Abstract
Purpose:
Kissing stent reconstruction is a widely used technique for the management of aortoiliac occlusive disease involving the aortic bifurcation or proximal common iliac arteries. The purpose of this study was to evaluate the results of self-expandable kissing stents in the aortic bifurcation.
Materials and Methods:
We reviewed medical records of the patients treated with a kissing stent retrospectively from January 2007 to December 2012. The primary and secondary patencies were determined with Kaplan-Meier analysis, and Cox regression was used to determine the factors associated with patency.
Results:
A total of 21 patients were included, and all were male (median age 53±15 years, range 48–78 years). Major symptoms were claudication (n=16, 61.9%), rest pain (n=5, 23.8%) and gangrene (n=5, 23.8%). Tans-Atlantic Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC) II classification was A 2 (9.5%), B 5 (23.8%), C 7 (33.3%) and D 8 (38%). The mean follow-up was 40.7 months. Major complication occurred in only one case which consisted of distal limb ischemia by emboli. Six patients developed symptomatic restenosis or occlusion. There was no major amputation, but minor amputation occurred in 3 patients. There were 2 mortalities not associated with the procedure (lung cancer and intracranial hemorrhage). Primary patency was 89.6% at 1 year, 74.7% at 3 years and 64.0% at 5 years. Secondary patency was 94.1% at 1 year, 88.2% at 3 years and 68.6% at 5 years. No risk factors for restenosis or occlusion were identified.
Conclusion:
Self-expandable kissing stents can be used successfully with comparable patency for endovascular treatment of symptomatic atherosclerotic occlusive lesions in the aortic bifurcation area.
Keywords: Kissing stents, Aortic bifurcation, Aortoiliac occlusive disease
INTRODUCTION
Aortoiliac occlusive disease is a common component of atherosclerosis which often presents with lower limb claudication and can potentially progress to critical limb ischemia [1]. According to existing guidelines, surgery is the gold standard for bilateral and extensive occlusive disease on the basis of excellent long term patency rate [2]. However, although these interventions are highly effective (5-year patency rate of 91%), they are also associated with significant morbidity (8.3%, including bleeding, cardiac failure, renal failure, pneumonia) and mortality (3.3%) [3]. Initially proposed as an alternative to traditional surgery, kissing stenting endovascular treatment with two non-covered embraced stents has gradually developed, as it is easy to perform [4]. Among the various endovascular techniques, the kissing stent technique has been proved to be feasible in patients with lesions involving the distal aorta and/or the origin of one or both iliac arteries; however, there is a limited number of studies dealing with long term outcomes of this technique [5]. The aim of this study was to analyze outcome after self-expandable kissing stent placement.
MATERIALS AND METHODS
Patients treated with kissing stents in the aortic bifurcation between 2007 and 2012 in Chonbuk National University Hospital were included. All intraoperative angiographies were reviewed for Tans-Atlantic Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC) II classification. The procedure notes were analyzed for type, model and size of stents inserted in the distal aorta, common and external iliac arteries. A retrospective analysis was performed for demographics, complications and follow-ups using patient records. Their pre-interventional symptoms were graded according to the Rutherford classification. All patients were evaluated with pre- and post-treatment computed tomography angiography and ankle-brachial index at least once each.
1). Technique
All procedures were performed in a dedicated angiosuite with a fixed C-arm system. All patients were treated percutaneously through bilateral common femoral arterial (CFA) punctures, in most cases with 6–8 French introducers. The CFA punctures were performed under ultrasound guidance, frequently with micro-puncture technique and contrast injections to confirm a correct location of the puncture. In patients with bilateral occlusions of the common iliac arteries or occlusion of the distal aorta, a left brachial access was used to facilitate the procedure. Stenoses were passed intraluminally and occlusions recanalized subintimally with a 0.035-inch hydrophilic guidewire (Terumo, Tokyo, Japan). Pre-dilatation was performed with 3–5 mm balloon dilatation catheters after guidewire passage. The model and size of stents were chosen based on lesion characteristics and availability; the same models were used on both sides. All stents were self-expanding nitinol stents and the models included Zilver vascular self-expanding stent (Zilver; Cook, Bloomington, MN, USA; n=7), EverFlex (EV3, Plymouth, MN, USA; n=5), Luminexx3 (Bard Peripheral Vascular, Tempe, AZ, USA; n=4), Smart (Cordis; Johnson & Johnson Company, Miami Lakes, FL, USA; n=2), and others (n=3). All kissing stents were deployed at the same proximal end level in the aorta above the native aortic bifurcation. Post-dilatation was performed to the nominal vessel diameter, as measured on pre-treatment angiogram. Technical success was defined as less than 30% residual stenosis in completion angiogram. After intervention, all patients remained in hospital for 2–3 days, and received anti-thrombotic agents orally. All patients continued with their ordinary anti-platelet agent at least 6 months after discharge from hospital.
2). Statistics
Statistical significance was defined as P<0.05. Categorical data was analyzed with chi-square and Fishers exact test. Patency rates were determined with Kaplan-Meier and life table analysis. Cox regression was used to analyze failure-related relative risks with a 95% confidence interval. A second analysis included all potential determinants in the same model. PASW Statistics ver. 18.0 (IBM Co., Armonk, NY, USA) was used for all statistical analysis.
RESULTS
Twenty-one male patients were included in this study. The patient characteristics are summarized in Table 1. Technical success was achieved in all patients (100%). Immediate complications included one case of distal emboli and three cases of bilateral groin hematomas. The groin hematomas recovered without additional procedures. The emboli in the proximal posterior tibial artery were removed with aspiration thrombectomy using a clot extraction device (Penumbra, Alameda, CA, USA). Iliac lesions were classified as TASC II A in 2 (9.5%), B in 5 (23.8%), C in 7 (33.3%), and D in 8 (38.0%) patients. The most frequent symptom was intermittent claudication in 13 (61%) patients and none had major tissue loss. The mean pre-treatment ankle-brachial index (ABI) was 0.53 and post-treatment ABI was 0.81.
Table 1.
Clinical characteristics of 21 patients who underwent self-expandable kissing stents in the aortic bifurcation
| Clinical characteristic | n (%) |
|---|---|
| Age (>60 y) | 15 (71.4) |
| Male | 21 (100.0) |
| Risk factor | |
| Past smoking | 17 (81.0) |
| Current smoking | 15 (71.4) |
| Diabetes mellitus | 7 (33.3) |
| Hypertension | 15 (71.4) |
| Hypercholesterolemia | 13 (61.9) |
| Ischemic heart disease | 5 (23.8) |
| Cerebral vascular disease | 5 (23.8) |
| Rutherford classification | |
| 1: mild claudication | 2 (9.5) |
| 2: moderate claudication | 7 (33.3) |
| 3: severe claudication | 4 (19.0) |
| 4: ischemia rest pain | 8 (38.0) |
| 5: minor tissue loss | 5 (23.8) |
| 6: major tissue loss | 0 (0) |
| TASC II classification | |
| A | 2 (9.5) |
| B | 5 (23.8) |
| C | 7 (33.3) |
| D | 8 (38.0) |
TASC, Tans-Atlantic Inter-Society Consensus for the Management of Peripheral Arterial Disease.
Bilateral iliac stenosis was found in 7 patients and distal aorta total occlusion in 2 patients. Additional access of the left brachial artery was performed in 3 patients: 2 in bilateral common iliac artery occlusions and 1 in distal aorta total occlusion. The mean diameter of the deployed stents was 8.76 mm (range: 6 to 10 mm) and the mean length was 94.7 mm (range: 60 to 150 mm). Nine (42.8%) patients had combined infrainguinal peripheral artery occlusive disease (PAOD); 5 of these patients needed a simultaneous percutaneous transluminal angioplasty (PTA) and/or superficial femoral artery (SFA) stenting.
No significant risk factors for restenosis or occlusion were identified (Table 2). During a mean follow-up of 40.7 months (range: 14 to 67), 6 of 21 (28.5%) patients had a recurrent symptom with in-stent stenosis or occlusion. Four of these 6 patients had infrainguinal PAOD, with PTA and/or SFA stenting being performed simultaneously. Restenosis or occlusion in kissing stents were treated with re-endovascular procedures or operation; one patient recovered after thrombolysis, another one recovered after PTA, and the other 4 patients needed surgery (3 toe amputation, 1 femoral-femoral bypass). There was no major amputation. Two deaths occurred during follow-up; the causes of deaths were lung cancer aggravation and intracranial hemorrhage.
Table 2.
Evaluation of possible risk factors for restenosis or occlusion
| Possible risk factor | P-value |
|---|---|
| Age | 0.293 |
| Hypertension | 0.762 |
| Diabetes mellitus | 0.273 |
| Ischemic heart disease | 0.657 |
| Cerebral vascular disease | 0.657 |
| Current smoking | 0.083 |
| Combined PAOD | 0.163 |
| TASC II classification | 0.558 |
| Rutherford classification 1, 2, 3 | 0.481 |
| Rutherford classification 4 | 0.484 |
| Rutherford classification 5 | 0.526 |
PAOD, peripheral arterial occlusive disease; TASC, Tans-Atlantic Inter-Society Consensus for the Management of Peripheral Arterial Disease.
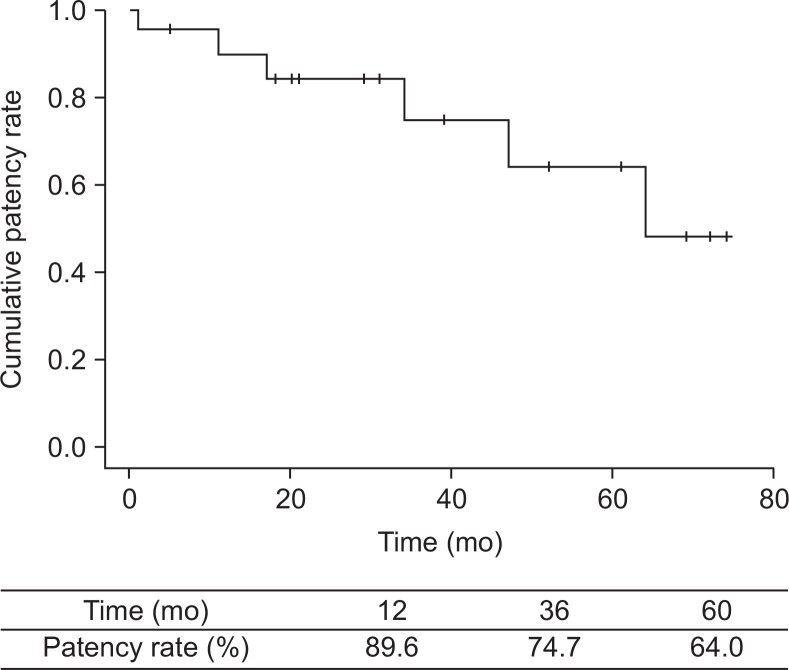
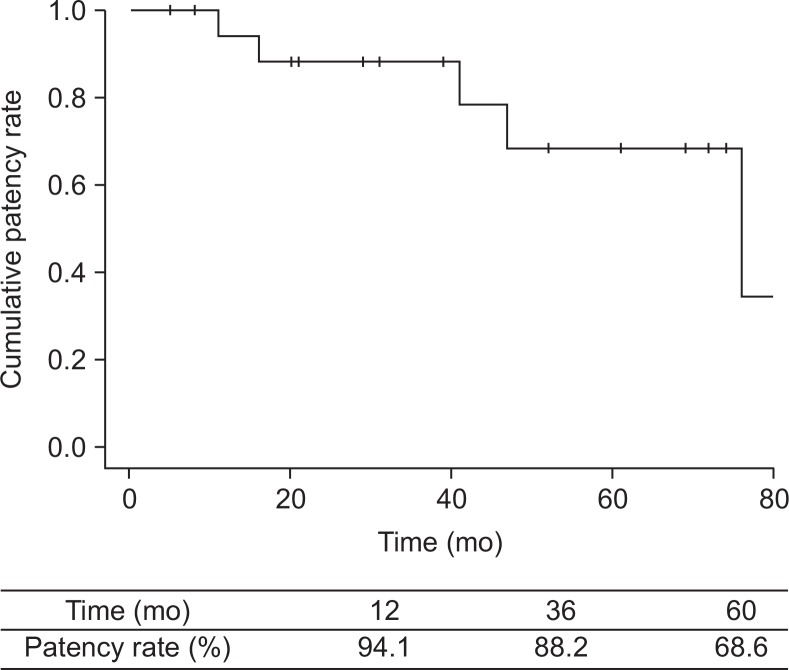
Primary patency at 1, 3, 5 years was 86.9%, 74.7%, 64.0% (Fig. 1) and secondary patency was 94.1%, 88.2%, 68.6% (Fig. 2), respectively. Post-treatment agents included aspirin (n=17), clopidogrel (n=7), cilostazol (n=6) and warfarin (n=2), and there was no significant patency improvement with each drug.
Fig. 1.
Kaplan-Meier plot of primary patency after kissing stents in the aortic bifurcation.
Fig. 2.
Kaplan-Meier plot of secondary patency after kissing stents in the aortic bifurcation.
DISCUSSION
Although endovascular treatment has become the most widely used treatment for aortic bifurcation lesions because of its very little invasive characteristics, surgery is still certainly effective with good patency [1,4,6]. The patency for aortobifemoral bypass is reported at 85%–89% at five years and 70%–85% at ten years in claudicants and 72%–82% at five years and 61%–76% at ten years in critical limb ischemia [7]. However, meta-analysis studies have shown an aggregated operative mortality rate of 3.3% and an aggregated systemic morbidity of 8.3% [6]. Moreover, surprising development of endovascular devices and skills lead to similar patency of kissing stents. The largest series follow-up of 106 patients by Houston et al. [8] showed primary and secondary-assisted patency rates of 79% and 98% at follow-up of 36 months. Brittenden et al. [9], Scheinert et al. [10] reported better results with a primary patency rate of 92% after 20 months, 87% at 2 years, and 80% after 3 years, respectively [3]. In our series, three-year follow-up for kissing stenting showed primary and secondary patency rates of 74.7% and 88.2%, and five-year follow-up showed 64.0% and 68.6%, respectively.
Several clinical, anatomical and technical factors have been advocated to significantly affect long term results of the kissing stent technique. Prior data suggest that the outcome in iliac stenting may be negatively influenced by younger age, smaller iliac vessel size, female gender, hormonal replacement therapy, individual aortic anatomy and stenting configuration, diseased external iliac artery, number of stents used, presence of multi-segment disease, presence of concomitant common femoral disease, TASC class C or D, longer-stented segment, presence of occlusion, and extensive distal runoff occlusive disease [11–14]. In our series, there were no significant risk factors related to outcome; the small number of patients and the retrospective nature limit the ability to analyze these factors definitely.
Some authors recommend the use of covered stents because they seem to be more appropriate in case of TASC C or D lesions [4]. Sabri et al. [15] recommended that covered balloon expandable kissing stents for atherosclerotic aortic bifurcation occlusive disease provides superior patency at 2 years as compared with bare metal balloon-expandable stents; covered stents rather than bare metal stents may provide more laminar flow, decreased thrombogenicity, less chance for prolapse of plaque through the covered stent, and less ingrowth of hyperplastic tissue. However, Groot Jebbink et al. [2] commented that although clinical data are still lacking, in vitro data suggest that the use of self-expandable nitinol kissing stents is to be preferred over bare metal balloon expandable stents because of significant reduction in mismatch area. Moreover, Tapping et al. [1] suggested that self-expanding stents (as used in all of our patients) also provide an even radial force and gradually expand after balloon dilatation, thus minimizing the risk of aortic rupture. They might also theoretically trap more atherosclerotic material, thus decreasing the chance of distal embolization. In our series, self-expandable stents were used with comparable long-term patency rates.
Most complications in endovascular treatment from the puncture sites are fairly mild; uncomplicated groin hematoma occurred in 6%–12% in other reports [7]. In our series, 3 groin hematomas in 21 patients occurred and recovered without additional procedures. A meticulous puncture technique, using fluoroscopy to confirm a CFA position below the inguinal ligament and above the femoral bifurcation, is critical in avoiding bleeding complications [16]. Major complications, such as vessel ruptures, distal embolizations and thromboses, also occurred in 2%–5% [13], and usually immediately solved with covered stents, aspiration and thrombolysis [7]. In our series, 1 distal embolization was immediately treated with aspiration thrombectomy.
CONCLUSION
Self-expandable kissing stents can be used successfully with comparable patency for endovascular treatment of symptomatic atherosclerotic occlusive lesions in the aortic bifurcation area.
Footnotes
Conflict of interest: None.
REFERENCES
- 1.Tapping CR, Ahmed M, Scott PM, Lakshminarayan R, Robinson GJ, Ettles DF, et al. Primary infrarenal aortic stenting with or without iliac stenting for isolated and aortoiliac stenoses: single-centre experience with long-term follow-up. Cardiovasc Intervent Radiol. 2013;36:62–68. doi: 10.1007/s00270-012-0372-6. [DOI] [PubMed] [Google Scholar]
- 2.Groot Jebbink E, Grimme FA, Goverde PC, van Oostayen JA, Slump CH, Reijnen MM. Geometrical consequences of kissing stents and the Covered Endovascular Reconstruction of the Aortic Bifurcation configuration in an in vitro model for endovascular reconstruction of aortic bifurcation. J Vasc Surg. 2014 doi: 10.1016/j.jvs.2013.12.026. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.van’t Riet M, Spronk S, Jonkman J, Den Hoed T. Endovascular treatment of atherosclerosis at the aortoiliac bifurcation with kissing stents or distal aortic stents: a temporary solution or durable improvement? J Vasc Nurs. 2008;26:82–85. doi: 10.1016/j.jvn.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 4.Abello N, Kretz B, Picquet J, Magnan PE, Hassen-Khodja R, Chevalier J, et al. Association Universitaire de Recherche en Chirurgie Vasculaire (AURC) Long-term results of stenting of the aortic bifurcation. Ann Vasc Surg. 2012;26:521–526. doi: 10.1016/j.avsg.2011.05.046. [DOI] [PubMed] [Google Scholar]
- 5.Pulli R, Dorigo W, Fargion A, Angiletta D, Azas L, Pratesi G, et al. Early and midterm results of kissing stent technique in the management of aortoiliac obstructive disease. Ann Vasc Surg. 2015;29:543–550. doi: 10.1016/j.avsg.2014.10.029. [DOI] [PubMed] [Google Scholar]
- 6.Mohamed F, Sarkar B, Timmons G, Mudawi A, Ashour H, Uberoi R. Outcome of “kissing stents” for aortoiliac atherosclerotic disease, including the effect on the non-diseased contralateral iliac limb. Cardiovasc Intervent Radiol. 2002;25:472–475. doi: 10.1007/s00270-001-0120-9. [DOI] [PubMed] [Google Scholar]
- 7.Björses K, Ivancev K, Riva L, Manjer J, Uher P, Resch T. Kissing stents in the aortic bifurcation--a valid reconstruction for aorto-iliac occlusive disease. Eur J Vasc Endovasc Surg. 2008;36:424–431. doi: 10.1016/j.ejvs.2008.06.027. [DOI] [PubMed] [Google Scholar]
- 8.Houston JG, Bhat R, Ross R, Stonebridge PA. Long-term results after placement of aortic bifurcation self-expanding stents: 10 year mortality, stent restenosis, and distal disease progression. Cardiovasc Intervent Radiol. 2007;30:42–47. doi: 10.1007/s00270-006-0111-y. [DOI] [PubMed] [Google Scholar]
- 9.Brittenden J, Beattie G, Bradbury AW. Outcome of iliac kissing stents. Eur J Vasc Endovasc Surg. 2001;22:466–468. doi: 10.1053/ejvs.2001.1481. [DOI] [PubMed] [Google Scholar]
- 10.Scheinert D, Schröder M, Balzer JO, Steinkamp H, Biamino G. Stent-supported reconstruction of the aortoiliac bifurcation with the kissing balloon technique. Circulation. 1999;100(19 Suppl):II295–II300. doi: 10.1161/01.CIR.100.suppl_2.II-295. [DOI] [PubMed] [Google Scholar]
- 11.Insall RL, Loose HW, Chamberlain J. Long-term results of double-balloon percutaneous transluminal angioplasty of the aorta and iliac arteries. Eur J Vasc Surg. 1993;7:31–36. doi: 10.1016/S0950-821X(05)80540-7. [DOI] [PubMed] [Google Scholar]
- 12.Schürmann K, Mahnken A, Meyer J, Haage P, Chalabi K, Peters I, et al. Long-term results 10 years after iliac arterial stent placement. Radiology. 2002;224:731–738. doi: 10.1148/radiol.2242011101. [DOI] [PubMed] [Google Scholar]
- 13.Yilmaz S, Sindel T, Golbasi I, Turkay C, Mete A, Lüleci E. Aortoiliac kissing stents: long-term results and analysis of risk factors affecting patency. J Endovasc Ther. 2006;13:291–301. doi: 10.1583/05-1708.1. [DOI] [PubMed] [Google Scholar]
- 14.Sharafuddin MJ, Hoballah JJ, Kresowik TF, Sharp WJ. Kissing stent reconstruction of the aortoiliac bifurcation. Perspect Vasc Surg Endovasc Ther. 2008;20:50–60. doi: 10.1177/1531003507313224. [DOI] [PubMed] [Google Scholar]
- 15.Sabri SS, Choudhri A, Orgera G, Arslan B, Turba UC, Harthun NL, et al. Outcomes of covered kissing stent placement compared with bare metal stent placement in the treatment of atherosclerotic occlusive disease at the aortic bifurcation. J Vasc Interv Radiol. 2010;21:995–1003. doi: 10.1016/j.jvir.2010.02.032. [DOI] [PubMed] [Google Scholar]
- 16.Fitts J, Ver Lee P, Hofmaster P, Malenka D, Northern New England Cardiovascular Study Group Fluoroscopy-guided femoral artery puncture reduces the risk of PCI-related vascular complications. J Interv Cardiol. 2008;21:273–278. doi: 10.1111/j.1540-8183.2008.00351.x. [DOI] [PubMed] [Google Scholar]