Abstract
Background
Traumatic brain injury (TBI) is one of the leading causes of neurological disability. In this retrospective study, serum total cholinesterase (ChE) activities were analyzed in 188 patients for diagnostic as well as predictive values for mortality.
Methods and Findings
Within 72 hours after injury, serum ChE activities including both acetylcholinesterase and butyrylcholinesterase were measured. Disease severity was evaluated with Acute Physiology and Chronic Health Evaluation (APACHE) II score, Glasgow Coma Score, length of coma, post-traumatic amnesia and injury feature. Neurocognitive and functional scores were assessed using clinical records. Of 188 patients, 146 (77.7%) survived and 42 (22.3%) died within 90 days. Lower ChE activities were noted in the non-survivors vs. survivors (5.94±2.19 vs. 7.04±2.16 kU/L, p=0.023), in septic vs. non-infected patients (5.93±1.89 vs. 7.31±2.45 kU/L, p=0.0005) and in patients with extremely severe injury vs. mild injury (6.3±1.98 vs. 7.57±2.48 kU/L, p=0.049). The trajectories of serum ChE levels were also different between non-survivors and survivors, septic and non-infected patients, mild and severely injured patients, respectively. Admission ChE activities were closely correlated with blood cell counts, neurocognitive and functional scores both on admission and at discharge. Receiver operating characteristic analysis showed that the area under the curve for ChE was inferior to that for either APACHE II or white blood cell (WBC) count. However, at the optimal cutoff value of 5 kU/L, the sensitivity of ChE for correct prediction of 90-day mortality was 65.5% and the specificity was 86.4%. Kaplan-Meier analysis showed that lower ChE activity (<5 kU/L) was more closely correlated with poor survival than higher ChE activity (>5 kU/L) (p=0.04). After adjusting for other variables, ChE was identified as a borderline independent predictor for mortality as analyzed by Binary logistic regression (P=0.078).
Conclusions
Lowered ChE activity measured on admission appears to be associated with disease severity and outcome for TBI patients.
Introduction
Traumatic brain injury (TBI) affects up to 10 million people globally [1], yet our ability to diagnose and treat TBI is deficient. Therefore, the identification of diagnostic and prognostic biomarkers that directly reflect injury to central nervous system (CNS) is imperative [2,3]. Stress, as in TBI, can be defined as a psychological, environmental, or physiologic threat on homeostasis [4], which largely involves the sympathetic and parasympathetic nervous systems. Catecholamine released from sympathetic nerve fibers launches a fight-or-flight reaction while eliciting both inflammatory and immunosuppressive responses [5]. The acetylcholine (ACh), a parasympathetic neurotransmitter, is another key contributor to stress to enhance neuronal excitability [6]. Aside from the vagus nerve, ACh could also be produced by peripheral leukocytes [7,8]. Then it can potently modulate classical immune response by activating α7 nicotinic acetylcholine receptor (α7 nAChR) on the leukocytes [9,10] in terms of “cholinergic anti-inflammatory response” [11].
Increasing evidence suggested that cholinergic status might be used to judge the disease severity and predict the potential risk of mortality [12]. Imbalanced sympathetic/parasympathetic activity was found to be associated with poor cardiovascular prognosis [13], worse stroke outcome [14], organ death in hypertension [15], and the sudden death as well as all-cause mortality [16]. Considering that ACh is extremely labile and difficult to use for clinical measurements [17], the employment of its hydrolyzing enzymes as an indirect measurement for parasympathetic dysfunction might be more suitable for clinical use. Cholinesterases (ChE), acetylcholinesterase (AChE), and the closely related enzyme butyrylcholinesterase (BChE), may contribute to the cholinergic status and parasympathetic dysfunction. AChE is the major cholinesterase in the brain in contrast to BChE, the major ACh-hydrolyzing enzyme in the circulation, both of which could mitigate the cholinergic anti-inflammatory pathway [18].
Although the morbidity and mortality of TBI are frequently attributed by the neurological consequences of the brain injury [19,20], non-neurological complications including cardiovascular, respiratory, and infection [21–23] could also affect its outcome. In fact, non-neurological consequences of brain injury show impressive similarities regardless of the type of brain insults, and appear to depend on the altered neuroimmune circuits [24], making patients more vulnerable to infection [25,26]. It has been documented that activation of the sympathetic nervous system (SNS) is crucial in CNS-induced immunodepression and inflammation, whereas depressed vagus activity may aggravate the inflammatory response [24]. Thus, cholinergic status as represented by ChE activity might be a potential biomarker for parasympathetic dysfunction in TBI.
So far, cholinergic status has been investigated mostly in brain tissue in TBI. Acutely elevated AChE activity was reported in the brain of ischemic [27] or blast injury [28], however, lowered AChE activity in the neocortex was seen in TBI patients with chronic cognitive symptoms [29]. For the practical purpose, the measurement of cholinergic status other than brain tissue is imperative. It was noted that serum ChE activity might be used in the diagnosis of stroke [14] and infection [30,31]. Although a significant decrease in serum ChE levels had been reported in human acute head injury [32], data regarding the association of ChE activity with blood cell counts, cognition, and neurofunctional outcome in TBI is extremely limited. Although it has not been verified yet, it is likely that increased vagal tone may account for the immune paralysis in TBI patients [33], in turn being prone to septic complications. Therefore, we assume that serum AChE activity would reflect the intensity of the cholinergic anti-inflammatory response toward brain damage and may be associated with TBI outcome. In the present study, we investigated the cholinergic predictor of the risk for the morbidity and mortality of TBI patients in two hospitals.
Materials and Methods
Patient inclusion and demographic data
Using a database of patients admitted to the Departments of Neurosurgery in two hospitals Affiliated to the Chinese PLA General Hospital (Beijing, China; Sanya, Hainan, China) between August 2009 and September 2013, we retrieved data on patients who were aged >15 years. Patients with leukemia, acute meningitis, hepatic disorder, cerebral vasculitis, or other recent CNS infection were excluded. The Institutional Review Board of Chinese PLA General Hospital approved the clinical study. Because the serum ChE activity was included in the panel examination monitoring the hepatic function, every patient with traumatic injury was tested for ChE activity on admission and frequently during hospital stay. Since the patients received no extra treatment or examination, the written informed consent from the patient was waived by our institutional review board. Nevertheless, the patient records were anonymized and de-identified prior to analysis.
Although most patients (100 in 188 patients) were insulted with multiple injuries, TBI was the most severe trauma and accounted for the main reason for admission. TBI severity was determined on the basis of the lowest recorded Glasgow Coma Score (GCS) (mild, 13–15; moderate, 9–12; severe, 6–8; extreme severe, 3–5), length of coma (LOC) (mild, <30 min; moderate, 20 min to 6 h; severe, >6 h; extreme severe, persistence), and/or post-traumatic amnesia (PTA) (mild, <60 min; moderate, >60 min to <24 h; severe, ≥24 h), injury feature (mild, concussion; moderate, no cerebral compression; severe, diffuse cerebral injury; extremely severe, severe primary injury, decerebrate rigidity or other organ injury, shock). When the GCS, LOC, and PTA scores for a participant did not all fall into a single category, the patient was assigned to the most severe category. All these variables had been reported to have prognostic value and were measured by the experienced neurological surgeons on admission.
Variables used to assess comparability were age, sex, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, baseline admission laboratory values, vital signs in the first 24 hours, and episode of infection from the hospital database. We used all-cause 90-day mortality as our primary endpoint, length of stay (LOS) in hospital and in intensive care unit (ICU) as the secondary outcomes.
Control patients
To these patients we matched 50 healthy controls by gender and age. Healthy controls were under routine physical examination in the same hospital. Exclusion criteria included a history of cerebral or cardiac event during the previous 12 months, known inflammatory diseases, history of acute febrile disease or infection during the previous 3 months, known malignancy, pregnancy, and invasive procedures during the previous 6 months.
Sample collection
Whole blood samples were obtained from all patients within 24 hours after hospital admission and up to 3 days after injury (mean 13.3+19.2 h after TBI onset), and were collected frequently during hospital stay. Samples were centrifuged at 2000 × g for 10 min at 4°C to pellet cellular bodies and debris. Patients were not included in the study if blood was not taken within 24 hours after admission or 72 hours after injury, or if patients were transferred from other hospitals.
Blood cell counts were performed with the Beckman Coulter 780 (Beckman Coulter, Nyon, Swiss). Total serum ChE activities including AChE and BChE were recorded for each patient. ChE activity was measured using reagent for creatine kinase test (Gcell, Jiuqiang Biotechnology, Beijing, China) with the Hitachi 7060 analyzer (Hitachi High-Technologies Corporation, Tokyo, Japan). The functional assay sensitivity (that is, the lowest concentration that can be quantified with a between-run imprecision of 0.030) met the Roche Diagnostics specification of 0.06 ng/mL. The respective within- and between-day coefficients of variation for ChE analyses were all less than 10%.
Sepsis, neurocognition and neurofunction evaluation
Systemic inflammatory response syndrome (SIRS), sepsis, and severe sepsis were evaluated according to established criteria [34]. Sepsis was defined as a systemic response to an infection including the criteria for SIRS plus microbiological evidence of a focal infection and/or a positive blood culture. Septic shock was defined as sepsis-induced hypotension, persisting despite adequate fluid resuscitation, along with the presence of hypoperfusion abnormalities or organ dysfunction [35]. Patients were considered to suffer from SIRS if they met the criteria defined in the guidelines of the American College of Chest Physicians/Society of Critical Care Medicine [36].
The database included the cognitive function was assessed by the use of GCS [37,38] and the Mini-Mental State Examination (MMSE; score range, 0 to 30, with lower scores indicating poorer performance) [39]. In addition, observers blind to biomarker level evaluated the neurofunctional scores for the first 24 hours and global outcome at discharge using medical records retrospectively. The instruments for neurofunctional evaluation include the Glasgow Outcome Score (GOS) [40], Functional Independence Measure (FIM) [39], Disability Rating Scale (DRS-F) [41], Modified Rankin Scale (MRS) [42], Referral Decision Scale (RDS) [43] and Quality of Life Index (QLI) [44]. GOS is the oldest and most widely outcome measure [40] defined as follows: 1 = death; 2 = persistent vegetative state; 3 = severe disability; 4 = moderate disability; and 5 = good recovery [40]. The FIM has two scales, one including 13 motor items and another with 5 cognitive items. The scores describe the patient’s levels of independence in self-care, continence, mobility, communication, and cognition [45,46]. DRS is designed to reflect disability and handicap via evaluation of physical impairment and cognitive ability [47]. Higher score on the DRS indicates greater functional impairment, whereas the inverse is true for the FIM [43]. The functional outcome was determined by MRS [48,49]. The 14-item RDS is a psychiatric evaluation for mental disorder [43]. QLI is a short self-administered scale evaluating five aspects of quality of life: activity, daily living, health, support and outlook, with a choice of three possible answers and with higher scores reflecting a better quality of life [50].
Statistical analysis
Continuous variables (ChE, age) were expressed as mean±SD. Continuous non-parametric variables (ICU and hospital stay, GCS, MMSE) were expressed as median (interquartile range, IQR). Categorical data were expressed as frequency and percentage. Continuous variables were compared between groups by the two-tailed Student t-test. We used the Chi-square test to compare categorical data and proportions, and Mann-Whitney U test as appropriate, to compare non-parametric data.
Spearman correlation coefficients were calculated to analyze the associations between admission ChE activity and the blood cell counts, cognitive and neurofunctional scores, as well as the hospital and ICU LOS. The Kruskal-Wallis test (non-parametric ANOVA) with post-hoc comparisons was utilized to identify differences in ChE levels, blood cell counts, APACHE II score, GCS and MMSE scores among the groups categorized by disease severity, infective status, or outcome. Dunn’s post-hoc tests were controlled for multiple comparisons. Sensitivity, specificity, and the receiver operating characteristic (ROC) curves were constructed and the areas under the curve (AUC) were also calculated.
The Binary logistic and Cox regression models (backward conditional step-wise) were used to identify the predicting factors (WBC, monocyte counts, neutrophil counts, MMSE, GCS, ChE, sepsis, hospital LOS, ICU LOS, and APACHE II) for death, adjusted for age and gender according to the established etiological basis for TBI. Then the variables that were significant different between the survivals and the non-survivals in the bivariable analysis were included in the final multivariable logistic regression analysis. All data in the present study were analyzed using SPSS version 16.0 (SPSS Inc, Chicago, USA).
Results
Enrollment
In this retrospective study, 15 initial ChE activities, 9 MMSE values, 5 lymphocyte counts, and 7 neutrophil counts were missing. Because the number of missing data was not so significant, they were ignored in the following statistic analysis. Patient demographics were shown in Table 1. Of the 188 TBI patients, 145 males and 33 females, with a mean age of 42.5 years (range 14–92), 42 (22.3%) died within 90 days after entry into the study. Patients were categorized by TBI severity as determined in the method with 23 mild brain trauma, 39 moderate brain trauma, 61 severe brain trauma, and 22 extremely severe brain trauma. At discharge, 32 patients had a GOS of 1 (death), 17 patient remained to be with a GOS of 2 (persistent vegetative state), 16 patients had a GOS of 3 (severe disability), 55 patients had a GOS of 4 (moderate disability), and 68 patients had a GOS of 5 (good recovery). No patients died within 3 days, whereas 10 (5.3%) died within 7 days, 18 (9.6%) died between 7–14 days, and 15 (8.0%) died between 14–31 days. Seventy-two (38.3%) patients developed infection, mostly in lungs (40, 55.6%), 38 (52.8%) of the infected patients died.
Table 1. Clinical characteristics of entire TBI patient cohort.
| Variables | Total | Mild | Moderate | Severe | Extreme Severe | p value | |
|---|---|---|---|---|---|---|---|
| (n = 188) | (n = 34) | (n = 53) | (n = 72) | (n = 29) | |||
| age, year (median±SEM) | 42.50±1.51 | 37.50±3.77 | 46.00±3.20 | 41.5±2.05 | 48.00±3.96 | 0.228 | |
| gender, male (n, %) | 145 (77.13) | 23 (67.65) | 39 (73.58) | 61 (84.72) | 22 (75.86) | 0.213 | |
| Diagnosis of TBI (n, %) | |||||||
| Skull fracture | 107 (56.91) | 17 (50.00) | 32 (60.38) | 33 (45.83) | 18 (62.07) | 0.293 | |
| Contusion | 114 (60.64) | 0 (0.00) | 33 (62.26) | 42 (58.33) | 20 (68.97) | 0.000 | |
| Primary injury | Subarachnoid hemorrhage | 83 (44.15) | 6 (17.65) | 20 (37.74) | 26 (36.11) | 16 (55.17) | 0.022 |
| Diffuse axonal injury | 24 (12.77) | 0 (0.00) | 0 (0.00) | 10 (13.89) | 7 (24.14) | 0.000 | |
| Second injury | Cerebral hernia | 28 (14.89) | 0 (0.00) | 0 (0.00) | 7 (9.72) | 19 (65.52) | 0.000 |
| Epidural hematoma | 39 (20.74) | 0 (0.00) | 14 (26.42) | 9 (12.50) | 7 (24.14) | 0.005 | |
| Subdural hematoma | 56 (29.79) | 2 (5.88) | 7 (13.21) | 21 (29.17) | 18 (62.07) | 0.000 | |
| Intracerebral hematoma | 40 (21.28) | 0 (0.00) | 8 (15.09) | 16 (22.22) | 12 (41.38) | 0.000 | |
| MMSE (median±SEM) | 12.00±0.89 | 25.00±0.48 | 22.50 ±1.23 | 0±1.10 | 0.00±0.97 | 0.000 | |
| APACHE‖(median±SEM) | 13.00±0.58 | 8.00±0.56 | 9.00±0.56 | 14.50±0.77 | 25.00±0.96 | 0.000 | |
| GCS (median±SEM) | 13.00±0.332 | 15.00±0.04 | 15.00±0.17 | 8.00±0.43 | 4.00±0.25 | 0.000 | |
| ICU LOS (d,median±SEM) | 5.00±5.83 | 2.20±1.32 | 3.00±9.91 | 7.00±13.12 | 8.00±4.71 | 0.000 | |
| Hospital LOS (d,median±SEM) | 13.00±6.85 | 8.00±1.34 | 12.00±2.79 | 18.00±7.06 | 9.00±41.14 | 0.000 | |
| Medication (n, %) | Sedative | 81 (43.09) | 4 (11.76) | 21 (39.62) | 28 (38.89) | 11 (37.93) | 0.027 |
| Resuscitant analeptic | 101 (53.72) | 11 (32.35) | 28 (52.83) | 27 (37.50) | 16 (55.17) | 0.100 | |
| Diuretic | 139 (73.94) | 6 (17.65) | 37 (69.81) | 45 (62.50) | 28 (96.55) | 0.000 | |
| Hormone | 111 (59.04) | 2 (5.88) | 21 (39.62) | 42 (58.33) | 27 (93.10) | 0.000 | |
| Ca2+ antagonist | 60 (31.91) | 6 (17.65) | 18 (33.96) | 14 (19.44) | 12 (41.38) | 0.046 | |
| Vasodilator | 8 (4.26) | 0 (0.00) | 6 (11.32) | 5 (6.94) | 7 (24.14) | 0.009 | |
| β-receptor blockers | 29 (15.43) | 2 (5.88) | 6 (11.32) | 5 (6.94) | 4 (13.79) | 0.587 | |
| Mortality (n, %) | 34 (18.09) | 0 (0.00) | 1 (1.89) | 18 (25) | 22 (75.86) | 0.000 | |
All nonparametric data were presented as median values with standard error of mean (SEM). All categorical data were presented as absolute numbers and percentages.
On admission, the patients presented with either skull fracture or contusion, or both of them. The contusion was mostly seen in extremely severe patients, whereas the skull fracture occurred randomly among the groups. TBI was also categorized into primary injury (subarachnoid hemorrhage, diffuse axonal injury) and secondary injury (cerebral hernia, epidural hematoma, subdural hematoma and intracerebral hematoma). All the injuries were mostly noted in the extremely severe patients. As expected, APACHE II and cognitive scores (GCS and MMSE) were significantly different among various groups, so were the secondary outcomes (ICU LOS and hospital LOS). It should be noticed that the extremely severe patients had the longest ICU LOS, and the severe patients had the longest hospital LOS. It could be explained by the fact that the extremely severe patients had the highest mortality rate (75.86%), thus they stayed less time in hospital than the severe patients.
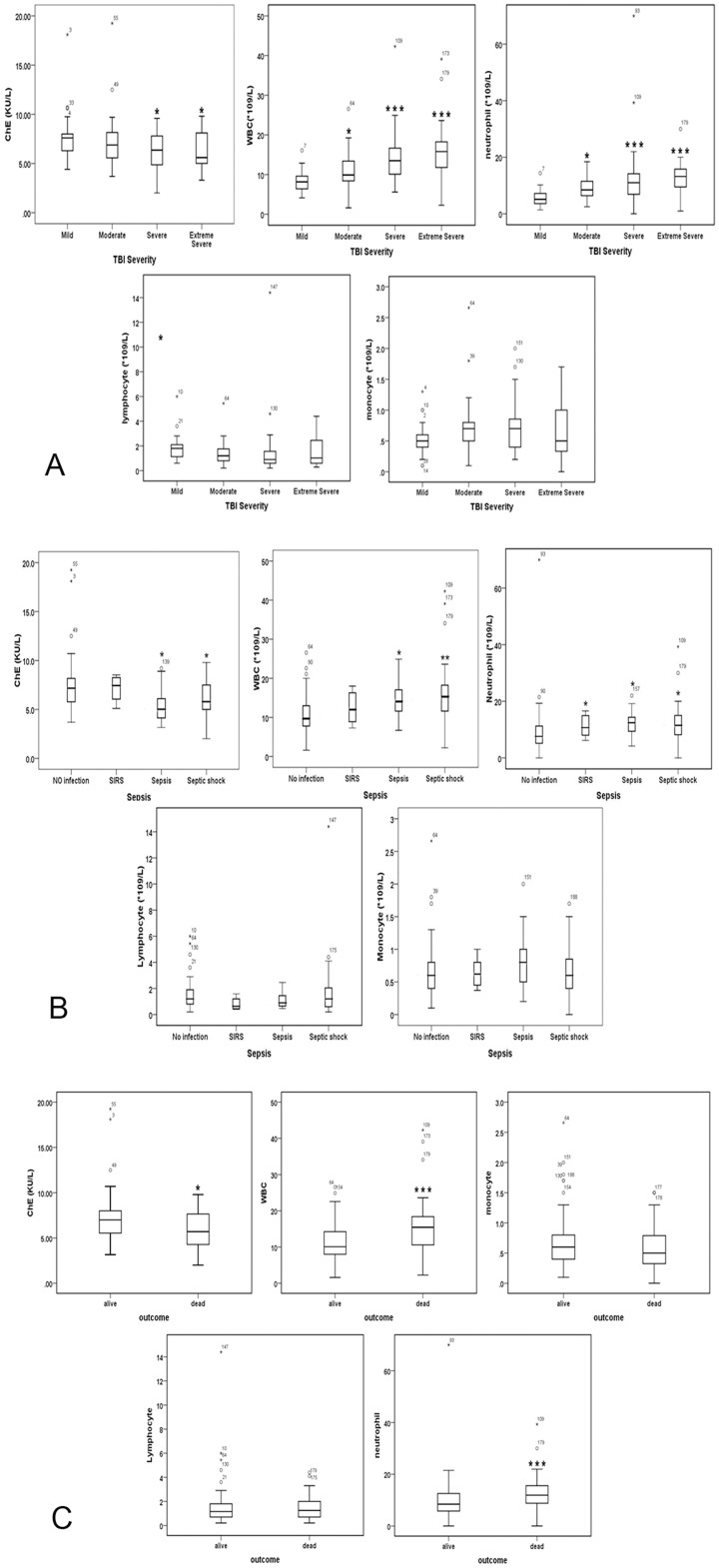
ChE activity was acutely decreased in non-surviving, septic patients with severe injury
Compared to matched controls, TBI patients showed lower serum AChE activity on admission (6.86±1.70 vs. 7.60±2.21, P = 0.029). To assess whether ChE activity was associated with the morbidity and mortality, subjects categorized by TBI severity, infected status (SIRS, sepsis, severe sepsis) and outcome (alive and dead) were analyzed by Post-hoc, Dunn’s multiple comparison tests following a Kruskal-Wallis test. Serum ChE activity on admission was significantly decreased in severe and extremely severe TBI patients as compared to that in mild patients. By contrast, both the white blood cell (WBC) counts and the neutrophil counts were elevated in groups of moderate, severe, and extremely severe patients in comparison to mild injured patients (Fig 1A). Similar results were seen in Fig 1B, in which ChE activity was significantly repressed in serum of infected patients as compared with non-infected patients. Non-survived patients also showed decreased ChE activity but increased WBC and neutrophil counts relative to survivors (Fig 1C). However, neither the lymphocyte nor the monocyte counts differed among groups of different categories.
Fig 1. Admission ChE activity and blood cell counts in TBI patients as classified according to the severity (A), infected status (B), and the outcome (C).
Boxes represented lower, median (line) and upper quartiles; whiskers showed the range of the data excluding outliers (。). *P<0.05, **P<0.01, ***P<0.001, compared with corresponding mild (A), non-infection (B) and survived (C) patients as analyzed by nonparametric test of several independent samples test (The Kruskal-Wallis H test).
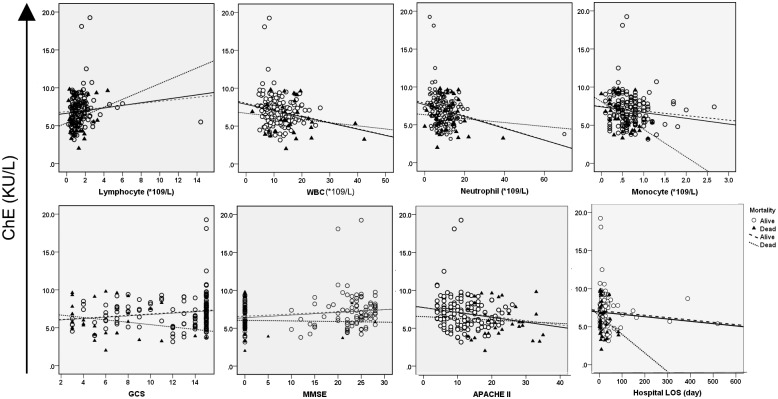
ChE activity was consistently depressed in non-survived, septic patients with severe injury
The trajectories of serum ChE activity in the first 2 weeks of injury were classified by TBI severity (Fig 2A), infected status (Fig 2B), and outcome (Fig 2C). ChE activity was decreased in mild TBI patients on day 4 post injury, then was elevated on day 6 until fully recovered on day 8. By contrast, in other three groups, serum ChE levels dropped sharply on day 2 post injury, and continued to decline during the observational period (Fig 2A). Likewise, septic or non-survived exhibited consistently lower levels of ChE relative to the corresponding non-infected or survived throughout their stay in hospital (Fig 2B and 2C).
Fig 2. Kinetics of serum ChE activities in TBI patients categorized by disease severity (A), infected status (B), and outcome (C).
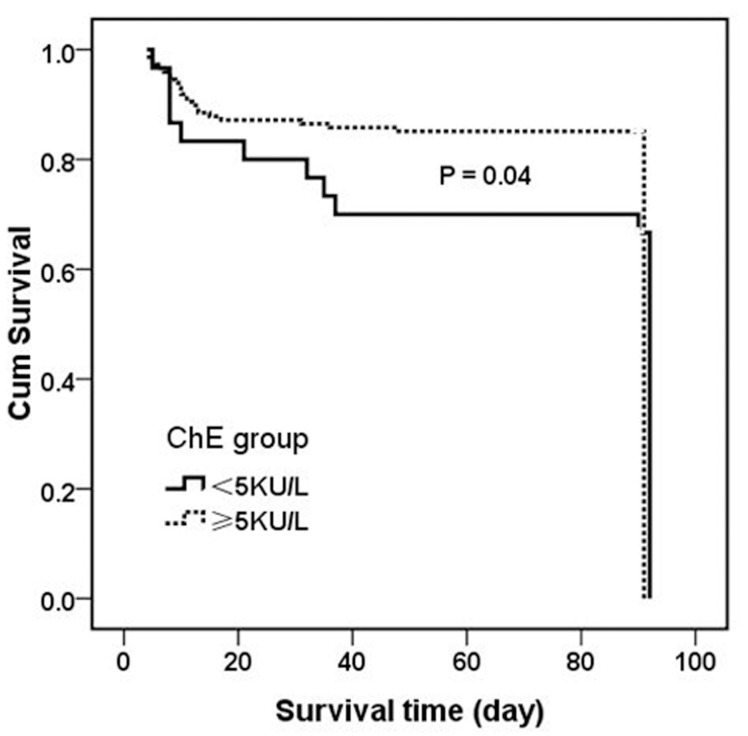
Association of ChE activity with clinical severity, neurocognitive and functional outcomes
Since serum ChE activities measured on admission were differentially reduced according to the severity, infected status and outcome, we wondered whether it could possibly be the diagnostic and prognostic biomarker for TBI. To this end, we examined the correlations of ChE activities with the blood cell counts, APACHE II score, cognitive and neurofunctional scores, and outcomes (ICU LOS, hospital LOS) in total population or in patients dichotomized by survival.
The modified scatter plots of ChE activities against the above parameters were constructed in total patients or patients classified by survival status (Fig 3). A calculated linear regression line was drawn for each plot followed by the Spearman correlation analysis. Admission ChE activities were significantly correlated with blood cell counts, APACHE II score, cognition scores and ICU LOS in total population. However, most of the correlations in the whole population did not apply to the subgroups of patients dichotomized by survival status (Table 2). It was noteworthy that the admission ChE activities were correlated positively with lymphocyte counts, negatively with WBC, neutrophil and monocyte counts. It could be possible that as a source of ChE, lymphocytes may respond toward brain injury differently from other cell types. Taken together, ChE on admission was indicated as a stratified biomarker in disease onset, severity stage, and final outcomes.
Fig 3. Scatterplot of the correlation of admission ChE activity with blood cell counts, neurocognitive scores, APACHE II score and hospital length of stay (LOS) in total population or in patients dichotomized by outcome.
Table 2. The correlation of serum ChE activity on admission with blood cell counts, neurocognitive scores, APACHE II score and hospital length of stay (LOS) in total or in patients with different outcome (Spearman’s correlation).
| Outcome | Correlation | WBC | lymphocyte | neutrophil | monocyte | APACHE II | GCS | MMSE | hospital LOS | ICU LOS |
|---|---|---|---|---|---|---|---|---|---|---|
| All | Coefficiency | -0.156 | 0.208 | -0.203 | -0.171 | -0.215 | 0.193 | 0.173 | -0.147 | -0.187 |
| P value | 0.041 | 0.007 | 0.009 | 0.028 | 0.005 | 0.011 | 0.026 | 0.054 | 0.014 | |
| alive | Coefficiency | -0.155 | 0.241 | -0.251 | -0.137 | -0.160 | 0.184 | 0.150 | -0.165 | -0.173 |
| P value | 0.067 | 0.004 | 0.003 | 0.107 | 0.059 | 0.029 | 0.084 | 0.050 | 0.040 | |
| dead | Coefficiency | -0.018 | 0.090 | 0.066 | -0.446 | 0.029 | -0.319 | -0.160 | -0.227 | -0.088 |
| P value | 0.920 | 0.629 | 0.726 | 0.015 | 0.875 | 0.075 | 0.380 | 0.211 | 0.631 |
There were significant correlations between serum ChE activity and the above parameters in all population, but not always so significant in subgroups dichotomized by outcome.
The above findings prompted us to evaluate the potential value of admission ChE level in foreseeing the cognitive and neurofunctional outcomes of TBI patients. Interestingly, serum ChE activity on admission was significantly associated with the cognitive (GCS and MMSE) and neurofunctional scores (GOS, FIM, RDS, DRS-F, MRS, QLI) assessed both on admission (in) and at discharge (out) as analyzed by two-tailed Spearman rank test (Table 3). Similarly, the admission ChE activities were correlated more significantly (less P values) with the parameters obtained at discharge than on admission, suggesting its long-term prognostic value on TBI functional recovery.
Table 3. Association of admission ChE activity with neurocognitive (GCS, MMSE) and functional scores examined both on admission (in) and at discharge (out) in TBI patients (Spearman’s correlation).
| Scales | GCS | MMSE | QLI | FIM | GOS | MRS | RDS | DRS-F | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Time | in | out | in | out | in | out | in | out | in | out | in | out | in | out | in | out |
| Median | 13 | 15 | 12 | 25 | 4 | 7 | 70 | 118 | 3 | 4 | 4 | 2 | 10 | 3 | 4 | 3 |
| SEM | 0.342 | 0.365 | 0.894 | 0.888 | 0.195 | 0.271 | 3.479 | 3.776 | 0.064 | 0.113 | 0.112 | 0.142 | 0.771 | 0.848 | 0.093 | 0.848 |
| Coefficiency | 0.179 | 0.216 | 0.162 | 0.212 | 0.186 | 0.254 | 0.176 | 0.218 | 0.217 | 0.219 | -0.15 | -0.23 | -0.17 | -0.24 | -0.17 | -0.23 |
| P value | 0.017 | 0.004 | 0.036 | 0.006 | 0.013 | 0.001 | 0.019 | 0.004 | 0.004 | 0.003 | 0.043 | 0.002 | 0.022 | 0.002 | 0.022 | 0.003 |
It was revealed the positive correlations of ChE activity with neurocognitive scores (GCS, MMSE) and neurofunctional score (QLI, FIM, GOS), but negatively with impairment scores (MRS, RDS, DRS-F).
ChE activity was not identified as the independent biomarker for mortality
To compare the importance of admission ChE activity along with other established markers in prediction of survival, both the bivariate analysis and multivariable analyses were performed. With bivariate logistic regression, using biomarkers as continuous independent variables, we found that ChE activity on admission and other variables such as the blood cell counts, cognitive scores, disease severity and infective status were significantly associated with 90-day mortality (Table 4). To avoid the influence caused by univariate analysis, a multivariable stepwise linear regression was also performed, taking into account the variables with clinical relevance (APACHE II), severity of illness (first hospital LOS, ICU LOS), neurocognitive scores (first GCS and MMSE), blood cell counts and the infective complication (sepsis) that were statistically significant in the bivariate analysis. As analyzed by Binary logistic regression after adjusting with age and gender, ChE on admission was not identified as an independent predictor for the probability of 90-day mortality (P = 0.078). However, the borderline p-value suggested that ChE on admission could possibly be used in predicting TBI mortality. Considering that some ChE values were missing, an different conclusion might be drawn if more data had been collected or multiple sampling had been met. Nevertheless, APACHE II score, sepsis, and ICU LOS were still independently associated with mortality (Table 4).
Table 4. Univariable and multivariable logistic regression model of prognosis the outcome at 90-days survival of TBI patients.
| Variables | Univariable Analysis | Multivariable Analysis | |||
|---|---|---|---|---|---|
| Nonsurvival(n = 42) | Survived(n = 146) | P value | OR (95%CI) | P value | |
| Age,year (Median,IQR) | 47.00 (32.00~71.25) | 41.00 (24.00~54.00) | 0.011 | 1.015 (0.961~1.072) | 0.589 |
| APACHE II (Median,IQR) | 22.50 (18.00~29.00) | 11.0 (6.00~15.00) | 0.000 | 1.316 (1.025~1.689) | 0.031 |
| GCS (Median,IQR) | 5.00 (3.00~7.25) | 15.0 (10.00~15.00) | 0.000 | 0.846 (0.537~1.332) | 0.469 |
| MMSE (Median,IQR) | 0.00 (0.00~0.00) | 20.0 (0.00~25.00) | 0.000 | 0.957 (0.848~1.079) | 0.471 |
| WBC,109/L (Median,IQR) | 15.47 (10.54~18.67) | 10.10 (8.00~14.28) | 0.000 | 1.081 (0.916~1.276) | 0.359 |
| Neutrophil,109/L (Median,IQR) | 11.92 (8.70~15.70) | 8.40 (5.75~12.61) | 0.000 | 1.008 (0.892~1.139) | 0.899 |
| Lymphocyte,109/L (Median,IQR) | 1.25 (0.65~2.05) | 1.15 (0.70~1.80) | 0.562 | 5.064 (1.216~21.038) | — |
| Monocyte,109/L (Median,IQR) | 0.50 (0.32~0.80) | 0.60 (0.40~0.80) | 0.137 | 0.003 (0.000~0.190) | — |
| ChE,KU/L (Median,IQR) | 5.70 (4.27~7.80) | 7.0 (5.50~8.00) | 0.023 | 0.660 (0.416~1.047) | 0.078 |
| Hospital LOS,day (Median,IQR) | 9.00 (5.00 ~17.50) | 14.00 (9.00~25.25) | 0.005 | 0.974 (0.936~1.011) | 0.159 |
| ICU LOS,day (Median,IQR) | 6.5(4.00~ 11.75) | 4.00 (2.00 ~10.00) | 0.006 | 1.007 (1.000~1.013) | 0.041 |
| Sepsis, n (%) | 38 (90.48%) | 34 (23.29%) | 0.000 | 1.819 (0.302~3.918) | 0.048 |
Data were expressed as number and percentage, or median and 25th and 75th percentiles. Differences between survivors and non-survivors were evaluated by the Mann-Whitney U test. CI: Confidence interval.
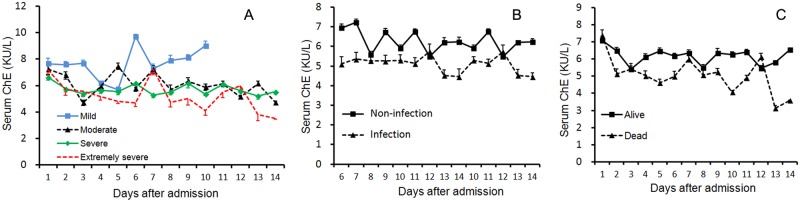
The predictive value of admission ChE activity for mortality
Since the admission ChE activity was closely associated with the worst outcome, we wondered to what extent it was of any value in predicting the mortality. Receiver operating characteristic (ROC) analysis (S1 Fig) showed that area under the curve (AUC) for ChE was 0.381 (P = 0.046), which was inferior to that for either APACHE II (0.914, P = 0.000) or WBC (0.695, P = 0.001) (S1 Table). However, at the cutoff value of 5 kU/L, the sensitivity of ChE for correct prediction of death was 82.4% and the specificity was 92.2%. When patients were divided into two subcohorts according to the optimal threshold for serum ChE level in ROC analysis, a ChE level less than 5 kU/L (lower ChE group) was correlated markedly with poor overall patient survivals compared with a ChE level higher than 5 kU/L (higher ChE group) as indicated by Kaplan-Meier analysis (p = 0.04 by log-rank test) (Fig 4). The 90-day survival rates for patients with a ChE level<5 kU/L vs. ≥5 kU/L were 62% vs. 80%, respectively.
Fig 4. Kaplan-Meier analysis comparing the cumulative percentages of patients who survived according to their serum ChE activities measured 72 hours after TBI.
Patients with serum ChE levels >5 kU/L showed a significantly higher chance to survive than patients with lower levels (log-rank test, p = 0.04).
Additional Cox regression analysis revealed that only hospital LOS and sepsis were associated with the surviving days, with the Cox regression hazard risk ratio of 0.996 [p = 0.044, 95% confidence interval (CI): 0.993–1.000] and 1.311 (p = 0.005, 95% CI: 1.087–1.581), respectively. Once again, serum ChE activity on admission was not significantly associated with the surviving days with hazard risk ratio of 1.021 (p = 0.601, 95% CI: 0.945–1.102).
Discussion
The cholinergic anti-inflammatory pathway has been recognized as a major regulatory component of stress response and was proposed to result in immune paralysis in TBI patients [33]. Our study identified prominent yet distinct correlations of on admission serum cholinergic parameter with TBI severity, infective status, survival, cognitive and neurofunctional outcomes, thus providing useful diagnostic and prognostic insights of TBI. Reduction in serum ChE activity and consequent increased ACh implied augmented cholinergic signaling after TBI, potentially serving as protection from uncontrolled inflammatory reactions.
Our study has several strengths in the following aspects. We for the first time found the acute decrease of serum ChE activity in the non-survivors vs. survivors after TBI. In addition to its neuroendocrinal effect as the pivotal neurotransmitter [24], accumulating evidence have demonstrated that ACh levels are also crucial for controlling immune response in both the brain and the peripheral tissues [51]. As AChE is a key contributor to sustain ACh level, several studies had shown dynamic changes in AChE activity in the brain after TBI [28,29]. Accordingly, the cerebellar expression of miR-132 which potentiated cholinergic anti-inflammatory signaling by targeting AChE [52] was down-regulated early after brain injury [28]. The physiological and pathological significance of cerebral AChE after brain damage remains to be identified. It is presumed that the initial stimulus induces excitation through ACh release, and feedback overexpression of AChE acts to dampen excessive neurotransmission back towards normal levels [6]. So far, only one study had identified serum ChE to be acutely decreased in 50 TBI patients, indicating severe damage and poor prognosis [32]. In accordance, the reduced serum ChE in our observation was also associated with TBI severity and mortality. Furthermore, consistent with previous study that serum cholinesterase activity could distinguish stroke patients from controls and predict 12-month mortality [14], admission ChE at cutoff level of 5 kU/L could also distinguish the survival from the non-survival in our TBI patients. In addition, the kinetics of serum ChE activity in survivals was also distinct from that in non-survivals. Although admission ChE did not reach its independent significance in predicting mortality, the borderline p-value still implied its prognostic value in clinic. Moreover, considering that the ChE data was from single blood test, multiple sampling might increase its specificity and sensitivity. As the reference, the trajectories of serum ChE activity could also predict the morbidity and mortality of TBI patients regardless of the treatment. Therefore, serum ChE activity should be followed for both diagnostic and prognostic purposes.
The decreased serum ChE level seemed to be in conflict with aforementioned increased AChE in the brain. We assume that serum AChE activity might reflect the cholinergic anti- inflammatory activity in response to TBI other than a neurotransmitter in the brain. Direct evidence of augmented sympathetic and attenuated parasympathetic drive was found in patients with brain damage in relation to the severity [53], thereby potentiating the pro-inflammatory response. Furthermore, serum AChE activity might potentially serve as predictor of risk of inflammatory response in healthy subjects [54] and patients with infective diseases [55,56]. Both in vitro and in vivo, AChE was substantially down-regulated after lipopolysaccharide challenge, suggesting that systemic reduction in AChE activity was an integral part of the post-inflammatory response [52]. Clinical study also showed that serum AChE activity was inversely and prominently correlated with inflammatory markers in post-stroke patients [14]. Our second intriguing finding was that serum ChE activity was decreased in patients with sepsis and septic shock in comparison to patients without septic complication. The trajectory of serum ChE activity also remained at lower level in septic vs. non-septic patients, further confirming serum ChE as a marker of infection [14]. In the current study, we determined the total ChE activities other than AChE alone in patients suffered from TBI. The summated ACh hydrolyzing activities of free AChE and BChE in the plasma might reflect the “Cholinergic Status” as a whole. Thus, a decrease serum ChE level in TBI patients might directly reflect the prominent inflammatory response toward TBI. Considering that sepsis was more frequently seen in non-survivors compared with survivors (90.5% vs. 23.3%), there would be possible a causal relationship among serum ChE level, sepsis and mortality.
The third highlight of the present study was that ChE activities were differentially reduced according to the disease severity. It was found that patients with severe and extremely severe TBI showed more reduction in ChE activity as opposed to patients with mild TBI, indicating that the extent of attenuation in cholinergic activity was related to TBI severity. Moreover, the trajectory of serum ChE activity could distinguish the patients of extremely severe TBI from the other three degrees of severity, implying that cholinergic activity was progressively differentiated according to injury severity.
TBI may lead to physical, emotional, intellectual and/or social changes for the survivors [57]. Our most encouraging finding was that ChE activity on admission was significantly associated with neurocognitive and functional scores assessed both on admission and at discharge, suggesting that serum ChE activity might act as a putative link to neurofunctional outcome following TBI. It is not uncommon that TBI patients may show cholinergic-dependent [58] transient delirium [59] and long-term cognitive decline [60]. As a support, serum AChE activity showed inverse, reciprocal associations with anxiety measures [54]. Thus, it was tempting to speculate the close relationship between serum ChE activity and the cognition scores (GCS, MMSE) assessed simultaneously on admission. However, it was extraordinarily surprising to notice that serum ChE level on admission was correlated to cognition scores more significantly at discharge than on admission. Since cholinergic depletion predisposes to development of acute cognitive deficits upon subsequent systemic inflammatory insult [61], the cholinergic hypothesis of delirium may be more relevant in patients with prior vulnerability in the cholinergic system [62]. Therefore, it was reasonable to speculate that admission ChE level that reflecting cholinergic signaling immediately after brain injury might be associated with the cognition outcome at discharge. Similar associations were also found between the serum ChE level on admission and the neurofunctional measures. The neurological outcome is mostly determined by the primary brain damage. Because admission serum ChE level may represent the parasympathetic activity following brain damage, the close association of admission serum ChE level with the neurological function scores was within expectation. For clinical practice, serum AChE activity could be a novel predictive parameter to improve and personalize TBI outcomes. Once again, serum ChE activity on admission was correlated highly with the neurofunctional scores at discharge than on admission, strongly supporting its prognostic potential for TBI recovery.
Conclusions
Taken together, acute serum ChE decrease in response to TBI might facilitate chronic inflammatory response, resulting in secondary injury and poor outcome after TBI. The extent of reduction might potentially predict surviving possibility, guiding treatment and rehabilitation practice. Although it was not the independent predictor for mortality, admission ChE activity could be included in one of the biomarker panel for the prognosis of TBI mortality.
Supporting Information
(TIF)
(XLSX)
(XLSX)
(DOCX)
(DOCX)
(DOCX)
(XLSX)
(DOCX)
(XLSX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
This study was supported by National Natural Science Foundation (81272089, 81130035, 81372054, 81121004) for QHZ and YMY in the collection and analysis of data, the National Basic Research Program of China (2012CB518102) for YMY in the writing of the manuscript and decision to submit the manuscript, and Twelve-Five Plan for Military Scientific Foundation (BWS12J050) for QHZ in the design and writing of the manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by National Natural Science Foundation (81272089, 81130035, 81372054, 81121004) for QHZ and YMY in the collection and analysis of data, the National Basic Research Program of China (2012CB518102) for YMY in the writing of the manuscript and decision to submit the manuscript, and Twelve-Five Plan for Military Scientific Foundation (BWS12J050) for QHZ in the design and in the collection of data.
References
- 1. Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC (2007) The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation 22: 341–353. [PubMed] [Google Scholar]
- 2. Adamczak S, Dale G, de Rivero Vaccari JP, Bullock MR, Dietrich WD, et al. (2012) Inflammasome proteins in cerebrospinal fluid of brain-injured patients as biomarkers of functional outcome: clinical article. J Neurosurg 117: 1119–1125. 10.3171/2012.9.JNS12815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Woodcock T, Morganti-Kossmann MC (2013) The role of markers of inflammation in traumatic brain injury. Front Neurol 4: 18 10.3389/fneur.2013.00018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chrousos GP (2009) Stress and disorders of the stress system. Nat Rev Endocrinol 5: 374–381. 10.1038/nrendo.2009.106 [DOI] [PubMed] [Google Scholar]
- 5. Padgett DA, Glaser R (2003) How stress influences the immune response. Trends Immunol 24: 444–448. [DOI] [PubMed] [Google Scholar]
- 6. Kaufer D, Friedman A, Seidman S, Soreq H (1998) Acute stress facilitates long-lasting changes in cholinergic gene expression. Nature 393: 373–377. [DOI] [PubMed] [Google Scholar]
- 7. Kawashima K, Fujii T (2000) Extraneuronal cholinergic system in lymphocytes. Pharmacol Ther 86: 29–48. [DOI] [PubMed] [Google Scholar]
- 8. Rosas-Ballina M, Olofsson PS, Ochani M, Valdes-Ferrer SI, Levine YA, Reardon C,et al. (2011) Acetylcholine-synthesizing T cells relay neural signals in a vagus nerve circuit. Science 334: 98–101. 10.1126/science.1209985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Borovikova LV, Ivanova S, Zhang M, Yang H, Botchkina GI, Watkins LR, et al. (2000) Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature 405: 458–462. [DOI] [PubMed] [Google Scholar]
- 10. Wang H, Yu M, Ochani M, Amella CA, Tanovic M, Susarla S, et al. (2003) Nicotinic acetylcholine receptor alpha7 subunit is an essential regulator of inflammation. Nature 421: 384–388. [DOI] [PubMed] [Google Scholar]
- 11. Gilboa-Geffen A, Hartmann G, Soreq H (2012) Stressing hematopoiesis and immunity: an acetylcholinesterase window into nervous and immune system interactions. Front Mol Neurosci 5: 30 10.3389/fnmol.2012.00030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ofek K, Krabbe KS, Evron T, Debecco M, Nielsen AR, Brunnsgaad H,et al. (2007) Cholinergic status modulations in human volunteers under acute inflammation. J Mol Med (Berl) 85: 1239–1251. [DOI] [PubMed] [Google Scholar]
- 13. Cole CR, Blackstone EH, Pashkow FJ, Snader CE, Lauer MS (1999) Heart-rate recovery immediately after exercise as a predictor of mortality. N Engl J Med 341: 1351–1357. [DOI] [PubMed] [Google Scholar]
- 14. Ben Assayag E, Shenhar-Tsarfaty S, Ofek K, Soreq L, Bova I, Shopin L, et al. (2010) Serum cholinesterase activities distinguish between stroke patients and controls and predict 12-month mortality. Mol Med 16: 278–286. 10.2119/molmed.2010.00015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li DJ, Evans RG, Yang ZW, Song SW, Wang P, Ma XJ, et al. (2011) Dysfunction of the cholinergic anti-inflammatory pathway mediates organ damage in hypertension. Hypertension 57: 298–307. 10.1161/HYPERTENSIONAHA.110.160077 [DOI] [PubMed] [Google Scholar]
- 16. Adabag AS, Grandits GA, Prineas RJ, Crow RS, Bloomfield HE, Neaton JD,et al. (2008) Relation of heart rate parameters during exercise test to sudden death and all-cause mortality in asymptomatic men. Am J Cardiol 101: 1437–1443. 10.1016/j.amjcard.2008.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Soreq H, Seidman S (2001) Acetylcholinesterase—new roles for an old actor. Nat Rev Neurosci 2: 294–302. [DOI] [PubMed] [Google Scholar]
- 18. Loewenstein-Lichtenstein Y, Schwarz M, Glick D, Norgaard-Pedersen B, Zakut H, Soreq H. (1995) Genetic predisposition to adverse consequences of anti-cholinesterases in 'atypical' BCHE carriers. Nat Med 1: 1082–1085. [DOI] [PubMed] [Google Scholar]
- 19. Andrews PJ, Sleeman DH, Statham PF, McQuatt A, Corruble V, Jones PA, et al. (2002) Predicting recovery in patients suffering from traumatic brain injury by using admission variables and physiological data: a comparison between decision tree analysis and logistic regression. J Neurosurg 97: 326–336. [DOI] [PubMed] [Google Scholar]
- 20. Collaborators MCT, Perel P, Arango M, Clayton T, Edwards P, Komolafe E, et al. (2008) Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ 336: 425–429. 10.1136/bmj.39461.643438.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Piek J, Chesnut RM, Marshall LF, van Berkum-Clark M, Klauber MR, Blunt BA, et al. (1992) Extracranial complications of severe head injury. J Neurosurg 77: 901–907. [DOI] [PubMed] [Google Scholar]
- 22. Schirmer-Mikalsen K, Vik A, Gisvold SE, Skandsen T, Hynne H, Klepstad P. (2007) Severe head injury: control of physiological variables, organ failure and complications in the intensive care unit. Acta Anaesthesiol Scand 51: 1194–1201. [DOI] [PubMed] [Google Scholar]
- 23. Zygun DA, Kortbeek JB, Fick GH, Laupland KB, Doig CJ (2005) Non-neurologic organ dysfunction in severe traumatic brain injury. Crit Care Med 33: 654–660. [DOI] [PubMed] [Google Scholar]
- 24. Catania A, Lonati C, Sordi A, Gatti S (2009) Detrimental consequences of brain injury on peripheral cells. Brain Behav Immun 23: 877–884. 10.1016/j.bbi.2009.04.006 [DOI] [PubMed] [Google Scholar]
- 25. Chamorro A, Urra X, Planas AM (2007) Infection after acute ischemic stroke: a manifestation of brain-induced immunodepression. Stroke 38: 1097–1103. [DOI] [PubMed] [Google Scholar]
- 26. Meisel C, Schwab JM, Prass K, Meisel A, Dirnagl U (2005) Central nervous system injury-induced immune deficiency syndrome. Nat Rev Neurosci 6: 775–786. [DOI] [PubMed] [Google Scholar]
- 27. Hu T, Fu Q, Liu X, Zhang H, Dong M (2009) Increased acetylcholinesterase and capase-3 expression in the brain and peripheral immune system of focal cerebral ischemic rats. J Neuroimmunol 211: 84–91. 10.1016/j.jneuroim.2009.04.002 [DOI] [PubMed] [Google Scholar]
- 28. Valiyaveettil M, Alamneh YA, Miller SA, Hammamieh R, Arun P, Wang Y, et al. (2013) Modulation of cholinergic pathways and inflammatory mediators in blast-induced traumatic brain injury. Chem Biol Interact 203: 371–375. 10.1016/j.cbi.2012.10.022 [DOI] [PubMed] [Google Scholar]
- 29. Ostberg A, Virta J, Rinne JO, Oikonen V, Luoto P, Någren K, et al. (2011) Cholinergic dysfunction after traumatic brain injury: preliminary findings from a PET study. Neurology 76: 1046–1050. 10.1212/WNL.0b013e318211c1c4 [DOI] [PubMed] [Google Scholar]
- 30. da Silva AS, Monteiro SG, Goncalves JF, Spanevello R, Schmatz R, Oliveira CB, et al. (2011) Trypanosoma evansi: immune response and acetylcholinesterase activity in lymphocytes from infected rats. Exp Parasitol 127: 475–480. 10.1016/j.exppara.2010.10.017 [DOI] [PubMed] [Google Scholar]
- 31. da Silva CB, Wolkmer P, da Silva AS, Paim FC, Tonin AA, Castro VS, et al. (2012) Cholinesterases as markers of the inflammatory process in rats infected with Leptospira interrogans serovar Icterohaemorrhagiae. J Med Microbiol 61: 278–284. 10.1099/jmm.0.035501-0 [DOI] [PubMed] [Google Scholar]
- 32. Rao CJ, Mohanty S, Shukla PK, Reddy YJ (1978) Significance of serum cholinesterase levels in human head injury. Indian J Med Res 68: 668–674. [PubMed] [Google Scholar]
- 33. Kox M, Pompe JC, Pickkers P, Hoedemaekers CW, van Vugt AB, van der Hoeven JG. (2008) Increased vagal tone accounts for the observed immune paralysis in patients with traumatic brain injury. Neurology 70: 480–485. 10.1212/01.wnl.0000279479.69502.3e [DOI] [PubMed] [Google Scholar]
- 34. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. (2003) 2001 SCCM/ESICM/ACCP/ ATS/SIS International Sepsis Definitions Conference. Crit Care Med 31: 1250–1256. [DOI] [PubMed] [Google Scholar]
- 35. Kiguchi T, Nakamori Y, Yamakawa K, Kitayama J, Wada D, Ogawa Y, et al. (2013) Maximal chemiluminescent intensity in response to lipopolysaccharide assessed by endotoxin activity assay on admission day predicts mortality in patients with sepsis. Crit Care Med 41: 1443–1449. 10.1097/CCM.0b013e31827ca960 [DOI] [PubMed] [Google Scholar]
- 36. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 101: 1644–1655. [DOI] [PubMed] [Google Scholar]
- 37. Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985) APACHE II: a severity of disease classification system. Crit Care Med 13: 818–829. [PubMed] [Google Scholar]
- 38. Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270: 2957–2963. [DOI] [PubMed] [Google Scholar]
- 39. Hammond FM, Grattan KD, Sasser H, Corrigan JD, Bushnik T, Zafonte RD. (2001) Long-term recovery course after traumatic brain injury: a comparison of the functional independence measure and disability rating scale. J Head Trauma Rehabil 16: 318–329. [DOI] [PubMed] [Google Scholar]
- 40. Jennett B, Bond M (1975) Assessment of outcome after severe brain damage. Lancet 1: 480–484. [DOI] [PubMed] [Google Scholar]
- 41. Rappaport M, Hall KM, Hopkins K, Belleza T, Cope DN (1982) Disability rating scale for severe head trauma: coma to community. Arch Phys Med Rehabil 63: 118–123. [PubMed] [Google Scholar]
- 42. Kang J, Park TH, Lee KB, Park JM, Ko Y, Lee SJ,et al. (2014) Symptomatic steno-occlusion in patients with acute cerebral infarction: prevalence, distribution, and functional outcome. J Stroke 16: 36–43. 10.5853/jos.2014.16.1.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Veysey BM, Steadman HJ, Morrissey JP, Johnsen M, Beckstead JW (1998) Using the Referral Decision Scale to screen mentally ill jail detainees: validity and implementation issues. Law Hum Behav 22: 205–215. [DOI] [PubMed] [Google Scholar]
- 44. Torrance GW, Feeny DH, Furlong WJ, Barr RD, Zhang Y, Wang Q. (1996) Multiattribute utility function for a comprehensive health status classification system. Health Utilities Index Mark 2. Med Care 34: 702–722. [DOI] [PubMed] [Google Scholar]
- 45. Hanks RA, Millis SR, Ricker JH, Giacino JT, Nakese-Richardson R, Frol AB, et al. (2008) The predictive validity of a brief inpatient neuropsychologic battery for persons with traumatic brain injury. Arch Phys Med Rehabil 89: 950–957. 10.1016/j.apmr.2008.01.011 [DOI] [PubMed] [Google Scholar]
- 46. Kouloulas EJ, Papadeas AG, Michail X, Sakas DE, Boviatsis EJ (2013) Prognostic value of time-related Glasgow coma scale components in severe traumatic brain injury: a prospective evaluation with respect to 1-year survival and functional outcome. Int J Rehabil Res 36: 260–267. 10.1097/MRR.0b013e32835fd99a [DOI] [PubMed] [Google Scholar]
- 47. Shukla D, Devi BI, Agrawal A (2011) Outcome measures for traumatic brain injury. Clin Neurol Neurosurg 113: 435–441. 10.1016/j.clineuro.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 48. Seong JW, Kim MH, Shin HK, Lee HD, Park JB, Yang DS. (2014) Usefulness of the combined motor evoked and somatosensory evoked potentials for the predictive index of functional recovery after primary pontine hemorrhage. Ann Rehabil Med 38: 13–18. 10.5535/arm.2014.38.1.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19: 604–607. [DOI] [PubMed] [Google Scholar]
- 50. De Filippis S, Erbuto D, Gentili F, Innamorati M, Lester D, Tatarelli R,et al. (2008) Mental turmoil, suicide risk, illness perception, and temperament, and their impact on quality of life in chronic daily headache. J Headache Pain 9: 349–357. 10.1007/s10194-008-0072-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Valvezan AJ, Klein PS (2012) GSK-3 and Wnt Signaling in Neurogenesis and Bipolar Disorder. Front Mol Neurosci 5: 1 10.3389/fnmol.2012.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Shaked I, Meerson A, Wolf Y, Avni R, Greenberg D, Gilboa-Geffen A,et al. (2009) MicroRNA-132 potentiates cholinergic anti-inflammatory signaling by targeting acetylcholinesterase. Immunity 31: 965–973. 10.1016/j.immuni.2009.09.019 [DOI] [PubMed] [Google Scholar]
- 53. Su CF, Kuo TB, Kuo JS, Lai HY, Chen HI (2005) Sympathetic and parasympathetic activities evaluated by heart-rate variability in head injury of various severities. Clin Neurophysiol 116: 1273–1279. [DOI] [PubMed] [Google Scholar]
- 54. Sklan EH, Lowenthal A, Korner M, Ritov Y, Landers DM, Rankinen T, et al. (2004) Acetylcholinesterase/ paraoxonase genotype and expression predict anxiety scores in Health, Risk Factors, Exercise Training, and Genetics study. Proc Natl Acad Sci U S A 101: 5512–5517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kawashima K, Ishikawa H, Mochizuki M (1980) Radioimmunoassay for acetylcholine in the rat brain. J Pharmacol Methods 3: 115–123. [DOI] [PubMed] [Google Scholar]
- 56. Wolkmer P, Lopes ST, Franciscato C, da Silva AS, Traesel CK, Siqueira LC, et al. (2010) Trypanosoma evansi: cholinesterase activity in acutely infected Wistar rats. Exp Parasitol 125: 251–255. 10.1016/j.exppara.2010.01.024 [DOI] [PubMed] [Google Scholar]
- 57. Kraus JF, McArthur DL (1996) Epidemiologic aspects of brain injury. Neurol Clin 14: 435–450. [DOI] [PubMed] [Google Scholar]
- 58. Cunningham C, Maclullich AM (2013) At the extreme end of the psychoneuroimmunological spectrum: delirium as a maladaptive sickness behaviour response. Brain Behav Immun 28: 1–13. 10.1016/j.bbi.2012.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kennedy RE, Nakase-Thompson R, Nick TG, Sherer M (2003) Use of the cognitive test for delirium in patients with traumatic brain injury. Psychosomatics 44: 283–289. [DOI] [PubMed] [Google Scholar]
- 60. Hopkins RO, Jackson JC (2006) Long-term neurocognitive function after critical illness. Chest 130: 869–878. [DOI] [PubMed] [Google Scholar]
- 61. Field RH, Gossen A, Cunningham C (2012) Prior pathology in the basal forebrain cholinergic system predisposes to inflammation-induced working memory deficits: reconciling inflammatory and cholinergic hypotheses of delirium. J Neurosci 32: 6288–6294. 10.1523/JNEUROSCI.4673-11.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ballard C, Gauthier S, Corbett A, Brayne C, Aarsland D, Jones E. (2011) Alzheimer's disease. Lancet 377: 1019–1031. 10.1016/S0140-6736(10)61349-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(XLSX)
(XLSX)
(DOCX)
(DOCX)
(DOCX)
(XLSX)
(DOCX)
(XLSX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.