Abstract
A 47-year-old woman presented with a history of vague abdominal pain for several years, which worsened over the past 2 months, with pain more prominent in the right upper quadrant. She also had a history of peptic ulcer disease. The ultrasound scan of right upper quadrant revealed normal gallbladder and oesophagogastroduodenoscopy was unremarkable. A 99mtechnetium labelled hepato iminodiacetic acid (HIDA) scan with cholecystokinin provocation demonstrated a decreased gallbladder ejection fraction (EF) of 32%. On this basis, the patient was diagnosed with biliary dyskinesia and underwent an elective laparoscopic cholecystectomy. Histopathological analysis revealed chronic cholecystitis with Cystoisospora belli identified in the gallbladder wall. Cystoisospora has been identified to cause an opportunistic acalculous cholecystitis among immunocompromised hosts, especially those with AIDS. This is the first case report of chronic cholecystitis due to C. belli in an immunocompetent patient.
Background
Cystoisospora belli (formerly known as Isospora belli) is a spore-forming intestinal protozoan parasite, and along with Cryptosporidium and Cyclospora, is an important intestinal pathogen in immunocompetent and immunocompromised hosts. Cystoisospora is a well-known cause of traveller's diarrhoea worldwide, and it is also known to rarely cause opportunistic cholecystitis and/or cholangiopathy in immunocompromised patients, in particular those with AIDS. To date, there is only one case report of chronic biliary cystoisosporiasis, but none of chronic cholecystitis in an immunocompetent patient. We report the case of a 47-year-old immunocompetent woman with chronic cholecystitis due to C. belli and summarise the literature on biliary cystoisosporal infections.
Case presentation
A 47-year-old Caucasian woman presented with a 2-month history of worsening right upper quadrant pain, on a background of pain that had been intermittently present for several years. The pain started without any preceding factors, was burning in character, typically lasted for less than 1 min and occasionally radiated to the right subscapular area. There was no relationship between meals and the pain. The patient denied any associated symptoms, including fever, nausea, vomiting, acid reflux, diarrhoea, back pain, dysuria, haematuria, or any signs of icterus. Furthermore, she had regular bowel movements and a normal appetite. She also denied recent travel or sick contacts.
Investigations
As the patient had intermittently experienced this pain for several years, she had previously undergone oesophagogastroduodenoscopy prior to the laparoscopic cholecystectomy, and a biopsy of the gastric mucosa demonstrated mild inactive chronic gastritis without evidence of helicobacter infection. An ultrasound scan of the right upper quadrant revealed normal appearances of the gallbladder and biliary tree, and a hepatic function panel was essentially normal except for a mildly elevated total bilirubin level. Complete blood count and other relevant laboratory work revealed the following: white cell count 6.5 k/µL, haemoglobin 14.3 g/dL, haematocrit 41.7%, platelet 284 k/µL, creatinine 0.79 mg/dL, blood urea nitrogen 9 mg/dL and glucose 88 mg/dL. A 99mtechnetium labelled hepatoiminodiacetic acid (HIDA) scan with cholecystokinin provocation was ordered and demonstrated a decreased gallbladder ejection fraction of 32%, consistent with a diagnosis of biliary dyskinesia.
Differential diagnosis
Bacterial/fungal or parasitic or obstructive cholecystitis.
Treatment
As the symptoms and HIDA scan result were consistent with biliary dyskinesia, after discussing the benefits and risks related to the procedure, the patient underwent laparoscopic cholecystectomy. The procedure was performed without complication and she was discharged home the same day. The specimen was sent to the histopathology department for further analysis.
Outcome and follow-up
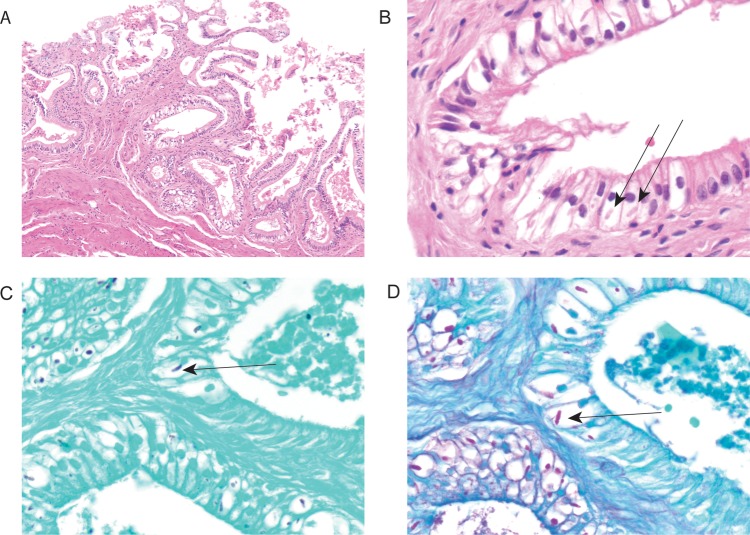
The gallbladder measured 7.7×1.9×1.2 cm with a smooth serosal surface. The wall thickness ranged from 0.2 to 0.4 cm, and no calculi were present within it. Sections from the gallbladder demonstrated mild chronic cholecystitis. Additionally, there were subnuclear vacuoles in some of the epithelial cells, which contained oval eosinophilic inclusions (figure 1A, B) that were highlighted by a Grocott’s methenamine silver stain (figure 1C), and a periodic acid-Schiff/fungal stain (figure 1D). The morphological features of these inclusions were consistent with Cystoisospora infection.
Figure 1.
Cystoisospora belli infection of gallbladder epithelium. The gallbladder demonstrates features of chronic cholecystitis with thickened muscularis and reactive epithelial changes (A) (original magnification—×200). There was only minimal chronic lymphocytic inflammation and only rare scattered eosinophils were found. There was no acute inflammation seen. The H&E stained slide demonstrates several infected epithelial cells with parasitophorous vacuoles meronts with merozoites (B), which are highlighted by Grocott's methenamine silver stain (C) and periodic acid-Schiff/fungus (D) (original magnification—×600) special stains. The arrows highlight the C. belli organisms. No oocytes or evidence of sexual reproduction was seen.
Postoperatively, the patient's symptom resolved. Although her stool was examined and showed no evidence of parasites or oocysts postoperatively, she was treated with trimethoprime-sulfamethoxazole empirically for the Cystoisospora infection. Her HIV status was also checked given the relationship between Cystoisospora infection and immunosuppression, and returned negative.
Discussion
C. belli is an obligate intracellular protozoan pathogen that infects the small intestinal epithelium and causes traveller's diarrhoea.1 Cystoisospora is endemic in tropical and subtropical climates and in developing areas, including South America, Africa, the Middle East and Southeast Asia.2 Symptoms are usually self-limiting in immunocompetent patients although diarrhoea and oocyst shedding may persist for several weeks after symptom resolution.1 On the other hand, in the USA, Cystoisospora is an infrequent but important opportunistic pathogen that causes severe chronic diarrhoea, malabsorption and even death in immunocompromised patients.3 In immunocompromised patients, typically those with HIV, symptoms and oocyst shedding can continue indefinitely without treatment and recurrence is also common in these populations.4
Typically, infection is diagnosed by detecting Cystoisospora oocysts that are typically 23–36 by 12–17 µm in faecal specimens. Multiple stool samples may be required for diagnosis as some patients intermittently shed the parasite.5 While oocysts can be identified in routine parasite examination in case of severe infection, the diagnosis may require acid-fast staining or specific fluorescent techniques in mild or moderate cases.6 A PCR assay has been developed for detecting Cystoisospora DNA in faecal samples. If the stool examination is not diagnostic, parasites may also be detected in duodenal aspirates or within intestinal biopsy tissue examined under light microscopy. Walther and Topazian7 have reported that PCR is a useful tool to detect Cystoisospora DNA in formalin-fixed, paraffin-embedded tissues, however, the test is not available for clinical testing in the USA.
The drug of choice for treatment is trimethoprim-sulfamethoxazole or pyrimethamine for patients allergic to sulfonamides. In HIV/AIDS patients with recurrent or persistent infection, the antibiotic therapy must be continued indefinitely.3 In immunocompetent patients, treatment leads to eradication of the parasite from the gastrointestinal tract.
C. belli is occasionally associated with extraintestinal infection, such as within mesenteric or mediastinal lymph nodes, the spleen, liver or biliary system, in immunocompromised patients.3 Extraintestinal infections probably occur as a result of spread through lymphatic channels, however, the incidence of extraintestinal infection is unclear.
Biliary infection produces two syndromes.6 The first is a sclerosing cholangtitis-type lesion that causes progressive, irregular obstruction and dilation of the intrahepatic and extrahepatic bile ducts. Patients typically have right upper quadrant pain and elevated alkaline phosphatase level.8 The second is acalculous cholecystitis caused by infection of the gallbladder wall, which commonly occurs in patients with AIDS.9
In the case presented, the patient had chronic cholecystitis with C. belli without clear evidence of intestinal cystoisosporasis as there was no history of chronic diarrhoea, malabsorption or weight loss, and no history suggestive of chronic damage to the biliary tree. Furthermore, she did not have any signs or symptoms of immunodeficiency and she was tested negative for HIV antibody at the time of other blood investigations. In addition, she denied any known contact with individuals who had experienced a cystoisosporal infection. While there have been a few case reports of acalculous cholecystitis with Cystoisospora in patients with AIDS, only one case of chronic biliary Isosporiasis in an immunocompetent patient has been reported.10 In the case in question, Bialek et al10 reported that chronic damage to the biliary tree, due to a previous history of severe cholangitis secondary to liver fluke infection, made the patient susceptible to biliary cystoisosporasis in a patient who was immunocompetent. There was no evidence of such an infection in the current case.
Learning points.
Cystoisospora belli is a well-known cause of traveller's diarrhoea worldwide, and it is also known to rarely cause acalculous cholecystitis and/or cholangiopathy among immunocompromised patients.
This is the first case report of chronic cholecystitis with C. belli in an immunocompetent patient.
The drug of choice for treatment is trimethoprim-sulfamethoxazole or pyrimethamine for patients allergic to sulfonamides.
Footnotes
Contributors: HT is the first author. GM-S supervised HT. GAF assisted HT to gather the patient information. MC assisted from a pathology perspective.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.DeHovitz JA, Pape JW, Boncy M et al. Clinical manifestations and therapy of Isospora belli infection in patients with the acquired immunodeficiency syndrome. New Engl J Med 1986;315:87–90. 10.1056/NEJM198607103150203 [DOI] [PubMed] [Google Scholar]
- 2.Rudrapatna JS, Kumar V, Sridhar H. Intestinal parasitic infections in patients with malignancy. J Diarrhoeal Dis Res 1997;17:71–4. [PubMed] [Google Scholar]
- 3.Chawla R, Ichhpujani RL. Enteric spore-forming opportunistic parasites in HIV/AIDS. Trop Parasitol 2010;1:15–19. 10.4103/0000-0205.72112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mathur M, Verma A, Makwana G et al. Study of opportunistic intestinal parasitic infections in human immunodeficiency virus/acquired immunodeficiency syndrome patients. J Global Infect Dis 2013;5:164–7. 10.4103/0974-777X.122012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaplan JE, Benson C, Holmes KK et al. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep 2009;58:1–207. [PubMed] [Google Scholar]
- 6.Goodgame RW. Understanding intestinal spore-forming protozoa: cryptosporidia, microsporidia, isospora, and cyclospora. Ann Intern Med 1996;124:429–41. 10.7326/0003-4819-124-4-199602150-00008 [DOI] [PubMed] [Google Scholar]
- 7.Walther Z, Topazian M. Isospora cholangiopathy: case study with histologic characterization and molecular confirmation. Hum Pathol 2009;40:1342–6. 10.1016/j.humpath.2009.01.020 [DOI] [PubMed] [Google Scholar]
- 8.Lagrange-Xélot M, Porcher R, Sarfati C et al. Isosporiasis in patients with HIV infection in the highly active antiretroviral therapy era in France. HIV Med 2008;9:126–30. 10.1111/j.1468-1293.2007.00530.x [DOI] [PubMed] [Google Scholar]
- 9.French A, Beaudet L, Benator D et al. Cholecystectomy in patients with AIDS: clinicopathologic correlations in 107 cases. Clin Infect Dis 1995;21:852–8. 10.1093/clinids/21.4.852 [DOI] [PubMed] [Google Scholar]
- 10.Bialek R, Overkamp D, Retting I et al. Nitazoxanide treatment failure in chronic isosporiasis. Am J Trop Med Hyg 2001;65:94–5. [DOI] [PubMed] [Google Scholar]