Abstract
The frequency and extent of the existence of a familial suicide prevention plan may differ across cultures. The aim of this work was, therefore, to determine how common it was for families to develop a suicide prevention plan and to compare the main measures used by families with and without such a plan, after an attempt to commit suicide was made by a member of a family living in a rural area of Korea. On the basis of the presence or absence of a familial suicide prevention plan, we compared 50 recruited families that were divided into 2 groups, with Group A (31 families) employing a familial suicide prevention plan after a suicide attempt by a family member, and Group B (19 families) not doing so. The strategy that was employed most frequently to prevent a reoccurrence among both populations was promoting communication among family members, followed by seeking psychological counseling and/or psychiatric treatment. Contrary to our expectation, the economic burden from medical treatment after a suicide attempt did not influence the establishment of a familial suicide prevention plan. It is a pressing social issue that 38% (19 of 50) of families in this study did not employ a familial suicide prevention plan, even after a family member had attempted suicide. Regional suicide prevention centers and/or health authorities should pay particular attention to these patients and their families.
Keywords: Suicide; Suicide, Attempted, Family; Suicide Prevention; Suicide Prevention Plan
INTRODUCTION
Suicide is one of the most common human tragedies, spanning all ages and countries around the world. (1, 2) It is an act of self-directed violence, infringing upon the dignity of human beings. Because of the remarkable growth in industry in Korea over the last several decades, there have been a number of sudden societal changes, for example, a shift from an agrarian to an industrial society, from a Confucian to a Westernized culture, and from a multigenerational family structure to smaller or single-person households. As a result, suicide has been ranked as the fourth most common cause of death in Korea. Therefore, suicide prevention is a project of national importance in Korea; (3, 4) however, suicide prevention is easier said than done, and this responsibility should be shared among the family of the patient, (5) regional health authorities, and the patients themselves where possible.
The aim of this work was to determine how many families have developed a suicide prevention plan, and to identify the main strategies used to prevent future suicide attempts after a member of a family in rural Korea has attempted suicide.
MATERIALS AND METHODS
Study subjects
Between January and September 2014, 150 individuals who had attempted suicide by ingesting chemical poison were admitted to the Institute of Pesticide Poisoning at the Soonchunhyang University Cheonan Hospital, a tertiary referral center for toxicology patients that is located in a rural area of Korea. Sixty of those 150 individuals who attempted suicide survived. In the study sample, we excluded families from which no family member visited the patient, those who were indifferent to the patient, and/or those who were not willing to respond to our questions. On the basis of these criteria, 50 of the 60 individuals who had attempted suicide and their families were enrolled in this study. The chemical poison taken to commit suicide was pesticide in 39 cases (comprising herbicide in 24 cases, pesticide in 13 cases, fungicide in 1 case, and surfactant in 1 case), and sleeping pills and/or psychiatric drugs in 11 cases.
Patient characteristics, including age, sex, income, amount of poison ingested, time lag after ingestion, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, hospitalization fee, and number of days spent in the hospital, are summarized in Table 1. Upon admission, patients received standardized medical emergency procedures. Patients who arrived at the emergency room within 2 hr of ingestion of a poison received gastric lavage. Hemodialysis or hemoperfusion was initiated according to the characteristics of the chemical (6, 7). The survey, shown in Table 2, was carried out just before patients were discharged, when the symptoms of the poison they had ingested had lapsed and the patients felt healthy.
Table 1. Comparison between Groups A and B in terms of demographics, income, amount of pesticide or drug ingested, time lag after ingestion, APACHE II score, and number of days spent in hospital.
| Parameters | Group A (plan prepared) | Group B (plan not prepared) | P value |
|---|---|---|---|
| Age (yr) | 50.4 ± 14.3 | 54.3 ± 12.1 | 0.325 |
| Body weight (kg) | 62.1 ± 10.5 | 65.9 ± 12.7 | 0.261 |
| Education (yr) | 9.7 ± 3.5 | 10.3 ± 3.0 | 0.531 |
| Monthly income (US$) | 290 ± 550 | 1,550 ± 1,340 | 0.295 |
| Total hospitalization fee (US$) | 5,280 ± 5,030 | 4,130 ± 2,010 | 0.346 |
| Patient's own expense (US$) | 1,960 ± 1,910 | 1,330 ± 7,650 | 0.178 |
| Number of tablets taken | 55.0 ± 44.4 | 36.7 ± 11.5 | 0.511 |
| Amount ingested (mL) | 152.2 ± 94.1 | 156.9 ± 119.8 | 0.892 |
| Time lag after ingestion (hr) | 8.1 ± 9.3 | 3.9 ± 1.7 | 0.067 |
| APACHE II score | 8.6 ± 6.9 | 6.5 ± 5.6 | 0.286 |
| ICU hospital days | 6.0 ± 6.8 | 4.3 ± 2.3 | 0.292 |
| Total days spent in hospital | 11.1 ± 9.7 | 7.7 ± 3.1 | 0.152 |
Number of tablets taken reflects the number of tablet ingested at once to commit suicide. Amount ingested is the volume of pesticide ingested to commit suicide.
Table 2. Survey items.
| Targets | Questions |
|---|---|
| Patients | 1. Do you perceive any change in your relationships with your family after your suicide attempt? |
| 2. If you experience the same situation in the future, will you attempt suicide again? | |
| 3. Did you plan suicide before making this attempt? | |
| 4. Did you attempt suicide to frighten or draw attention from your family? | |
| 5. Do you believe that someone would have helped, if you had asked them? | |
| 6. Do you regret your suicide attempt? | |
| 7. What do you think is the most effective measure for suicide prevention? | |
| 8. Do you have medical history of mental illness, including insomnia? | |
| Family member of the patient | 1. Who is/are the responsible guardian/s of the patient, among the family members? |
| 2. What do you think is the cause of your family member's suicide attempt? | |
| 3. Has there been any change in the relationships among your family members after the patient's suicide attempt? | |
| 4. Did your family feel there was a lack of familial preventative action before the patient attempted suicide? | |
| 5. Will the patient's medical bills be a financial burden on the family? | |
| 6. Who will pay for the medical expenses incurred by the suicide attempt? | |
| 7. What do you think is the most effective measure for suicide prevention? |
Group A comprised families with a suicide prevention plan in place, and Group B comprised those without such a plan. The following parameters were compared between Groups A and B: age, sex, number of children, family living situation, employment status, possibility of repeated attempt of suicide, whether the attempt was premeditated or accidental, whether the attempt was made in order to alert other family members to the patient's problem, whether the patient thought that he or she would not have attempted suicide if there had been familial help available, whether there had been a change in the relationships between the patient and other family members after the suicide attempt, whether the patient regretted their suicide attempt, whether the patient had previously been diagnosed with a mental illness (including insomnia), presence or absence of responsible guardians in the home environment, whether or not the family had been aware of the lack of preventive action by the family with regard to suicide.
Analytical parameters
Parameters obtained from the responsible family members were: change in the relationships among family members after the suicide attempt, whether the medical bills were a financial burden on the family, the person who was responsible for payment of the medical bills, the family's planned measure(s) to prevent a reoccurrence, and the seriousness of the toxic symptoms of the patient while in the hospital. We interviewed the family member who appeared most concerned about the patient's clinical status, and/or the patient's most frequent visitor among the family members.
The seriousness of the toxic symptoms was evaluated using the Workload Management System for Critical Care Nurses (WMSCN) (8) and APACHE II scores. (9) According to the workload of the intensive care unit nurse, the seriousness of the toxic symptoms was classified using the WMSCN as either Class 1 (patient able to care for themselves, minimal degree of nursing care required), Class 2 (moderate degree of nursing care required), Class 3 (acute degree of nursing required), Class 4 (intensive degree of nursing required), Class 5 (continual nursing required), or Class 6 (intensive nursing from 2 or more nurses required).
The APACHE II score was calculated from the patient's age and the following 12 routine physiological measurements: PaO2, body temperature, blood pressure, arterial pH, heart rate, respiratory rate, Na+ and K+ in serum, creatinine, hematocrit, white blood cell count, and Glasgow Coma Scale score. These measurements were taken during the first 24 hr after admission.
Statistics
Data presented are means and standard deviations (SD) unless otherwise marked. A chi-square test was used to compare categorical variables and continuous variables were compared using a t-test, with the significance threshold set at 0.05. SPSS version 17.0 for Windows was used for all analyses.
Ethics statement
The study was approved by the institutional review board of Soonchunhyang Cheonan Hospital (IRB No. 201502002). Informed consent was waived by the board.
RESULTS
Demographics
There was no difference in the number of males and females between Group A (M:F=15:16) and Group B (M:F=14:5), P=0.071. According to their family living situation, Groups A and B were divided into the following 3 subgroups: a) living with spouse, b) living alone, or c) living with others, such as a sibling. There was no difference in the living situation between Groups A (a:b:c =16:8:7) and B (a:b:c=12:4:3), P=0.788.
Groups A and B were divided into the following 3 subgroups according to their number of children: a (0), b (1-2), or c (>3). There was no difference in the number of children between Groups A (a:b:c=6:13:12) and B (a:b:c=3:12:4), P=0.342.
There was no significant difference in the cause of the suicide attempt between the groups, with 11 within Group A reporting depression; 7, economic problems; and 13, conflict among family members, and within Group B, 9 reported depression; 4, economic problems; and 6, conflict among family members, P=0.705.
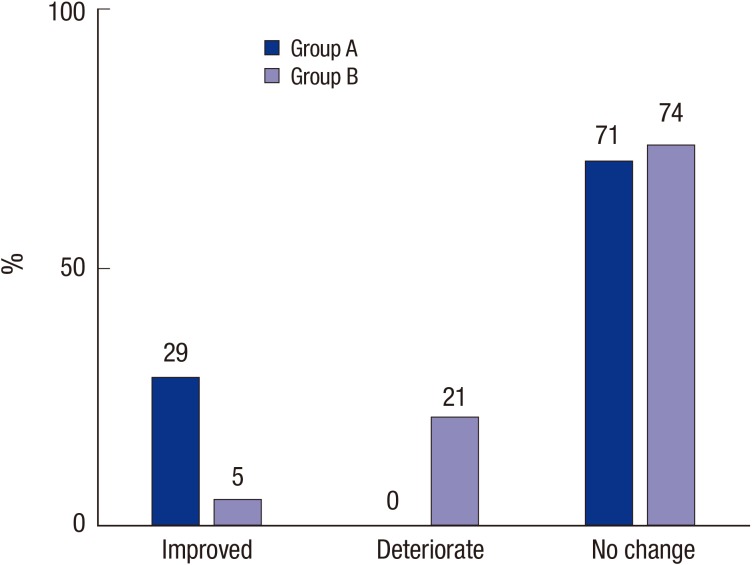
Results from patient interviews
The ratio of families whose relationships improved, deteriorated, or showed no change was 9:0:22, respectively, within Group A, and 1:4:14, respectively, within Group B, P=0.007 (Fig. 1). In Group A, the number of patients who repeatedly attempted suicide was 9 of 31, while the number was 8 of 19 for Group B, P=0.260. In Group A, the ratio of planned to impulsive suicide attempts was 12:19 and 12:7 in Group B, P=0.082. The number of patients who attempted suicide to alert other family members to their problem was 6 of 31 for Group A, and 3 of 19 for Group B, P=0.532. Twenty of 31 patients in Group A regretted their suicide attempt and in Group B, 10 of 19 patients did, P=0.295. The number of patients who had symptoms of a mental illness, including insomnia, was 15 of 31 in Group A and 6 of 19 in Group B, P=0.192. Employment status was higher in Group B (14 of 19 patients) than in Group A (14 of 31 patients), P=0.045.
Fig. 1. Change in the relationships among family members after the patient's suicide attempt. Note that the relationships among families improved in Group A, while they deteriorated in Group B, P=0.007.
Results from family member interviews
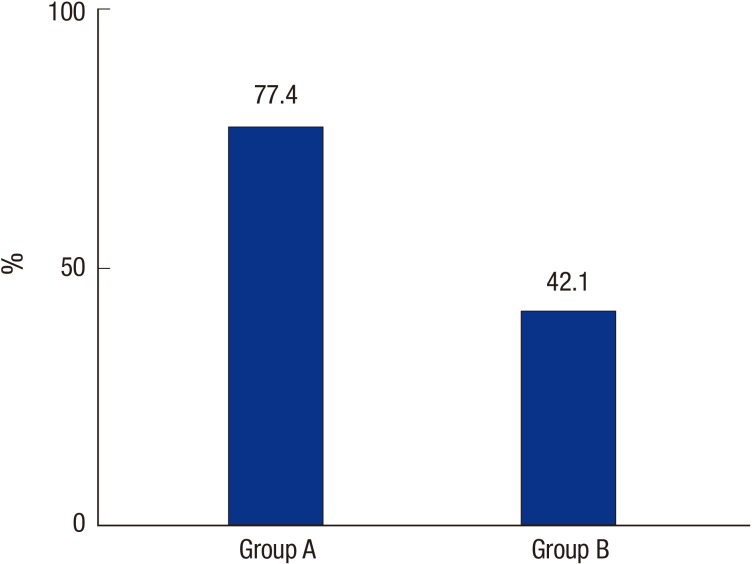
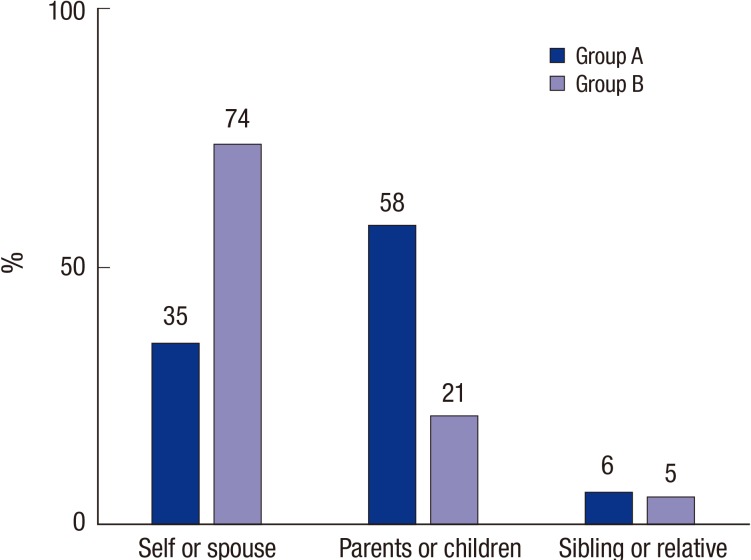
Of 31 patients in Group A, 17 thought that he or she would not have attempted suicide if there had been familial help. This also applied to 10 of the 19 patients in Group B, P=0.555. The ratio of people in the responsible guardian groups was spouse: parents or children: sibling or other relatives 12:11:8 in Group A and 14:4:1 in Group B, P=0.79. The number of families whose relationships improved, versus those whose relationship deteriorated or showed no change was 10:21 in Group A and 2:17 in Group B, P=0.077. The proportion of families that were aware of the lack of preventive action was greater in Group A (24 of 31) than in Group B (8 of 19), P=0.013 (Fig. 2). The patient's medical bills were a financial burden for 22 of 31 families for Group A and 12 of 19 families for Group B, P=0.394. The ratio of patients themselves or a spouse: parents or children: sibling or other relatives who paid the bills was 11:18:2 in Group A and 14:4:1 in Group B, P=0.016 (Fig. 3).
Fig. 2. Proportion of families that were aware of a lack of familial preventative action. The proportion of families that were aware of the lack of preventative action was greater in Group A (24 out of 31) than in Group B (8 of 19), P=0.013.
Fig. 3. The person who paid the hospital expenses. In Group A, the parents and/or children were most often responsible for bearing the patient's medical costs, while in Group B, it was often the patients themselves or their spouses (P<0.016).
The patient's plan to prevent a reoccurrence of the suicide attempt included promoting communication within the family, unsure about what the best plan is, and receiving psychological counseling and/or psychiatric treatment. The number in each category was 8:17:6 in Group A and 5:8:6 in Group B, P=0.600.
The family's plan to prevent a reoccurrence of the suicide attempt included promoting communication within the family, no idea of the best plan, and psychological counseling and/or psychiatric treatment. The number in each category was 11:1:7 in Group A and 16:2:13 in Group B, P=0.895.
The number of patients whose WMSCN score was greater than 3 was 20 of 31 in Group A and 13 of 19 in Group B, P=0.513. The APACHE II score was 6.5±5.6 in Group A and 8.6±6.9 in Group B, P=0.286.
DISCUSSION
Any person who attempts suicide causes problems in the management of public health. (10, 11) First, a person with a past history of a suicide attempt is classified as high risk for future suicide. They attract public attention and in some cases become a burden on family and friends, with relatives needing to manage the cost of medical expenses. Furthermore, relatives may feel guilty or ashamed of having a history of suicide in the family. The consequences of an unsuccessful suicide attempt may be manifold, depending on one's cultural and economic background, and the situation may worsen or improve as time passes. Therefore, gaining insight from the family of the patient at discharge is an effective means to prevent other suicide attempts. We observed that 31 of 50 families (Group A) in our sample had a familial suicide prevention plan in place. Interestingly, the answers from the Group B (no familial suicide prevention plan) participants were very similar to those of the Group A participants. Promotion of communication between family members was the leading measure for suicide prevention planned in both Groups A and B, so what makes it so hard to put the plan into practice in Group B?
The characteristics of the families in Group A include unconditional love between family members and being far-sighted enough to provide care for the patients. Contrary to our expectations, the number of patients putting an economic burden on their families was greater in Group A than in Group B (70.9% vs. 60.3%). This suggests that economic difficulties do not detract from the love between family members. The number of unemployed patients was greater in Group A than in Group B. This further indicates that employment status does not affect familial love. We cannot explain why the love between family members was lower in Group B. Perhaps the patients' persistent illness reduced the family members' tolerance, or the familial environment was too stressful. We believe that suicide prevention centers should primarily target families without a suicide prevention plan (i.e., those in Group B).
There was also no significant difference between Groups A and B in terms of the number of children the patient had, living situation, the cause of the suicide attempt, whether or not the patient had made previous attempts at suicide, whether the suicide attempt was planned or spontaneous, the identity of the responsible guardians, or the seriousness of the toxic symptoms of the patient after admission to the hospital. The issue of chemical causes of suicide attempts is beyond the scope of this article. However, we did find that the ingestion of pesticide was the most common method of suicide, and there was no difference in the number of patients who ingested pesticide between Groups A and B.
In summary, signs that we perceive as being promising in regard to the future of patients with a familial suicide prevention plan are as follows: improved relationships among family members after the suicide attempt and family members' regret about the lack of preventive action.
Footnotes
This work was carried out with the support of the "Cooperative Research Program for Agriculture Science & Technology Development (Project No. PJ01083201)" Rural Development Administration, Republic of Korea.
DISCLOSURE: The authors declare no conflicts of interest, and the authors are responsible for the content and writing of the article.
AUTHOR CONTRIBUTION: Study conception and design: Gil H. Data acquisition: Cho HD, Kim NY. Data analysis and interpretation: Jeong D. Drafting and revision: Hong S. Final approval: all authors.
References
- 1.Clayton PJ. Suicide. Psychiatr Clin North Am. 1985;8:203–214. [PubMed] [Google Scholar]
- 2.Sudak HS, Ford AB, Rushforth NB. Adolescent suicide: an overview. Am J Psychother. 1984;38:350–363. doi: 10.1176/appi.psychotherapy.1984.38.3.350. [DOI] [PubMed] [Google Scholar]
- 3.Lim AY, Lee AR, Hatim A, Tian-Mei S, Liu CY, Jeon HJ, Udomratn P, Bautista D, Chan E, Liu SI, et al. Clinical and sociodemographic correlates of suicidality in patients with major depressive disorder from six Asian countries. BMC Psychiatry. 2014;14:37. doi: 10.1186/1471-244X-14-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chung JH, Moon K, Kim do H, Min JW, Kim TH, Hwang HJ. Suicidal ideation and suicide attempts among diabetes mellitus: the Korea National Health and Nutrition Examination Survey (KNHANES IV, V) from 2007 to 2012. J Psychosom Res. 2014;77:457–461. doi: 10.1016/j.jpsychores.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 5.Goldfarb S, Tarver WL, Sen B. Family structure and risk behaviors: the role of the family meal in assessing likelihood of adolescent risk behaviors. Psychol Res Behav Manag. 2014;7:53–66. doi: 10.2147/PRBM.S40461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gil HW, Kim SJ, Yang JO, Lee EY, Hong SY. Clinical outcome of hemoperfusion in poisoned patients. Blood Purif. 2010;30:84–88. doi: 10.1159/000318585. [DOI] [PubMed] [Google Scholar]
- 7.Seok SJ, Kim JH, Gil HW, Yang JO, Lee EY, Hong SY. Comparison of patients starting hemodialysis with those underwent hemodialysis 15 years ago at the same dialysis center in Korea. Korean J Intern Med. 2010;25:188–194. doi: 10.3904/kjim.2010.25.2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Italian Multicenter Group of ICU research (GIRTI) Time oriented score system (TOSS): a method for direct and quantitative assessment of nursing workload for ICU patients. Intensive Care Med. 1991;17:340–345. doi: 10.1007/BF01716193. [DOI] [PubMed] [Google Scholar]
- 9.Waters M, Nightingale P, Edwards JD. A critical study of the APACHE II scoring system using earlier data collection. Arch Emerg Med. 1990;7:16–20. doi: 10.1136/emj.7.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Di Thiene D, Alexanderson K, Tinghög P, La Torre G, Mittendorfer-Rutz E. Suicide among first-generation and second-generation immigrants in Sweden: association with labour market marginalisation and morbidity. J Epidemiol Community Health. 2015;69:467–473. doi: 10.1136/jech-2014-204648. [DOI] [PubMed] [Google Scholar]
- 11.Farrell CT, Bolland JM, Cockerham WC. The role of social support and social context on the incidence of attempted suicide among adolescents living in extremely impoverished communities. J Adolesc Health. 2015;56:59–65. doi: 10.1016/j.jadohealth.2014.08.015. [DOI] [PubMed] [Google Scholar]