Summary
Low-dose exposures to common environmental chemicals that are deemed safe individually may be combining to instigate carcinogenesis, thereby contributing to the incidence of cancer. This risk may be overlooked by current regulatory practices and needs to be vigorously investigated.
Abstract
Lifestyle factors are responsible for a considerable portion of cancer incidence worldwide, but credible estimates from the World Health Organization and the International Agency for Research on Cancer (IARC) suggest that the fraction of cancers attributable to toxic environmental exposures is between 7% and 19%. To explore the hypothesis that low-dose exposures to mixtures of chemicals in the environment may be combining to contribute to environmental carcinogenesis, we reviewed 11 hallmark phenotypes of cancer, multiple priority target sites for disruption in each area and prototypical chemical disruptors for all targets, this included dose-response characterizations, evidence of low-dose effects and cross-hallmark effects for all targets and chemicals. In total, 85 examples of chemicals were reviewed for actions on key pathways/mechanisms related to carcinogenesis. Only 15% (13/85) were found to have evidence of a dose-response threshold, whereas 59% (50/85) exerted low-dose effects. No dose-response information was found for the remaining 26% (22/85). Our analysis suggests that the cumulative effects of individual (non-carcinogenic) chemicals acting on different pathways, and a variety of related systems, organs, tissues and cells could plausibly conspire to produce carcinogenic synergies. Additional basic research on carcinogenesis and research focused on low-dose effects of chemical mixtures needs to be rigorously pursued before the merits of this hypothesis can be further advanced. However, the structure of the World Health Organization International Programme on Chemical Safety ‘Mode of Action’ framework should be revisited as it has inherent weaknesses that are not fully aligned with our current understanding of cancer biology.
Introduction
Cancer is a burden on humanity and among the leading causes of morbidity and mortality worldwide, with ~14 million new cases and 8.2 million cancer-related deaths in 2012 (1). In general, both genetic and environmental factors play a role in an individual’s cancer susceptibility (2,3), so there has been a long-standing emphasis on avoidable ‘lifestyle’ factors (i.e. those that can be modified to reduce the incidence of the disease) and a parallel focus on exogenous chemical exposures (e.g. agricultural, occupational and so on) (4). But advances in our understanding of the complexity of cancer biology have resulted in serious critiques of current risk assessment practices related to exogenous exposures (5) along with calls for an expanded focus on research that will allow us to evaluate the (potentially carcinogenic) effects of in-utero exposures and low-level exposures to combinations of chemicals that occur throughout our lifetime (6,7).
The 2008–09 President’s Cancer Panel Annual Report in the USA (8) opined that the ‘true burden of environmentally induced cancer has been grossly underestimated’ (7), whereas Parkin et al. (9) estimated in a British study that the fraction of cancer that can now be attributed to both lifestyle and environmental factors is only 43% (i.e. the underlying cause of 57% of all cancers is still unexplained). However, an expanded focus on research that will allow us to evaluate the (potentially carcinogenic) contribution of low-level exposures to combinations of chemicals that occur in utero and throughout our lifetime is not a trivial undertaking.
First of all, the number of chemicals to which we are exposed is substantial, and many have not been adequately tested. Christiani (6) cited increased and persistently high incidence rates of various cancers and called on the National Institutes of Health to expand their investigation of environmental causes of cancer noting that ‘Massive gaps exist in toxicologic data, even in the case of widely used synthetic chemicals. Only about 50% of chemicals classified by the Environmental Protection Agency (EPA) as “high production volume” have undergone even minimal testing for carcinogenicity’. But even though the incidence of cancer attributable to environmental exposures has not been definitively established (3,6), it remains an important focus of our prevention efforts [with credible estimates from the World Health Organization [WHO] and the IARC suggesting that the fraction of cancers attributable to toxic environmental exposures is between 7% and 19%] (10,11).
The possibility that unanticipated low-dose effects (LDE) are also a factor in environmental carcinogenesis further complicates matters. Vandenberg et al. (12) recently reviewed the accumulating evidence that points to LDE that occur at levels that are well below those used for traditional toxicological studies. This review identified several hundred examples of non-monotonic dose-response relationships (i.e. examples where the relationship between dose and effect is complex and the slope of the curve changes sign—from positive to negative or vice versa—somewhere within the range of doses examined). Drawing on the known actions of natural hormones and selected environmental chemicals examined in cell cultures, animals and epidemiology, the authors emphasized that when non-monotonic dose-response curves occur, the effects of low doses cannot be predicted by the effects observed at high doses. However, endocrine disruption research to this point has been aimed primarily at chemicals that disrupt developmental processes through a relatively small subset of hormones (e.g. estrogen, androgen, thyroid and so on), and thus, many commonly encountered chemicals have not been tested at all for these effects (at environmentally relevant dose levels) and, to date, mechanisms that relate to carcinogenesis have typically not been the focus of these studies.
Generally for chemical risk assessments, toxicity studies are conducted with individual chemicals in animal models based on regulatory test guidelines [e.g. Organization for Economic Co-operation and Development (OECD) test guidelines (13)] with a key objective of providing a dose-response assessment that estimates a point of departure [traditionally the no-observed-adverse-effect level or the lowest-observed-adverse-effect level (LOAEL)], which is then used to extrapolate the quantity of substance above which adverse effects can be expected in humans. The no-observed-adverse-effect level, combined with uncertainty factors (which acknowledge gaps in the available data), is then used to establish safety criteria for human exposure. However, in order to be able to detect adverse effects utilizing classical toxicological endpoints, dose selection has historically involved the use of high dose levels and appropriate dose level spacing to obtain the LOAEL or no-observed-adverse-effect level thresholds. Techniques such as linear extrapolation or benchmark dose modeling (14) are then employed to predict safety margins for low-dose exposures. This approach to risk assessment depends on the use of appropriate and sensitive endpoints, and on valid assumptions for extrapolation estimates (e.g. dose-response linearity) and calculations, and on the existence of thresholds of effects (15–17). So when the potential for non-linear dose-response relationships is combined with the possibility of synergism between and amongst low doses of mixtures of individual chemicals in the environment, it appears plausible that chemicals that are not individually carcinogenic may be capable of producing carcinogenic synergies that would be missed using current risk assessment practices.
The complex nature of the biology of cancer adds another layer of complexity for risk assessment. In a landmark paper in 1979, Ames (18) noted that damage to DNA appeared to be a major cause of most cancers and suggested that natural chemicals in the human diet and the tens of thousands of man-made chemicals that had been introduced into the environment in the preceding decades be tested for their ability to damage DNA. In doing so, he sketched out the difficulty of dealing with complex chemical mixtures and he proposed the use of rapid mutagenicity assays to identify environmental mutagens and carcinogens. The strategy was sound at the time, but it led to a scientific and regulatory emphasis on ‘mutagens as carcinogens’, whereas the issue of complex environmental mixtures, or carcinogens that are not mutagens, was never vigorously pursued. Instead, what followed was an international quest to find individual chemicals and a few well-defined mixtures (e.g. diesel exhaust) that could be shown to be ‘complete’ carcinogens (i.e. substances that could cause cancer on their own).
However, advances in cancer biology have revealed the limitations of this approach. Armitage and Doll first laid out a multistage theory of carcinogenesis in 1954 (19), and by 1990, initiation and promotion were well established as discrete steps in the evolution towards malignancy, along with the influence of ‘free radicals’, proto-oncogenes, oncogenes, epigenetic mechanisms and other synergistic or antagonistic factors (20). In 2000, Hanahan et al. (21) gave structure to this rapidly growing field of research with the proposal that ‘the vast catalog of cancer cell genotypes [could be organized into] a manifestation of six essential alterations in cell physiology that collectively dictate malignant growth’. They called these alterations the Hallmarks of Cancer, defined as ‘… acquired capabilities’ common to most cancers that ‘… incipient cancer cells … [must acquire to] enable them to become tumorigenic and ultimately malignant.’ The hallmarks delineated at the time were as follows:
Self-sufficiency in growth signals (later renamed proliferative signaling)—cancer cells grow at a seemingly unlimited rate.
Insensitivity to antigrowth signals (evading growth suppressors)—cancer cells are not subject to antigrowth signals or withdrawal of normal growth signals.
Evading apoptosis (resisting cell death)—cancer cells avoid the usual process whereby abnormal or redundant cells trigger internal self-destroying (as opposed to cell death) mechanisms.
Limitless replicative potential (enabling replicative immortality)—cancer cells do not senesce (or age) and die after a limited number of cell divisions.
Sustained angiogenesis (inducing angiogenesis)—cancer cells elicit new blood vessels to sustain growth.
Tissue invasion and metastasis (activating invasion and metastasis)—in situ or non-invasive cancers, e.g. ductal carcinoma in situ in the breast or carcinoma in situ in colon polyps, grow into pre-existing spaces but invasive tumors must create a space to expand into normal tissue.
From this perspective risk assessments based on limited ‘mode of action’ information, assumptions of linear dose-response relationships and a focus on individual chemicals (as complete carcinogens) appeared to be inadequate to estimate human cancer risks. So in 2005, a scientist at the United States EPA called for a shift in risk assessment practices that would move the field towards the development of biomarkers directly related to the pathways found within the Hallmarks of Cancer framework (22).
The Hallmarks of Cancer framework was subsequently revisited by Hanahan et al. (21) and expanded to encompass additional areas suggested by subsequent cancer research (23). This expansion included the following:
-
Two enabling characteristics:
Genome instability and mutation, which allows changes in one cell to pass to daughter cells through mutation or epigenetic changes in the parent cell DNA.
Tumor-promoting inflammation, which helps cancer cells grow via the same growth signals normal cells provide to each other during wound healing and embryonic growth; inflammation further contributes to the survival of malignant cells, angiogenesis, metastasis and the subversion of adaptive immunity (24).
Two ‘emerging’ hallmarks:
Avoiding immune destruction whereby tumor cells avoid immune surveillance that would otherwise mark them for destruction.
Dysregulated metabolism, one of the most recognizable features of cancer; its exclusion from the original list of hallmarks (21) probably represented a significant oversight, as it constitutes one of the earliest described hallmarks of cancer (25,26). It is needed to support the increased anabolic and catabolic demands of rapid proliferation and is likely an enabler of cancer development and its other associated hallmarks.
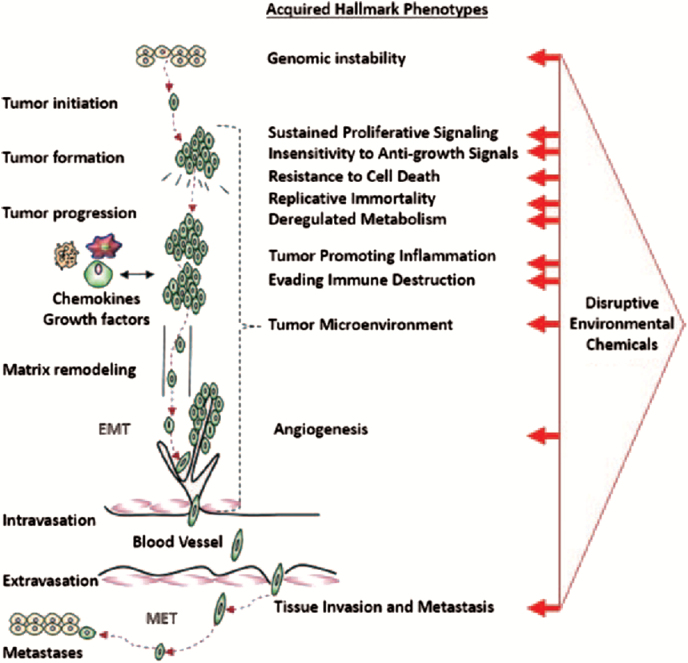
Unfortunately, risk assessment practices that are currently used to assess the carcinogenic potential of chemicals have changed very little (despite the vast literature that now underpins the main tenants of the Hallmarks of Cancer framework). For example, a chemical that disrupts DNA repair capacity might prove to be non-carcinogenic at any level of exposure (when tested on its own), but that very same chemical may have the potential to be an important contributor to carcinogenesis (e.g. in the presence of mutagens that cause DNA damage). Similarly, a chemical that has immuno-suppressive qualities may not be carcinogenic on its own, but if it acts to suppress the immune response, it may contribute to carcinogenesis (by dismantling an important layer of defense) in the presence of other disruptive chemicals. Considering the multistep nature of cancer and the acquired capabilities implied by each of these hallmarks, it is therefore a very small step to envision how a series of complementary exposures acting in concert might prove to be far more carcinogenic than predictions related to any single exposure might suggest (see Figure 1). Interacting contributors need not act simultaneously or continuously, they might act sequentially or discontinuously. So a sustained focus on the carcinogenicity of individual chemicals may miss the sorts of synergies that might reasonably be anticipated to occur when combinations of disruptive chemicals (i.e. those that can act in concert on the key mechanisms/pathways related to these hallmarks) are encountered.
Figure 1.
Disruptive potential of environmental exposures to mixtures of chemicals. Note that some of the acquired hallmark phenotypes are known to be involved in many stages of disease development, but the precise sequencing of the acquisition of these hallmarks and the degree of involvement that each has in carcinogenesis are factors that have not yet been fully elucidated/defined. This depiction is therefore only intended to illustrate the ways in which exogenous actions might contribute to the enablement of these phenotypes.
To address the biological complexity issue associated with chronic diseases, the EPA and other agencies have begun to pursue risk assessment models that incorporate biological information. This is the basis of the Adverse Outcome Pathway concept, a construct that is gaining momentum because it ties existing knowledge of disease pathology (i.e. concerning the linkage between a direct molecular initiating event and an adverse outcome at a biological level of organization) to risk assessment (27,28). This line of thinking inspired a recent initiative by the EPA, where the agency tested a proposal for characterizing the carcinogenic potential of chemicals in humans, using in-vitro high-throughput screening (HTS) assays. The selected HTS assays specifically matched key targets and pathways within the Hallmarks of Cancer framework. The authors tested 292 chemicals in 672 assays and were successfully able to correlate the most disruptive chemicals (i.e. those that were most active across the various hallmarks) with known levels of carcinogenicity. Chemicals were classified as ‘possible’/‘probable’/‘likely’ carcinogens or designated as ‘not likely’ or with ‘evidence of non-carcinogenicity’ and then compared with in-vivo rodent carcinogenicity data in the Toxicity Reference Database to evaluate their predictions. The model proved to be a good predictive tool, but it was developed only as a means to help the EPA prioritize many untested individual chemicals for their carcinogenic potential (i.e. in order to establish priorities for individual chemical testing (29)).
What is still needed, is an approach employing the Hallmarks of Cancer framework that can be used to identify priority mixtures (i.e. those with substantive carcinogenic potential). Without a way to anticipate the carcinogenicity of complex mixtures, an important gap in capability exists and it creates a significant weakness in current risk assessment practices. Countries around the globe have made a significant investment in the regulatory infrastructure and risk assessment practices that protect us from unwanted exposures to harmful chemicals and carcinogens, so we wanted to review the biology of cancer to map out the challenges associated with the development of an approach that would help us assess the carcinogenic potential of low-dose exposures to chemical mixtures in the environment. Such an approach was seen as a reasonable step to provide impetus for progress in this area of research and ultimately to inform risk assessment practices worldwide.
Materials and methods
In 2012, the non-profit organization ‘Getting to Know Cancer’ instigated an initiative called ‘The Halifax Project’ to develop such an approach using the ‘Hallmarks of Cancer’ framework as a starting point. The aim of the project was to produce a series of overarching reviews of the cancer hallmarks that would collectively assess biologically disruptive chemicals (i.e. chemicals that are known to have the ability to act in an adverse manner on important cancer-related mechanisms, but not deemed to be carcinogenic to humans) that might be acting in concert with other seemingly innocuous chemicals and contributing to various aspects of carcinogenesis (i.e. at levels of exposure that have been deemed to be safe via the traditional risk assessment process). The reviews were to be written by 12 writing teams.
The writing teams were recruited by Getting to Know Cancer circulating an email in July 2012 to a large number of cancer researchers, asking about their interest in the project. Respondents were asked to submit personal details through a dedicated webpage that provided additional project information. A total of 703 scientists responded to the email, and from that group, 11 team leaders were selected to lead reviews of each hallmark (10 Hallmarks plus an 11th team to consider the tumor microenvironment as a whole) and one leader for the cross-validation team (see below). Writing group leaders were asked to form individual teams drawn from the pool of researchers who expressed interest in the project and from their own circles of collaborators. Leaders were encouraged to engage junior researchers as well. Team leaders received project participation guidelines and ongoing communication from the project leaders, L.Lowe and M.Gilbertson. Each team included: a lead author with a published expertise in the hallmark area; domain experts who assisted in the production of the descriptive review of the biology; environmental health specialists (e.g. specialists in toxicology, endocrine disruption, or other related disciplines) and support researchers.
Each writing team was charged to describe the hallmark, its systemic and cellular dysfunctions and its relationships to other hallmarks. A priority list of relevant (i.e. prototypical) target sites for disruption was to be developed by the team and a list of corresponding chemicals in the environment that have been shown to have the potential to act on those targets was requested, along with a discussion of related issues and future research needed (in the context of project goals).
Selection of target sites for disruption
A ‘target’ was broadly defined as a procarcinogenic disruption at the system level (e.g. the hypothalamic–pituitary–gonadal axis), organ level, tissue level or cellular level. It was assumed from the outset that a project intended to develop an approach for the assessment of the carcinogenic potential of low-dose exposures to chemical mixtures in the environment would encounter a practical upper limit to the number of potential targets that any given team could realistically review. Therefore, each team was asked to identify up to 10 relevant targets for their domain (bearing in mind that each target would also serve as a starting point for the identification of a disruptive environmental chemical that had already shown a demonstrated ability to act on that target). In theory, it was understood that this could lead to as many as 110 targets for the entire project, and as the teams were also asked to select one disruptive chemical for each target, a maximum of 110 chemicals.
In this phase, teams were asked to focus on specific gene changes common to many cancers as identified by The Cancer Genome Project (30) in order to estimate how the function of specific genes might be altered, not by specific gene mutations, but rather either by direct action or by epigenetic changes that might lead to the same functional ends. Most of these pathways and processes are found within both the hallmarks of cancer and the genomic frameworks, so teams were asked to evaluate both models and consider non-mutagenic/epigenetic pathways of interference as well (given that epigenetic changes such as DNA methylation and histone acetylation are relevant for cancer and often inducible by chemicals and may be transmitted to daughter cells).
Selection of disruptive chemicals
Teams were then asked to identify ‘prototypical’ chemicals in the environment that had demonstrated an ability to act on the selected targets. During workshops in Halifax, the teams settled on the following criteria to guide their choices:
Chemicals should be ubiquitous in the environment because we wanted the broadest possible relevance for the general population.
Chemicals should selectively disrupt individual targets such as specific receptors, specific pathways or specific mechanisms. Hypothetically speaking, a chemical could affect more than one pathway, receptor and so on; indeed, we expected that most chemicals would likely exert a multitude of actions. However, we used the term ‘selectively disruptive’ to encourage teams to avoid choosing mutagens that are randomly destructive in their action (i.e. unpredictable and capable of producing varying types of damage across a wide range of pathways).
Chemicals should not be ‘lifestyle’ related, such as those encountered from tobacco, poor diet choices (e.g. red meats, French fries, lack of fruit and vegetables and so on), alcohol consumption, obesity, infections (e.g. human papillomavirus) and so on.
Chemicals should not be known as ‘carcinogenic to humans’ (i.e. not IARC Group 1, carcinogens).
The choice to focus on environmental pollutants in this project was intentionally restrictive. Countries around the globe have made significant investments in regulatory infrastructure and risk assessment practices to protect us from unwanted exposures to harmful chemicals and carcinogens. Therefore, we focused on chemicals that are commonly encountered in the environment. Primarily, we wanted to generate insights that would be valuable for cancer researchers who are specifically interested in environmental chemical exposures to chemical mixtures and/or those who are focused on risk assessment practices in general.
Dose-response characterizations and LDE
Given that much of the evidence in the toxicological literature that documents the disruptive actions of various chemicals has been produced under a wide range of differing experimental circumstances, we wanted to assess the quality and relevance of data that were gathered for exposures discussed in this review. Specifically, for each chemical selected and each mechanism identified, teams were additionally tasked to identify any dose-response characterization results and/or relevant low-dose research evidence that might exist. The term ‘low dose’ was defined using the European Food Safety Authority definition (i.e. responses that occur at doses well below the traditional lowest dose of 1mg/kg that are used in toxicology tests) and the definition for ‘LDE’ was based on the EPA definition (31)—as follows:
Any biological changes occurring
(a) in the range of typical human exposures or
(b) at doses lower than those typically used in standard testing protocols, i.e. doses below those tested in traditional toxicology assessments (32), or
(c) at a dose below the lowest dose for a specific chemical that has been measured in the past, i.e. any dose below the lowest observed effect level (LOEL) or LOAEL (33)
(d) occurring at a dose administered to an animal that produces blood concentrations of that chemical in the range of what has been measured in the general human population (i.e. not exposed occupationally, and often referred to as an environmentally relevant dose because it creates an internal dose relevant to concentrations of the chemical measured in humans) (34,35).
Each team was then asked to categorize each chemical by using one of five possible categories (to determine the relevance and relative strength of the underlying evidence for each of the chemicals being considered). The categories were as follows: (i) LDE (i.e. levels that are deemed relevant given the background levels of exposure that exist in the environment); (ii) linear dose-response with LDE; (iii) non-linear dose-response with LDE; (iv) threshold (i.e. this action on this mechanism/pathway does not occur at low-dose levels) and (v) unknown. Additional details of the descriptions for each of these categories are shown in Table 1.
Table 1.
Dose-response characterization
| Review team | Chemical name | Disruptive action on key mechanism/pathway | Low-dose effect (LDE, LLDE, NLDE, threshold, unknown) |
|---|---|---|---|
| Angiogenesis | Diniconazole | Vascular cell adhesion molecule and cytokine signaling | Threshold (H-PC) (36) |
| Ziram | Vascular cell adhesion molecule and cytokine signaling | Threshold (H-PC) (36,37) | |
| Chlorothalonil | Thrombomodulin, vascular proliferation and cytokine signaling | Unknown (H-PC) (36), NLDE (A-in vivo) (38) | |
| Biphenyl | Angiogenic cytokine signaling | Unknown (H-PC) (36) | |
| Tributyltin chloride | Vascular cell proliferation and adhesion molecule signaling | Unknown (H-PC) (36) | |
| Methylene bis(thiocyanate) | Plasminogen activating system and cytokine signaling | Unknown (H-PC) (36) | |
| HPTE | Vascular cell adhesion molecule and cytokine signaling | Unknown (H-PC) (36), threshold (A-Ia) (39), LDE (A-Ia) (40) | |
| PFOS | Angiogenic cytokine signaling | Threshold (H-PC) (36), LDE (H-CL) (41) | |
| Bisphenol AF | Matrix metalloproteinase expression and estrogen receptor signaling | Unknown (H-PC) (36) | |
| C.I. solvent yellow 14 | AhR and hypoxic signaling | Unknown (H-PC) (36) | |
| Dysregulated metabolism | Cypermethrin | AR and ER expression, reduction of ATP and mitochondrial enzymes, mitochondrial membrane potential | LLDE (A-I) (42), NLDE (A-I) (42), NLDE (H-CL) (36,43,44) |
| Acrolein | p53 activation, DNA repair inhibition, PERK phosphorylation, mitochondrial dysfunction, cell survival | LLDE (A-I, A-CL, H-PC, H-CL) (45–50), NLDE (49), threshold (46) | |
| Rotenone | Cell cycle, DNA damage response, proliferation, differentiation, mitochondria | LLDE (H-CL) (51–53), NLDE (H-CL) (51,53), unknown (H-CL,H- PC) (36) | |
| Copper | p53 activation, p21 up-regulation, cell viability | LLDE (H-CL) (54–56) | |
| Nickel | Neutrophil apoptosis, E-cadherin regulation, matrix metallopeptidase (MMP) production | LLDE (H-CL) (57), NLDE (H-CL) (58), Threshold (H-CL) (58) | |
| Cadmium | p53-dependent apoptosis, cell proliferation | LLDE (H-CL) (59), threshold (H-CL) (60) | |
| Diazinon | AChE activity, neuronal cytotoxicity | Unknown (A-PC) (61), LLDE (H-CL) (62), threshold (H-CL) (36) | |
| Iron | KRAS mutations | LLDE (A-I) (63) | |
| Malathion | Lymphocyte Mutations, Cytotoxicity | Unknown (H-PC, H-E) (36,64) | |
| Tissue invasion and metastasis | BPA | MMP-2 and MMP-9 expression, increased migration, invasion, EMT, oxidative stress, ER signaling | LDE (H-CL) (65,66), threshold (H-CL, H-PC) (36) |
| Hexacholorobenzene | Activation of c-Src, HER1, STAT5b and ERK1/2 signaling | LLDE (H-CL, A-I) (67) | |
| Sulfur dioxide | MMP-9 expression | Unknown (A-PC) (68) | |
| Phthalates | MMP-2 and MMP-9 expression | LDE (H-CL) (66), Unknown (H-CL, H-PC) (36) |
|
| Iron | ROI generation, NF-κB activation, uPA expression | Unknown (H-CL) (69) | |
| Biorhythms/melatonin | GSK3β activation, EMT regulation | Unknown (H-CL, H-E) (70,71) | |
| Resistance to cell death | BPA | Inhibition of GJIC, activation of mTOR pathway, down-regulation of p53, p21 and BAX, binding to ER-α, weakly binds to TH receptor and AR, activation of ERK1/2 and p38 | NLDE(H-CL, A-CL) (72–74) Threshold (H-CL, H-PC) (36) |
| Dibutyl phthalate | Activation of PPAR-α, inhibition of GJIC, expression of cyclin D and cdk-4, activation of AhR/HDAC6/c-Myc pathway | NLDE (H-CL) (75), unknown (H-CL, H-PC) (36) | |
| Chlorothalonil | Up-regulation of ErbB-2 tyrosine kinase and MAP kinase, aromatase inhibitor | Threshold-based (i.e. non-linear) (A-I) (76), unknown (H-PC) (36), threshold (H-CL) (36) | |
| Lindane | Induction of MAPK/ERK pathways | Threshold-based (i.e. non-linear) (A-I) (77), threshold (H-CL) (36) | |
| Dichlorvos | Expression of p16, Bcl-2 and c-myc | LLDE (A-I) (78), threshold (H-CL) (36) | |
| MXC | Binding to ER-α receptor, up-regulation of cyclin D1, down-regulation of p21 | LLDE (H-CL, A-CL) (75,79), unknown (H-PC) (36), threshold (H-CL) (36) | |
| Oxyfluorfen | Expression of Cyp2b10 and Cyp4a10 transcripts (markers of PPAR-α activation) | Threshold (A-I) (80), unknown (H-CL, H-PC) (36) | |
| DEHP | Activation of PPAR-α, inhibition of GJIC | Threshold-based (i.e. non-linear) (A-I) (81) | |
| Linuron | Hypersecretion of LH, inhibition of GJIC | Unknown (H-CL) (82) | |
| Replicative immortality | Nickel-derived compounds, (e.g. nickel chloride) | Epigenetic silencing of p16 | LLDE (H-CL, A-PC) (83) |
| Diethylstilbestrol | Allelic loss and point mutation in ETRG-1 gene | LLDE (A-I) (84) | |
| Reserpine | Epigenetic modifications | Unknown (A-PC) (85), threshold (H-CL) (36) | |
| Phenobarbital | Reduces expression of the CDKN1A product p21, CAR activation | LLDE (A-I) (86,87) | |
| Acetaminophen | Cellular energy loss, mitochondrial damage, telomerase activation | LDE (H-CL, A-I, A-CL) (88–92) | |
| Cotinine | Telomerase activation | LLDE (H-PC) (93) | |
| Nitric oxide | p53 inactivation | LLDE (H-PC, H-CL, A-CL, A-I) (94) | |
| Na-selenite | p53 promoter methylation | LLDE (A-CL, A-I) (95,96) | |
| Lead | p53 inactivation | LLDE (H-PC, H-CL, A-CL, A-I) (94) | |
| Sustained proliferative signaling | BPA | Estrogen receptor activation, cell cycle/senescence | LLDE (A-I, H-CL, H-E) (12,97), NLDE (A-I) (98,99), threshold (H-CL) (36) |
| Cyprodinil | Increased proliferation signaling, AhR activation | Unknown (H-PC, H-CL) (36,100,101), threshold (H-CL) (36) | |
| Imazalil | AR signaling | NLDE (A-I) (102,103), threshold (H-CL, H-PC) (36) | |
| Maneb | Nitric oxide signaling | Unknown (A-CL, H-CL, H-PC) (36,104,105) | |
| Methoxyclor | ER signaling | Threshold (H-CL) (36), LDE (A-I) (106,107), NLDE (A-I) (108) | |
| PFOS | Nuclear hormone receptors | Threshold (H-CL) (36), LLDE (A-I) (109,110) | |
| Phthalates | CAR, ER signaling | Unknown (H-CL) (36), LDE (A-I) (111–113) | |
| Phosalone | Increased proliferation, PXR signaling | Unknown (H-PC, H-CL) (36,114,115) | |
| PBDEs | ER signaling | LDE (A-I) (116,117) | |
| Prochloraz | ER signaling | LDE (A-I) (118,119) | |
| Trenbolone acetate | Insulin-like growth hormone-1 and AR signaling | Unknown, LDE (A-I, H-CL, H-E) (120,121) | |
| Tumor-promoting inflammation | BPA | Immune cell proliferation, proinflammatory cytokine induction | Threshold (H-PC) (36), LDE (A-I, H-CL, H-E) (122–126) |
| Phthalates | Immunomodulation of macrophages, lymphocytes, eosinophils and neutrophils | Unknown (H-PC, H-CL, H-E) (36,127) | |
| PBDEs | Induction of pro-inflammatory cytokines (IL-6, IL8 and CRP), inhibition of anti-inflammatory cytokines (IL-10) | Threshold (H-PC, H-CL) (128–131) | |
| Atrazine | Immunomodulation of T cell and B cells, proinflammatory cytokines | Unknown (H-PC, A-I) (36,132,133) | |
| Vinclozolin | Proinflammatory cytokine induction, NF-κB activation | Unknown (H-PC, A-I) (36,134–136) | |
| 4-NP | Proinflammatory cytokine induction, NF-κB activation, iNOS induction | Unknown (A-CL, H-CL, H-PC) (36,137,138) | |
| Immune system evasion | Pyridaben | Chemokine signaling, TGF-β, FAK, HIF-1a, IL-1a pathways | Unknown (H-CL, H-PC, A-CL) (36,139,140), threshold (A-I) (141) |
| Triclosan | Chemokine signaling, TGF-β, FAK, IL-1a pathways | Threshold (H-CL, H-PC, A-I) (36,142–144), LDE (A-I, H-CL) (145,146) | |
| Pyraclostrobin | Chemokine signaling, TGF-β, IL-1a pathways | Unknown (H-CL, H-PC) (36) | |
| Fluoxastrobin | Chemokine signaling, EGR, HIF-1a, IL-1a pathways | Unknown (H-CL, H-PC) (36) | |
| BPA | Chemokine signaling, TGF-β pathway | Threshold (H-PC) (36), LDE (A-I) (12), NLDE (H-CL) (147), NLDE (A-CL) (148–151), NLDE (A-I) (152–155) | |
| Maneb | PI3K/Akt signaling, chemokine signaling, TGF-β, FAK, IGF-1, IL-6, IL-1a pathways | Unknown (H-CL, H-PC) (36,139,156–158), LDE (A-I) (159), threshold (A-I) (139,160), threshold (A-CL, A-I) (161) | |
| Evasion of antigrowth signaling | DDT | Induces MDM2, cyclin D1, E2F1 expression, disrupts gap junctions | NLDE (A-I, H-CL, A-CL) (162–164) |
| Chlorpyrifos | Increases proliferation | LDE (H-CL, H-PC) (165,166) | |
| Folpet | Disrupts G1–S checkpoint kinases, down-regulates p53, promotes proliferation | LDE(A-C) (167) | |
| Atrazine | Induces estrogen production and proliferation | LDE(H-CL, A-I) (168–170) | |
| BPA | Reduced p53, reduced connexin 43 expression, increased proliferation | NLDE (H-CL, A-I) (171–174) | |
| Tumor microenvironment | Nickel | ROS and cellular stress | NLDE (A-I) (175) |
| BPA | IL-6 expression, improper DC maturation and polarization, ROS production | LLDE (A-I) (176), NLDE (A-I) (176) | |
| Butyltins (such as tributyltin) | NK cell inhibition | LDE (A-I) (177) | |
| MeHg | Chronic oxidative stress | LDE (H-PC, H-CL) (178,179) | |
| Paraquat | Chronic ROS production, cellular stress | Unknown (A-I) (180) | |
| Genome instability | Lead | Dysfunctional DNA repair, defect in telomere maintenance | Unknown (A-CL) (181–183), threshold (H-CL, H-E) (184,185) |
| Acrylamide | Inactivation of DNA repair proteins/enzymes | Unknown (A-CL, A-I, H-CL) (186,187) | |
| Quinones | Affect free cysteine residues in catalytic center of DNA methyltransferases (DNMT) | Unknown (A-CL) (188) | |
| Nickel | Affect enzymes that modulate post-translational histone modification | LDE (H-E) (189,190), LDE (A-CL, H-CL) (191) | |
| BPA | Epigenetic changes via interactions with miRNA | Threshold (H-PC) (192) | |
| Alloy particles (tungsten/nickel/ cobalt) | Disruption of DNA damage/redox signaling involving Nrf, NF-κB, Egr, and so on | LDE (A-I) (193) | |
| Titanium dioxide NPs | Decreased NADH levels and impaired mitochondrial membrane potential and mitochondrial respiration, ROS generation | Unknown (A-PC) (194) | |
| Benomyl | Spindle defects leading to formation of micronuclei | Threshold (H-CL) (195), Threshold (A-CL) (196) | |
| Carbon nanotubes | Spindle defects leading to formation of micronuclei | LLDE (A-CL) (197,198), unknown (A-I) (198) |
Each chemical in the table was categorized by using one of five possible categories (to determine the relevance and relative strength of the underlying evidence for each of the chemicals being considered)—as follows: (1) LDE (low-dose effect)—the ability of this chemical to exert this particular effect is not well characterized at a range of dose levels, but the evidence suggests that this chemical can exert this effect at low-dose levels (i.e. levels that are deemed relevant given the background levels of exposure that exist in the environment and as further defined below). (2) LLDE (linear dose-response with low-dose effects)—the ability of this chemical to exert this particular effect is well characterized at a range of dose levels and the evidence suggests that a linear dose-response relationship exists with effects at low-dose levels being evident (i.e. levels that are lower than the LOEL/LOAEL or threshold and deemed relevant given the background levels of exposure that exist in the environment). Note: a linear dose-response model implies no threshold. Effects at low doses are the same as at higher doses even if at a lesser extent. The effect is directly proportional to the dose. (3) NLDE (non-linear dose-response with low-dose effects)—the ability of this chemical to exert this particular effect is well characterized at a range of dose levels and the evidence suggests that a non-linear dose-response relationship exists with exaggerated effects at low-dose levels being evident (i.e. levels that are lower than the LOEL/LOAEL or threshold and deemed relevant given the background levels of exposure that exist in the environment). Note: a non-linear dose-response with low-dose effect implies that the effect does not vary according to the dose of the agent. The effect at low doses may be the same as at the higher doses or different. The non-linear dose-response may have or not have a threshold. It is represented by a sigmoid curve. The non-linear dose-response at low doses may be a non-monotonic dose-response. (4) Threshold—the ability of this chemical to exert this particular effect is well characterized at a range of dose levels, and a threshold has been established for this chemical that suggests that this action on this mechanism/pathway does not occur at low-dose levels (i.e. levels that are lower than the threshold and deemed relevant given the background levels of exposure that exist in the environment). (5) Unknown—although the ability of this chemical to exert this particular effect has been shown at higher dose levels, this effect is not well characterized at a range of dose levels, so a LOEL /LOAEL or a threshold has not been determined for this chemical and there is no evidence showing that this chemical exerts this action at low-dose levels (i.e. levels that are lower than the LOEL/LOAEL or threshold and deemed relevant given the background levels of exposure that exist in the environment). A-I, in-vivo animal models; A-CL, animal cell lines; A-PC, animal primary cells; H-PC, human primary cells; H-CL, human cell lines; H-E, human epidemiological studies. With respect to the human primary cell (H-PC) data from ToxCast (36): unknown signifies that the compound was tested across a range of doses and showed statistically significant activity against the specified targets at the lowest test concentrations (~0.01 µM); therefore, a threshold could not be established. Threshold in this data set signifies that there was no activity against the targets at one or more of the lowest concentrations tested.
aExtrapolated from in-vivo data on the parent compound, MXC.
Cross-hallmark relationships
In recognition of the network of signaling pathways involved and the degree of overlap/interconnection between the acquired capabilities described in each hallmark area, the project included a cross-validation step to create a more complete mapping of the actions that might be anticipated as the result of an action on the target sites identified or by the disruptive effects of the chemicals selected. Given the diversity of the targets involved in the 11 hallmark areas, it was anticipated that inhibiting or stimulating a target relevant to one hallmark may have an impact on other targets that are relevant, especially if both are linked via signaling pathways.
Accordingly, the cross-validation team conducted additional background literature review of submitted targets and chemicals from each writing team, searching for evidence to identify cross-hallmark activity. Each potential target-hallmark or approach-hallmark interaction was assessed to determine whether the inhibition or activation of each target and the corresponding biological activity of each chemical might reasonably be expected to have either a procarcinogenic or anticarcinogenic effect on key pathways/processes in the various hallmark areas.
The cross-validation team also sought out controversial interactions (i.e. mixed indications of hallmark-like effects) and instances where no known relationship existed. It was our belief that target sites or chemicals that demonstrated a substantial number of ‘anticarcinogenic’ effects in other hallmark areas would be less suitable to serve as instigating constituents in the design of carcinogenic mixtures (where procarcinogenic synergy was being sought).
It is important to note that the cross-validation team was not given any restrictions for literature selection for this effort, and contributing authors were restricted neither to results from low-dose testing, nor to that of cancer-related research. This approach was taken because it was realized at the outset that this sort of breadth and homogeneity (of low-dose evidence) does not yet exist in the literature. As a result, the types and sources of data gathered in this effort varied considerably, resulting in an admixture of reviews and original studies. Moreover, many studies that were cited in this effort only considered a chemical’s ability to instigate or promote an action that mimics a hallmark phenotype in a manner directionally consistent with changes that have been associated with cancer. So, although we have referred to these actions as procarcinogenic and anticarcinogenic, as these changes are frequently neither fixed nor specific for cancer, the specificity of these changes and implications for carcinogenesis cannot and should not be immediately inferred from this data set. Short-term toxicity and toxic responses—particularly in data from in-vitro HTS platforms—must be distinguished from truly ‘carcinogenic’ long-term changes. In other words, the tabularized results from this particular aspect of the project were only compiled to serve as a starting point for future research. Where cross-hallmark effects were reported (at any dose level and in any tissue type), we wanted samples of that evidence to share with researchers who might be trying to anticipate the types of effects that might be encountered in future research on mixtures of chemicals (in a wide range of possible research contexts).
Results
The results are presented roughly sequenced in a manner that captures the acquired capabilities found in many/most cancers. The section begins with two enabling characteristics found in most cancers Genetic instability and Tumor-promoting inflammation, followed by Sustained proliferative signaling and Insensitivity to antigrowth signals, the two related hallmarks that ensure that proliferation is unabated in immortalized cells. These sections are followed by Resistance to cell death and Replicative immortality, two critical layers of defense that are believed to be bypassed in all cancers and then by dysregulated metabolism. Sections on Angiogenesis and Tissue invasion and metastasis follow and speak to the progression of the disease, and finally, the Tumor microenvironment and Avoiding immune destruction sections offer summaries related to the very last lines of defense that are defeated in most cancers. Additionally, dose-response characterizations and evidence of LDE are then presented for all of these areas and the results from the cross-validation activity are summarized and reviewed.
Genetic instability
The phenotypic variations underlying cancer result from interactions among many different environmental and genetic factors, occurring over long time periods (199). One of the most important effects of these interactions is genome instability—loosely defined as an increased likelihood of the occurrence of potentially mutagenic and carcinogenic changes in the genome. The term is used to describe both the presence of markers of genetic change (such as DNA damage and aneuploidy) and intrinsic factors that permit or induce such change (such as specific gene polymorphisms, defective DNA repair or changes in epigenetic regulation).
DNA damage—which can be caused by exposure to external chemicals or radiation, or by endogenous agents such as reactive oxygen or faulty replication—is an event that can initiate the multistep process of carcinogenesis (200). Protection is afforded at different levels; removal of damaging agents before they reach the DNA, by antioxidant defenses and the phase I/phase II xenobiotic metabolizing enzymes; a second line of defense, DNA repair, operating on the damage that occurs despite the primary protection; and as a last resort, apoptosis (programmed cell death), disposing of heavily damaged cells.
A clear sign of genome instability is aneuploidy—a deviation from the normal number of chromosomes (201). Aneuploidy is a very common feature of human cancers. Another hallmark of cancer is loss of the normal mechanism of telomere shortening, which allows abnormal cells to escape senescence, by avoiding the body’s ‘editing’ processes that normally eliminate aging cells with their accumulated genome aberrations (202,203).
The genes of most significance for cancer are the (proto)-oncogenes which, if defective, or abnormally expressed, lead to uncontrolled cell proliferation; tumor suppressor genes, the normal products of which tend to switch off replication to allow repair, and promote cell death if damage is excessive; and genes such as those involved in DNA repair that can—if faulty—lead to a ‘mutator phenotype’. Mutated proto-oncogenes and tumor suppressor genes are found in most if not all cancers and play key roles in cancer etiology (204–207). Rare mutations in DNA repair genes greatly increase the risk of cancer (208,209). However, the evidence for links between common variants of repair genes and cancer is generally inconclusive (210).
The term ‘epigenetics’ refers to covalent modifications of the DNA (methylation of cytosine in ‘CpG islands’ within regulatory regions of genes) or of the histones. These modifications can control gene expression and the pattern of modifications is altered in many cancers (211,212). For instance, hypomethylation of proto-oncogenes can lead to overexpression, which is undesirable. MicroRNAs (miRNAs) are responsible for specific down-regulation of gene expression at a post-transcriptional level, by preventing translation from messenger RNAs. miRNAs participate in DNA damage responses and some miRNAs are deregulated in many cancers (213–215).
Mutations in germ and stem cells are potentially more serious than those in other cells as they are passed to the cells’ progeny within the developing embryo or regenerating tissue (216,217). There is a presumed survival benefit when stem cells tend to show a particularly stringent maintenance of genome integrity through cell cycle regulation and enhanced responses to DNA damage (218).
The selected ‘chemical disruptors’ that induce genome instability include chemicals that not only directly damage DNA or cause mutations, but act indirectly, via pathways such as DNA damage signaling, DNA repair, epigenetic regulation or mitochondrial function. They include the following:
Metals such as lead, nickel, cobalt and mercury (common water pollutants) are known to disrupt DNA repair (181,219), whereas nickel also affects epigenetic histone modification (189,191) and lead causes defective telomere maintenance (184,220). Alloy particles, containing tungsten, nickel and cobalt, can be inhaled and disrupt redox signaling (193,221). Titanium dioxide nanoparticles are also common in many consumer products and foods and have been reported to disrupt mitochondrial function and increase oxidative stress, as well as inhibit DNA repair and disrupt mitosis (194,222,223).
Acrylamide occurs in many fried and baked food products, and (apart from the well-known DNA adduct formation) can inactivate many critical proteins by binding sulfhydryl groups (186).
Bisphenol A (BPA) is a plasticizer used for manufacturing polycarbonate plastics and epoxy resins, and it can leach from plastics into food and water. It is implicated in disruption of DNA methylation, histone acetylation and disturbance of miRNA binding (192,224,225), redox signaling (226) and induction of micronuclei through spindle defects in mitosis (227).
The fungicide benomyl is metabolized to carbendazim; both are classified as possible human carcinogens at present. The route of exposure is most likely ingestion via residues in crops. Benomyl disrupts the microtubules involved in the function of the spindle apparatus during cell division, leading to production of micronuclei (Frame,S.R. et al., unpublished report, Schneider,P.W. et al., unpublished report, (228)).
Halobenzoquinones are disinfection by-products in chlorinated drinking water (229). Quinones are electrophilic compounds, known to react with proteins and DNA to form adducts. These electrophylic chemicals can interact with functional thiol groups via Michaelis–Menton type addition, causing modification of enzymes involved in methylation and demethylation (188). This mechanism might be shared by other xenobiotics that increase reactive oxygen species (ROS).
Human exposure to nano-sized materials used in cosmetics, biomedical compounds, textiles, food, plastics and paints has increased not only in a conscious way but also passively by the leakage of nanomaterials from different objects. Nanoparticles can induce genome instability via mitochondrial-related apoptosis (230), decreased DNA repair (222,230,231), hypoacetylation of histones (232), disruption of DNA methylation (231), up-regulation of miRNA (233), reducing telomerase activity (220) and—more specifically for carbon nanotubes—interacting with components of the mitotic spindle during cell division or interacting with proteins directly or indirectly involved in chromosome segregation (197,234). Nano-sized materials can also produce inflammation and alteration of the antioxidant defenses that can lead to genome instability.
Tumor-promoting inflammation
One of the earliest hypothesized causes of tumors subsequently supported experimentally was the irritation hypothesis proposed by Virchow. Although it was recognized initially that injury alone was insufficient for carcinogenesis, it was also recognized that ‘irritation may have an accessory or predisposing influence in tumor formation, and that it may be enough finally to upset the balance of a group of cells which for some other reason were already hovering on the brink of abnormal growth’ (235). Indeed, it is now recognized that inflammatory responses, similar to those associated with wound healing or infection, support the development of invasive carcinomas by altering the microenvironment in favor of proliferation, cell survival, angiogenesis and tumor cell dissemination while also disrupting antitumor immune surveillance mechanisms. In other words, inflammation plays a critical role in tumorigenesis (23,24).
Inflammation is an immediate and necessary host defense mechanism in response to infection or tissue injury by noxious stimuli. In tumor-associated inflammation, both the epithelium and the immune cells express receptors that signal the activation and production of a wide array of biologically active proteins most analogous to an unhealed wound. The sustained or uncontrolled release of potent and reactive molecules such as prostaglandins, cytokines, ROS and chemokines from both the tumor cell and the microenvironment constituents lead to progressive genomic instability, alterations in the integrity and function of the microenvironment including alterations in the vasculature (e.g. vascular hyperpermeability, neovascularization and angiogenesis), as well as alterations in local immune dynamics. The cellular and molecular mechanisms include a diverse array of immune- and tumor-cell-derived effector molecules such as the proinflammatory reactive oxygen and nitrogen species, a number or cytokines, chemokines as well as cyclooxygenase-2 and its product, prostaglandin E2.
In general, there is a paucity of experimentation, and when present, inconsistent findings for the role of environmental chemicals as proinflammatory molecules and more so for a proinflammatory action as a co-factors in carcinogenesis. However, some recent studies provide a credible mechanistic basis, particularly early life exposures that might act by disrupting the immune cell balance toward inflammation, and that manifest in adulthood. One example is BPA, one of the most abundant and best studied environmental endocrine disruptors, and its controversial role as an immune disruptor. Specifically, studies in male rats found that early life BPA exposure leads to the development of prostate intraepithelial neoplasia (a prostate cancer precursor lesion) through a pathological process that includes BPA-dependent epigenetic reprogramming of genes involved in the development of lateral prostate inflammation in adulthood (236,237).
This work in prostate is complemented by a much more extensive study of BPA effects on immune cell components, particularly the T-cell compartment, demonstrating that BPA acts as an immune disruptor by promoting ‘immune’ cell proliferation though the exact nature of the effect on specific cells of the immune system is poorly delineated. Most interesting is the work by Yan et al. (122), who reported findings suggesting that the timing of BPA exposure during development (prenatally, early life or adult) alters the effect of BPA on regulatory T cells. BPA actions also map over to the effects on the immune system including the promiscuity of BPA for a number of nuclear receptors relevant to immune cells such as the estrogen receptor and the aryl hydrocarbon receptor (AhR). As well, bulky BPA analogs may act as antagonists of members of the peroxisome proliferator-activated receptor (PPAR) family, an important family of nuclear receptors with potent anti-inflammatory function (238,239). Effects on the PPAR nuclear receptors may also explain inflammation-associated phenotypes observed with exposures to certain phthalates and nonylphenol (4-NP).
A second example is the reported immunotoxic effects of atrazine (6-chloro-N-ethyl-N-(1-methylethyl)-1,3,5-triazine-2,4-diamine) (240), a chemical that is the most commonly detected triazine herbicide in USA soil and water. Atrazine is banned by the European Union and drinking water exposures are supposed to be limited in the USA to <3 µg/l (although exposures exceed this limit regularly), but the use of this chemical is high and increasing in Asia and other countries. Thus, atrazine is an important pesticide to which humans are exposed. Atrazine exhibits weak mutagenicity and low oncogenic properties, but research by a number of authors is emerging that suggests that immune system disruption might be a concern (132,240,241).
Although the majority of work on atrazine has been focused on its endocrine disrupting properties, there is also evidence to support immunotoxicity including effects on T-lymphocytes composition with oral dosing (242,243), modulation of nitric oxide production (244) and potential generation of ROS (245,246). The local production of reactive nitrogen species and ROS by mast cells and macrophages are among the better studied immune modulatory molecules for which recent evidence supports important roles both in the tumor microenvironment and in the tumor progression (247–249). Notably, these reactive species trigger oxidative/nitrosative modifications, which can initiate redox signaling that tightly modulates the inflammatory response in a manner that is highly relevant for carcinogenesis (250,251).
We also looked at polybrominated diphenyl ethers (PBDEs) and their effects on inflammatory cytokines. Peltier et al. (128) recently found that placental explants treated with a mixture of the cogeners BDE-47, -99 and -100 and then exposed to Escherichia coli were ‘reprogrammed’ toward a proinflammatory response (increased IL-1β and tumor necrosis factor α) and away from the expected anti-inflammatory response (decreased IL-10) compared with untreated placenta. Although these studies are preliminary, chronic PBDE exposure may lower the threshold for bacteria to stimulate a proinflammatory response, which has potential relevance given the established link between bacteria and certain cancers (e.g. Helicobacter pylori and gastric cancer), where tumor development is dependent on inflammation.
Vinclozolin was also of particular interest as an environmental chemical because transient early life exposures in utero have been linked to both adult-onset disease and transgenerational disease that involves inflammation (134,135). For example, transient vinclozolin exposure in utero has been shown to promote inflammation in the prostate (prostatitis) of postpubertal rats coupled with a down-regulation of the androgen receptor and increase in nuclear factor-κB (NF-κB). The late or delayed effect of exposure is hypothesized to reflect a mechanism whereby vinclozolin exposure during a critical development window imprints an irreversible alteration in DNA methyltransferase activity, leading to reprogramming of the androgen receptor (AR) gene(s), which manifest as inflammation in early adult life with adverse effects on spermatid number.
Similarly, 4-NP has been shown to increase progenitor white adipose levels, body weight and overall body size in rodents exposed prenatally. Like vinclozolin, 4-NP effects on adipogenesis in the perinatal period confer transgenerational inheritance of the obesogenic effects observable in F2 offspring, consistent with genome reprogramming through an epigenetic process (252) and others have reported immune and inflammation-related effects (137,138) making it relevant to carcinogenesis a deserving further investigation.
Sustained proliferative signaling
Sustained proliferative potential is an essential component of cancerous growth. Progressive conversion of normal cells into cancer cells requires a series of genetic alterations, where each alteration confers one or more types of growth advantage. One such alteration that affords the transformed cell a distinct growth advantage over its normal counterparts is the acquired capacity of the cancer cell to proliferate in a sustained manner, so as to crowd out and outnumber the normal cell population (23). One of the fundamental differences between a normal and a transformed cell is that normal cells halt proliferation when subjected to growth inhibitory signals or in the absence of growth stimulatory signals (253). But tumor cells act to sustain proliferative signaling in several different ways. They can activate specific genes to produce relevant growth factors, which in turn bind to signaling receptors giving rise to an autocrine loop (254). Growth factors produced by tumor cells can also stimulate the proliferation of stromal cells that in turn produce growth factors to sustain tumor cell proliferation (255). Sustained proliferation can additionally be maintained at the receptor level by truncation of signaling receptor proteins whereby the ligand-activated switch is missing (256). Alternatively, the number of high-affinity receptor proteins may be increased to levels that will sustain proliferative signaling in otherwise normal growth factor levels. Finally, sustained proliferative signaling may well be the result of perpetual activation of the intracellular signaling chain independent of growth factors or receptors (e.g. mutated ras (257) or truncated src (258) are intermediaries of a normal proliferation signaling chain responsible for sustained proliferation).
We hypothesized that disruptive environmental chemicals acting in a procarcinogenic manner by inducing what is referred to as ‘sustained cell proliferation’ likely exerted their action by interfering with some basic control mechanisms (23,253). For instance, they could achieve this by positively regulating targets within and outside the cell known to promote cell proliferation or negatively regulating targets within and outside the cell known to halt cell proliferation. In this way, such chemicals could confer proliferative advantage to a distinct cell population and contribute to that population’s capability to successfully breach innate anticancer defense mechanisms and to become progressively autonomous.
Specifically, we identified a total of 15 ubiquitous chemical disruptors capable of producing sustained cell proliferation. The majority of these chemicals interacted with multiple targets, and we have tabled this information in our review. In summary, we identified several commonly used insecticides and fungicides capable of causing sustained proliferation. These included cyprodinil, etoxazole, imazalil, lactofen, maneb, methoxychlor (MXC), phosalone, prochloraz and pyridaben, all of which targeted estrogen receptor α and frequently other steroid hormone receptors such as androgen receptor (102,259–275). Most of these chemicals also targeted growth factors and their receptors (264,267) and induced cytokines and cytokine receptors (identified by ToxCast high throughput assay). Top disrupting chemical fungicides and insecticides were MXC and cyprodinil, which each interacted with a total of six individual targets that further included the AhR (100), B-lymphocyte markers (ToxCast 2009 high-throughput assay, both chemicals), AP-1 proteins/transcription/translation regulators, downstream signaling molecules and cell cycle regulators (276,277). Other strong performers for sustained proliferation were BPA (activated all targets activated by the insecticides and fungicides above except growth factors and their receptors, B lymphocyte markers and PPAR, but included cell cycle regulators alongside AP-1 proteins/transcription/translation regulators and downstream signaling) (272,276,278,279) (also identified in ToxCast high-throughput assay, 2009), polyfluorinated octinoid sulfate and polybrominated diphenylethers (flame retardants) that either activated AhR (280,281) or up to five other targets that included steroid receptors, growth factors, cytokines and cell cycle regulators (109) (ToxCast high-throughput assay 2009). Three other contenders were phthalates (plasticizers that acted via three targets that included AhR, steroid hormone receptors and PPAR) (282–285), trenbolone acetate (a synthetic anabolic steroid that unsurprisingly acted through steroid hormone receptors) (120,286–290) and finally, edible oil adulterants (food contaminants produced during food processing that acted via downstream signaling) (291,292).
We have shown estrogen and androgen receptors to be important targets in relation to sustained proliferative signaling (293), and note that environmental estrogens and androgens are frequently recognized as prototypical disruptor(s) of this hallmark. Although this is a small sample, there are a great number of chemicals in the environment, both naturally occurring and man-made, are estrogenic, interact with estrogen receptor and produce estrogen metabolites (just as naturally derived ovarian estrogen does during metabolic breakdown). Catechol estrogens (hydroxyl derivatives of estrogens), which are formed during estradiol metabolism, are also potentially important mediators of endogenous estradiol levels, and therefore of sustained proliferative signaling and oncogenesis (294).
Insensitivity to antigrowth signals
Cell cycle arrest is important for maintaining genomic integrity and for preventing genetic errors from being propagated. The normal cell cycle contains multiple checkpoints to safeguard against DNA-damaging agents. Specific proteins at these checkpoints are activated in response to harmful stimuli, ensuring that cellular proliferation, growth and/or division of cells with damaged DNA are blocked.
There are multiple key mediators of growth inhibition that may become compromised during carcinogenesis. Some, such as p53, RB1, and checkpoint kinases cause cells to arrest at the G1–S phase transition when they are activated by DNA damage. Mutations in the p53 gene occur in ~50% of all cancers, although certain tumor types, such as lung and colon, show a higher than average incidence (295). Similarly, pRb hyperphosphorylation (296), direct mutations (297), loss of heterozygosity (298) and disruption of the INK4–pRb pathway (INK4–CDK4/6–pRb–E2Fs) (299) are common events in the development of most types of cancer. Cancer cells may also evade the growth inhibitory signals of transforming growth factor-β (TGF-β) (300) and modulate the action of downstream effectors as well as crosstalk with other pathways.
Cells also receive growth inhibitory signals through intercellular communication via gap junctions. Gap junctions disperse and dilute growth-inhibiting signals, thereby suppressing cell proliferation. In contrast, loss of gap junctions increases intracellular signaling, leading to enhanced proliferation and tumor formation. The molecular components of gap junctions are the connexin proteins (301). Connexins are recognized as tumor suppressors and have been documented to reduce tumor cell growth. Numerous environmental stimuli have been reported to directly affect gap junction intercellular communication. Adherens junction machinery mediates contact inhibition of growth, and loss of contact inhibition is a mediator of tumor cell growth.
Chemicals that may contribute to insensitivity to antigrowth signals through multiple targets of this hallmark are BPA, a common constituent of everyday plastics, and pesticides such as DDT, folpet and atrazine. BPA promotes proliferation by disrupting the growth inhibitory signals of p53 and gap junction communication (171,302). DDT has also been shown to enhance proliferation by increasing the expression of Ccnd1 (cyclin D1)/E2f, inducing phosphorylation of pRb, increasing the expression of p53-degrading protein Mdm2 (a negative regulator of p53) (162) and disrupting gap-junctional intercellular communication (163,164). Folpet down-regulates the functions of p53 and ATM/ATR checkpoint kinases (167) and promotes proliferation, whereas atrazine shows genotoxic effects at subacute dose on Wistar rats. Genotoxicity was also associated with increased transcription of connexin accompanied with increased oxidative stress (303).
Resistance to cell death
Cell death is an actively controlled and genetically regulated program of cell suicide that is essential for maintaining tissue homeostasis and for eliminating cells in the body that are irreparably damaged. Cell death programs include: apoptosis, necrosis, autophagy senescence and mitotic catastrophe (21). Defects in these pathways are associated with initiation and progression of tumorigenesis. Normally, cells accumulate from an imbalance of cell proliferation and cell death, permissive cell survival amidst antigrowth signals such as hypoxia and contact inhibition, resistance to the killing mechanisms of immune cell attack and anoikis resistance (304). Increased resistance to apoptotic cell death involves inhibition of both intrinsic and extrinsic apoptotic pathways.
The link between malignancy and apoptosis is exemplified by the ability of oncogenes, such as MYC and RAS, and tumor suppressor genes, such as TP53 and RB, to engage both apoptosis and the aberrant alterations of apoptosis regulatory proteins such as BCL-2 and c-FLIP in various solid tumors (305). This variety of signals driving tumor evolution provides the selective pressure to alter apoptotic programs during tumor development. Some chemical carcinogens and sources of radiation cause DNA damage and increase genetic and/or epigenetic alterations of oncogenes and tumor suppressor genes leading to loss of cellular homeostasis (306). Other signals include growth/survival factor depletion, hypoxia, oxidative stress, DNA damage, cell cycle checkpoint defects, telomere malfunction and oncogenic mutations, and exposure to chemotherapeutic agents and heavy metals (307,308).
Cancer cells resist apoptotic cell death by up-regulation of antiapoptotic molecules and the down-regulation, inactivation or alteration of pro-apoptotic molecules. Activation of p53 usually induces expression of pro-apoptotic proteins (Noxa and PUMA) and facilitates apoptotic cell death (309). Antiapoptotic Bcl-2 family proteins suppress pro-apoptotic Bax/Bak [which would otherwise inhibit mitochondrial outer membrane permeabilization]. Mitochondrial outer membrane permeabilization releases cytochrome c and triggers apoptosis through an intrinsic pathway (310). Thus, regulation of apoptosis can be achieved by inhibiting the antiapoptotic Bcl-2 family proteins and Bcl-XL proteins as this restores a cell’s ability to undergo apoptosis. In the process, mitochondrial outer membrane permeabilization, mitochondrial proteins (Smac/DIABLO and Omi/HtrA2), which inhibit the X-linked inhibitor of the apoptosis protein, are leaked to trigger caspase activity in apoptosis (311,312).
Normal cellular metabolism is important for the survival of cells, whereas dysregulated metabolism in cells (see Dysregulated metabolism) can induce either apoptosis or resistance to apoptotic stimuli (313). In the liver, nearly every enzyme in glycolysis, in the tricarboxylic acid cycle, in the urea cycle, in gluconeogenesis and in fatty acid and glycogen metabolism is found to be acetylated, and this N-α-acetylation confers sensitivity to apoptotic stimuli (314). The antiapoptotic protein, Bcl-xL reduces the efflux of acetyl-CoA from the mitochondria to the cytosol in the form of citrate and decreases N-α-acetylation of apoptotic proteins, which enables cells less sensitive toward apoptotic stimuli to mediate cell proliferation, growth and survival. Thus, N-α-acetylation might be a major factor in overcoming apoptotic resistance in cancer cells (315,316).
Death receptor ligands such as TRAIL—which is bound to DR4/DR5—induce receptor oligomerization and recruitment of FADD and caspase-8 to form death-inducing signaling complex, which leads to subsequent cell death via apoptosis. Thus, expression of death receptors and their decoy receptors (Dcr1/2) mediates apoptosis in tumor cells (317). When normal cells lose contact with their extracellular matrix or neighboring cells, they undergo an apoptotic cell death pathway known as ‘anoikis’ (304). During the metastatic process, cancerous cells acquire anoikis resistance and dissociate from primary sites, travel through the vascular system and proliferate in distant target organs.
A blockage of gap junction intracellular communication (GJIC) between normal and preneoplastic cells also creates an intra-tissue microenvironment in which tumor-initiated preneoplastic cells are isolated from growth controlling factors of normal surrounding cells resulting in clonal expansion (318). Gap junction channels and Cxs control cell apoptosis by facilitating the influx and flux of apoptotic signals between adjacent cells and hemi-channels between the intracellular and extracellular environments, and Cx proteins in conjunction with their intracytoplasmic localization, may act as signaling effectors that are able to activate the canonical mitochondrial apoptotic pathway (319).
Several anthropogenic chemicals can affect resistance to cell death. For example, BPA has been shown to strikingly impair TP53 activity and its downstream targets, cell cycle regulators, p21WAF1 and RB, or pro-apoptotic BAX, thereby enhancing the threshold for apoptosis (172).
Chlorothalonil, a broad-spectrum fungicide that is used on vegetables, fruit trees and agricultural crops, is considered to be non-genotoxic but classified as ‘likely’ to be a human carcinogen by all routes of exposure (29). In a eukaryotic system, chlorothalonil reacted with proteins and decreased cell viability by formation of substituted chlorothalonil-reduced glutathione derivatives and inhibition of specific nicotinamide adenine dinucleotide thiol-dependent glycolytic and respiratory enzymes (320). Caspases (cysteine-dependent proteases) and transglutaminase are some of the thiol-dependent enzymes involved in apoptosis, so inhibition of these thiol-dependent enzymes in tumor-initiated cells may disrupt apoptotic cell death and aid in tumor survival.
Dibutyl phthalate and diethylhexyl phthalate (DEHP) are diesters of phthalic acid and commonly referred to as phthalates. In general, mimic the function or activity of the endogenous estrogen 17β-estradiol (E2) and bind to estrogen receptors. Interestingly, phthalates can mimic estrogen in the inhibition of TAM-induced apoptosis in human breast cancer cell lines by increasing intracellular Bcl-2/Bax ratio in breast cancer (321).
Lindane, an organochlorine pesticide, bioaccumulates in wildlife and humans. Exposure to lindane induces tumor formation in the mouse 42GPA9 Sertoli cell line by disrupting the autophagic pathway and sustained activation of the mitogen-activated protein kinase (MAPK)/extracellular signal-regulated kinase (ERK) pathway (322).
MXC (1,1,1-trichloro-2,2-bis(4-methoxyphenyl)ethane) is a DDT derivative that was developed after the ban of DDT and it exhibits antiandrogenic and estrogenic activity. MXC stimulates proliferation and human breast cancer cell growth by the up-regulation of genes that involve cell cycle (cyclin D1), and the down-regulation of genes p21 and Bax affecting G1/S transition and apoptosis, respectively, through ERα signaling (323).
Replicative immortality
Cellular senescence is a state of irreversible arrest of cellular proliferation characterized by changes in transcription, chromatin conformation, cytoplasmic and nuclear morphology, DNA damage signaling and a strong increase in the secretion of proinflammatory cytokines (324) Senescence is the first line of defense against potentially transformed cells (325). Progression to malignancy correlates with a bypass of cellular senescence. Thus, senescence inhibits the activation of the tumorigenic process (325). Senescence has been observed in vitro and in vivo in response to various stimuli, including telomere shortening (replicative senescence), oncogenic stress, oxidative stress and chemotherapeutic agents (326).
Cellular senescence exhibits several layers of redundant regulatory pathways. These pathways converge to arrest the cell cycle through the inhibition of CDKs. The best-known effector pathways are the p16INK4a/pRB, the p19ARF/p53/p21CIP1 and the PI3K/mammalian target of rapamycin (mTOR)/FOXO pathways (327–330), which show a high degree of interconnection. Additionally, the pRb and the mTOR pathways are two routes that have been proposed to be responsible for permanent arrest of the cell cycle (331). More pathways and genes are being discovered, increasing the complexity of our knowledge of this physiological process (329). Most, if not all of these genes have been related to human tumorigenesis.
Despite the relevance of senescence as a gatekeeper in the process of tumorigenesis, there is not a large body of information exploring the effect of chemicals on this safeguard. Little research has been undertaken on chemicals that alter gene expression regulating senescence and few genes have been identified (e.g. telomerase, p53, pRb, INK4a) (83,332,333). Traditional protocols for the assessment of the carcinogenic risk rely on the detection of tumors induced by agents that alter many different pathways at the same time (including senescence). These agents are mainly unspecific mutagens or epigenetic modifiers. The effect of some compounds is being explored including nickel-derived compounds (e.g. nickel chloride), diethylstilbestrol, reserpine or phenobarbital (83,334–337).
There may be environmental chemicals that are not mutagens or epigenetic modifiers, but that target specific proteins on the senescence pathways and may affect the initiation of tumorigenesis by other compounds allowing senescence bypass. The contribution of these compounds to the carcinogenesis process is largely unknown. A few compounds bypass senescence in this specific manner—acetaminophen, cotinine, nitric oxide, Na-selenite and lead. Other chemicals known to alter senescence only are mostly unknown (86,88–91,338–341).
Senescence has strong fail-safe mechanisms, and experimental attempts to bypass senescence are usually recognized as unwanted signals and trigger a senescence response anyway. However, these conclusions are based on the interpretations of experimental designs in which acute molecular or cellular alterations are produced. There are few experiments regarding the effects of chronic, low-dose alterations and even fewer studies that consider the different cellular and molecular contexts that can arise over the course of a lifetime.
Dysregulated metabolism
The highly glycolytic cancer phenotype described by Warburg et al. (25) in the early 20th century determined much of the initial direction in cancer research (26). Other characteristic metabolic abnormalities have also been described (25,26,342,343) and have recently garnered increased attention (344–348). These changes are neither fixed nor specific for cancer (349–351), but the universality of metabolic dysregulation suggests major roles in cancer genesis, maintenance and progression. Precise definitions of what constitutes cancer metabolism, and when such changes first occur during the course of cancer development, are lacking. From a teleological perspective, alterations in both intermediary metabolism and its control are not surprising insofar as highly proliferative cancer cells exhibit increased energy demands and expanded requirements for macromolecular precursors to support nucleic acid and protein biosynthesis, as well as membrane biogenesis, for increased biomass. Metabolic reprogramming ostensibly equips cancer cells to cope with these demands, as well as accompanying cellular stresses. Although much of the attention on cancer metabolism has focused on enhanced glucose utilization via glycolytic and pentose phosphate pathways, cancer cells are also capable of the oxidative utilization of carbohydrates, lipids and peptides, and the metabolism of these individual substrate classes remain intimately intertwined as in normal cells (26,345,352).
Major control of glycolysis is traditionally ascribed to glucose transport, hexokinase, phosphofructokinase and pyruvate kinase (352). Glyceraldehyde-3-phosphate dehydrogenase also normally couples glycolytic flux to mitochondrial metabolism in the presence of oxygen and to lactate generation in its absence, but this relationship is fundamentally altered in cancer (26,345,353,354). Given the central importance of the pentose phosphate pathway to anabolic metabolism and redox homeostasis, glucose-6-phosphate dehydrogenase and its redox coupling partners represent similarly attractive carcinogenic targets (355). In addition, the enzymes of the tricarboxylic acid cycle, such as fumarate hydratase, succinate dehydrogenase and isocitrate dehydrogenase, play crucial roles in oxidative energy metabolism and the interconversion of metabolic intermediates, making them appealing candidates for study as well (356,357).
The central importance of the mitochondrial electron transport chain to oxidative energy metabolism and its established role in toxic responses and dysregulated mitochondrial function in cancer makes its assembly and function attractive topics for study (358–360). Despite well-established roles for lipid and amino acid metabolism in cancer development and progression, they have historically received less attention than carbohydrate metabolism (26). Lipogenic, lipolytic and lipophagic phenotypes are now widely recognized (344,361–363), so targets such as acetyl-CoA carboxylase, fatty acid synthase, cellular lipases and lipid transporters represent additional attractive targets for study. Amino acid metabolism—particularly glutamine and serine metabolism—also has well-established roles in cancer (364–366), providing additional potential targets for study that include 3-phosphoglycerate dehydrogenase (346,365,367,368) and cellular transaminase coupling mechanisms. Study of both lipid and protein metabolism must accommodate the fact that cancer cells exhibit substrate preferences, including well-described endogenous lipid- and protein-sparing effects of exogenous glucose availability in cancer cells.
The metabolic capacity of both normal cells and cancer cells generally exceed their catabolic and anabolic requirements (364,369,370), and only a fraction of the available potential energy is ultimately required for cell survival (371,372). Moreover, very small changes in metabolic flux can have profound phenotypic consequences, and metabolic control analysis has suggested that the importance of increased cancer-associated glycolytic and glutaminolytic fluxes may lie not in their magnitudes, but in the maintenance and control of smaller branched pathway fluxes (364). For these reasons, rigorous functional validation is needed for all cancer-associated changes in gene expression or metabolite accumulation. Well-described moonlighting functions for many metabolic enzymes (373–375), including the novel antiapoptotic roles of mitochondrial hexokinases (376), cannot be simply extrapolated from our knowledge of classical roles in cellular metabolism.
These enzymes and their pathways constitute broad categories of potential targets for disruption that could serve to enable the observed metabolic phenotypes of cancer cells (377). Although metabolic control is broadly distributed over all individual steps for a given pathway (352,378), the most obvious targets for conceptual and experimental scrutiny involve major rate-controlling elements of pathways capable of supporting the anabolic and catabolic needs of rapidly proliferating cancer cells.
Numerous studies have demonstrated cancer-associated changes in metabolism or related gene expression (26). We looked at acrolein, copper, cypermethrin, diazinon, hexythiazox, iron, malathion and rotenone as chemicals that had been reported to show relevant disruptive potential (51,379–383); however, the toxicological data that are available for many suspected or known environmental disruptors, generally lacks mechanistic information regarding their potential roles as determinants of the observed metabolic hallmarks of cancer. Even prior metabolic screening platforms, including tetrazolium reduction assays, have limited specificity and can be profoundly influenced by experimental screening conditions. Unfortunately, standardized chemical screening has typically not been conducted under controlled or limiting substrate conditions that would directly inform our understanding of the functional relevance of observed changes. None have established unambiguous causal relationships between specific chemical exposures and the parallel or sequential development of dysregulated metabolism of cancer in the same model, and most observed changes in gene expression with potential relevance to cancer metabolism have not been accompanied by validating functional studies.
Angiogenesis
Angiogenesis, the process of formation of new blood vessels from existing blood vessels, is a critical process for normal organ function, tissue growth and regeneration (e.g. wound healing, female menstruation, ovulation and pregnancy) as well as for pathological conditions (e.g. cancer and numerous non-cancerous diseases, such as age-related macular degeneration, diabetic retinopathy, rheumatoid arthritis, endometriosis, diabetes and psoriasis) (384,385).
Tumor angiogenesis is an early critical event for tumor development: A tumor cannot grow beyond 1mm3 (by estimate) without angiogenesis (386). Tumor growth, invasion and metastasis depend on blood vessels and neovascular development to provide nutrients, oxygen and removal of metabolic waste as tumors grow in primary sites, invade adjacent tissues and metastasize to distant organs (387,388). Inhibition or eradication of tumor angiogenesis by antiangiogenic inhibitors (389,390) or by antineovascular agents (such as vascular-disrupting agents (391–393) and fVII/IgG Fc (394), the latter also called ICON (395–397)) can treat pathological angiogenesis-dependent diseases, including cancer and many non-cancerous diseases.
Under physiological conditions, angiogenesis is well balanced and controlled by endogenous proangiogenic factors and antiangiogenic factors. Factors produced by cancer cells can shift the balance to favor tumor angiogenesis. Such factors include vascular endothelial growth factor (VEGF) and tissue factor (TF). VEGF, one of the most potent proangiogenic factors produced by cancer stem cells and cancer cells, binds to vascular endothelial cells via its receptor VEGFR, initiating VEGF/VEGFR intracellular signal transduction pathways and activating many gene transcriptions and translations toward angiogenesis. TF is a transmembrane receptor (398) not expressed on quiescent endothelial cells (399,400). Upon stimulation of VEGF, TF is selectively expressed by angiogenic endothelial cells, the inner layer of the tumor neovasculature. Thus, TF is a specific biomarker for tumor angiogenesis (408–410). Both of the membrane-bound receptors VEGFR and TF can mediate separate intracellular signaling pathways that contribute to tumor angiogenesis.
Environmental exposures can promote tumor development, but the role of chemicals in tumor angiogenesis, particularly the role of low-dose non-carcinogens, is largely unknown. Some food-use pesticides that are non-genotoxic act as tumor promoters, and other chemicals affect various hallmarks such as apoptosis, proliferative signaling, evading growth suppression, enabling replicative immortality, metastasis, avoiding immune destruction, tumor-promoting inflammation and deregulating cellular energetics—in addition to tumor angiogenesis.
Chemical disruptors that may promote tumor angiogenesis included diniconazole, 2,2-bis-(p-hydroxyphenyl)-1,1,1-trichloroethane (HPTE), methylene bis(thiocyanate), perfluorooctane sulfonate (PFOS), Ziram, biphenyl, chlorothalonil, tributyltin chloride and bisphenol AF. Diniconazole (pesticide), for example, targets certain angiogenic molecules (CXCL9, CXCL10, MMP1, uPAR, VCAM1 and THBD) in vitro (29). MXC (the parent compound to HPTE) induces histological expression of angiogenic factors such as VEGF, VEGFR2 and ANG1 in rat pituitary and uterus (39), and exposure to PFOS induces actin filament remodeling, endothelial permeability changes and ROS production in human microvascular endothelial cells (41). Ziram can induce angiogenesis through activation of MAPK and decreases cytolytic protein levels in human natural killer (NK) cells (404,405).
Tissue invasion and metastasis
Tissue invasion and metastasis are also key processes of tumor progression. In normal cells, E-cadherin holds the epithelial cells together as a society of cells that are well differentiated and otherwise quiescent (406). Carcinomas constitute almost 90% of cancers and upon oncogenic transformation, the process of tissue invasion and metastasis begins with the down-regulation of E-cadherin. Concomitant with this down-regulation of E-cadherin is the conversion of epithelial to mesenchymal cells (EMT) (407). The transcription factors that control EMT, such as snail, slug, Twist and Zeb1/2, are some of the best-characterized signaling molecules in biology (408,409). During the process of EMT, a number of inflammatory cells are attracted to the growing tumor mass (410). Upon attaining mesenchymal characteristics, tumor cells are able to move out of their natural environment, aided by cross talk between them and stromal cells, resulting in the secretion of matrix degrading enzymes such as matrix metalloproteinases (411). This process is accelerated by chronic inflammation mediated by NF-κB (410). Other invasion mediating molecules include hepatocyte growth factor, secreted mainly by tumor-associated fibroblasts to signal metastatic cells to move upon their interactions with their cell surface receptor cMet (412).
Attracted by chemokines, metastatic cells move to the nearest blood vessel or lymphatic vessel, where they complete the process of intravasation, entering the capillaries and are then transported to the capillary bed in their colonized site or new environment (413). In this new location, tumor cells undergo extravasation where they come out of the capillaries or lymphatic vessels, most likely again following the cues emanating from the chemokines in their new microenvironments. To survive in their new home, they may have to revert back and assume the cuboidal morphology of epithelial cells-undergoing the reversal of EMT otherwise known as mesenchymal to epithelial transition (414). At this point, they may remain dormant for a very long time until conditions for their division and growth become favorable.
Mounting evidence supports the involvement of exosomes (nano-vesicles secreted by tumor or cancer-associated fibroblasts) in adhesion and motility of metastatic cells. The secretion of exosomes is accelerated by increases in intracellular calcium ions, and low-dose environmental mixtures that increase intracellular calcium may promote the secretion of exosomes and the subsequent invasion and metastasis processes of the tumor cells.
Environmental chemicals, such as tetrabromobisphenol A and its metabolites, BPA and tetrabromobisphenol A dimethyl ether, which mediate the activation of EMT enzymes or drive their synthesis, may also contribute to the process of tissue invasion (415). Low-dose exposure to hexavalent chromium may accelerate the EMT transition (416). Other contributing factors may also be low-dose environmental contaminants, such as formaldehyde, or bacteria, e.g. H. pylori, that drive the transcription of NF-κB and exacerbate the process (417,418).
Tumor microenvironment
The tumor microenvironment is a complex mix of cells in addition to tumor cells themselves; it is constructed of a complex balance of blood vessels that feed the tumor, the extracellular matrix that provides structural and biochemical support, signaling molecules that send messages, soluble factors such as cytokines and many other cell types. Tumors can influence the microenvironment and vice versa. The micro-environmental reaction to early tumor cells begins with the recruitment and activation of multipotent stromal cells/mesenchymal stem cells, fibroblasts, endothelial cell precursors, antigen-presenting cells such as dendritic cells (DCs) and other white blood cells. All of these tumor stromal cells secrete a variety of growth factors and chemokines that, together with the tumor cells and secreted factors, culminate in the generation of the tumor microenvironment (419–422).
The tumor microenvironment is important because any cell within this process has the potential to be affected by carcinogens, either alone or in mixtures, or by the inflammation that results from the carcinogenic insult (423). Although often associated with infection, chronic inflammation can be caused by exposure to carcinogens such as irradiation or environmental chemicals. Carcinogenesis can also be fostered via effects on the tissue context surrounding preneoplastic lesions. For example, transplantation experiments of preneoplastic cells have clearly documented that a growth-constrained tissue microenvironment can promote the growth and progression of preneoplastic cell populations (424).
Several compounds appear to influence the complex heterogeneity that forms the support network for cancer growth. The exposure to nickel chloride has been associated with the generation of ROS and inflammation (425). ROS are important because they can stimulate the induction of angiogenesis growth factors, such as VEGF, and can promote cell proliferation and immune evasion and play a role in cell survival (57,426–428). Prenatal exposure to BPA in experimental animals disrupts ERα and triggers angiogenesis, and other BPA exposure studies have demonstrated that BPA interplays with cell proliferation (226), genomic instability (429), inflammation (430) and cell immortalization (431). Butyltins, and specifically tributyltin, which is suspected to act as an endocrine disruptor, have been found to inhibit the cytotoxic activity of NK cells (432), affect inflammation (432) and disrupt membrane metalloproteinases (432). Cooperatively, disruption of these processes can lead to proliferation, migration and angiogenesis. Methylmercury (MeHg) is a neurotoxic compound deriving from metallic mercury through bacteria-supported metabolism in an aquatic environment. Bio-concentration in fish and shellfish poses a risk for sensitive population categories such as pregnant women and infants. MeHg-induced ROS production may be involved in inflammation and apoptosis (433) as well as endothelial cell cytotoxicity (434). We also looked at paraquat, which may also have relevance for the tumor microenvironment via its role in oxidative stress (435,436).
Avoiding immune destruction
The concept of immune surveillance suggests that the host immune system could identify tumor cells and destroy them. If this is true, tumor cells need to be poor stimulators of or challenging targets for the host immune system. To provide an effective immune response, multiple types of the cells are involved within innate and adaptive immune ‘arm’ with some cells (e.g. DCs and the NK cells) ‘bridging’ these two types of immunity (437). To avoid a strong immune response of the host, the expression of tumor antigens may be down-regulated or altered (resulting in decreased or impossible recognition of malignant cells) (438) and various soluble factors and cytokines may be released resulting in subverted effectiveness of antitumor immune response (439–441). Tumor cells can also escape host immune response by inducing apoptosis in activated T cells (442).
Multiple genes involved in immune evasion mechanisms and, therefore, can interfere with chemical exposures from anthropogenic environment: ADORA1 (adenosine A1 receptor), AKT1 (v-akt murine thymoma viral oncogene homolog 1), CCL2 (chemokine C-C motif ligand 2), CCL26 (chemokine C-C motif ligand 26), CD40, CD69, COL3A1 (type III collagen of extracellular matrix), CXCL10 (also called interferon-inducible protein-10), CXCL9 (monokine induced by interferon-γ), EGR1 (early growth response protein 1), HIF-1α (hypoxia-inducible factor), IGF1R (insulin-like growth factor 1 receptor) and interleukins (IL) such as IL-1α and IL-6. Based on available studies, several candidate signaling pathways that are related to the host immune response can be identified for further study; e.g. the pathways involving PI3K/Akt, chemokines, TGF-β, FAK, IGF-1, HIF-1α, IL-6, IL-1α, CTLA-4 and PD-1/PDL-1.
Biologically disruptive environmental chemicals can affect the host immune responses as follows: (i) if a certain chemical is immunotoxic, and, in particular, if it affects activity of DCs, T cells or NK cells, it is also likely to affect tumor immuno-surveillance and enable malignant growth to proceed; (ii) if a chemical targets the immune system, it can increase the cancer risk related to other factors/exposures; (iii) exposures to certain toxins or toxicants can dramatically increase the number of cancerous cells and impact immuno-regulatory signals suppressing the mechanisms of immune control. Collectively, these sorts of actions suppress the immune system, so it cannot be effectively stimulated and cannot eliminate tumor cells, thus allowing some tumor cells to escape and metastasize.
We looked at several groups of environmentally ubiquitous chemicals such as pesticides and personal care products that might potentially interrelate with mechanisms of tumor immuno-surveillance. Although none of them are recognized as human carcinogens (443–445), the research on these chemicals and their interactions with the immune response may be valuable. For example, the fungicide maneb is a cortisol disruptor (446) that has shown a wide spectrum of potential effects on multiple pathways, including some that are relevant to immune evasion (139,156–158,447). By comparison, pyraclostrobin and fluoxastrobin (448) interfere with a narrower spectrum of cancer hallmarks (36,449–452). Atrazine has also shown potential to impact immune system evasion by directly targeting maturation of DCs and decreasing the levels of major histocompatibility complex class I molecules (243,453). The insecticides pyridaben and azamethiphos can also both be disruptive to immuno-surveillance (139,140,454,455).
Commonly used in personal care products, triclosan and BPA (456), are endocrine disruptors (457–459) that are often detected in waters downstream in urban areas (460,461). In addition to immune evasion mechanisms (36,142,145), they interfere with wide spectrum of cancer-related mechanisms (36,173,429,462–464). DEHP (472) is also an endocrine disruptor (466,467) that can impact multiple hallmarks such as immune evasion, resistance to cell death, evasion of antiproliferative signaling, sustained proliferative signaling and tumor-promoting inflammation (36,288,468,469).
Knowing whether or not cumulative low-dose exposures to these chemicals interfere with the host immune response can help to stimulate further studies (e.g. on screening of lesions at the pre-malignant stage of tumor development) to determine the influence of such exposures on host immunity and to evaluate their potential to increase the risk of tumor cell survival.
Dose-response characterizations and LDE
For all the chemicals selected and target sites for disruption that were identified, dose-response characterization results and/or relevant low-dose research evidence were reviewed and categorized using the criteria mentioned in the Materials and methods. Table 1 sets out these results and the supporting references.
In total, 85 examples of environmental chemicals were reviewed (for specific actions on key pathways/mechanisms that are important for carcinogenesis) and 59% of them (i.e. 50/85) were found to exert LDE (at levels that are deemed relevant given the background levels of exposure that exist in the environment) with 15 of the 50 demonstrating their LDE in a non-linear dose-response pattern. Indeed, all of the teams selected at least one or more disruptive chemicals that exerted their effects on the target sites at low-dose levels. In contrast, only 15% of the chemicals reviewed (i.e. 13/85) showed evidence of a threshold.
The remaining 26% of the chemicals reviewed (i.e. 22/85) were categorized as ‘unknown’. Some of these chemicals (5 of the 22) had been tested using human primary cell data from ToxCast and had showed statistically significant activity across a full range of doses against the specified targets (i.e. they were active even at the lowest test concentrations of ~0.01 µM). However, even though no threshold could be discerned for these chemicals, we did not characterize them as having LDE (because it was not clear that the lowest test concentrations were low enough to be equated to levels of exposure that are normally seen in the environment).
Evidence of cross-hallmark relationships
Teams then evaluated the chemicals selected and target sites for disruption for known effects on the other cancer hallmark pathways. Evidence in the literature that showed procarcinogenic actions or anticarcinogenic actions in other hallmark areas were reported, and in instances where no literature support was found, this was documented as well. The same approach was used for the chemicals that were reviewed. A sample of these cross-hallmark results is provided in Table 2—Sample of cross-hallmark relationships of target pathways/mechanisms and in Table 3—Cross-hallmark relationships of selected chemical disruptors.
Table 2.
Sample of cross-hallmark relationships of target pathways/mechanisms
| Insensitivity to antigrowth signals (targets) | Antigrowth | Dysreg metab | Gen instab | Angio | Cell death | Immun | Immort | Prolif | Metas | Inflamm | Tumor micro | PRO | ANTI | MIX |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| p53 | n/a | +/− | - | +/− | − | +/− | − | − | − | + | + | 2 | 5 | 3 |
| pRB | n/a | +/− | − | − | − | 0 | − | − | − | + | + | 2 | 6 | 1 |
| TGF-β | n/a | + | − | + | − | + | − | + | + | + | + | 7 | 3 | 0 |
| LKB1 | n/a | + | − | + | +/− | 0 | 0 | + | − | + | + | 5 | 2 | 1 |
| Connexins | n/a | − | − | 0 | 0 | 0 | 0 | − | +/− | + | + | 2 | 3 | 1 |
| Contact inhibition | n/a | +/− | − | 0 | 0 | + | 0 | − | − | + | − | 2 | 4 | 1 |
One set of results (from the insensitivity to antigrowth signals review) is shown here without references to support a discussion on the range of effects that have been reported for the selected targets in each article. Specific references supporting these effects for any given hallmark area can be found in the individual reviews within this special issue. Cross-hallmark relationships are reported in the first 11 columns of the table—table heading abbreviations are as follows:gen instab, genetic instability; dysreg metab, dysregulated metabolism; antigrowth, insensitivity to antigrowth signals; angio, angiogenesis; cell death, resistance to cell death; immun, avoiding immune destruction; immort, replicative immortality; prolif, sustained proliferative signaling; metas, tissue invasion and metastasis; inflamm, tumor-promoting inflammation; tumor micro, tumor microenvironment. The number of procarcinogenic (PRO), anticarcinogenic (ANTI) and mixed (MIX) (i.e. procarciniogenic and anticarcinogenic reports) cross-hallmark relationships for each target have been summed and are reported in the last three columns of the table. Target pathways/mechanisms for each hallmark area were evaluated by each team for known effects in other cancer hallmark pathways. Targets that were found to have anticarcinogenic actions in another hallmark area were indicated with ‘−’, whereas targets that were found to have procarcinogenic actions in another hallmark area were indicated with ‘+’. In instances where reports on relevant actions in other hallmark areas were mixed (i.e. reports showing both procarcinogenic potential and anticarcinogenic potential), the symbol ‘+/−’ was used. Finally, in instances where no literature support was found to document the relevance of a target in a particular aspect of cancer’s biology, we documented this as ‘0’.
Table 3.
Cross-hallmark relationships of selected chemical disruptors
| Insensitivity to antigrowth signals (disruptors) | Antigrowth | Dereg metab | Gen instab | Angio | Cell death | Immun | Immort | Prolif | Metas | Inflamm | Tumor micro | PRO | ANTI | MIX |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BPA | n/a | + | + | + | +/− | 0 | + | + | + | + | 0 | 7 | 0 | 1 |
| DDT | n/a | 0 | + | + | + | + | + | + | 0 | + | 0 | 7 | 0 | 0 |
| Folpet | n/a | 0 | + | 0 | + | 0 | 0 | + | 0 | + | 0 | 4 | 0 | 0 |
| Atrazine | n/a | 0 | + | 0 | 0 | 0 | 0 | + | 0 | + | 0 | 3 | 0 | 0 |
One set of results (from the insensitivity to antigrowth signals review) is shown here without references to support a discussion on the range of effects that have been reported for the selected disruptors in each review. Specific references supporting these effects for any given hallmark area can be found in the individual reviews within this special issue. Cross-hallmark relationships are reported in the first 11 columns of the table— table heading abbreviations are as follows:gen instab, genetic instability; dereg metab, dysregulated metabolism; antigrowth, insensitivity to antigrowth signals; angio, angiogenesis; cell death, resistance to cell death; immun, avoiding immune destruction; immort, replicative immortality; prolif, sustained proliferative signaling; metas, tissue invasion and metastasis; inflamm, tumor-promoting inflammation; tumor micro, tumor microenvironment. The number of procarcinogenic (PRO), anticarcinogenic (ANTI) and mixed (MIX) (i.e. procarciniogenic and anticarcinogenic reports) cross-hallmark relationships for each target have been summed and are reported in the last three columns of the table. Prototypical chemical disruptors selected by each team were evaluated for reported actions in other cancer hallmark pathways. Disruptors that were found to have anticarcinogenic actions in a particular hallmark area were indicated with ‘−’, whereas disruptors that were found to have procarcinogenic actions in a particular hallmark area were indicated with ‘+’. In instances where reports on relevant actions in other hallmarks were mixed (i.e. reports showing both procarcinogenic potential and anticarcinogenic potential), the symbol ‘+/−’ was used. Finally, in instances where no literature support was found to document the relevance of a chemical in a particular aspect of cancer’s biology, we documented this as ‘0’. Specific references supporting these effects for any given area can be found in the individual reviews in this special issue.
Note that Tables 2 and 3 contain just a single set of unreferenced results from the review on the hallmark insensitivity to antigrowth signals. This is intended only to illustrate the categories of cross-hallmark effects that were reviewed and to show how they were presented. Fully referenced results for each hallmark area can be found in each of the individual reviews within this special issue.
The decision to review target sites for disruption and prototypical disruptors for cross-hallmark effects was driven by the fact that many individual studies and reviews of chemical exposures fail to account systematically for the spectrum of incidental actions that can result from exposures to a single given chemical. It was our belief that this approach constitutes a better way to ensure that we had assembled a reasonably complete view of the literature (i.e. where any sort of evidence of cross-hallmark activity had been reported). Future research will likely involve empirical testing of mixtures, so we wanted to create a heuristic that could serve as a starting point for other researchers who might be considering such research.
For researchers focused on low-dose exposure research intended to produce carcinogenesis, we anticipated that there would be interest in chemicals that had been reported to exhibit a large number of procarcinogenic actions across a number of hallmarks and we anticipated that a lack of anticarcinogenic potential would be important to identify (as targets or approaches that exert anticarcinogenic actions would potentially represent a confounding influence/factor in empirical research aimed at the identification of carcinogenic synergies). To that end, Table 4 provides a summary of the aggregated number of procarcinogenic actions, anticarcinogenic actions and instances where mixed actions (i.e. procarciniogenic and anticarcinogenic) have been found for each pathway/mechanism (across the full range of hallmark domains—i.e. from all of the areas covered by the reviews in this special issue). Similarly, Table 5 provides a summary of the aggregated number of procarcinogenic actions, anticarcinogenic actions and mixed actions (i.e. procarcinogenic and anticarcinogenic), where cross-hallmark effects have been reported for each chemical (across the full range of hallmark domains—i.e. from all of the areas covered by the reviews in this special issue).
Table 4.
Aggregated evidence of cross-hallmark effects for selected pathways/mechanisms
| Key targets | Originating review | Procarcinogenic | Anticarcinogenic | Mixed |
|---|---|---|---|---|
| Adenosine A1 receptor (ADORA1) | ISE | 3 | 1 | 0 |
| AhR | Ang | 7 | 0 | 2 |
| SPS | 7 | 0 | 2 | |
| Bcl-2/p53 | RCD | 6 | 2 | 1 |
| Cell cycle/cell division: spindle defect | GI | 6 | 0 | 1 |
| Checkpoint kinase 1 and checkpoint kinase 2 (Chk1/2) | EAS | 4 | 3 | 1 |
| Chemokine (C-C motif) ligand 2 (CCL2) | Ang | 8 | 1 | 0 |
| Chemokine (C--XC motif) ligand 10 (CXCL10) | Ang | 4 | 1 | 1 |
| Chemokine (C--XC motif) ligand 9 (CXCL9) | Ang | 3 | 2 | 0 |
| Chemokine signaling pathway (CCL2, CCL26, CXCL9, CXCL10) | ISE | 6 | 1 | 2 |
| Chronic oxidative stress | TM | 6 | 1 | 1 |
| Clock-genes-mediated metastasis | TIM | 5 | 1 | 0 |
| Collagen type III (COLIII) | Ang | 3 | 0 | 0 |
| Contact inhibition | EAS | 4 | 3 | 0 |
| cSrc/Her1/STAT5B/ERK1/2 | TIM | 3 | 1 | 1 |
| Cyclin D, IL8, CXCL | SPS | 4 | 0 | 2 |
| Cyclooxygenase expression and stimulation calcium signaling in migration. | TIM | 8 | 1 | 0 |
| Cyclooxygenase-2 | TPI | 8 | 1 | 0 |
| DNA damage signaling: disturbed by Redox signaling (NF-κB, Nrf, EGR) | GI | 8 | 1 | 0 |
| DNA repair pathways | GI | 6 | 2 | 1 |
| Eck fatty acid metabolism | DM | 6 | 1 | 2 |
| Electron transport chain complexes II and IV | DM | 3 | 2 | 0 |
| Epidermal growth factor receptor | SPS | 6 | 0 | 1 |
| Epigenetic pathways | ||||
| Disturbed miRNA binding | GI | 6 | 0 | 2 |
| DNA methylation | GI | 7 | 0 | 1 |
| Histone acetylation | GI | 6 | 1 | 1 |
| EMT | TIM | 5 | 0 | 1 |
| EMT, catenin-Wnt pathway | TIM | 6 | 1 | 1 |
| ErbB-2/HER-2 tyrosine kinase | RCD | 6 | 1 | 0 |
| ERK/MAPK | RCD | 8 | 2 | 0 |
| Estrogen receptor | TPI | 5 | 3 | 1 |
| Estrogen receptor α (binding to) | RCD | 5 | 1 | 1 |
| Gap junction connexins | EAS | 2 | 2 | 2 |
| GJIC | RCD | 2 | 1 | 1 |
| Gluconeogenesis | DM | 5 | 3 | 0 |
| Glycolysis | DM | 8 | 1 | 0 |
| Hexokinase 2 | DM | 6 | 1 | 0 |
| H-Ras | SPS | 6 | 1 | 2 |
| Hypersecretion of luteinizing hormone by gonadotroph cells in pituitary gland | RCD | 2 | 1 | 0 |
| HIF-1-α pathway | ISE | 8 | 0 | 2 |
| Inducible nitric oxide synthase | TPI | 6 | 1 | 0 |
| IGF-1 signaling pathway | ISE | 6 | 2 | 1 |
| Intercellular adhesion molecule 1 (ICAM1) | Ang | 6 | 3 | 0 |
| IL-6 | TPI | 7 | 0 | 0 |
| IL-6 expression, improper DC maturation and polarization | TM | 5 | 2 | 0 |
| Jun/Fos/AP1 | SPS | 4 | 1 | 3 |
| Lipid metabolism/cholesterol metabolism | DM | 4 | 2 | 1 |
| Liver kinase B1 (Lkb1) | EAS | 4 | 2 | 2 |
| MMP 1 | Ang | 6 | 1 | 0 |
| MMP-9 activation | TIM | 5 | 1 | 1 |
| Mitochondrial function | GI | 5 | 2 | 2 |
| MAPK | RCD | 9 | 0 | 1 |
| mTOR activation | DM | 7 | 1 | 1 |
| mTOR inactivation | RI | 3 | 6 | 1 |
| NK cell inhibition | TM | 4 | 3 | 0 |
| NF-κB | TPI | 4 | 2 | 0 |
| Oxidative stress and IL-6 production | TM | 3 | 1 | 1 |
| P16/p53 | RCD | 4 | 4 | 0 |
| P53 inactivation | EAS | 10 | 0 | 0 |
| RCD | 10 | 0 | 0 | |
| RI | 10 | 0 | 0 | |
| PPAR | SPS | 5 | 2 | 0 |
| PPAR-α | RCD | 3 | 3 | 1 |
| PI3K/Akt signaling pathway | ISE | 9 | 0 | 1 |
| Pyruvate dehydrogenase (PDH) | DM | 1 | 5 | 0 |
| ROS (increase) | DM | 6 | 0 | 4 |
| ROS and cellular stress | TM | 5 | 0 | 4 |
| Retinoblastoma protein (pRb) inactivation | EAS | 9 | 0 | 0 |
| RI | 9 | 0 | 0 | |
| Steroid hormone receptors | SPS | 5 | 0 | 1 |
| Telomerase activation | RI | 9 | 1 | 0 |
| Telomere loss | GI | 4 | 4 | 0 |
| The tricarboxylic acid cycle | DM | 5 | 4 | 0 |
| Thrombomodulin | Ang | 2 | 3 | 0 |
| Transforming growth factor β | EAS | 6 | 3 | 1 |
| Tumor necrosis factor α | TPI | 8 | 0 | 1 |
| Urokinase receptor (uPAR) | Ang | 6 | 2 | 0 |
| Vascular cell adhesion molecule 1 (VCAM1) | Ang | 6 | 0 | 0 |
Aggregated number of procarcinogenic actions, anticarcinogenic actions and instances where mixed actions (i.e. procarciniogenic and anticarcinogenic) where cross-hallmark effects have been reported (for each pathway/mechanism across the full range of hallmark domains—i.e. from all of the areas covered by the reviews in this special issue)—see samples of this data in Table 2. Note: fully referenced data for these cross-hallmark effects can be found in each of the reviews in this special issue. ANG, angiogenesis; DM, dysregulated metabolism; EAS, evasion of antigrowth signaling; GI, genetic instability; ISE, immune system evasion; RCD, resistance to cell death; RI, replicative immortality; SPS, sustained proliferative signaling; TIM, tissue invasion and metastasis; TM, tumor microenvironment; TPI, tumor-promoting inflammation.
Table 5.
Aggregated evidence of cross-hallmark effects for selected chemical disruptors
| Chemicals | Originating review | Procarcinogenic | Anticarcinogenic | Mixed |
|---|---|---|---|---|
| 12-O-Tetradecanoylphorbol-13-acetate | SPS | 5 | 1 | 0 |
| HPTE | ANG | 4 | 0 | 0 |
| Acetaminophen | RI | 0 | 4 | 2 |
| Acrolein | DM | 3 | 3 | 3 |
| Acrylamide | GI | 3 | 1 | 1 |
| Atrazine | ISE | 3 | 0 | 1 |
| EAS | 4 | 0 | 1 | |
| TPI | 3 | 0 | 1 | |
| Azamethiphos | ISE | 1 | 0 | 0 |
| Benomyl | GI | 0 | 3 | 1 |
| Benzo(a)pyrene | SPS | 8 | 1 | 0 |
| Biorhythms | TIM | 3 | 2 | 0 |
| Biphenyl | ANG | 2 | 2 | 1 |
| BPA | EAS | 6 | 0 | 1 |
| GI | 6 | 0 | 1 | |
| ISE | 7 | 0 | 1 | |
| RCD | 7 | 0 | 0 | |
| SPS | 6 | 0 | 1 | |
| TIM | 7 | 0 | 1 | |
| TM | 7 | 0 | 1 | |
| TPI | 6 | 0 | 1 | |
| Bisphenol AF | ANG | 5 | 1 | 0 |
| Butyltins (such as tributyltin) | TM | 4 | 2 | 0 |
| C.I. solvent yellow 14 | ANG | 4 | 0 | 0 |
| Carbendazim | GI | 0 | 2 | 1 |
| Carbon black | GI | 5 | 1 | 0 |
| Chlorothalonil | ANG | 5 | 1 | 0 |
| RCD | 5 | 0 | 0 | |
| Cobalt | GI | 5 | 2 | 0 |
| Copper | DM | 6 | 0 | 3 |
| Cotinine | RI | 4 | 1 | 0 |
| Cypermethrin | DM | 5 | 0 | 0 |
| DDT | EAS | 6 | 0 | 0 |
| Diazinon | DM | 2 | 3 | 0 |
| Dibutyl phthalate | RCD | 4 | 0 | 0 |
| Dichlorvos | RCD | 4 | 0 | 0 |
| DEHP | ISE | 4 | 0 | 1 |
| RCD | 4 | 0 | 0 | |
| Diniconazole | ANG | 2 | 0 | 0 |
| Fluoxastrobin | ISE | 2 | 1 | 0 |
| Folpet | EAS | 2 | 1 | 0 |
| Hexachlorobenzene | TIM | 5 | 2 | 0 |
| Hexythiazox | DM | 0 | 0 | 0 |
| Imazalil | SPS | 3 | 1 | 0 |
| Iron | DM | 5 | 1 | 3 |
| TIM | 5 | 1 | 2 | |
| Lactofen | SPS | 2 | 0 | 0 |
| Lead | GI | 3 | 1 | 0 |
| RI | 3 | 1 | 0 | |
| Lindane | RCD | 5 | 0 | 0 |
| Linuron | RCD | 2 | 0 | 0 |
| Malathion | DM | 5 | 0 | 0 |
| Maneb | ISE | 4 | 2 | 0 |
| Mercury | GI | 3 | 2 | 1 |
| MXC | RCD | 3 | 0 | 0 |
| Methylene bis(thiocyanate) | ANG | 2 | 1 | 0 |
| MeHg | TM | 5 | 2 | 0 |
| Na-selenite | RI | 0 | 4 | 2 |
| Nickel | GI | 6 | 1 | 1 |
| TM | 6 | 1 | 1 | |
| Nickel chloride | RI | 6 | 0 | 2 |
| Nitric oxide | RI | 5 | 2 | 2 |
| 4-NP | TPI | 2 | 1 | 0 |
| Oxyfluorfen | RCD | 4 | 0 | 0 |
| Paraquat | GI | 4 | 2 | 0 |
| TM | 4 | 2 | 0 | |
| PFOS | ANG | 4 | 1 | 0 |
| SPS | 4 | 1 | 0 | |
| Phosalone | SPS | 1 | 1 | 0 |
| Phthalates | TIM | 6 | 0 | 1 |
| TPI | 6 | 0 | 1 | |
| PBDEs | TPI | 2 | 0 | 2 |
| Pyraclostrobin | ISE | 2 | 1 | 0 |
| Pyridaben | ISE | 1 | 3 | 1 |
| Quinones | GI | 1 | 6 | 1 |
| Rotenone | DM | 2 | 5 | 1 |
| Sulfur dioxide | TIM | 5 | 1 | 0 |
| Titanium dioxide NPs | GI | 3 | 1 | 1 |
| Tributyltin chloride | ANG | 3 | 1 | 0 |
| Triclosan | GI | 2 | 2 | 1 |
| ISE | 3 | 2 | 1 | |
| Tungsten | GI | 2 | 1 | 1 |
| Vinclozolin | TPI | 2 | 1 | 0 |
| Ziram | ANG | 3 | 1 | 1 |
Aggregated number of procarcinogenic actions, anticarcinogenic actions and mixed actions (i.e. procarciniogenic and anticarcinogenic) where cross-hallmark effects have been reported (for each chemical across the full range of hallmark domains—i.e. from all of the areas covered by the reviews in this special issue)—see samples of this how this data were reported in Table 3. Note: fully referenced data for these cross-hallmark effects can be found in each of the reviews in this special issue. ANG, angiogenesis; DM, dysregulated metabolism; EAS, evasion of antigrowth signaling; GI, genetic instability; ISE, immune system evasion; RCD, resistance to cell death; RI, replicative immortality; SPS, sustained proliferative signaling; TIM, tissue invasion and metastasis; TM, tumor microenvironment; TPI, tumor-promoting inflammation.
Note that, in some instances, the underlying evidence used to support the indication of cross-hallmark relationships was robust, consisting of multiple studies involving detailed in-vitro and in-vivo findings. In other instances, the underlying evidence that was used to report the existence of a cross-hallmark relationship was quite weak (e.g. consisting of only a single in-vitro study involving a single cell-type). The selected prototypical disruptors are likely biased towards agents that have been extensively studied, and not necessarily those that will prove to be the most important biologically. Finally, there are examples of chemicals that are known to exert different effects at different dose levels, but dose levels were not used to discriminate when gathering evidence of cross-hallmark effects. So, the referenced cross-validation results in the individual tables (reported in the many reviews within this special issue) should be seen only as a starting point for those who are pursuing mixtures research (e.g. references would need to be further scrutinized to determine whether or not the dose levels noted for specific results are suitable points of reference for the type of research that is being undertaken).
Particular attention should also be given to results related to the endocrine system due to mechanistic complexity. For example, xeno-estrogen compounds are typically compared with estradiol based on binding affinity strength. However, many xeno-estrogens that are ‘weak’ by this measure can alter the steroidogenic cascade (e.g. significantly up-regulate the activity of P450 aromatase, the enzyme that increases intracellular estradiol synthesis within estrogen-sensitive cells (470–473) or alter levels of ERα or the ratio of ERα:ERβ (260)). In other words, a weak xeno-estrogen can stimulate the production of estradiol, a potent endogenous carcinogen (474) or alter the receptors with which a cell will respond to estrogen.
Nonetheless, given that the overarching goal in this project was to create a foundation that would allow researchers to look systematically across the literature in each of these areas, the tables should serve as a useful starting point as long as they are approached with these caveats in mind. We believe that this heuristic will be useful to consider synergies that might be anticipated in testing that involves certain target sites for disruption and/or mixtures of chemical constituents that are being considered for procarcinogenic effects. Future research efforts to improve this approach could involve a large-scale collaborative effort to generate high-quality in-vitro data and low-dose in-vivo data in a range of predefined tissues.
Discussion
Getting to Know Cancer hosted the initial project meeting in Halifax, Nova Scotia giving participants an opportunity to have presentations, break-out sessions, and chances for conversation and debate among experts who came from a range of different disciplines. Cancer biologists with specialized expertise in areas related to individual hallmarks met with specialists from other areas such as environmental health, toxicology and endocrinology. Although some researchers in the field of environmental health are cancer scientists in their own right, many conference participants commented on the novelty of having an opportunity to work so closely with cancer biology specialists. As a result, many interdisciplinary barriers were removed and the discussions that ensued were challenging but productive.
At the outset, participants overwhelmingly agreed that the Hallmarks of Cancer provides a useful organizing heuristic for systematic review of ways that biologically disruptive chemicals might exert procarcinogenic and anticarcinogenic influences in biological systems. Most of the individual writing teams were then readily able to identify ubiquitous environmental contaminants with disruptive potential in their respective areas of study. The only teams that had significant challenges in this regard were the ones that focused on the bypassing of senescence (i.e. replicative immortality) and dysregulated metabolism, both being areas of cancer research that have not yet received a lot of attention from researchers in the field of toxicology.
Considerable discussion was devoted to the criteria that were used to select prototypical disruptors from the long list of known potential contaminants. Indeed, it seems that much of the population is now exposed to a wide variety of exogenous chemicals that have some disruptive potential, but we did not have any intention of implicating any of the selected chemicals as being carcinogenic per se. It was simply agreed that chemicals would be chosen that met the basic criteria and that then could be used as ‘prototypical’ disruptors. In other words, the chemicals that were selected for this review were not deemed to be the most important, and they were not selected to somehow imply (based on current information) that they are endangering us. Rather, we simply wanted to illustrate that many non-carcinogenic chemicals (that are ubiquitous in the environment) have also been shown to exert effects at low doses, which are highly relevant to the process of carcinogenesis. We also wanted to lay out a heuristic framework that would be helpful for other researchers who are interested in considering these and other chemicals as potential constituents for low-dose mixtures research.
LDE, chemical mixtures and carcinogenicity
Although we did not specifically ask the teams to focus on disruptive chemicals that were known to exert LDE, the summary of dose-response characterizations for the chemicals that were selected by these teams is dominated by chemicals (i.e. 50/85) that have been shown to produce LDE, and 15 of the 50 showed evidence of a non-linear dose-response. Surprisingly, only 15% of the chemicals reviewed (i.e. 13/85) showed evidence of a threshold. We believe that this helps to validate the idea that chemicals can act disruptively on key cancer-related mechanisms at environmentally relevant levels of exposure.
Historically, the axiom ‘the dose makes the poison’ has had some merit, so many people remain skeptical about the idea that adverse outcomes can result from minute exposures to commonly encountered chemicals. But we are now at a point in time where our knowledge of the biology of cancer has advanced considerably, and we know that carcinogenesis can begin when key events have occurred in a single cell, between cells or in the surrounding microenvironment. So the idea that LDE from many environmental chemicals (acting together) might serve to instigate, support or fully enable carcinogenesis, no longer appears to be an unreasonable assertion.
At this stage, we are not making any assumptions about whether or not future empirical research will find support for this hypothesis, nor are we assuming that this a significant problem. We are simply impressed by the fact that we are now starting to see evidence of a wide range of LDE (that are directly related to carcinogenesis) that can be exerted by chemicals that are ubiquitous and unavoidable in the environment. As a result, we are compelled to explore and consider this possibility.
In-utero exposures and transgenerational effects
Additionally, a number of the teams cited in-utero exposure studies in their reviews and presented evidence on transgenerational effects. Although this detail is not fully captured in the team summaries offered in this capstone paper (please see the individual reviews in this special issue for complete details), these effects are important to acknowledge. For example, the inflammation team noted that transient early life exposures in utero to vinclozolin have been linked to both adult-onset disease and transgenerational disease that involves inflammation. Similarly, the immune system evasion team reported that there is increasing evidence from animal studies that in-utero or neonatal exposures to BPA are associated with higher risk of immune system dysregulation that may develop later in life.
Taken together, these and other similar types of examples raise intriguing possibilities about vulnerabilities at the population level, and the contributions that in utero and early life exposures to mixtures of those chemicals might make towards cancer susceptibility. Single-generation experimental models are inadequate to detect this sort of disruptive activity (for exposures to a given chemical or to mixtures of chemicals), but these sorts of effects may increase cancer risks by promoting and/or enabling tumorigenesis.
The interplay between genetic factors and environmental factors
Given the number of key cancer-related mechanisms that can apparently be disrupted by chemicals that are commonly found in the environment, and the possibility that in-utero and/or early life exposures may also contribute to population vulnerability, the interplay between genetic factors and environmental factors should also be mentioned. For example, a hereditary genetic vulnerability (such as mutations to BRCA1/2 genes which greatly increase the lifetime risk of breast and ovarian cancer (482)) can predispose someone to a higher risk of cancer. But many hereditary genetic mutations and somatic mutations do not result in cancer, presumably because additional actions (e.g. sustained proliferative signaling) are needed or additional biological safeguards still need to be suppressed or defeated (e.g. apoptosis, senescence, immuno-surveillance and so on) before a fully immortalized cellular phenotype can emerge. In these instances, cancer may not be assured, but it is easy to see how the disruptive effects of low-dose exposures to certain chemicals might act on key pathways/mechanisms and play a supporting role in the steps involved in carcinogenesis and/or increase the overall risk of getting cancer.
This same issue applies to other sensitive subpopulations who might be predisposed to higher levels of cancer risk. In some instances, vulnerabilities that exist are genetic in nature (e.g. cancer patients in remission), due to endogenous factors (e.g. due to obesity) or due to external influences (i.e. smoking). But in all cases, the enhanced risks in these subpopulations leave the affected individuals vulnerable to carcinogenesis. Although a detailed investigation of this type of interaction is beyond the scope of this project, it is important to consider that low dose, disruptive chemical effects on key pathways and mechanisms in these subpopulations may serve to further enhance cancer susceptibility, or even fully enable carcinogenesis.
The low-dose carcinogenesis hypothesis
It is important to reiterate that this group has no interest in implicating any of the chemicals that were reviewed in this project as individual carcinogens per se. We fully realized at the outset that much of the evidence in the toxicological literature that documented the disruptive actions of these chemicals had been produced under a wide range of differing experimental circumstances. So it was agreed at the beginning that we would not make leaps between different lines of evidence nor draw any specific conclusions about chemical mixtures that might prove to be carcinogenic. Nonetheless, we are intrigued by the number of chemicals that we reviewed that were found to be capable of disruptive LDE on key pathways/mechanisms across all of the areas that were reviewed. Many of the environmental chemicals that we chose are well known as environmental contaminants, but they represent only a small fraction of the thousands of chemicals that are now ubiquitous and unavoidable in the environment. So although we cannot draw any firm conclusions at this stage, we emerge from this effort with a better understanding of the evidence that is available to support the merits of our initial hypothesis (i.e. that low-dose exposures to disruptive chemicals that are not individually carcinogenic may be capable of instigating and/or enabling carcinogenesis).
Although the breadth and scope of this review effort was daunting, we now believe that we have enough supporting evidence to offer a holistic overview of this issue. At a minimum, we hope that the studies cited in this review, the gaps that we have identified and the framework that we have proposed for future research will be useful to researchers who are encouraged to explore this hypothesis in greater detail.
The implications for risk assessment
Thirty-five years ago, the work of Ames and others who followed set in motion a quest for individual chemicals as (complete) ‘carcinogens’ that became a dominant paradigm that has shaped our thinking for decades (226). So dominant has the focus been on single chemicals, that combinations of chemicals are rarely tested or even considered. For example, although IARC has focused on extensive monographs of the carcinogenic nature of individual chemicals, little has been done to evaluate the possibility of carcinogenic effects attributable to chemical mixtures except in a few instances where mixtures of concern are encountered during occupational exposures (e.g. polychlorinated dibenzo-p-dioxins and polychlorinated dibenzofurans) or as a result of personal and cultural habits (e.g. cigarette smoke, diesel and gasoline engine exhausts).
But the search for mutagenic carcinogens was never matched with a corresponding search for chemicals that might contribute to the promotion of carcinogenesis along with other chemicals. We now know that individual chemicals can produce unique disruptions of cellular biology and specific combinations of non-carcinogenic chemicals have been able to demonstrate potent carcinogenic effects. Yet, we have only scratched the surface of the biology of mixtures, and we need to look carefully at the synergistic effects.
In risk assessments, the risks associated with exposures to mixtures of chemicals are often estimated using relatively simple, component-based approaches (476). Risk analysts evaluate information regarding the mode of action associated with individual mixture components and then use either ‘dose addition’ or ‘response addition’ to predict effects. Dose addition is an appropriate approach to assess mixtures risks, when the chemicals of interest act through a common mode of action. Although response addition assumes that constituent agents act independently of each other (cause the same outcome via different modes of action). In general, a dose addition approach would be appropriate for mixtures risk assessment if we wanted to consider a series of chemicals that were carcinogenic in their own right, and if they all produced the cancer by the same mode of action. The Hallmarks of Cancer framework suggests that we should be equally, if not more, concerned about mixtures of chemicals that are not individually carcinogenic but disruptive in a manner that is collectively procarcinogenic (i.e. potentially capable of producing carcinogenic synergies when combined with other chemicals that are acting on the diverse series of mechanisms involved in carcinogenesis).
With this in mind, there should be concern that the World Health Organization International Programme on Chemical Safety (WHO IPCS) has spent the past decade developing a risk analysis agenda predicated mainly on a ‘Mode of Action’ framework (477–480), where ‘mode of action’ is defined as a sequence of key events and processes, starting with interaction of an agent with a cell, proceeding through operational and anatomical changes and resulting in an adverse outcome, in this case, cancer formation. The OECD guidance on the conduct and design of chronic toxicity and carcinogenicity (which is followed by many nations) now also reflects this approach (480). This analysis of risks from cumulative effects of chemical exposures is restrictive because it suggests that regulators should only focus on groupings of individual chemicals that are as follows:
(a) known to act via a common sequence of key events and processes;
(b) known to act on a common target/tissue and
(c) known to produce a common adverse outcome (e.g. cancer).
So, for example, in the USA, the Food Quality Protection Act provides legislated guidance on testing for cumulative effects by using the term ‘common mechanism of toxicity’ (481), which is interpreted to mean ‘mode of action’ or ‘the major steps leading to an adverse health effect following interaction of a pesticide with biological targets’. Similarly, in Canada, the Pest Control Products Act requires the government to assess the cumulative effects of pest control products that have a ‘common mechanism of toxicity’. In the USA, there has also been a tradition of employing an additional restriction requiring chemical structural similarity when selecting groups of chemicals to be subjected to mixtures risk assessment (other than a few instances where whole mixtures have been assessed, e.g. diesel exhaust, combinations of chemicals that are not similar structurally have been largely ignored (489)). In light of current knowledge of cancer biology, these criteria appear to be inappropriately restrictive, and thus demand a number of considerations—as follows:
Cumulative risk assessment should anticipate synergies of chemicals acting via dissimilar sequences/processes.
From the Hallmarks of Cancer framework, it becomes evident that chemicals that act via dissimilar pathways/targets or that produce different sorts of key events and/or employ different processes could very well produce synergies within carcinogenesis that would be relevant for cumulative risk assessment purposes. For example, ethylenediaminetetraacetic acid (EDTA) is a ubiquitous, presumably non-carcinogenic chemical that disrupts DNA repair (483,484), and it is well established that it influences chromosome breakage by mutagenic agents. In particular, when applied in combination with chemical mutagens, EDTA enhances mutagen-induced aberration frequencies and contributes to genetic instability (485). But within the mode of action framework, a chemical that is a mutagenic carcinogen, would not be assessed for the cumulative risks associated with an additional exposure to a chemical that disrupts DNA repair (a key layer of cancer defense) because it is not known to produce a common sequence of key events and processes.
A 2008 report on phthalates and cumulative risk assessment emphasized that the chemicals considered for cumulative risk assessment should be ones that cause the same health outcomes or the same types of health outcomes, not ones that cause the health outcomes only by a specific pathway (486). Similarly, The European Food Safety Authority Panel on Plant Protection Products and their Residues (PPR Panel) produced a scientific opinion on the relevance of dissimilar modes of action and their relevance for cumulative risk assessment of pesticides residues in food (482). The PPR Panel found good evidence that combination effects can arise from co-exposure to chemicals that produce common (adverse) outcomes through entirely different modes of action and recommended cumulative risk assessment methods to evaluate mixtures of pesticides in foods that have dissimilar modes of action (396).
Cumulative risk assessment should anticipate synergies of chemicals acting on different targets/tissues.
The Hallmarks of Cancer framework suggest that spatiotemporal aspects of chemical exposures are likely important as well. For example, the many constituent parts of the immune system and its distributed nature (e.g. lymph vessels, thymus, bone marrow and so on), the hypothalamic–pituitary–adrenal axis and cortisol in circulation, which are used to suppress macrophage migration inhibitory factor and control inflammation (487–489) and the surrounding tissues of the tumor microenvironment, are all relevant targets that could be chemically disrupted to produce procarcinogenic contributions to carcinogenesis.
For example, as noted previously, maneb is a fungicide with a potentially disrupting effect on cortisol (446), which could impact the body’s response to inflammation suppression, whereas atrazine affects the host immune response by directly targeting maturation of DCs and decreasing the levels of major histocompatibility complex class I molecules (243,453). Both are highly relevant forms of disruption for carcinogenesis, but within the mode of action framework, the cumulative effects of these chemicals (and other chemicals acting on these and similarly distributed targets) would never be assessed together because they do not act on a common biological target.
The PPR Panel recently pointed out that there is no empirical evidence for the validity of independent action as a predictive concept for multicomponent mixtures in the mammalian toxicological literature. Further, they argued that although overlapping toxic effects in different organs/systems may exist, it is difficult to identify a combination effect. Thus, the panel specifically restricted their focus to chemicals that ultimately produce a common adverse outcome (e.g. cancer) in the same target organ/system (482). Although it may be difficult to identify this sort of an effect, that does not mean, however, that we should ignore this possibility (i.e. now that our understanding of the biology of cancer has improved).
Cumulative risk assessment should anticipate synergies of non-carcinogens.
The WHO IPCS mode of action framework accepts the notion of a common toxic endpoint and therefore that chemicals need to first be carcinogens themselves before they can be considered as possible constituents of carcinogenic mixtures. However, it is now evident that not every procarcinogenic action resulting from a chemical exposure must be the result of a chemical that is a carcinogen itself. Continued focus on individual carcinogens reflects a lingering paradigm that overlooks the examples of synergies such as those highlighted in this project. Low-dose mechanistic effects may be very important so approaches are needed that take this into account. In chronic and complex diseases, establishing dose thresholds using the whole disease as the endpoint (e.g. cancer) may be inappropriate, especially when exposures to individual chemicals can produce relevant (but not disease causing) mechanistic effects at much lower dose levels.
Cumulative risk assessment should anticipate synergies of structurally dissimilar chemicals.
The EPA’s emphasis on structurally similar classes of chemicals for mixtures risk assessments is unnecessarily restrictive. The dissimilar chemicals reviewed within this special issue are testament to the fact that similar disruptive effects can be produced by a wide range of chemical structures and failure to adapt testing to this fact is no longer acceptable (486).
In sum, it is concerning that the WHO IPCS approach is so highly restrictive when it comes to the assessment of cumulative effects. The OECD guidelines acknowledge that cancers originating from at least some cell types may arise by a variety of independent pathways, but the guidance is fundamentally focused on the identification of individual carcinogens and cumulative effects of carcinogens, specifically noting that the approach is intended to ‘avoid misidentification of non-tumorigenic compounds as possible human carcinogens’ (480). But in practice, as in-vitro and in-vivo evidence for many chemicals is frequently not available (i.e. to prove that they individually act via a common sequence of key events or process a common target/tissue to produce cancer), it means that risk assessments of the cumulative effects of exposures to mixtures of chemicals on carcinogenesis are rarely conducted.
The International Life Sciences Institute, which is a non-profit organization with members comprised largely of major corporate interests from the food and beverage, agricultural, chemical and pharmaceutical industries, has worked closely with the WHO IPCS to support this approach. But while it may serve to ensure the avoidance of the misidentification of (non-tumorigenic) chemicals/compounds as possible human carcinogens, it simultaneously discourages regulatory agencies from exploring the sorts of synergies that might plausibly be expected to occur. Indeed, the biology of cancer suggests that the cumulative effects of non-carcinogenic chemicals acting on different pathways that are relevant to cancer, and on a variety of cancer-relevant systems, organs, tissues and cells may very well conspire to produce carcinogenic synergies that will be overlooked entirely as long as the mode of action framework (and the restrictions that it imposes) remains in use.
As mentioned briefly previously, a considerable effort has been made by toxicologists to advance a new approach called the Adverse Outcome Pathway framework. This is an extension of the Mode of Action framework and is primarily being developed as an alternative solution to in-vivo toxicity testing. The framework is based on the idea that any adverse human health effect caused by exposure to an exogenous substance can be described by a series of causally linked biochemical or biological key events with measurable parameters (28,490). Although the Adverse Outcome Pathway framework anticipates the possibility that multiple pathways may need to be defined (i.e. different pathways that can produce the same adverse human health effect), the concept is currently aligned with the mode of action approach and focuses mainly on individual chemical effects that follow a well-described pathway to produce an adverse health outcome. So as it is currently conceived, it has some of the same limitations that apply to the mode of action framework.
Nonetheless, this focus at a mechanistic level is progressive in nature and some researchers in this area are starting to call for the adoption of practices within the framework that can account for epigenetic effects, transgenerational effects and chronic toxicity (detrimental effects arising in individual or at the population level following long-term continuous or fluctuating exposure to chemicals at sublethal concentrations—i.e. concentrations not high enough to cause mortality or directly observable impairment following acute, short-term exposure, but able to induce specific effects potentially leading to adverse outcomes occurring at a later point in time) (28).
So this framework may be suitable for research that is focused on mixtures of chemicals and the pathways involved in carcinogenesis, so long as the adherents to this approach are open to the possibility that all relevant pathways need not have adverse health outcomes as endpoints, and that synergies between pathways may need to be anticipated. In other words, a series of seemingly benign actions on different pathways may be needed to conspire to produce the adverse health outcome that is of interest. This is the case in cancer. There are so many layers of redundancy and safeguards in place that individual disruptions of certain pathways may never cause disease on their own. Yet, when a number of these pathways are enabled, they can produce a discernable adverse health outcome (i.e. cancer). If this approach is robust enough to anticipate this type of complexity, it may be a model that will allow us to move past the limitations imposed by the mode of action model.
Many regulatory agencies that conduct chemical risk assessments also have a mandate to ensure that adequate safety margins are in place to protect sensitive subpopulations. So they will need to place an increasing emphasis on the interplay between environmental factors and genetic factors and also consider in-utero exposures and the potential for transgenerational effects. Some progress has been made in tackling the gene-environment interaction problem using pathway analysis to demonstrate the role of genetic variants in exposure-related cancer susceptibility (c.f. Malhotra et al. (498)), but very little research has been done on in-utero exposures to mixtures of chemicals that act on cancer-related mechanisms. An approach that focuses on defining mixtures of constituents that act disruptively on key mechanisms that are related to individual hallmarks may serve as a useful starting point to find evidence of relevant transgenerational effects (c.f. Singh et al. (499)). This is definitely an area where additional research and regulatory input is needed.
Research needs: cancer versus carcinogenesis
One of the main challenges in this project has been the need to better understand carcinogenesis as a process characterized by a long latency—and the corollary possibility of both direct and indirect effects—rather than cancer as a disease endpoint that must occur rapidly and in the majority of exposed persons to be relevant. This was also accompanied the recognition that the Hallmarks of Cancer are frequently neither fixed nor specific for cancer (349–351). Numerous experimental models have been used in cancer research over the years, and Vineis et al. (493) summarized them into at least five separate classes of models—see below:
(a) Mutational models
(b) Genome instability
(c) Models based on non-genotoxic mechanisms, clonal expansion and epigenetics
(d) ‘Darwinian’ or ‘somatic cellular selection’, and
(e) ‘Tissue organization’.
All of these models have had significant support in the scientific literature (based upon empirical evidence) and there is considerable overlap between them. But our collective understanding of carcinogenesis is still largely constrained by a historically monolithic toxicology-based approach that has been focused on the effects of mutagens and the disease itself. So although the Hallmarks of Cancer framework helps us to better conceptualize the many acquired capabilities of the disease, it leaves much to the imagination when it comes to advancing our understanding of carcinogenesis per se. This lacuna was recently highlighted by Brash et al. (494,495) in an article on what they called ‘the mysterious steps in carcinogenesis’.
Carcinogenesis appears to be an evolution of factors that ultimately conspire towards various acquired capabilities (i.e. those delineated within the Hallmarks of Cancer framework), but how much does the sequencing of these acquired capabilities matter and in what order are these capabilities acquired? Figure 1 implies a rough sequencing of these capabilities, but do we know for certain that all hallmarks for established cancer are important for carcinogenesis as well (i.e. which hallmarks are necessary for all tumors, and of those, which are sufficient or perhaps distinct for certain cancers?). Other important questions to ask relate to whether or not the individual hallmarks are a cause or a consequence of cancer development? Do the individual hallmarks need to be expressed simultaneously or sequentially along the continuum of carcinogenesis (from exposure to unambiguous cancer phenotype development)? More importantly, how does our understanding of this framework inform our general approach to the study of carcinogenesis?
We have partial answers to some of these questions, but some of these questions remain unanswered, and given the prolonged latency of many cancers, these are important questions. Our lack of knowledge in this regard makes it difficult to draw immediate conclusions about the effects that exposures to mixtures of disruptive chemicals might cause and the synergies they might produce. Public health protection is challenged by the combinatorial complexity posed, not only by multiple exposures to chemicals at environmentally relevant doses (either simultaneously or sequentially) but also through the different mechanisms played out in temporospatial manners (including life stages of development, which are different from those applied in traditional toxicologic and carcinogenic screening).
We, therefore, need to consider an expanded research agenda to include the origins, determinants and temporospatial evolution of the various cancer hallmarks and their interrelatedness. The key questions of reversibility and of cause versus consequence must also be rigorously addressed at every step from initiating carcinogenic exposure to established cancer, recognizing that not all hallmarks are either fixed or specific for any given cancer type.
Research needs: the Hallmarks of Cancer
Current approaches to the study of chemical exposures and carcinogenesis have not been designed to address effects at low concentrations or in complex mixtures. Procarcinogenic agents may be directly genotoxic, indirectly genotoxic or non-genotoxic. In principle, not every disruptive effect resulting in a change that mimics a cancer hallmark is necessarily carcinogenic. Such associations, when observed, still require rigorous validation to ensure that exposures are unequivocally linked to the development of both cancer and accompanying phenotypic hallmarks. These complex interactional possibilities, coupled with the fact that low-dose combinatorial effects on cancer development and progression have not been rigorously or comprehensively addressed, speak to major gaps in our understanding of environmental cancer risk and the specific role that mixtures of environmental chemical exposures might play in the incidence of cancer at the population level.
Unfortunately, the known effects for chemicals examined in isolation and at higher concentrations cannot be readily extrapolated to effects at lower concentrations. Interactions within complex mixtures will also occur against the backdrop of complex interactions with other environmental, genetic and epigenetic factors, so there is a need for expanded or complementary conceptual and experimental frameworks to better understand the determinants and specific functional contributions of environmental exposures in cancer.
A considerable amount of energy is now being placed on the development of research and technologies that can support the ‘exposome’ (496), an emerging concept aimed at representing the totality of chemical exposures received by a person during a lifetime. This approach encompasses all sources of toxicants and is intended to help researchers discern some of the contributing factors that are driving chronic diseases such as cancer. Related projects are expected to involve extensive biomonitoring (e.g. blood and urine sampling) and other techniques to assess biomarkers that might be relevant, and this information should be extremely helpful. Longitudinal studies should also be carried out in animal models to assess the tissue distribution of mixtures of chemical metabolites. To truly make good use of this information, we are going to need a better mechanistic understanding of the process of carcinogenesis itself and better early markers of cancer development.
It therefore makes sense to pursue empirical research based on our current understandings of the disease to test the effects of real-world environmental mixtures at relevant dose levels. Basic studies should be designed to test joint toxic action (of carefully designed combinations of chemicals) to assess both dose additivity (via common mode of action) and response additivity (via disparate modes of action). Research designs should anticipate the many layers of inherent defense and incorporate chemical constituents specifically intended to demonstrate predictable synergies and mechanistic relevance. It would also be useful to know whether or not the chemical induction of certain numbers/combinations of hallmarks is sufficient to consistently produce in-vivo carcinogenesis.
Mixtures research that focuses on the carcinogenic synergies of non-carcinogenic constituents would be particularly useful. In addition, compounds or classes of chemicals already considered to be (complete) carcinogens in the classical sense may also contribute to carcinogenesis in complex mixtures at concentrations not traditionally deemed carcinogenic. For this reason and for completeness, ‘classic’ carcinogens with an established environmental presence at levels that are presumed to be inconsequential may still have pathogenic relevance and should be routinely included in the analysis.
Target sites that are being manipulated and disruptive chemicals that are being selected to produce carcinogenic effects should be scrutinized for confounding effects. Table 4 contains aggregated evidence of cross-hallmark effects for selected pathways/mechanisms, and although some target sites for disruption may be compelling starting points for researchers focused on a given phenotype (e.g. genetic instability), cross-hallmark relationships should be explored. So, for example, telomere loss is seen as a disruptive (procarcinogenic) effect from the perspective of the the genetic instability team (i.e. the group in this project who selected this target) and it has also been shown to exert procarcinogenic effects in four other hallmark areas. But evidence also exists that suggests that telomere loss can have anticarcinogenic effects in four other hallmark areas. The exact circumstances of the various studies that support these cross-hallmark relationships would need to be reviewed to better understand the implications/relevance of these reported effects. But checking planned disruptions of each target across all of the other hallmark areas is a way to ensure that confounding (i.e. anticarcinogenic) effects are not inadvertantly introduced into experiments that are aimed at producing carcinogenesis, or phenotypes that can support/contribute to carcinogenesis. Similarly, Table 5 contains aggregated evidence of cross-hallmark effects for the chemical disruptors in this review, so this table can be used for the same purpose.
It may also be productive to identify ‘reference compounds’ (ideal and prototypical disruptors) for each hallmark pathway as a guide to predict different combinations of chemicals that might act in a procarcinogenic manner on any one of the hallmarks. This may involve different systems and organs that have relevance to cancer and this sort of research could also be combined with similar sorts of research on other reference compounds or mixtures that are shown to enable other hallmarks. In doing so, researchers should evaluate epigenetic changes in multiple samples/organs/tissues from exposed animals/other experimental models using gene array technology, ‘omics’ approaches, real-time imaging of tumors in 3D both in-vitro (primary cells) and in-vivo models combined with molecular biomarkers of disease progression, and cellular immune parameters. The combination of use of computational chemical genomics virtual screening (497), system biology/pharmacology and high-quality imaging techniques should help us find quantitative-structure-activity-relationship correlations between the chemical structure of dissimilar disruptors and experimental data on biological activity, physiological changes, in-vivo toxicity and 3D cellular protein dynamics.
It is also conceivable that the combined effects of hundreds of chemicals in the environment may be involved in the process of enabling carcinogenesis at the population level, so basic empirical research that can demonstrate carcinogenic effects with minimalistic combinations may initially be needed to reveal the more granular aspects of carcinogenesis. For example, initial research might test our assumptions of the step-wise progression of carcinogenesis using targeted mixtures of chemicals that exert LDE to test combinations of 2, 3, 4 chemicals etc. against specific hallmarks and then adding additional targets to move through the various steps that are believed to be needed to fully enable the process. Experiments of this nature may reveal increases as well as decreases in cancer risk when different mechanisms are disrupted and corresponding hallmark phenotypes are enabled (depending on the timing of various disruptive exposures). Batteries of tests may ultimately be needed to evaluate whole mixtures and key components individually and in various combinations. HTS approaches will be particularly helpful here, and a tiered approach may make sense to look for disruptive combinations, which can then be applied in vivo. Exposure sequencing and dosage may also be important and should be evaluated based on our current understandings of the biology of cancer.
In terms of setting research priorities, tissue fate is also a matter for consideration. It has been known for many years that certain chemicals have affinities for certain tissues, and radiotracer labeling studies that have been conducted on chemicals for regulatory purposes illustrate how certain chemicals tend to accumulate in certain tissues. Additionally, it is well known that some tissue types give rise to human cancers millions of times more often than other tissue types (498). So, researchers may want to focus their work on mixtures of disruptive chemicals that prove to be complementary at a mechanistic level and individually known to accumulate in the same types of tissues, while at the same time choosing tissue types that are known to produce cancers more rapidly.
The work that has been done by the WHO IPCS on mode of action has been very useful. Understanding when chemicals operate through the same mode of action is definitely good information for analytical purposes, but given that we now recognize that non-carcinogens acting at very low-dose levels on different targets and mechanisms can still activate carcinogenesis-related pathways, the combined (carcinogenic) potential of the many commonly encountered chemicals within the environment still needs to be evaluated.
Increasingly, our information is improving and there are several tools that researchers can use to improve their research designs. For example, ToxCast™ is an approach launched by the EPA in 2007 to develop ways to predict potential toxicity of chemicals and to develop a cost-effective approach for prioritizing the thousands of chemicals that need toxicity testing. The ToxCast™ database was used in this project by a number of the teams and an incredible amount of data are available on in-vitro tests (produced using HTS) for a wide range of chemicals. For example, there are many results that are direct measures of actions related to important mechanisms found within the Hallmarks of Cancer framework, which would be useful for research focused along these lines.
Although the hallmark phenotypes in this project represent areas of cancer research for which there is considerable agreement, one critique of this framework is that it ignores the ‘missing hallmark’ of dedifferentiation (351). As well, the complexity encompassed by each of these areas of research is humbling. Moreover, cancer is not a singular or fixed entity, which frequently limits the ability to generalize about cancer biology (349–351). In a recent reflection on his career, Weinberg et al. (499) noted not only widespread acceptance of the ‘Hallmarks of Cancer’ heuristic but also that this attempt to simplify the disease is rapidly being eclipsed by calls from the next generation of researchers who are now focused on assembling and analyzing enormous data sets to gain an increasingly sophisticated understanding of cancer (e.g. genomes, transcriptomes, proteomes—including isoforms, post-translational modifications and proteoforms, epigenomes, kinomes, methylomes, glycomes and matrisomes—each one of which encompasses staggering amounts of accumulated information) (499).
Many researchers have called for an analytical use of systems biology to transcend the study of individual genes/proteins and to integrate this complexity into higher order phenotypes (500,501). Systems biology enables researchers to identify properties that emerge from complex chemical–biological systems by probing how changes in one part affect the others and the behavior of the whole system. The combined effects of tens, if not hundreds, of simultaneous exposures may need to be accounted for. The fundamental challenge is that such models require parameters that are driven by data, but there are very few good examples of research on mixtures at environmentally relevant dose levels (502) (c.f. Porter et al. (510)), and there are fewer still that are focused on cancer.
Nonetheless, in the near term, this basic framework should serve as a useful starting point for foundational research and government funding agencies should consider new ways to support large-scale, team-based holistic approaches to this problem.
Regulatory priorities (in the face of combinatorial complexity)
It will take time before we fully understand the carcinogenic potential of low-dose exposures to chemical mixtures in the environment. Nonetheless, we cannot afford to lose sight of the fact that the incidence of cancer remains unacceptably high, and that the unavoidable (i.e. not lifestyle related) causative factors that are, in part, underpinning this trend are still not fully understood (9–11,504,505). Populations worldwide are continually exposed to a wide range of chemicals, so keeping the precautionary principle in mind (506), there is a need to take the risks related to the cumulative effects of these chemicals seriously (422). Of primary concern is the fact that WHO IPCS mode of action framework (477) and the OECD guidelines for risk assessment (480) are restrictive to the point that regulators could be underestimating the risks posed by exposures to low doses of mixtures of chemicals.
National regulatory agencies and cancer research foundations must proactively pursue empirical research programs to assess any basic relationships that can be discerned between exposures to mixtures of commonly encountered chemicals and carcinogenicity. For example, systematic exploratory research in appropriate rodent models exposed to ‘whole-mixtures’ that consist of multiple chemical constituents at environmentally relevant dose levels could demonstrate the carcinogenic potential of complex mixtures that are relevant to the population. There is also a compelling need for complementary basic research to address specific causal relationships between environmental exposures and the associated development of cancer and its characteristic hallmarks.
Hypothetically speaking, such a ‘whole mixture’ should be composed of non-carcinogens and potential carcinogens given that individual chemicals that are not carcinogenic could act on a range of different systems, tissues and/or cells and act synergistically with other chemicals to instigate carcinogenesis. The goal of such investigations would not be to single out any given chemical as a carcinogen, but rather to determine whether or not unanticipated (procarcinogenic) synergies of many commonly encountered chemicals when combined are endangering public health.
In line with the 3Rs (Reduction, Replacement and Refinement) guiding principles for more ethical use of animals in scientific experiments, there has been a significant push for researchers and regulatory agencies to move away from in-vivo testing (e.g. European Union REACH legislation and in the USA, the NRC Toxicology for the 21st Century vision (507)) to take advantage of HTS and other new technologies. The EPA’s effort to search for environmental chemicals that are most active in relevant assays across the various cancer hallmarks, and then to compare those results with in-vivo rodent carcinogenicity data for the same chemicals, was a definite step in this direction (29). However, HTS models of carcinogenicity will require validation, and significant hurdles remain before this sort of testing will be ready to replace in-vivo research (508). Therefore, in the near term, in-vivo testing still remains an important avenue for developing data sets to address cancer risks of complex mixtures.
Summary/Conclusions
For several decades, there has been a concerted effort to identify individual chemicals and other agents that are carcinogenic. At the same time, however, little has been done to determine whether or not chronic lifetime exposures to mixtures of non-carcinogenic chemicals in the environment (at low-dose levels) have carcinogenic potential. Many chemicals are known to accumulate in bodily tissues over time, but little is known about their combined effects at a mechanistic level and their impact on cancer-related mechanisms and carcinogenesis. In this project, teams of cancer biologists worked with researchers in the field of environmental health for the very first time to explore this possibility.
Teams that reviewed these cancer-related phenotypes (i.e. genetic instability, tumor-promoting inflammation, sustained proliferative signaling, insensitivity to antigrowth signals, resistance to cell death, angiogenesis, tissue invasion and metastasis, the tumor microenvironment and avoiding immune destruction) readily identified individual (non-carcinogenic) chemicals that are ubiquitous in the environment that have some potential to act on key/priority functional targets in each of these domains. In contrast, the teams focused on replicative immortality and dysregulated metabolism found examples of chemicals to consider but noted a significant lack of useful toxicological research in these areas.
In total, 85 examples of environmental chemicals were reviewed as prototypical disruptors (for specific actions on key pathways/mechanisms that are important for carcinogenesis) and 59% of them (i.e. 50/85) were found to exert LDE (at levels that are deemed relevant given the background levels of exposure that exist in the environment) with 15 of the 50 demonstrating their LDE in a non-linear dose-response pattern. Only 15% of the chemicals reviewed (i.e. 13/85) were found to have a dose-response threshold and the remaining 26% (i.e. 22/85) were categorized as ‘unknown’ due to a lack of dose-response information.
Cross-hallmark effects for all target sites for disruption and for all chemicals were found, but the evidence supporting these results varied considerably in strength and in context.
A number of the teams also cited relevant in-utero exposure studies in their reviews and presented data on transgenerational effects related to different aspects of the disease (e.g. inflammation, immune evasion and so on). These examples raise intriguing possibilities about vulnerabilities at the population level, and the contributions that in-utero and early life exposures to mixtures of those chemicals might make towards cancer susceptibility.
Therefore, current regulations in many countries (that consider only the cumulative effects of exposures to individual carcinogens that act via a common sequence of key events and processes on a common target/tissue to produce cancer) should be revisited. Our current understanding of the biology of cancer suggests that the cumulative effects of (non-carcinogenic) chemicals acting on different pathways that are relevant to cancer, and on a variety of cancer-relevant systems, organs, tissues and cells could conspire to produce carcinogenic synergies that will be overlooked using current risk assessment methods. Cumulative risk assessment methods that are based on ‘common mechanisms of toxicity’ or common ‘modes of action’ may therefore be underestimating cancer-related risks. In-utero and early life exposures, transgenerational effects and the interplay between the low-dose mechanistic effects of chemical mixtures in the environment and the vulnerabilities of subpopulations who are predisposed to cancer (i.e. via genetics or other influences) must also be considered. Current policies and practices do not adequately address these issues and should therefore be revisited if regulatory agencies hope to better understand and assess these risks.
Finally, given the long latency period in most cancers, early detection to cancer is key so an improved understanding of the biology within originating tissues (during the latency period) would be very helpful. If we can use the heuristic presented in this review to better assess the combined effects of common exposures to chemical mixtures in the environment, it will help us improve our understanding of carcinogenesis and identify exogenous triggers and enabling factors (in utero and during this important latency period), all of which will be key for the development of effective strategies for prevention and early detection.
Contributions
The first draft of this manuscript (prepared by W.H.G.) was distributed to all of the contributors within the task force for feedback and additional inputs. The many responses that followed were managed by W.H.G. (with the assistance of L.Lo., M.G. and D.O.C.). Then, multiple rounds of inputs were solicited from the entire task force with several subsequent rounds of revisions and refinements prior to submission. In addition to the contributions mentioned previously, The Halifax Project also benefited from the involvement of D.J.C. (who provided details, at the workshop in Halifax, Nova Scotia, Canada, of National Institute of Environmental Health Sciences priorities and the agency’s interest in unravelling the health effects of environmental mixtures) and from Glenn Rice (who gave a Halifax workshop presentation on the chemical mixtures as a consideration in cancer risk assessment). Both of these presenters were included in the iterative rounds of manuscript revisions mentioned previously, and both offered inputs that resulted in refinements to the manuscript. Finally, the journal’s peer-review process was important, and resulted in the collection of additional evidence from the teams that related to thresholds, LDE and of non-monotonic dose-response relationships. The reviewer’s critical analysis on these topics resulted in a substantial improvement to the data presented in this capstone document, which ultimately served to highlight the extent to which low-dose exposures to individual chemical constituents (within mixtures of environmental chemicals) might have relevance for the process of carcinogenesis. Dose-response characterization data and inputs were then submitted by all teams and subsequently reviewed and compiled by N.K., A.Co. and R.M.
The Halifax Project Task Force that worked on this manuscript involved nearly 200 people, many of whom contributed to, and signed on to this capstone article. The design of the Halifax Project was conceived by L.Lo. with scientific advice from M.G. Funding provided by the National Institute for Environmental Health Sciences was arranged by D.O.C., and this manuscript was first drafted by W.H.G. Starting with the Hallmarks of Cancer framework (Hanahan et al. (21)), 11 teams of international cancer biologists and toxicologists were established to review the literature on key cancer-related mechanisms/pathways in their respective domains and to also look at the disruptive potential of low-dose exposures to chemicals commonly encountered in the environment (i.e. as it relates to those same mechanisms/pathways). Each team had a leader and each team was responsible for contributing a section of related content within the capstone manuscript. The contributing authors from these teams are as follows: (1) Angiogenesis (Z.H., C-W.H., H-Y.H., L-T.L., M.X., N.K., S.A.B., T.M., V.D., W.K.R.); (2) Dysregulated metabolism (R.B.R., A.C.S., A.B., E.Ry., D.B., F.C., F.L.M., G.Wi., J.We., N.B.K., R.P.); (3) Evasion of antigrowth signaling (R.N., A.L., C.C.N., D.W.L., D.R., G.S.G., G.M.C., H.Kr., J.V., K.A.C-S., M.W., N.C., P.A.M., P.De., R.A-V., R.V., R.D.F., R.P-C., R.C.C., S.N.B.), (4) Genetic instability (S.A.S.L., A.L.d.C.S., A.Az., A.K.C., A.R.C., A-K.O., E.Ro., F.D., F.J.V.S., G.K., G.B., L.Go., L.Le., L.Z., M.Val., M.K-V., N.v L., P.O-W., S.Pav., T.C.); (5) Immune system evasion (H.K.L., E.C., J.K., M.A.W., M.H.M., T.O., W.K.D.), (6) Replicative immortality (A.Ca., C.B-A., H.Y., H.Ko., J.P.W., J.F.M-L., M.L., S.S.W.); (7) Resistance to cell death (H.H.P., A.M.A., B.J.B., C.Y., E.R., K.B.N., L.S.D’A., L.Li., M.F.R., M.J.G., P.M.G., P.S.L., Q.(S.) C., R.K.S., R.D., S.Ro., S.L., T-J.L., Y.R.); (8) Sustained proliferative signaling (W.E., A.W., G.Wa., H.S., J.E.K., J.R., K.M., L.Gu., M.V.K., P.V., P.Da., R.M., S.Er., T.S., T.H.); (9) Tissue invasion and metastasis (J.O., B.P.Z., C.D., G.N., G.T.W., I.K., I.R.M., L.J.M., N.A., O.O., P.N-M., S.El., S.Pap., V.O-M., Y.L., Z.C.); (10) Tumor microenvironment (D.W.F., C.S.C., D.C.K., E.L., F.M., J.Ro., J.C., J.R.W., L.S., L.V., M.C., P.K.K., P.H., S.Ry., S.C.C., V.M-S.) and (11) Tumor-promoting inflammation (P.T., C.B., E-Y. M., J.S., L.J., M.K., S.H., T.G., V.S.).** Additionally, a special cross-functional team was established to investigate whether or not the chemicals that were identified by the teams as having disruptive potential for key mechanisms/pathways in a particular domain might also have been shown in other research to exert relevant effects on mechanisms/pathways in other domains. The results of the efforts from this team have been compiled and summarized in this article and can be found within Table 4. This team was comprised as follows: W.H.B., A.Am., I.S., A.Co., C.M., D.B., E.Ry., F.A-M., H.A.H., H.K.S., J.Ra., J.Wo., K.R.P., L.M., M.Vac., N.S., R.A-T., R.R., R.A.H. and S.F.** **Note that team leaders are denoted by the first set of initials in each team list.
Funding/Acknowledgements
We gratefully acknowledge the support of the National Institute of Health-National Institute of Environmental Health Sciences (NIEHS) conference grant travel support (R13ES023276); Glenn Rice, Office of Research and Development, United States Environmental Protection Agency, Cincinnati, OH, USA also deserves thanks for his thoughtful feedback and inputs on the manuscript; William H.Goodson III was supported by the California Breast Cancer Research Program, Clarence Heller Foundation and California Pacific Medical Center Foundation; Abdul M.Ali would like to acknowledge the financial support of the University of Sultan Zainal Abidin, Malaysia; Ahmed Lasfar was supported by an award from the Rutgers Cancer Institute of New Jersey; Ann-Karin Olsen and Gunnar Brunborg were supported by the Research Council of Norway (RCN) through its Centres of Excellence funding scheme (223268/F50), Amancio Carnero’s lab was supported by grants from the Spanish Ministry of Economy and Competitivity, ISCIII (Fis: PI12/00137, RTICC: RD12/0036/0028) co-funded by FEDER from Regional Development European Funds (European Union), Consejeria de Ciencia e Innovacion (CTS-1848) and Consejeria de Salud of the Junta de Andalucia (PI-0306-2012); Matilde E. Lleonart was supported by a trienal project grant PI12/01104 and by project CP03/00101 for personal support. Amaya Azqueta would like to thank the Ministerio de Educacion y Ciencia (‘Juande la Cierva’ programme, 2009) of the Spanish Government for personal support; Amedeo Amedei was supported by the Italian Ministry of University and Research (2009FZZ4XM_002), and the University of Florence (ex60%2012); Andrew R.Collins was supported by the University of Oslo; Annamaria Colacci was supported by the Emilia-Romagna Region - Project ‘Supersite’ in Italy; Carolyn Baglole was supported by a salary award from the Fonds de recherche du Quebec-Sante (FRQ-S); Chiara Mondello’s laboratory is supported by Fondazione Cariplo in Milan, Italy (grant n. 2011-0370); Christian C.Naus holds a Canada Research Chair; Clement Yedjou was supported by a grant from the National Institutes of Health (NIH-NIMHD grant no. G12MD007581); Daniel C.Koch is supported by the Burroughs Wellcome Fund Postdoctoral Enrichment Award and the Tumor Biology Training grant: NIH T32CA09151; Dean W. Felsher would like to acknowledge the support of United States Department of Health and Human Services, NIH grants (R01 CA170378 PQ22, R01 CA184384, U54 CA149145, U54 CA151459, P50 CA114747 and R21 CA169964); Emilio Rojas would like to thank CONACyT support 152473; Ezio Laconi was supported by AIRC (Italian Association for Cancer Research, grant no. IG 14640) and by the Sardinian Regional Government (RAS); Eun-Yi Moon was supported by grants from the Public Problem-Solving Program (NRF-015M3C8A6A06014500) and Nuclear R&D Program (#2013M2B2A9A03051296 and 2010-0018545) through the National Research Foundation of Korea (NRF) and funded by the Ministry of Education, Science and Technology (MEST) in Korea; Fahd Al-Mulla was supported by the Kuwait Foundation for the Advancement of Sciences (2011-1302-06); Ferdinando Chiaradonna is supported by SysBioNet, a grant for the Italian Roadmap of European Strategy Forum on Research Infrastructures (ESFRI) and by AIRC (Associazione Italiana Ricerca sul Cancro; IG 15364); Francis L.Martin acknowledges funding from Rosemere Cancer Foundation; he also thanks Lancashire Teaching Hospitals NHS trust and the patients who have facilitated the studies he has undertaken over the course of the last 10 years; Gary S.Goldberg would like to acknowledge the support of the New Jersey Health Foundation; Gloria M.Calaf was supported by Fondo Nacional de Ciencia y Tecnología (FONDECYT), Ministerio de Educación de Chile (MINEDUC), Universidad de Tarapacá (UTA); Gudrun Koppen was supported by the Flemish Institute for Technological Research (VITO), Belgium; Hemad Yasaei was supported from a triennial project grant (Strategic Award) from the National Centre for the Replacement, Refinement and Reduction (NC3Rs) of animals in research (NC.K500045.1 and G0800697); Hiroshi Kondoh was supported in part by grants from the Ministry of Education, Culture, Sports, Science, and Technology of Japan, Japan Science and Technology Agency and by JST, CREST; Hsue-Yin Hsu was supported by the Ministry of Science and Technology of Taiwan (NSC93-2314-B-320-006 and NSC94-2314-B-320-002); Hyun Ho Park was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) of the Ministry of Education, Science and Technology (2012R1A2A2A01010870) and a grant from the Korea Healthcare Technology R&D project, Ministry of Health and Welfare, Republic of Korea (HI13C1449); Igor Koturbash is supported by the UAMS/NIH Clinical and Translational Science Award (UL1TR000039 and KL2TR000063) and the Arkansas Biosciences Institute, the major research component of the Arkansas Tobacco Settlement Proceeds Act of 2000; Jan Vondráček acknowledges funding from the Czech Science Foundation (13-07711S); Jesse Roman thanks the NIH for their support (CA116812); John Pierce Wise Sr. and Sandra S.Wise were supported by National Institute of Environmental Health Sciences (ES016893 to J.P.W.) and the Maine Center for Toxicology and Environmental Health; Jonathan Whitfield acknowledges support from the FERO Foundation in Barcelona, Spain; Joseph Christopher is funded by Cancer Research UK and the International Journal of Experimental Pathology; Julia Kravchenko is supported by a philanthropic donation by Fred and Alice Stanback; Jun Sun is supported by a Swim Across America Cancer Research Award; Karine A.Cohen-Solal is supported by a research scholar grant from the American Cancer Society (116683-RSG-09-087-01-TBE); Laetitia Gonzalez received a postdoctoral fellowship from the Fund for Scientific Research–Flanders (FWO-Vlaanderen) and support by an InterUniversity Attraction Pole grant (IAP-P7-07); Laura Soucek is supported by grant #CP10/00656 from the Miguel Servet Research Contract Program and acknowledges support from the FERO Foundation in Barcelona, Spain; Liang-Tzung Lin was supported by funding from the Taipei Medical University (TMU101-AE3-Y19); Linda Gulliver is supported by a Genesis Oncology Trust (NZ) Professional Development Grant, and the Faculty of Medicine, University of Otago, Dunedin, New Zealand; Louis Vermeulen is supported by a Fellowship of the Dutch Cancer Society (KWF, UVA2011-4969) and a grant from the AICR (14–1164); Mahara Valverde would like to thank CONACyT support 153781; Masoud H. Manjili was supported by the office of the Assistant Secretary of Defense for Health Affairs (USA) through the Breast Cancer Research Program under Award No. W81XWH-14-1-0087 Neetu Singh was supported by grant #SR/FT/LS-063/2008 from the Department of Science and Technology, Government of India; Nicole Kleinstreuer is supported by NIEHS contracts (N01-ES 35504 and HHSN27320140003C); P.K. Krishnakumar is supported by the Funding (No. T.K. 11-0629) of King Abdulaziz City for Science and Technology, Riyadh, Saudi Arabia; Paola A.Marignani is supported by the Dalhousie Medical Research Foundation, The Beatrice Hunter Cancer Institute and CIHR and the Nova Scotia Lung Association; Paul Dent is the holder of the Universal Inc.Chair in Signal Transduction Research and is supported with funds from PHS grants from the NIH (R01-CA141704, R01-CA150214, R01-DK52825 and R01-CA61774); Petr Heneberg was supported by the Charles University in Prague projects UNCE 204015 and PRVOUK P31/2012, and by the Czech Science Foundation projects P301/12/1686 and 15-03834Y; Po Sing Leung was supported by the Health and Medical Research Fund of Food and Health Bureau, Hong Kong Special Administrative Region, Ref. No: 10110021; Qiang Cheng was supported in part by grant NSF IIS-1218712; R. Brooks Robey is supported by the United States Department of Veterans Affairs; Rabindra Roy was supported by United States Public Health Service Grants (RO1 CA92306, RO1 CA92306-S1 and RO1 CA113447); Rafaela Andrade-Vieira is supported by the Beatrice Hunter Cancer Research Institute and the Nova Scotia Health Research Foundation; Renza Vento was partially funded by European Regional Development Fund, European Territorial Cooperation 2007–13 (CCI 2007 CB 163 PO 037, OP Italia-Malta 2007–13) and grants from the Italian Ministry of Education, University and Research (MIUR) ex-60%, 2007; Riccardo Di Fiore was a recipient of fellowship granted by European Regional Development Fund, European Territorial Cooperation 2007–2013 (CCI 2007 CB 163 PO 037, OP Italia-Malta 2007–2013); Rita Dornetshuber-Fleiss was supported by the Austrian Science Fund (FWF, project number T 451-B18) and the Johanna Mahlke, geb.-Obermann-Stiftung; Roberta Palorini is supported by a SysBioNet fellowship; Roslida Abd Hamid is supported by the Ministry of Education, Malaysia-Exploratory Research Grant Scheme-Project no: ERGS/1-2013/5527165; Sabine A.S.Langie is the beneficiary of a postdoctoral grant from the AXA Research Fund and the Cefic-LRI Innovative Science Award 2013; Sakina Eltom is supported by NIH grant SC1CA153326; Samira A.Brooks was supported by National Research Service Award (T32 ES007126) from the National Institute of Environmental Health Sciences and the HHMI Translational Medicine Fellowship; Sandra Ryeom was supported by The Garrett B. Smith Foundation and the TedDriven Foundation; Thierry Massfelder was supported by the Institut National de la Santé et de la Recherche Médicale INSERM and Université de Strasbourg; Thomas Sanderson is supported by the Canadian Institutes of Health Research (CIHR; MOP-115019), the Natural Sciences and Engineering Council of Canada (NSERC; 313313) and the California Breast Cancer Research Program (CBCRP; 17UB-8703); Tiziana Guarnieri is supported by a grant from Fundamental Oriented Research (RFO) to the Alma Mater Studiorum University of Bologna, Bologna, Italy and thanks the Fondazione Cassa di Risparmio di Bologna and the Fondazione Banca del Monte di Bologna e Ravenna for supporting the Center for Applied Biomedical Research, S.Orsola-Malpighi University Hospital, Bologna, Italy; W.Kimryn Rathmell is supported by the V Foundation for Cancer Research and the American Cancer Society; William K.Decker was supported in part by grant RP110545 from the Cancer Prevention Research Institute of Texas; William H.Bisson was supported with funding from the NIH P30 ES000210; Yon Rojanasakul was supported with NIH grant R01-ES022968; Zhenbang Chen is supported by NIH grants (MD004038, CA163069 and MD007593); Zhiwei Hu is grateful for the grant support from an institutional start-up fund from The Ohio State University College of Medicine and The OSU James Comprehensive Cancer Center (OSUCCC) and a Seed Award from the OSUCCC Translational Therapeutics Program.
Glossary
Abbreviations
- AhR
aryl hydrocarbon receptor
- BPA
bisphenol A
- EMT
epithelial-mesenchymal transition
- EPA
environmental protection agency
- HTS
high-throughput screening
- IARC
International Agency for Research on Cancer
- IL
interleukin
- LDE
low-dose effects
- LOAEL
lowest-observed-adverse-effect level
- LOEL
lowest observed effect level
- miRNA
microRNAs
- 4-NP
nonylphenol
- MXC
methoxychlor
- NF-κB
nuclear factor-κB
- PBDE
polybrominated diphenyl ethers
- PPAR
peroxisome proliferator-activated receptor
- ROS
reactive oxygen species
References
- 1. (2014) World cancer report 2014. In Wild C.P. and Stewart B.W (eds). World Health Organization. [Google Scholar]
- 2. Malhotra J. (2014) Molecular and genetic epidemiology of cancer in low- and medium-income countries. Ann. Glob. Health, 80, 418–425. [DOI] [PubMed] [Google Scholar]
- 3. McGuinn L.A., et al. (2012) Cancer and environment: definitions and misconceptions. Environ. Res., 112, 230–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sankpal U.T., et al. (2012) Environmental factors in causing human cancers: emphasis on tumorigenesis. Tumour Biol., 33, 1265–1274. [DOI] [PubMed] [Google Scholar]
- 5. Trosko J.E., et al. (2005) The emperor wears no clothes in the field of carcinogen risk assessment: ignored concepts in cancer risk assessment. Mutagenesis, 20, 81–92. [DOI] [PubMed] [Google Scholar]
- 6. Christiani D.C. (2011) Combating environmental causes of cancer. N. Engl. J. Med., 364, 791–793. [DOI] [PubMed] [Google Scholar]
- 7. Clapp R. (2011) Chemicals policy in the 2008-2009 President's Cancer Panel Report. New Solut., 21, 447–455. [DOI] [PubMed] [Google Scholar]
- 8. Reuben S.H. (2008–2009) Reducing environmental cancer risk: what we can do now. In Panel T.P.s.C. (ed.), Bethesda, Maryland. [Google Scholar]
- 9. Parkin D.M., et al. (2011) The fraction of cancer attributable to lifestyle and environmental factors in the UK in 2010. Br. J. Cancer, 105(Suppl 2), S77–S81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. (2009) Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. World Health Organization, Geneva. [Google Scholar]
- 11. Straif K. (2008) The burden of occupational cancer. Occup. Environ. Med., 65, 787–788. [DOI] [PubMed] [Google Scholar]
- 12. Vandenberg L.N., et al. (2012) Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr. Rev., 33, 378–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. (2009) OECD Guidelines for the Testing of Chemicals, Section 4 Health Effects, Test No. 451: Carcinogenicity Studies. OECD. [Google Scholar]
- 14. Wignall J.A., et al. (2014) Standardizing benchmark dose calculations to improve science-based decisions in human health assessments. Environ. Health Perspect., 122, 499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Myers J.P., et al. (2009) A clash of old and new scientific concepts in toxicity, with important implications for public health. Environ. Health Perspect., 117, 1652–1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vandenberg L.N., et al. (2013) Regulatory decisions on endocrine disrupting chemicals should be based on the principles of endocrinology. Reprod. Toxicol., 38, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bergman A., et al. (2013) Science and policy on endocrine disrupters must not be mixed: a reply to a “common sense” intervention by toxicology journal editors. Environ. Health, 12, 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ames B.N. (1979) Identifying environmental chemicals causing mutations and cancer. Science, 204, 587–593. [DOI] [PubMed] [Google Scholar]
- 19. Armitage P., et al. (1954) The age distribution of cancer and a multi-stage theory of carcinogenesis. Br. J. Cancer, 8, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Truhaut R. (1990) [Recent progress in the evaluation of the dangers of chemical carcinogens]. J. Pharm. Belg., 45, 131–140. [PubMed] [Google Scholar]
- 21. Hanahan D., et al. (2000) The hallmarks of cancer. Cell, 100, 57–70. [DOI] [PubMed] [Google Scholar]
- 22. Preston R.J. (2005) Extrapolations are the Achilles heel of risk assessment. Mutat. Res., 589, 153–157. [DOI] [PubMed] [Google Scholar]
- 23. Hanahan D., et al. (2011) Hallmarks of cancer: the next generation. Cell, 144, 646–674. [DOI] [PubMed] [Google Scholar]
- 24. Colotta F., et al. (2009) Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis, 30, 1073–1081. [DOI] [PubMed] [Google Scholar]
- 25. Warburg O. (ed.) (1930) The Metabolism of Tumours: Investigations from the Kaiser Wilhelm Institute for Biology, Berlin-Dahlen. Constable & Company Limited, London. [Google Scholar]
- 26. Aisenberg A.C. (1961) The Glycolysis and Respiration of Tumors. Academic Press, New York, NY. [Google Scholar]
- 27. Ankley G.T., et al. (2010) Adverse outcome pathways: a conceptual framework to support ecotoxicology research and risk assessment. Environ. Toxicol. Chem., 29, 730–741. [DOI] [PubMed] [Google Scholar]
- 28. Groh K.J., et al. (2015) Development and application of the adverse outcome pathway framework for understanding and predicting chronic toxicity: I. Challenges and research needs in ecotoxicology. Chemosphere, 120, 764–777. [DOI] [PubMed] [Google Scholar]
- 29. Kleinstreuer N.C., et al. (2013) In vitro perturbations of targets in cancer hallmark processes predict rodent chemical carcinogenesis. Toxicol. Sci., 131, 40–55. [DOI] [PubMed] [Google Scholar]
- 30. Yates L.R., et al. (2012) Evolution of the cancer genome. Nat. Rev. Genet., 13, 795–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. (2001) National Toxicology Program’s report of the endocrine disruptors low dose peer review. National Institute of Environmental Health Sciences, National Toxicology Program, Research Triangle Park, NC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Melnick R., et al. (2002) Summary of the National Toxicology Program's report of the endocrine disruptors low-dose peer review. Environ. Health Perspect., 110, 427–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Welshons W.V., et al. (2006) Large effects from small exposures. III. Endocrine mechanisms mediating effects of bisphenol A at levels of human exposure. Endocrinology, 147(Suppl 6), S56–S69. [DOI] [PubMed] [Google Scholar]
- 34. Vandenberg L.N., et al. (2007) Human exposure to bisphenol A (BPA). Reprod. Toxicol., 24, 139–177. [DOI] [PubMed] [Google Scholar]
- 35. Brucker-Davis F., et al. (2001) Significant effects of mild endogenous hormonal changes in humans: considerations for low-dose testing. Environ. Health Perspect., 109( Suppl 1 ), 21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. EPA, U.S. The U.S. Environmental Protection Agency ToxCast Phase I/II data http://www.epa.gov/ncct/toxcast/data.html.
- 37. Taylor T.R., et al. (2011) Ziram activates mitogen-activated protein kinases and decreases cytolytic protein levels in human natural killer cells. Toxicol. Mech. Methods, 21, 577–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. McMahon T.A., et al. (2011) The fungicide chlorothalonil is nonlinearly associated with corticosterone levels, immunity, and mortality in amphibians. Environ. Health Perspect., 119, 1098–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Goldman J.M., et al. (2004) Methoxychlor-induced alterations in the histological expression of angiogenic factors in pituitary and uterus. J. Mol. Histol., 35, 363–375. [DOI] [PubMed] [Google Scholar]
- 40. Chapin R.E., et al. (1997) The effects of perinatal/juvenile methoxychlor exposure on adult rat nervous, immune, and reproductive system function. Fundam. Appl. Toxicol., 40, 138–157. [DOI] [PubMed] [Google Scholar]
- 41. Qian Y., et al. (2010) Perfluorooctane sulfonate (PFOS) induces reactive oxygen species (ROS) production in human microvascular endothelial cells: role in endothelial permeability. J. Toxicol. Environ. Health A, 73, 819–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hu J.X., et al. (2013) Toxic effects of cypermethrin on the male reproductive system: with emphasis on the androgen receptor. J. Appl. Toxicol., 33, 576–585. [DOI] [PubMed] [Google Scholar]
- 43. Jin M., et al. (2010) Estrogenic activities of two synthetic pyrethroids and their metabolites. J. Environ. Sci. (China), 22, 290–296. [DOI] [PubMed] [Google Scholar]
- 44. Kakko I., et al. (2004) Oestradiol potentiates the effects of certain pyrethroid compounds in the MCF7 human breast carcinoma cell line. Altern. Lab. Anim., 32, 383–390. [DOI] [PubMed] [Google Scholar]
- 45. Feng Z., et al. (2006) Acrolein is a major cigarette-related lung cancer agent: preferential binding at p53 mutational hotspots and inhibition of DNA repair. Proc. Natl Acad. Sci. USA, 103, 15404–15409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Günther M., et al. (2008) Acrolein: unwanted side product or contribution to antiangiogenic properties of metronomic cyclophosphamide therapy? J. Cell. Mol. Med., 12(6B), 2704–2716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Luo C., et al. (2013) A cigarette component acrolein induces accelerated senescence in human diploid fibroblast IMR-90 cells. Biogerontology, 14, 503–511. [DOI] [PubMed] [Google Scholar]
- 48. Roy J., et al. (2010) Acrolein induces apoptosis through the death receptor pathway in A549 lung cells: role of p53. Can. J. Physiol. Pharmacol., 88, 353–368. [DOI] [PubMed] [Google Scholar]
- 49. Tanel A., et al. (2014) Acrolein activates cell survival and apoptotic death responses involving the endoplasmic reticulum in A549 lung cells. Biochim. Biophys. Acta, 1843, 827–835. [DOI] [PubMed] [Google Scholar]
- 50. Tang M.S., et al. (2011) Acrolein induced DNA damage, mutagenicity and effect on DNA repair. Mol. Nutr. Food Res., 55, 1291–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cabeza-Arvelaiz Y., et al. (2012) Transcriptome analysis of a rotenone model of parkinsonism reveals complex I-tied and -untied toxicity mechanisms common to neurodegenerative diseases. PLoS One, 7, e44700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Deng Y.T., et al. (2010) Rotenone induces apoptosis in MCF-7 human breast cancer cell-mediated ROS through JNK and p38 signaling. Mol. Carcinog., 49, 141–151. [DOI] [PubMed] [Google Scholar]
- 53. Gonçalves A.P., et al. (2011) Involvement of p53 in cell death following cell cycle arrest and mitotic catastrophe induced by rotenone. Biochim. Biophys. Acta, 1813, 492–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Li Y., et al. (2013) Copper induces cellular senescence in human glioblastoma multiforme cells through downregulation of Bmi-1. Oncol. Rep., 29, 1805–1810. [DOI] [PubMed] [Google Scholar]
- 55. Ostrakhovitch E.A., et al. (2005) Role of p53 and reactive oxygen species in apoptotic response to copper and zinc in epithelial breast cancer cells. Apoptosis, 10, 111–121. [DOI] [PubMed] [Google Scholar]
- 56. Parr-Sturgess C.A., et al. (2012) Copper modulates zinc metalloproteinase-dependent ectodomain shedding of key signaling and adhesion proteins and promotes the invasion of prostate cancer epithelial cells. Mol. Cancer Res., 10, 1282–1293. [DOI] [PubMed] [Google Scholar]
- 57. Freitas M., et al. (2013) Nickel induces apoptosis in human neutrophils. Biometals, 26, 13–21. [DOI] [PubMed] [Google Scholar]
- 58. Wu C.H., et al. (2012) Nickel-induced epithelial-mesenchymal transition by reactive oxygen species generation and E-cadherin promoter hypermethylation. J. Biol. Chem., 287, 25292–25302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Aimola P., et al. (2012) Cadmium induces p53-dependent apoptosis in human prostate epithelial cells. PLoS One, 7, e33647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Yuan D., et al. (2013) Long-term cadmium exposure leads to the enhancement of lymphocyte proliferation via down-regulating p16 by DNA hypermethylation. Mutat. Res., 757, 125–131. [DOI] [PubMed] [Google Scholar]
- 61. Aluigi M.G., et al. (2010) Apoptosis as a specific biomarker of diazinon toxicity in NTera2-D1 cells. Chem. Biol. Interact., 187, 299–303. [DOI] [PubMed] [Google Scholar]
- 62. Giordano G., et al. (2007) Organophosphorus insecticides chlorpyrifos and diazinon and oxidative stress in neuronal cells in a genetic model of glutathione deficiency. Toxicol. Appl. Pharmacol., 219, 181–189. [DOI] [PubMed] [Google Scholar]
- 63. Gilsing A.M., et al. (2013) Dietary heme iron and the risk of colorectal cancer with specific mutations in KRAS and APC. Carcinogenesis, 34, 2757–2766. [DOI] [PubMed] [Google Scholar]
- 64. Pluth J.M., et al. (1996) Increased frequency of specific genomic deletions resulting from in vitro malathion exposure. Cancer Res., 56, 2393–2399. [PubMed] [Google Scholar]
- 65. Chen Z.J., et al. (2014) Bisphenol A modulates colorectal cancer protein profile and promotes the metastasis via induction of epithelial to mesenchymal transitions. Arch Toxicol. [DOI] [PubMed] [Google Scholar]
- 66. Zhu H., et al. (2010) Environmental endocrine disruptors promote invasion and metastasis of SK-N-SH human neuroblastoma cells. Oncol. Rep., 23, 129–139. [PubMed] [Google Scholar]
- 67. Pontillo C.A., et al. (2013) Action of hexachlorobenzene on tumor growth and metastasis in different experimental models. Toxicol. Appl. Pharmacol., 268, 331–342. [DOI] [PubMed] [Google Scholar]
- 68. O'Brien D.W., et al. (2004) A mechanism of airway injury in an epithelial model of mucociliary clearance. Respir. Res., 5, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Ornstein D.L., et al. (2007) Iron stimulates urokinase plasminogen activator expression and activates NF-kappa B in human prostate cancer cells. Nutr. Cancer, 58, 115–126. [DOI] [PubMed] [Google Scholar]
- 70. Mao L., et al. (2012) Circadian gating of epithelial-to-mesenchymal transition in breast cancer cells via melatonin-regulation of GSK3β. Mol. Endocrinol., 26, 1808–1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Papagerakis S., et al. (2014) The circadian clock in oral health and diseases. J. Dent. Res., 93, 27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Bouskine A., et al. (2009) Low doses of bisphenol A promote human seminoma cell proliferation by activating PKA and PKG via a membrane G-protein-coupled estrogen receptor. Environ. Health Perspect., 117, 1053–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Hernández L.G., et al. (2013) A mode-of-action approach for the identification of genotoxic carcinogens. PLoS One, 8, e64532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Wetherill Y.B., et al. (2002) The xenoestrogen bisphenol A induces inappropriate androgen receptor activation and mitogenesis in prostatic adenocarcinoma cells. Mol. Cancer Ther., 1, 515–524. [PubMed] [Google Scholar]
- 75. Park S.H., et al. (2009) Cell growth of ovarian cancer cells is stimulated by xenoestrogens through an estrogen-dependent pathway, but their stimulation of cell growth appears not to be involved in the activation of the mitogen-activated protein kinases ERK-1 and p38. J. Reprod. Dev., 55, 23–29. [DOI] [PubMed] [Google Scholar]
- 76. Wilkinson C.F., et al. (1996) A mechanistic interpretation of the oncogenicity of chlorothalonil in rodents and an assessment of human relevance. Regul. Toxicol. Pharmacol., 24(1 Pt 1), 69–84. [DOI] [PubMed] [Google Scholar]
- 77. Vesselinovitch S.D., et al. (1983) Lindane bioassay studies and human cancer risk assessment. Toxicol. Pathol., 11, 12–22. [DOI] [PubMed] [Google Scholar]
- 78. Wang Q.L., et al. (2013) Risk assessment of mouse gastric tissue cancer induced by dichlorvos and dimethoate. Oncol. Lett., 5, 1385–1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Lee H.R., et al. (2012) Treatment with bisphenol A and methoxychlor results in the growth of human breast cancer cells and alteration of the expression of cell cycle-related genes, cyclin D1 and p21, via an estrogen receptor-dependent signaling pathway. Int. J. Mol. Med., 29, 883–890. [DOI] [PubMed] [Google Scholar]
- 80. Stagg N.J., et al. (2012) Assessment of possible carcinogenicity of oxyfluorfen to humans using mode of action analysis of rodent liver effects. Toxicol. Sci., 128, 334–345. [DOI] [PubMed] [Google Scholar]
- 81. Doull J., et al. (1999) A cancer risk assessment of di(2-ethylhexyl)phthalate: application of the new U.S. EPA Risk Assessment Guidelines. Regul. Toxicol. Pharmacol., 29, 327–357. [DOI] [PubMed] [Google Scholar]
- 82. Mazzoleni G., et al. (1994) Influence of the herbicide Linuron on growth rate and gap-junctional intercellular communication of cultured endothelial cells. J. Environ. Pathol. Toxicol. Oncol., 13, 1–10. [PubMed] [Google Scholar]
- 83. Yasaei H., et al. (2013) Carcinogen-specific mutational and epigenetic alterations in INK4A, INK4B and p53 tumour-suppressor genes drive induced senescence bypass in normal diploid mammalian cells. Oncogene, 32, 171–179. [DOI] [PubMed] [Google Scholar]
- 84. Singh K.P., et al. (2008) Allelic loss and mutations in a new ETRG-1 gene are early events in diethylstilbestrol-induced renal carcinogenesis in Syrian hamsters. Gene, 408, 18–26. [DOI] [PubMed] [Google Scholar]
- 85. Tsutsui T., et al. (1994) Reserpine-induced cell transformation without detectable genetic effects in Syrian hamster embryo cells in culture. Carcinogenesis, 15, 11–14. [DOI] [PubMed] [Google Scholar]
- 86. Martens U., et al. (1996) Low expression of the WAF1/CIP1 gene product, p21, in enzyme-altered foci induced in rat liver by diethylnitrosamine or phenobarbital. Cancer Lett., 104, 21–26. [DOI] [PubMed] [Google Scholar]
- 87. Geter D.R., et al. (2014) Dose-response modeling of early molecular and cellular key events in the CAR-mediated hepatocarcinogenesis pathway. Toxicol. Sci., 138, 425–445. [DOI] [PubMed] [Google Scholar]
- 88. Bader A., et al. (2011) Paracetamol treatment increases telomerase activity in rat embryonic liver cells. Pharmacol. Rep., 63, 1435–1441. [DOI] [PubMed] [Google Scholar]
- 89. Tsuruga Y., et al. (2008) Establishment of immortalized human hepatocytes by introduction of HPV16 E6/E7 and hTERT as cell sources for liver cell-based therapy. Cell Transplant., 17, 1083–1094. [PubMed] [Google Scholar]
- 90. Nguyen T.H., et al. (2005) Treatment of acetaminophen-induced acute liver failure in the mouse with conditionally immortalized human hepatocytes. J. Hepatol., 43, 1031–1037. [DOI] [PubMed] [Google Scholar]
- 91. Bode-Böger S.M., et al. (2005) Aspirin reduces endothelial cell senescence. Biochem. Biophys. Res. Commun., 334, 1226–1232. [DOI] [PubMed] [Google Scholar]
- 92. Heinloth A.N., et al. (2004) Gene expression profiling of rat livers reveals indicators of potential adverse effects. Toxicol. Sci., 80, 193–202. [DOI] [PubMed] [Google Scholar]
- 93. Jacob T., et al. (2009) The effect of cotinine on telomerase activity in human vascular smooth muscle cells. J. Cardiovasc. Surg. (Torino), 50, 345–349. [PubMed] [Google Scholar]
- 94. Brüne B., et al. (2001) Transcription factors p53 and HIF-1alpha as targets of nitric oxide. Cell. Signal., 13, 525–533. [DOI] [PubMed] [Google Scholar]
- 95. Davis C.D., et al. (2000) Dietary selenium and arsenic affect DNA methylation in vitro in Caco-2 cells and in vivo in rat liver and colon. J. Nutr., 130, 2903–2909. [DOI] [PubMed] [Google Scholar]
- 96. Arnér E.S., et al. (2006) The thioredoxin system in cancer. Semin. Cancer Biol., 16, 420–426. [DOI] [PubMed] [Google Scholar]
- 97. vom Saal F.S., et al. (2007) Chapel Hill bisphenol A expert panel consensus statement: integration of mechanisms, effects in animals and potential to impact human health at current levels of exposure. Reprod. Toxicol., 24, 131–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Qin X.Y., et al. (2012) Effects of bisphenol A exposure on the proliferation and senescence of normal human mammary epithelial cells. Cancer Biol. Ther., 13, 296–306. [DOI] [PubMed] [Google Scholar]
- 99. Peluso M.E., et al. (2014) Bisphenol-A exposures and behavioural aberrations: median and linear spline and meta-regression analyses of 12 toxicity studies in rodents. Toxicology, 325, 200–208. [DOI] [PubMed] [Google Scholar]
- 100. Fang C.C., et al. (2013) Cyprodinil as an activator of aryl hydrocarbon receptor. Toxicology, 304, 32–40. [DOI] [PubMed] [Google Scholar]
- 101. Bharadwaj R., et al. (2004) The spindle checkpoint, aneuploidy, and cancer. Oncogene, 23, 2016–2027. [DOI] [PubMed] [Google Scholar]
- 102. Orton F., et al. (2011) Widely used pesticides with previously unknown endocrine activity revealed as in vitro antiandrogens. Environ. Health Perspect., 119, 794–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Tanaka T., et al. (2013) Effects of maternal exposure to imazalil on behavioral development in F₁-generation mice. Birth Defects Res. B Dev. Reprod. Toxicol., 98, 334–342. [DOI] [PubMed] [Google Scholar]
- 104. Ahmad I., et al. (2008) The involvement of nitric oxide in maneb- and paraquat-induced oxidative stress in rat polymorphonuclear leukocytes. Free Radic. Res., 42, 849–862. [DOI] [PubMed] [Google Scholar]
- 105.US Environmental Protection Agency (1988) US Integrated Risk Information System—Maneb (CASRN 12427-38-2). http://www.epa.gov/iris/subst/0249.htm . [Google Scholar]
- 106. Miller K.P., et al. (2006) Methoxychlor metabolites may cause ovarian toxicity through estrogen-regulated pathways. Toxicol. Sci., 93, 180–188. [DOI] [PubMed] [Google Scholar]
- 107. Du X., et al. (2014) Perinatal exposure to low-dose methoxychlor impairs testicular development in C57BL/6 mice. PLoS One, 9, e103016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Palanza P., et al. (2001) Effects of prenatal exposure to low doses of diethylstilbestrol, o,p'DDT, and methoxychlor on postnatal growth and neurobehavioral development in male and female mice. Horm. Behav., 40, 252–265. [DOI] [PubMed] [Google Scholar]
- 109. Du G., et al. (2013) Perfluorooctane sulfonate (PFOS) affects hormone receptor activity, steroidogenesis, and expression of endocrine-related genes in vitro and in vivo . Environ. Toxicol. Chem., 32, 353–360. [DOI] [PubMed] [Google Scholar]
- 110. Kim H.S., et al. (2011) Induction of apoptosis and CYP4A1 expression in Sprague-Dawley rats exposed to low doses of perfluorooctane sulfonate. J. Toxicol. Sci., 36, 201–210. [DOI] [PubMed] [Google Scholar]
- 111. Eveillard A., et al. (2009) Di-(2-ethylhexyl)-phthalate (DEHP) activates the constitutive androstane receptor (CAR): a novel signalling pathway sensitive to phthalates. Biochem. Pharmacol., 77, 1735–1746. [DOI] [PubMed] [Google Scholar]
- 112. Nakai M., et al. (1999) Binding characteristics of dialkyl phthalates for the estrogen receptor. Biochem. Biophys. Res. Commun., 254, 311–314. [DOI] [PubMed] [Google Scholar]
- 113. Grande S.W., et al. (2006) A dose-response study following in utero and lactational exposure to di(2-ethylhexyl)phthalate: effects on female rat reproductive development. Toxicol. Sci., 91, 247–254. [DOI] [PubMed] [Google Scholar]
- 114. Kojima H., et al. (2011) Comparative study of human and mouse pregnane X receptor agonistic activity in 200 pesticides using in vitro reporter gene assays. Toxicology, 280, 77–87. [DOI] [PubMed] [Google Scholar]
- 115. (2006) Phosalone Reregistration Eligibility Decision (RED). The United States Environmental Protection Agency Office of Pesticide Programs. [Google Scholar]
- 116. Li X., et al. (2013) Structure-dependent activities of hydroxylated polybrominated diphenyl ethers on human estrogen receptor. Toxicology, 309, 15–22. [DOI] [PubMed] [Google Scholar]
- 117. Berger R.G., et al. (2014) Exposure to an environmentally relevant mixture of brominated flame retardants affects fetal development in Sprague-Dawley rats. Toxicology, 320, 56–66. [DOI] [PubMed] [Google Scholar]
- 118. Hofmeister M.V., et al. (2004) Effects of the pesticides prochloraz and methiocarb on human estrogen receptor alpha and beta mRNA levels analyzed by on-line RT-PCR. Toxicol. In Vitro, 18, 427–433. [DOI] [PubMed] [Google Scholar]
- 119. Jacobsen P.R., et al. (2012) Persistent developmental toxicity in rat offspring after low dose exposure to a mixture of endocrine disrupting pesticides. Reprod. Toxicol., 34, 237–250. [DOI] [PubMed] [Google Scholar]
- 120. Kamanga-Sollo E., et al. (2008) Roles of IGF-I and the estrogen, androgen and IGF-I receptors in estradiol-17beta- and trenbolone acetate-stimulated proliferation of cultured bovine satellite cells. Domest. Anim. Endocrinol., 35, 88–97. [DOI] [PubMed] [Google Scholar]
- 121. Yarrow J.F., et al. (2010) Tissue selectivity and potential clinical applications of trenbolone (17beta-hydroxyestra-4,9,11-trien-3-one): a potent anabolic steroid with reduced androgenic and estrogenic activity. Steroids, 75, 377–389. [DOI] [PubMed] [Google Scholar]
- 122. Yan H., et al. (2008) Exposure to bisphenol A prenatally or in adulthood promotes T(H)2 cytokine production associated with reduction of CD4CD25 regulatory T cells. Environ. Health Perspect., 116, 514–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Erden E.S., et al. (2014) Investigation of Bisphenol A as an endocrine disruptor, total thiol, malondialdehyde, and C-reactive protein levels in chronic obstructive pulmonary disease. Eur. Rev. Med. Pharmacol. Sci., 18, 3477–3483. [PubMed] [Google Scholar]
- 124. Kharrazian D. (2014) The potential roles of bisphenol A (BPA) pathogenesis in autoimmunity. Autoimmune Dis., 2014, 743616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Liu Y., et al. (2014) Modulation of cytokine expression in human macrophages by endocrine-disrupting chemical Bisphenol-A. Biochem. Biophys. Res. Commun., 451, 592–598. [DOI] [PubMed] [Google Scholar]
- 126. Rogers J.A., et al. (2013) Review: endocrine disrupting chemicals and immune responses: a focus on bisphenol-A and its potential mechanisms. Mol. Immunol., 53, 421–430. [DOI] [PubMed] [Google Scholar]
- 127. Deutschle T., et al. (2008) A controlled challenge study on di(2-ethylhexyl) phthalate (DEHP) in house dust and the immune response in human nasal mucosa of allergic subjects. Environ. Health Perspect., 116, 1487–1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Peltier M.R., et al. (2012) Polybrominated diphenyl ethers enhance the production of proinflammatory cytokines by the placenta. Placenta, 33, 745–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Park H.R., et al. (2014) Involvement of reactive oxygen species in brominated diphenyl ether-47-induced inflammatory cytokine release from human extravillous trophoblasts in vitro . Toxicol. Appl. Pharmacol., 274, 283–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Park H.R., et al. (2014) Protective effect of nuclear factor E2-related factor 2 on inflammatory cytokine response to brominated diphenyl ether-47 in the HTR-8/SVneo human first trimester extravillous trophoblast cell line. Toxicol. Appl. Pharmacol., 281, 67–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Koike E., et al. (2014) Penta- and octa-bromodiphenyl ethers promote proinflammatory protein expression in human bronchial epithelial cells in vitro . Toxicol. In Vitro, 28, 327–333. [DOI] [PubMed] [Google Scholar]
- 132. Zhao S., et al. (2013) Sub-acute exposure to the herbicide atrazine suppresses cell immune functions in adolescent mice. Biosci. Trends, 7, 193–201. [PubMed] [Google Scholar]
- 133. Rowe A.M., et al. (2006) Immunomodulatory effects of maternal atrazine exposure on male Balb/c mice. Toxicol. Appl. Pharmacol., 214, 69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Skinner M.K., et al. (2007) Epigenetic transgenerational actions of vinclozolin on the development of disease and cancer. Crit. Rev. Oncog., 13, 75–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Anway M.D., et al. (2008) Transgenerational effects of the endocrine disruptor vinclozolin on the prostate transcriptome and adult onset disease. Prostate, 68, 517–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Cowin P.A., et al. (2008) Early-onset endocrine disruptor-induced prostatitis in the rat. Environ. Health Perspect., 116, 923–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Zhou H.R., et al. (2003) Rapid, sequential activation of mitogen-activated protein kinases and transcription factors precedes proinflammatory cytokine mRNA expression in spleens of mice exposed to the trichothecene vomitoxin. Toxicol. Sci., 72, 130–142. [DOI] [PubMed] [Google Scholar]
- 138. Shin S.G., et al. (2005) Suppression of inducible nitric oxide synthase and cyclooxygenase-2 expression in RAW 264.7 macrophages by sesquiterpene lactones. J. Toxicol. Environ. Health A, 68, 2119–2131. [DOI] [PubMed] [Google Scholar]
- 139. Gollamudi S., et al. (2012) Concordant signaling pathways produced by pesticide exposure in mice correspond to pathways identified in human Parkinson's disease. PLoS One, 7, e36191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Morgan J.B., et al. (2010) The marine sponge metabolite mycothiazole: a novel prototype mitochondrial complex I inhibitor. Bioorg. Med. Chem., 18, 5988–5994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.(1997) BASF Corporation Pyridaben (Sanmite) Pesticide Tolerance Petition 3/97, US EPA [PF-721; FRL-5592 -7], http//pmep.cce.cornell. edu/profiles/insect-mite/mevinphos-propargite/pyridaben/ pyridab_pet_0397.html (accessed 7 May 2015) [Google Scholar]
- 142. Barros S.P., et al. (2010) Triclosan inhibition of acute and chronic inflammatory gene pathways. J. Clin. Periodontol., 37, 412–418. [DOI] [PubMed] [Google Scholar]
- 143. Wallet M.A., et al. (2013) Triclosan alters antimicrobial and inflammatory responses of epithelial cells. Oral Dis., 19, 296–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Bhargava H.N., et al. (1996) Triclosan: applications and safety. Am. J. Infect. Control, 24, 209–218. [DOI] [PubMed] [Google Scholar]
- 145. Winitthana T., et al. (2014) Triclosan potentiates epithelial-to-mesenchymal transition in anoikis-resistant human lung cancer cells. PLoS One, 9, e110851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Stoker T.E., et al. (2010) Triclosan exposure modulates estrogen-dependent responses in the female wistar rat. Toxicol. Sci., 117, 45–53. [DOI] [PubMed] [Google Scholar]
- 147. Shioda T., et al. (2006) Importance of dosage standardization for interpreting transcriptomal signature profiles: evidence from studies of xenoestrogens. Proc. Natl Acad. Sci. USA, 103, 12033–12038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Welshons W.V., et al. (1999) Low-dose bioactivity of xenoestrogens in animals: fetal exposure to low doses of methoxychlor and other xenoestrogens increases adult prostate size in mice. Toxicol. Ind. Health, 15, 12–25. [DOI] [PubMed] [Google Scholar]
- 149. Alyea R.A., et al. (2009) Differential regulation of dopamine transporter function and location by low concentrations of environmental estrogens and 17beta-estradiol. Environ. Health Perspect., 117, 778–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Wozniak A.L., et al. (2005) Xenoestrogens at picomolar to nanomolar concentrations trigger membrane estrogen receptor-alpha-mediated Ca2+ fluxes and prolactin release in GH3/B6 pituitary tumor cells. Environ. Health Perspect., 113, 431–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Jeng Y.J., et al. (2011) Combinations of physiologic estrogens with xenoestrogens alter ERK phosphorylation profiles in rat pituitary cells. Environ. Health Perspect., 119, 104–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Cabaton N.J., et al. (2011) Perinatal exposure to environmentally relevant levels of bisphenol A decreases fertility and fecundity in CD-1 mice. Environ. Health Perspect., 119, 547–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Jones B.A., et al. (2011) Pre- and postnatal bisphenol A treatment results in persistent deficits in the sexual behavior of male rats, but not female rats, in adulthood. Horm. Behav., 59, 246–251. [DOI] [PubMed] [Google Scholar]
- 154. Lemos M.F., et al. (2010) Protein differential expression induced by endocrine disrupting compounds in a terrestrial isopod. Chemosphere, 79, 570–576. [DOI] [PubMed] [Google Scholar]
- 155. Markey C.M., et al. (2001) The mouse uterotrophic assay: a reevaluation of its validity in assessing the estrogenicity of bisphenol A. Environ. Health Perspect., 109, 55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Filipov N.M., et al. (2005) Manganese potentiates in vitro production of proinflammatory cytokines and nitric oxide by microglia through a nuclear factor kappa B–dependent mechanism. Toxicol. Sci., 84, 139–148. [DOI] [PubMed] [Google Scholar]
- 157. Knudsen T.B., et al. (2011) Disruption of embryonic vascular development in predictive toxicology. Birth Defects Res. Part C, 93, 312–323. [DOI] [PubMed] [Google Scholar]
- 158. Qin R., et al. (2011) Protection by tetrahydroxystilbene glucoside against neurotoxicity induced by MPP+: the involvement of PI3K/Akt pathway activation. Toxicol. Lett., 202, 1–7. [DOI] [PubMed] [Google Scholar]
- 159. Manfo F.P., et al. (2011) Effects of maneb on testosterone release in male rats. Drug Chem. Toxicol., 34, 120–128. [DOI] [PubMed] [Google Scholar]
- 160. Matsushita T., et al. (1976) Experimental study on contact dermatitis caused by dithiocarbamates maneb, mancozeb, zineb, and their related compounds. Int. Arch. Occup. Environ. Health, 37, 169–178. [DOI] [PubMed] [Google Scholar]
- 161. Barlow, B. et al. (2005) Modulation of antioxidant defense systems by the environmental pesticide Maneb in dopaminergic cells. Neurotoxicol., 26, 63–75 . [DOI] [PubMed] [Google Scholar]
- 162. Kazantseva Y.A., et al. (2013) Dichlorodiphenyltrichloroethane technical mixture regulates cell cycle and apoptosis genes through the activation of CAR and ERα in mouse livers. Toxicol. Appl. Pharmacol., 271, 137–143. [DOI] [PubMed] [Google Scholar]
- 163. Lin Z.X., et al. (1986) Inhibition of gap junctional intercellular communication in human teratocarcinoma cells by organochlorine pesticides. Toxicol. Appl. Pharmacol., 83, 10–19. [DOI] [PubMed] [Google Scholar]
- 164. Ruch R.J., et al. (1987) Inhibition of intercellular communication between mouse hepatocytes by tumor promoters. Toxicol. Appl. Pharmacol., 87, 111–120. [DOI] [PubMed] [Google Scholar]
- 165. Ventura C., et al. (2012) Differential mechanisms of action are involved in chlorpyrifos effects in estrogen-dependent or -independent breast cancer cells exposed to low or high concentrations of the pesticide. Toxicol. Lett., 213, 184–193. [DOI] [PubMed] [Google Scholar]
- 166. Mense S.M., et al. (2006) The common insecticides cyfluthrin and chlorpyrifos alter the expression of a subset of genes with diverse functions in primary human astrocytes. Toxicol. Sci., 93, 125–135. [DOI] [PubMed] [Google Scholar]
- 167. Santucci M.A., et al. (2003) Cell-cycle deregulation in BALB/c 3T3 cells transformed by 1,2-dibromoethane and folpet pesticides. Environ. Mol. Mutagen., 41, 315–321. [DOI] [PubMed] [Google Scholar]
- 168. Albanito L., et al. (2008) G-protein-coupled receptor 30 and estrogen receptor-alpha are involved in the proliferative effects induced by atrazine in ovarian cancer cells. Environ. Health Perspect., 116, 1648–1655. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 169. Tsuda H., et al. (2005) High susceptibility of human c-Ha-ras proto-oncogene transgenic rats to carcinogenesis: a cancer-prone animal model. Cancer Sci., 96, 309–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Wetzel L.T., et al. (1994) Chronic effects of atrazine on estrus and mammary tumor formation in female Sprague-Dawley and Fischer 344 rats. J. Toxicol. Environ. Health, 43, 169–182. [DOI] [PubMed] [Google Scholar]
- 171. Andersson H., et al. (2012) Proangiogenic effects of environmentally relevant levels of bisphenol A in human primary endothelial cells. Arch. Toxicol., 86, 465–474. [DOI] [PubMed] [Google Scholar]
- 172. Dairkee S.H., et al. (2013) Bisphenol-A-induced inactivation of the p53 axis underlying deregulation of proliferation kinetics, and cell death in non-malignant human breast epithelial cells. Carcinogenesis, 34, 703–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Betancourt A.M., et al. (2012) Altered carcinogenesis and proteome in mammary glands of rats after prepubertal exposures to the hormonally active chemicals bisphenol A and genistein. J. Nutr, 142, 1382S–1388S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Andrysík Z., et al. (2013) Aryl hydrocarbon receptor-mediated disruption of contact inhibition is associated with connexin43 downregulation and inhibition of gap junctional intercellular communication. Arch. Toxicol., 87, 491–503. [DOI] [PubMed] [Google Scholar]
- 175. Haber L.T., et al. (2000) Hazard identification and dose response of inhaled nickel-soluble salts. Regul. Toxicol. Pharmacol., 31, 210–230. [DOI] [PubMed] [Google Scholar]
- 176. LN V., et al. (2013) Low dose effects of bisphenol A: an integrated review of in vitro, laboratory animal and human studies. Endocrine Disruptors, 1, e1.1–e1.20. [Google Scholar]
- 177. Tryphonas H., et al. (2004) Oral (gavage), in utero and post-natal exposure of Sprague-Dawley rats to low doses of tributyltin chloride. Part II: effects on the immune system. Food Chem. Toxicol., 42, 221–235. [DOI] [PubMed] [Google Scholar]
- 178. Watanabe J., et al. (2013) Low dose of methylmercury (MeHg) exposure induces caspase mediated-apoptosis in cultured neural progenitor cells. J. Toxicol. Sci., 38, 931–935. [DOI] [PubMed] [Google Scholar]
- 179. Petroni D., et al. (2012) Low-dose methylmercury-induced oxidative stress, cytotoxicity, and tau-hyperphosphorylation in human neuroblastoma (SH-SY5Y) cells. Environ. Toxicol., 27, 549–555. [DOI] [PubMed] [Google Scholar]
- 180. McCormack A.L., et al. (2005) Role of oxidative stress in paraquat-induced dopaminergic cell degeneration. J. Neurochem., 93, 1030–1037. [DOI] [PubMed] [Google Scholar]
- 181. Hartwig A., et al. (2002) Interference by toxic metal ions with DNA repair processes and cell cycle control: molecular mechanisms. Environ. Health Perspect., 110( Suppl 5 ), 797–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Asmuss M., et al. (2000) Differential effects of toxic metal compounds on the activities of Fpg and XPA, two zinc finger proteins involved in DNA repair. Carcinogenesis, 21, 2097–2104. [DOI] [PubMed] [Google Scholar]
- 183. McNeill D.R., et al. (2004) Inhibition of Ape1 nuclease activity by lead, iron, and cadmium. Environ. Health Perspect., 112, 799–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Pottier G., et al. (2013) Lead exposure induces telomere instability in human cells. PLoS One, 8, e67501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Zhang X., et al. (2013) Environmental and occupational exposure to chemicals and telomere length in human studies. Occup. Environ. Med., 70, 743–749. [DOI] [PubMed] [Google Scholar]
- 186. Exon J.H. (2006) A review of the toxicology of acrylamide. J. Toxicol. Environ. Health B. Crit. Rev., 9, 397–412. [DOI] [PubMed] [Google Scholar]
- 187. Sickles D.W., et al. (2007) Acrylamide effects on kinesin-related proteins of the mitotic/meiotic spindle. Toxicol. Appl. Pharmacol., 222, 111–121. [DOI] [PubMed] [Google Scholar]
- 188. Wang X., et al. (2013) Epigenotoxicity of environmental pollutants evaluated by a combination of DNA methylation inhibition and capillary electrophoresis-laser-induced fluorescence immunoassay. Anal. Bioanal. Chem., 405, 2435–2442. [DOI] [PubMed] [Google Scholar]
- 189. Arita A., et al. (2012) Global levels of histone modifications in peripheral blood mononuclear cells of subjects with exposure to nickel. Environ. Health Perspect., 120, 198–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Cantone L., et al. (2011) Inhalable metal-rich air particles and histone H3K4 dimethylation and H3K9 acetylation in a cross-sectional study of steel workers. Environ. Health Perspect., 119, 964–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Chervona Y., et al. (2012) Carcinogenic metals and the epigenome: understanding the effect of nickel, arsenic, and chromium. Metallomics, 4, 619–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Avissar-Whiting M., et al. (2010) Bisphenol A exposure leads to specific microRNA alterations in placental cells. Reprod. Toxicol., 29, 401–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Roedel E.Q., et al. (2012) Pulmonary toxicity after exposure to military-relevant heavy metal tungsten alloy particles. Toxicol. Appl. Pharmacol., 259, 74–86. [DOI] [PubMed] [Google Scholar]
- 194. Freyre-Fonseca V., et al. (2011) Titanium dioxide nanoparticles impair lung mitochondrial function. Toxicol. Lett., 202, 111–119. [DOI] [PubMed] [Google Scholar]
- 195. Elhajouji A., et al. (2011) Potential thresholds for genotoxic effects by micronucleus scoring. Mutagenesis, 26, 199–204. [DOI] [PubMed] [Google Scholar]
- 196. Ermler S., et al. (2013) Seven benzimidazole pesticides combined at sub-threshold levels induce micronuclei in vitro . Mutagenesis, 28, 417–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Sargent L.M., et al. (2012) Single-walled carbon nanotube-induced mitotic disruption. Mutat. Res., 745, 28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Muller J., et al. (2008) Clastogenic and aneugenic effects of multi-wall carbon nanotubes in epithelial cells. Carcinogenesis, 29, 427–433. [DOI] [PubMed] [Google Scholar]
- 199. Thomas D. (2010) Gene–environment-wide association studies: emerging approaches. Nat. Rev. Genet., 11, 259–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Santella R.M., et al. (2005) DNA adducts, DNA repair genotype/phenotype and cancer risk. Mutat. Res., 592, 29–35. [DOI] [PubMed] [Google Scholar]
- 201. (2011) Cytogenetic Dosimetry: Applications in Preparedness for and Response to Radiation Emergencies. International Atomic Energy Agency, Vienna. [Google Scholar]
- 202. De Lange T. (2005) Telomere-related genome instability in cancer. Cold Spring Harb. Symp. Quant. Biol., 70, 197–204. [DOI] [PubMed] [Google Scholar]
- 203. Frias C., et al. (2012) Telomere dysfunction and genome instability. Front. Biosci. (Landmark Ed), 17, 2181–2196. [DOI] [PubMed] [Google Scholar]
- 204. Hollstein M., et al. (1991) p53 mutations in human cancers. Science, 253, 49–53. [DOI] [PubMed] [Google Scholar]
- 205. Jang J.W., et al. (2006) Isoform-specific ras activation and oncogene dependence during MYC- and Wnt-induced mammary tumorigenesis. Mol. Cell. Biol., 26, 8109–8121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Muñoz D.M., et al. (2013) Loss of p53 cooperates with K-ras activation to induce glioma formation in a region-independent manner. Glia, 61, 1862–1872. [DOI] [PubMed] [Google Scholar]
- 207. Pierotti, M.A. et al. Mechanisms of oncogene activation. Kufe DW, Pollock RE, Weichselbaum RR, and et al. Holland-Frei Cancer Medicine. 6th. 2003. Hamilton (ON), BC Decker . [Google Scholar]
- 208. Mazzei F., et al. (2013) Role of MUTYH in human cancer. Mutat. Res., 743–744, 33–43. [DOI] [PubMed] [Google Scholar]
- 209. Sancar A. (1995) Excision repair in mammalian cells. J. Biol. Chem., 270, 15915–15918. [DOI] [PubMed] [Google Scholar]
- 210. Vineis P., et al. (2009) A field synopsis on low-penetrance variants in DNA repair genes and cancer susceptibility. J. Natl Cancer Inst., 101, 24–36. [DOI] [PubMed] [Google Scholar]
- 211. Bohacek J., et al. (2013) Epigenetic inheritance of disease and disease risk. Neuropsychopharmacology, 38, 220–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212. Esteller M. (2007) Cancer epigenomics: DNA methylomes and histone-modification maps. Nat. Rev. Genet., 8, 286–298. [DOI] [PubMed] [Google Scholar]
- 213. Caffarelli E., et al. (2011) Epigenetic regulation in cancer development. Front. Biosci. (Landmark Ed), 16, 2682–2694. [DOI] [PubMed] [Google Scholar]
- 214. Croce C.M. (2009) Causes and consequences of microRNA dysregulation in cancer. Nat. Rev. Genet., 10, 704–714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Wang Y., et al. (2013) MicroRNAs and DNA damage response: implications for cancer therapy. Cell Cycle, 12, 32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Devalle S., et al. (2012) Implications of aneuploidy for stem cell biology and brain therapeutics. Front. Cell. Neurosci., 6, 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. Linschooten J.O., et al. (2013) Paternal lifestyle as a potential source of germline mutations transmitted to offspring. FASEB J., 27, 2873–2879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218. Leyns L., et al. (2012) Genomic integrity of mouse embryonic stem cells. In Embryogenesis. Intech. pp. 333–358. [Google Scholar]
- 219. Blessing H., et al. (2004) Interaction of selenium compounds with zinc finger proteins involved in DNA repair. Eur. J. Biochem., 271, 3190–3199. [DOI] [PubMed] [Google Scholar]
- 220. Zhang X., et al. (2013) Environmental and occupational exposure to chemicals and telomere length in human studies. Postgrad. Med. J., 89, 722–728. [DOI] [PubMed] [Google Scholar]
- 221. Lombaert N., et al. (2013) Hard-metal (WC-Co) particles trigger a signaling cascade involving p38 MAPK, HIF-1α, HMOX1, and p53 activation in human PBMC. Arch. Toxicol., 87, 259–268. [DOI] [PubMed] [Google Scholar]
- 222. Jugan M.L., et al. (2012) Titanium dioxide nanoparticles exhibit genotoxicity and impair DNA repair activity in A549 cells. Nanotoxicology, 6, 501–513. [DOI] [PubMed] [Google Scholar]
- 223. Song M.F., et al. (2012) Metal nanoparticle-induced micronuclei and oxidative DNA damage in mice. J. Clin. Biochem. Nutr., 50, 211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Doshi T., et al. (2011) Hypermethylation of estrogen receptor promoter region in adult testis of rats exposed neonatally to bisphenol A. Toxicology, 289, 74–82. [DOI] [PubMed] [Google Scholar]
- 225. Kundakovic M., et al. (2013) Sex-specific epigenetic disruption and behavioral changes following low-dose in utero bisphenol A exposure. Proc. Natl Acad. Sci. USA, 110, 9956–9961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Pupo M., et al. (2012) Bisphenol A induces gene expression changes and proliferative effects through GPER in breast cancer cells and cancer-associated fibroblasts. Environ. Health Perspect., 120, 1177–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Ribeiro-Varandas E., et al. (2013) Bisphenol A at concentrations found in human serum induces aneugenic effects in endothelial cells. Mutat. Res., 751, 27–33. [DOI] [PubMed] [Google Scholar]
- 228. Marshall H. (2002) Fact sheet: carbendazim. Pesticides News, 57, 20–21. [Google Scholar]
- 229. Zhao Y., et al. (2010) Characterization and determination of chloro- and bromo-benzoquinones as new chlorination disinfection byproducts in drinking water. Anal. Chem., 82, 4599–4605. [DOI] [PubMed] [Google Scholar]
- 230. Piao M.J., et al. (2011) Silver nanoparticles induce oxidative cell damage in human liver cells through inhibition of reduced glutathione and induction of mitochondria-involved apoptosis. Toxicol. Lett., 201, 92–100. [DOI] [PubMed] [Google Scholar]
- 231. Gong C., et al. (2012) Methylation of PARP-1 promoter involved in the regulation of nano-SiO2-induced decrease of PARP-1 mRNA expression. Toxicol. Lett., 209, 264–269. [DOI] [PubMed] [Google Scholar]
- 232. Choi A.O., et al. (2008) Quantum dot-induced epigenetic and genotoxic changes in human breast cancer cells. J. Mol. Med. (Berl), 86, 291–302. [DOI] [PubMed] [Google Scholar]
- 233. Balansky R., et al. (2013) Transplacental clastogenic and epigenetic effects of gold nanoparticles in mice. Mutat. Res., 751–752, 42–48. [DOI] [PubMed] [Google Scholar]
- 234. Liu Y., et al. (2013) Understanding the toxicity of carbon nanotubes. Acc. Chem. Res., 46, 702–713. [DOI] [PubMed] [Google Scholar]
- 235. Chisholm H. (1910–1911) 11th Edition of Encyclopedia Britannica. Cambridge University Press, Cambridge, UK. [Google Scholar]
- 236. Stoker T.E., et al. (1999) Prepubertal exposure to compounds that increase prolactin secretion in the male rat: effects on the adult prostate. Biol. Reprod., 61, 1636–1643. [DOI] [PubMed] [Google Scholar]
- 237. Ho S.M., et al. (2006) Developmental exposure to estradiol and bisphenol A increases susceptibility to prostate carcinogenesis and epigenetically regulates phosphodiesterase type 4 variant 4. Cancer Res., 66, 5624–5632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238. Riu A., et al. (2011) Characterization of novel ligands of ERalpha, Erbeta, and PPARgamma: the case of halogenated bisphenol A and their conjugated metabolites. Toxicol. Sci, 122, 372–82. [DOI] [PubMed] [Google Scholar]
- 239. Riu A., et al. (2011) Peroxisome proliferator-activated receptor γ is a target for halogenated analogs of bisphenol A. Environ. Health Perspect., 119, 1227–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240. Thueson L.E., et al. (2015) In vitro exposure to the herbicide atrazine inhibits T cell activation, proliferation, and cytokine production and significantly increases the frequency of Foxp3+ regulatory T cells. Toxicol. Sci., 143, 418–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241. Hooghe R.J., et al. (2000) Effects of selected herbicides on cytokine production in vitro . Life Sci., 66, 2519–2525. [DOI] [PubMed] [Google Scholar]
- 242. Filipov N.M., et al. (2005) Immunotoxic effects of short-term atrazine exposure in young male C57BL/6 mice. Toxicol. Sci., 86, 324–332. [DOI] [PubMed] [Google Scholar]
- 243. Karrow N.A., et al. (2005) Oral exposure to atrazine modulates cell-mediated immune function and decreases host resistance to the B16F10 tumor model in female B6C3F1 mice. Toxicology, 209, 15–28. [DOI] [PubMed] [Google Scholar]
- 244. Basini G., et al. (2012) Atrazine disrupts steroidogenesis, VEGF and NO production in swine granulosa cells. Ecotoxicol. Environ. Saf., 85, 59–63. [DOI] [PubMed] [Google Scholar]
- 245. Chen J.Y., et al. (2013) Immunotoxicity of atrazine in Balb/c mice. J. Environ. Sci. Health B., 48, 637–645. [DOI] [PubMed] [Google Scholar]
- 246. Chen J., et al. (2015) Effects of atrazine on the proliferation and cytotoxicity of murine lymphocytes with the use of carboxyfluorescein succinimidyl ester-based flow cytometric approaches. Food Chem. Toxicol., 76, 61–69. [DOI] [PubMed] [Google Scholar]
- 247. Danelli L., et al. (2015) Mast cells boost myeloid-derived suppressor cell activity and contribute to the development of tumor-favoring microenvironment. Cancer Immunol. Res., 3, 85–95. [DOI] [PubMed] [Google Scholar]
- 248. Grimm E.A., et al. (2013) Molecular pathways: inflammation-associated nitric-oxide production as a cancer-supporting redox mechanism and a potential therapeutic target. Clin. Cancer Res., 19, 5557–5563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249. Costa A., et al. (2014) The role of reactive oxygen species and metabolism on cancer cells and their microenvironment. Semin. Cancer Biol., 25, 23–32. [DOI] [PubMed] [Google Scholar]
- 250. Lei Y., et al. (2015) Redox regulation of inflammation: old elements, a new story. Med. Res. Rev., 35, 306–340. [DOI] [PubMed] [Google Scholar]
- 251. Wu Y., et al. (2014) Molecular mechanisms underlying chronic inflammation-associated cancers. Cancer Lett., 345, 164–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252. Zhang H.Y., et al. (2014) Perinatal exposure to 4-nonylphenol affects adipogenesis in first and second generation rats offspring. Toxicol. Lett., 225, 325–332. [DOI] [PubMed] [Google Scholar]
- 253. Mitchison J. (1971) The Biology of the Cell Cycle. Cambridge University Press. [Google Scholar]
- 254. Keating M.T., et al. (1988) Autocrine stimulation of intracellular PDGF receptors in v-sis-transformed cells. Science, 239, 914–916. [DOI] [PubMed] [Google Scholar]
- 255. Skobe M., et al. (1998) Tumorigenic conversion of immortal human keratinocytes through stromal cell activation. Proc. Natl Acad. Sci. USA, 95, 1050–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256. Lemmon M.A. (2009) Ligand-induced ErbB receptor dimerization. Exp. Cell Res., 315, 638–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257. Kerkhoff E., et al. (1998) Cell cycle targets of Ras/Raf signalling. Oncogene, 17, 1457–1462. [DOI] [PubMed] [Google Scholar]
- 258. Mezquita B., et al. (2014) Unlocking doors without keys: activation of Src by truncated C-terminal intracellular receptor tyrosine kinases lacking tyrosine kinase activity. Cells, 3, 92–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259. Grünfeld H.T., et al. (2004) Effect of in vitro estrogenic pesticides on human oestrogen receptor alpha and beta mRNA levels. Toxicol. Lett., 151, 467–480. [DOI] [PubMed] [Google Scholar]
- 260. Symonds D.A., et al. (2005) Methoxychlor induces proliferation of the mouse ovarian surface epithelium. Toxicol. Sci., 83, 355–362. [DOI] [PubMed] [Google Scholar]
- 261. Murono E.P., et al. (2004) The effects of the reported active metabolite of methoxychlor, 2,2-bis(p-hydroxyphenyl)-1,1,1-trichloroethane, on testosterone formation by cultured Leydig cells from young adult rats. Reprod. Toxicol., 19, 135–146. [DOI] [PubMed] [Google Scholar]
- 262. Gaido K.W., et al. (2000) Interaction of methoxychlor and related compounds with estrogen receptor alpha and beta, and androgen receptor: structure-activity studies. Mol. Pharmacol., 58, 852–858. [PubMed] [Google Scholar]
- 263. Paulose T., et al. (2011) Increased sensitivity of estrogen receptor alpha overexpressing antral follicles to methoxychlor and its metabolites. Toxicol. Sci., 120, 447–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264. Wilard S, et al. (2009) Growth factors differentially augment the effects of HPTE on estrogen response element-mediated gene transcription in a dose- and time-dependent manner among human breast cancer cell lines. Res. J. Med. Med. Sci. 4, 171–180. [Google Scholar]
- 265. Kojima H., et al. (2010) Endocrine-disrupting potential of pesticides via nuclear receptors and aryl hydrocarbon receptor. J. Health Sci., 56, 374–386. [Google Scholar]
- 266. Noriega N.C., et al. (2005) Late gestational exposure to the fungicide prochloraz delays the onset of parturition and causes reproductive malformations in male but not female rat offspring. Biol. Reprod., 72, 1324–1335. [DOI] [PubMed] [Google Scholar]
- 267. Cocco P. (2002) On the rumors about the silent spring. Review of the scientific evidence linking occupational and environmental pesticide exposure to endocrine disruption health effects. Cad. Saude. Publica., 18, 379–402. [DOI] [PubMed] [Google Scholar]
- 268. Kleinstreuer N.C., et al. (2011) Identifying developmental toxicity pathways for a subset of ToxCast chemicals using human embryonic stem cells and metabolomics. Toxicol. Appl. Pharmacol., 257, 111–121. [DOI] [PubMed] [Google Scholar]
- 269. Cummings A.M., et al. (1989) Antifertility effect of methoxychlor in female rats: dose- and time-dependent blockade of pregnancy. Toxicol. Appl. Pharmacol., 97, 454–462. [DOI] [PubMed] [Google Scholar]
- 270. Gray L.E., Jr, et al. (1989) A dose-response analysis of methoxychlor-induced alterations of reproductive development and function in the rat. Fundam. Appl. Toxicol., 12, 92–108. [DOI] [PubMed] [Google Scholar]
- 271. Metcalf J.L., et al. (1996) Methoxychlor mimics the action of 17 beta-estradiol on induction of uterine epidermal growth factor receptors in immature female rats. Reprod. Toxicol., 10, 393–399. [DOI] [PubMed] [Google Scholar]
- 272. Kuiper G.G., et al. (1998) Interaction of estrogenic chemicals and phytoestrogens with estrogen receptor beta. Endocrinology, 139, 4252–4263. [DOI] [PubMed] [Google Scholar]
- 273. Andersen H.R., et al. (2002) Effects of currently used pesticides in assays for estrogenicity, androgenicity, and aromatase activity in vitro . Toxicol. Appl. Pharmacol., 179, 1–12. [DOI] [PubMed] [Google Scholar]
- 274. Vinggaard A.M., et al. (2006) Prochloraz: an imidazole fungicide with multiple mechanisms of action. Int. J. Androl., 29, 186–192. [DOI] [PubMed] [Google Scholar]
- 275. Liu C., et al. (2011) Effects of prochloraz or propylthiouracil on the cross-talk between the HPG, HPA, and HPT axes in zebrafish. Environ. Sci. Technol., 45, 769–775. [DOI] [PubMed] [Google Scholar]
- 276. Zhang W., et al. (2013) Known and emerging factors modulating estrogenic effects of estrogen-disrupting chemicals. Environ. Rev., 21, 1–12. [Google Scholar]
- 277. Medjakovic S., et al. (2014) Effect of nonpersistent pesticides on estrogen receptor, androgen receptor, and aryl hydrocarbon receptor. Environ. Toxicol., 29, 1201–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278. Jenkins S., et al. (2009) Oral exposure to bisphenol a increases dimethylbenzanthracene-induced mammary cancer in rats. Environ. Health Perspect., 117, 910–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279. Goodson W.H., III, et al. (2011) Activation of the mTOR pathway by low levels of xenoestrogens in breast epithelial cells from high-risk women. Carcinogenesis, 32, 1724–1733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280. Meironyté D., et al. (1999) Analysis of polybrominated diphenyl ethers in Swedish human milk. A time-related trend study, 1972–1997. J. Toxicol. Environ. Health A, 58, 329–341. [DOI] [PubMed] [Google Scholar]
- 281. Brown D.J., et al. (2004) Analysis of Ah receptor pathway activation by brominated flame retardants. Chemosphere, 55, 1509–1518. [DOI] [PubMed] [Google Scholar]
- 282. Hsieh T.H., et al. (2012) Phthalates induce proliferation and invasiveness of estrogen receptor-negative breast cancer through the AhR/HDAC6/c-Myc signaling pathway. FASEB J., 26, 778–787. [DOI] [PubMed] [Google Scholar]
- 283. Janjua N.R., et al. (2007) Systemic uptake of diethyl phthalate, dibutyl phthalate, and butyl paraben following whole-body topical application and reproductive and thyroid hormone levels in humans. Environ. Sci. Technol., 41, 5564–5570. [DOI] [PubMed] [Google Scholar]
- 284. Liu W.L., et al. (2010) [Distribution characteristics of phthalic acid esters in soils and plants at e-waste recycling sites in Taizhou of Zhejiang, China]. Ying Yong Sheng Tai Xue Bao, 21, 489–494. [PubMed] [Google Scholar]
- 285. Wormuth M., et al. (2006) What are the sources of exposure to eight frequently used phthalic acid esters in Europeans? Risk Anal., 26, 803–824. [DOI] [PubMed] [Google Scholar]
- 286. Galbraith H. (2002) Hormones in international meat production: biological, sociological and consumer issues. Nutr. Res. Rev., 15, 293–314. [DOI] [PubMed] [Google Scholar]
- 287. Boettcher M., et al. (2011) Low-dose effects and biphasic effect profiles: is trenbolone a genotoxicant? Mutat. Res., 723, 152–157. [DOI] [PubMed] [Google Scholar]
- 288. Kongsuwan K., et al. (2012) The effect of combination treatment with trenbolone acetate and estradiol-17β on skeletal muscle expression and plasma concentrations of oxytocin in sheep. Domest. Anim. Endocrinol., 43, 67–73. [DOI] [PubMed] [Google Scholar]
- 289. Hotchkiss A.K., et al. (2007) An environmental androgen, 17beta-trenbolone, affects delayed-type hypersensitivity and reproductive tissues in male mice. J. Toxicol. Environ. Health A, 70, 138–140. [DOI] [PubMed] [Google Scholar]
- 290. Zhao J.X., et al. (2011) Trenbolone enhances myogenic differentiation by enhancing β-catenin signaling in muscle-derived stem cells of cattle. Domest. Anim. Endocrinol., 40, 222–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291. Ansari K.M., et al. (2010) Skin tumor promotion by argemone oil/alkaloid in mice: evidence for enhanced cell proliferation, ornithine decarboxylase, cyclooxygenase-2 and activation of MAPK/NF-kappaB pathway. Food Chem. Toxicol., 48, 132–138. [DOI] [PubMed] [Google Scholar]
- 292. Mishra V., et al. (2012) Role of ErbB2 mediated AKT and MAPK pathway in gall bladder cell proliferation induced by argemone oil and butter yellow. Argemone oil and butter yellow induced gall bladder cell proliferation. Cell Biol. Toxicol., 28, 149–159. [DOI] [PubMed] [Google Scholar]
- 293. Parker M. (1991) Nuclear Hormone Receptors: Molecular Mechanisms, Cellular Functions, Clinical Abnormalities. Academic Press, London. [Google Scholar]
- 294. Gulliver L.S.M. (2013) Estradiol synthesis and metabolism and risk of ovarian cancer in older women taking prescribed or plant-derived estrogen supplementation. J. Steroids Horm. Sci., S12:003. [Google Scholar]
- 295. Leroy B., et al. (2014) TP53 mutations in human cancer: database reassessment and prospects for the next decade. Hum. Mutat., 35, 672–688. [DOI] [PubMed] [Google Scholar]
- 296. De Blasio A., et al. (2005) Differentiative pathway activated by 3-aminobenzamide, an inhibitor of PARP, in human osteosarcoma MG-63 cells. FEBS Lett., 579, 615–620. [DOI] [PubMed] [Google Scholar]
- 297. Nielsen G.P., et al. (1998) CDKN2A gene deletions and loss of p16 expression occur in osteosarcomas that lack RB alterations. Am. J. Pathol., 153, 159–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298. Pietruszewska W., et al. (2008) Loss of heterozygosity for Rb locus and pRb immunostaining in laryngeal cancer: a clinicopathologic, molecular and immunohistochemical study. Folia Histochem. Cytobiol., 46, 479–485. [DOI] [PubMed] [Google Scholar]
- 299. Myong N.H. (2008) Cyclin D1 overexpression, p16 loss, and pRb inactivation play a key role in pulmonary carcinogenesis and have a prognostic implication for the long-term survival in non-small cell lung carcinoma patients. Cancer Res. Treat., 40, 45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300. Ikushima H., et al. (2010) TGFbeta signalling: a complex web in cancer progression. Nat. Rev. Cancer, 10, 415–424. [DOI] [PubMed] [Google Scholar]
- 301. Su V., et al. (2014) Connexins: mechanisms regulating protein levels and intercellular communication. FEBS Lett., 588, 1212–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302. Li M.W., et al. (2010) Connexin 43 is critical to maintain the homeostasis of the blood-testis barrier via its effects on tight junction reassembly. Proc. Natl Acad. Sci. USA, 107, 17998–18003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303. Campos-Pereira F.D., et al. (2012) Early cytotoxic and genotoxic effects of atrazine on Wistar rat liver: a morphological, immunohistochemical, biochemical, and molecular study. Ecotoxicol. Environ. Saf., 78, 170–177. [DOI] [PubMed] [Google Scholar]
- 304. Stenner-Liewen F., et al. (2003) Apoptosis and cancer: basic mechanisms and therapeutic opportunities in the postgenomic era. Cancer Res., 63, 263–268. [Google Scholar]
- 305. Thompson C.B. (1995) Apoptosis in the pathogenesis and treatment of disease. Science, 267, 1456–1462. [DOI] [PubMed] [Google Scholar]
- 306. Shortt J., et al. (2012) Oncogenes in cell survival and cell death. Cold Spring Harb. Perspect. Biol., 4, a009829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307. Alberts B., et al. (2002) Extracellular control of cell division, cell growth, and apoptosis. In Molecular Biology of the Cell. Garland Science, New York, NY. [Google Scholar]
- 308. Roos W.P., et al. (2006) DNA damage-induced cell death by apoptosis. Trends Mol. Med., 12, 440–450. [DOI] [PubMed] [Google Scholar]
- 309. Fridman J.S., et al. (2003) Control of apoptosis by p53. Oncogene, 22, 9030–9040. [DOI] [PubMed] [Google Scholar]
- 310. Adams J.M. (2003) Ways of dying: multiple pathways to apoptosis. Genes Dev., 17, 2481–2495. [DOI] [PubMed] [Google Scholar]
- 311. Deveraux Q.L., et al. (1999) IAP family proteins–suppressors of apoptosis. Genes Dev., 13, 239–252. [DOI] [PubMed] [Google Scholar]
- 312. Yang Y.L., et al. (2000) The IAP family: endogenous caspase inhibitors with multiple biological activities. Cell Res., 10, 169–177. [DOI] [PubMed] [Google Scholar]
- 313. Wu W., et al. (2013) Metabolic changes in cancer: beyond the Warburg effect. Acta Biochim. Biophys. Sin. (Shanghai), 45, 18–26. [DOI] [PubMed] [Google Scholar]
- 314. Gonzalez M.J., et al. (2012) The bio-energetic theory of carcinogenesis. Med. Hypotheses, 79, 433–439. [DOI] [PubMed] [Google Scholar]
- 315. Ferreira L.M., et al. (2012) Metabolic reprogramming of the tumor. Oncogene, 31, 3999–4011. [DOI] [PubMed] [Google Scholar]
- 316. Yi C.H., et al. (2011) Metabolic regulation of protein N-alpha-acetylation by Bcl-xL promotes cell survival. Cell, 146, 607–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317. Wu G.S. (2009) TRAIL as a target in anti-cancer therapy. Cancer Lett., 285, 1–5. [DOI] [PubMed] [Google Scholar]
- 318. Klaunig J.E., et al. (1990) Gap-junctional intercellular communication and murine hepatic carcinogenesis. Prog. Clin. Biol. Res., 331, 277–291. [PubMed] [Google Scholar]
- 319. Carette D., et al. (2014) Connexin a check-point component of cell apoptosis in normal and physiopathological conditions. Biochimie, 101, 1–9. [DOI] [PubMed] [Google Scholar]
- 320. Leung-Toung R., et al. (2006) Thiol proteases: inhibitors and potential therapeutic targets. Curr. Med. Chem., 13, 547–581. [DOI] [PubMed] [Google Scholar]
- 321. Kim I.Y., et al. (2004) Phthalates inhibit tamoxifen-induced apoptosis in MCF-7 human breast cancer cells. J. Toxicol. Environ. Health A, 67, 2025–2035. [DOI] [PubMed] [Google Scholar]
- 322. Corcelle E., et al. (2006) Disruption of autophagy at the maturation step by the carcinogen lindane is associated with the sustained mitogen-activated protein kinase/extracellular signal-regulated kinase activity. Cancer Res., 66, 6861–6870. [DOI] [PubMed] [Google Scholar]
- 323. Kim J.Y., et al. (2014) Methoxychlor and triclosan stimulates ovarian cancer growth by regulating cell cycle- and apoptosis-related genes via an estrogen receptor-dependent pathway. Environ. Toxicol. Pharmacol., 37, 1264–1274. [DOI] [PubMed] [Google Scholar]
- 324. Carnero A. (2013) Markers of cellular senescence. Methods Mol. Biol., 965, 63–81. [DOI] [PubMed] [Google Scholar]
- 325. Serrano M., et al. (2001) Putting the stress on senescence. Curr. Opin. Cell Biol., 13, 748–753. [DOI] [PubMed] [Google Scholar]
- 326. Shay J.W., et al. (2004) Hallmarks of senescence in carcinogenesis and cancer therapy. Oncogene, 23, 2919–2933. [DOI] [PubMed] [Google Scholar]
- 327. Ohtani N., et al. (2004) The p16INK4a-RB pathway: molecular link between cellular senescence and tumor suppression. J. Med. Invest., 51, 146–153. [DOI] [PubMed] [Google Scholar]
- 328. Sherr C.J., et al. (2002) The RB and p53 pathways in cancer. Cancer Cell, 2, 103–112. [DOI] [PubMed] [Google Scholar]
- 329. Vergel M., et al. (2010) Bypassing cellular senescence by genetic screening tools. Clin. Transl. Oncol., 12, 410–417. [DOI] [PubMed] [Google Scholar]
- 330. Zanella F., et al. (2010) Understanding FOXO, new views on old transcription factors. Curr. Cancer Drug Targets, 10, 135–146. [DOI] [PubMed] [Google Scholar]
- 331. Ruiz L., et al. (2008) Characterization of the p53 response to oncogene-induced senescence. PLoS One, 3, e3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332. Newbold R.F., et al. (1982) Induction of immortality is an early event in malignant transformation of mammalian cells by carcinogens. Nature, 299, 633–635. [DOI] [PubMed] [Google Scholar]
- 333. Russo I., et al. (1998) A telomere-independent senescence mechanism is the sole barrier to Syrian hamster cell immortalization. Oncogene, 17, 3417–3426. [DOI] [PubMed] [Google Scholar]
- 334. Newbold R.F., et al. (1980) Mutagenicity of carcinogenic methylating agents is associated with a specific DNA modification. Nature, 283, 596–599. [DOI] [PubMed] [Google Scholar]
- 335. Lehman T.A., et al. (1993) p53 mutations in human immortalized epithelial cell lines. Carcinogenesis, 14, 833–839. [DOI] [PubMed] [Google Scholar]
- 336. Lafarge-Frayssinet C., et al. (1989) Over expression of proto-oncogenes: ki-ras, fos and myc in rat liver cells treated in vitro by two liver tumor promoters: phenobarbital and biliverdin. Cancer Lett., 44, 191–198. [DOI] [PubMed] [Google Scholar]
- 337. Arita A., et al. (2009) Epigenetics in metal carcinogenesis: nickel, arsenic, chromium and cadmium. Metallomics, 1, 222–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338. Trott D.A., et al. (1995) Mechanisms involved in the immortalization of mammalian cells by ionizing radiation and chemical carcinogens. Carcinogenesis, 16, 193–204. [DOI] [PubMed] [Google Scholar]
- 339. Rivedal E., et al. (2000) Morphological transformation and effect on gap junction intercellular communication in Syrian hamster embryo cells as screening tests for carcinogens devoid of mutagenic activity. Toxicol. In Vitro, 14, 185–192. [DOI] [PubMed] [Google Scholar]
- 340. Zhou X., et al. (2009) Effects of nickel, chromate, and arsenite on histone 3 lysine methylation. Toxicol. Appl. Pharmacol., 236, 78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341. Creton S., et al. (2010) Acute toxicity testing of chemicals-Opportunities to avoid redundant testing and use alternative approaches. Crit. Rev. Toxicol., 40, 50–83. [DOI] [PubMed] [Google Scholar]
- 342. Dickens F., et al. (1933) The metabolism of normal and tumour tissue: The effects of lactate, pyruvate and deprivation of substrate. Biochem. J., 27, 1134–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343. MEDES G., et al. (1953) Metabolism of neoplastic tissue. IV. A study of lipid synthesis in neoplastic tissue slices in vitro . Cancer Res., 13, 27–29. [PubMed] [Google Scholar]
- 344. Menendez J.A., et al. (2007) Fatty acid synthase and the lipogenic phenotype in cancer pathogenesis. Nat. Rev. Cancer, 7, 763–777. [DOI] [PubMed] [Google Scholar]
- 345. Deberardinis R.J., et al. (2008) Brick by brick: metabolism and tumor cell growth. Curr. Opin. Genet. Dev., 18, 54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346. Vander Heiden M.G., et al. (2011) Metabolic pathway alterations that support cell proliferation. Cold Spring Harb. Symp. Quant. Biol., 76, 325–334. [DOI] [PubMed] [Google Scholar]
- 347. Currie E., et al. (2013) Cellular fatty acid metabolism and cancer. Cell Metab., 18, 153–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348. Kamphorst J.J., et al. (2013) Hypoxic and Ras-transformed cells support growth by scavenging unsaturated fatty acids from lysophospholipids. Proc. Natl Acad. Sci. USA, 110, 8882–8887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349. Lazebnik Y. (2010) What are the hallmarks of cancer? Nat. Rev. Cancer, 10, 232–233. [DOI] [PubMed] [Google Scholar]
- 350. Berridge M.V., et al. (2010) Metabolic flexibility and cell hierarchy in metastatic cancer. Mitochondrion, 10, 584–588. [DOI] [PubMed] [Google Scholar]
- 351. Floor S.L., et al. (2012) Hallmarks of cancer: of all cancer cells, all the time? Trends Mol. Med., 18, 509–515. [DOI] [PubMed] [Google Scholar]
- 352. Newsholme E.A., et al. (1973) Regulation in Metabolism. Wiley, London, New York. [Google Scholar]
- 353. Shim H., et al. (1997) c-Myc transactivation of LDH-A: implications for tumor metabolism and growth. Proc. Natl Acad. Sci. USA, 94, 6658–6663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354. Fantin V.R., et al. (2006) Attenuation of LDH-A expression uncovers a link between glycolysis, mitochondrial physiology, and tumor maintenance. Cancer Cell, 9, 425–434. [DOI] [PubMed] [Google Scholar]
- 355. Stanton R.C. (2012) Glucose-6-phosphate dehydrogenase, NADPH, and cell survival. IUBMB Life, 64, 362–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356. Raimundo N., et al. (2011) Revisiting the TCA cycle: signaling to tumor formation. Trends Mol. Med., 17, 641–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357. Mullen A.R., et al. (2012) Genetically-defined metabolic reprogramming in cancer. Trends Endocrinol. Metab., 23, 552–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358. Wallace D.C. (2005) A mitochondrial paradigm of metabolic and degenerative diseases, aging, and cancer: a dawn for evolutionary medicine. Annu. Rev. Genet., 39, 359–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359. Santidrian A.F., et al. (2013) Mitochondrial complex I activity and NAD+/NADH balance regulate breast cancer progression. J. Clin. Invest., 123, 1068–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360. Lapuente-Brun E., et al. (2013) Supercomplex assembly determines electron flux in the mitochondrial electron transport chain. Science, 340, 1567–1570. [DOI] [PubMed] [Google Scholar]
- 361. Zaidi N., et al. (2013) Lipogenesis and lipolysis: the pathways exploited by the cancer cells to acquire fatty acids. Prog. Lipid Res, 52, 585–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362. Weidberg H., et al. (2009) Lipophagy: selective catabolism designed for lipids. Dev. Cell, 16, 628–630. [DOI] [PubMed] [Google Scholar]
- 363. Liu K., et al. (2013) Regulation of lipid stores and metabolism by lipophagy. Cell Death Differ., 20, 3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364. Newsholme E.A., et al. (1991) Application of metabolic-control logic to fuel utilization and its significance in tumor cells. Adv. Enzyme Regul., 31, 225–246. [DOI] [PubMed] [Google Scholar]
- 365. Kalhan S.C., et al. (2012) Resurgence of serine: an often neglected but indispensable amino Acid. J. Biol. Chem., 287, 19786–19791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366. Locasale J.W. (2013) Serine, glycine and one-carbon units: cancer metabolism in full circle. Nat. Rev. Cancer, 13, 572–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367. Cho H.M., et al. (2000) Nucleotide sequence and differential expression of the human 3-phosphoglycerate dehydrogenase gene. Gene, 245, 193–201. [DOI] [PubMed] [Google Scholar]
- 368. Owen O.E., et al. (2002) The key role of anaplerosis and cataplerosis for citric acid cycle function. J. Biol. Chem., 277, 30409–30412. [DOI] [PubMed] [Google Scholar]
- 369. Meyerhof O. (1951) Mechanisms of glycolysis and fermentation. Can. J. Med. Sci., 29, 63–77. [DOI] [PubMed] [Google Scholar]
- 370. Lowry O.H., et al. (1964) The relationships between substrates and enzymes of glycolysis in brain. J. Biol. Chem., 239, 31–42. [PubMed] [Google Scholar]
- 371. Warburg O., et al. (1958) [Partial anaerobiosis and radiation-sensitivity of cancer cells]. Arch. Biochem. Biophys., 78, 573–586. [DOI] [PubMed] [Google Scholar]
- 372. Robey R.B. (2011) On dogma and the metabolic gestalt of tumor cells, Science, E-Letters. https://www.sciencemag.org/content/330/ 6009/1338/reply (7 May 2015, date last accessed). [Google Scholar]
- 373. Copley S.D. (2003) Enzymes with extra talents: moonlighting functions and catalytic promiscuity. Curr. Opin. Chem. Biol., 7, 265–272. [DOI] [PubMed] [Google Scholar]
- 374. Luo W., et al. (2012) Emerging roles of PKM2 in cell metabolism and cancer progression. Trends Endocrinol. Metab., 23, 560–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375. Gao X., et al. (2012) Pyruvate kinase M2 regulates gene transcription by acting as a protein kinase. Mol. Cell, 45, 598–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376. Robey R.B., et al. (2006) Mitochondrial hexokinases, novel mediators of the antiapoptotic effects of growth factors and Akt. Oncogene, 25, 4683–4696. [DOI] [PubMed] [Google Scholar]
- 377. Hu J., et al. (2013) Heterogeneity of tumor-induced gene expression changes in the human metabolic network. Nat. Biotechnol., 31, 522–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378. Kacser H., et al. (1973) The control of flux. Symp. Soc. Exp. Biol., 27, 65–104. [PubMed] [Google Scholar]
- 379. Agarwal A.R., et al. (2013) Metabolic shift in lung alveolar cell mitochondria following acrolein exposure. Am. J. Physiol. Lung Cell. Mol. Physiol., 305, L764–L773. [DOI] [PubMed] [Google Scholar]
- 380. Ishida S., et al. (2013) Bioavailable copper modulates oxidative phosphorylation and growth of tumors. Proc. Natl Acad. Sci. USA, 110, 19507–19512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381. George J., et al. (2011) Cypermethrin exposure leads to regulation of proteins expression involved in neoplastic transformation in mouse skin. Proteomics, 11, 4411–4421. [DOI] [PubMed] [Google Scholar]
- 382. Tsitsimpikou C., et al. (2013) Histopathological lesions, oxidative stress and genotoxic effects in liver and kidneys following long term exposure of rabbits to diazinon and propoxur. Toxicology, 307, 109–114. [DOI] [PubMed] [Google Scholar]
- 383. Abdollahi M., et al. (2004) Pesticides and oxidative stress: a review. Med. Sci. Monit., 10, RA141–RA147. [PubMed] [Google Scholar]
- 384. Folkman J. (1995) Angiogenesis in cancer, vascular, rheumatoid and other disease. Nat. Med., 1, 27–31. [DOI] [PubMed] [Google Scholar]
- 385. Carmeliet P. (2005) Angiogenesis in life, disease and medicine. Nature, 438, 932–936. [DOI] [PubMed] [Google Scholar]
- 386. Folkman J. (1971) Tumor angiogenesis: therapeutic implications. N. Engl. J. Med., 285, 1182–1186. [DOI] [PubMed] [Google Scholar]
- 387. Carmeliet P., et al. (2011) Molecular mechanisms and clinical applications of angiogenesis. Nature, 473, 298–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388. Ferrara N., et al. (2005) Angiogenesis as a therapeutic target. Nature, 438, 967–974. [DOI] [PubMed] [Google Scholar]
- 389. Folkman J. (2003) Fundamental concepts of the angiogenic process. Curr. Mol. Med., 3, 643–651. [DOI] [PubMed] [Google Scholar]
- 390. Folkman J. (2003) Angiogenesis inhibitors: a new class of drugs. Cancer Biol. Ther., 2, S127–S133. [PubMed] [Google Scholar]
- 391. Siemann D.W., et al. (2005) Differentiation and definition of vascular-targeted therapies. Clin. Cancer Res., 11(2 Pt 1), 416–420. [PubMed] [Google Scholar]
- 392. Thorpe P.E. (2004) Vascular targeting agents as cancer therapeutics. Clin. Cancer Res., 10, 415–427. [DOI] [PubMed] [Google Scholar]
- 393. Patterson D.M., et al. (2007) Vascular damaging agents. Clin. Oncol. (R. Coll. Radiol.), 19, 443–456. [DOI] [PubMed] [Google Scholar]
- 394. Hu Z., et al. (1999) Targeting tumor vasculature endothelial cells and tumor cells for immunotherapy of human melanoma in a mouse xenograft model. Proc. Natl Acad. Sci. USA, 96, 8161–8166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395. Hu Z., et al. (2000) Intratumoral injection of adenoviral vectors encoding tumor-targeted immunoconjugates for cancer immunotherapy. Proc. Natl Acad. Sci. USA, 97, 9221–9225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396. Hu Z., et al. (2001) Targeting tissue factor on tumor vascular endothelial cells and tumor cells for immunotherapy in mouse models of prostatic cancer. Proc. Natl Acad. Sci. USA, 98, 12180–12185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397. Hu Z., et al. (2010) Natural killer cells are crucial for the efficacy of Icon (factor VII/human IgG1 Fc) immunotherapy in human tongue cancer. BMC Immunol., 11, 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398. Konigsberg W.H., et al. (1988) Molecular cloning of the cDNA for human tissue factor. Cell, 52, 639–640. [DOI] [PubMed] [Google Scholar]
- 399. Contrino J., et al. (1996) In situ detection of tissue factor in vascular endothelial cells: correlation with the malignant phenotype of human breast disease. Nat. Med., 2, 209–215. [DOI] [PubMed] [Google Scholar]
- 400. Hu Z. (2011) Factor VII-Targeted Photodynamic Therapy for Breast Cancer and Its Therapeutic Potential for Other Solid Cancers and Leukemia, Breast Cancer—Current and Alternative Therapeutic Modalities. In EsraGunduz and MehmetGunduz (eds), InTech, Rijeka, Croatia. http://www.intechopen.com/articles/show/title/factor-vii-targeted-photodynamic-therapy-for-breast-cancer-and-its-therapeutic-potential-for-other-s ISBN: 978-953-307-776-5. [Google Scholar]
- 401. Hu Z., et al. (2010) Targeting tissue factor on tumour cells and angiogenic vascular endothelial cells by factor VII-targeted verteporfin photodynamic therapy for breast cancer in vitro and in vivo in mice. BMC Cancer, 10, 235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402. Duanmu J., et al. (2011) Effective treatment of chemoresistant breast cancer in vitro and in vivo by a factor VII-targeted photodynamic therapy. Br. J. Cancer, 104, 1401–1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403. Hu Z., et al. (2011) Selective and effective killing of angiogenic vascular endothelial cells and cancer cells by targeting tissue factor using a factor VII-targeted photodynamic therapy for breast cancer. Breast Cancer Res. Treat., 126, 589–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404. Jessen-Eller K.K.J., et al. (2002) A new invertebrate member of the p53 gene family is developmentally expressed and responds to polychlorinated biphenyls. Environ. Health Perspect., 110, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405. Taylor T.R., et al. (2011) Ziram activates mitogen-activated protein kinases and decreases cytolytic protein levels in human natural killer cells. Toxicol. Mech. Methods, 21, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406. Berx G., et al. (2009) Involvement of members of the cadherin superfamily in cancer. Cold Spring Harb. Perspect. Biol., 1, a003129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407. Klymkowsky M.W., et al. (2009) Epithelial-mesenchymal transition: a cancer researcher's conceptual friend and foe. Am. J. Pathol., 174, 1588–1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408. Micalizzi D.S., et al. (2010) Epithelial-mesenchymal transition in cancer: parallels between normal development and tumor progression. J. Mammary Gland Biol. Neoplasia, 15, 117–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409. Yang J., et al. (2008) Epithelial-mesenchymal transition: at the crossroads of development and tumor metastasis. Dev. Cell, 14, 818–829. [DOI] [PubMed] [Google Scholar]
- 410. Kawata M., et al. (2012) TGF-β-induced epithelial-mesenchymal transition of A549 lung adenocarcinoma cells is enhanced by pro-inflammatory cytokines derived from RAW 264.7 macrophage cells. J. Biochem., 151, 205–216. [DOI] [PubMed] [Google Scholar]
- 411. Nagase H., et al. (2006) Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc. Res., 69, 562–573. [DOI] [PubMed] [Google Scholar]
- 412. Chen H.C., et al. (1998) Tyrosine phosphorylation of focal adhesion kinase stimulated by hepatocyte growth factor leads to mitogen-activated protein kinase activation. J. Biol. Chem., 273, 25777–25782. [DOI] [PubMed] [Google Scholar]
- 413. Al-Mehdi A.B., et al. (2000) Intravascular origin of metastasis from the proliferation of endothelium-attached tumor cells: a new model for metastasis. Nat. Med., 6, 100–102. [DOI] [PubMed] [Google Scholar]
- 414. Chang C.C., et al. (2013) Connective tissue growth factor activates pluripotency genes and mesenchymal-epithelial transition in head and neck cancer cells. Cancer Res., 73, 4147–4157. [DOI] [PubMed] [Google Scholar]
- 415. McCormick J.M., et al. (2010) Embryonic exposure to tetrabromobisphenol A and its metabolites, bisphenol A and tetrabromobisphenol A dimethyl ether disrupts normal zebrafish (Danio rerio) development and matrix metalloproteinase expression. Aquat. Toxicol., 100, 255–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416. Ding S.Z., et al. (2013) Epithelial-mesenchymal transition during oncogenic transformation induced by hexavalent chromium involves reactive oxygen species-dependent mechanism in lung epithelial cells. Toxicol. Appl. Pharmacol., 269, 61–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417. Hsiang C.Y., et al. (2007) Acetaldehyde induces matrix metalloproteinase-9 gene expression via nuclear factor-kappaB and activator protein 1 signaling pathways in human hepatocellular carcinoma cells: association with the invasive potential. Toxicol. Lett., 171, 78–86. [DOI] [PubMed] [Google Scholar]
- 418. Seo J.H., et al. (2004) Helicobacter pylori in a Korean isolate activates mitogen-activated protein kinases, AP-1, and NF-kappaB and induces chemokine expression in gastric epithelial AGS cells. Lab. Invest., 84, 49–62. [DOI] [PubMed] [Google Scholar]
- 419. Olumi A.F., et al. (1999) Carcinoma-associated fibroblasts direct tumor progression of initiated human prostatic epithelium. Cancer Res., 59, 5002–5011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420. Le Bitoux M.A., et al. (2008) Tumor-host interactions: the role of inflammation. Histochem. Cell Biol., 130, 1079–1090. [DOI] [PubMed] [Google Scholar]
- 421. Maffini M.V., et al. (2005) Stromal regulation of neoplastic development: age-dependent normalization of neoplastic mammary cells by mammary stroma. Am. J. Pathol., 167, 1405–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422. Weaver V.M., et al. (2004) Watch thy neighbor: cancer is a communal affair. J. Cell Sci., 117, 1287–1290. [DOI] [PubMed] [Google Scholar]
- 423. Maguer-Satta V. (2011) The stem cell niche: the black master of cancer. Cancer Stem Cells Theories and Practices, ISBN 978-953-307-225-8. [Google Scholar]
- 424. Laconi S., et al. (2001) A growth-constrained environment drives tumor progression invivo. Proc. Natl Acad. Sci. USA, 98, 7806–7811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425. Ding J., et al. (2009) TNF-alpha induction by nickel compounds is specific through ERKs/AP-1-dependent pathway in human bronchial epithelial cells. Curr. Cancer Drug Targets, 9, 81–90. [DOI] [PubMed] [Google Scholar]
- 426. Li J., et al. (2004) Nickel compounds act through phosphatidylinositol-3-kinase/Akt-dependent, p70(S6k)-independent pathway to induce hypoxia inducible factor transactivation and Cap43 expression in mouse epidermal Cl41 cells. Cancer Res., 64, 94–101. [DOI] [PubMed] [Google Scholar]
- 427. Ding J., et al. (2006) Nickel compounds render anti-apoptotic effect to human bronchial epithelial Beas-2B cells by induction of cyclooxygenase-2 through an IKKbeta/p65-dependent and IKKalpha- and p50-independent pathway. J. Biol. Chem., 281, 39022–39032. [DOI] [PubMed] [Google Scholar]
- 428. Zhang J., et al. (2013) The alteration of miR-222 and its target genes in nickel-induced tumor. Biol. Trace Elem. Res., 152, 267–274. [DOI] [PubMed] [Google Scholar]
- 429. Allard P., et al. (2010) Bisphenol A impairs the double-strand break repair machinery in the germline and causes chromosome abnormalities. Proc. Natl Acad. Sci. USA, 107, 20405–20410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430. Hassan Z.K., et al. (2012) Bisphenol A induces hepatotoxicity through oxidative stress in rat model. Oxid. Med. Cell. Longev., 2012, 194829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 431. Takahashi A., et al. (2004) Bisphenol A from dental polycarbonate crown upregulates the expression of hTERT. J. Biomed. Mater. Res. B. Appl. Biomater., 71, 214–221. [DOI] [PubMed] [Google Scholar]
- 432. Hurt K., et al. (2013) Tributyltin and dibutyltin alter secretion of tumor necrosis factor alpha from human natural killer cells and a mixture of T cells and natural killer cells. J. Appl. Toxicol., 33, 503–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433. Patel E., et al. (2013) Methylmercury impairs motor function in early development and induces oxidative stress in cerebellar granule cells. Toxicol. Lett., 222, 265–272. [DOI] [PubMed] [Google Scholar]
- 434. Sherwani S.I., et al. (2013) Eicosanoid signaling and vascular dysfunction: methylmercury-induced phospholipase D activation in vascular endothelial cells. Cell Biochem. Biophys., 67, 317–329. [DOI] [PubMed] [Google Scholar]
- 435. Black A.T., et al. (2008) Increased oxidative stress and antioxidant expression in mouse keratinocytes following exposure to paraquat. Toxicol. Appl. Pharmacol., 231, 384–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436. Chang X., et al. (2013) Paraquat inhibits cell viability via enhanced oxidative stress and apoptosis in human neural progenitor cells. Chem. Biol. Interact., 206, 248–255. [DOI] [PubMed] [Google Scholar]
- 437. Khatami M. (2014) Chronic inflammation: synergistic interactions of recruiting macrophages (TAMs) and eosinophils (Eos) with host mast cells (MCs) and tumorigenesis in CALTs. M-CSF, suitable biomarker for cancer diagnosis! Cancers (Basel), 6, 297–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438. Whiteside T.L. (2006) Immune suppression in cancer: effects on immune cells, mechanisms and future therapeutic intervention. Semin Cancer Biol., 16, 3–15. [DOI] [PubMed] [Google Scholar]
- 439. Whiteside T.L. (2002) Tumor-induced death of immune cells: its mechanisms and consequences. Semin Cancer Biol., 12, 43–50. [DOI] [PubMed] [Google Scholar]
- 440. Yang L., et al. (2010) TGF-β and immune cells: an important regulatory axis in the tumor microenvironment and progression. Trends Immunol., 31, 220–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 441. Mocellin S., et al. (2004) The multifaceted relationship between IL-10 and adaptive immunity: putting together the pieces of a puzzle. Cytokine Growth Factor Rev., 15, 61–76. [DOI] [PubMed] [Google Scholar]
- 442. Zou W. (2005) Immunosuppressive networks in the tumour environment and their therapeutic relevance. Nat. Rev. Cancer, 5, 263–274. [DOI] [PubMed] [Google Scholar]
- 443. IARC (2013) IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Agents classified by the IARC Monographs. International Agency for Research and Cancer, Lyon. [Google Scholar]
- 444. IARC (1982) Monograph on the Evaluation of Carcinogenic Risk to Humans. Some Industrial Chemicals and Dyestuffs. Di(2-ethylhexyl) Phthalate. International Agency for Research and Cancer, Lyon, pp. 257–280. [Google Scholar]
- 445. IARC (2000) Monograph on the Evaluation of Carcinogenic Risk to Humans. Some Industrial Chemicals. Di(2-ethylhexyl) Phthalate. International Agency for Research and Cancer, Lyon, pp. 41–148. [Google Scholar]
- 446. Odermatt A., et al. (2008) Disruption of glucocorticoid and mineralocorticoid receptor-mediated responses by environmental chemicals. CHIMIA Int. J. Chem., 62, 335–339. [Google Scholar]
- 447. Santos P.M., et al. (2009) Insights into yeast adaptive response to the agricultural fungicide mancozeb: a toxicoproteomics approach. Proteomics, 9, 657–670. [DOI] [PubMed] [Google Scholar]
- 448. Kuster M., et al. (2009) Liquid chromatography–tandem mass spectrometric analysis and regulatory issues of polar pesticides in natural and treated waters. J. Chromatogr. A, 1216, 520–529. [DOI] [PubMed] [Google Scholar]
- 449. Kim J.H., et al. (2013) Synergism of antifungal activity between mitochondrial respiration inhibitors and kojic acid. Molecules, 18, 1564–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450. Çayır A., et al. (2014) Micronuclei, nucleoplasmic bridges, and nuclear buds induced in human lymphocytes by the fungicide signum and its active ingredients (boscalid and pyraclostrobin). Environ. Toxicol, 29, 723–732. [DOI] [PubMed] [Google Scholar]
- 451. Judson R.S., et al. (2010) In vitro screening of environmental chemicals for targeted testing prioritization: the ToxCast project. Environ. Health Persp. (Online), 118, 485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 452. Pereboeva L., et al. (2013) DNA damage responses and oxidative stress in dyskeratosis congenita. PLoS One, 8, e76473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453. Pinchuk L.M., et al. (2007) In vitro atrazine exposure affects the phenotypic and functional maturation of dendritic cells. Toxicol. Appl. Pharmacol., 223, 206–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454. Kavlock R., et al. (2012) Update on EPA’s ToxCast program: providing high throughput decision support tools for chemical risk management. Chem. Res. Toxicol., 25, 1287–1302. [DOI] [PubMed] [Google Scholar]
- 455. Martin M.T., et al. (2011) Predictive model of rat reproductive toxicity from ToxCast high throughput screening. Biol. Reprod., 85, 327–339. [DOI] [PubMed] [Google Scholar]
- 456. Metzler M., et al. (2001) Chemistry of natural and anthropogenic endocrine active compounds. In M.Metzler (ed) The Handbook of Environmental Chemistry Vol. 3, Part L. Endocrine Disruptors–Part I. Springer, Berlin Heidelberg, pp. 63–80. [Google Scholar]
- 457. Gatidou G., et al. (2007) Simultaneous determination of the endocrine disrupting compounds nonylphenol, nonylphenol ethoxylates, triclosan and bisphenol A in wastewater and sewage sludge by gas chromatography–mass spectrometry. J. Chromatogr. A, 1138, 32–41. [DOI] [PubMed] [Google Scholar]
- 458. Foran C., et al. (2000) Developmental evaluation of a potential non-steroidal estrogen: triclosan. Mar. Environ. Res., 50, 153–156. [DOI] [PubMed] [Google Scholar]
- 459. Ishibashi H., et al. (2004) Effects of triclosan on the early life stages and reproduction of medaka Oryzias latipes and induction of hepatic vitellogenin. Aquat. Toxicol., 67, 167–179. [DOI] [PubMed] [Google Scholar]
- 460. Boyd G.R., et al. (2003) Pharmaceuticals and personal care products (PPCPs) in surface and treated waters of Louisiana, USA and Ontario, Canada. Sci. Total Environ., 311, 135–149. [DOI] [PubMed] [Google Scholar]
- 461. Kolpin D.W., et al. (2002) Pharmaceuticals, hormones, and other organic wastewater contaminants in US streams, 1999–2000: a national reconnaissance. Environ. Sci. Technol., 36, 1202–1211. [DOI] [PubMed] [Google Scholar]
- 462. Vandhana S., et al. (2013) Biochemical changes accompanying apoptotic cell death in retinoblastoma cancer cells treated with lipogenic enzyme inhibitors. Biochim. Biophys. Acta (BBA)-Molecular and Cell Biology of Lipids, 1831, 1458–1466. [DOI] [PubMed] [Google Scholar]
- 463. Zuckerbraun H.L., et al. (1998) Triclosan, cytotoxicity, mode of action, and induction of apoptosis in human gingival cells in vitro . Eur. J. Oral Sci., 106, 628–636. [DOI] [PubMed] [Google Scholar]
- 464. Terasaka H., et al. (2005) Cytotoxicity and apoptosis-inducing activity of bisphenol A and hydroquinone in HL-60 cells. Anticancer Res., 25, 2241–2247. [PubMed] [Google Scholar]
- 465. The Australian National Industrial Chemicals Notification and Assessment Scheme (2006) Diethylhexyl Phthalate (DEHP) Factsheet. CAS: 117-81-7. http://www.nicnas.gov.au/communications/publications/information-sheets/existing-chemical-info-sheets/diethylhexyl-phthalate-dehp-factsheet (7 May 2015, date last accessed). [Google Scholar]
- 466. Jobling S., et al. (1995) A variety of environmentally persistent chemicals, including some phthalate plasticizers, are weakly estrogenic. Environ. Health Persp., 103, 582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467. Hao C., et al. (2012) Perinatal exposure to diethyl-hexyl-phthalate induces obesity in mice. Front. Biosci. (Elite edition), 5, 725–733. [DOI] [PubMed] [Google Scholar]
- 468. Moushumi Priya A., et al. (2012) Induction of Apoptosis and cell cycle arrest by Bis (2-ethylhexyl) phthalate produced by Marine Bacillus pumilus MB 40. Chem. Biol. Interact., 195, 133–143. [DOI] [PubMed] [Google Scholar]
- 469. Park M.A., et al. (2012) Cell growth of BG-1 ovarian cancer cells is promoted by di-n-butyl phthalate and hexabromocyclododecane via upregulation of the cyclin D and cyclin-dependent kinase-4 genes. Mol. Med. Rep., 5, 761–766. [DOI] [PubMed] [Google Scholar]
- 470. Kinoshita Y., et al. (2003) Induction of aromatase (CYP19) expression in breast cancer cells through a nongenomic action of estrogen receptor alpha. Cancer Res., 63, 3546–3555. [PubMed] [Google Scholar]
- 471. Prins G.S. (2008) Endocrine disruptors and prostate cancer risk. Endocr. Relat. Cancer, 15, 649–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 472. Laville N., et al. (2006) Modulation of aromatase activity and mRNA by various selected pesticides in the human choriocarcinoma JEG-3 cell line. Toxicology, 228, 98–108. [DOI] [PubMed] [Google Scholar]
- 473. Bulun S.E., et al. (2007) Aromatase excess in cancers of breast, endometrium and ovary. J. Steroid Biochem. Mol. Biol., 106, 81–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474. (2012) A Review of Human Carcinogens—Pharmaceuticals IARC Monographs on the Evaluation of Caricinogenic Risk to Humans. Vol. 100, World health Organization IARC, Geneva, Switzerland. [Google Scholar]
- 475. Paul A., et al. (2014) The breast cancer susceptibility genes (BRCA) in breast and ovarian cancers. Front. Biosci. (Landmark Ed), 19, 605–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 476. Supplementary Guidance for Conducting Health Risk Assessment of Chemical Mixtures (2000) U.S. Environmental Protection Agency Report No. EPA/630/R-00/002, Washington, DC. [Google Scholar]
- 477. Dellarco V., et al. (2012) Mode of action: moving toward a more relevant and efficient assessment paradigm. J. Nutr., 142, 2192S–2198S. [DOI] [PubMed] [Google Scholar]
- 478. Meek M.E., et al. (2003) A framework for human relevance analysis of information on carcinogenic modes of action. Crit. Rev. Toxicol., 33, 591–653. [DOI] [PubMed] [Google Scholar]
- 479. Boobis A.R., et al. (2006) IPCS framework for analyzing the relevance of a cancer mode of action for humans. Crit. Rev. Toxicol., 36, 781–792. [DOI] [PubMed] [Google Scholar]
- 480. (2012) OECD Guidance Document 116 On The Conduct And Design Of Chronic Toxicity And Carcinogenicity Studies, Supporting Test Guidelines 451, 452 And 453, 2nd Edition, Series on Testing and Assessment, ENV/JM/MONO(2011)47. OECD Environment Directorate Joint Meeting of the Chemicals Committee and the Working Party on Chemicals, Pesticides and Biotechnology, Paris, France. [Google Scholar]
- 481. U.S.E.P.A. (2002) Guidance on Cumulative Risk Assessment of Pesticide Chemicals That Have a Common Mechanism of Toxicity. In Office of Pesticide Programs, Washington, D.C. 20460. [Google Scholar]
- 482. EFSA PPR Panel (EFSA Panel on Plant Protection Products and their Residues) (2013). Scientific opinion on the relevance of dissimilar mode of action and its appropriate application for cumulative risk assessment of pesticides residues in food. EFSA J., 11, 40. [Google Scholar]
- 483. Driedger A.A., et al. (1971) Demonstration of two types of DNA repair in X-irradiated Micrococcus radiodurans. Can. J. Microbiol., 17, 495–499. [DOI] [PubMed] [Google Scholar]
- 484. Mason P.A., et al. (2003) Mismatch repair activity in mammalian mitochondria. Nucleic Acids Res., 31, 1052–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 485. Heindorff K., et al. (1983) Genetic toxicology of ethylenediaminetetraacetic acid (EDTA). Mutat. Res., 115, 149–173. [DOI] [PubMed] [Google Scholar]
- 486. Cory-Slechta, D. et al. (2008) Phthalates Cumulative Risk Assessment—The Tasks Ahead. In National Research Council, N.A.o.S., Board on Environmental Science and Technology, Committee on Phthalates Health Risks. National Academy Press, Washington, DC, p. 208. [Google Scholar]
- 487. Bucala R. (1996) MIF rediscovered: cytokine, pituitary hormone, and glucocorticoid-induced regulator of the immune response. FASEB J., 10, 1607–1613. [DOI] [PubMed] [Google Scholar]
- 488. Bucala R., et al. (2007) Macrophage migration inhibitory factor: a probable link between inflammation and cancer. Immunity, 26, 281–285. [DOI] [PubMed] [Google Scholar]
- 489. Grieb G., et al. (2010) Macrophage migration inhibitory factor (MIF): a promising biomarker. Drug News Perspect., 23, 257–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 490. Landesmann B., et al. (2013) Adverse outcome pathway-based screening strategies for an animal-free safety assessment of chemicals. Altern. Lab. Anim., 41, 461–471. [DOI] [PubMed] [Google Scholar]
- 491. Malhotra J., et al. (2015) Effect of occupational exposures on lung cancer susceptibility: a study of gene-environment interaction analysis. Cancer Epidemiol. Biomarkers Prev., 24, 570–579. [DOI] [PubMed] [Google Scholar]
- 492. Singh S., et al. (2012) Epigenetic effects of environmental chemicals bisphenol a and phthalates. Int. J. Mol. Sci., 13, 10143–10153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 493. Vineis P., et al. (2010) Models of carcinogenesis: an overview. Carcinogenesis, 31, 1703–1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 494. Brash D., et al. (2009) The mysterious steps in carcinogenesis. Br. J. Cancer, 101, 379–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 495. Brash D., et al. (2009) The mysterious steps in carcinogenesis: addendum. Br. J. Cancer, 101, 1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 496. Rappaport S.M., et al. (2010) Epidemiology. Environment and disease risks. Science, 330, 460–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 497. Bisson W.H. (2012) Editorial: computational chemogenomics in drug design and discovery. Curr. Top. Med. Chem., 12, 1867–1868. [DOI] [PubMed] [Google Scholar]
- 498. Tomasetti C., et al. (2015) Cancer etiology. Variation in cancer risk among tissues can be explained by the number of stem cell divisions. Science, 347, 78–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 499. Weinberg R.A. (2014) Coming full circle-from endless complexity to simplicity and back again. Cell, 157, 267–271. [DOI] [PubMed] [Google Scholar]
- 500. Koutsogiannouli E., et al. (2013) Complexity in cancer biology: is systems biology the answer? Cancer Med., 2, 164–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 501. Alberghina L., et al. (2004) Systems biology and the molecular circuits of cancer. Chembiochem, 5, 1322–1333. [DOI] [PubMed] [Google Scholar]
- 502. Carvalho R.N., et al. (2014) Mixtures of chemical pollutants at European legislation safety concentrations: how safe are they? Toxicol. Sci., 141, 218–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 503. Porter W.P., et al. (1999) Endocrine, immune, and behavioral effects of aldicarb (carbamate), atrazine (triazine) and nitrate (fertilizer) mixtures at groundwater concentrations. Toxicol. Ind. Health, 15, 133–150. [DOI] [PubMed] [Google Scholar]
- 504. Tarone R.E., et al. (2011) Combating environmental causes of cancer. N. Engl. J. Med., 364, 2266–2267. [DOI] [PubMed] [Google Scholar]
- 505. Willett W.C., et al. (2011) Combating environmental causes of cancer. N. Engl. J. Med., 364, 2266. [DOI] [PubMed] [Google Scholar]
- 506. Richter E.D., et al. (2004) The precautionary principle, epidemiology and the ethics of delay. Int. J. Occup. Med. Environ. Health, 17, 9–16. [PubMed] [Google Scholar]
- 507. Pohl H.R., et al. (2010) Chemical risk assessment and uncertainty associated with extrapolation across exposure duration. Regul. Toxicol. Pharmacol., 57, 18–23. [DOI] [PubMed] [Google Scholar]
- 508. Tice R.R., et al. (2013) Improving the human hazard characterization of chemicals: a Tox21 update. Environ. Health Perspect., 121, 756–765. [DOI] [PMC free article] [PubMed] [Google Scholar]