Abstract
The diagnosis of a food allergy generally has a considerable impact on patients. Not does it result in dietary restrictions, it is often also associated with a constant threat scenario, given the risk of sudden allergic reactions, including life-threatening anaphylaxis. It is essential for patients to receive training on how to deal with emergency situations and make the correct decision regarding the use of emergency medication. Severe allergic reactions occur only rarely if patients are well informed. However, the fear of allergic reactions results in a significant impairment in quality of life (QoL).
In recent years, numerous studies have been carried out on QoL in food-allergy and anaphylaxis patients. These studies provide insight into patient behaviour in everyday life. More importantly, by means of targeted and specific counselling, they also make it possible to reduce adverse effects on QoL and improve avoidance behaviour and compliance in terms of the requisite emergency measures.
The present article summarizes the available data and formulates recommendations aimed at improving the care of food-allergy patients in terms of QoL and compliance.
Key words: Food allergy, anaphylaxis, quality of life, children, adolescents, adults
Background
Anaphylaxis is a potentially life-threatening disease. All too often, food-allergy patients or their relatives are confronted with situations in which affected individuals suddenly develop symptoms that may be an allergic reaction. These symptoms can be initially mild, developing at varying speeds into life-threatening symptoms such as respiratory distress, impaired consciousness or severe abdominal cramping. The fact that neither the time of onset nor the intensity of the reaction is predictable can significantly reduce quality of life (QoL).
However, recent reviews and studies have shown that the occurrence of a fatal reaction in food allergic patients is rare [1, 2], with an annual incidence of 1.8 in adults and 3.25 in children and adolescents per million person-years. Thus, a food allergic patient in Europe is more likely to die as a result of murder or fire than of an allergic reaction. The fact that only few fatalities are seen — despite often inadequate treatment and a failure to use adrenaline — is yet another clear sign of the often benign course of severe adverse reactions [2, 3]. Therefore, preventing fatalities is not the sole and central aim of treating and informing patients at risk of anaphylaxis; instead, emphasis should be put on increasing everyday safety and prescribing medication suited to controlling the acute symptoms of an adverse reaction rapidly and sustainably.
Instruments to measure the efficacy of therapeutic or diagnostic measures based on the patient’s own perception of symptoms (patient-reported outcomes such as symptom-medication scores) have been developed. Since mortality is low in food allergy patients an symptoms in daily life are generally rare, other parameters need to be considered [4]. Thus, studies on QoL can be helpful in this regard. In recent years, an increasing number of QoL-studies on patients with food allergies and anaphylaxis, as well as how they deal with emergency medication and food, have been published. The results provide an insight into why children, adolescents and their parents behave in the way they do and which issues need to be addressed during consultations. The results of these studies are summarized in the present article.
QoL studies are generally carried out using standardized questionnaires. Health-related QoL (HRQoL) questionnaires that measure general health parameters are primarily of relevance in medicine [4, 5]. Here, the differences between individual disease groups or with healthy subjects are recorded. However, questionnaires specifically designed to measure the QoL of food-allergy patients or their parents have existed for a number of years [6]. Although these disease-specific questionnaires do not permit comparisons with other disease groups, they do make it possible to draw conclusions on, for example, disease course following intervention. The instrument most frequently used is the food allergy quality of life questionnaire (FAQLQ) developed for the international EuroPrevall project; the questionnaire is validated in several languages and is available in various forms tailored to adult patients, teenagers, parents and children aged 8 years and over [7, 8, 9, 10, 11]. It records parameters such as emotional burden, fear of foods as well as social and dietary restrictions.
Some studies also make use of standardised interviews. Although quantitative conclusions are not possible with this approach, it does offer the advantage of permitting an individual evaluation of particular issues as well as the opportunity to generate new hypotheses.
General aspects of quality of life in children and adolescents
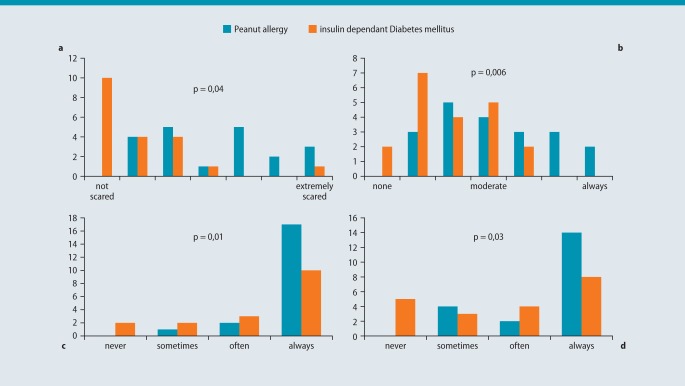
In one of the first studies on QoL of affected children in 2003, Avery et al. demonstrated that the QoL of children with peanut allergy was significantly lower than that of patients with type-1 diabetes [12, 13]. The most significant impairment was the persistent fear of an adverse reaction, which was perceived as not calculable (see Fig. 1). This prevailing fear could be measured in several subsequent studies and affects not only allergic children and adolescents, but also their parents [14, 15, 16].
Fig. 1:
A comparison of patients with peanut allergy (blue) and insulin-dependent diabetes (orange) a: Fear of eating peanuts or to suffer a hypoglycaemia. b: Risk to suffer a severe reaction or to become very ill. c: I must be careful what I eat. d: I must be careful if I eat in a restaurant. (according to [12])
When asked about their general health, children and adolescents with food allergies perform worse in overall health scores than their non-allergic siblings or healthy controls [14]. Moreover, girls report a greater negative impact on their QoL than boys [17, 18]. This is attributed to gender-specific behaviour and role expectations, whereby girls integrate their disease in their social environment whilst boys downplay the situation [13].
The reduction in QoL also depends on age. A working group in Switzerland recently showed that older children experience a greater reduction in QoL than younger children [19]. This is an effect of the greater independence that may be perceived by food-allergic children as a burden. Their concerns are even greater when they are away from their parents [14]. In some cases, children and their parents perceive the use of public transport, going to parties or travelling on holiday as life-threatening [12].
QoL is reduced even further in cases where children suffer allergies to more than one food [16, 17, 20]. Concomitant allergic diseases such as asthma and atopic dermatitis also contribute to further reducing QoL. Gastrointestinal symptoms due to allergy are a greater burden in all age groups through to adulthood than, for example, respiratory symptoms [17, 22]. Some children even develop anxiety or eating disorders following a severe allergic reaction [23].
The presence of a food allergy also affects school performance; on average, allergic children have a greater number of school absences and are less likely to be in full-time employment later on than their healthy peers [20, 22].
A very recent US study investigated bullying behaviour towards food-allergic children at school and during leisure time [24]. The study clearly showed that allergic children are affected significantly more often than the control population. It is assumed that they are seen as easy prey and have their allergy used against them in that, for example, they are threatened with various foodstuffs. The children reported, among others things, having food allergens thrown at them or being forced to come into contact with allergens. Many children did not report this sort of teasing at home for fear of causing their parents more concern. On the other hand, QoL improved when children discussed these issues with their parents.
General aspects of quality of life in parents and carers
The QoL in parents of food-allergic children is in many respects lower — yet in others higher — compared with the average population [14]. Significant contributing factors here include social support and family cohesion, which many families report to be above averagely good [16, 17, 20]. However, family tension can arise when caring for a child’s safety and the preservation of their QoL falls mainly to one partner, usually the mother [21]. In such cases, the mother’s quality of life is generally poorer than the father’s [14]. The in part restrictive diets that need to be adhered to by the patient are often complied with by the whole family, which has a negative impact on all family members [23].
The fear of a child experiencing an allergic reaction is of crucial significance. If one compares families with food-allergic children and families with children with rheumatic disease, the restrictions in daily activities are perceived as greater in the former [25]. Virtually all outdoor activities, such as school events, school trips, overnight stays with friends and parties, are affected [20]. Many children are either excluded from these events or need to be accompanied by their parents until they reach young adulthood. Although parents perceive the resulting overprotectiveness as unbeneficial for their child, they see no alternative [26, 27]. The fear experienced and the restrictions to everyday activities are greater in families with younger children than those with older children.
Parents sometimes display an exaggerated level of caution, which other people may find irritating. Almost 30 % of parents interviewed reported visiting their child’s school at least once a month to discuss aspects of their child’s allergy with teachers and carers [16].
The extent to which a family’s QoL is impaired varies over time, with impairment beginning at the time of diagnosis [21]. Treating physicians should be aware that the consultation at which the diagnosis is communicated is of crucial importance. Receiving a clear diagnosis with clear recommendations on avoidance can ease the situation for the parents. However, fear first starts to develop from the moment the parents learn of the risk of anaphylaxis, i. e. as soon as they grasp the possible consequences associated with the disease [25, 28]. A large number of parents questioned in a survey before and after the first consultation in an allergy outpatients department expressed fear of the diagnosis. This suggests that a calm conversational technique and a realistic assessment of the risks of the disease can be crucial to the family’s QoL for a long period of time.
In addition to an accurate diagnosis including challenge testing (see below), it is important for the patient to be given clearly formulated recommendations to hand in the case of an adverse reaction. An interesting approach was recently investigated in Ireland [29]: a group of patients were given access to a 24-h telephone hotline for 6 months, where they should call for advice in the event of an adverse reaction. Alone the reassurance this option offered (only two of 24 patients used the hotline on three occasions over the 6 months) significantly improved the measured QoL, and continued to do so for 6 months after the study time. Indeed, many patients are unsure as to how and when they should use an autoinjector [30, 31], and even when this step has been taken, they are unclear about how to proceed (e. g. necessity for inpatient monitoring). Since setting up a hotline is unrealistic in everyday life, readily available recommendations like the ones formulated in the anaphylaxis identity card can provide assistance in the decision-making process.
With time, most parents learn to cope with the situation and become more relaxed as a routine is established [21]. With this, daily restrictions are perceived as less significant. In addition, long anaphylaxis-free periods serve to reduce fears [26]. On the other hand, new situations that fall outside of the familiar routine, such as parties or school outings, tend to raise fears to a new level. Starting school and the transition to adolescence are seen as particularly stressful. Parents find it difficult to imagine handing over responsibility for their children. As such, parents with children who have experienced long periods free from adverse allergic reactions are concerned that their children have been lulled into a false sense of security [21].
Actual anaphylactic reactions do not affect parents’ QoL [20]. Indeed, expectations in terms of the possible consequences of allergen contact have a greater impact than the adverse reactions themselves. This is another factor that can be affected through consultation.
A major cause of parental frustration is the fact that they feel misunderstood by other people and by the public in general. They experience their children being excluded from events or activities, such as sleeping away from home. Parents also often find themselves confronted with family members or carers who question the relevance of their child’s food allergy [26]
Particular aspects in adolescence
The effect of a food allergy on daily life is seen by many adolescents and young adults as less relevant than concerns about school performance, general physical fitness or indeed having friends [32]. Their environment perceives the negative impact of the allergy to be greater than they do themselves [33].
Many adolescents with food allergies are burdened by the fact that they feel misunderstood by their extra-familial environment, which they feel is unreliable. As a result, friends who are informed about avoidance and therapy are frequently perceived as providing particularly positive and valuable support [34].
Affected adolescents see being “different” as a burden. They do not wish to discuss their food allergy or their emergency medication with their friends. On the other hand, they report that they would feel a sense of relief if their social environment was aware of and appropriately informed about their allergy [32, 34].
Many adolescents cannot remember their last anaphylactic reaction, which in turn reduces the impact their allergy has on their daily lives; however, this serves to increase parents’ concern about the excessive carelessness of youth [35].
Adolescents develop particular strategies to deal with avoiding allergens and keeping emergency medication available. They decide what risks to take when consuming unfamiliar foods depending on parameters such as whether they are eating in a familiar environment, whether their parents are present, the distance to the next emergency department or the availability of an adrenaline autoinjector (AAI) [34, 36, 37]. Where no information on food ingredients is available, adolescents often report using a strategy whereby they try small amounts and, in the absence of an adverse reaction, continue eating until symptoms appear. This approach has been proven to lead to more frequent adverse reactions. In a British study, a third of adolescents reported that they had not checked the list of ingredients prior to their last adverse reaction. Only a quater consistently refrained from consuming products containing trace elements of the relevant allergen [34].
Assuming responsibility for oneself is an important step in adolescence; however, this tends to be delayed in food allergic adolescents as they leave it to their parents to ask about allergens in restaurants or to carry an AAI [34, 36].
The impact of food allergy on adult patients
Only scant studies on adult patients have been published. The impact of food allergy on the quality of life in adult patients varies widely. It was found in a small collective of patients recruited to a population-based study on food allergies that there are indeed patients who have experienced sometimes severe adverse allergic reactions, yet who have never sought relevant medical assistance [38]. These patients had a distinctly better QoL than patients who actively sought medical help. The implication here is that the perceived reduction in QoL prompts earlier consultation with a physician. In general, perceived HRQoL is worse among women than among men [39]. A recent study of Swedish adults with immunoglobulin E (IgE)-mediated allergies to basic foodstuffs (milk, eggs or wheat) showed no gender differences in terms of HRQoL, as measured using the FAQLQ-AF [40]. This study showed the reduction in QoL to be greatest in the area of avoidance and dietary restrictions. QoL was also worse in patients who had been prescribed an autoinjector and who had concomitant asthma, which was considered an indicator of allergy severity. Prior anaphylactic episodes, on the other hand, had no significant impact.
In another study, QoL in adults with peanut allergy was compared with other disease groups. In contrast to children, the former group was observed to have better QoL than rheumatological patients [25].
Cross-reactive food allergies also have an impact on QoL. A working group led by Professor Treudler at the University of Leipzig studied patients with birch pollen-associated food allergy: they found a clear reduction in QoL, which was more pronounced in women than in men, and which worsened with the number of foodstuffs not tolerated, age and the severity of previous symptoms. The chief problem here was patients’ general concern about their own health, which was markedly pronounced in this group, as well as their fear of experiencing a sudden adverse reaction [41, 42].
What influences the use of an autoinjector?
A British study showed that prescribing an autoinjector increases QoL in mothers whose children suffer from nut or peanut allergy. Interestingly, this improvement was independent of whether or not children carried the AAI [43]. An Australian study found wholly contrasting results, whereby QoL dropped following the prescription of an AAI. However, there was no clear definition here as to when precisely the prescription was made following diagnosis and whether the diagnosis itself was more likely the cause of the worsened QoL rather than the fear of having to carry an AAI [44]. Canadian allergologists were recently able to show in a large collective (1,209 parents of peanut-allergic children) that 56 % of parents fear using an AAI. The risk of fear was greater in the case of dissatisfaction with AAI training and among patients who had never experienced a severe adverse reaction, but lower in the case of long-standing disease and higher age of the mother [45].
In general, the rate of adolescents and young adults prescribed an AAI who actually carry the device with them is low at between 15 % and 60 %. A number of studies in British and US adolescents [32, 34, 36, 46] found that an AAI was more likely to be carried when travelling, followed by visiting a restaurant, when at school or when staying over at friends. An AAI was only rarely carried for sports activities (19 % and 43 %). However, factors that are not necessarily of primary concern to the treating physician also influence whether or not an AAI is carried, such as wearing tight-fitting clothes or going dancing, both of which strongly reduce the likelihood. In this context, the size and unwieldiness of the AAI are reasons not to carry the device, and more so in boys than in girls [34, 46].
Adolescents tend to weigh up the risks when deciding whether or not to carry an AAI in certain situations [36]. The higher they consider the risk of an adverse reaction to be, the more likely they are to carry an AAI. Conversely, they report more cautious behaviour when they have no AAI with them [34].
A variety of factors influence AAI-carrying behaviour. For example, many older children and adolescents can no longer remember having had an anaphylactic reaction. The rate of adolescents who carry an AAI with them drops as the period of time since the last adverse reaction increases. On the other hand, children and adolescents who are more aware of possible symptoms are more likely to carry an AAI. Thus, food challenge tests can help patients to experience adverse reactions under controlled conditions.
Furthermore, social acceptance — particularly that of an adolescent’s peer group — plays an important role. In cases where adolescents or children have already experienced teasing due to their allergy, they attempt to hide their disease and conceal their AAI, if they carry it at all [34].
A Scottish study in adolescents and their parents who were not cared for in a specialized centre showed in summary that the reasons for not using an AAI in the case of anaphylactic reaction were multifaceted. Of relevance is not only the ability to use the AAI on a technical level, but also to recognize an anaphylactic reaction. Furthermore, the patient or their parents must be aware of precisely the right point in time to use the AAI and they should also be prepared for the emotional challenge of dealing with an acute, potentially life-threatening adverse reaction.
A summary of factors that promote the use of an AAI include in particular: appropriate empowerment (see Tab. 1), training by qualified personnel on how to use the device and previous successful use.
Table 1.
Proposals to improve the management of food allergies and emergency situations in adolescents (according to [37])
| Necessary information | _Explain the basis of the diagnosis and the prognosis of a food allergy _Explain in particular the specific symptoms that should prompt the use of adrenaline _Go through the with the patient the symptoms he or she has experienced during anaphylaxis _Stress the importance of allergen avoidance _Explain which foods are safe and what is to be understood by declaration |
| Readiness in emergency situations | _Find out whether the patient carries an AAI and, if not, formulate suggestions on carrying the device in a concealed manner or depositing it safely _Make an AAI trainer available _Stress that, in the case of severe symptoms, the use of the AAI takes priority over the use of an antihistamine or visiting an outpatient department _Arrange regular follow-up appointments |
| Empowerment-based self-management | _Consider together with the adolescent whether it might be useful to involve friends in his or her allergy management _Inquire whether bullying due to the allergy is taking place _Offer consultations without the parents in order to discuss the patient’s interaction with his or her parents |
| Mode of interaction | _Maintain an open and impartial conversational style _Openly discuss the adolescent’s decision-making process when dealing with reactions or allergen avoidance |
AAI, adrenaline autoinjector
Food ingredient declaration and quality of life
Uncertainty when reading the declaration of ingredients and trace elements on packaged food products is bothersome for both patient and parent. A US study found that only around 50 % of parents were able to correctly identify peanut as an ingredient on a product. The rate was 10 % for cow’s milk. However, the rate rose to 90 % when parents had attended a self-help group [47]. Parents reported always reading lists of ingredients several times, since in their experience the relevant food was identified only on reading the list of ingredients for the third time, thereby significantly compounding their insecurity [23]. Thus when shopping, only those products that have already been consumed in the past tend to be chosen. When shopping in a hurry, images on food packaging often serve as guidance; however, these can be misleading [48]. Products are categorized and subjected to closer scrutiny depending on risk assessment (e. g. nut-allergy sufferers: muesli, chocolate, bakery products = high risk; fruit or milk products = low risk) [49]. Moreover, large companies and local products are more trusted. Unfamiliar products are also subjected to sensory scrutiny.
Adolescents often ignore trace allergen labelling completely, seeing it as a reflection of a company’s exaggerated need for security. In addition, many assume that they tolerate a product if they have already consumed it without consequence in the past [34, 49].
Patients who were allowed to ignore trace allergen labelling on the basis of their medical history or challenge test results, i. e. they repeatedly reacted only to large amounts of allergens, experienced a significant improvement in QoL [43].
Food challenges and quality of life
It is important for both the patient and their parents to be given clear and unambiguous food allergy information. Conflicting and contradictory information from physicians leads to frustration. The aim of comprehensive diagnosis is to unequivocally identify hazardous allergens, while providing the widest possible range of safe foods. Where appropriate, diagnosis includes food challenges to conclusively confirm an allergy.
Furthermore, food challenges also affect the QoL of parents as well as patients. Several studies have repeatedly shown the predominantly long-term positive effect food challenges have on QoL [50, 51, 52, 53, 54]. Interestingly, this positive effect does not depend on the outcome of food challenges. Even an allergic reaction that follows a “controlled” course in the context of challenge tests can effectively demonstrate to parents and children that appropriate and successful treatment is possible. Children and adolescents find it instructive to experience first-hand the course of an adverse reaction and, where necessary, the use of an AAI and its rapid onset of effect. As a result, fear levels in parents and children can drop significantly following challenge testing [53], with a resultant rise in QoL [28]. A similar improvement is also seen in adult patients, following both a negative and a positive challenge [50], albeit somewhat weaker in the latter case. No changes were seen in the case of equivocal results, demonstrating that clarity about the diagnosis is of primary importance in this patient group. Our own working group was recently able to show that the QoL in parents of children with milk and egg allergies was improved after establishing that their children tolerated baked products [54]. This was the case in spite of persisting egg and milk allergies, thereby demonstrating that an expansion of possible foods also contributes to improved QoL.
A number of authors point out that the goal is not to remove all fear from patients [13, 26]. A “healthy” degree of fear helps maintain vigilance in terms of allergen avoidance. Too much fear can paralyze the patient in an emergency situation, whilst too little fear prevents due caution, such as carrying medication.
Many of the issues relevant to anaphylaxis, such as recognizing an allergic reaction, how to behave in an emergency, advice on allergen avoidance and food labelling as well as dealing with the social environment, are discussed in detail in the anaphylaxis training programme (Arbeitsgemeinschaft Anaphylaxie Training und Education, AGATE) recently introduced in Germany. For this reason, every attempt should be made to offer the training program in a comprehensive manner and all patients prescribed an autoinjector should be automatically included in the training program.
Summary
Numerous factors influence the QoL of affected patients and their families. The physician’s duty is to provide qualified advice. The central points of this advice include a thorough diagnosis, a realistic assessment of the risk of an inadvertent adverse reaction and clear recommendations on allergen avoidance and dealing with emergency situations. Together, these points serve not only to ensure the patient’s safety but also to maintain their QoL.
Concrete recommendations
It is becoming ever clearer in all areas of medicine that providing appropriate support and information to the patient forms the basis of a good therapeutic outcome. A number of recommendations can be derived from the available data on treating food-allergy patients at risk of anaphylaxis.
The majority of restrictions in the QoL of affected families result from exaggerating the risks; for this reason, patients and their parents should be given realistic perspectives in terms of the risks of the disease at the time of diagnosis, without, however, trivializing the dangers.
As part of the diagnostic procedure, patients should receive clear advice on targeted allergen avoidance.
Good information on declaration guidelines, e. g. in the context of nutrition counselling, is essential.
The patient must be aware of how to recognize an anaphylactic reaction and which measures are necessary. These issues are discussed in detail in the AGATE training programme.
Instructions on emergency medication must be clear, easy to understand and should stress the importance of the prompt use of an autoinjector in the event of severe symptoms. An anaphylaxis identity card, for example, is helpful in this regard.
The fear of using the adrenaline autoinjector is seen as a considerable obstacle for many patients. This fear needs to be addressed during consultations.
Discussing pressures caused by the social environment and providing assistance where possible is advisable.
The aim of consultations must be to create “respect” for a food allergy.
Acknowledgement
My thanks go to Prof. Dr. Uwe Gieler for his critical review of the manuscript.
Abbreviations
- AAI
Adrenaline autoinjector
- AGATE
Arbeitsgemeinschaft Anaphylaxie Training und Edukation e.V.
- FAQLQ
Food allergy quality of life questionnaire
- FAQLQ-AF
Food allergy quality of life questionnaire adult form
- HRQoL
Health-related quality of life
- IgE
Immunglobulin E
- QoL
Quality of life
Footnotes
Conflict of interest
The corresponding author states that there are no conflicts of interest
Cite this as
Lange L. Quality of life in the setting of anaphylaxis and food allergy. Allergo J Int 2014; 23:252–60 DOI: 10.1007/s40629-014-0029-x
Literatur
- 1.Umasunthar T, Leonardi-Bee J, Hodes M, Turner PJ, Gore C, Habibi P, et al. Incidence of fatal food anaphylaxis in people with food allergy: a systematic review and meta-analysis. Clin Exp Allergy. 2013;43:1333–41. doi: 10.1111/cea.12211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beyer K, Eckermann O, Hompes S, Grabenhenrich L, Worm M. Anaphylaxis in an emergency setting - elicitors, therapy and incidence of severe allergic reactions. Allergy. 2012;67:1451–6. doi: 10.1111/all.12012. [DOI] [PubMed] [Google Scholar]
- 3.Grabenhenrich L, Hompes S, Gough H, Ruëff F, Scherer K, Pföhler C, et al. Implementation of anaphylaxis management guidelines: a register-based study. PLoS One. 2012;7:e35778. doi: 10.1371/journal.pone.0035778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flokstra-de Blok BM, Dubois AE. Quality of life measures for food allergy. Clin Exp Allergy. 2012;42:1014–20. doi: 10.1111/j.1365-2222.2011.03927.x. [DOI] [PubMed] [Google Scholar]
- 5.Flokstra-de Blok BM, Dubois AE. Quality of life in food allergy: valid scales for children and adults. Curr Opin Allergy Clin Immunol. 2009;9:214–21. doi: 10.1097/ACI.0b013e32832aa59f. [DOI] [PubMed] [Google Scholar]
- 6.Flokstra-de Blok BMJ, Dubois AEJ, Vlieg-Boerstra BJ, Oude Elberink JNG, Raat H, DunnGalvin A, et al. Health related quality of life of food allergic patients: comparison with the general population and other diseases. Allergy. 2010;65:238–44. doi: 10.1111/j.1398-9995.2009.02121.x. [DOI] [PubMed] [Google Scholar]
- 7.Flokstra-de Blok BM, DunnGalvin A, Vlieg-Boerstra BJ, Oude Elberink JN, Duiverman EJ, Hourihane JO, et al. Development and validation of a self-administered Food Allergy Quality of Life Questionnaire for children. Clin Exp Allergy. 2009;39:127–37. doi: 10.1111/j.1365-2222.2008.03120.x. [DOI] [PubMed] [Google Scholar]
- 8.Flokstra-de Blok BM, DunnGalvin A, Vlieg-Boerstra BJ, Oude Elberink JN, Duiverman EJ, Hourihane JO, et al. Development and validation of the self-administered Food Allergy Qualityof Life Questionnaire for adolescents. J Allergy Clin Immunol. 2008;122:139–44. doi: 10.1016/j.jaci.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Flokstra-de Blok BM, van der Meulen GN, DunnGalvin A, Vlieg-Boerstra BJ, Oude Elberink JN, Duiverman EJ, et al. Development and validation of the Food Allergy Quality of Life Questionnaire - adult form. Allergy. 2009;64:1209–17. doi: 10.1111/j.1398-9995.2009.01968.x. [DOI] [PubMed] [Google Scholar]
- 10.DunnGalvin A, Flokstra de Blok BM, Burks AW, Dubois AE, Hourihane JO. Food allergy QoL questionnaire for children aged 0-12 years: content, construct, and cross-cultural validity. Clin Exp Allergy. 2008;38:977–86. doi: 10.1111/j.1365-2222.2008.02978.x. [DOI] [PubMed] [Google Scholar]
- 11.van der Velde JL, Flokstra-de Blok BM, Vlieg-Boerstra BJ, Oude Elberink JN, Schouten JP, Dunngalvin A, et al. Testretest reliability of the Food Allergy Quality of Life Questionnaires (FAQLQ) for children, adolescents and adults. Qual Life Res. 2009;18:245–51. doi: 10.1007/s11136-008-9434-2. [DOI] [PubMed] [Google Scholar]
- 12.Avery NJ, King RM, Knight S, Hourihane JO. Assessment of quality of life in children with peanut allergy. Pediatr Allergy Immunol. 2003;14:378–82. doi: 10.1034/j.1399-3038.2003.00072.x. [DOI] [PubMed] [Google Scholar]
- 13.Cummings AJ, Knibb RC, King RM, Lucas JS. The psychosocial impact of food allergy and food hypersensitivity in children, adolescents and their families: a review. Allergy. 2010;65:933–45. doi: 10.1111/j.1398-9995.2010.02342.x. [DOI] [PubMed] [Google Scholar]
- 14.King RM, Knibb RC, Hourihane JO. Impact of peanut allergy on quality of life, stress and anxiety in the family. Allergy. 2009;64:461–8. doi: 10.1111/j.1398-9995.2008.01843.x. [DOI] [PubMed] [Google Scholar]
- 15.Lyons AC, Forde EM. Food allergy in young adults: perceptions and psychological effects. J Health Psychol. 2004;9:497–504. doi: 10.1177/1359105304044032. [DOI] [PubMed] [Google Scholar]
- 16.Sicherer SH, Noone SA, Munoz-Furlong A. The impact of childhood food allergy on quality of life. Ann Allergy Asthma Immunol. 2001;87:461–4. doi: 10.1016/S1081-1206(10)62258-2. [DOI] [PubMed] [Google Scholar]
- 17.Marklund B, Ahlstedt S, Nordstrom G. Health-related quality of life in food hypersensitive schoolchildren and their families: parents’ perceptions. Health Qual Life Outcomes. 2006;4:48. doi: 10.1186/1477-7525-4-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marklund B, Ahlstedt S, Nordstrom G. Health-related quality of life among adolescents with allergy-like conditions - with emphasis on food hypersensitivity. Health Qual Life Outcomes. 2004;2:65. doi: 10.1186/1477-7525-2-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wassenberg J, Cochard MM, Dunngalvin A, Ballabeni P, Flokstra-de Blok BM, Newman CJ, et al. Parent perceived quality of life is age-dependent in children with food allergy. Pediatr Allergy Immunol. 2012;23:412–9. doi: 10.1111/j.1399-3038.2012.01310.x. [DOI] [PubMed] [Google Scholar]
- 20.Bollinger ME, Dahlquist LM, Mudd K, Sonntag C, Dillinger L, McKenna K. The impact of food allergy on the daily activities of children and their families. Ann Allergy Asthma Immunol. 2006;96:415–21. doi: 10.1016/S1081-1206(10)60908-8. [DOI] [PubMed] [Google Scholar]
- 21.Gillespie CA, Woodgate RL, Chalmers KI, Watson WT. „Living with risk’’: mothering a child with food-induced anaphylaxis. J Pediatr Nurs. 2007;22:30–42. doi: 10.1016/j.pedn.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 22.Calsbeek H, Rijken M, Dekker J, van Berge Henegouwen GP. Disease characteristics as determinants of the labour market position of adolescents and young adults with chronic digestive disorders. Eur J Gastroenterol Hepatol. 2006;18:203–9. doi: 10.1097/00042737-200602000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Munoz-Furlong A. Daily coping strategies for patients and their families. Pediatrics. 2003;111:1654–61. [PubMed] [Google Scholar]
- 24.Shemesh E, Annunziato RA, Ambrose MA, Ravid NL, Mullarkey C, Rubes M, Chuang K, Sicherer M, Sicherer SH. Child and parental reports of bullying in a consecutive sample of children with food allergy. Pediatrics. 2013;131:e10–7. doi: 10.1542/peds.2012-1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Primeau MN, Kagan R, Joseph L, Lim H, Dufresne C, Duffy C, et al. The psychological burden of peanut allergy as perceived by adults with peanut allergy and the parents of peanut-allergic children. Clin Exp Allergy. 2000;30:1135–43. doi: 10.1046/j.1365-2222.2000.00889.x. [DOI] [PubMed] [Google Scholar]
- 26.Mandell D, Curtis R, Gold M, Hardie S. Anaphylaxis: how do you live with it? Health Soc Work. 2005;30:325–35. doi: 10.1093/hsw/30.4.325. [DOI] [PubMed] [Google Scholar]
- 27.Herbert LJ, Dahlquist LM. Perceived history of anaphylaxis and parental overprotection, autonomy, anxiety, and depression in food allergic young adults. J Clin Psychol Med Settings. 2008;15:261–9. doi: 10.1007/s10880-008-9130-y. [DOI] [PubMed] [Google Scholar]
- 28.Knibb RC, Semper HM. Anxiety and depression in parents with food allergic children before and after food allergy diagnosis. Psychol Health. 2008;23:161. [Google Scholar]
- 29.Kelleher MM, Dunngalvin A, Sheikh A, Cullinane C, Fitzsimons J, Hourihane JO. Twenty four-hour helpline access to expert management advice for food-allergy-triggered anaphylaxis in infants, children and young people: a pragmatic, randomized controlled trial. Allergy. 2013;68:1598–604. doi: 10.1111/all.12310. [DOI] [PubMed] [Google Scholar]
- 30.Simons FER, Clark S, Camargo CA., Jr Anaphylaxis in the community: learning from the survivors. J Allergy Clin Immunol. 2009;124:301–6. doi: 10.1016/j.jaci.2009.03.050. [DOI] [PubMed] [Google Scholar]
- 31.Arkwright PD, Farragher AJ. Factors determining the ability of parents to effectively administer intramuscular adrenaline to food allergic children. Pediatr Allergy Immunol. 2006;17:227–9. doi: 10.1111/j.1399-3038.2006.00392.x. [DOI] [PubMed] [Google Scholar]
- 32.Sampson MA, Munoz-Furlong A, Sicherer SH. Risk-taking and coping strategies of adolescents and young adults with food allergy. J Allergy Clin Immunol. 2006;117:1440–5. doi: 10.1016/j.jaci.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 33.Lyons AC, Forde EM. Food allergy in young adults: perceptions and psychological effects. J Health Psychol. 2004;9:497–504. doi: 10.1177/1359105304044032. [DOI] [PubMed] [Google Scholar]
- 34.Monks H, Gowland MH, MacKenzie H, Erlewyn-Lajeunesse M, King R, Lucas JS, Roberts G. How do teenagers manage their food allergies? Clin Exp Allergy. 2010;40:1533–40. doi: 10.1111/j.1365-2222.2010.03586.x. [DOI] [PubMed] [Google Scholar]
- 35.Akeson N, Worth A, Sheikh A. The psychosocial impact of anaphylaxis on young people and their parents. Clin Exp Allergy. 2007;37:1213–20. doi: 10.1111/j.1365-2222.2007.02758.x. [DOI] [PubMed] [Google Scholar]
- 36.Macadam C, Barnett J, Roberts G, Stiefel G, King R, Erlewyn-Lajeunesse M, et al. What factors affect the carriage of epinephrine auto-injektors by teenagers. Clin Trans Allergy. 2012;2:3. doi: 10.1186/2045-7022-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marrs T, Lack G. Why do few food-allergic adolescents treat anaphylaxis with adrenaline? — Reviewing a pressing issue. Pediatr Allergy Immunol. 2013;24(3):222–9. doi: 10.1111/pai.12013. [DOI] [PubMed] [Google Scholar]
- 38.Le TM, Flokstra-de Blok BM, van Hoffen E, Lebens AF, Goossens NJ, Dubois AE, et al. Quality of life is more impaired in patients seeking medical care for food allergy. Int Arch Allergy Immunol. 2013;162:335–9. doi: 10.1159/000354925. [DOI] [PubMed] [Google Scholar]
- 39.Ellert U, Kurth BM. [Health-related quality of life in adults in Germany: results of the German Health Interview and Examination Survey for Adults (DEGS1)] Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2013;56:643–9. doi: 10.1007/s00103-013-1700-y. [DOI] [PubMed] [Google Scholar]
- 40.Jansson SA, Heibert-Arnlind M, Middelveld RJ, Bengtsson UJ, Sundqvist AC, Kallström-Bengtsson I. Health-related quality of life, assessed with a disease-specific questionnaire, in Swedish adults suffering from well-diagnosed food allergy to staple foods. Clin Transl Allergy. 2013;3:21. doi: 10.1186/2045-7022-3-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kramer S, Franke A, Simon JC, Treudler R. Health related Quality of Life bei 73 Birkenpollenallergikern mit pollenassoziierter Nahrungsmittelallergie. Allergo J. 2010;19:17. [Google Scholar]
- 42.Kramer S, Simon JC, Treudler R. Allergy. 2009. Birch associated soy allergy is frequent and causes impairment of quality of life; p. 64:47. [Google Scholar]
- 43.Cummings AJ, Knibb RC, Erlewyn-Lajeunesse M, King RM, Roberts G, Lucas JS. Management of nut allergy influences quality of life and anxiety in children and their mothers. Pediatr Allergy Immunol. 2010;21:586–94. doi: 10.1111/j.1399-3038.2009.00975.x. [DOI] [PubMed] [Google Scholar]
- 44.Pinczower GD, Bertalli NA, Bussmann N, Hamidon M, Allen KJ, Dunngalvin A, et al. The effect of provision of an adrenaline autoinjector on quality of life in children with food allergy. J Allergy Clin Immunol. 2013;131:238–40. doi: 10.1016/j.jaci.2012.09.038. [DOI] [PubMed] [Google Scholar]
- 45.Chad L, Ben-Shoshan M, Asai Y, Cherkaoui S, Alizadehfar R, St-Pierre Y, et al. A majority of parents of children with peanut allergy fear using the epinephrine auto-injector. Allergy. 2013;68:1605–9. doi: 10.1111/all.12262. [DOI] [PubMed] [Google Scholar]
- 46.Gallagher M, Worth A, Cunningham-Burley S, Sheikh A. Epinephrine autoinjector use in adolescents at risk of anaphylaxis: a qualitative study in Scotland, UK. Clin Exp Allergy. 2011;41:869–77. doi: 10.1111/j.1365-2222.2011.03743.x. [DOI] [PubMed] [Google Scholar]
- 47.Joshi P, Mofidi S, Sicherer SH. Interpretation of commercial food ingredient labels by parents of food-allergic children. J Allergy Clin Immunol. 2002;109:1019–21. doi: 10.1067/mai.2002.123305. [DOI] [PubMed] [Google Scholar]
- 48.Barnett J, Leftwich J, Muncer K, Grimshaw K, Shepherd R, Raats MM, et al. How do peanut and nut-allergic consumers use information on the packaging to avoid allergens? Allergy. 2011;66:969–78. doi: 10.1111/j.1398-9995.2011.02563.x. [DOI] [PubMed] [Google Scholar]
- 49.Barnett J, Vasileiou K, Gowland MH, Raats MM, Lucas JS. Beyond labelling: What strategies do nut allergic individuals employ to make food choices? A qualitative study. PLoS One. 2013;8:e55293. doi: 10.1371/journal.pone.0055293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.van der Velde JL, Flokstra-de Blok BM, de Groot H, Oude-Elberink JN, Kerkhof M, Duiverman EJ, et al. Food allergyrelated quality of life after double-blind, placebo-controlled food challenges in adults, adolescents, and children. J Allergy Clin Immunol. 2012;130:1136–43. doi: 10.1016/j.jaci.2012.05.037. [DOI] [PubMed] [Google Scholar]
- 51.Knibb RC, Ibrahim NF, Stiefel G, Petley R, Cummings AJ, King RM, et al. The psychological impact of diagnostic food challenges to confirm the resolution of peanut or tree nut allergy. Clin Exp Allergy. 2012;42:451–9. doi: 10.1111/j.1365-2222.2011.03905.x. [DOI] [PubMed] [Google Scholar]
- 52.DunnGalvin A, Cullinane C, Daly DA, Flokstra-de Blok BM, Dubois AE, Hourihane JO. Longitudinal validity and responsiveness of the Food Allergy Quality of Life Questionnaire - Parent Form in children 0-12 years following positive and negative food challenges. Clin Exp Allergy. 2010;40:476–85. doi: 10.1111/j.1365-2222.2010.03454.x. [DOI] [PubMed] [Google Scholar]
- 53.Zijlstra WT, Flinterman AE, Soeters L, Knulst AC, Sinnema G, L’Hoir MP, Pasmans SG. Parental anxiety before and after food challenges in children with suspected peanut and hazelnut allergy. Pediatr Allergy Immunol. 2010;21:439–45. doi: 10.1111/j.1399-3038.2009.00929.x. [DOI] [PubMed] [Google Scholar]
- 54.Finger A, Pfannenstiel C, Schönfelder A, Frank F, Buderus S, Lange L. Improvement of quality of life in children with milk and egg allergy after proof of tolerance to baked products. Allergy. 2012;67:87. [Google Scholar]