Abstract
A great deal of clinical cancer care is delivered in the home by informal caregivers (e.g. family, friends), who are often untrained. Caregivers' context varies widely, with many providing care despite low levels of resources and high levels of additional demands.
Background
Changes in health care have shifted much cancer care to the home, with limited data to inform this transition. We studied the characteristics, care tasks, and needs of informal caregivers of cancer patients.
Methods
Caregivers of seven geographically and institutionally defined cohorts of newly diagnosed colorectal and lung cancer patients completed self-administered questionnaires (n = 677). We combined this information with patient survey and chart abstraction data and focused on caregivers who reported providing, unpaid, at least 50% of the patient's informal cancer care.
Results
Over half of caregivers (55%) cared for a patient with metastatic disease, severe comorbidity, or undergoing current treatment. Besides assisting with activities of daily living, caregivers provided cancer-specific care such as watching for treatment side effects (68%), helping manage pain, nausea or fatigue (47%), administering medicine (34%), deciding whether to call a doctor (30%), deciding whether medicine was needed (29%), and changing bandages (19%). However, half of caregivers reported not getting training perceived as necessary. In addition, 49% of caregivers worked for pay, 21% reported poor or fair health, and 21% provided unpaid care for other individuals. One in four reported low confidence in the quality of the care they provided.
Conclusions
Much assistance for cancer patients is delivered in the home by informal caregivers, often without desired training, with a significant minority having limited resources and high additional demands. Future research should explore the potentially high yield of addressing caregiver needs in improving quality of cancer care and both survivors' and caregivers' outcomes.
Keywords: cancer, oncology, caregivers, burden, stress, informal care
Background
Approximately 1.4 million individuals in the United States were diagnosed with cancer in 2008 [1]. With this diagnosis, the individual will face significant life disruptions associated with cancer treatments, symptoms, and financial burdens. In addition, the impact of a cancer diagnosis extends well beyond those diagnosed to affect the entire family [2–4]. Family and friends may be called upon to provide emotional and instrumental support and often assume the patient's responsibilities while simultaneously experiencing their own emotional response to their loved-one's illness [5,6]. Across all chronic conditions, there may be as many as 44 million of these informal caregivers in the United States, with an estimated 4 million caring for loved ones with cancer [7].
The burden on informal (unpaid family and friend) caregivers of cancer patients has increased in recent years as a result of the shift of the majority of cancer care from inpatient to outpatient settings. Family members are increasingly asked to perform clinical care tasks that until recently would have been performed by trained health-care providers. Caregivers of elderly cancer patients face an increasingly complex set of challenges created by the patient's pre-existing comorbid conditions combined with more aggressive treatment and prolonged survival after diagnosis [5,8].
Characterizing the experiences of caregivers of cancer patients is challenging because patient characteristics vary widely [9] and cancer caregivers themselves are a highly heterogeneous group. While some family caregivers have a deep well of personal, social, and economic resources to draw upon to cope with the stress of caregiving, others have a very shallow pool of resources. Many must also cope with competing demands or stressors including employment, childcare, and their own poor health.
Despite widespread acknowledgement of the crucial role played by family caregivers of cancer patients, our knowledge of the care tasks that family caregivers perform, their other stressors and demands, and the resources they can bring to caregiving is limited. While there has been increasing research attention to cancer caregivers over the past decade, many of the published studies involve nonrepresentative convenience samples and the majority of studies solely examine survey data from the caregiver. Thus, despite providing important information, these analyses cannot place the caregiver's reported burden in the context of the cancer patient's objective clinical need for care.
This study represents a step toward filling some of these gaps in our understanding of the diverse experiences of cancer caregivers. We describe the characteristics, care tasks, resources, and other role demands/stressors experienced by the primary family caregivers of 677 lung and colorectal cancer patients who were ascertained from five geographically dispersed cancer registries and two nationally dispersed health-care systems. We use these findings to guide suggestions for future research and policy directions.
Materials and methods
Sample
Caregivers were nominated by recently diagnosed lung and colorectal cancer patients who participated in the Share Thoughts on Care survey conducted by the Cancer Care Outcomes Research and Surveillance (CanCORS) consortium. The CanCORS consortium was composed of seven independent study sites that used identical lockstep data collection methods. Five of the sites ascertained cancer patients from cancer registries and two from health-care systems. The CanCORS study of lung and colorectal cancer patients has been described in more detail elsewhere [10].
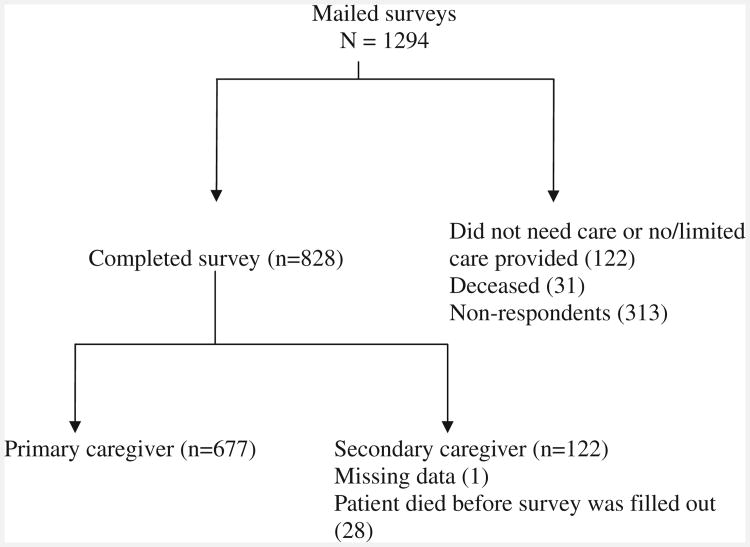
This study utilizes both medical record and patient survey data in addition to caregiver survey data. Patients were interviewed approximately four months after their diagnosis and their medical records were abstracted about a year later. A consecutive subsample of patients was asked to name and provide contact information for the caregiver, or the person who was ‘most likely to care for you should you need it’. Within three weeks of the patient interview, the 1294 caregivers identified by the patient were mailed a self-administered questionnaire, information about the study, a postage-paid return envelope, and $20 incentive. Thus, caregiver data were collected approximately 5–6 months after the patients' cancer diagnosis. As shown in Figure 1, of the 1294 caregivers who were identified through the patient interview and sent questionnaires, 122 provided information indicating that either the patient did not need care or the caregiver did not provide any care, and 31 reported that the patient had died. These cases were eliminated from the sample, leaving 1141 caregivers. Of these, 828 (73%) completed and returned a questionnaire. Of the 828, 122 reported that they provided less than half the informal care the patient needed, 28 were removed when medical records information indicated that the patient had died before the caregiver completed the survey, and one respondent failed to indicate the amount of care provided, leaving a sample of 677 primary caregivers.
Figure 1. Caregivers of cancer patients: total response rate and eligibility for analysis flowchart.
Measures
Objective caregiver burden
Patient clinical need was based on documentation in the cancer patient medical record of one or more of the following: metastatic disease, having undergone cancer treatment within the four weeks prior to the survey, and/or severe comorbidity. Each patient was assigned an overall comorbidity score on an ordinal scale of mild, moderate, and severe according to the highest ranked single ailment of the 25 ailments in the ACE-27 [11]. In cases where two or more ailments in different organ systems were scored ‘moderate’, the overall comorbidity score was designated as severe.
Average hours per week spent providing care is the product of two items on the caregiver questionnaire: ‘Thinking about all the care you provide to your Care Recipient due to his or her illness, on average, on how many days a week do you provide care?’ and ‘On a typical day, about how many hours do you provide some care to your Care Recipient due to his or her illness?’ The results were divided into three categories: ‘less than 20 h per week’, ‘21–40h per week’, or ‘more than 40 h per week’. Assistance with Activities of Daily Living (ADL), Instrumental Activities of Daily Living (IADL), and Clinical Care Tasks were assessed by asking respondents whether they performed a series of tasks in the past two weeks. Response options were ‘yes’, ‘no’, or ‘not needed’. The development of the Clinical Care tasks measure was guided by the CanCORS steering committee, a committee is composed of nationally recognized cancer-care providers, researchers, cancer survivors, and caregivers, and then refined during cognitive interviews.
Caregiver resources
Self-efficacy/perceived preparedness for Caregiving was assessed using two items from the preparedness subscale of the Family Caregiving Inventory [12] that measure how confident the respondent feels regarding caring for the patient's emotional needs and caring for the patient's physical needs. Response options range from ‘not at all confident’ to ‘extremely confident’ on a 5-point scale. Perceived social support was measured using the MOS Social Support Scale, a widely used [13–15] 16-item scale developed for the Medical Outcomes Study [15]. This scale also has strong internal consistency (Cronbach's alpha50.97). Whether they had used paid help was assessed by asking ‘Have you had any paid helpers assisting you or your Care Recipient as a result of his or her cancer?’ Caregiver training was assessed by asking caregivers: ‘Sometimes doctors, nurses, home health aides, social workers, or some other health-care provider will train, teach, or show caregivers how to do the things their care recipients need. Did any health care or other provider give you any training or show you how to change bandages, administer medicine, manage nausea, manage pain, manage fatigue, manage other side effects or symptoms, and provide other treatments?’ Household Income was assessed using a standard item asking ‘What was your total household income from all sources for the past year? (Include income from jobs, self-employment, Social Security, Railroad Retirement, other retirement income, Supplemental Security Income (SSI), pensions, interest, and any other sources).’ Proportion under the poverty threshold and 150% of the poverty threshold was calculated by dividing household income by the number of people in the household. The result was compared to the poverty threshold established by the US Census every year [16].
Other role demands and stressors
In this cross-sectional study, caregiver poor health status was conceptualized as an additional burden with its own set of coping demands. Caregiver health was measured using a single item that composes the General Health subscale of the SF-12, [17] a relatively robust predictor of mortality in US populations [18,19]. Caregivers were asked ‘In general, how would you say your health is now?’ Response options were ‘excellent’, ‘very good’, ‘good’, ‘fair’, or ‘poor’. Caregivers were considered to have poor health status if they responded ‘fair’ or ‘poor’. To assess employment status, caregivers were asked if they worked for pay, ‘Yes’ or ‘No’. Responsibility for caring for others was determined by responses to ‘Do you provide unpaid care to any other adults in addition to your Care Recipient (who has a lung or colorectal disease such as cancer)?’ and ‘Do you provide unpaid care for children (yours or someone else's)?’ If they answered yes to either, they were coded as having other care responsibilities. Role strain was measured using a single question: ‘In general, how difficult is it for you to balance work and caregiving demands?’ with five response options ranging from ‘Not at all difficult’ to ‘Extremely difficult’.
Results
Caregiver characteristics
There were few differences between caregivers of lung and colorectal cancer patients. More lung cancer patient caregivers (37%, n = 124) than colorectal cancer caregivers (28%, n = 92) were in the over 65 age group (p = 0.03), and more colorectal cancer patients than lung cancer patients were black (20 vs 10%, respectively) or Hispanic (7 vs 2%, respectively). Otherwise, there were no significant differences between the two groups. Therefore, in Table 1 we present characteristics of all caregivers. Over half (63%, n = 426) of the caregivers were married to the patient (50% wives, 13% husbands), while 12% (n = 83) were adult children of the patient (10% daughters, 2% sons). Twenty-five percent of the caregivers (n = 167) had other relationships to the patient, primarily other family members. Most caregivers were women (79%, n = 525). Overall, 25% (n = 165) of primary caregivers reported being members of a racial and/or ethnic minority group, similar to the proportion of cancer patients for whom they provided care. Caregivers ranged in age from 21 to over 80, with most of the sample (67%, n = 443) under age 65. Most caregivers had at least a high-school education, with only 13% (n = 84) reporting not completing high school. The majority of respondents were married (79%, n = 524).
Table 1. Characteristics of 677 informal caregivers for lung and colorectal cancer patients.
| Caregiver characteristic | % (n =) |
|---|---|
| Relationship to patient | |
| Spouse | 63% (426) |
| Adult child | 12% (83) |
| Other | 25% (167) |
| Sex | |
| Male | 21% (136) |
| Female | 79% (525) |
| Race | |
| Black | 15% (99) |
| Native American | 3% (20) |
| Hispanic | 4% (27) |
| Asian | 2% (12) |
| White | 75% (499) |
| Other | 1% (7) |
| Age | |
| 21–50 | 24% (161) |
| 51–65 | 43% (282) |
| Over 65 years | 33% (216) |
| Education | |
| Less than high-school diploma | 13% (84) |
| High-school graduate | 28% (190) |
| Some college or 2 year degree | 41% (276) |
| College graduate or higher | 18% (118) |
| Marital status | |
| Married | 79% (524) |
| Unmarried (any reason) | 21% (142) |
| Health status | |
| Poor | 3% (18) |
| Fair | 18% (122) |
| Good | 36% (247) |
| Very good | 31% (207) |
| Excellent | 11% (74) |
Objective burden
Cancer patients varied widely in their clinical characteristics and the corresponding level of care they need. Twenty-seven percent (n = 180) had metastatic disease at the time of the caregiver survey, 20% (n = 125) had severe comorbidity, and 31% (n = 211) had undergone treatment (surgery, chemotherapy, or radiation) within two weeks of the caregiver survey. Over half (54%, n = 366) had one or more of these clinical factors, thus falling into the high-need category. Of these, 19% (n = 130) had two or more high clinical need markers.
Tables 2 and 3 present caregivers' report on their objective burden. After taking into account patient clinical need, care tasks did not differ significantly by cancer site with the exception of the task ‘Give oxygen, give a nebulizer treatment or perform chest percussions’ which is specific to lung cancer and so caregivers of patients with both cancer sites are presented together. More than half of the care-givers (63%, n = 396) spent fewer than 20h a week, 20% (n = 125) between 21 and 40h, and 17% (n = 108) reported over 40 h a week providing care. Those caring for a ‘high-need patient’ reporting significantly more caregiving hours than their counterparts and were more likely to perform almost all specific care tasks.
Table 2. Intensity of care for informal caregivers of cancer patients, by level of cancer patient need.
| Not high-needa PATIENT (N = 311) | High-need patient*** (N = 366) | Combined (N = 677) | Sig. | |
|---|---|---|---|---|
| Average number of hours per week provided care % (N) | ||||
| Less than 20 | 70% (202) | 57% (194) | 63% (396) | 0.002 |
| 21–40 | 16% (47) | 23% (78) | 20% (125) | |
| Over 40 | 13% (38) | 21% (70) | 17% (108) | |
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| Mean number of unique activities of daily living caregiver assisted with in last two weeks | 0.96 (1.82) | 1.44 (2.11) | 1.22 (1.20) | 0.002 |
| Mean number of unique instrumental activities of daily living caregiver assisted with in last two weeks | 3.00 (2.39) | 3.89 (2.22) | 3.48 (2.34) | 0.000 |
| Mean Number of Unique Clinical Care Tasks Caregiver performed in last two weeks | 2.32 (2.23) | 3.60 (2.03) | 3.01 (2.21) | 0.000 |
| Mean Number of All Care Tasks Combined in last Two Weeks | 6.28 (5.43) | 8.93 (4.99) | 7.71 (5.36) | 0.000 |
High-need patient = a patient with metastatic disease, severe comorbidity, or undergoing treatment at time survey was filled out.
All differences between high need and not high need groups are statistically significant at p<0.05.
Table 3. Proportion of informal cancer caregivers reporting performing specific task in past two weeks, by level of cancer patient need.
| In past two weeks, have you helped your care recipient… | Not high-need patienta (%) (N = 311) | High-need patient*** (%) (N = 366) | Combined (%) (N = 677) | Sig. | |
|---|---|---|---|---|---|
| Activities of daily living | Get around inside | 17 | 26 | 22 | 0.003 |
| Get around outside | 17 | 28 | 23 | 0.002 | |
| Eat | 11 | 13 | 12 | ns | |
| Get in or out of bed | 11 | 15 | 13 | ns | |
| Get dressed | 16 | 22 | 19 | ns | |
| Bathe | 13 | 20 | 17 | 0.011 | |
| Get on or off the toilet | 4 | 7 | 5 | ns | |
| Clean him or herself after s/he used the toilet | 5 | 8 | 6 | ns | |
| With a bedpan | 1 | 1 | 1 | ns | |
| With a catheter or colostomy bag | 6 | 10 | 8 | 0.043 | |
| Instrumental activities of daily living | Managed his or her money | 36 | 47 | 42 | 0.006 |
| Made telephone calls for your Care Recipient | 38 | 51 | 45 | 0.001 | |
| Done housework your wouldn't normally do | 43 | 54 | 49 | 0.005 | |
| Washed laundry you wouldn't normally do | 33 | 41 | 38 | 0.029 | |
| Shopped for your Care Recipient's groceries | 56 | 67 | 62 | 0.002 | |
| Driven your Care Recipient to a doctor's office, clinic or hospital | 52 | 65 | 59 | 0.001 | |
| Had to do other chores and tasks your Care Recipient would normally do if he or she was not ill | 53 | 72 | 63 | 0.000 | |
| Clinical care tasks | Help administer medicine to your Care Recipient | 27 | 40 | 34 | 0.000 |
| Make a decision about whether your Care Recipient needed medication | 19 | 37 | 29 | 0.000 | |
| Keep track of or watch for side effects from your Care Recipient's treatment | 53 | 81 | 68 | 0.000 | |
| Spend time assisting your Care Recipient manage or control symptoms such as nausea/vomiting, fatigue or pain | 35 | 57 | 47 | 0.000 | |
| Change your Care Recipient's bandages | 15 | 22 | 19 | 0.024 | |
| Give oxygen, give a nebulizer treatment or perform chest percussions | 6 | 8 | 7 | ns | |
| Decide whether to call a doctor | 23 | 36 | 30 | 0.000 | |
| Accompany your Care Recipienttotreatmentsordoctor's appointments | 61 | 83 | 73 | 0.000 |
High-need patient = a patient with metastatic disease, severe comorbidity, or undergoing treatment at time survey was filled out.
All differences between high need and not high need groups statistically significant at p<0.05.
Caregiver training
As shown in Table 4, for each of six clinical care tasks, caregivers reported whether they received, did not receive, or did not need training for the tasks they performed. There were no significant differences by cancer site in reports on training received. Depending on the task, between one half and one third of caregivers reported needing, but not receiving training for the following: managing fatigue, administering medications, managing nausea, managing pain, changing wound bandages, and managing other symptoms.
Table 4. Training in clinical care tasks received by cancer caregivers, by perception of need for training.
| Training not received % (n) | Training received % (n) | Training not needed % (n) | |
|---|---|---|---|
| …manage fatigue? | 47% (314) | 29% (192) | 24% (156) |
| …administer medicine? | 44% (297) | 22% (148) | 33% (218) |
| …manage nausea? | 43% (282) | 22% (145) | 36% (235) |
| …manage pain? | 41% (274) | 29% (189) | 30% (201) |
| …change bandages? | 36% (238) | 19% (129) | 45% (297) |
| …manage other side effects or symptoms? | 49% (324) | 26% (175) | 25% (163) |
Other role demands and stressors
Most caregivers face other role demands or stressors in addition to the stress of caring for the cancer patient: 21% (n = 142) cared for at least one other individual and 49% (n = 312) were employed (including 2/3 full time). One in five reported suffering from ‘poor’ to ‘fair’ health. Examining all these role demands/stressors together, 67% (n = 453) of caregivers faced at least one, and 19% (n = 131) faced two or more of these additional demands. However, of those who worked, 28% (86) reported that it was somewhat-to-extremely difficult to balance work and caregiving demands.
Resources
The majority of caregivers felt ‘very’ to ‘extremely’ confident 71% (n = 472) when asked about providing physical care for the care recipient. However, they felt much less confident when asked about care of emotional needs of the care recipients, with only 49% (n = 312) feeling ‘very’ to ‘extremely’ confident and 12% (n = 80) feeling ‘a little’ to ‘not at all’ confident.
Variations in the availability of social resources were also noted. In this sample, 63% (n = 407) of the caregivers reported they alone provided all of the care their loved one needed, while 37% (n = 235) received some assistance from at least one other person. A significant minority reported getting very little social support of any kind. MOS global social support scores fell below 3 on a scale ranging from 1 to 5 for 22% (n = 149) of the sample, indicating that social support is available to them either ‘not at all’ or only ‘a little’ of the time. Only 12% (n = 76) responded ‘yes’ when asked if they had any assistance from paid helpers. Of these, 61 (76%) reported that a ‘nurse, doctor, therapist, or social worker’ had come to their home, 39 (49%) had ‘a paid helper for household chores’, and 32 (40%) had assistance from a ‘home health aide’ as a result of their care recipient's cancer.
Caregivers varied widely in their financial resources, with 27% (n = 160) reporting that they lived in households bringing in less than $20 000 year, 29% (n = 171) were in households earning $20 000–$40 000, and 44% (n = 267) had household incomes over $40 000. Applying the Department of Health and Human Service's criteria for defining households as above or below the poverty threshold, 13% (n = 89) of caregivers are below the poverty threshold and 22% (n = 148) are below 150% of the poverty threshold.
Discussion
The 677 informal lung and colorectal cancer caregivers in this study were preponderantly relatives of the patient (spouse or adult child), female, and over 50 years old, with about 40% spending on caregiving the equivalent of adding an additional half-time job to their pre-existing life demands (at least 21 h per week). About half cared for patients who had one or more clinical characteristics associated with high need for care: metastatic disease, currently undergoing cancer treatment, or severe comorbidity, with large portions of caregivers assisting patients, whether high need or not, in activities that would have been provided by trained nursing personnel in hospital. Further, large proportions of caregivers perceived unmet needs for training in providing this assistance.
The relationship between objective burden and caregiver mental-health and physical-health outcomes has been found to vary by caregiver resources, such that caregivers with significant coping, social, and material resources are less likely to suffer deleterious consequences as a result of caregiving demands, while those with few resources are at elevated risk [20–25]. Given this prior evidence, a significant proportion of the caregivers are at high risk for poor outcomes. Over half shouldered the burden of caregiving with little or no help from other informal caregivers. Only 12% had help from paid caregivers. Over 20% (n = 149) had low levels of any kind of social support. Furthermore, a significant proportion of caregivers reported limited financial resources. Most caregivers in this sample reported having major life demands in addition to caregiving.
Other life stressors and demands have the potential to influence caregiver outcomes both through exacerbating role conflict and disruption [9,26,27] as well as by increasing total burden on the caregiver or allostatic load [28]. Almost half (49%, n = 313) of the caregivers reported paid employment, with 32% (n = 213) working full time. Twenty-one percent (n = 142) had responsibility for the care of at least one other person. In addition, 21% (n = 140) reported providing care while struggling with significant health problems. Poor health is an emotionally and physically depriving experience that creates a variety of coping demands [29,30]. These results suggest that most caregivers who serve as the primary source of care for lung or colorectal cancer patients face significant life demands in addition to cancer caregiving, with 19% (n = 131) in this sample dealing with two major demands on top of caregiving. These demands have the potential to result in significant allostatic load and may create secondary stress in terms of role conflict. Indeed, overall 28% (n = 86) of the respondents who were working either full or part time reported having difficulty balancing work and caregiving demands. Thus, significant proportions of caregivers are at risk for strain, poor mental health, and diminished quality of life [31].
We know little about the role of informal caregiving on patient outcomes. In our sample, caregivers provided a great deal of clinical care. About half of informal caregivers helped patients mange symptoms such as nausea, vomiting, fatigue, or pain; one-third helped to decide whether to call a physician, and about 70% monitored side effects of cancer treatment. Yet, depending on the specific activity, between one-third and one-half of caregivers providing such assistance perceived unmet training needs in the activity.
Limitations
The results of this study should be interpreted in light of survey nonresponse bias. At least 27% (313) of caregivers did not return a survey. In addition, caregivers participating in this study were nominated by patients who participated in a larger stratified random sample study of lung and colorectal cancer patients with a 60% response rate. The characteristics of the nonresponding caregivers are unknown, but there is considerable evidence from other studies to suggest that nonrespondents are more likely to be low-income, members of a racial and/or ethnic minority group, and sicker than respondents [32,33]. This would suggest that these results may underestimate the experiences of caregivers of the sickest cancer patients, as well as the proportion of caregivers who are poor and themselves struggling with ill health.
Future directions
The results of this study point to five areas that need further research and program or policy formation. First, we need to better understand what these results mean for patients and patient care. Thirteen percent of patients (n = 89) are depending on caregivers who are living in poverty and 19% (n = 131) on caregivers who have two or more other significant stressors or demands. A large amount of activities that might be delivered by professionals visiting the home is relegated to informal caregivers. In many cases, the caregiver did not get desired training in the clinical care tasks they deliver. Since so much of cancer care is being provided by unpaid family caregivers, the current focus and priority on assessing and improving quality of cancer care should be extended to the care provided in the home.
Second, we need valid and feasible strategies for assessing cancer caregiver training needs and greater understanding of the best methods and timing for providing such training. Although there are a number of existing programs with some evaluation [34–38], there is considerable room for the development of new interventions targeting caregiver skills.
Third, these findings point to the responsibility that cancer-care providers have for assessing family caregivers' needs for support and training as part of quality care for cancer patients. When performed, this assessment should then lead to training in the skills caregivers need to take care of the patient at home. However, since cancer patients and caregivers may interact with many cancer providers, it is not always clear which provider should take on this responsibility. Thus, without adequate care coordination, caregiver training may be neglected. Care systems should develop policies and procedures that will result in care coordination that includes caregiver assessment, training, and support as part of routine care. In addition, cancer providers themselves may need training and other resources in order to gain competence and comfort in assessing and remedying gaps in caregiver skills.
Fourth, the large number of low-income caregivers observed in this study points to the need for material and instrumental resources. There is little question that such programs have benefited dementia patient caregivers [39], but their ideal structure for cancer caregivers is unknown. In 2000, the US Congress enacted legislation establishing the National Family Caregiver Support Program, which is intended to provide services that will support and sustain the primary, unpaid caregiver. However, this has been unevenly implemented and, thus far, there has been no implementation, process, or outcome evaluation of its impact. Some states have programs that pay family caregivers to provide homemaker, chore, and personal care services. Most use state funds to compensate families, while other states use Medicaid waiver funds. Furthermore, the large percentage of cancer caregivers who combine work for pay and caregiving highlights the great need for more intensive research and policy development focused on the needs of caregivers in the workforce. Cancer providers can make a significant impact by identifying resource gaps and pointing patients and caregivers to health system and community resources that can help address those gaps.
Fifth, too many caregivers are functioning with little social support. Unfortunately, the best way to increase social support for cancer caregivers is uncertain. Very few of the caregivers in this sample reported having ever attended a support group. In addition, while there has been extensive research on the nature and effectiveness of support groups for dementia caregivers, there has been little focus on cancer caregivers. The development and evaluation of innovative approaches to increased available support, including web-based support groups [40], should be a priority for future research.
Last, it is clear that no one-size-fits-all approach will be adequate. The results presented here point to the need for tailoring both the types and intensity of help to the specific level of burden, available resources, and additional demands family caregivers face.
In summary, our findings suggest that focusing on the quality of care delivered to cancer patients in their home may be an important avenue to improve their overall outcomes. Further, a large group of informal caregivers may themselves be at risk for deleterious health and social consequences due to their cancer caregiver burden. As the US population ages and cancer becomes increasingly prevalent, these issues may have profound health policy implications.
Acknowledgments
This study is supported by grants from the National Cancer Institute (U01 CA93324, U01 CA93326, U01 CA93329, U01 CA93332, U01 CA93339, U01 CA93344, and U01 CA93348) and the Department of Veterans Affairs (CRS 02-164).
Footnotes
The contributions of Joan Griffin, Audie Atienza and Julia Rowland to this article were prepared as part of their official duties as United States Federal Government employees
None of the authors have a financial disclosure or conflict of interest. The views expressed represent those of the authors and not those of the National Cancer Institute, National Institutes of Health.
References
- 1.Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007;57(1):43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 2.Kim Y, Given BA. Quality of life of family caregivers of cancer survivors: across the trajectory of the illness. Cancer. 2008;112(11 Suppl):2556–2568. doi: 10.1002/cncr.23449. [DOI] [PubMed] [Google Scholar]
- 3.Davis-Ali S, Chesler M, Chesney B. Recognizing cancer as a family disease: worries and support reported by patients and spouses. OC Work Health Care. 1993;19(2):45–65. doi: 10.1300/J010v19n02_02. [DOI] [PubMed] [Google Scholar]
- 4.Deeken JF, Taylor KL, Mangan P, Yabroff KR, Ingham JM. Care for the caregivers: a review of self-report instruments developed to measure the burden, needs, and quality of life of informal caregivers. J Pain Symptom Manage. 2003;26(4):922–953. doi: 10.1016/s0885-3924(03)00327-0. [DOI] [PubMed] [Google Scholar]
- 5.Given B, Sherwood P. Family care for the older person with cancer. Semi Oncol Nurs. 2006;22(1):43–50. doi: 10.1016/j.soncn.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 6.Madden J. The problem of distress in patients with cancer. Clin J Oncol Nurs. 2006;10(5):615–619. doi: 10.1188/06.CJON.615-619. [DOI] [PubMed] [Google Scholar]
- 7.Caregiving in the US: Bethesda: National Alliance for Caregiving. Washington, DC: AARP; 2004. [Google Scholar]
- 8.Weitzner MA, Haley WE, Chen H. The family caregiver of the older cancer patient. Hematol Oncol Clin North Am. 2000;14(1):269–281. doi: 10.1016/s0889-8588(05)70288-4. [DOI] [PubMed] [Google Scholar]
- 9.Nijboer C, Triemstra M, Tempelaar R, Sanderman R, van den Bos GA. Determinants of caregiving experiences and mental health of partners of cancer patients. Cancer. 1999;86(4):577–588. doi: 10.1002/(sici)1097-0142(19990815)86:4<577::aid-cncr6>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 10.Ayanian JZ, Chrischilles EA, Fletcher RH, et al. Understanding cancer treatment and outcomes: the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2004;22(15):2992–2996. doi: 10.1200/JCO.2004.06.020. [DOI] [PubMed] [Google Scholar]
- 11.Piccirillo J, Costas I, Claybour P, Borah A, Grove L, Jeffe D. The measurement of comorbidity by cancer registries. J Registry Manage. 2003;30(8):8–14. [Google Scholar]
- 12.Schumacher KL, Stewart BJ, Archbold PG. Conceptualization and measurement of doing family caregiving well. Image J Nurs Sch. 1998;30(1):63–69. doi: 10.1111/j.1547-5069.1998.tb01238.x. [DOI] [PubMed] [Google Scholar]
- 13.Grunfeld E, Coyle D, Whelan T, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ. 2004;170(12):1795–1801. doi: 10.1503/cmaj.1031205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sherbourne CD, Hays RD, Ordway L, DiMatteo MR, Kravitz RL. Antecedents of adherence to medical recommendations: results from the Medical Outcomes Study. J Behav Med. 1992;15(5):447–468. doi: 10.1007/BF00844941. [DOI] [PubMed] [Google Scholar]
- 15.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 16.2007 HHS Poverty Guidelines Federal Register. 2007;72(15):3147–3148. [Google Scholar]
- 17.Ware JE, Jr, Kosinski M, Turner-Bowker D, Gandek B. How to Score Version 2 of the SF-12 Health Survey. QualityMetric, Inc.; Lincoln, RI: 2005. [Google Scholar]
- 18.Idler Y, Benyami S. Self rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 19.Chandola T, Crispin J. Validating self-rated health in different ethnic groups. Ethn Health. 2000;5:115–151. doi: 10.1080/713667451. [DOI] [PubMed] [Google Scholar]
- 20.Kim Y, Baker F, Spillers RL, Wellisch DK. Psychological adjustment of cancer caregivers with multiple roles. Psycho-Oncology. 2006;15(9):795–804. doi: 10.1002/pon.1013. [DOI] [PubMed] [Google Scholar]
- 21.Pinquart M, Sorensen S. Gender differences in caregiver stressors, social resources, and health: an updated meta-analysis. J Gerontol B Psychol Sci Soc Sci. 2006;61(1):33–45. doi: 10.1093/geronb/61.1.p33. [DOI] [PubMed] [Google Scholar]
- 22.Cameron JI, Herridge MS, Tansey CM, McAndrews MP, Cheung AM. Well-being in informal caregivers of survivors of acute respiratory distress syndrome. Crit Care Med. 2006;34(1):81–86. doi: 10.1097/01.ccm.0000190428.71765.31. [DOI] [PubMed] [Google Scholar]
- 23.Hirst M. Carer distress: a prospective, population-based study. Soc Sci Med. 2005;61(3):697–708. doi: 10.1016/j.socscimed.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 24.Aneshensel CS, Botticello AL, Yamamoto-Mitani N. When caregiving ends: the course of depressive symptoms after bereavement. J Health Soc Behav. 2004;45(4):422–440. doi: 10.1177/002214650404500405. [DOI] [PubMed] [Google Scholar]
- 25.Coon DW, Rubert M, Solano N, et al. Well-being, appraisal, and coping in Latina and Caucasian female dementia caregivers: findings from the REACH study. Aging Ment Health. 2004;8(4):330–345. doi: 10.1080/13607860410001709683. [DOI] [PubMed] [Google Scholar]
- 26.Cameron JI, Franche RL, Cheung AM, Stewart DE. Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer. 2002;94(2):521–527. doi: 10.1002/cncr.10212. [DOI] [PubMed] [Google Scholar]
- 27.Devins GM. Illness intrusiveness and the psychosocial impact of lifestyle disruptions in chronic life-threatening disease. Adv Ren Replace Ther. 1994;1(3):251–263. doi: 10.1016/s1073-4449(12)80007-0. [DOI] [PubMed] [Google Scholar]
- 28.Stewart JA. The detrimental effects of allostasis: allostatic load as a measure of cumulative stress. J Physiol Anthropol. 2006;25(1):133–145. doi: 10.2114/jpa2.25.133. [DOI] [PubMed] [Google Scholar]
- 29.Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychol Bull. 2007;133(6):920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- 30.LeMaistre J. After the Diagnosis: From Crisis to Personal Renewal for Patients with Chronic Illness. Ulysses Press; Berkeley, CA: 1995. [Google Scholar]
- 31.Penson RT, Dignan FL, Canellos GP, Picard CL, Lynch TJ., Jr Burnout: caring for the caregivers. Oncologist. 2000;5(5):425–434. [PubMed] [Google Scholar]
- 32.Edwards P, Roberts I, Clarke M, et al. Methods to increase response rates to postal questionnaires. Cochrane database of systematic reviews. 2007;(2):MR000008. doi: 10.1002/14651858.MR000008.pub3. Online. [DOI] [PubMed] [Google Scholar]
- 33.Groves RM, Dillman DA, Eltinge J, Little RA. Survey Nonresponse. Wiley; New York, NY: 2001. [Google Scholar]
- 34.Ferrell BR, Ferrell BA, Ahn C, Tran K. Pain management for elderly patients with cancer at home. Cancer. 1994;74(7 Suppl):2139–2146. doi: 10.1002/1097-0142(19941001)74:7+<2139::aid-cncr2820741722>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 35.Riley-Clark A, Shuman E. Tool facilitates multiple caregiver teaching. Oncol Nurs Forum. 1993;20(5):825. [PubMed] [Google Scholar]
- 36.Cashman R, Bernstein LJ, Bilodeau D, et al. Evaluation of an educational program for the caregivers of persons diagnosed with a malignant glioma. Can Oncol Nurs J. 2007;17(1):6–15. doi: 10.5737/1181912x171610. [DOI] [PubMed] [Google Scholar]
- 37.Ortiz de Cuevas LH, Lopez Campo JH. A program for the home care of patients with a symptomatic malignant terminal disease. Cancer Nurs. 1995;18(5):368–373. [PubMed] [Google Scholar]
- 38.Reis J, McGinty B, Jones S. An e-learning caregiving program for prostate cancer patients and family members. J Med Syst. 2003;27(1):1–12. doi: 10.1023/a:1021040911088. [DOI] [PubMed] [Google Scholar]
- 39.Bass DM, Noelker LS, Rechlin LR. The moderating influence of service use on negative caregiving consequences. J Gerontol B Psychol Sci Soc Sci. 1996;51(3):S121–S131. doi: 10.1093/geronb/51b.3.s121. [DOI] [PubMed] [Google Scholar]
- 40.Monnier J, Laken M, Carter CL. Patient and caregiver interest in internet-based cancer services. Cancer Pract. 2002;10(6):305–310. doi: 10.1046/j.1523-5394.2002.106005.x. [DOI] [PubMed] [Google Scholar]