Abstract
Introduction:
Pessary use is the preferred non-surgical treatment option for female pelvic organ prolapse. As pessaries can be used chronically to alter pelvic floor anatomy, consideration of short-and long-term complications is important in patient management. We systematically reviewed articles describing the complications of pessary use to determine frequency and severity.
Methods:
A systematic search via MEDLINE and PubMed using the key terms “complications,” “pessary,” “pelvic organ prolapse,” “side effects” was conducted for the years 1952 to 2014 inclusively. Selected articles cited in the publications identified were also considered. Only full-text material published in English was reviewed. All pessary-related complications described were collated; overall frequency within case reports and case series were calculated and severity was graded using the Clavien-Dindo classification.
Results:
In total, 61 articles met the inclusion criteria. The most common complications reported were vaginal discharge/vaginitis, erosion, and bleeding. Complications were related to pessary shape and material, and duration in situ. Clavien-Dindo classification of complication severity found that all 5 grade levels were attributed to pessary use; serious grade 4 and 5 complications included cancer, adjacent organ fistula and death.
Conclusion:
There are few detailed reports of complications of pessary use relative to the estimated frequency of pessary use worldwide. Prospective studies documenting complications by shape, material, and size, and objectively classifying complication severity are required. As serious grade 4 and 5 complications of pessary use occur, further development of clinical follow-up guidelines for long-term pessary users is justified.
Introduction
Pelvic organ prolapse (POP) is a widespread and troublesome condition related to loss of anatomic support of the pelvic organs.1,2 Recognition of the condition can be traced back to Egypt in 1500 BC and treatment with pessary use was demonstrated by Hippocrates in 400 BC.3,4 The word “pessary” derives from the Greek word “peso” – an oval stone. The origin for all intrauterine devices is probably the use of oval stones inserted into the uterus in saddle camels to prevent conception during long desert journeys.5–8
The use of pessaries is common; more than 85% of gynecologists9 and nearly 98% of urogynecologists prescribe them.10 They provide anatomic support and can be used as a treatment of choice or in those who decline surgery (e.g., women who plan future childbearing, require temporary relief of prolapse while waiting for surgery or during pregnancy, or do not want surgical repair11,12).
Pessaries have few complications, although some authors suggest that they require lifestyle modification,13,14 and the variety of shapes and sizes available affords choice and individual fitting.15 However, data on complications relevant to appropriate discussion of consent with patients and planning of long-term follow up strategies are limited. The side effects of pessary use are not obvious; moreover it is not clear whether the therapeutic impact is high enough to overlook possible risks or which patients benefit the most from pessary treatment.16 Few studies have tested the relative value of different practice models for pessary use, although pessaries have assumed growing importance in the treatment of POP.17
A 2004 Cochrane review of pessaries use for POP and updated in 201313,18 found only 1 randomized controlled trial examining the efficacy of pessary use.13 Complications were described as rare and there was no consensus on complication management. Furthermore, there was no reference to complication severity grading.
In this study, we conducted an integrative review of reported complications related to pessary use, and classified them according to a standardized severity scale. Since pessaries were used as an alternative to surgical treatment, and are a physical therapy akin to surgical therapy, the Clavien-Dindo19 complication severity grading system was used. Conceptually this provided a comparison to reported surgical complications and also provided a means to appropriately inform patients about complications in the context of informed consent. A secondary objective was to categorize complications according to pessary shape, size, and material used.
Methods
Systematic review search strategy
A systematic search via MEDLINE and PubMed using the key terms “complications,” “pessary,” “pelvic organ prolapse,” “side effects” was conducted for the years 1952 to 2014 inclusively. Included articles had to have been published in English, peer-reviewed journals, with the full-text available. Review articles were excluded because they either did not contain original material or duplicated extant reports.
Analytic process
The authors reviewed each article to extract the following: complication(s) of pessary use, number of subjects, age, type of pessary (ring, shelf, Gellhorn, and cube), size, and material composition (silicon, polythene, gold, and metallic). In papers in which the nature or management of the complication was described, we categorized complication severity according to the Clavien-Dindo system.19 In the instance of multiple reports of a single complication, we reported the severity of the outcome in more than 1 grade based on description of the management. Removal of a pessary as a management strategy, or a change from the treatment plan of self-care to dependent care was classified as a Grade 1 complication. This was felt to be akin to deviation from a standard protocol in the surgical setting.
Results
In total, we identified 99 full-text articles. Of these, 61 met the inclusion criteria (Fig. 1): 25 original case studies and 36 case reports. We excluded 21 review articles and 17 additional articles due to duplication or unrelated content (Fig. 1).
Fig. 1.
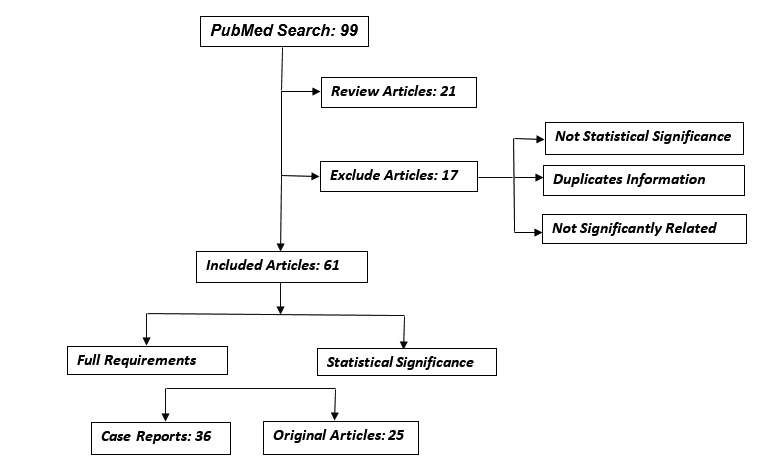
Flowchart of citation review and inclusion strategy.
In 34 papers, we were able to assess type, shape, size or composition of the pessary with complications (Table 2). Thirteen papers discussed complications related to pessary size.20–31 By combining the data in both case reports and case studies, we found that the most frequent complications were: vaginal discharge, bleeding, vesicovaginal fistula, erosion, ulceration, and foul odor (Table 1). We graded the reported complications using the Clavien-Dindo classification (Table 3).
Table 2.
| Type of pessary | Gellhorn | Ring | Shelf | Porcelain | Doughnut | Cube | Metallic ring | Total |
|---|---|---|---|---|---|---|---|---|
| No. studies | 6 | 15 | 8 | 1 | 1 | 1 | 2 | 34 |
| No. patients | 7 | 397 | 9 | 1 | 1 | 1 | 3 | 419 |
| Erosion | 2 | 40 | 2 | 0 | 0 | 0 | 0 | |
| Vesicovaginal fistula | 6 | 2 | 4 | 1 | 0 | 0 | 0 | |
| Infection | 3 | 13 | 0 | 0 | 0 | 0 | 0 | |
| Ulceration | 0 | 4 | 1 | 0 | 0 | 1 | 0 | |
| Bleeding | 1 | 28 | 3 | 1 | 0 | 0 | 1 | |
| Death | 0 | 0 | 2 | 0 | 0 | 0 | 0 | |
| Discomfort | 1 | 10 | 1 | 0 | 0 | 0 | 0 | |
| Vaginal discharge | 1 | 47 | 2 | 0 | 1 | 1 | 2 | |
| Fibrosis | 1 | 1 | 1 | 0 | 0 | 0 | 0 | |
| Foul odor | 1 | 23 | 0 | 0 | 0 | 0 | 0 | |
| Slipped | 0 | 16 | 0 | 0 | 0 | 0 | 0 | |
| Ureteric obstruction | 0 | 2 | 2 | 0 | 1 | 0 | 0 | |
| Cancer | 1 | 6 | 0 | 0 | 0 | 0 | 0 | |
| Vaginitis | 0 | 18 | 2 | 0 | 0 | 0 | 0 | |
| Rectovaginal fistula | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
Table 1.
| Type of study | Case report | Case series | Total |
|---|---|---|---|
| No. studies | 34 | 25 | 61 |
| No. total subjects | 52 | 1138 | 1190 |
| Erosion | 11 | 44 | 55 |
| Infection | 6 | 13 | 18 |
| Vesicovaginal fistula | 16 | 18 | 34 |
| Bleeding | 19 | 10 | 29 |
| Ulceration | 10 | 4 | 14 |
| Death | 4 | 5 | 9 |
| Pain and discomfort | 2 | 60 | 62 |
| Vaginitis | 3 | 14 | 17 |
| Vaginal discharge | 21 | 35 | 56 |
| Foul odor | 9 | 18 | 27 |
| Cancer | 9 | 0 | 9 |
| Fibrosis | 2 | 0 | 22 |
| Rectovaginal fistula | 2 | 0 | 2 |
| Bilateral hydronephrosis with urosepsis | 1 | 0 | 1 |
| Bowel obstruction | 1 | 0 | 1 |
| Unilateral hydronephrosis | 1 | 0 | 1 |
| Ureteric obstruction | 1 | 0 | 1 |
| Hydronephrosis | 1 | 0 | 1 |
Table 3.
Classification of complications using the Clavien-Dindo system based on management strategies reported in the literature
| Grades (Contracted form) | Definition | Complications |
|---|---|---|
| Grade I | Deviation from the standard course of therapy. Allowed therapeutic regimens including drugs: (antiemetics, antipyretics, analgesics, diuretics, electrolytes) and physiotherapy. | Vaginal Discharge Ulceration Pain Bleeding Constipation Material Allergy Inability to self-replace or insert |
| Grade II | Requiring pharmacological treatment (drugs other than allowed for grade I complications), blood transfusions, total parenteral nutrition. | Vaginal discharge Erosion Vaginitis Ulceration Acute pyelonephritis Vesicovaginal fistula Rectovaginal fistula Ureteric obstruction |
| Grade III | Surgical, endoscopic or radiological interventions | Retained pessary requiring surgical removal Decubitus ulceration of the uterus Hydronephrosis – unilateral and bilateral Bowel obstruction Vaginal fibrosis |
| Grade IV | Life-threatening complication. Single or multi-organ dysfunction. | Vaginal cancer Cervical cancer Small bowel incarceration |
| Grade V | Death of a patient | Incarceration Enterovesical Fistula Obstructive uropathy Urosepsis |
In the case where multiple instances of a single complication was reported, the complication may appear in more than 1 grade based on how the complication was managed as reported in the literature.
Discussion
We systematically reviewed the complications of pessary use to treat POP. The frequency of complications varied widely between individual reports and between case series and case reports. Vaginal discharge, bleeding, and odor were frequently reported; however in rare instances, dangerous complications included death, particularly if the pessary was neglected.20 We have documented that all 5 Clavien-Dindo grades of complication occurred as a consequence of pessary use. The Clavien-Dindo approach is based on the type of therapy used to correct a specific complication, and is a form of classification used increasingly in surgical research to provide an objective and reproducible ranking for the reporting of complication severity. Hence, extrapolation to pessary use was considered justified, because, like surgery, pessaries offer a physical treatment which makes this type of classification more suitable than those used for pharmacologic treatments.
Despite the frequency of pessary use, complication reports predominantly came from case reports rather than case series.32 Some authors described pessaries as “outdated” and “risky;”33,34 there was even reference to the “dangerous pessary.”7 We felt it was not appropriate to state the overall frequency of complications related to pessaries from the reviewed literature. As the denominator is either small or unknown in most studies, we were cautious in our data interpretation. Others have reported that complications affect <10% of patients.35,36 Overall, very few reports defined pessary complications by type, shape, material, or size and objective classification of severity was lacking. This information is important to ensure patients are properly informed and to ensure proper patient consent in patients undertaking long-term pessary use and in their follow-up care.
It is important to discuss the following points with patients. A superficial vaginal mucosal erosion is the most frequently reported complication of a pessary,33,34,37–41 presenting as foul odor, purulent discharge, irregular blood stained discharge, and increased vaginal fluid. Localized pressure effects can result in ulceration and abrasions of the vaginal mucosa,42,43 and in rare cases reduced local blood flow secondary to chronic pressure has caused decubitus ulceration of the uterus.44 Reported risk factors for erosion include long-term uninterrupted use or placement of a pessary that was too large.31 Recommendations associated with this literature stress the need for proper sizing and performance of periodic examination.28,43
Vaginal flora are affected by pessary use. Many patients have a physiologic watery discharge; this finding is not considered an infectious process unless accompanied by other symptoms (e.g., itching, burning, or foul odor).43 Vaginal discharge and infection may affect as many as one-third of users;45 bleeding, pain, and constipation were also often reported.16,46 These issues have led to changes in pessary shape design.4,47
Serious complications include fistulae. Unlike minor complications which occur across all design types and materials, fistula frequency and location vary depending on pessary shape and material. Vesicovaginal fistulas (VVFs), although uncommon, are among the most serious complications of neglected pessaries.48 The reports identify Gellhorn and shelf designs most often;12 rectovaginal fistula and VVFs appear more common with rubber or PVC pessaries when compared with polythene pessaries.35 Fistula formation may also be associated with fecal impaction, hydronephrosis, and urosepsis,32 however, these complications were generally reported in the setting of neglect.22,23 Although serious complications caused by neglected pessaries are rare,49 in case reports describing VVFs, bowel fistulae, and incarcerated pessaries, 91% were correlated to neglected pessaries,12 and patients with dementia and nursing home residents could be at higher risk.39
Several reports implicated pessaries as a causal mechanism for both vaginal and cervical cancer.25 Chronic inflammation in association with viral infections has been suggested to predispose patients to such cancers as the tumours appeared at the site of pessary placement.50 It has been proposed that wearing a vaginal ring or cup-and-stem pessary for a long time may cause cancer of the vagina, ulcerative vaginitis, or fistulae. Primary cancer of the vagina was reported in 6 women among a group of 13 with major pelvic complications correlated to long-term pessary use,38 and in a women who developed vaginal and cervical cancer after 18 years of pessary use.50 Other mechanisms proposed included the generation of metaplastic and subsequent dysplastic change of the squamous mucosa,51 and the potential for personal cleanliness to play a role in carcinogenesis.52 Although, primary vaginal cancers are uncommon (1%–2% of gynecological malignancies51) Jain and colleagues reported that two vaginal cancers occurred in users of shelf pessaries among 9 cases of vaginal carcinoma reported between 2003 and 2005.52
Death has resulted from pessary use. An 82-year-old woman with a ring pessary developed vaginal bleeding; biopsies showed extensive surface ulceration, necrosis, and suppurative inflammation, and she died from acute pyelonephritis with hydronephrosis.20 A 77-year-old using a shelf pessary for 18 years reported vaginal bleeding and a foul-smelling discharge; examination revealed a vesicovaginal and a rectovaginal fistula, and she also died from acute pyelonephritis and hydronephrosis.38 Also, an 88-year-old patient died following erosion of a pessary into the upper rectum.53
The literature reviewed contained sparse information regarding the materials used in pessaries causing complications. This is an omission as pessaries are manufactured from an assortment of materials, including fruit, metal, porcelain, rubber, and acrylic,54 with each material having certain advantages and disadvantages. Most are made of medical grade silicone covering components of surgical steel;55 some pessaries are radiolucent with elements of silicone, rubber, acrylic, latex, or plastic.51 Medical-grade silicone pessaries are long-lasting, biologically inactive, do not cause allergy, and are not carcinogenic. Patients find them easy to wash and disinfect, using autoclave, boiling water, or a cold sterilization product.47,56,57 Pessaries rarely cause an allergic reaction. They may change colour with use and their material rarely fails or breaks, which would necessitate replacement.58
No single pessary design was complication free. Historically, a large number of physical shapes exist; the American Medical Association had identified 123 types of pessaries by 1867.55 Pessary shapes can be classified as supportive or space-occupying, with or without mechanisms to reduce urinary incontinence. Supportive pessaries consist of ring and lever designs, including the Smith, Hodge, Risser, and Gehrung. Space-occupying pessaries for advanced prolapse include Gellhorn, doughnut, and cube designs. Ring pessaries are generally easy to displace and Gellhorn/shelf pessaries can be more difficult to remove, resulting in pain and bleeding.57 Sometimes anesthesia is required.59
Our review has its limitations. It is limited to English literature. The overall frequency of individual complications of pessary use is unclear as the literature consists principally of case reports rather than prospective randomized studies. Although literature from over 50 years was reviewed, the number of patients studied is not large; hence the frequency of complications from pessary use may be underreported.
Conclusions
There are few detailed reports of complications of pessary use relative to the estimated frequency of pessary use worldwide. High-grade complications appear related to longevity of pessary use and lack of appropriate maintenance care. The incidence of complications in general also mandates follow-up of all women using pessaries in the long-term. Prospective studies documenting pessary complications by shape, material, and size, and objective classification of severity are required to further the scientific literature related to pessary use. Death, although rare, is a reported compilation and should be included in the informed consent of patients undertaking long-term pessary use.
Footnotes
Competing interests: The authors declare no competing financial or personal interests.
This paper has been peer-reviewed.
References
- 1.Mouritsen L. Classification and evaluation of prolapse. Best Pract Res Clin Obstet Gynaecol. 2005;19:895–911. doi: 10.1016/j.bpobgyn.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Brubaker L, Bump R, Jacquetin B, et al. Pelvic organ prolapse. In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence. 2nd ed. Plymouth: Health Publication Ltd; 2002. pp. 243–66. 2nd International Consultation on Incontinence, July 1–9, 2001; Paris, France. [Google Scholar]
- 3.Loret de Mola JR, Carpenter SE. Management of genital prolapse in neonates and young women. Obstet Gynecol Surv. 1996;51:253–60. doi: 10.1097/00006254-199604000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Bash KL. Review of vaginal pessaries. Obstet Gynecol Surv. 2000;55:455–60. doi: 10.1097/00006254-200007000-00025. [DOI] [PubMed] [Google Scholar]
- 5.Tegerstedt G, Maehle-Schmidt M. Prevalence of symptomatic pelvic organ prolapse in a Swedish population. Int Urogynecol J. 2005;16:497–503. doi: 10.1007/s00192-005-1326-1. [DOI] [PubMed] [Google Scholar]
- 6.Thys SD, Roovers JP, Geomini PM, et al. Do patients prefer a pessary or surgery as primary treatment for pelvic organ prolapse. Gynecol Obstet Invest. 2012;74:6–12. doi: 10.1159/000336634. [DOI] [PubMed] [Google Scholar]
- 7.Oliver R, Thakar R, Sultan AH. The history and usage of the vaginal pessary: A review. Eur J Obstet Gynecol Reprod Biol. 2011;156:125–30. doi: 10.1016/j.ejogrb.2010.12.039. [DOI] [PubMed] [Google Scholar]
- 8.Raja AM, Seema SR. Mechanical devices in pelvic organ prolapse. Int J Med Res Health Sci. 2013;2:643–7. doi: 10.5958/j.2319-5886.2.3.046. [DOI] [Google Scholar]
- 9.Pott-Grinstein E, Newcomer JR. Gynecologists’ patterns of prescribing pessaries. J Reprod Med. 2001;46:205–8. [PubMed] [Google Scholar]
- 10.Cundiff GW, Weidner AC, Visco AG, et al. A survey of pessary use by members of the American Urogynecologic Society. Obstet Gynecol. 2000;95:931–5. doi: 10.1016/S0029-7844(00)00788-2. [DOI] [PubMed] [Google Scholar]
- 11.Pushplata S, Devyani M, Pyari JS, et al. Bizarre foreign objects in the genital tract—our experience and review of literature. Open J Obstet Gynecol. 2014;4:427–31. doi: 10.4236/ojog.2014.47063. [DOI] [Google Scholar]
- 12.Arias BE, Ridgeway B, Barber MD. Complications of neglected vaginal pessaries: Case presentation and literature review. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1173–8. doi: 10.1007/s00192-008-0574-2. [DOI] [PubMed] [Google Scholar]
- 13.Adams E, Thomson A, Maher C, et al. Mechanical devices for pelvic organ prolapse in women. Cochrane Database Syst Rev. 2004:CD004010. doi: 10.1002/14651858.cd004010.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Farrell SA. Pessaries in clinical practice. Springer; 2007. Selection of a patient for pessary care; pp. 25–31. [Google Scholar]
- 15.Friedman S, Sandhu KS, Wang C, et al. Factors influencing long-term pessary use. Int Urogynecol J. 2010;21:673–8. doi: 10.1007/s00192-009-1080-x. [DOI] [PubMed] [Google Scholar]
- 16.Lamers BH, Broekman BM, Milani AL. Pessary treatment for pelvic organ prolapse and health-related quality of life: A review. Int Urogynecol J. 2011;22:637–44. doi: 10.1007/s00192-011-1390-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mutone MF, Terry C, Hale DS, et al. Factors which influence the short-term success of pessary management of pelvic organ prolapse. Am J Obstet Gynecol. 2005;193:89–94. doi: 10.1016/j.ajog.2004.12.012. [DOI] [PubMed] [Google Scholar]
- 18.Bugge C, Adams EJ, Gopinath D, et al. Pessaries (mechanical devices) for pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013:CD004010. doi: 10.1002/14651858.CD004010.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–9. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Penrose KJ, Yin JM, Tsokos N. Delayed vesicovaginal fistula after ring pessary usage. Int Urogynecol J. 2014;25:291–3. doi: 10.1007/s00192-013-2143-6. [DOI] [PubMed] [Google Scholar]
- 21.Manchana T. Ring pessary for all pelvic organ prolapse. Arch Gynecol Obstet. 2011;284:391–5. doi: 10.1007/s00404-010-1675-y. [DOI] [PubMed] [Google Scholar]
- 22.Grody MH, Nyirjesy P, Chatwani A. Intravesical foreign body and vesicovaginal fistula: A rare complication of a neglected pessary. Int Urogynecol J Pelvic Floor Dysfunct. 1999;10:407–8. doi: 10.1007/s001920050070. [DOI] [PubMed] [Google Scholar]
- 23.Ray A, Esen U, Nwabineli J. Iatrogenic vesico-vaginal fistula caused by shelf pessary. J Obstet Gynaecol. 2006;26:275–6. doi: 10.1080/01443610600559826. [DOI] [PubMed] [Google Scholar]
- 24.Emmert C. Neglected porcelain pessary causing postmenopausal bleeding and vesicovaginal fistula. J Obstet Gynaecol. 2007;27:867–8. doi: 10.1080/01443610701788456. [DOI] [PubMed] [Google Scholar]
- 25.Ott R, Richter H, Behr J, et al. Small bowel prolapse and incarceration caused by a vaginal ring pessary. Br J Surg. 1993;80:1157. doi: 10.1002/bjs.1800800931. [DOI] [PubMed] [Google Scholar]
- 26.Dasgupta P, Booth CM. Uraemia due to ureteric obstruction of a solitary kidney by a vaginal ring pessary. Scand J Urol Nephrol. 1996;30:493–4. doi: 10.3109/00365599609182330. [DOI] [PubMed] [Google Scholar]
- 27.Cumming GP, Narayansingh GV, Parkin DE, et al. Vesicovaginal fistula occurring 48 hours after insertion or a ring pessary. J Obstet Gynaecol. 2000;20:637. doi: 10.1080/01443610020001549. [DOI] [PubMed] [Google Scholar]
- 28.Hay DP, Martin WL, Darné FJ. Potentially dangerous complication of an ineffective shelf pessary. J Obstet Gynaecol. 1999;19:669. doi: 10.1080/01443619964067. [DOI] [PubMed] [Google Scholar]
- 29.Mohammed M, Sidra L, Haldipur N, et al. Incarcerated appendices epiploicae through the posterior vaginal defect secondary to a ring pessary. J Obstet Gynaecol. 2008;28:252–4. doi: 10.1080/01443610801975870. [DOI] [PubMed] [Google Scholar]
- 30.Popli K, Ranka P, Mustafa FA. Massive vesico-vaginal fistula caused by a shelf pessary. J Obstet Gynaecol. 2007;27:635–6. doi: 10.1080/01443610701577370. [DOI] [PubMed] [Google Scholar]
- 31.Liang SJ, Chow PK, Chou SY, et al. Incarcerated vaginal pessary: A rare complication. Taiwan J Obstet Gynecol. 2004;43:149–50. doi: 10.1016/S1028-4559(09)60073-5. [DOI] [Google Scholar]
- 32.Jelovsek JE, Maher C, Barber MD. Pelvic organ prolapse. Lancet. 2007;369:1027–38. doi: 10.1016/S0140-6736(07)60462-0. [DOI] [PubMed] [Google Scholar]
- 33.Sivasuriya M. Cervical entrapment of a polythene vaginal ring pessary--a clinical curiosity. Aust N Z J Obstet Gynaecol. 1987;27:168–9. doi: 10.1111/j.1479-828X.1987.tb00975.x. [DOI] [PubMed] [Google Scholar]
- 34.Summers JL, Ford ML. The forgotten pessary: A medical oddity. Am J Obstet Gynecol. 1971;111:307–8. doi: 10.1016/0002-9378(71)90911-2. [DOI] [PubMed] [Google Scholar]
- 35.Nanda SS, Dash S, Behera A. Prolonged retention of ring pessary resulting in vaginal wall fibrosis: A case report. Sch J Med Case Rep. 2014;2:50–1. [Google Scholar]
- 36.Wu V, Farrell SA, Baskett TF, et al. A simplified protocol for pessary management. Obstet Gynecol. 1997;90:990–4. doi: 10.1016/S0029-7844(97)00481-X. [DOI] [PubMed] [Google Scholar]
- 37.Methfessel HD. Rare foreign body fistulas of the female bladder. Z Urol Nephrol. 1987;80:545–9. [PubMed] [Google Scholar]
- 38.Russell JK. The dangerous vaginal pessary. Br Med J. 1961;2:1595–7. doi: 10.1136/bmj.2.5267.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Poma PA. Management of incarcerated vaginal pessaries. J Am Geriatr Soc. 1981;29:325–7. doi: 10.1111/j.1532-5415.1981.tb01274.x. [DOI] [PubMed] [Google Scholar]
- 40.Grody MH, Nyirjesy P, Chatwani A. Intravesical foreign body and vesicovaginal fistula: A rare compication of a neglected pessary. Int Urogynecol J Pelvic Floor Dysfunct. 1999;10:407–8. doi: 10.1007/s001920050070. [DOI] [PubMed] [Google Scholar]
- 41.Goldstein I, Wise GJ, Tancer ML. A vesicovaginal fistula and intravesical foreign body. A rare case of the neglected pessary. Am J Obstet Gynecol. 1990;163:589–91. doi: 10.1016/0002-9378(90)91204-P. [DOI] [PubMed] [Google Scholar]
- 42.Roberge RJ, McCandlish MM, Dorfsman ML. Urosepsis associated with vaginal pessary use. Ann Emerg Med. 1999;33:581–3. doi: 10.1016/S0196-0644(99)70347-1. [DOI] [PubMed] [Google Scholar]
- 43.Davila GW. Vaginal prolapse: Management with nonsurgical techniques. Postgrad Med. 1996;99:171–6. 181, 184–5. [PubMed] [Google Scholar]
- 44.Levine JM, Shua-Haim J, Gross J. Decubitus on uterus: An unusual complication of procidentia. Resident Staff Physician. 1995;41:38–48. [Google Scholar]
- 45.Alnaif B, Drutz HP. Bacterial vaginosis increases in pessary users. Int Urogynecol J. 2000;11:219–23. doi: 10.1007/PL00004026. [DOI] [PubMed] [Google Scholar]
- 46.Sarma S, Ying T, Moore KH. Long-term vaginal ring pessary use: Discontinuation rates and adverse events. BJOG. 2009;116:1715–21. doi: 10.1111/j.1471-0528.2009.02380.x. [DOI] [PubMed] [Google Scholar]
- 47.Atnip S, O’Dell K. Vaginal support pessaries: Indications for use and fitting strategies. Urol Nurs. 2012;32:114–24. [PubMed] [Google Scholar]
- 48.Chow SH, LaSalle MD, Rosenberg GS. Urinary incontinence secondary to a vaginal pessary. Urology. 1997;49:458–9. doi: 10.1016/S0090-4295(96)00453-0. [DOI] [PubMed] [Google Scholar]
- 49.Hanavadi S, Durham-Hall A, Oke T, et al. Forgotten vaginal pessary eroding into rectum. Ann R Coll Surg Engl. 2004;86:W18–9. doi: 10.1308/147870804182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schraub S, Sun XS, Maingon P, et al. Cervical and vaginal cancer associated with pessary use. Cancer. 1992;69:2505–9. doi: 10.1002/1097-0142(19920515)69:10<2505::AIDCNCR2820691020>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 51.Merino MJ. Vaginal cancer: The role of infectious and environmental factors. Am J Obstet Gynecol. 1991;165:1255–62. doi: 10.1016/S0002-9378(12)90738-3. [DOI] [PubMed] [Google Scholar]
- 52.Jain A, Majoko F, Freites O. How innocent is the vaginal pessary? Two cases of vaginal cancer associated with pessary use. J Obstet Gynaecol. 2006;26:829–30. doi: 10.1080/01443610600994825. [DOI] [PubMed] [Google Scholar]
- 53.Kankam OK, Geraghty R. An erosive passery. J R Soc Med. 2002;95:507. doi: 10.1258/jrsm.95.10.507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shah SM, Sultan AH, Thakar R. The history and evolution of pessaries for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:170–5. doi: 10.1007/s00192-005-1313-6. [DOI] [PubMed] [Google Scholar]
- 55.Zeitlin MP, Lebherz TB. Pessaries in the geriatric patient. J Am Geriatr Soc. 1992;40:635–9. doi: 10.1111/j.1532-5415.1992.tb02118.x. [DOI] [PubMed] [Google Scholar]
- 56.Magali R, Schulz JA, Harvey MA. Technical update on pessary use. J Obstet Gynaecol Can. 2013;35:664–74. doi: 10.1016/S1701-2163(15)30888-4. [DOI] [PubMed] [Google Scholar]
- 57.Jones KA, Harmanli O. Pessary use in pelvic organ prolapse and urinary incontinence. Rev Obstet Gynecol. 2010;3:3–9. [PMC free article] [PubMed] [Google Scholar]
- 58.Schulz JA, Kwon E. Pelvic organ prolapse pessary treatment. In: Baessler K, Schüssler B, Burgio KL, Moore K, Stanton SL, editors. Pelvic floor re-education. London: Springer; 2008. pp. 271–7. [DOI] [Google Scholar]
- 59.Khaja A, Freeman RM. How often should shelf/Gellhorn pessaries be changed? A survey of IUGA urogynaecologists. Int Urogynecol J. 2014;25:941–6. doi: 10.1007/s00192-014-2329-6. [DOI] [PubMed] [Google Scholar]
- 60.Wheeler LD, Lazarus R, Torkington J, et al. Lesson of the week: Perils of pessaries. Age Ageing. 2004;33:510–1. doi: 10.1093/ageing/afh170. [DOI] [PubMed] [Google Scholar]
- 61.Martin C, Hong L, Siddighi S. What is hiding behind the pessary? Int Urogynecol J. 2013;24:873–5. doi: 10.1007/s00192-012-1864-2. [DOI] [PubMed] [Google Scholar]
- 62.Kaaki B, Mahajan ST. Vesicovaginal fistula resulting from a well-cared-for pessary. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:971–3. doi: 10.1007/s00192-006-0275-7. [DOI] [PubMed] [Google Scholar]
- 63.Uprety DK, Regmi MC, Budhathoki B, et al. Metallic vaginal ring pessary: A rare entity. Kathmandu Univ Med J. 2008;6:508–10. doi: 10.3126/kumj.v6i4.1745. [DOI] [PubMed] [Google Scholar]
- 64.Esin S, Harmanli O. Large vesicovaginal fistula in women with pelvic organ prolapse: The role of colpocleisis revisited. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1711–3. doi: 10.1007/s00192-008-0636-5. [DOI] [PubMed] [Google Scholar]
- 65.Pankaj S, Choudhary V, Singh RK, et al. Forgotten vaginal pessary retrieved after 35 and 24 years of insertation two case reports. J Evol Med Dent Sci. 2013;2:7312–6. doi: 10.14260/jemds/1300. [DOI] [Google Scholar]
- 66.Meinhardt W, Schuitemaker NW, Smeets MJ, et al. Bilateral hydronephrosis with urosepsis due to neglected pessary. Case report. Scand J Urol Nephrol. 1993;27:419–20. doi: 10.3109/00365599309180458. [DOI] [PubMed] [Google Scholar]
- 67.Duncan LE, Foltzer M, O’Hearn M. Unilateral hydronephrosis, pyelonephritis, and bacteremia caused by a neglected vaginal ring pessary. J Am Geriatr Soc. 1997;45:1413–4. doi: 10.1111/j.1532-5415.1997.tb02952.x. [DOI] [PubMed] [Google Scholar]
- 68.Fernando RJ, Sultan AH, Thakar R, et al. Management of the neglected vaginal ring pessary. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:117–9. doi: 10.1007/s00192-006-0089-7. [DOI] [PubMed] [Google Scholar]
- 69.Rogo-Gupta L, Le NB, Raz S. Foreign body in the bladder 11 years after intravaginal pessary. Int Urogynecol J. 2012;23:1311–3. doi: 10.1007/s00192-012-1722-2. [DOI] [PubMed] [Google Scholar]
- 70.Handa VL, Jones M. Do pessaries prevent the progression of pelvic organ prolapse? Int Urogynecol J. 2002;13:349–52. doi: 10.1007/s001920200078. [DOI] [PubMed] [Google Scholar]
- 71.Fernando RJ, Thakar R, Sultan AH, et al. Effect of vaginal pessaries on symptoms associated with pelvic organ prolapse. Obstet Gynecol. 2006;108:93–9. doi: 10.1097/01.AOG.0000222903.38684.cc. [DOI] [PubMed] [Google Scholar]
- 72.Alperin M, Khan A, Dubina E, et al. Patterns of pessary care and outcomes for medicare beneficiaries with pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2013;19:142–7. doi: 10.1097/SPV.0b013e31827e857c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Potter C. Complications following the use of the gold spring pessary. Am J Surg. 1930;10:143–8. doi: 10.1016/S0002-9610(30)90174-2. [DOI] [Google Scholar]
- 74.Hanson LA, Schulz JA, Flood CG, et al. Vaginal pessaries in managing women with pelvic organ prolapse and urinary incontinence: Patient characteristics and factors contributing to success. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:155–9. doi: 10.1007/s00192-005-1362-x. [DOI] [PubMed] [Google Scholar]
- 75.Bai SW, Yoon BS, Kwon JY, et al. Survey of the characteristics and satisfaction degree of the patients using a pessary. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:182–6. doi: 10.1007/s00192-004-1226-9. discussion 186. [DOI] [PubMed] [Google Scholar]
- 76.Clemons JL, Aquilar VC, Sokol ER, et al. Patient characteristics that are associated with continued pessary use versus surgery after 1 year. Am J Obstet Gynecol. 2004;191:159–64. doi: 10.1016/j.ajog.2004.04.048. [DOI] [PubMed] [Google Scholar]
- 77.Clemons JL, Aquilar VC, Tillinghast TA, et al. Patient satisfaction and changes in prolapse and urinary symptoms in women who were fitted successfully with a pessary for pelvic organ prolapse. Am J Obstet Gynecol. 2004;190:1025–9. doi: 10.1016/j.ajog.2003.10.711. [DOI] [PubMed] [Google Scholar]
- 78.Abdelmagied A, Karoshi M, Yoong W. Egg on my face: An unusual way of reducing prolapse. J Obstet Gynaecol. 2005;25:222–3. doi: 10.1080/01443610500050926. [DOI] [PubMed] [Google Scholar]
- 79.Roberge RJ, Keller C, Garfinkel M. Vaginal pessary-induced mechanical bowel obstruction. J Emerg Med. 2001;20:367–70. doi: 10.1016/S0736-4679(01)00313-4. [DOI] [PubMed] [Google Scholar]
- 80.Clemons JL, Aquilar VC, Tillinghast TA, et al. Risk factors associated with an unsuccessful pessary fitting trial in women with pelvic organ prolapse. Am J Obstet Gynecol. 2004;190:345–50. doi: 10.1016/j.ajog.2003.08.034. [DOI] [PubMed] [Google Scholar]


