Abstract
Background
Over the last 20 years, numerous research articles and clinical guidelines aimed at optimizing resource utilization for emergency department (ED) patients presenting with syncope have been published.
Hypothesis
We hypothesized there would be temporal trends in syncope-related ED visits and associated trends in imaging, hospital admissions, and diagnostic frequencies.
Methods
The ED component of National Hospital Ambulatory Medical Care Survey was analyzed from 2001 through 2010, comprising over 358,000 visits (representing an estimated 1.18 billion visits nationally). We selected ED visits with a reason for visit of syncope or fainting and calculated nationally representative weighted estimates for prevalence of such visits, and associated rates of advanced imaging utilization and admission. For admitted patients from 2005 to 2010, the most frequent hospital discharge diagnoses were tabulated.
Results
During the study period, there were over 3,500 actual ED visits (representing 11.9 million visits nationally) related to syncope, representing roughly 1% of all ED visits. Admission rates for syncope patients ranged from 27% to 35% and showed no significant downward trend (p=0.1). Advanced imaging rates increased from about 21% to 45% and showed a significant upward trend (p < 0.001). For admitted patients, the most common hospital discharge diagnosis was the symptomatic diagnosis of “syncope and collapse” (36.4%).
Conclusions
Despite substantial efforts by medical researchers and professional societies, resource utilization associated with ED visits for syncope appears to have actually increased. There have been no apparent improvements in diagnostic yield for admissions. Novel strategies may be needed to change practice patterns for such patients.
Keywords: Syncope, Emergency Medicine, Hospital Admission, Diagnostic Imaging
1.1 INTRODUCTION
Syncope, defined as a transient loss of consciousness, is a common and challenging complaint in the emergency department (ED). From 1992 to 2000, there were an estimated 740,000 ED visits per year in the United States (US) related to syncope. Approximately one third of such visits resulted in hospital admission, though rates vary widely depending on the practice setting.[1] Such admissions often confer limited diagnostic or therapeutic yield [2, 3] as many patients leave the hospital with a diagnosis identical to their chief complaint. As a result, there has also been increasing pressure on emergency physicians from federal agencies via Recovery Audit Contractors to reduce admissions for syncope.
Over the last two decades, there has been a substantial amount of clinical research devoted to improving the diagnostic evaluation and risk-stratification of ED syncope patients. [4–6] Multiple professional societies have published guidelines to standardize clinical practice and reduce unnecessary services for patients with syncope.[3, 7–9] More recently, as part of the “Choosing Wisely” campaign to reduce low-value activities, neuroimaging for syncope without neurological deficits was identified as commonly overused service.
It is important to understand how recent research and clinical guidelines have made an impact on ED practice patterns for syncope. A change in diagnostic imaging and admission rates could provide information as to whether such efforts have been effective at reducing resource utilization.
Our primary objective was to describe national trends in ED visits, advanced diagnostic imaging and admission rates from 2001–2010 for patients presenting with syncope. Secondly, we sought to describe the diagnoses of admitted patients from 2005–2010 (years for which discharge diagnoses were available).
1.2 METHODS
1.2.1 Study Design and Population
We conducted an analysis of the ED portion of the National Hospital Ambulatory Medical Care Survey (NHAMCS) ED database for 2001 through 2010. The NHAMCS is a nationally representative sample of U.S. ED visits obtained by the National Center for Health Statistics (NCHS) branch of the Centers for Disease Control and Prevention. The data abstraction forms include information pertaining to the sampled visit including demographic information, 3 patient “reason for visit” fields, ED tests performed, 3 International Classification of Diseases, 9th Revision (ICD-9) ED discharge diagnoses, and starting in 2005, 1 hospital discharge diagnosis. Further data collection methods and sampling design are described in detail on the NCHS Web site (http://www.cdc.gov/nchs). This study was exempted from review by our institutional review board. The funding organization had no involvement in the conduct or reporting of this study.
Our study sample consisted of all ED visits where any of the three patient “Reasons For Visit” included “1030.0, fainting (syncope); includes blacking out, passing out, fainting spells; excludes unconsciousness” based on coding from the Reason for Visit Classification for Ambulatory Care, a standardized sourcebook used in NCHS studies. For frequency of visits, admission rates, and advanced imaging estimates, data from 2001–2010 were included. NHAMCS started collecting data on hospital discharge diagnoses in 2005, so relevant analyses were conducting using data from 2005–2010.
1.2.2 Outcome Measures
Our main outcome measures were prevalence of ED visits for syncope, rates of hospital admission, rates of advanced imaging, and hospital discharge diagnostic frequencies for admitted patients, by year. We defined hospital admission as a disposition of “admit to hospital” or “transferred to outside hospital”. We defined hospital discharge diagnoses based on ICD-9 codes. Admissions with a discharge diagnosis of “780.2 Syncope and collapse” were considered non-diagnostic, since presumably no specific etiology for syncope was determined during the in-patient stay. The ten most frequent hospital discharge diagnoses were compiled. Diagnoses were combined when sufficient similarities were felt to exist, e.g. “Anemia, unspecified” and “Anemia due to chronic blood loss”, as well as “convulsions, not elsewhere classified” and “epilepsy, not otherwise specified”. Cardiac dysrhythmias were also grouped into one category. This category included “cardiac dysrhythmias, not otherwise specified/not elsewhere classified”, “paroxysmal ventricular tachycardia”, “sinoatrial node dysfunction”, “atrioventricular block, not otherwise specified”, “atrioventricular block complete”, “atrial fibrillation” and “atrial flutter”.
To create these groupings, two investigators, aware of the study hypothesis, (MAP, HKK) independently categorized each diagnosis, with a senior investigator serving as arbitrator in the event of disagreement. Advanced diagnostic imaging was defined as receipt of either magnetic resonance imaging (MRI) or computed tomography (CT) scan during the ED visit. We also analyzed data on ultrasound utilization for syncope visits. The NHAMCS data form varies from year to year. From 2001–2004, the survey collected information on MRI or CT without differentiating between the two. From 2005–2010, CT and MRI were recorded separately. From 2007–2010, CT Head was recorded separately from “Any CT”. For years 2007–2008, MRI Head was recorded separately from “Any MRI”. For simplicity, we examined trends for receipt of any advanced imaging (any CT or MRI) over the 10-year period. The dataset does not allow for differentiation of various types of ultrasounds, e.g. cardiac versus lower extremity studies. Thus data for “any ultrasound” are presented.
1.2.3 Data Analysis
We performed all statistical analyses with STATA (version 13.1; StataCorp LP, College Station, TX), Sudaan (version 11.0; RTI International, Research Triangle Park, North Carolina) and SAS (version 9.3; SAS Institute, Cary, North Carolina) using standard methods for analyzing survey-weighted data. Using the SVY (survey) command from STATA, which takes into account the multilevel sample design to produce national estimates, we determined point estimates and 95% confidence intervals (95%CI) of basic demographic characteristics as well as imaging and admission rates for all ED visits containing a “Reason For Visit” of syncope. We additionally tabulated frequencies of hospital discharge diagnoses. To assess for changes in advanced imaging, admission, and non-diagnostic admission rates over the study period, we performed survey-weighted trend analysis using weighted least squares regression with SAS. We used Sudaan to calculate standard errors and 95% confidence intervals accounting for complex survey design. Nationally representative estimates were determined using NCHS-assigned patient weights. Estimates based on < 30 sample records were excluded as they are considered to be unreliable due to high relative standard errors. We did not perform any imputation other than what was done centrally by NCHS.
1.3 RESULTS
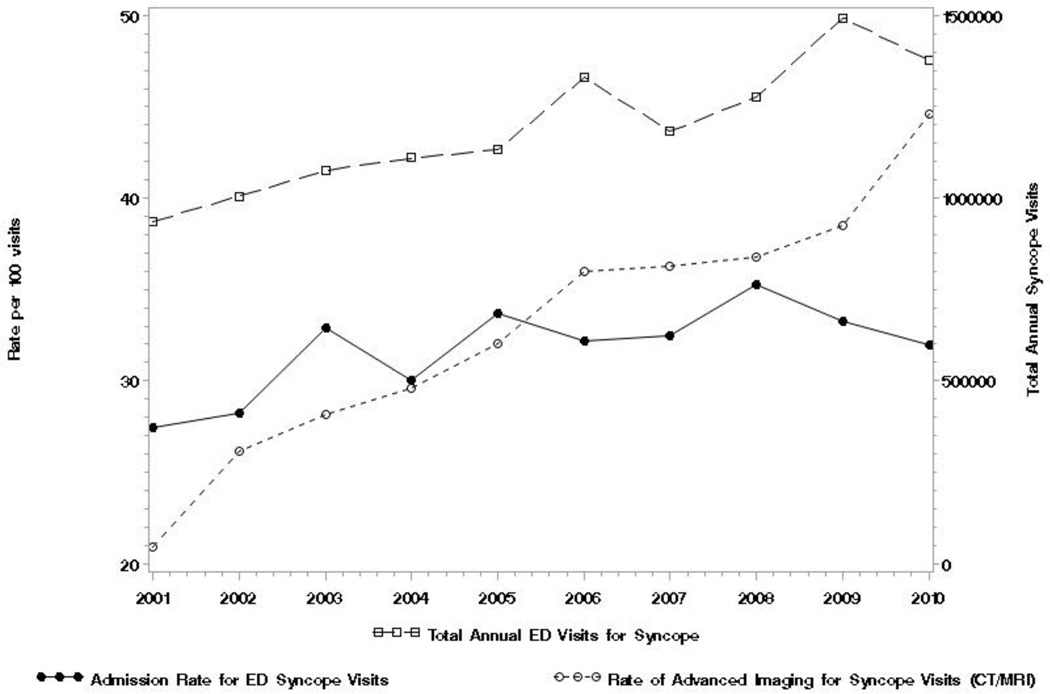
From 2001–2010, there were 3,549 actual ED visits in the NHAMCS database related to syncope, representing an estimated 11.9 million visits nationally. This corresponds to roughly 1% [95%CI 0.9% to 1.1%] of all ED visits during that time period. The proportion of syncope visits as a percentage of total ED visits remained constant over the 10-year period ranging from 0.9% to 1.1%. The overall admission rate was 32% [95%CI 28% to 36%], increasing from 27.4% in 2001 to nearly 32% in 2010 (See table 1). Admission rates exhibited no significant trend over the 10-year study period (p=0.11 for 10-year trend). The rates of advanced imaging (CT or MRI) showed a clear upward trend over the 10-year study period, increasing from 20.9% [95%CI 16.7% to 25.9%] in 2001 to 44.6% [95%CI 38.7% to 50.1%] in 2010 (p < 0.0001 for 10-year trend). [See Figure 1] Looking at rates of head CTs alone shows a similar trend from 2007–2010, increasing from 29.8% to 39.3% over 4 years (data not shown) (p < 0.001 for 4-year trend). Rates of ultrasound utilization for syncope visits also showed an upward trend increasing from 1.26% in 2001 to 3.4% in 2010 (data not shown).
Table 1.
Emergency Department Visits for Syncope in the United States, 2001–2010
| ED Visits | ED Visits | Estimated ED Visits per 100 Population |
Rate Difference |
P-value for trend |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unweighted | Weighted | (95% Confidence Interval) | ||||||||
| 2001 | 2010 | 2001 | 2010 | 2001 | 95% CI | 2010 | 95% CI | (2001–2010) | ||
| Total Syncope Visits | 304 | 362 | 936,000 | 1,376,000 | 0.87 | (0.77, 0.99) |
1.06 | (0.92, 1.2) |
−0.19 | 0.019 |
| Visits by age | ||||||||||
| Under 18 | 30 | 34 | 97,000 | 131,000 | 10.4 | (6.96, 15.3) |
9.49 | (6.1, 14.5) |
0.91 | 0.66 |
| 18–44 | 111 | 122 | 332,000 | 450,000 | 35.5 | (29.31, 42.2) |
32.7 | (26.6, 39.4) |
2.81 | 0.023 |
| 45–64 | 60 | 93 | 188,000 | 363,000 | 20.1 | (14.84, 26.5) |
26.4 | (20.9, 32.7) |
−6.31 | 0.024 |
| Over 65 | 103 | 113 | 319,000 | 433,000 | 34.0 | (27.59, 41.1) |
31.5 | (25.7, 37.8) |
2.59 | 0.49 |
| Total | 304 | 362 | 936,000 | 1,376,000 | ||||||
| Visits by Sex | ||||||||||
| Male | 128 | 149 | 395,000 | 500,000 | 42.2 | (36.19, 48.5) |
36.35 | (29.5, 43.8) |
5.89 | 0.87 |
| Female | 176 | 213 | 540,000 | 876,000 | 57.8 | (51.48, 63.8) |
63.65 | (56.2, 70.5) |
−5.89 | |
| Visits by Ethnicity | ||||||||||
| Hispanic | 20 | 38 | NR | 145,000 | NR | NR | 10.5 | (3.1, 9.5) | NR | NR |
| Non-Hispanic | 226 | 324 | 701,000 | 1,231,000 | 74.9 | (67.0, 81.5) |
89.5 | (85.0, 92.7) |
−14.56 | 0.18 |
| Visits by Race | ||||||||||
| White | 241 | 282 | 75,000 | 1,094,000 | 80.1 | (74.22, 84.9) |
79.54 | (73.2, 84.6) |
0.56 | 0.48 |
| Black | 54 | 62 | 152,000 | 244,000 | 16.2 | (12.2, 21.2) |
17.77 | (12.9, 24.0) |
−1.53 | 0.6 |
| Other | 9 | 18 | NR | NR | NR | NR | NR | NR | NR | NR |
| Advanced Imaging* | ||||||||||
| Yes | 68 | 152 | 196,000 | 614,000 | 20.9 | (16.7, 25.9) |
44.59 | (38.7, 50.7) |
−23.69 | <.0001 |
| No | 236 | 210 | 740,000 | 762,000 | 79.1 | (74.1, 83.3) |
55.41 | (49.3, 61.3) |
23.69 | |
| Hospital Admission | ||||||||||
| Yes | 89 | 103 | 257,000 | 440,000 | 27.4 | (22.0, 33.6) |
31.94 | (25.2, 39.5) |
−4.52 | 0.11 |
| No | 215 | 259 | 680,000 | 936,000 | 72.6 | (66.4, 78.0) |
68.06 | (60.5, 74.8) |
4.52 | |
| Total | 304 | 362 | 936,000 | 1,376,000 | ||||||
| Non-diagnostic admission | 2005 | 2010 | 2005 | 2010 | 2005 | 95% CI | 2010 | 95% CI | (2010–2005) | |
| Yes | 37 | 37 | 119,000 | 169,000 | 31.2 | (21.6, 42.8) |
38.4 | (25.0, 54.0) |
−7.2 | 0.87 |
| No | 32 | 16 | 112,000 | 67,000 | 29.4 | (21.0, 39.5) |
15.29 (8.6, 25.6) |
14.1 | ||
| Total | 115 | 103 | 382,000 | 236,000 | ||||||
NR: Not reliable due to insufficient sample size (<30)
Computed Tomography or Magnetic Resonance Imaging
Figure 1.
Trends in Resource Utilization for U.S. Emergency Department Visits for Syncope, 2001–2010.
 Total Annual ED Visits for Syncope
Total Annual ED Visits for Syncope
 Admission Rate for ED Syncope Visits
Admission Rate for ED Syncope Visits
 Rate of Advance Imaging for Syncope Visits (CT/MRI)
Rate of Advance Imaging for Syncope Visits (CT/MRI)
The most common ICD-9 hospital discharge diagnosis was “780.2 syncope and collapse,” which was the primary diagnosis in 36.4% [95%CI 29.3% to 43.4%] of all admissions. This value was 31.3% [95%CI 21.6% to 42.8%] in 2005 and 38.4% [95%CI 25.0% to 54.0%] in 2010, peaking at 41.7% [95%CI 31.6 to 52.6%] in 2006. There was no statistically significant trend from 2005–2010 (p=0.87 for 5-year trend). Cardiac dysrhythmias were the second most common hospital discharge diagnosis, comprised primarily of “atrial fibrillation” (1.5%) and “paroxysmal ventricular tachycardia” (0.86%).
1.4 DISCUSSION
We attempted to assess the effects of recent research and clinical guidelines by analyzing advanced imaging and admission rates for syncope in US EDs from 2001–2010. Our data show that overall ED visits have increased over the last 10 years, consistent with other studies [10]. ED visits for syncope have as well, but the proportion (about 1%) has remained stable. This represents prevalence slightly greater than previously reported from the same dataset in the previous decade: 0.77% [95%CI 0.69% to 0.85%][1]. Admissions rates for syncope visits have not decreased from 2001–2010 and have remained stable overall as compared with those from 1992–2000 (32%) [1]. The rate of non-diagnostic admissions remained persistently high across the 10-year study period, with over one third of admitted patients leaving the hospital with a diagnosis identical to their chief complaint. These findings should be validated using other national datasets. This figure may be even higher if looking at only patients who do not receive a diagnosis in the ED yet were still admitted for further diagnostic testing and/or monitoring. The finding that convulsions/epilepsy (2.2%) was the fourth most common hospital discharge diagnosis is likely due to the inherent challenges of clinically differentiating, in the acute setting, between a syncopal event and a seizure. Ultrasound utilization, although not as common as CT/MRI, also increased during the study period. The rate of advanced imaging (CT or MRI) during ED syncope visits increased significantly during the 10-year study period, consistent with prior studies of trends in ED imaging utilization. Using NAHMCS data for injury-related visits, Korley et al. found and three-fold increase in CT/MRI use from 1998–2007 [11]. Similarly, Kocher et al. found that CT use in the ED increased over three-fold across all reasons for visit over the same time period [12]. Our data suggest that the current, myriad risk-stratification tools and clinical guidelines have not significantly impacted resource utilization surrounding ED syncope. This may be due to a number of reasons: due to the challenges of dissemination, ED clinicians may be unaware of these tools, or may choose to use their own clinical judgment instead. Alternatively, perhaps not enough time has elapsed for these instruments and guidelines to be adopted by ED clinicians. Another possibility is that clinical management may be predominantly guided by other factors such as medico-legal concerns, financial incentives and “customary practice”. The current culture among many physicians of “zero-tolerance” for missed adverse events due to acts of omission, although well-intentioned, may actually be detrimental to patients in aggregate and represent an inappropriate use of resources. Other strategies may be needed to improve resource utilization in this context, such as increased use of syncope observation unit protocols, outpatient ambulatory cardiac monitoring without admission, and shared decision-making for intermediate risk patients who have not had a serious condition revealed during their ED evaluation. All of the above approaches would depend on accurate identification of intermediate risk patients, which would require the development of novel, reliable, well-validated risk-stratification tools.
1.4.1 LIMITATIONS
The results of our study are dependent on the quality of the NHAMCS data itself, which may suffer from miscoding and errors in data entry [13]. The fact that NHAMCS contains only one single hospital discharge diagnosis per admission means that key secondary diagnoses are not available to help in the diagnostic categorization and may have affected our results. Similarly, the case definition of syncope may include ED visits where the chief complaint was actually chest pain, dyspnea or headache, with syncope as a secondary complaint. However, we feel that syncope is a cardinal complaint that often supersedes most associated symptoms in guiding the clinical management of the ED patient. The vast majority of ED visits in our sample had syncope or collapse as the primary reason for visit. Importantly, NHAMCS is the largest and only nationally representative dataset that can provide epidemiological data on emergency conditions in the US. Finally, our diagnostic summary data is based on ICD-9 codes, which can lack specificity and accuracy.
1.5 CONCLUSIONS
According to our data on ED visits for syncope, admission rates have remained stable while advanced imaging rates have increased from 2001–2010. There have been no apparent improvements in diagnostic yield for admissions. Novel strategies may be needed to change ED practice patterns for such patients.
Table 2.
Survey-Weighted Most Common Hospital Discharge Diagnoses for Patients Admitted after an Emergency Department visit for Syncope, 2005–2010
| Diagnosis | Weighted Count | Percent |
|---|---|---|
| Syncope and collapse | 93,900 | 36.4% |
| Cardiac dysrhythmias | 11,100 | 4.3% |
| Dehydration | 6,700 | 2.6% |
| Convulsions/Epilepsy, not elsewhere classified | 5,700 | 2.2% |
| Pneumonia, organism not otherwise specified | 4,300 | 1.7% |
| Anemia/Chronic blood loss, not otherwise specified | 4,100 | 1.6% |
| Chest pain, not otherwise specified | 2,800 | 1.1% |
| Gastrointestinal hemorrhage/Hematemesis | 2,800 | 1.1% |
| Dizziness and giddiness | 2,500 | 1.0% |
| Coronary atherosclerosis of unspecified type | 2,500 | 1.0% |
Acknowledgments
Funding Sources
This work was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number 5K12 HL109005-03 (Dr. Probst) and Award Number R01 HL111033 (Dr. Sun). Dr. Kanzaria was supported by the Robert Wood Johnson Foundation Clinical Scholars Program and the US Department of Veterans Affairs. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, US Department of Veterans Affairs, or the Robert Wood Johnson Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
There are no other conflicts of interest.
Contributor Information
Marc A. Probst, Email: mprobst@gmail.com.
Hemal K. Kanzaria, Email: hemal.kanzaria@gmail.com.
Misato Gbedemah, Email: misato.gbedemah@mountsinai.org.
Lynne D. Richardson, Email: lynne.richardson@mountsinai.org.
Benjamin C. Sun, Email: sunb@ohsu.edu.
REFERENCES
- 1.Sun BC, Emond JA, Camargo CA., Jr Characteristics and admission patterns of patients presenting with syncope to US emergency departments, 1992–2000. Acad Emerg Med : official journal of the Society for Academic Emergency Medicine. 2004;11:1029–1034. doi: 10.1197/j.aem.2004.05.032. [DOI] [PubMed] [Google Scholar]
- 2.Crane SD. Risk stratification of patients with syncope in an accident and emergency department. Emerg Med J. 2002;19:23–27. doi: 10.1136/emj.19.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Linzer M, Yang EH, Estes NA, 3rd, Wang P, Vorperian VR, Kapoor WN. Diagnosing syncope. Part 1: Value of history, physical examination, and electrocardiography. Clinical Efficacy Assessment Project of the American College of Physicians. Ann Intern Med. 1997;126:989–996. doi: 10.7326/0003-4819-126-12-199706150-00012. [DOI] [PubMed] [Google Scholar]
- 4.Colivicchi F, Ammirati F, Melina D, Guido V, Imperoli G, Santini M. Development and prospective validation of a risk stratification system for patients with syncope in the emergency department: the OESIL risk score. Euro Heart J. 2003;24:811–819. doi: 10.1016/s0195-668x(02)00827-8. [DOI] [PubMed] [Google Scholar]
- 5.Quinn JV, Stiell IG, McDermott DA, Sellers KL, Kohn MA, Wells GA. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004;43:224–232. doi: 10.1016/s0196-0644(03)00823-0. [DOI] [PubMed] [Google Scholar]
- 6.Reed MJ, Newby DE, Coull AJ, Prescott RJ, Jacques KG, Gray AJ. The ROSE (risk stratification of syncope in the emergency department) study. J Am Coll Card. 2010;55:713–721. doi: 10.1016/j.jacc.2009.09.049. [DOI] [PubMed] [Google Scholar]
- 7.Huff JS, Decker WW, Quinn JV, Perron AD, Napoli AM, Peeters S, et al. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with syncope. Ann Emerg Med. 2007;49:431–444. doi: 10.1016/j.annemergmed.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Strickberger SA, Benson DW, Biaggioni I, Callans DJ, Cohen MI, Ellenbogen KA, et al. AHA/ACCF Scientific Statement on the evaluation of syncope: from the American Heart Association Councils on Clinical Cardiology, Cardiovascular Nursing, Cardiovascular Disease in the Young, and Stroke, and the Quality of Care and Outcomes Research Interdisciplinary Working Group; and the American College of Cardiology Foundation: in collaboration with the Heart Rhythm Society: endorsed by the American Autonomic Society. Circulation. 2006;113:316–327. doi: 10.1161/CIRCULATIONAHA.105.170274. [DOI] [PubMed] [Google Scholar]
- 9.Moya A, Sutton R, Ammirati F, Blanc JJ, Brignole M, Dahm JB, et al. Guidelines for the diagnosis and management of syncope (version 2009) Euro Heart J. 2009;30:2631–2671. doi: 10.1093/eurheartj/ehp298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA. 2010 Aug 11;304(6):664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998–2007. JAMA. 2010 Oct 6;304(13):1465–1471. doi: 10.1001/jama.2010.1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kocher KE, Meurer WJ, Fazel R, Scott PA, Krumholz HM, Nallamothu BK. National trends in use of computed tomography in the emergency department. Ann Emerg Med. 2011 Nov;58(5):452–462. doi: 10.1016/j.annemergmed.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 13.Cooper RJ. NHAMCS: does it hold up to scrutiny? Ann of Emerg Med. 2012 Dec;60(6):722–725. doi: 10.1016/j.annemergmed.2012.10.013. [DOI] [PubMed] [Google Scholar]