Description
A 69-year-old man, with no significant medical history, presented with weakness, fatigue and melena 4 days after knee surgery. This was not associated with nausea, vomiting or any abdominal discomfort. His medications included aspirin, statin and non-steroidal anti-inflammatory drugs (NSAIDs) for the knee pain. His blood work revealed normocytic normochromic anaemia with haemoglobin of 6 g/dL. Physical examination and the rest of his blood chemistries were unremarkable.
Upper endoscopy showed mild oesophagitis, a few 1–2 mm non-bleeding ulcers on gastric mucosa and 10–12 cm long big pedunculated duodenal polyp with friable mucosa and active bleeding (figures 1–3). Endoscopically, partial polypectomy was performed owing to the size of the polyp. Biopsy of the partially resected polyp showed Brunner’s gland hamartoma with low-grade dysplasia (figures 4 and 5). Therefore, laparoscopic duodenal polyp resection and pyloroplasty was performed for complete removal of the tumour.
Figure 1.
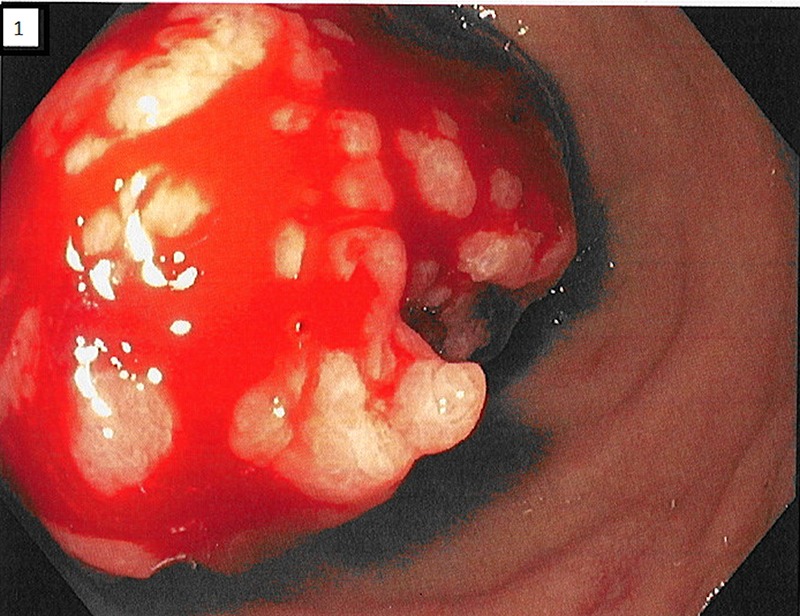
Endoscopic images of a giant Brunner's gland hamartoma.
Figure 2.
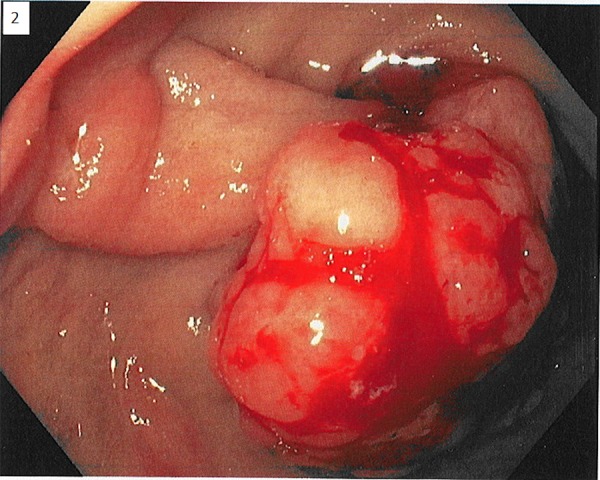
Endoscopic images of a giant Brunner's gland hamartoma.
Figure 3.
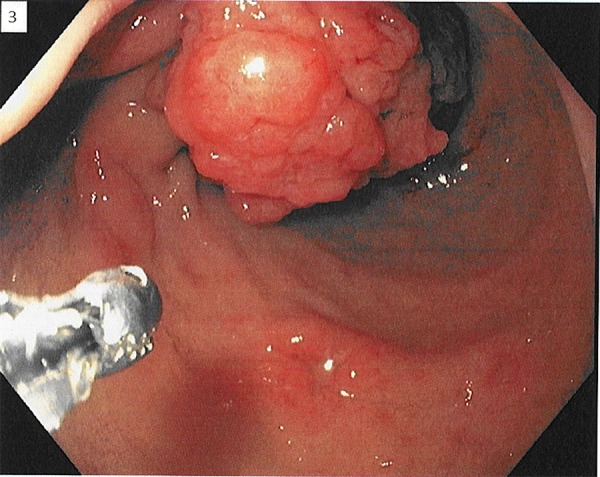
Endoscopic images of a giant Brunner's gland hamartoma.
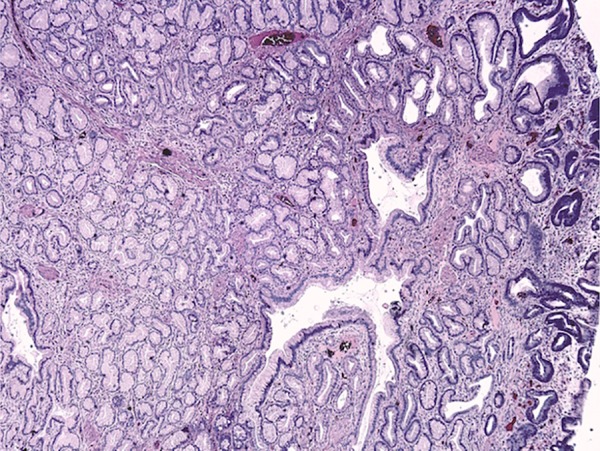
Figure 4.
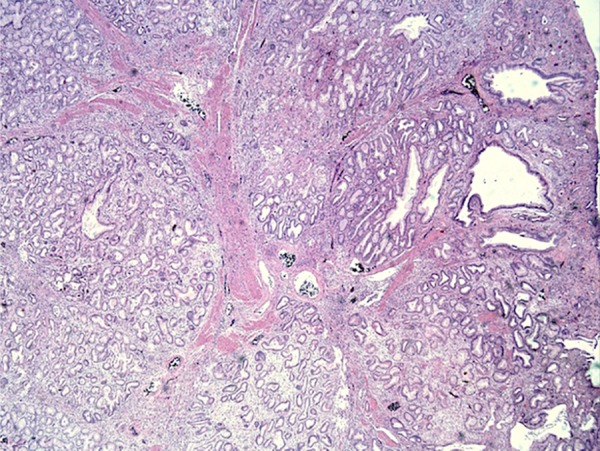
Histopathological image of polyp with admixture of fibromuscular and adipose tissue within and surrounding lobules of Brunner glands, few of which are cystically dilated (H&E; ×400).
Figure 5.
Histopathological image of Brunner's gland hamartoma dysplasia: focus of glands revealing nuclei with mild hyperchromaticity, increased nuclear—cytoplasmic ratio and pseudostratification suggestive of low-grade dysplasia (H&E; ×400).
Brunner's gland adenoma, also known as Brunneroma or polypoid hamartoma, is a rare, benign, proliferative lesion arising from the acinotubular mucin-secreting submucosal glands of duodenum and accounts for 10.6% of benign tumours of the duodenum. The lesions demonstrate an admixture of normal tissues such as Brunner's glands, ducts, adipose and lymphoid tissues. Usually they are asymptomatic, but can present in the form of gastrointestinal bleed or obstruction. Precipitating factors involve any sort of mucosal irritation, including drugs such as NSAIDs.1 Endoscopic resection is the most cost-effective approach of resection.2 These tumours have a malignant potential. Surgical resection through laparoscopic approach or laparotomy is needed for complete resection in case endoscopic resection is unsuccessful and if malignancy is suspected.3
Learning points.
Brunner's gland hamartoma is a rare cause of first time gastrointestinal bleed, especially in the seventh decade of life.
An increasing incidence of such lesions is seen in patients taking drugs irritating the gastrointestinal mucosa, especially non-steroidal anti-inflammatory drugs.
These hamartomas do have a malignant potential, especially seen in tumours >2 cm in size.
It can be resected endoscopically, but large hamartomas or hamartomas with suspected malignant transformation may require surgical resection.
Footnotes
Twitter: Follow Abhinav Agrawal at @re_innervated
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Levine JA, Burgart LJ, Batts KP et al. Brunner's gland hamartomas: clinical presentation and pathological features of 27 cases. Am J Gastroenterol 1995;90:290–4. [PubMed] [Google Scholar]
- 2.Gao YP, Zhu JS, Zheng WJ. Brunner's gland adenoma of duodenum: a case report and literature review. Word J Gastroenterol 2004;10:2616–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart ZA, Hruban RH, Fishman EF et al. Surgical management of giant Brunner's gland hamartoma: case report and literature review. World J Surg Oncol 2009;7:68 doi:10.1186/1477-7819-7-68 [DOI] [PMC free article] [PubMed] [Google Scholar]


