Introduction
The main objective in managing priapism, a recurrent disorder of prolonged, undesired penile erection, has traditionally centered on achieving its prompt clinical resolution, i.e., return to normal penile flaccidity. Pharmacologic and surgical approaches such as intracavernosal sympathomimetics and penile aspiration or shunt procedures, respectively, have been implemented specifically for this purpose.1–4 This management focus is reasonable not only to remedy the conspicuous and often painful prolonged penile erection but also to preserve sexual function maximally in lieu of expected erectile tissue damage resulting from untreated priapism. However, the measure of therapeutic success that is based solely on resolving the abnormal erection event underestimates the scope and magnitude of the problem perceived by the patient. The variety of complications associated with priapism includes physical effects such as erectile dysfunction (ED) and penile deformity and mental health effects such as feelings of despair, anxiety, embarrassment, and isolation.5–7
Given the considerable health adversity of priapism, it is timely to invoke a more comprehensive approach toward both monitoring the well-being of patients with this disorder and gauging the success of its clinical management. The field of sexual medicine features the study of the subjective social, emotional and general physical ill-health effects of sexual dysfunctions, and rigor in this effort has been met by developing and applying dysfunction-specific psychometric scales and instruments.8–12 Similarly, the availability of a patient reported outcome measure for priapism offers to advance the science and healthcare of this dysfunction. We conceptualized an instrument that would incorporate elements such as those found in a general health-related quality of life measure or a treatment satisfaction scale although the content would refer specifically to the personal experience of priapism and the consequences of its control or lack thereof. Briefly, as a conceptual framework for an introductory questionnaire applied to this patient population, we proposed relevant areas of interest to be general health perception, assessment of erectile function ability, and rating of physical functioning. Herein, we report our development and initial validation of an instrument offered to serve this purpose, termed the Priapism Impact Profile (PIP).
Material and Methods
Item Generation
Preliminary development of the PIP involved a review of the medical literature related to this subject matter whereby information on symptomatic descriptions of priapism presentations was collected. Additionally, patients were interviewed using open-ended cognitive questions (individually, n= 15, and as part of two focus groups, n= 12) for further qualitative ascertainment of subjective descriptors. Plausible items were reviewed by external experts (i.e., clinicians specializing in the care of patients with sickle cell disease-related genitourinary complications) both from treatment centers in the United States and Jamaica and modified based on their feedback.
Patient Questionnaire Composition
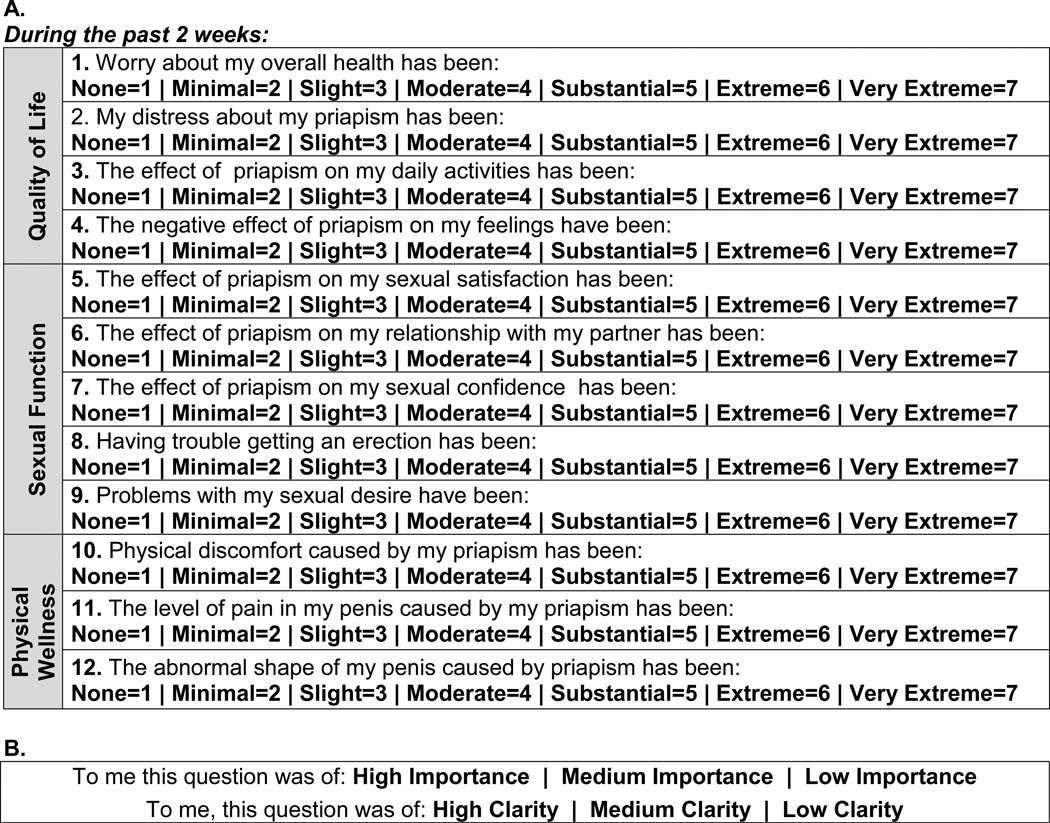
Construct items were generated and then reduced (from approximately 20–25 items) based qualitatively on our clinical and research judgment to a set of 12 items, comprising a Priapism Impact Profile (PIP) (Fig. 1A). This instrument was structured to encompass 3 intrinsic subscales or domains presumed to be affected adversely by priapism: quality-of-life (QoL), sexual function (SF), and physical wellness (PW). Each item was structured as a subjective statement such as, “My distress about my priapism has been:”, followed by a 7-point scale ranging from 1 (absent) to 7 (very extreme). We elected to use a 2-week interval empirically as a duration that was useful for patient recall and has worked well in prior assessments.13 The instrument was designed with expectations that a respondent would be able to complete the questionnaire in approximately 15 minutes. Items were prepared in accordance with guidelines for preparing forms that ensure patient readability and interpretability, as recommended by the Johns Hopkins Medicine Office of Human Subjects Research.
Figure 1.
A. Priapism Impact Profile (PIP) questionnaire. B. Descriptive rating of questionnaire items for importance and clarity.
Questionnaire Administration
This voluntary, uncompensated research study was proposed and approved by the institutional review board of the Johns Hopkins Medical Institutions. Adult patients (≥ 18 years of age) presenting to the urology and hematology clinics at the Johns Hopkins Hospital from January 2011 to May 2014 with clinical histories of priapism were identified and consented to participate. Inclusion criteria were self-reports of recurrent undesired, prolonged erection events irrespective of etiology. Because patients were not presenting with active priapism, cavernosal blood gas determinations were not done to establish ischemic vs non-ischemic forms of this disorder.14,15 Exclusion criteria were surgical treatments, i.e., penile shunt surgery, penile prosthesis implantation, and penile vascular surgery, or androgen ablative therapies for priapism (as possible confounding factors of patient assessments), concurrent major health debilitation, and inability to comprehend and self-complete the questionnaire. Pertinent demographic information, health histories, and detailed priapism histories were obtained.
Patients were instructed to complete the PIP questionnaire without assistance. They were next instructed to evaluate the instrument by descriptively rating each of the items in terms of clarity (for understanding) and importance as low, medium or high (Fig. 1B). Patients were requested to return for a second visit approximately 2–4 weeks following the first visit to assess test-retest reliability of the measure. However, because of infrequent timely return visits (less than 1 in 10 patients), combined with regularly inaccessible residences for mailing and means of communication with patients, the opportunity for repeat questionnaire administrations appropriately was limited.
Validation Testing
Content validation was assessed based on the descriptive rating of the items both as an initial analysis of the first 20 enrolled patients and at the final analysis consisting of all enrolled patients. Internal consistency coefficients for the total PIP questionnaire and the 3 subscales (domains) were generated using Cronbach’s α. Because questionnaires were inconsistently repeated, test-retest reliability testing was not performed. Criterion-oriented validity was assessed by evaluating the PIP’s ability to distinguish between patient subgroups based on priapism activity, priapism severity, and ED existence. Additionally, a priori hypotheses, specifically positive correlations between PIP questionnaire scores and actively present priapism, severity of priapism, and ED, were also tested. Active priapism was defined as ongoing priapism recurrences without spontaneous remission; spontaneous remission was defined as no active priapism episodes at least within the past year. Priapism of high severity was defined as priapism recurrences with regularly extended durations of episodes (> 2 hours). ED was defined as erection loss inclusive of mild to moderate, moderate or severe descriptors using specified ranges of the International Index of Erectile Function (IIEF) questionnaire-Erectile Function (EF) Domain (scores <22) or its short form comprising 5 questions (IIEF-5) (scores <17).8,10,16,17
Statistical analysis was performed using Stata 11 (StataCorp, College Station, TX, USA) and GraphPad Prism 5 (Graphpad Software Inc, La Jolla, CA, USA). Means ± standard deviations were determined. Interquartile range (IQR) served to indicate variance for median values. Continuous data were compared using the Mann-Whitney U nonparametric test. Categorical data were compared using the Chi Square or Fisher’s Exact test where appropriate. Correlations between PIP scores and patient subgroups were determined using Spearman’s rank correlation coefficient. Correlation coefficients of 0.1 – 0.3 were considered weak, 0.3 – 0.5 were considered moderate, and >0.5 were considered high.18 A P value < 0.05 was considered statistically significant. Cronbach’s α was calculated with acceptable values ranging from 0.70 to 0.95.19
Results
A total of 54 patients with priapism histories were enrolled, categorized etiologically into 2 groups: sickle cell disease (SCD), confirmed as SS or SC hemoglobinopathy (67%), and other associations (non-SCD) (33%), including idiopathic (n=15) and drug-related (n=3) etiologies (Table 1). Mean ages of SCD patients were more than a decade lower than that of non-SCD patients (p < 0.001). With respect to priapism histories, SCD patients reported priapism experiences starting at a younger mean age (p < 0.001), with a longer mean duration of priapism (p < 0.01), and with a greater mean proportion of “very minor” priapism episodes (p = 0.001), although with a similar priapism episode frequency (p > 0.05), compared with their non-SCD counterparts. With respect to ED, SCD patients reported a greater mean rate (p > 0.05) than non-SCD patients.
Table 1.
Demographic and clinical characteristics of SCD and non-SCD patients
| SCD Patients (n=36) |
Non-SCD Patients (n=18) |
P-Value | |
|---|---|---|---|
| Mean Age, yrs (SD) | 27.7 (8.2) | 39.7 (13.0) | 0.0004 |
| Race, n (%) | <0.0001* | ||
| Caucasian | 0/36 (0) | 8/18 (44.4) | |
| African American | 36/36 (100) | 9/18 (50) | |
| Hispanic | 0/36 (0) | 1/18 (5.6) | |
| Marital Status, n (%) | 0.0295 | ||
| Married | 4/36 (11.1) | 7/18 (38.9) | |
| Unmarried | 32/36 (88.9) | 11/18 (61.1) | |
| Priapism History | |||
| Age of Onset, yrs (SD) | 17.93 (7.6) | 34.06 (15.0) | 0.0002 |
| Overall Duration, yrs (SD) | 9.8 (7.0) | 5.6 (9.2) | 0.0026 |
| Episode Frequency, n (%) | |||
| Daily (1–7 episodes/wk) | 20/36 (55.6) | 10/18 (55.6) | 1.0000 |
| Monthly (<4 episodes/mo) | 15/36 (41.7) | 5/18 (27.8) | 0.3191 |
| Episode Duration†, n (%) | n = 35 | n = 15 | |
| ≤2 hrs (“very minor”) | 30/35 (85.7) | 4/35 (26.7) | 0.0001 |
| 2–5 hrs (“minor”) | 3/35 (8.6) | 1/35 (6.7) | 1.0000 |
| 5+ hrs (“major”) | 2/35 (5.7) | 10/35 (66.7) | 0.0001 |
| Erectile Dysfunction‡, n (%) | n = 32 | n = 16 | |
| 13/32 (40.6) | 3/16 (18.8) | 0.1296 |
SCD = sickle cell disease, n = number, yrs = years, wk = week, mo = month, SD = standard deviation,
combined Caucasian and Hispanic groups for Fisher’s exact test,
values absent for 4 patients,
values absent for 6 patients
The PIP questionnaire appeared to perform well in several respects. Patients completed the PIP questionnaire uniformly within 10–15 minutes. Content validity was determined to be good qualitatively based on medium to high ratings of “clarity” and “importance” for > 70% of questionnaire items by the initial 20 patients, all with “active” priapism. Based on this interim analysis, all items were retained in the instrument for completion by all subsequent study participants. At final analysis, all questions were rated as having medium or high “clarity” and “importance” by an average of 93% and 78% of patients, respectively (Table 2). PIP questionnaire internal consistency was demonstrated for the 3 assigned domains (in which higher scores indicate inferior experience): quality-of-life (QoL), sexual function (SF), and physical wellness (PW). The item-total Cronbach’s α reliability coefficient for the PIP score was 0.90. Individual item-subscales (domains) had α coefficients of 0.79 for QoL, 0.81 for SF, and 0.77 for PW. These values are consistent with a good (r > 0.70) item-domain/total instrument interrelatedness.
Table 2.
Patient evaluation of item importance and clarity
| N=54 | Item Rating as Medium or High | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | Q12 | |
|
Importance, n (%) |
48/54 (89) |
41/54 (76) |
43/54 (80) |
37/54 (69) |
42/54 (78) |
41/54 (76) |
42/54 (78) |
37/54 (69) |
41/54 (76) |
48/54 (89) |
49/54 (91) |
36/54 (67) |
|
Clarity*, n (%) |
51/53 (96) |
50/53 (94) |
48/53 (91) |
49/53 (92) |
49/53 (92) |
50/53 (94) |
49/53 (92) |
47/53 (89) |
50/53 (94) |
50/53 (94) |
52/53 (98) |
46/53 (87) |
N = number,
1 patient did not complete the clarity section,
Q = question
PIP questionnaire criterion-oriented validity was evaluated using several a priori hypotheses. We demonstrated the ability of both the total and subscale dimensions of this instrument in distinguishing between subgroups, finding uniformly higher scores for active priapism, high priapism severity, and existent ED relative to their converse conditions (Table 3A). We also found moderately positive correlations between the instrument scores and these a priori hypotheses (Table 3B). High severity of priapism was most marked for elevated PIP questionnaire scores (all p < 0.05). We also evaluated whether priapism etiology related to PIP questionnaire scores (Table 3A). Interestingly, PIP questionnaire scores were higher for non-SCD patients than that for SCD patients for all dimensions (all p < 0.05, except for PW).
Table 3.
| A PIP questionnaire criterion-oriented validity based on patient subgroups | ||||
|---|---|---|---|---|
| Item | Total | QoL | SF | PW |
| Priapism Activity†, median (IQR) | ||||
| Active (n=42) | 45.5 (30.8–57.3) | 18.5 (12.8–21.0) | 15.5 (9.0–21.3) | 13.0 (8.8–16.0) |
| Remission (n=8) | 21.5 (16.5–42.3) | 10.0 (8.0–14.8) | 7.5 (5.3–17.3) | 4.0 (3.0–8.8) |
| P Value | 0.0106 | 0.0159 | 0.0921 | 0.0017 |
| Priapism Severity†, median (IQR) | ||||
| High (n=16) | 55.5 (40.5–67.0) | 20.5 (18.3–23.8) | 20.5 (11.3–26.3) | 15.0 (11.8–18.0) |
| Low (n=34) | 35.0 (24.5–48.3) | 14 (4.0–19.3) | 10.0 (6.0–19.3) | 9.0 (4.8–13.0) |
| P Value | 0.0019 | 0.0020 | 0.0244 | 0.0007 |
| Erectile Dysfunction‡, median (IQR) | ||||
| Present (n=16) | 53.0 (32.8–63.3) | 19.5 (12.0–24.0) | 21.5 (13.0–27.0) | 11.5 (7.3–18.8) |
| Absent (n=32) | 36.0 (24.3–51.8) | 16.5 (10.3–20.0) | 10.5 (6.3–19.5) | 9.5 (6.3–14.8) |
| P Value | 0.0250 | 0.1366 | 0.0024 | 0.2498 |
| Priapism Etiology, median (IQR) | ||||
| SCD (n=36) | 38.5 (25.3–52.3) | 16.0 (10.3–19.8) | 12.0 (7.0–19.8) | 10.0 (6.3–14.0) |
| Non-SCD (n=18) | 52.0 (36.5–68.5) | 20 (15.3–24.3) | 20.0 (10.3–24.8) | 12.0 (8.0–16.5) |
| P Value | 0.0318 | 0.0170 | 0.0432 | 0.1596 |
| B Correlation coefficients for a priori hypotheses | ||||||||
|---|---|---|---|---|---|---|---|---|
| Item | Total | P Value | QoL | P Value | SF | P Value | PW | P Value |
| Priapism Activity† (Active vs Remission) |
0.367 | 0.009 | 0.346 | 0.014 | 0.243 | 0.090 | 0.451 | 0.001 |
| Priapism Severity† (High vs Low) |
0.446 | 0.001 | 0.443 | 0.001 | 0.323 | 0.022 | 0.487 | 0.0003 |
| Erectile Dysfunction‡ (Present vs Absent) |
0.329 | 0.023 | 0.219 | 0.135 | 0.444 | 0.002 | 0.170 | 0.249 |
PIP = priapism impact profile, QoL = quality of life, SF = sexual function, PW = physical wellness SCD = sickle cell disease, yrs = years, IQR = Interquartile Range,
values absent for 4 patients,
values absent for 6 patients
Comment
The PIP questionnaire was designed to address the need for a patient-reported outcome measure which validly represents the experience of priapism, familiarly known to healthcare providers for patients with this sexual dysfunction to exert profound mental and physical health consequences.5,6 The availability of an instrument which measures the adverse general health impact of the disorder offers an important direction for understanding and managing priapism. As such, the instrument may also prove useful for assessing the roles of conceivable interventions for treating priapism, which extends beyond simply accepting whether or not the intervention achieves the physical response of penile detumescence effectively and safely. Our preliminary investigation of this novel questionnaire indicates that it offers clinical utility for its intended purpose. Indeed, further study and validation of the psychometric performance of this instrument and its ongoing evaluation in clinical settings at baseline and after administration of valid treatments remain necessary.
We performed a series of evaluations that determined the practical feasibility and psychometric sensitivity of the PIP questionnaire. The instrument was constructed applying both internal and external expert input throughout the development process. In use, the instrument was successfully self-administered and rated highly by patients. Our study was inclusive of both SCD and non-SCD patient populations, although analyses to establish criterion-oriented validity were performed according to non-etiologic priapism characteristics. It is conceivable then that the tool may be useful irrespective of the etiology of priapism. However, further investigative work may be necessary to explore etiologically specific effects as well as effects based on priapism type (i.e., ischemic versus non-ischemic).
The instrument performed well according to various scale properties including reliability and validity measures where this was possible. We demonstrated internal consistency (Cronbach’s α), as a reliability measure of item intercorrelations, to be >0.75 for all total and domain scores, deeming the high performance of our instrument based on the good interrelatedness of its items with its subscale domains and the instrument as a whole.19,20 It is noteworthy that calculating test-retest reliability was problematic in the course of our study, in which major health and socioeconomic constraints encountered by our patients frequently hampered opportunities to re-evaluate the temporal stability of the instrument. Prior studies have also observed challenges of obtaining return clinic visits among individuals with priapism.13,21
Validity of the instrument, i.e., that it measured what it intends to measure, was shown preliminarily in our study. Content validity for the actual complications of priapism was suggested by assessments of the initial subset of patients. Criterion-oriented validity was evaluated by its correlations with hypothesized adverse outcomes of priapism. Our purpose of hypothesis testing applied outcomes referable to expert opinion as well as a validated, well-known tool for assessing erection ability, the IIEF.8,10 As ED of varying degrees can be a concurrent complication of recurrent priapism, it can certainly influence patient perceptions regarding sexual function, and is therefore relevant to a priapism impact questionnaire. It was interesting to observe that non-SCD patients generated higher scores on the PIP questionnaire compared with SCD patients in this study. A possible explanation for this observation is that SCD patients may have better accommodated to the global impact and complications of their underlying SCD condition relative to the likely more healthy non-SCD patients at baseline.
Several potential limitations of this study merit consideration. We recognize that development and administration of this tool at a single institution limits its external validity (generalizability). We acknowledge that the instrument may not fully capture the range of emotional and psychosocial concerns of patients experiencing priapism. Further study of this subject may reveal additional themes requiring measurement. We also acknowledge the importance of clinical history in assessing overall health status. Notably, in a recent study, we found that in areas except tobacco use, clinical history did not differ significantly between cohorts of SCD and non-SCD patients.22 We realize that our work conceivably represents a very preliminary investigation of this research arena. The next study at a larger scale, possibly involving multiple institutions may lend additional evidence in support of our findings and suggest how this instrument may be further developed and applied. Sponsorship of such a study providing sufficient mechanisms for patient support and retention would be advantageous in this regard. Fundamental limitations of recall bias and subjectivity are inherent in this type of investigation although further evaluations involving prospective serial monitoring and possibly objective assessments of priapism (e.g., classification type, progression level) may permit more precise associations of impact scores and priapism characteristics.
Conclusions
The PIP questionnaire was introduced as an easily administered, clinically relevant tool for measuring the impact of priapism from the patient’s perspective. It refers specifically to symptomatology and subjective outcomes in domains of quality-of-life, sexual function and physical wellness impacted adversely by priapism. Although the content items seem straightforward, the objective of assembling complications of this disorder into a patient-reported outcome measure may permit an efficient and effective way to better understand and manage priapism. Although a clinical role for this instrument was shown herein, its further testing and development in additional priapism cohorts is necessary to define its psychometric properties. Such a fully validated tool will be most useful to advance priapism clinical research, and the clinical management of patients with priapism.
ACKNOWLEDGMENTS
We thank Drs. Linda Smith-Resar and Sophie Lanzkron for providing additional patients to evaluate this questionnaire. We also thank Irene N. Trueheart for her assistance in questionnaire administration.
Footnotes
Conflict of Interest: The authors declare that they have no conflicts of interest.
References
- 1.Kovac JR, Mak SK, Garcia MM, et al. A pathophysiology-based approach to the management of early priapism. Asian journal of andrology. 2013;15:20–26. doi: 10.1038/aja.2012.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morrison BF, Burnett AL. Stuttering priapism: insights into pathogenesis and management. Current urology reports. 2012;13:268–276. doi: 10.1007/s11934-012-0258-9. [DOI] [PubMed] [Google Scholar]
- 3.Burnett AL. Surgical management of ischemic priapism. The journal of sexual medicine. 2012;9:114–120. doi: 10.1111/j.1743-6109.2011.02446.x. [DOI] [PubMed] [Google Scholar]
- 4.Burnett AL, Bivalacqua TJ. Priapism: new concepts in medical and surgical management. The Urologic clinics of North America. 2011;38:185–194. doi: 10.1016/j.ucl.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 5.Addis G, Spector R, Shaw E, et al. The physical, social and psychological impact of priapism on adult males with sickle cell disorder. Chronic illness. 2007;3:145–154. doi: 10.1177/1742395307081505. [DOI] [PubMed] [Google Scholar]
- 6.Broderick GA, Kadioglu A, Bivalacqua TJ, et al. Priapism: pathogenesis, epidemiology, and management. The journal of sexual medicine. 2010;7:476–500. doi: 10.1111/j.1743-6109.2009.01625.x. [DOI] [PubMed] [Google Scholar]
- 7.Burnett AL. Anxiety disorders in patients with idiopathic priapism: risk factor and pathophysiologic link? The journal of sexual medicine. 2009;6:1712–1718. doi: 10.1111/j.1743-6109.2009.01246.x. [DOI] [PubMed] [Google Scholar]
- 8.Cappelleri JC, Rosen RC, Smith MD, et al. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999;54:346–351. doi: 10.1016/s0090-4295(99)00099-0. [DOI] [PubMed] [Google Scholar]
- 9.Quirk FH, Heiman JR, Rosen RC, et al. Development of a sexual function questionnaire for clinical trials of female sexual dysfunction. Journal of women's health & gender-based medicine. 2002;11:277–289. doi: 10.1089/152460902753668475. [DOI] [PubMed] [Google Scholar]
- 10.Rosen RC, Cappelleri JC, Smith MD, et al. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. International journal of impotence research. 1999;11:319–326. doi: 10.1038/sj.ijir.3900472. [DOI] [PubMed] [Google Scholar]
- 11.Porst H, Gilbert C, Collins S, et al. Development and validation of the quality of erection questionnaire. The journal of sexual medicine. 2007;4:372–381. doi: 10.1111/j.1743-6109.2006.00422.x. [DOI] [PubMed] [Google Scholar]
- 12.Symonds T, Boolell M, Quirk F. Development of a questionnaire on sexual quality of life in women. Journal of sex & marital therapy. 2005;31:385–397. doi: 10.1080/00926230591006502. [DOI] [PubMed] [Google Scholar]
- 13.Burnett AL, Anele UA, Trueheart IN, et al. Randomized controlled trial of sildenafil for preventing recurrent ischemic priapism in sickle cell disease. The American journal of medicine. 2014;127:664–668. doi: 10.1016/j.amjmed.2014.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berger R, Billups K, Brock G, et al. Report of the American Foundation for Urologic Disease (AFUD) Thought Leader Panel for evaluation and treatment of priapism. International journal of impotence research. 2001;13(Suppl 5):S39–S43. doi: 10.1038/sj.ijir.3900777. [DOI] [PubMed] [Google Scholar]
- 15.Montague DK, Jarow J, Broderick GA, et al. American Urological Association guideline on the management of priapism. The Journal of urology. 2003;170:1318–1324. doi: 10.1097/01.ju.0000087608.07371.ca. [DOI] [PubMed] [Google Scholar]
- 16.Mulhall JP, Bivalacqua TJ, Becher EF. Standard operating procedure for the preservation of erectile function outcomes after radical prostatectomy. The journal of sexual medicine. 2013;10:195–203. doi: 10.1111/j.1743-6109.2012.02885.x. [DOI] [PubMed] [Google Scholar]
- 17.Teloken P, Valenzuela R, Parker M, et al. The correlation between erectile function and patient satisfaction. The journal of sexual medicine. 2007;4:472–476. doi: 10.1111/j.1743-6109.2005.00164.x. [DOI] [PubMed] [Google Scholar]
- 18.Cohen RK, Swerdlik ME. Psychological testing and assessment: An introduction to tests and measurement. New York: McGraw-Hill; 2010. [Google Scholar]
- 19.Tavakol MDR. Making sense of Cronbach’s alpha. International Journal of Medical Education. 2011;2:53–55. doi: 10.5116/ijme.4dfb.8dfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang YGS. Coefficient Alpha: A Reliability Coefficient for the 21st Century? Journal of Psychoeducational Assessment. 2011;29:377–392. [Google Scholar]
- 21.Olujohungbe AB, Adeyoju A, Yardumian A, et al. A prospective diary study of stuttering priapism in adolescents and young men with sickle cell anemia: report of an international randomized control trial--the priapism in sickle cell study. Journal of andrology. 2011;32:375–382. doi: 10.2164/jandrol.110.010934. [DOI] [PubMed] [Google Scholar]
- 22.Anele UA, Burnett AL. Erectile Dysfunction after Sickle Cell Disease-Associated Recurrent Ischemic Priapism: Profile and Risk Factors. The journal of sexual medicine. 2015 doi: 10.1111/jsm.12816. [DOI] [PMC free article] [PubMed] [Google Scholar]