Abstract
Background:
The impact strength of denture base resin is of great concern and many approaches have been made to strengthen acrylic resin dentures. The objective of this study was to compare the impact strength of the denture base resin with and without reinforcement and to evaluate the impact strength of denture base resin when reinforced with stainless steel mesh, glass fiber, and polyethylene fibers in the woven form.
Materials and Methods:
The specimens (maxillary denture bases) were fabricated using a standard polyvinylsiloxane mold with conventional heat cured polymethyl methacrylate resin. The specimens were divided into four groups (n = 10). Group I specimens or control group were not reinforced. Group II specimens were reinforced with stainless steel mesh and Group III and Group IV specimens were reinforced with three percent by weight of glass fibers and polyethylene fibers in weave form respectively. All the specimens were immersed in water for 1-week before testing. The impact strength was measured with falling weight impact testing machine. One-way analysis of variance and Tukey’s post-hoc test were used for statistical analysis.
Results:
Highest impact strength values were exhibited by the specimens reinforced with polyethylene fibers followed by glass fibers, stainless steel mesh, and control group.
Conclusions:
Reinforcement of maxillary complete dentures showed a significant increase in impact strength when compared to unreinforced dentures. Polyethylene fibers exhibit better impact strength followed by glass fibers and stainless steel mesh. By using pre-impregnated glass and polyethylene fibers in woven form (prepregs) the impact strength of the denture bases can be increased effectively.
Keywords: Acrylic resin, glass fibers, impact strength, polyethylene fibers, polymethyl methacrylate, reinforcement, stainless steel mesh
Introduction
Acrylic resins (polymethyl methacrylate [PMMA]) are the most commonly used denture base materials since early 1940’s. The properties such as excellent appearance, ease in processing and ease in repair contribute to its success as a denture base material. However, the acrylic resins have the disadvantages like poor strength characteristics which include low impact strength and low fatigue resistance.1,2 The fatigue failure occurs when the denture base deforms repeatedly through occlusal forces and impact failure occurs when the dentures are accidentally dropped on a hard surface. Hence, the dentures tend to break during usage in the due course of time.2
In order to improve the strength of the material, various methods have been proposed like:
Using Polycarbonates and polyamides as substitutes for PMMA.
Chemical modification of PMMA by the addition of rubber in the form of butadiene styrene.
The incorporation of fibers or metal inserts into the denture bases.1-4
Polycarbonates and polyamides although improve the strength are expensive and technique sensitive. Modification of the chemical structure by the addition of cross-linking agents like polyethylene glycol or by copolymerization with rubber in the form of Butadiene styrene have been tried, but this did not show significant enhancement on the strength properties.2,4 Different types of fibers like carbon, Kevlar, aramid, polyethylene, and glass fibers have been used for reinforcement.
Carbon and Kevlar fibers are not in use because of their undesirable color and toxicity.4-7 Glass fibers and Polyethylene fibers are biocompatible and esthetically satisfactory, so are being used for reinforcement of dentures. Metal inserts in the form of wires, mesh, and plates are being used to reinforce acrylic resins since long.1-4
The present study is carried out by reinforcing the denture bases with glass fibers, polyethylene fibers, and stainless steel mesh and the impact strength is evaluated using falling weight impact testing machine.2
Objectives
To compare the impact strength of the conventional heat cure denture base resin with and without reinforcement.
To evaluate the impact strength of the conventional heat cure denture base resin when reinforced with stainless steel mesh, glass, and polyethylene fibers in weave form.
Materials and Methods
This study was conducted to investigate the effect of fibers and metal reinforcement in the maxillary complete dentures on the impact strength.
The materials and methods used in this study have been described in the following order.
Materials
Armamentarium and equipments
-
Methodology
- Fabrication of complete denture
- Preparation of putty mold
- Obtaining wax models
- Flasking
-
Packing and processing of specimens
- Control group
- Dentures reinforced with metal mesh
- Dentures reinforced with glass fibers
- Dentures reinforced with polyethylene fibers
- Evaluation of impact strength
Materials (Figure 1)
Figure 1.

Falling weight impact testing machine.
Conventional heat cure polymethyl methacrylate denture base resin in powder and liquid form (DPI limited, Mumbai)
Self-cure polymethyl methacrylate denture base resin in powder and liquid form (DPI limited, Mumbai)
Polyethylene fibers (Reliance India ltd, Gujarat, India)
Glass fibers (Reliance India ltd, Gujarat, India)
Stainless steel mesh (Dentaurum, Germany)
Dental stone (type III) (Asian chemicals, Rajkot, India)
Dental plaster (type II) (Asian chemicals, Rajkot, India)
Modeling wax (DPI limited, Mumbai, India)
Acrylic teeth sets (Premadent M123, Mumbai, India)
-
Elastomeric impression materials
- Putty impression material (Aquasil ultra DENTSPLY)
- Light body impression material (Aquasil, Ultra USA)
Putty impression material (Aquasil ultra DENTSPLY)
Light body impression material (Aquasil, Ultra USA)
Alginate separating media (cold-mold seal DPI, India)
Pumice
Cellophane separating sheets (DPI, India)
Petroleum Jelly(Jyothi laboratories, Bengalooru, India)
Armamentarium and equipment
Edentulous rubber mold
Light body dispensing gun (Dentsply, USA)
Dental flasks and clamp (Jabbar and Kavo, India)
Acrylizer (Confident, India)
Vernier caliper
Mechanical vibrator (Confident, India)
Camel Hair brush
Bowl and spatula
Micro motor and handpiece (Kavo, Germany)
Steel carbide burs
Silicon carbide sand papers (100, 120, 150 grit)
Falling weight impact testing machine (Figure 1)
Blowtorch
Hydraulic press (Kavo, Germany)
Sandpaper mandrel
Wax bath
Lecron’s carver
Wax knife
Wax spatula
Metal scale
Electronic weighing machine
Methodology
The specimens (maxillary complete dentures) were fabricated using heat cure denture base resin (PMMA). For standardization of specimens, a maxillary denture was fabricated with which an elastomeric mold was fabricated. The other specimens were fabricated using the elastomeric mold. Unreinforced dentures were used as control group. Dentures reinforced with glass fibers (weave form), polyethylene fibers (weave form) and stainless steel mesh were fabricated according to the manufacturer’s instructions, impact strength was calcualted and the results were compared with control group. Total 40 maxillary dentures were fabricated 10 for each group.
Fabrication of complete denture (Figure 2)
Figure 2.

Standardization by fabrication of a denture.
Standard edentulous rubber mold was used to obtain stone casts from which denture base of 2 mm thickness was fabricated with self-cure denture base resin.9 Wax occlusal rims of adequate dimensions were prepared with modeling wax. Teeth arrangement and carving were done. Flasking and dewaxing were carried out and the mold was packed with conventional heat cure denture base resin (DPI, India). Then the flask was immersed in water in an acrylizer at room temperature and processed according to the manufacturer’s instructions. After curing, denture was deflasked, trimmed, finished, and polished.
Preparation of putty mold (Figure 3)
Figure 3.
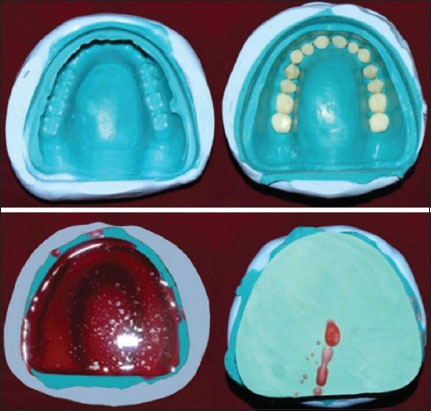
Mold fabrication using putty material.
The finished maxillary denture was adapted with putty elastomeric material mix, after it was set the denture was separated to obtain a putty mold. The inner surface of the putty mold was scrapped and light body polyvinylsiloxane material was dispensed into the putty mold with light body dispensing gun and the denture along with the cast was placed into the putty mold. After the light body material was set the denture along with the cast was removed to obtain the final mold.
Obtaining wax models (Figure 3)
The teeth set of similar mold (Premadent M1, 23) was used. Each tooth was placed in its space in the putty mold and then molten modeling wax was poured. The stone cast in which a hole was made to allow for air escape was placed into the mold. The mold was allowed to cool for 1-h after which the duplicated wax denture was retrieved. Forty such dentures were obtained by this method.
Flasking (Figure 4)
Figure 4.

Control group without reinforcement.
The wax models were flasked using Jabbar flasks, Kavo clamp, dental stone, and dental plaster by the conventional method. Then dewaxing was carried and they were allowed to cool.
Packing
Control group (Group I) (Figure 4): Heat cure acrylic denture base material was mixed according to the manufacturer’s instructions. Separating media was applied to the 2 halves of the flasks obtained. The material was packed in the dough stage. After trial packing, the cellophane paper was removed. Then final closure was done by applying pressure at 10,000 N in a hydraulic press. Bench curing and acrylization was done as for the standard specimen. The specimens were finished and polished and ten such dentures were obtained.
Dentures reinforced with stainless steel mesh (Group II) (Figure 5): All the steps were followed as for the control group until the application of separating media. Then the equal amount of heat cure material mix in dough stage was placed in both halves of the flask and cellophane paper was placed in between and trial closure was done. After trial closure, the cellophane paper was removed and the properly adapted stainless steel metal mesh was placed between the 2 halves of the flasks, covering the entire palatal surface till the crest of the ridge. Then the flasks were pressed in the hydraulic press, at 10,000 N. Then they were bench cured, and processed as for the Group I. Dentures recovered were finished and polished.
Figure 5.

Reinforcement using stainless steel mesh.
Dentures reinforced with glass fibers (Figure 6): All the steps were followed as for the control group until trial closure. After trial closure, three layers of glass fiber weave (3% by weight) were wetted with monomer and 10 drops of heat cure monomer and some amount of polymer powder was sprinkled to obtain a prepreg.10 This prepreg was placed between the 2 halves of the flasks in the same manner as the metal mesh was placed. Flasks were pressed under the hydraulic press, bench cured and processed in an acrylizer as for Group I. Dentures were finished and polished.
Figure 6.
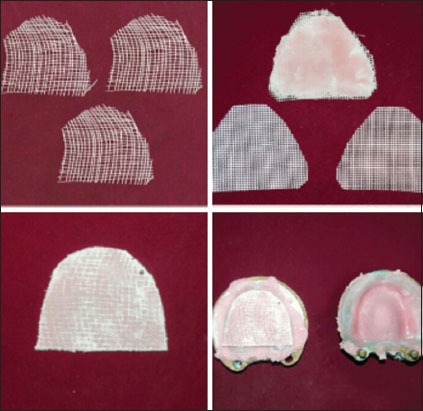
Reinforcement using glass fiber and polyethylene prepreg.
Dentures reinforced with polyethylene fibers (Figure 6): Similarly for these specimens all the steps were followed as for the glass fiber group until final closure. However, in this group the prepreg was prepared with two layers (3% by weight) of polyethylene fibers. After final closure, the dentures were bench cured acrylized, finished, and polished as for Group I.
Evaluation of the impact strength (Figure 1)
The specimens were grouped as follows:
Group I (Control group): Maxillary dentures without reinforcement (ten specimens)
Group II: Maxillary dentures reinforced with stainless steel mesh (ten specimens)
Group III: Maxillary dentures reinforced with glass fibers (ten specimens)
Group IV: Maxillary dentures reinforced with polyethylene fibers (ten specimens).
All the specimens were stored in water for 1-week before testing.2,11,12 The impact strength was evaluated using falling weight impact testing machine. It consisted of a 1.25 m long plastic tube and an impactor. The plastic tube had three windows to minimize the resistance between the tube and the impactor. The impactor was made out of hard wood and had a hemisphere end of radius 50 mm and a mass of 0.836 kg. The tube was mounted on a wooden platform. The testing apparatus was placed on a flat surface while testing. The denture was positioned on the wooden platform and the impactor was dropped at different heights through the plastic tube. First, the values were recorded for 0.30 m height. If the denture did not break at this height after 40 repetitions, then the height was increased to 0.50 m and testing was done until complete fracture (CF) occurred for all the specimens.
Two values were measured:
Crack initiation (CI) energy and
CF energy.
The impact strength was calculated using the formula:

Where E: Impact strength (impact energy, J)
m: weight of impactor (0.836 kg)
g: acceleration of gravity (9.8 m/s2)
h: height from which impactor was dropped: number of impacts
Results
The present study was conducted to compare the impact strength of the specimens (maxillary complete dentures) fabricated with conventional heat cure denture base resin which were reinforced with glass fibers and polyethylene fibers in weave form and stainless steel mesh with the unreinforced dentures. The specimens were grouped as follows:
Group I: Control group, which consisted of unreinforced maxillary dentures
Group II: Maxillary dentures reinforced with stainless steel mesh
Group III: Maxillary dentures reinforced with glass fibers in weave form
Group IV: Maxillary dentures reinforced with polyethylene fibers in weave form.
Ten specimens were made for each group. The strength of the specimens was measured with the falling weight impact testing machine. CI and CF were the two values determined for each group. The specimens were first tested at 0.30 m height for 40 attempts then the height was increased to 0.50 m. The weight of the impactor was 0.836 kg and was kept constant.
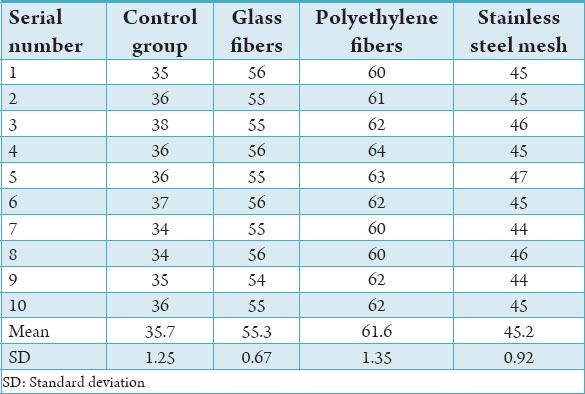
Tables 1 and 2 give the number of attempts at which the CI and CF occurred. The mean values for CI attempts for the Groups I, II, III, and IV were 30.4, 45.4, 55.9, and 34.6 and the standard deviations were 1.25, 1.26, 1.19, and 1.07, respectively. The mean for CF for the Groups I, II, III, and IV were 35.7, 55.3, 61.6 and 45.2 and the standard deviations were 1.25, 0.67, 1.35, and 0.92, respectively. The impact strength for the four groups of specimens was determined using the formula:
Table 1.
Crack initiation.
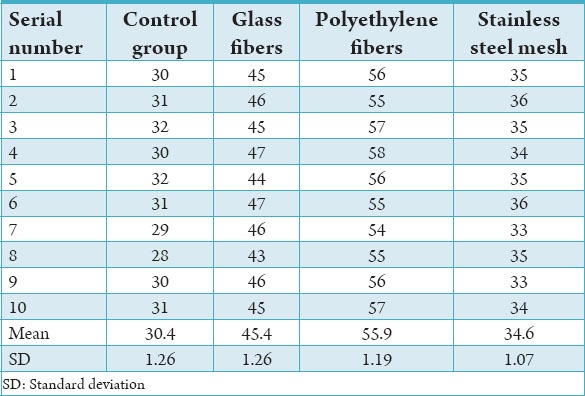
Table 2.
Complete fracture.

Tables 3 and 4 give the impact strength values for all the groups at CI and CF. The mean of the impact strength for the Groups I, II, III, and IV at CI was 74.72, 85.04, 185.98, and 228.99 and the standard deviations were 3.11, 2.64, 5.18, and 4.90, respectively. The mean of the impact strength for the Groups I, II, III, and IV at CF was 87.74, 185.16, 226.53, and 252.34 and the standard deviation were 3.07, 3.76, 2.76, and 5.53, respectively.
Table 3.
Impact strength at crack initiation.
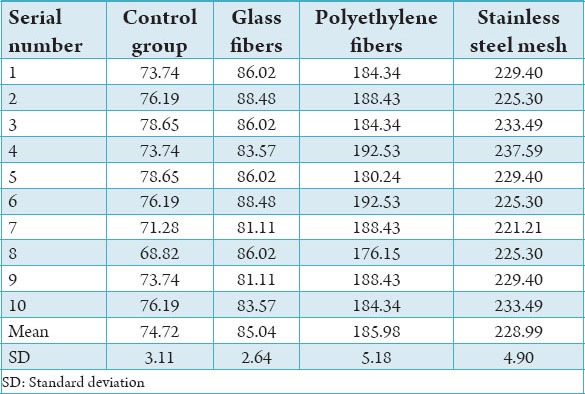
Table 4.
Impact strength at complete fracture.
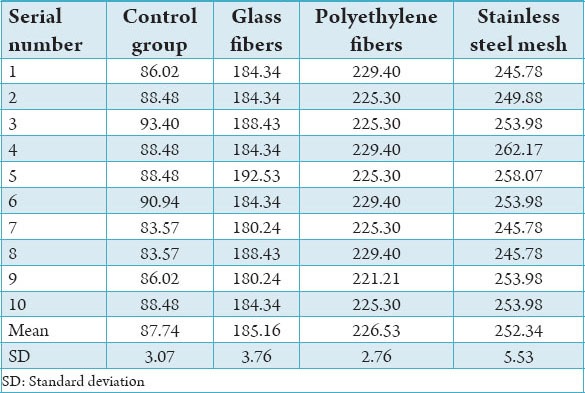
Table 5 shows the descriptive statistics of all the groups for CI and CF. Table 6 shows the comparison of the impact strength values for CI and CF with repeated measures ANOVA test for the Groups I, II, III, and IV and the test was highly significant with P < 0.001. Table 7 shows the pair-wise comparison of the impact strengths at CI and CF within the groups. The Tukey’s test shows that the test was statistical significant (P < 0.05).
Table 5.
Descriptive statistics.
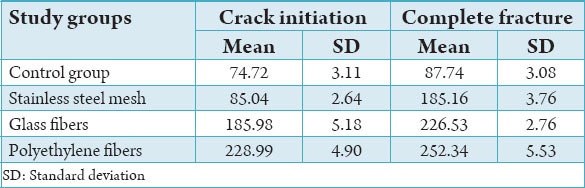
Table 6.
Repeated measures ANOVA for comparison of crack initiation and complete fracture strengths among the groups.
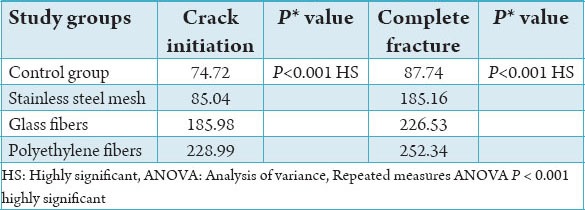
Table 7.
Tukey’s test for comparison of crack initiation and complete fracture within the groups.
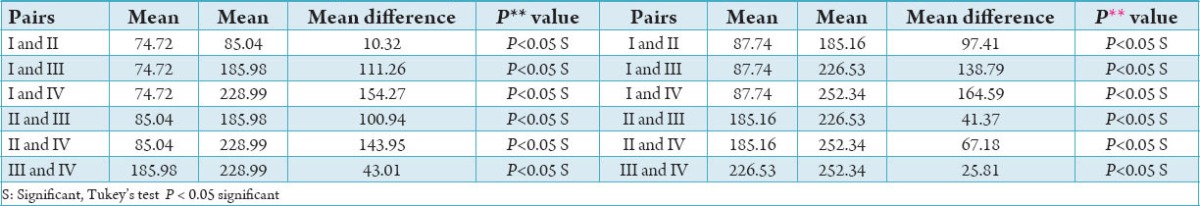
The Graphs 1 and 2 shows the impact strengths at CI and CF, respectively for the Groups I, II, III, and IV.
Graph 1.
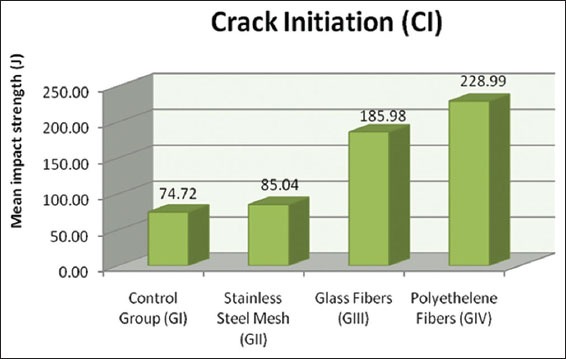
Repeated measures analysis of variance: P < 0.001 highly significant.
Graph 2.
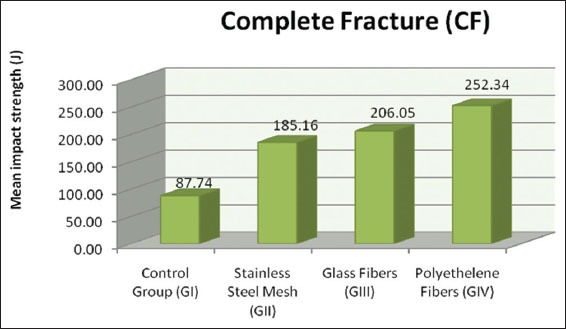
Repeated measures analysis of variance: Tukey’s test P < 0.05 significant.
Discussion
PMMA resin which is widely used in prosthetic dentistry for fabrication of denture bases has many advantages, but it has certain disadvantages like poor inherent strength characteristics which include low impact strength and low fatigue resistance.
Breakage of dentures may result from impact failure when the denture is accidentally dropped on a hard surface or by fatigue failure when the denture base deforms repeatedly through occlusal forces.2,9 The ratio of maxillary to mandibular denture fractures is about 2:1. The most common causes of fracture include poor fit and lack of balanced occlusion.13 The maxillary dentures fracture by a combination of fatigue and impact failure whereas about 80% of the mandibular dentures fracture due to impact failure.2 Maxillary dentures fracture due to various reasons which include:
When the prosthesis is opposed to a natural dentition in the lower jaw, particularly if the position or alignment of the teeth is such that it is difficult to achieve an even or balanced occlusion.
Other factors which influence the failure of the dentures during service are deep frenal notches, prominent torus palatines, and inaccurate fit of the dentures.6
When the dentures are accidentally dropped on a hard surface.2
The stress distribution within the dentures has been studied by many investigators by using various techniques and theoretic models. They suggested that the maxillary dentures are subjected to bending deformation, with tensile stresses occurring at the labial aspect and lingually to the incisors on the polished surfaces. The area lingual to the incisors i.e., the incisive papilla is the most heavily stressed and the incisal notch represents a point of weakness which might act as a stress raiser and contribute to midline fractures of maxillary dentures.3,13 The maximal biting force of patients with complete dentures can be up to 200 N in the molar region and up to 80 N in the incisor region but during normal mastication process, this biting force remains lower than normal.9
Detailed photoelastic stress analysis indicated that compressive stresses occur in the maxillary base adjacent to the supporting tissues with tensile stresses elsewhere. The compressive stresses occurred toward the tissue surface with greater values beneath the teeth and on the ridge than those toward the palate. The stress distribution will be affected by functional loading with the lowest stress occurring at the midline of the maxillary dentures. Stresses increase from the anterior to the posterior region over the ridge with maximum stresses occurring in the molar region in the centric occlusion.13
Midline fracture of a denture base is a flexural fatigue, resulting from cyclic deformation of the denture base during the function. Any factor that exacerbates deformation of the denture base or alters its stress distribution will predispose the denture to fracture. Fracture is a result of the initiation and propagation of a crack and this requires the presence of a stress raiser or a point of localized stress. Midline palatal fractures of acrylic dentures occur because the midline of the palate serves as a fulcrum and superior displacement of the dentures results in fracture into two halves of the denture.3
Therefore, many attempts have been made to enhance the strength properties of acrylic denture bases like:
Modification of chemical structure, by the addition of cross-linking agents such as polyethylene glycol di-methacrylate or by copolymerization with rubber has been tried, but there was no significant increase in the strength of the material.
Using polycarbonates and polyamides as substitutes for PMMA, since they are expensive and highly technique sensitive they are not used.
The incorporation of the fibers or the metal inserts into the denture bases.2-4
Various methods have been tried to reinforce the acrylic resin denture bases.2 Metal inserts have been used in the form of wires, meshes, and plates2,3,7,14 and the different fibers include carbon, aramid, glass, and polyethylene fibers.10,15,16 The carbon and aramid fibers because of their undesirable color and toxicity are not used.2,6 The glass and polyethylene fibers because of their stiffness, strength, biocompatibility, white translucent appearance, and negligible water absorption are used for reinforcement successfully.9,17 In the present study, stainless steel mesh, glass, and polyethylene fibers are used for reinforcement of the maxillary dentures.
The denture base can be reinforced in two ways, i.e., the entire denture base can be reinforced or reinforcement can be done at the weak region of the denture.16 Researchers have found that mastication and swallowing procedures occur by an increase or decrease of the curvature of the denture base at the midline accompanied by a small extension and compression of the flanges. Therefore, the entire denture base should be reinforced with the fibers oriented in the lateral direction and further improvement can be achieved by reinforcing with the parallel fibers in the horizontal plane.18 In this study, the reinforcement was done in the entire palatal surface till the crest of the ridge for the maxillary dentures.
The fiber reinforcement can be done either with individual fibers in continuous parallel and chopped forms and with woven mats.3,18 The woven reinforcement is very effective in arresting the crack propagation.19 For maximum reinforcement, the resin should penetrate the weave, ensuring no voids at fiber/resin interface. The consistency of heat-cure acrylic resin being a dough-type material may prevent the penetration of the resin into the weave. Hence, the fiber insert should be wetted with PMMA monomer or thin PMMA slurry prior to final closure to prepare a prepreg.2,6,10
Researchers have shown that for better strength, optimum percentage of fiber incorporation has to be done. Incorporation of about 3% by weight of fibers results in good impact strength.20,21 During service, dentures absorb water and saliva. Over the initial 3 months immersion a linear dimensional change of about 0.3% in the flange to flange dimensions may occur. This may affect the deformation under loading, while long-term water sorption will lower the fatigue resistance of the acrylic resin.13 The fibers are hydrophobic, hence higher fiber content is associated with lower water absorption.22 Water immersion generally has little effect on the mechanical properties and interface strength of dental resins reinforced with fibers.23,24 Studies have shown that 2-7% by weight of fiber content in denture bases will not affect the dimensional accuracy of the acrylic resin. In this study, 3% by weight of woven glass and polyethylene fibers in the form of prepregs were used for reinforcement and the specimens were stored in water for 1-week.
Many studies have been conducted to test the impact strength of acrylic resin reinforced with various kinds of fibers and metal inserts. All the tests used specimens of rectangular acrylic resin blocks and the tests were carried out with flexed beam impact methods such as Charpy type pendulum impact tester or Zwick pendulum impact tester2,20,22 but by using falling weight impact testing machine, the clinical conditions in service of a denture can be simulated.2 The present study was conducted by using the falling weight impact testing machine to evaluate the impact strength of the dentures for the following groups:
Group I Control group): Unreinforced dentures
Group II: Dentures reinforced with stainless steel mesh
Group III: Dentures reinforced with glass fibers in weave form
Group IV: Dentures reinforced with polyethylene fibers in weave form.
Two energies were determined for each group, CI and CF energies. Graphs 1 and 2 shows the CI and CF values for all the groups. The Group I shows the least CI (74.72 J) and CF (87.74 J) values compared to other three groups. The Group II specimens had better CI (85.04 J) and CF (185.16 J) values when compared to Group I but less than Group III and Group IV. Group III had better impact strength values at CI (185.98) and CF (206.05) when compared to Group I and Group II but less than Group IV. Group IV had highest impact strength values (CI = 228.99 J, CF = 252.34 J) among all the groups.
Group I showed least value because the dentures were not reinforced. Groups II, III, and IV showed high impact strength because of reinforcement with metal, glass, and polyethylene fibers in weave form respectively.
The dentures reinforced with stainless steel mesh in Group II exhibited less impact strength when compared to the Groups III and Group IV. This may be due to the use of pre-impregnated woven fibers or the prepregs. The pre-impregnated fiber systems or the prepregs provide interpenetrating polymer network bond with acrylic resin which is not achieved by using stainless steel mesh.2,25
Though prepreg technique was used for both Groups III and Group IV, i.e., glass and polyethylene fibers in weave form, Group IV exhibited better strength, this may be because, the polyethylene fibers are ductile and not brittle and they have high modulus of elasticity when compared to glass fibers and they undergo least deformation before fracture, which will contribute to their impact strength.1,5
Thus, to improve the impact strength of the maxillary denture bases reinforcement is a better option and good results can be obtained with easier techniques.
Conclusion
Reinforcement of maxillary complete dentures showed a significant increase in impact strength when compared to unreinforced dentures.
Polyethylene fibers exhibit better impact strength followed by glass fibers and stainless steel mesh. By using pre-impregnated glass and polyethylene fibers in woven form, (prepregs) the impact strength of the denture bases can be increased effectively.
Summary
Impact strength of denture base resins is of great concern, and many approaches have been used to strengthen acrylic resin dentures.
This in vitro study was done to compare the effect of reinforcement on the impact strength of conventional heat cure denture base resin by reinforcing with stainless steel mesh, glass, and polyethylene fibers in woven form.
Four groups of specimens (n = 10) were fabricated for impact strength test. Specimens for Group I (control) were made of heat cured PMMA. For Group II, the specimens (maxillary dentures) were reinforced with stainless steel mesh, for Group III and Group IV, the specimens were reinforced with 3% by weight of woven glass and polyethylene fibers in the prepreg form. All the specimens were stored in water for 1-week before testing.
The impact strength was measured with falling weight impact testing machine. For multiple group and pairwise comparison one-way ANOVA and Tukey’s post-hoc tests were done.
The reinforcement significantly increased the impact strength of the specimens. Highest impact strength values were exhibited by the specimens reinforced with polyethylene fibers followed by glass fibers, metal mesh, and the control specimens (P < 0.001).
Annexures
Statistical analysis
Descriptive data are presented as mean and standard deviation and were used for analysis. One-way analysis of variance was used for multiple group comparisons followed by post-hoc Tukey's Test for pairwise comparison.
Formulae:
Standard deviation 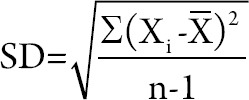
X = Set of values
X̄= Mean
n = Number of values
One-way ANOVA 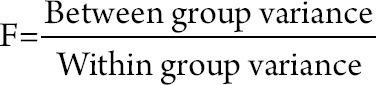
Tukey's post-hoc test,
Lowest Significance Difference (LSD) = 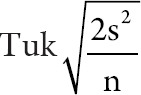
Where Tuk = table value
s2 = Mean square error
n= Number of samplesreinforced
Footnotes
Conflicts of Interest: None
Source of Support: Nil
References
- 1.Uzun G, Hersek N, Tinçer T. Effect of five woven fiber reinforcements on the impact and transverse strength of a denture base resin. J Prosthet Dent. 1999;81(5):616–20. doi: 10.1016/s0022-3913(99)70218-0. [DOI] [PubMed] [Google Scholar]
- 2.Kim SH, Watts DC. The effect of reinforcement with woven E-glass fibers on the impact strength of complete dentures fabricated with high-impact acrylic resin. J Prosthet Dent. 2004;91(3):274–80. doi: 10.1016/j.prosdent.2003.12.023. [DOI] [PubMed] [Google Scholar]
- 3.Kawano F, Miyamoto M, Tada N, Matsumoto N. Reinforcing effect of a Ni-Cr alloy plate on an acrylic resin denture base. Int J Prosthodont. 1991;4(4):327–31. [PubMed] [Google Scholar]
- 4.Jagger DC, Harrison A, Jandt KD. An investigation of self-reinforced poly (methyl methacrylate) denture base acrylic resin using scanning electron and atomic force microscopy. Int J Prosthodont. 2000;13(6):526–31. [PubMed] [Google Scholar]
- 5.Braden M, Davy KW, Parker S, Ladizesky NH, Ward IM. Denture base poly(methyl methacrylate) reinforced with ultra-thin modulus polyethylene fibers. Br Dent J. 1988;164(4):109–13. doi: 10.1038/sj.bdj.4806373. [DOI] [PubMed] [Google Scholar]
- 6.Clarke DA, Ladizesky NH, Chow TW. Acrylic resins reinforced with highly drawn linear polyethylene woven fibres 1. Construction of upper denture bases. Aust Dent J. 1992;37(5):394–9. doi: 10.1111/j.1834-7819.1992.tb00766.x. [DOI] [PubMed] [Google Scholar]
- 7.Diaz-Arnold AM, Vargas MA, Shaull KL, Laffoon JE, Qian F. Flexural and fatigue strengths of denture base resin. J Prosthet Dent. 2008;100(1):47–51. doi: 10.1016/S0022-3913(08)60136-5. [DOI] [PubMed] [Google Scholar]
- 8.Chow TW, Cheng YY, Ladizesky NH. Polyethylene fibers reinforced PMMA – Water sorption and dimensional changes during immersion. J Dent. 1993;21(6):367–72. doi: 10.1016/0300-5712(93)90014-h. [DOI] [PubMed] [Google Scholar]
- 9.Vallittu PK, Lessila VP, Lappalainel R. Transverse and fatigue strength of denture arylic glass fiber composite. Dent Mater. 1994;10(2):116–21. doi: 10.1016/0109-5641(94)90051-5. [DOI] [PubMed] [Google Scholar]
- 10.Bowman AJ, Manley TJ. The elimination of breakages in upper dentures by reinforcement with carbon fibers. Br Dent J. 1984;156(3):87–9. doi: 10.1038/sj.bdj.4805275. [DOI] [PubMed] [Google Scholar]
- 11.Aydin C, Yilmaz H, Caglar A. Effect of glass fiber reinforcement on the flexural strength on the diferrent denture base resins. Quintessence Int. 2002;33(6):457–63. [PubMed] [Google Scholar]
- 12.Zappini GL, Kammall A, Wochter W. Comparison of fracture tests of denture base materials. J Prosthet Dent. 2003;90(6):578–85. doi: 10.1016/j.prosdent.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Beyli MS, Von Fraunhofer JA. An analysis of causes of fracture of acrylic resin dentures. J Prosthet Dent. 1981;46(3):238–41. doi: 10.1016/0022-3913(81)90206-7. [DOI] [PubMed] [Google Scholar]
- 14.Vallitu PK, Lassila VP. Effect of metal strengtheners surface roughness on fracture resistance of acrylic denture base material. J Oral Rehabil. 1992;19(4):385–91. doi: 10.1111/j.1365-2842.1992.tb01580.x. [DOI] [PubMed] [Google Scholar]
- 15.Mullarky RH. Aramid fiber reinforcement of acrylic appliances. J Clin Orthod. 1985;91(9):655–8. [PubMed] [Google Scholar]
- 16.Ladizesky NH, Cheng YY, Chow TW, Ward IM. Acrylic resin reinforced with chopped high performance polyethylene fiber – Properties and denture construction. Dent Mater. 1993;9(2):128–35. doi: 10.1016/0109-5641(93)90089-9. [DOI] [PubMed] [Google Scholar]
- 17.Chow TW, Ladizesky NH, Clarke JA. Acrylic resins reinforced with woven highly drawn linear polyethylene fibers. Water sorption and clinical trials. Aust Dent. 1992;37(6):433–8. doi: 10.1111/j.1834-7819.1992.tb05897.x. [DOI] [PubMed] [Google Scholar]
- 18.Ladizesky NH, Chow TW. Reinforcement of complete denture bases with continuous high performance polyethylene fibers. J Prosthet Dent. 1992;68(6):934–9. doi: 10.1016/0022-3913(92)90554-n. [DOI] [PubMed] [Google Scholar]
- 19.Ladizesky NH, Chow TW, Pang MK, Ward IM. Acrylic resins reinforced with woven highly drawn linear polyethylene fibers. Mechanical properties and further aspects of denture construction. Aust Dent J. 1993;38(1):28–38. doi: 10.1111/j.1834-7819.1993.tb05448.x. [DOI] [PubMed] [Google Scholar]
- 20.Gutteridge DL. The effect of including ultrahigh modulous polyethylene fibers on the impact strength of acrylic resin. Br Dent J. 1988;164:177–80. doi: 10.1038/sj.bdj.4806395. [DOI] [PubMed] [Google Scholar]
- 21.Gutteridge DL. Reinforcement of PMMA with ultrahigh modulous polyethylene fibers. J Dent. 1992;20(1):50–4. doi: 10.1016/0300-5712(92)90012-2. [DOI] [PubMed] [Google Scholar]
- 22.Ladizesky NH, Chow TW, Clarke DA. Acrylic resins reinforced with highly drawn linear polyethylene fibers. Water absorption and clinical trials. Aust Dent J. 1992;37(6):433–8. doi: 10.1111/j.1834-7819.1992.tb05897.x. [DOI] [PubMed] [Google Scholar]
- 23.Ladizesky NH, Chow TW. The effect of interface adhesion, water immersion and anatomical notches on the mechanical properties of denture base resins reinforced with continuous highly drawn linear polyethylene fibers. Aust Dent J. 1992;37(4):277–89. doi: 10.1111/j.1834-7819.1992.tb04744.x. [DOI] [PubMed] [Google Scholar]
- 24.Miettinen VM, Vallittu PK. Water sorption and solubility of glass fiber reinforced PMMA resin. J. Prosthet Dent. 1996;76(5):531–4. doi: 10.1016/s0022-3913(97)70147-1. [DOI] [PubMed] [Google Scholar]
- 25.Vallittu PK. Flexural properties of acrylic resin polymers reinforced with unidirectional and woven fibers. J Prosthet Dent. 1999;81(5):318–26. doi: 10.1016/s0022-3913(99)70276-3. [DOI] [PubMed] [Google Scholar]


