Abstract
This study was conducted to evaluate the impact of implementation of an automated liquid culture system on the diagnosis of tuberculous pleurisy in an HIV-uninfected patient population. We retrospectively compared the culture yield, time to positivity, and contamination rate of pleural effusion samples in the BACTEC Mycobacteria Growth Indicator Tube 960 (MGIT) and Ogawa media among patients with tuberculous pleurisy. Out of 104 effusion samples, 43 (41.3%) were culture positive on either the MGIT or the Ogawa media. The culture yield of MGIT was higher (40.4%, 42/104) than that of Ogawa media (18.3%, 19/104) (P<0.001). One of the samples was positive only on the Ogawa medium. The median time to positivity was faster in the MGIT (18 days, range 8-32 days) than in the Ogawa media (37 days, range 20-59 days) (P<0.001). No contamination or growth of nontuberculous mycobacterium was observed on either of the culture media. In conclusion, the automated liquid culture system could provide approximately twice as high yields and fast results in effusion culture, compared to solid media. Supplemental solid media may have a limited impact on maximizing sensitivity in effusion culture; however, further studies are required.
Graphical Abstract
Keywords: Tuberculosis, Pleural Effusion, Pleurisy, Culture Media
INTRODUCTION
An automated liquid culture system is one of the major achievements in tuberculosis (TB) diagnostics. It increases the case yield by 10% over solid media and reduces the diagnostic delay (1, 2). However, liquid media are more prone to bacterial contamination and isolation of nontuberculous mycobacteria (NTM) (3). In addition, some strains grow only on solid media. Therefore, the current international guidelines have recommended the combined use of liquid and solid media on all specimens to maximize sensitivity (4, 5). However, this recommendation was primarily based on studies with respiratory specimens.
Pleural effusion cultures using solid media have been considered minimally helpful for the diagnosis of TB pleurisy in clinical practice because of their low sensitivity and diagnostic delay (6). The yield of effusion culture has increased considerably by implementation of liquid culture methods (7, 8, 9, 10, 11). However, previous studies were too heterogeneous to quantify the impact of liquid media in the diagnosis of HIV-uninfected patients with TB pleurisy.
We conducted a head-to-head comparison of liquid and solid media in effusion culture in order to evaluate how much the diagnostic yield is increased in HIV-uninfected patients by implementation of the liquid culture system, as compared to solid media. This study also aimed to assess whether the combined use of liquid and solid media is necessary to maximize the sensitivity of effusion culture and to determine the predictors of culture-positive effusion.
MATERIALS AND METHODS
Subjects and data collection
We included consecutive patients with TB pleurisy who underwent diagnostic thoracentesis at the Pusan National University Yangsan Hospital, Korea, from January 2011 to December 2013. An automated liquid culture system was introduced in the hospital in August 2010, and was routinely performed in combination with solid media on all specimens from January 2011. If patients could not expectorate sputum spontaneously, sputum induction was performed according to the standardized protocol.
We retrospectively reviewed the patients' medical records for collection of demographic, radiological, and microbiological information. The initial chest radiographs and computed tomography (CT) scans were reviewed by a blinded radiologist. The amount of pleural effusion was graded as small, moderate, or large based on the chest radiographs before thoracentesis (12).
Diagnostic criteria
A definitive diagnosis of TB pleurisy was made if one of the following criteria were met: 1) positive mycobacterial culture in pleural fluid or pleural biopsy tissue samples; 2) granulomatous inflammation in pleural biopsy tissue samples; 3) positive mycobacterial culture of sputum and pleural effusion that was resolved with anti-tuberculous treatment. TB pleurisy was considered probable in patients with lymphocytic exudates from the first or subsequent thoracentesis, high pleural fluid ADA levels (>40 U/l), negative cytological results, and effusions that cleared in response to anti-TB treatment.
Laboratory methods
Pleural fluid was collected into 50 mL sterile polypropylene tubes and transported to the laboratory. Pleural fluid samples were concentrated by centrifugation without decontamination procedures. The pellet was resuspended in 1-2 mL of sterile phosphate buffer (pH 6.8), and both Ziehl-Neelsen- and auramine-stained smear were examined. About 0.5 mL of sediment was cultured using the BACTEC MGIT 960 system (MGIT) (BD Diagnostic Systems, Sparks, MD, USA) according to the manufacturer's instructions, and another 0.5 mL was inoculated onto the Ogawa medium (Korean Institute of Tuberculosis, Seoul, Korea). The Ogawa media were incubated under an atmosphere containing 5% CO2 at 37℃ and were observed on a weekly interval till 8 weeks, whereas the MGIT were processed till 6 weeks.
Statistical analysis
The chi-square test or Fisher's exact test was performed to compare categorical variables, and Student's t-test or Mann-Whitney U-test was used to compare continuous variables. To identify the predictors of positive effusion culture, binary logistic regression analysis with the backward elimination method was performed for variables with P<0.2 in the univariate analysis, and the Hosmer-Lemeshow test was used to test the goodness-of-fit of the models. All analyses were performed using SPSS version 15.0 (SPSS Inc, Chicago, IL, USA), and results with P<0.05 were considered statistically significant.
Ethics statement
The protocol for this study was approved by the institutional review board of the Pusan National University Yangsan Hospital (IBB No. 05-2015-001) and informed consent was waived.
RESULTS
Diagnosis of tuberculous pleurisy
A total of 104 patients with TB pleurisy were included in this study. The mean age of the patients was 50 (range 16-96) yr, and 59 (56.7%) of them were male. HIV-ELISA tests were performed on 24 patients, and all were sero-negative.
Among the 104 patients, 76 (73.1%) were diagnosed as definite TB pleurisy, while the remaining 28 (26.9%) were probable TB pleurisy. The sensitivity of each method for the diagnosis of TB pleurisy is presented in Table 1. The sensitivity of effusion culture was 41.3%, which was about five times higher than that of TB-PCR (8.4%). The combination of the effusion and sputum cultures contributed to a good diagnostic yield of 66.3% (69/104), while 25 (24.0%) patients were culture positive with regard to the pleural fluid alone. Medical thoracoscopic biopsy was performed on 20 patients, all of whom showed granuloma or were culture positive on pleural tissue samples.
Table 1. Sensitivity of diagnostic methods for tuberculous pleurisy.
| Parameters | n=104 | % |
|---|---|---|
| Smear, effusion | 2 | 1.9 |
| Smear, sputum | 20 | 19.2 |
| Culture, effusion | 43 | 41.3 |
| Solid media | 19 | 18.3 |
| Liquid media | 42 | 40.4 |
| Culture, sputum | 44 | 42.3 |
| Culture, either effusion or sputum | 69 | 66.3 |
| TB-PCR, effusion | 8/95 | 8.4 |
| Pleural biopsy | 20/20 | 100 |
| ADA >40 U/l alone | 95 | 91.3 |
| ADA >40 U/+Lymphocytes >50% | 76 | 73.1 |
TB, tuberculosis; PCR, polymerase chain reaction; ADA, adenosine deaminase.
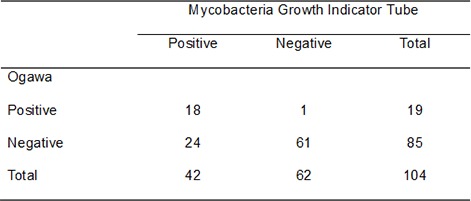
Comparison of culture media in effusion culture
Of the 104 pleural fluid samples, 43 (41.3%) were culture positive on either the MGIT or the Ogawa media. The culture yield of MGIT was higher (40.4%, 42/104) than that of Ogawa media (18.3%, 19/104) (P<0.001) (Table 2). One pleural fluid sample was positive only in the Ogawa medium. The median time to positivity was faster in the MGIT (18 days, range 8-32 days) than in the Ogawa media (37 days, range 20-59 days) (P<0.001). No contamination or growth of NTM was observed on either of the culture media.
Table 2. Comparison of solid and liquid culture media for isolation of Mycobacterium tuberculosis from pleural fluid.
| Mycobacteria Growth Indicator Tube | |||
|---|---|---|---|
| Positive | Negative | Total | |
| Ogawa | |||
| Positive | 18 | 1 | 19 |
| Negative | 24 | 61 | 85 |
| Total | 42 | 62 | 104 |
Predictors of culture-positive effusion
Patients with culture-positive effusion were younger than those with culture-negative effusion; however, there were no significant differences in other demographic characteristics (Table 3). The number of patients with lung infiltration on chest CT was higher while the number of patients who showed sputum-smear positivity was lower in the effusion culture-positive group than in the effusion culture-negative group. However, these differences were not statistically significant (P=0.171 and P=0.099, respectively). With regard to pleural fluid findings, patients with culture-positive effusion had significantly lower lymphocyte percentage, pH, and glucose level, and higher polymorphonuclear leukocytes (PMNL) percentage and LDH level than patients with culture-negative effusion.
Table 3. Comparison of patients with culture-positive and culture-negative pleural effusion.
| Parameters | Culture (-) N=61 |
Culture (+) N=43 |
Total N=104 |
P value |
|---|---|---|---|---|
| Demographics | ||||
| Male | 33 (54.1) | 26 (60.5) | 59 (56.7) | 0.519 |
| Age (yr) | 53.6±22.3 | 43.9±20.9 | 49.6±22.2 | 0.026 |
| BMI | 21.5±3.4 | 21.1±3.0 | 21.3±3.2 | 0.506 |
| Smoker | 23 (37.7) | 13 (30.2) | 36 (34.6) | 0.430 |
| Former tuberculosis | 8 (13.1) | 4 (9.3) | 12 (11.5) | 0.757 |
| Diabetes | 9 (14.8) | 2 (4.7) | 11 (10.6) | 0.118 |
| Microbiological | ||||
| Sputum AFB smear | 15 (24.6) | 5 (11.6) | 20 (19.2) | 0.099 |
| Sputum culture | 26 (42.6) | 18 (41.9) | 44 (42.3) | 0.938 |
| PF AFB smear | 0 (0) | 2 (4.7) | 2 (1.9) | 0.169 |
| Radiological | ||||
| Lung infiltrate, CXR | 35 (57.4) | 20 (46.5) | 55 (52.9) | 0.274 |
| Lung infiltrate, CT | 42/59 (71.2) | 25 (58.1) | 67/102 (65.7) | 0.171 |
| Cavity, CXR | 3 (4.9) | 1 (2.3) | 4 (3.8) | 0.641 |
| Cavity, CT | 6/59 (10.2) | 3 (7.0) | 9 (8.8) | 0.730 |
| Amount of effusion | 0.162 | |||
| Small | 18 (29.5) | 20 (46.5) | 38 (36.5) | |
| Moderate | 30 (49.2) | 14 (32.6) | 44 (42.3) | |
| Large | 13 (21.3) | 9 (20.9) | 22 (21.2) | |
| Blood | ||||
| WBC | 6,935±2,723 | 7,621±3,372 | 7,219±3,012 | 0.255 |
| CRP | 7.7±5.9 | 8.8±6.8 | 8.2±6.3 | 0.384 |
| Protein | 7.2±0.8 | 7.2±0.6 | 7.2±0.7 | 0.769 |
| Albumin | 3.7±0.5 | 3.9±0.5 | 3.8±0.5 | 0.155 |
| LDH | 394±111 | 416±164 | 403±135 | 0.415 |
| Pleural fluid | ||||
| Total cells | 3,008±3,601 | 3,485±5,908 | 3,204±4,674 | 0.611 |
| Lymphocytes (%) | 76.2±22.6 | 55.8±30.7 | 67.7±28.0 | <0.001 |
| PMNL (%) | 11.4±20.3 | 32.5±31.5 | 20.1±27.5 | <0.001 |
| pH | 7.62±0.24 | 7.48±0.24 | 7.56±0.25 | 0.003 |
| Glucose | 104±47 | 71.7±65 | 91±57 | 0.004 |
| Protein | 5.1±0.8 | 5.1±0.6 | 5.1±0.7 | 0.792 |
| Albumin | 2.8±0.5 | 2.9±0.5 | 2.8±0.5 | 0.383 |
| LDH | 763±452 | 1,325±751 | 995±653 | <0.001 |
| ADA | 80.5±28.7 | 88.6±29.3 | 83.8±29.1 | 0.166 |
Data are presented as number (%) or mean±SD. BMI, body mass index; AFB, acid-fast bacilli; PF, pleural fluid; CXR, chest radiograph; CT, computed tomography; WBC, white blood cell; CRP, c-reactive protein; LDH, lactate dehydrogenase; PMNL, polymorphonuclear leukocytes; ADA, adenosine deaminase.
The multivariate logistic regression model identified three independent predictors of the culture-positive effusion, including effusion PMNL percentage (aOR 1.026; 95% CI 1.006-1.046), effusion pH level (aOR 0.06; 95% CI 0.005-0.757), and effusion LDH level (U/l) (aOR 1.002; 95% CI 1.001-1.003) (Table 4).
Table 4. Predictors for culture-positive effusion among patients with tuberculous pleurisy.
| Variables | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| OR (95% CI) | P value | aOR (95% CI) | P value | |
| Age | 0.979 (0.961-0.998) | 0.029 | ||
| Diabetes | 0.28 (0.058-1.376) | 0.118 | ||
| Sputum AFB smear | 0.404 (0.134-1.212) | 0.106 | 0.249 (0.047-1.328) | 0.104 |
| Lung infiltrates, CT | 0.56 (0.246-1.286) | 0.172 | ||
| Effusion amount, small | 2.077 (0.921-4.686) | 0.078 | ||
| Seurm albumin | 1.806 (0.799-4.083) | 0.155 | ||
| Pleural fluid | ||||
| Lymphocyte (%) | 0.972 (0.957-0.988) | 0.001 | ||
| PMNL (%) | 1.032 (1.014-1.050) | <0.001 | 1.026 (1.006-1.046) | 0.011 |
| pH | 0.066 (0.009-0.464) | 0.006 | 0.06 (0.005-0.757) | 0.030 |
| Glucose | 0.984 (0.972-0.995) | 0.006 | ||
| LDH | 1.002 (1.001-1.003) | <0.001 | 1.002 (1.001-1.003) | 0.001 |
OR, odds ratio; AFB, acid-fast bacilli; CT, computed tomography; PMNL, polymorphonuclear leukocytes; LDH, lactate dehydrogenase.
DISCUSSION
This study aimed to evaluate the impact of the implementation of automated liquid culture systems on the diagnosis of TB pleurisy. The results showed that the use of automated liquid culture systems can provide approximately twice as high yields and fast results in effusion culture in HIV-uninfected patients, as compared to those obtained using solid media. Effusion culture provided a confirmatory diagnosis in about 40% of patients when liquid media alone were used, and in nearly two thirds of the patients when combined with sputum culture. Although effusion culture using solid media has been considered minimally helpful because of its low sensitivity, the role of effusion culture should be reconsidered with the implementation of the automated liquid culture system. Mycobacterial culture remains the gold standard for the detection of and drug susceptibility tests in TB pleurisy. The higher yield obtained using liquid culture media may facilitate early and adequate treatment, consequently improving the outcome of patients with TB pleurisy.
Studies using liquid media reported approximately 40%-60% of sensitivity in effusion culture (7, 8, 9, 10, 11). However, previous studies were too heterogeneous to quantify the impact of liquid media in the diagnosis of HIV-uninfected patients with TB pleurisy. Some of these studies did not directly compare the performance of liquid and solid media (7, 10, 11), included HIV-infected patients who often show higher yields in effusion culture (10, 11), or used bedside inoculation (7, 8, 11). In one study, the BACTEC system provided positive cultures in 24% of HIV-negative patients and 75% of HIV-positive patients (9). Studies using bedside inoculation of pleural fluid showed higher sensitivity of mycobacterial culture than that observed with laboratory inoculation (7, 8, 11). Due to the heterogeneity of these studies, it is still unclear how much the diagnostic yield is increased in effusion culture in an HIV-uninfected patient population with the implementation of the liquid culture system as compared to solid media. The approximately 40% yield of effusion culture was comparable to the values reported in previous studies in consideration of an HIV-uninfected patient population and using the laboratory inoculation in this study.
The major limitations of using liquid culture in respiratory specimens were higher contamination rate and higher isolation of NTM, which often has an ambiguous clinical significance. In addition, some of the strains grew only on the solid media. Due to the above reasons, supplemental solid media have been recommended to maximize culture sensitivity. In this study, no contamination or NTM isolation was observed on solid or liquid media from pleural fluid. Pleural effusion samples are sterile, and therefore, less likely to be contaminated than respiratory samples. In addition, one of the effusion samples grew only on the Ogawa medium. The combined use of liquid and solid media increased the sensitivity only by a further 1% when compared to that observed using the liquid medium alone. Although supplemental solid media showed little effect on maximizing sensitivities in effusion culture in this study, further large-scale studies are required in this regard.
Another interesting finding of this study is the fact that a higher percentage of PMNL is an independent predictor of culture-positive effusion. This finding is consistent with those of previous studies using solid or liquid media (10, 13, 14). It has been suggested that PMNL-rich effusion appears in early phase, when the immune system has not yet developed an effective defense against the bacillus (14, 15). The proportion of PMNL-dominant effusion was reported to be about 10% of TB pleurisy (16), which was related to higher mortality mainly because of delayed diagnosis (13, 17). If TB pleurisy is suspected but unlikely due to a higher percentage of PMNL, the collection of sputum and pleural fluid samples for mycobacterial culture should be encouraged.
This study has inherent limitations because of the small sample size and retrospective study design. Therefore, further studies to validate our findings are warranted. Further, HIV-ELISA tests in this study were only performed on 24 patients. Since Korea is a low-HIV burden country with a reported prevalence below 0.1% (18), the HIV-ELISA test is not a routine test for patients with suspected tuberculosis. None of the patients included in this study were diagnosed with HIV infection during the follow-up period.
In summary, when compared with solid media, an automated liquid culture system could generate approximately twice as high yields and fast results in effusion culture in HIV-uninfected patients. Such diagnostic improvements could facilitate adequate patient treatment, and potentially diminish the morbidity and mortality resulting from TB pleurisy. Supplemental solid media appears to have a limited impact in maximizing sensitivity in effusion culture; however, further studies are warranted.
Footnotes
This study was supported by Research Institute for Convergence of Biomedical Science and Technology Grant (30-2015-007), Pusan National University Yangsan Hospital, Korea.
DISCLOSURE: The authors have no conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conception and coordination of the study: Lee BH, Jeon D, Kim YS. Design of ethical issues: Lee SE, Lee SJ. Acquisition of data: Yoon SH, Yeo HJ, Kim DW. Data review: Lee BH, Cho WH, Lee SJ, Jeon D. Statistical analysis: Lee SE. Manuscript preparation: Lee BH, Yoon SH, Jeon D. Manuscript approval: all authors.
References
- 1.Cruciani M, Scarparo C, Malena M, Bosco O, Serpelloni G, Mengoli C. Meta-analysis of BACTEC MGIT 960 and BACTEC 460 TB, with or without solid media, for detection of mycobacteria. J Clin Microbiol. 2004;42:2321–2325. doi: 10.1128/JCM.42.5.2321-2325.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dinnes J, Deeks J, Kunst H, Gibson A, Cummins E, Waugh N, Drobniewski F, Lalvani A. A systematic review of rapid diagnostic tests for the detection of tuberculosis infection. Health Technol Assess. 2007;11:1–196. doi: 10.3310/hta11030. [DOI] [PubMed] [Google Scholar]
- 3.Anthony RM, Cobelens FG, Gebhard A, Klatser PR, Lumb R, Rüsch-Gerdes S, van Soolingen D. Liquid culture for Mycobacterium tuberculosis: proceed, but with caution. Int J Tuberc Lung Dis. 2009;13:1051–1053. [PubMed] [Google Scholar]
- 4.Tenover FC, Crawford JT, Huebner RE, Geiter LJ, Horsburgh CR, Jr, Good RC. The resurgence of tuberculosis: is your laboratory ready? J Clin Microbiol. 1993;31:767–770. doi: 10.1128/jcm.31.4.767-770.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Canadian Thoracic Society. Canadian Tuberculosis Standards, 7th Edition. Can Respir J. 2013;20:1A–173A. [Google Scholar]
- 6.Gopi A, Madhavan SM, Sharma SK, Sahn SA. Diagnosis and treatment of tuberculous pleural effusion in 2006. Chest. 2007;131:880–889. doi: 10.1378/chest.06-2063. [DOI] [PubMed] [Google Scholar]
- 7.Maartens G, Bateman ED. Tuberculous pleural effusions: increased culture yield with bedside inoculation of pleural fluid and poor diagnostic value of adenosine deaminase. Thorax. 1991;46:96–99. doi: 10.1136/thx.46.2.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng AF, Tai VH, Li MS, Chan CH, Wong CF, Yew WW, Hui M, Chan CY, Lee JC. Improved recovery of Mycobacterium tuberculosis from pleural aspirates: bedside inoculation, heparinized containers and liquid culture media. Scand J Infect Dis. 1999;31:485–487. doi: 10.1080/00365549950164012. [DOI] [PubMed] [Google Scholar]
- 9.Luzze H, Elliott AM, Joloba ML, Odida M, Oweka-Onyee J, Nakiyingi J, Quigley M, Hirsch C, Mugerwa RD, Okwera A, et al. Evaluation of suspected tuberculous pleurisy: clinical and diagnostic findings in HIV-1-positive and HIV-negative adults in Uganda. Int J Tuberc Lung Dis. 2001;5:746–753. [PubMed] [Google Scholar]
- 10.Ruan SY, Chuang YC, Wang JY, Lin JW, Chien JY, Huang CT, Kuo YW, Lee LN, Yu CJ. Revisiting tuberculous pleurisy: pleural fluid characteristics and diagnostic yield of mycobacterial culture in an endemic area. Thorax. 2012;67:822–827. doi: 10.1136/thoraxjnl-2011-201363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.von Groote-Bidlingmaier F, Koegelenberg CF, Bolliger CT, Chung PK, Rautenbach C, Wasserman E, Bernasconi M, Friedrich SO, Diacon AH. The yield of different pleural fluid volumes for Mycobacterium tuberculosis culture. Thorax. 2013;68:290–291. doi: 10.1136/thoraxjnl-2012-202338. [DOI] [PubMed] [Google Scholar]
- 12.Kwon JS, Cha SI, Jeon KN, Kim YJ, Kim EJ, Kim CH, Park JY, Jung TH. Factors influencing residual pleural opacity in tuberculous pleural effusion. J Korean Med Sci. 2008;23:616–620. doi: 10.3346/jkms.2008.23.4.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu SF, Liu JW, Lin MC. Characteristics of patients suffering from tuberculous pleuritis with pleural effusion culture positive and negative for Mycobacterium tuberculosis, and risk factors for fatality. Int J Tuberc Lung Dis. 2005;9:111–115. [PubMed] [Google Scholar]
- 14.Bielsa S, Palma R, Pardina M, Esquerda A, Light RW, Porcel JM. Comparison of polymorphonuclear- and lymphocyte-rich tuberculous pleural effusions. Int J Tuberc Lung Dis. 2013;17:85–89. doi: 10.5588/ijtld.12.0236. [DOI] [PubMed] [Google Scholar]
- 15.Antony VB, Sahn SA, Antony AC, Repine JE. Bacillus Calmette-Guérin-stimulated neutrophils release chemotaxins for monocytes in rabbit pleural spaces and in vitro. J Clin Invest. 1985;76:1514–1521. doi: 10.1172/JCI112131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jolobe OM. Atypical tuberculous pleural effusions. Eur J Intern Med. 2011;22:456–459. doi: 10.1016/j.ejim.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 17.Lin MT, Wang JY, Yu CJ, Lee LN, Yang PC TAMI Group. Mycobacterium tuberculosis and polymorphonuclear pleural effusion: incidence and clinical pointers. Respir Med. 2009;103:820–826. doi: 10.1016/j.rmed.2008.12.023. [DOI] [PubMed] [Google Scholar]
- 18.Korea Centers for Disease Control and Prevention. Annual report on the notified HIV/AIDS in Korea, 2013. Seoul: Korea Center for Disease Control & Prevention; 2014. [Google Scholar]


