Abstract
The facet joint has been increasingly implicated as a potential source of lower back pain. Diagnosis can be challenging as there is not a direct correlation between facet joint disease and clinical or radiological features. The purpose of this article is to review the diagnosis, treatment, and current imaging modality options in the context of degenerative facet joint disease. We describe each modality in turn with a pictorial review using current evidence. Newer hybrid imaging techniques such as single photon emission computed tomography/computed tomography (SPECT/CT) provide additional information relative to the historic gold standard magnetic resonance imaging. The diagnostic benefits of SPECT/CT include precise localization and characterization of spinal lesions and improved diagnosis for lower back pain. It may have a role in selecting patients for local therapeutic injections, as well as guiding their location with increased precision.
Keywords: Facet joint disease, imaging, lower back pain
INTRODUCTION
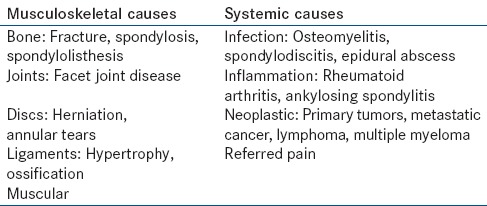
Lower back pain is a considerable problem affecting one-third of the UK adult population each year, of which 20% consult their general practitioner.[1] The causes of lower back pain are wide ranging and can be broadly divided into musculoskeletal and systemic causes [Table 1].
Table 1.
Causes of lower back pain
The etiology of lower back pain is often multifactorial and there are a variety of potential pain generators in the lumbar spine. The facet joint has been increasingly implicated as a significant source of pain since it was first described by Goldthwaite in 1911.[2] Pain can arise from any structure within the facet joint complex including the fibrous capsule, synovial membrane, hyaline cartilage, and bone.[3] Estimation of the prevalence of symptomatic facet joint arthropathy in the general population depends on the diagnostic criteria used and varies from 5% to 15%.[4] A large epidemiological multicenter study over 5 years in the USA found a prevalence of 4.8% with prevalence rates increasing with increasing age.[5] The L4-L5 facet joints are the most commonly and severely implicated with L3-L4 and L5-S1 also often involved.[6]
The majority of cases of facet joint arthropathy are attributable to repetitive stress and low-grade trauma and are often related to age and degeneration of the intervertebral disks.[7] Several conditions predispose individuals to developing facet joint pain. These include structural changes due to disk degeneration, spondylolysis or spondylolisthesis, and also inflammatory joint diseases including rheumatoid arthritis and seronegative arthritis. Other predisposing conditions include synovial impingement, meniscoid entrapment, chondromalacia facetae, pseudogout, villonodular synovitis, and acute and chronic infection.[4]
An increased sagittal-orientation may be the cause or result of degenerative spondylosis.[8,9] Traumatic disruption of the facet joints or vertebral body may also predispose to degenerative change and may lead to low back pain. For the purpose of this review, we will be focusing on back pain arising from the facet joint.
FUNCTIONAL ANATOMY
The facet joints in the spinal column are located posterior to the vertebral body. Each vertebra has two facet joints. The superior articular facet faces upward and articulates with the inferior articular facet of the vertebra above. Together with the intervertebral disk and its articulation with the adjacent vertebra they form a three joint complex which stabilizes the spine and allow it to flex, extend, and rotate through a wide range of motion.
The inner surface of the facet joint serves as the outer wall of the foramen of a spinal nerve, through which it exits. The disk and the junction of the two vertebral bodies serve as the inner wall of this foramen. The facet joint is surrounded by a joint capsule and its inner membrane produces synovial fluid lubricating the joint. The complex is a motion-restricting joint, able to resist stress, and withstand compressive, axial, and shearing forces.
Each facet joint is innervated by the medial branch of the dorsal ramus, which is held in place by the mamillo-accessory ligament. Each medial branch then gives off two further branches, one to the facet branch at the same level and one to the level below, that is, there is dual innervation of each facet joint. Triple innervation with the dorsal ramus innervating the joint above has also been suggested.[10] The reliable position of the medial branch of the dorsal ramus relative to the mamillo-accessory ligament and suitable vertebral landmarks allow ready radiographic identification and facilitates fluoroscopic intervention. In addition, aberrant innervation to the facet joints can occur and may account for the false negative rate seen in diagnostic blocks.[11]
The mechanisms postulated for the generation of pain from the facet joints are believed to be both biomechanical and inflammatory. The facet joint receives increasing loads as the spine is extended and is thought to carry up to 33% of the dynamic axial load.[12] Disk degeneration can alter the mechanical load distribution and increase axial rotation resulting in increased stress through the facet joint and hypertrophic changes in the capsule.[13] The result of repetitive loading is a release of cytokines and inflammatory mediators by the synovium leading to effusion and subsequent distension of the facet joints. The resulting stretching of the joint capsule causes pain via synovial and capsular nociceptors.[14] Inflammation may involve the adjacent nerve root causing radicular symptoms.[15] Chronic inflammatory changes can result in hypertrophy leading to foraminal narrowing and impingement on local nerve roots, and may potentially cause radicular symptoms.[3]
DIAGNOSIS
Diagnosing pain as deriving from the facet joints can be challenging. There is no physical examination technique, laboratory test or imaging modality, which is both sensitive and specific. Current standard criteria for the diagnosis of facet joint pain is reduction in symptoms following the direct introduction of local anesthetic into the facet joint or block of local innervation.[16] The procedure is considered diagnostic is there is pain relief of more than 50%.[17] The management of low back pain from facet joint arthropathy is based on a multidisciplinary approach and includes physiotherapy and exercise programs, medical management with nonsteroidal anti-inflammatory drugs, muscle relaxants, antidepressants, psychological therapy, and potentially also alternative therapies such as yoga or acupuncture.[4] As an adjunct to conservative management or if conservative management has failed, additional therapeutic intra-articular local anesthetic administration or regional neural blockade may provide additional symptomatic relief.[18]
RADIOLOGICAL IMAGING
Plain radiograph
Plain radiographs are of only limited use in investigating chronic back pain. However, they have a role in excluding acute presentations such as when osteoporotic collapse is suspected.[19] Typical findings in facet joint disease on plain radiograph include joint space narrowing, subchondral sclerosis, intra-articular gas and osteophyte formation.[20] Disk space narrowing is more readily visualized on plain radiographs [Figures 1 and 2]. Oblique radiographs are potentially the most useful at detecting abnormalities given the curved configuration, sagittal orientation of the lumbar facet joints, and multiple superimposed structures. One study reported that oblique radiographs had 55% sensitivity and 69% specificity in identifying the presence of degenerative change in the L3-4 and L5-S1 facet joints.[21] Plain radiographs may be good at identifying trauma and degenerative disease and assessing spine alignment. Sensitivity and specificity, however is poor as plain radiographs generally only demonstrate late degenerative changes and have a high false positive rate.[22] They also have little value in being able to predict response to facet joint interventions.
Figure 1.
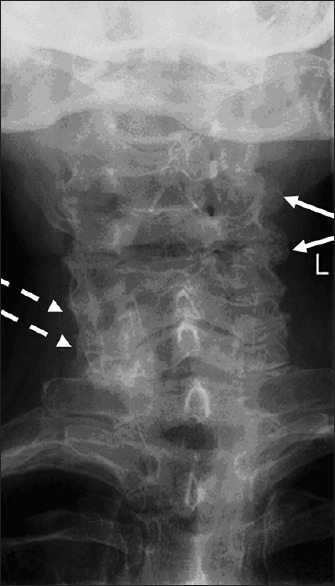
AP plan radiograph cervical spine: Cervical facet joint degeneration. Mid cervical facet (straight arrows) and lower cervical facet joint
Figure 2.
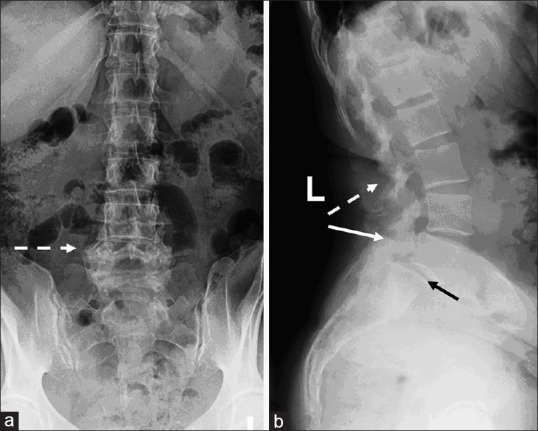
(a) AP and (b) Lat plan radiographs L-spine: Degenerate L4/5 (dashed arrows) and L5/S1 (straight arrows) facets joints with degenerate spondylolisthesis at L5/S1 (black arrow) (b)
Computed tomography
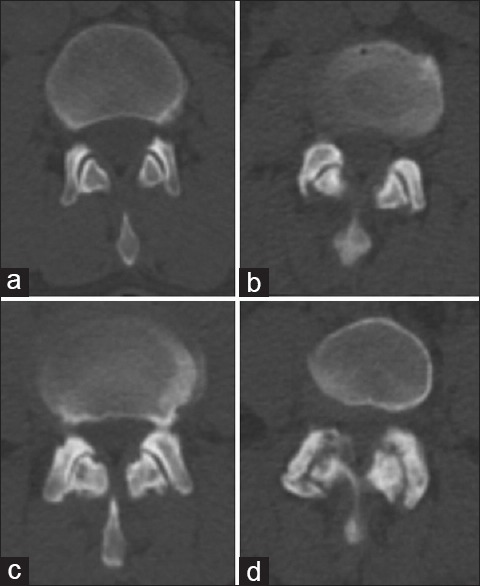
Computed tomography (CT) is used in the investigation of chronic back pain when magnetic resonance imaging (MRI) is contraindicated or when further assessment of spondylolyses is required.[19] CT is more sensitive than plain radiographs at demonstrating the degenerative changes of facet joints due to the high contrast between bony structures and soft tissues.[23] CT is good at delineating osteophytosis, subchondral sclerosis and erosions, and capsular calcification and can also show associated soft tissue changes such as synovial and ligamentum flavum hypertrophy. CT has the ability to detect age-related changes earlier than plain radiographs and has a potential role in grading of disease [Figures 3 and 4]. Pathria devised a grading system for facet joint degeneration using CT,[24] which classifies changes according to a 4 point scale [Table 2] to aid objective assessment of disease progression and severity [Figure 5].
Figure 3.
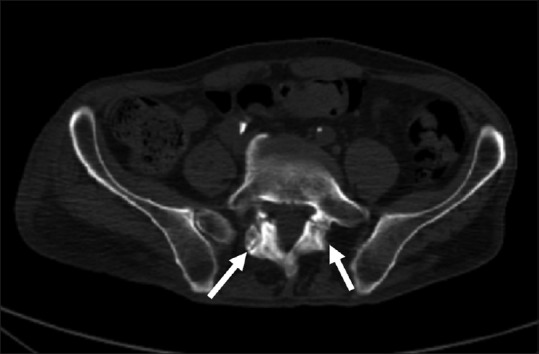
Computed tomography scan (L5/S1) showing bilateral pars defects (arrows)
Figure 4.
Computed tomography scan showing anterolisthesis at L5/S1 (arrow)
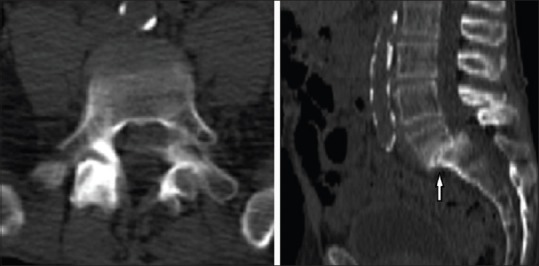
Table 2.
Criteria for grading facet joint arthropathy using CT
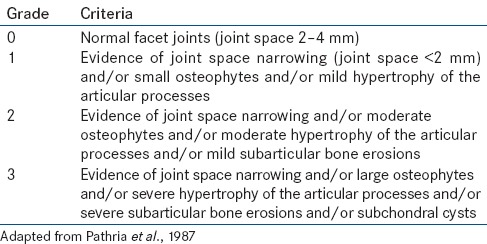
Figure 5.
Computed tomography Criteria for grading facet joint arthropathy (a) Normal facet joints (joint space 2–4 mm) (b) joint space narrowing (joint space <2 mm) and/or small osteophytes and/or mild hypertrophy of the articular processes (c) joint space narrowing and/or moderate osteophytes and/or moderate hypertrophy of the articular processes and/or mild subarticular bone erosions (d). Joint space narrowing and/or large osteophytes and/or severe hypertrophy of the articular processes and/or severe subarticular bone erosions and/or subchondral cysts
However, some studies found a poor correlation between radiologically identified facet joint arthritis on CT and lower back pain in a community-based setting.[25] Carrera used CT to image 100 consecutive patients with lower back pain and found 65 to have facet joint abnormality. The study concluded CT to be sensitive for identifying facet-mediated pain but not specific.[26] CT also has a poor differentiation of soft tissues within the spine and it is not optimal in demonstrating cartilage abnormalities which may indicate early facet degeneration.
Magnetic resonance imaging
Magnetic resonance imaging is the preferred investigation for the diagnosis of most spinal diseases as it has a superior delineation of soft tissues compared to other imaging modalities[19] [Figure 6]. T1-weighted sequences can exquisitely delineate the anatomy of the facet joints, ligamentum flavum, spinal cord, and nerve roots. T2-weighted sequences are useful in identifying fluid in facet joint effusions, periarticular cysts and also better delineate cartilage defects. Normal facet joints with intact capsules may hold between 1 and 2 ml of fluid. A larger effusion may indicate a loss of capsular function with subsequent abnormal facet joint motion. One study retrospectively looked at the relationship between the amount of facet joint fluid present and the degree of lumbar instability and found a positive linear correlation.[27] However, MRI is less sensitive for evaluating cortical anatomy, calcified structures, and is less accurate in the assessment of subchondral sclerosis. One study found that MRI tended to underestimate the severity of facet joint osteoarthritis compared with CT.[28] Gorbach found in a cohort of 42 patients undergoing facet joint blocks that the extent of facet joint arthropathy defined anatomically on MRI and CT was not a significant predictor for the outcome.[29] Despite this, MRI remains the gold standard currently for imaging facet joint disease. It is also helpful in identifying those patients who may benefit when planning a surgical intervention.
Figure 6.
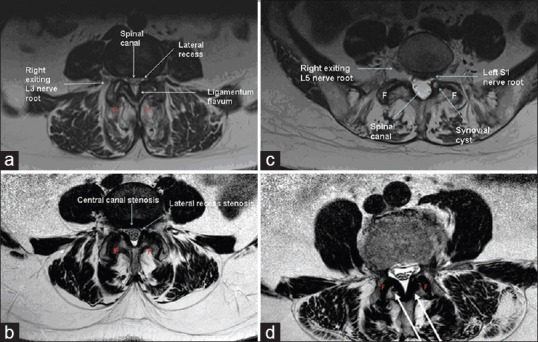
(a) Degenerate disc bulge which in combination with subluxed L3/4 facet joints leading to bilateral lateral recess (F = Degenerate L3/4 facet joint with subluxation). (b) Synovial cyst arising from the left L5/S1 facet joint with impingement on the left S1 nerve root within the lateral recess. (c) Central canal stenosis, lateral canal stenosis with Facet Joint degeneration and subluxation. (d) L3/4 facet joint degeneration and flaval hypertrophy
RADIONUCLIDE IMAGING
Bone scan
99mTc methylene diphosphonate (MDP) bone scintigraphy is a highly sensitive method for detecting disease in bone and can allow the detection of pathophysiology of trauma at a nascent stage.[30] Due to its excellent sensitivity it is often used as a screening tool, however limited anatomical detail results in poor specificity in accurately localizing site of facet joint involvement. It can either be performed as limited or whole body bone scintigraphy. Dynamic imaging, showing uptake and blood pool phase, can increase specificity in the diagnosis of inflammatory pathology, but is not routinely used in the assessment of facet joint disease.
Single photon emission computed tomography
In patients with chronic low back pain, bone single photon emission computed tomography (SPECT) with 99mTc MDP has been reported to be more sensitive than plain radiograph or conventional planar bone scan.[31] In addition, approximately one-third of abnormalities/lesions may not be visualized on the planar bone scan.[32] Bone SPECT is useful in the investigation of facet disease as a cause of low back pain (pain generator). First, it is useful in predicting patients who are likely to benefit from interventions such as denervation or local facet joint injections.[33] Second, it can identify nonfacetal causes of low back pain.[33,34] It can help in the evaluation of patients with back pain following spinal surgery as it is more sensitive than planar imaging alone.[35] It can locate the level of maximum instability or the cause of symptoms distal from the operative site[36,37] and it is not hampered by artifacts caused by surgical metal-work. Furthermore, Holder found that SPECT imaging of the lumbar spine in 58 consecutive patients with possible facet joint syndrome was 100% sensitive and 71% specific for the clinical diagnosis of facet disease.[38] In a hospital-wide population study looking at patients with spinal pain, increased facet joint uptake on SPECT was found in 42.9% of patients with the incidence increasing significantly with advancing age.[16]
Single photon emission computed tomography/computed tomography
Three-dimensional (3D) data acquisition using SPECT has improved spatial resolution and in combination with CT enables better anatomic localization. It has been used in patients with spinal pain for the diagnosis of facet joint arthritis.[39] Its use in other musculoskeletal conditions including the foot[40] and wrist[41,42] has previously been documented and is useful in localization of uptake at the sites with complex structural anatomy. Focal increased osteoblastic activity correlates to areas of mechanical stress and degenerative change in the absence of other pathology.[43] Studies have shown SPECT ± CT to be a sensitive modality with 20–50% greater lesion detection than planar 99mTc MDP imaging.[44,45] A recent retrospective study where patients with chronic back pain and inconclusive MRI/CT scans who underwent SPECT/CT showed that SPECT/CT precisely localized positive facet joint targets in 65% of the referral population[43] [Figures 7 and 8]. SPECT ± CT is useful in identifying associated pathology including endplate sclerosis, osteophytes, cystic lesions, and fractures. SPECT/CT is emerging as an ideal modality for imaging the facet joint due to the ability to accurately localize the site of pain and in the differentiation of pars defects or other degenerative changes from facet joint disease. Advantages include the detail of information it provides. However, its use as an appropriate imaging modality should be considered carefully given the increased radiation dose in young individuals with the benign disease and altered low dose CT protocols should be considered.
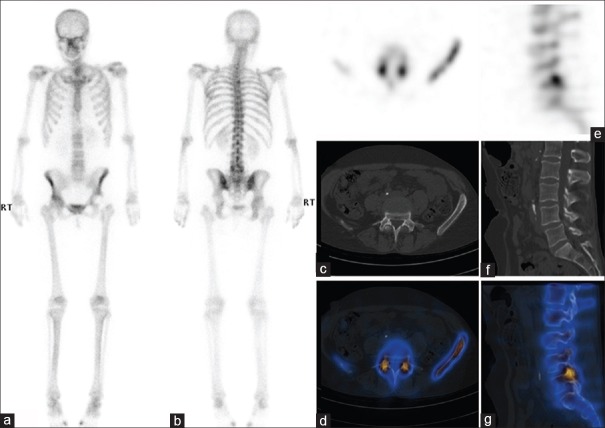
Figure 7.
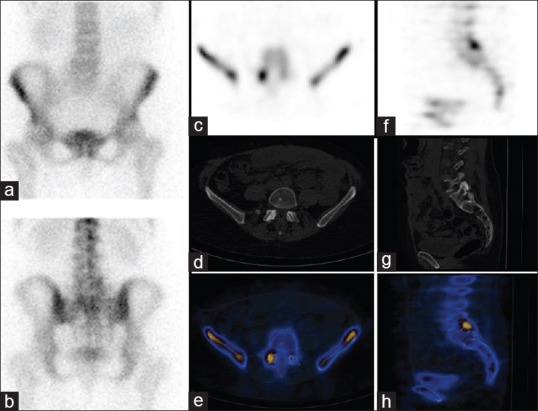
99mTc-MDP Bone scan: Patient with low back pain: (a, b) planar images showing subtle in-homogenous tracer uptake at the lower lumbar spine on the right side (b). (c-h) bone SPECT-CT scan demonstrates increased tracer uptake at the right L5/S1 facet joint. Scan findings consistent with active inflammatory disease involving the facet joint
Figure 8.
99mTc-methylene diphosphonate bone scan: Patient with low back pain: (a) Whole body bone scan shows subtle in-homogenous tracer uptake in the lower lumbar spine. A left hip prosthesis is noted (b-g) bone single photon emission computed tomography/computed tomography scan demonstrates increased tracer uptake at the L5/S1 facet joints bilaterally. Scan findings are consistent with active inflammatory disease involving the L5/S1 facet joints
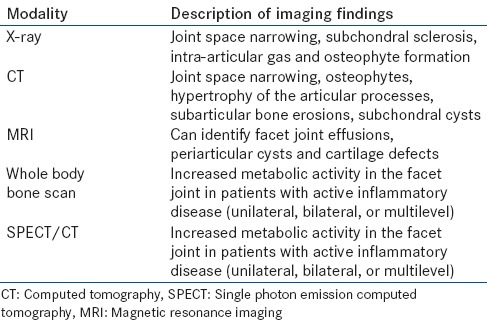
We have summarized the relative advantages and disadvantages of each imaging modality in Table 3 in diagnosing facet joint arthropathy. We have summarized the findings of facet joint arthropathy in different imaging modalities in Table 4.
Table 3.
Advantages and disadvantages of each imaging modality in the investigation of facet joint disease
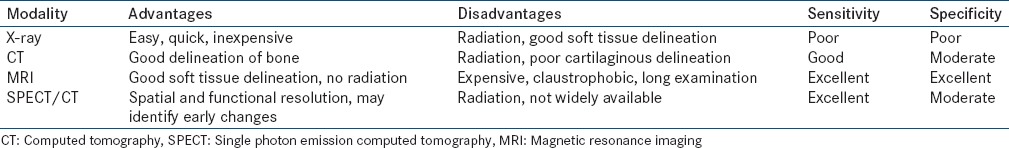
Table 4.
Findings of facet joint arthropathy in different imaging modalities
Predicting response to injection
With rising attention on outcomes and cost-effectiveness of treatment, there is a push toward positively identifying patients prospectively that will benefit from treatment. Dolan assessed 58 patients with lumbar facet joint disease using SPECT. Twenty-two patients with isotope uptake and 36 patients with negative scans had intra-articular corticosteroid injections. They found a 95% response at 1 month and 79% response at 3 months in the scan positive patients which was significantly greater compared to the control group.[46] Pneumaticos randomized 47 patients with lower back pain scheduled for facet joint injections into one group who underwent bone scintigraphy with SPECT prior to injection and one group who received injection only. The group undergoing the scan with positive uptake was injected at the site of increased uptake with the patients with negative scans and those not scanned injected at the levels indicated by the referring physician. The change in pain score at 1 month was significantly higher (P < 0.004) in the group who received scans and had positive uptake compared to those without positive uptake and those who did not receive scans. In the patients with positive scans, 13 out of 15 had a significant improvement in pain, compared with 2 out of 16 in the patients with negative scans and 5 out of 16 patients who were not scanned at all.[47] A study by Matar et al. retrospectively scanned patients with SPECT/CT with clinical facet joint disease. They found that SPECT/CT identified potential pain generators in 86% of lumbar spine scans and influenced the clinical decision to inject in 60% of cases of patients with positively localized facet joints.[43]
Conversely, a more recent study by Lehman et al. found that in patients undergoing targeted percutaneous treatment, there was discordance in clinical findings and activity on technetium 99mTc MDP SPECT/CT in 70% of patients. They reported that 46% had a side discrepancy and 53% of treated facet joints did not have increased activity.[48] Deciding which medial branch level should be blocked accurately can be difficult as facet joint disease may not correlate with physical signs and symptoms or radiological findings. This has led to overuse of treatment agents and unsuccessful procedures resulting in negative cost-effectiveness. The studies discussed suggest more research is required to determine the clinical significance of facet joint activity using SPECT/CT, but SPECT ± CT may be useful to identify the location of facet joint disease which are a potential pain generator and guide therapeutic injections.
THE ROLE OF IMAGING IN TREATMENT
Image-guided intra-articular injections
Large prospective trials have shown that intra-articular facet injections may have an important role in certain clinical scenarios [Figure 9]. Their use in nondegenerative facet joint disease has not been superior to placebo as of yet.[49] Nor is their use endorsed for routine therapeutic pain relief. However, they have been advocated in the elderly with facet joint arthropathy with or without synovitis as a palliative option.[33,47] Facet joint injections are considered in the patients with >3 months of persistent nonradicular pain not responding to conventional medical management and/or physiotherapy and resulting in functional disability.[50] Good results with injections of steroids[47] or hyaluronic acid[51] have been documented for lumbar facet joint disease. Total patient steroid dose during a 12 month period must be monitored, especially if the patient is an insulin-dependent diabetic. Intra-articular injections can either be fluoroscopy or CT-guided. Fluoroscopy can be performed in real-time and is easily accessible, whereas CT has the benefit of 3D imaging, allowing precise localization of the needle within the joint in cases where normal anatomy has been significantly altered by degenerative disease. A multi-society consensus recommended one therapeutic facet joint injection, per level affected, per year as reasonable.[17] However, if the patient has >50% sustained relief for at least 3 months and radiofrequency ablation (RFA) is contraindicated or refused by the patient, individuals may receive one additional therapeutic injection per level per year. As of yet, no formally validated functional outcome tool has been developed to assess response and as a minimum clinicians should document whether pain relief is achieved when patients perform maneuver that typically exacerbate their pain. Functional outcome assessments are recommended before and at intervals following the intervention for a minimum of 7–10 days and thereafter at 3 and 6 months. An analogue pain diary, patient specific functional improvement score, or quality of life scale such as SF-12 or SF-36 would be appropriate to use in this instance.
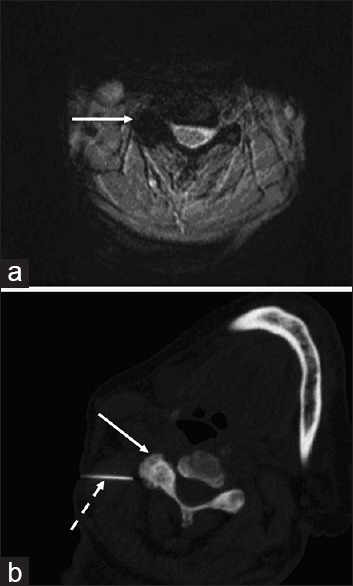
Figure 9.
Patient with severe neck pain: (a) Magnetic resonance imaging shows degenerate changes at right C3/4 facet joint (arrow). (b) Patient underwent computed tomography guided facet joint injection (arrow) (dashed arrow = spinal needle)
Radiofrequency ablation of medial branch nerve
Radiofrequency ablation may be considered when there is at least 50% pain relief in response to medial branch anesthetic blocks. Radio-frequency probes are inserted under fluoroscopic guidance to the appropriate level and heat deposited in adjacent tissue. The medial branch is located between the intervertebral foramen and mamillo accessory ligament using dorsal, lateral, and oblique projections. The heating effect is produced from the distal shaft of the electrode rather than at the tip.[52] This means that the RFA probe should be placed parallel to the medial branch rather than perpendicular. Suggested retreatment interval is 6–12 months with improved pain relief reported after serial treatments. RFA should only be repeated if the patient reports >50% pain relief with functional improvement for a minimum of 6 months. If facet joint pain should then recur, the procedure can be repeated with a recommendation of no more than 2 ablations per year per level.[17] Two high quality randomized controlled trials evaluating RFA of medial branch nerves versus placebo blocks showed a >50% pain relief at 4–8 weeks.[3,53]
Computed tomography-guided decompression of synovial cysts
Synovial cysts are associated with facet joint arthropathy and most common at the L4/5 level.[54] They communicate directly with the facet synovial joint, and therefore they can be accessed percutaneously with CT guidance. This is preferred over fluoroscopy given the associated osteoarthritic changes.[49] A mixture of steroid, anesthetic, and contrast is injected into the joint space leading to rupture of the cyst. Successful decompression of the cyst is confirmed by the epidural spread of contrast on CT. Pain should be reassessed following the treatment to confirm success.
CONCLUSION
Imaging is important in identifying facet joint disease as the cause for lower back pain given the low specificity of clinical examination. Techniques with good anatomical delineation such as CT are useful in ruling out other pathology. Newer hybrid imaging techniques such as SPECT/CT provide additional information relative to the historic gold standard MRI. The diagnostic benefits of SPECT/CT may include precise localization and characterization of spinal lesions, better diagnostic tool for lower back pain and it may have a role in selecting patients for local therapeutic injections, as well as guiding their location with increased precision. Overall therefore SPECT/CT may provide additional information to current imaging modalities to help guide therapy and improve patient outcomes.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Nice Guidelines. Low back pain: Early management of persistent non-specific low back pain. 2009. [Last accessed on 2015 Feb 12]. Available from: http://www.nice.org.uk/guidance/cg88/resources/guidance-low-back-pain-pdf .
- 2.Goldthwaite JE. The lumbosacral articulation: An explanation of many cases of lumbago, sciatica, and paraplegia. Boston Med Surg J. 1911;164:365–72. [Google Scholar]
- 3.van Kleef M, Barendse GA, Kessels A, Voets HM, Weber WE, de Lange S. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine (Phila Pa 1976) 1999;24:1937–42. doi: 10.1097/00007632-199909150-00013. [DOI] [PubMed] [Google Scholar]
- 4.Cohen SP, Raja SN. Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiology. 2007;106:591–614. doi: 10.1097/00000542-200703000-00024. [DOI] [PubMed] [Google Scholar]
- 5.Long DM, BenDebba M, Torgerson WS, Boyd RJ, Dawson EG, Hardy RW, et al. Persistent back pain and sciatica in the United States: Patient characteristics. J Spinal Disord. 1996;9:40–58. [PubMed] [Google Scholar]
- 6.Eubanks JD, Lee MJ, Cassinelli E, Ahn NU. Prevalence of lumbar facet arthrosis and its relationship to age, sex, and race: An anatomic study of cadaveric specimens. Spine (Phila Pa 1976) 2007;32:2058–62. doi: 10.1097/BRS.0b013e318145a3a9. [DOI] [PubMed] [Google Scholar]
- 7.Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, Reilly J. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine (Phila Pa 1976) 1978;3:319–28. doi: 10.1097/00007632-197812000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Grobler LJ, Robertson PA, Novotny JE, Pope MH. Etiology of spondylolisthesis. Assessment of the role played by lumbar facet joint morphology. Spine (Phila Pa 1976. 1993;18:80–91. [PubMed] [Google Scholar]
- 9.Boden SD, Riew KD, Yamaguchi K, Branch TP, Schellinger D, Wiesel SW. Orientation of the lumbar facet joints: Association with degenerative disc disease. J Bone Joint Surg Am. 1996;78:403–11. doi: 10.2106/00004623-199603000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Paris SV. Anatomy as related to function and pain. Orthop Clin North Am. 1983;14:475–89. [PubMed] [Google Scholar]
- 11.Kaplan M, Dreyfuss P, Halbrook B, Bogduk N. The ability of lumbar medial branch blocks to anesthetize the zygapophysial joint. A physiologic challenge. Spine (Phila Pa 1976. 1998;23:1847–52. doi: 10.1097/00007632-199809010-00008. [DOI] [PubMed] [Google Scholar]
- 12.Yang KH, King AI. Mechanism of facet load transmission as a hypothesis for low-back pain. Spine (Phila Pa 1976) 1984;9:557–65. doi: 10.1097/00007632-198409000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Boszczyk BM, Boszczyk AA, Korge A, Grillhösl A, Boos WD, Putz R, et al. Immunohistochemical analysis of the extracellular matrix in the posterior capsule of the zygapophysial joints in patients with degenerative L4-5 motion segment instability. J Neurosurg. 2003;99:27–33. doi: 10.3171/spi.2003.99.1.0027. [DOI] [PubMed] [Google Scholar]
- 14.Dory MA. Arthrography of the lumbar facet joints. Radiology. 1981;140:23–7. doi: 10.1148/radiology.140.1.6454162. [DOI] [PubMed] [Google Scholar]
- 15.Willburger RE, Wittenberg RH. Prostaglandin release from lumbar disc and facet joint tissue. Spine (Phila Pa 1976) 1994;19:2068–70. doi: 10.1097/00007632-199409150-00011. [DOI] [PubMed] [Google Scholar]
- 16.Makki D, Khazim R, Zaidan AA, Ravi K, Toma T. Single photon emission computerized tomography (SPECT) scan-positive facet joints and other spinal structures in a hospital-wide population with spinal pain. Spine J. 2010;10:58–62. doi: 10.1016/j.spinee.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 17.Hecker B, Waldmann G, Mangold W. Multisociety Facet Task Force Consensus Response. 2009. [Last accessed on 2015 Feb 12]. Available from: http://www.asipp.org/documents/task_force_facetFINAL.pdf .
- 18.Gopinathan A, Peh W. Image guided facet joint injection. Biomed Imaging Interv J. 2011;7:e4. doi: 10.2349/biij.7.1.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.iRefer. The Royal College of Radiologists Imaging Guidelines for Chronic Lumbar Backpain with no clinical or serological indicators of infection or neoplasia. [Last accessed on 2015 Feb 12]. Available from: http://www.guidelines.irefer.org.uk/adult/#Tpc151 .
- 20.DePalmer M. New York, USA: Demos MEDICAL; 2011. iSPINE Evidence-based Interventional Spine Care. [Google Scholar]
- 21.Pathria M, Sartoris DJ, Resnick D. Osteoarthritis of the facet joints: Accuracy of oblique radiographic assessment. Radiology. 1987;164:227–30. doi: 10.1148/radiology.164.1.3588910. [DOI] [PubMed] [Google Scholar]
- 22.Jackson M, Simpson K. Chronic back pain. Contin Educ Anaesth Crit Care Pain. 2006;6:152–5. [Google Scholar]
- 23.Weishaupt D, Zanetti M, Boos N, Hodler J. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol. 1999;28:215–9. doi: 10.1007/s002560050503. [DOI] [PubMed] [Google Scholar]
- 24.Pathria M, Sartoris DJ, Resnick D. Osteoarthritis of the facet joints: Accuracy of oblique radiographic assessment. Radiology. 1987;164:227–30. doi: 10.1148/radiology.164.1.3588910. [DOI] [PubMed] [Google Scholar]
- 25.Kalichman L, Li L, Kim DH, Guermazi A, Berkin V, O’Donnell CJ, et al. Facet joint osteoarthritis and low back pain in the community-based population. Spine (Phila Pa 1976) 2008;33:2560–5. doi: 10.1097/BRS.0b013e318184ef95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carrera GF. Lumbar facet joint injection in low back pain and sciatica: Preliminary results. Radiology. 1980;137:665–7. doi: 10.1148/radiology.137.3.6449717. [DOI] [PubMed] [Google Scholar]
- 27.Rihn JA, Lee JY, Khan M, Ulibarri JA, Tannoury C, Donaldson WF, 3rd, et al. Does lumbar facet fluid detected on magnetic resonance imaging correlate with radiographic instability in patients with degenerative lumbar disease? Spine (Phila Pa 1976) 2007;32:1555–60. doi: 10.1097/BRS.0b013e318067dc55. [DOI] [PubMed] [Google Scholar]
- 28.Fujiwara A, Tamai K, Yamato M, An HS, Yoshida H, Saotome K, et al. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: An MRI study. Eur Spine J. 1999;8:396–401. doi: 10.1007/s005860050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gorbach C, Schmid MR, Elfering A, Hodler J, Boos N. Therapeutic efficacy of facet joint blocks. AJR Am J Roentgenol. 2006;186:1228–33. doi: 10.2214/AJR.04.1042. [DOI] [PubMed] [Google Scholar]
- 30.Van der Wall H, Lee A, Magee M, Frater C, Wijesinghe H, Kannangara S. Radionuclide bone scintigraphy in sports injuries. Semin Nucl Med. 2010;40:16–30. doi: 10.1053/j.semnuclmed.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 31.Cook GJ, Gibson T, Fogelman I. Back pain: Can we make a contribution? Eur J Nucl Med. 1997;24:363–7. doi: 10.1007/BF00881806. [DOI] [PubMed] [Google Scholar]
- 32.Ryan PJ, Evans PA, Gibson T, Fogelman I. Chronic low back pain: Comparison of bone SPECT with radiography and CT. Radiology. 1992;182:849–54. doi: 10.1148/radiology.182.3.1531544. [DOI] [PubMed] [Google Scholar]
- 33.Dolan AL, Ryan PJ, Arden NK, Stratton R, Wedley JR, Hamann W, et al. The value of SPECT scans in identifying back pain likely to benefit from facet joint injection. Br J Rheumatol. 1996;35:1269–73. doi: 10.1093/rheumatology/35.12.1269. [DOI] [PubMed] [Google Scholar]
- 34.Holder LE, Machin JL, Asdourian PL, Links JM, Sexton CC. Planar and high-resolution SPECT bone imaging in the diagnosis of facet syndrome. J Nucl Med. 1995;36:37–44. [PubMed] [Google Scholar]
- 35.Slizofski WJ, Collier BD, Flatley TJ, Carrera GF, Hellman RS, Isitman AT. Painful pseudarthrosis following lumbar spinal fusion: Detection by combined SPECT and planar bone scintigraphy. Skeletal Radiol. 1987;16:136–41. doi: 10.1007/BF00367762. [DOI] [PubMed] [Google Scholar]
- 36.Lusins JO, Danielski EF, Goldsmith SJ. Bone SPECT in patients with persistent back pain after lumbar spine surgery. J Nucl Med. 1989;30:490–6. [PubMed] [Google Scholar]
- 37.Gates GF, McDonald RJ. Bone SPECT of the back after lumbar surgery. Clin Nucl Med. 1999;24:395–403. doi: 10.1097/00003072-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Holder LE, Machin JL, Asdourian PL, Links JM, Sexton CC. Planar and high-resolution SPECT bone imaging in the diagnosis of facet syndrome. J Nucl Med. 1995;36:37–44. [PubMed] [Google Scholar]
- 39.Dutton JA, Hughes SP, Peters AM. SPECT in the management of patients with back pain and spondylolysis. Clin Nucl Med. 2000;25:93–6. doi: 10.1097/00003072-200002000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Lagroudi B, Mohan H, Gnanasegaran G. SPECT-CT in the assessment of bony foot pathology. J Nucl Med. 2007;48(Suppl 2):122. [Google Scholar]
- 41.Huellner M, Strobel K, Hug U. SPECT/CT in diagnostics of the hand joint. Radiologe. 2012;52:621–8. doi: 10.1007/s00117-011-2269-9. [DOI] [PubMed] [Google Scholar]
- 42.Schleich FS, Schürch M, Huellner MW, Hug U, von Wartburg U, Strobel K, et al. Diagnostic and therapeutic impact of SPECT/CT in patients with unspecific pain of the hand and wrist. EJNMMI Res. 2012;2:53. doi: 10.1186/2191-219X-2-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matar HE, Navalkissoor S, Berovic M, Shetty R, Garlick N, Casey AT, et al. Is hybrid imaging (SPECT/CT) a useful adjunct in the management of suspected facet joints arthropathy? Int Orthop. 2013;37:865–70. doi: 10.1007/s00264-013-1811-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gates GF. Oblique angle bone SPECT imaging of the lumbar spine, pelvis, and hips. An anatomic study. Clin Nucl Med. 1996;21:359–62. doi: 10.1097/00003072-199605000-00001. [DOI] [PubMed] [Google Scholar]
- 45.Carstensen MH, Al-Harbi M, Urbain JL, Belhocine TZ. SPECT/CT imaging of the lumbar spine in chronic low back pain: A case report. Chiropr Man Therap. 2011;19:2. doi: 10.1186/2045-709X-19-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dolan AL, Ryan PJ, Arden NK, Stratton R, Wedley JR, Hamann W, et al. The value of SPECT scans in identifying back pain likely to benefit from facet joint injection. Br J Rheumatol. 1996;35:1269–73. doi: 10.1093/rheumatology/35.12.1269. [DOI] [PubMed] [Google Scholar]
- 47.Pneumaticos SG, Chatziioannou SN, Hipp JA, Moore WH, Esses SI. Low back pain: Prediction of short. term outcome of facet joint injection with bone scintigraphy. Radiology. 2006;238:693–8. doi: 10.1148/radiol.2382041930. [DOI] [PubMed] [Google Scholar]
- 48.Lehman VT, Murphy RC, Kaufmann TJ, Diehn FE, Murthy NS, Wald JT, et al. Frequency of discordance between facet joint activity on technetium Tc99m methylene diphosphonate SPECT/CT and selection for percutaneous treatment at a large multispecialty institution. AJNR Am J Neuroradiol. 2014;35:609–14. doi: 10.3174/ajnr.A3731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Falco FJ, Erhart S, Wargo BW, Bryce DA, Atluri S, Datta S, et al. Systematic review of diagnostic utility and therapeutic effectiveness of cervical facet joint interventions. Pain Physician. 2009;12:323–44. [PubMed] [Google Scholar]
- 50.Bykowski JL, Wong WH. Role of facet joints in spine pain and image-guided treatment: A review. AJNR Am J Neuroradiol. 2012;33:1419–26. doi: 10.3174/ajnr.A2696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fuchs S, Erbe T, Fischer HL, Tibesku CO. Intraarticular hyaluronic acid versus glucocorticoid injections for nonradicular pain in the lumbar spine. J Vasc Interv Radiol. 2005;16:1493–8. doi: 10.1097/01.RVI.0000175334.60638.3F. [DOI] [PubMed] [Google Scholar]
- 52.Bogduk N, Macintosh J, Marsland A. Technical limitations to the efficacy of radiofrequency neurotomy for spinal pain. Neurosurgery. 1987;20:529–35. doi: 10.1227/00006123-198704000-00004. [DOI] [PubMed] [Google Scholar]
- 53.Gallagher J, Petriccione di Vadi PL, Wedley JR. Radiofrequency facet joint denervation in the treatment of low back pain: A prospective controlled double-blind study to assess its efficacy. Pain Clin. 1994;7:193–8. [Google Scholar]
- 54.Sabo RA, Tracy PT, Weinger JM. A series of 60 juxtafacet cysts: Clinical presentation, the role of spinal instability, and treatment. J Neurosurg. 1996;85:560–5. doi: 10.3171/jns.1996.85.4.0560. [DOI] [PubMed] [Google Scholar]