.66) | (9.25–19.01) | (0.68–4.83) | (0.40–0.80) | (101.95–167.49) | (1.44–2.60) | |||||||||
| G3 | 68 | 26.07 | 13.82 | 2.67 | 0.9 | 122.73 | 2.18 | |||||||
| (15.75–62.43) | (9.70–24.82) | (0.81–12.19) | (0.50–1.70) | (101.09–205.83) | (1.49–3.32) | |||||||||
| Metas. | ||||||||||||||
| Yes | 14 | 20.51 | 0.689 | 14.26 | 0.97 | 4.96 | 0.019 | 1 | 0.021 | 138.71 | 0.522 | 2.3 | 0.231 | |
| (11.86–59.16) | (7.28–23.54) | (1.05–48.76) | (0.65–1.73) | (108.04–243.000) | (1.40–4.63) | |||||||||
| No | 268 | 21.54 | 12.47 | 1.49 | 0.6 | 130 | 1.89 | |||||||
| (14.09–44.40) | (9.12–18.99) | (0.58–4.94) | (0.40–0.90) | (105.14–177.72) | (1.43–2.67) | |||||||||
| Recur. | ||||||||||||||
| Yes | 12 | 17.37 | 0.994 | 11.38 | 0.808 | 11.14 | 0.001 | 0.7 | 0.081 | 140.35 | 0.384 | 2.9 | 0.031 | |
| (9.62–274.60) | (7.55–50.66) | (2.38–63.18) | (0.50–4.10) | (92.98–332.45) | (1.85–5.09) | |||||||||
| No | 270 | 21.47 | 12.5 | 1.47 | 0.6 | 130.25 | 1.88 | |||||||
| (14.13–41.76) | (9.10–18.83) | (0.59–4.83) | (0.40–1.00) | (105.94–177.31) | (1.42–2.67) | |||||||||
P-v: p value; Type: types of endometrial carcinoma; FIGO: the FIGO stage; Grade: Histopathological grade; D-D: D dimer; PLR: platelet to lymphocyte ratio; NLR: neutrophil to lymphocyte ratio; Metas.: metastasis; Recur.: recurrence
Methods
All data on six blood biomarkers (CA125, CA15-3, CRP, D-D, PLR, and NLR) were collected from preoperative medical records of patients studied. Peripheral blood samples drawn from patients less than 2 weeks prior to surgery were analysed in the SYSUCC clinical laboratory. A Modular Analytics E170 immunoassay unit (Roche Diagnostics, Germany) was used to determine concentrations of tumour markers (CA125, CA15-3), a Hitachi 7600 automated chemistry analyser (Hitachi Co, Japan) was used to determine CRP concentrations, a latex agglutination assay for D-D concentrations (Sekisui Medical Co, Ltd, Japan) and a Sysmex XE-5000 system (Sysmex Co, Japan) for blood cell counts. NLR (absolute neutrophil count divided by absolute lymphocyte count) and PLR (absolute platelet count divided by absolute lymphocyte count) were both computed. Patients were separately divided into two groups with high or low concentrations by the cut-points (CA125 ≥35 U/ml, CA15-3 ≥25 U/ml, CRP, ≥8.2 mg/L, D-D ≥1.5 mg/l, PLR ≥250, and NLR ≥4.68) as recommended by reagent manufacturers or cited other authors [12, 13, 19–23].
The interrelationships of clinicopathologic features, serum biomarker concentrations, and cancer prognosis were analysed. Each patient returned on a semi-annual basis for clinical follow-up visits by a specified division of SYSUCC, and follow-up information accrued until death or a maximum of 75 months (mean: 51.2 months, range: 0.3–75.8 months) at the time of study completion (March 2014).
Ethical Statement
The study was approved by the Clinical Research Ethics Committee of SYSUCC. Patient records and information were anonymized and de-identified prior to analysis.
Statistical analysis
Data analysis relied on standard software (SPSS v 17.00; SPSS Inc., Chicago, IL, USA). Survival curves were constructed via Kaplan-Meier method and comparisons were made using the log-rank test. For univariate and multivariate analyses of prognostic factors, Cox proportional hazards regression was applied. Statistical comparisons among the three tiers of patients were achieved through one-way ANOVA, with Student-Newman-Keuls post hoc testing. Student's t-test or Mann-Whitney U-test was used to assess significance of between-groups differences. Statistical significance was set at P<0.05.
Results
Relationships between clinicopathologic characteristics and serum biomarker concentrations
A total 282 patients with endometrial cancer who were treated surgically and fully met our criteria were included in the study. Patient demographics, clinicopathologic characteristics, and biomarker concentrations are summarised in Table 1. Higher CRP concentrations (P<0.01) and lower PLR concentrations (P<0.01) were observed in older subjects (≥50 years). In patients with Type II endometrial carcinoma, higher concentrations (P<0.01) of CRP, PLR and NLR were observed. Concentrations of tumour markers (CA125 and CA15-3) rose significantly (P<0.01) as FIGO stage and histopathologic tumour grade worsened. Concentrations of CRP were clearly elevated in patients with tumour metastases or recurrences (Table 1). Median D-D concentration (0.6 mg/l) exceeded the reagent provided normal reference value (<0.5 mg/l); and 34 patients with D-D plasma concentrations >1.5 mg/l were felt to be at risk of silent VTE. Significant elevations of NLR (P<0.01) were confined to patients with recurrent neoplasms.
Prognostic value of biomarkers in endometrial cancer
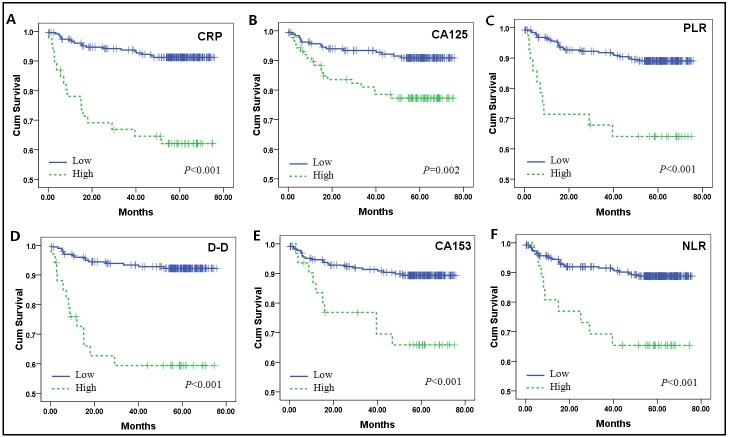
Patient survival curves, assigned by concentrations of biomarkers to high and low groups, were constructed via Kaplan-Meier method and were compared using the log-rank test (Fig 1). Mean survival of the cohort was 67.9 months, with a 5-year overall survival (OS) of 86.5%. As shown in Table 2 and Fig 1, elevations of all biomarkers assessed (CA125, CA15-3, CRP, D-D, PLR, and NLR) were significantly predictive of poor 5-year OS (P<0.01). Among these variables, only CRP and D-D concentrations were identified as independent prognostic variables, based on the Cox proportional hazards model depicted in Table 3. Respective hazard ratios for CRP and D-D were 0.215 (95% CI: 0.084–0.549) and 0.252 (95% CI: 0.095–0.670)
Fig 1. Kaplan-Meier survival estimates for patients with endometrial cancer.
Disease-specific survival curves of patients grouped as low and high risk, according to biomarker cut-points (log-rank test used to calculate P-values).
Table 2. Univariate analysis of biomarkers predictive of survival time (S.T) and the 5-year overall survival (OS).
| n | S T(month) | 5-year OS (%) | P-v | |
|---|---|---|---|---|
| Mean (95%,CI) | Mean±SD | Log-Rank | ||
| Total | 282 | 67.9(65.4–70.4) | 86.5±1.9 | |
| CRP | ||||
| low | 232 | 70.9(68.7–73.1) | 91.2±1.9 | <0.001 |
| high | 46 | 51.8(42.7–60.8) | 62.1±7.3 | |
| D-D | ||||
| low | 202 | 71.2(68.9–73.5) | 92.2±1.9 | <0.001 |
| high | 34 | 48.4(37.3–59.6) | 59.4±8.7 | |
| CA125 | ||||
| low | 187 | 70.6(68.1–73.1) | 90.9±2.2 | 0.002 |
| high | 88 | 61.8(56.4–67.3) | 77.3±4.6 | |
| CA15-3 | ||||
| low | 229 | 69.6(67.1–72.0) | 89.4±21 | <0.001 |
| high | 31 | 56.4(46.5–66.3) | 65.9±8.8 | |
| PLR | ||||
| low | 254 | 69.6(67.3–71.9) | 89.5±2.0 | <0.001 |
| high | 28 | 52.1(40.3–63.8) | 64.1±9.1 | |
| NLR | ||||
| low | 256 | 69.3(66.9–71.7) | 89.2±2.0 | <0.001 |
| high | 26 | 54.3(43.2–65.4) | 65.4±9.3 |
Cut-off values for each biomarker: CA125 35U/ml; CA15-3 25U/ml; CRP 8.2mg/L; D-D 1.5mg/l; PLR 250, NLR 4.68.
Table 3. Multivariate Cox regression analyzes of serum biomarkers prognostic factors for surgical patients with endometrial cancer.
| Coefficient | SE | P-v | HR | 95.0% CI for HR | |
|---|---|---|---|---|---|
| CRP | -1.536 | 0.477 | 0.001 | 0.215 | 0.084–0.549 |
| DD | -1.376 | 0.498 | 0.006 | 0.252 | 0.095–0.670 |
| CA125 | 0.071 | 0.526 | 0.893 | 1.073 | 0.383–3.009 |
| CA15-3 | -0.621 | 0.540 | 0.250 | 0.537 | 0.186–1.550 |
| PLR | -0.007 | 0.621 | 0.991 | 0.993 | 0.294–3.357 |
| NLR | 0.832 | 0.622 | 0.181 | 2.298 | 0.679–7.781 |
SE: standard error; P-v: P value; HR: hazard ratios; CI: confidence interval.
A novel prognostic grouping system combining independent risk factors
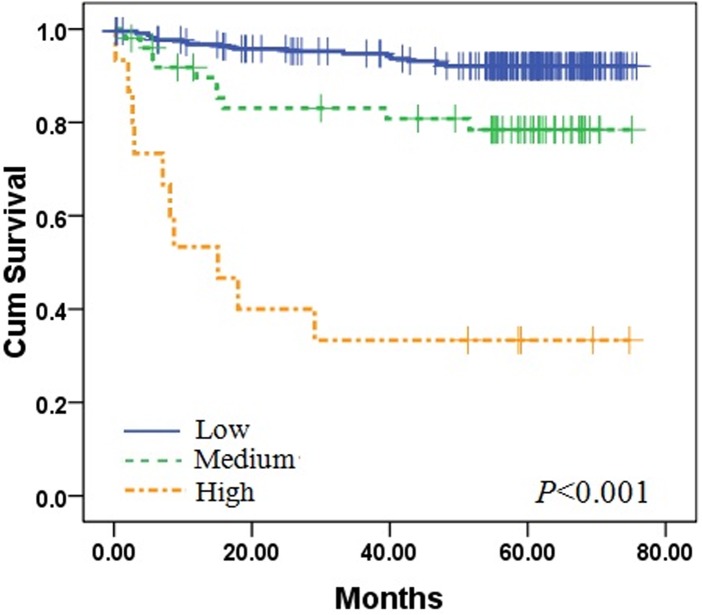
As independent risk factors in this analysis, CRP and D-D concentrations prompted a new prognostic hierarchy where stipulated subsets better reflected actual outcomes of patients with endometrial cancer. Patients were assigned as follows: low risk (CRP <8.2 mg/l and D-D <1.5 mg/l), medium risk (CRP ≥8.2 mg/l, or D-D≥1.5 mg/l), and high risk (CRP ≥8.2 mg/l and D-D≥1.5 mg/l). Patient survival differed significantly by group (Fig 2; P<0.001), with mean survival times as follows: low risk, 71.5 months (95% CI: 69.6–73.6; n = 217); medium risk, 62.6 months (95% CI: 55.5–69.7; n = 50); and high risk, 31.2 months (95% CI:15.2–47.2; n = 15). Respective 5-year OS rates were 92.1%±1.9, 78.4%±6.1, and 33.3%±12.2.
Fig 2. Three-tiered stratification of patients with endometrial cancer, incorporating two independent prognostic variables (CRP and D-D Concentrations).
Survival in low-risk (CRP <8.2 mg/l and D-D <1.5 mg/l), medium-risk (CRP ≥8.2 mg/l, or D-D ≥1.5 mg/l), and high-risk (CRP ≥8.2 mg/l and D-D ≥1.5 mg/l) groups differed significantly (log-rank test used to calculate P-values).
Discussion
In the course of this study, the prognostic values of six blood biomarkers in patients with endometrial cancer were evaluated. To our knowledge, this is the first effort where CRP and D-D concentrations have been identified as independent prognostic factors in endometrial cancer.
Although the 5-year survival rates of endometrial cancer are favourable in general [24], some patients have poor outcomes. Clinicopathologic characteristics of endometrial cancer, including patient age, histologic type/grade, clinical stage, lymphatic vascular space invasion, and other parameters, have been well-studied previously [25–27]. Current efforts increasingly have targeted molecular biomarkers that may advance the histologic classification of tumours, improve our ability to identify more aggressive cancers [28–32], and potentially enable staging revisions, resulting in more personalized therapy and better clinical outcomes. In this study, we successfully defined a poor prognosis group by incorporating the above independent risk factors in a new system of patient stratification (Fig 2).
As the goal of this investigation, relationships between concentrations of certain biomarkers and clinicopathologic characteristics of endometrial cancer were analysed. Patient age clearly is an important risk factor here. In the 15% of patients diagnosed with endometrial cancer before the age of 50 [33], the 5-year survival rate is nearly 96.3% [25]. Our evidence shows that both CRP concentration and PLR are significantly aligned with patient age. In addition, FIGO surgical staging (recommended as a formal step in initial treatment)[1] showed significant associations with CA125, CA15-3, CRP, and D-D Concentrations in our study, these indicate that they are closely related with tumour pathophysiology. There have been many reports on the risk factors and molecular markers associated with Type I and Type II endometrial cancer [18, 34], in this study we found that CRP, PLR and NLR in the blood were significantly associated with histologic subtypes of endometrial cancer.(Table 1), These differences may be the result of more severe system inflammation in Type II endometrial cancer. We also found that the histologic grades of tumours correlated with CA125, CA15-3, CRP, and D-D Concentrations, however, only CRP and D-D elevations were seen in patients with metastatic or recurrent tumours (Table 1). The above findings suggest that these risk factors are all interrelated.
We further analysed the prognostic value of the panel of biomarkers via Kaplan-Meier method and Cox proportional hazards regression. In univariate analyses, all six biomarkers correlated significantly with survival time (Fig 1), but in multivariate analyses, only CRP and D-D concentrations were independently linked with endometrial cancer prognosis. Elevated serum CA125 concentrations carry a number of connotations in patients with endometrial cancer, implying advanced age and tumour stage, shortened survival, and extrauterine spread, among other features [22, 23]. Consistent with previous findings, high serum CA125 concentration (CA125 ≥35 U/ml) was also a risk factor for poor prognosis (5-year OS,77.3%±4.6) on this occasion. Although the CA15-3 biomarker was similarly indicative of poor prognosis in this cohort, no highly significant association with shortened survival was evident in multivariate analysesas previously found [35]; this lack of significance may be due to its poor specificity for endometrial cancer.
Chronic inflammation may well play a central role in development of endometrial cancer [36]. As CRP is the prevailing index of inflammation [37], the CRP concentration elevations seemingly validate a link between obesity and endometrial cancer [29, 30]. We have shown that 5-year OS rates differed significantly (P<0.01) in patients with low (91.2%) and high (14.4%) CRP concentration. In addition, the considerable significance of CRP concentration elevation was sustained in multivariate analyses, coupled with a greater hazard ratio (Table 3). PLR and NLR are also indices of systemic inflammation, which recently have been explored as prognosticators in various cancers (pancreatic, colorectal, ovarian, gastric, and endometrial). However, the prognostic role of PLR in cancer currently remains controversial [12, 13, 32]. In Table 1, PLR showed a significant association with age, and NLR correlated significantly with FIGO stage and tumour recurrence. In terms of survival, both parameters proved significant by univariate analyses but not in the Cox regression model.
High D-D concentration (>1.5 mg/l) is likely a harbinger of VTE [38]. One previous study documented silent or subclinical VTE prior to surgery in at least 10% of patients with endometrial cancer, underscoring that D-D determination should be considered before treating any of these patients [19]. In this study, D-D concentrations were significantly aligned with FIGO stage and histologic tumour grade, as well as with tumour metastasis and recurrence. Understandably, those patients (9.2%) with high D-D concentrations (>1.5 mg/l) had even worse prognoses (Table 2), and D-D concentration was found to be an independent prognosticator via Cox regression model.
Detection of VTE and inflammatory conditions prior to surgical treatment is a very important aspect of therapeutic strategy and postoperative care [1, 19, 39]. In this study, both CRP and D-D concentrations were identified in multivariate analyses as independent prognostic variables for survival in patients with endometrial cancer. Hence, we developed a new prognostic hierarchy for grouping of patients, incorporating CRP and D-D cut-points. Survival of patients postoperatively differed significantly at these three new tiers of patient risk (Fig 2). We feel this is useful tool for preoperative assessment of patients with endometrial cancer. Furthermore, this approach may provide more objective biologic evidence to improve the existing system of clinical staging.
At present, FIGO surgical staging relies on pre- and intraoperative pathologic assessment of tumour grade and depth of invasion, but by some accounts, one-third of grade 1 endometrial cancers are upgraded, and one-third are upstaged once final pathology reports are issued [39, 40]. Serum biomarker determinations may outperform histologic and even imaging studies as a means of tumour assessment, enabling better appreciation of biologic attributes in a more timely fashion. The molecular signatures of cancers provide clues to the cellular microenvironment, offering opportunities for personalised treatment strategies [39].
In patients surgically treated for endometrial cancer, preoperative concentrations of the above six biomarkers studied showed prognostic value. Moreover, CRP and D-D concentrations were proven (via Cox regression model) to be independent indices of prognosis in this setting, prompting the development of a novel patient stratification system.
Data Availability
Due to ethical restrictions related to patient confidentiality, all relevant data are available upon request to the corresponding author.
Funding Statement
The authors have no support or funding to report.
References
- 1.Burke WM, Orr J, Leitao M, Salom E, Gehrig P, Olawaiye AB, et al. Endometrial cancer: A review and current management strategies: Part I. Gynecol Oncol 2014. [DOI] [PubMed]
- 2. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010;127: 2893–2917. 10.1002/ijc.25516 [DOI] [PubMed] [Google Scholar]
- 3. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011;61: 69–90. 10.3322/caac.20107 [DOI] [PubMed] [Google Scholar]
- 4. Ho CM, Chien TY, Huang SH, Wu CJ, Shih BY, Chang SC. Multivariate analysis of the prognostic factors and outcomes in early cervical cancer patients undergoing radical hysterectomy. Gynecol Oncol 2004;93: 458–464. [DOI] [PubMed] [Google Scholar]
- 5. Kamura T, Tsukamoto N, Tsuruchi N, Saito T, Matsuyama T, Akazawa K, et al. Multivariate analysis of the histopathologic prognostic factors of cervical cancer in patients undergoing radical hysterectomy. Cancer 1992;69: 181–186. [DOI] [PubMed] [Google Scholar]
- 6. Takeda N, Sakuragi N, Takeda M, Okamoto K, Kuwabara M, Negishi H, et al. Multivariate analysis of histopathologic prognostic factors for invasive cervical cancer treated with radical hysterectomy and systematic retroperitoneal lymphadenectomy. Acta Obstet Gynecol Scand 2002;81: 1144–1151. [DOI] [PubMed] [Google Scholar]
- 7. Fotiou S, Vlahos N, Kondi-Pafiti A, Zarganis P, Papakonstantinou K, Creatsas G. Intraoperative gross assessment of myometrial invasion and cervical involvement in endometrial cancer: Role of tumor grade and size. Gynecol Oncol 2009;112: 517–520. 10.1016/j.ygyno.2008.11.009 [DOI] [PubMed] [Google Scholar]
- 8. Lo KW, Cheung TH, Yim SF, Chung TK. Preoperative hysteroscopic assessment of cervical invasion by endometrial carcinoma: a retrospective study. Gynecol Oncol 2001;82: 279–282. [DOI] [PubMed] [Google Scholar]
- 9. Haldorsen IS, Berg A, Werner HM, Magnussen IJ, Helland H, Salvesen OO, et al. Magnetic resonance imaging performs better than endocervical curettage for preoperative prediction of cervical stromal invasion in endometrial carcinomas. Gynecol Oncol 2012;126: 413–418. 10.1016/j.ygyno.2012.05.009 [DOI] [PubMed] [Google Scholar]
- 10. Yurkovetsky Z, Ta'Asan S, Skates S, Rand A, Lomakin A, Linkov F, et al. Development of multimarker panel for early detection of endometrial cancer. High diagnostic power of prolactin. Gynecol Oncol 2007;107: 58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brennan DJ, Hackethal A, Metcalf AM, Coward J, Ferguson K, Oehler MK, et al. Serum HE4 as a prognostic marker in endometrial cancer—a population based study. Gynecol Oncol 2014;132: 159–165. 10.1016/j.ygyno.2013.10.036 [DOI] [PubMed] [Google Scholar]
- 12. Wang D, Yang JX, Cao DY, Wan XR, Feng FZ, Huang HF, et al. Preoperative neutrophil-lymphocyte and platelet-lymphocyte ratios as independent predictors of cervical stromal involvement in surgically treated endometrioid adenocarcinoma. Onco Targets Ther 2013;6: 211–216. 10.2147/OTT.S41711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhou X, Du Y, Huang Z, Xu J, Qiu T, Wang J, et al. Prognostic Value of PLR in Various Cancers: A Meta-Analysis. PLoS One 2014;9: e101119 10.1371/journal.pone.0101119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Toyoda M, Satoh T, Takano K, Sato NO, Oki A, Tsunoda H, et al. Successful diagnosis of thromboembolism before surgery in a woman with clear cell adenocarcinoma of the endometrium. Int J Clin Oncol 2005;10: 444–446. [DOI] [PubMed] [Google Scholar]
- 15. Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol 1983;15: 10–17. [DOI] [PubMed] [Google Scholar]
- 16. Emons G, Fleckenstein G, Hinney B, Huschmand A, Heyl W. Hormonal interactions in endometrial cancer. Endocr Relat Cancer 2000;7: 227–242. [DOI] [PubMed] [Google Scholar]
- 17. Liu FS. Molecular carcinogenesis of endometrial cancer. Taiwan J Obstet Gynecol 2007;46: 26–32. [DOI] [PubMed] [Google Scholar]
- 18. Hecht JL, Mutter GL. Molecular and pathologic aspects of endometrial carcinogenesis. J Clin Oncol 2006;24: 4783–4791. [DOI] [PubMed] [Google Scholar]
- 19. Satoh T, Matsumoto K, Uno K, Sakurai M, Okada S, Onuki M, et al. Silent venous thromboembolism before treatment in endometrial cancer and the risk factors. Br J Cancer 2008;99: 1034–1039. 10.1038/sj.bjc.6604658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kawaguchi R, Furukawa N, Kobayashi H. Cut-off value of D-dimer for prediction of deep venous thrombosis before treatment in ovarian cancer. J Gynecol Oncol 2012;23: 98–102. 10.3802/jgo.2012.23.2.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bozkurt M, Yumru AE, Aral I. Evaluation of the importance of the serum levels of CA-125, CA15-3, CA-19-9, carcinoembryonic antigen and alpha fetoprotein for distinguishing benign and malignant adnexal masses and contribution of different test combinations to diagnostic accuracy. Eur J Gynaecol Oncol 2013;34: 540–544. [PubMed] [Google Scholar]
- 22. Dotters DJ. Preoperative CA 125 in endometrial cancer: is it useful? Am J Obstet Gynecol 2000;182: 1328–1334. [DOI] [PubMed] [Google Scholar]
- 23. Chao A, Tang YH, Lai CH, Chang CJ, Chang SC, Wu TI, et al. Potential of an age-stratified CA125 cut-off value to improve the prognostic classification of patients with endometrial cancer. Gynecol Oncol 2013;129: 500–504. 10.1016/j.ygyno.2013.02.032 [DOI] [PubMed] [Google Scholar]
- 24. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin 2013;63: 11–30. 10.3322/caac.21166 [DOI] [PubMed] [Google Scholar]
- 25. Zaino RJ, Kurman RJ, Diana KL, Morrow CP. Pathologic models to predict outcome for women with endometrial adenocarcinoma: the importance of the distinction between surgical stage and clinical stage—a Gynecologic Oncology Group study. Cancer 1996;77: 1115–1121. [PubMed] [Google Scholar]
- 26. Lee NK, Cheung MK, Shin JY, Husain A, Teng NN, Berek JS, et al. Prognostic factors for uterine cancer in reproductive-aged women. Obstet Gynecol 2007;109: 655–662. [DOI] [PubMed] [Google Scholar]
- 27. Guntupalli SR, Zighelboim I, Kizer NT, Zhang Q, Powell MA, Thaker PH, et al. Lymphovascular space invasion is an independent risk factor for nodal disease and poor outcomes in endometrioid endometrial cancer. Gynecol Oncol 2012;124: 31–35. 10.1016/j.ygyno.2011.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Binder PS, Mutch DG. Update on prognostic markers for endometrial cancer. Womens Health (Lond Engl) 2014;10: 277–288. [DOI] [PubMed] [Google Scholar]
- 29. Wang T, Rohan TE, Gunter MJ, Xue X, Wactawski-Wende J, Rajpathak SN, et al. A prospective study of inflammation markers and endometrial cancer risk in postmenopausal hormone nonusers. Cancer Epidemiol Biomarkers Prev 2011;20: 971–977. 10.1158/1055-9965.EPI-10-1222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dossus L, Rinaldi S, Becker S, Lukanova A, Tjonneland A, Olsen A, et al. Obesity, inflammatory markers, and endometrial cancer risk: a prospective case-control study. Endocr Relat Cancer 2010;17: 1007–1019. 10.1677/ERC-10-0053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Walentowicz-Sadlecka M, Sadlecki P, Bodnar M, Marszalek A, Walentowicz P, Sokup A, et al. Stromal derived factor-1 (SDF-1) and its receptors CXCR4 and CXCR7 in endometrial cancer patients. PLoS One 2014;9: e84629 10.1371/journal.pone.0084629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Suh DH, Kim HS, Chung HH, Kim JW, Park NH, Song YS, et al. Pre-operative systemic inflammatory response markers in predicting lymph node metastasis in endometrioid endometrial adenocarcinoma. Eur J Obstet Gynecol Reprod Biol 2012;162: 206–210. 10.1016/j.ejogrb.2012.02.028 [DOI] [PubMed] [Google Scholar]
- 33. Gallup DG, Stock RJ. Adenocarcinoma of the endometrium in women 40 years of age or younger. Obstet Gynecol 1984;64: 417–420. [PubMed] [Google Scholar]
- 34. Setiawan VW, Yang HP, Pike MC, McCann SE, Yu H, Xiang YB, et al. Type I and II endometrial cancers: have they different risk factors? J Clin Oncol 2013;31: 2607–2618. 10.1200/JCO.2012.48.2596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lo S, Cheng D, Ng TY, Wong LC, Ngan H. Prognostic significance of tumour markers in endometrial cancer. Tumor biology 1997;18: 241–249. [DOI] [PubMed] [Google Scholar]
- 36. Mantovani A, Savino B, Locati M, Zammataro L, Allavena P, Bonecchi R. The chemokine system in cancer biology and therapy. Cytokine Growth Factor Rev 2010;21: 27–39. 10.1016/j.cytogfr.2009.11.007 [DOI] [PubMed] [Google Scholar]
- 37. Black S, Kushner I, Samols D. C-reactive Protein. J Biol Chem 2004;279: 48487–48490. [DOI] [PubMed] [Google Scholar]
- 38. Cushman M, Folsom AR, Wang L, Aleksic N, Rosamond WD, Tracy RP, et al. Fibrin fragment D-dimer and the risk of future venous thrombosis. Blood 2003;101: 1243–1248. [DOI] [PubMed] [Google Scholar]
- 39. Ghezzi F, Cromi A, Siesto G, Giudici S, Serati M, Formenti G, et al. Prognostic significance of preoperative plasma fibrinogen in endometrial cancer. Gynecol Oncol 2010;119: 309–313. 10.1016/j.ygyno.2010.07.014 [DOI] [PubMed] [Google Scholar]
- 40. Case AS, Rocconi RP, Straughn JJ, Conner M, Novak L, Wang W, et al. A prospective blinded evaluation of the accuracy of frozen section for the surgical management of endometrial cancer. Obstet Gynecol 2006;108: 1375–1379. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to ethical restrictions related to patient confidentiality, all relevant data are available upon request to the corresponding author.