Abstract
Background
With the development of assisted reproductive technology, more patients with infertility prefer to get pregnant by in vitro fertilization and embryo transplantation (IVF-ET). But the indications of IVF-ET must be strictly controlled by the clinicians.
Case report
We described a case of a 29-year-old pregnant Chinese woman with military tuberculosis. She was admitted to the hospital with complaints of fever and shortness of breath. She received IVF-ET 83 days ago, because of infertility with bilateraltubal occlusion, and was in pregnancy status. We presented the clinical, laboratory and two chest CT scan features of the patient. The second chest CT scan showed randomly distributed, innumerable tiny, military nodules throughout the lungs. The fluorescence quantitative PCR of the bronchoalveolar lavage fluid (BALF) was positive for Mycobacterium tuberculosis. The M. tuberculosis was cultured from BALF on Day 29. So we made the diagnosis of military tuberculosis.
Conclusion
It is important to rule out tuberculosis for the infertility patients especially with bilateraltubal occlusion before IVF-ET in order to avoid tuberculosis disseminate during pregnancy.
Keywords: military tuberculosis, in vitro fertilization and embryo transplantation
Introduction
Tuberculosis has been a major health problem all over the world. Currently, about one-third of the human population is infected with tuberculosis worldwide1. Genital tuberculosis is one of the most common causes of female infertility2. With the development of assisted reproductive technology, more infertility patients prefer to get pregnant by in vitro fertilization and embryo transplantation (IVF-ET). But we found one patient who showed tuberculosis dissemination during pregnancy after IVF-ET.
Case report
A 29-year-old woman was admitted to the hospital with complaints of fever and shortness of breath. She got a fever for five days with no reasons and felt breathlesson exertion for two days. The highest temperature was 38.4°C, she had no chills and rogors. She denied any complaints of cough, sputum, abdominal pain, diarrhea, urinary frequency, urgency of urination, urodynia, night sweats or weight loss. She had received amoxicillin but without any effect. Her remaining medical history was bilateral tubal occlusion. She had amenorrhea for three and a half month, and had received IVF-ET 83 days ago. She was in pregnancy status for 69 days according to the high level of the human chorionic gonadotropin (HCG) in blood, and two gestational sac and embryocardia had been found in her uterus through the ultrasonography 55 days ago. After IVF-ET she had taken 10mg dydrogesterone orally and 10mg progesterone by intramuscular injection per day for one month. She had no history of prior pulmonary infection.
On physical examination, her temperature was 37.9°C; BP, 117/79 mmHg, pulse, 110 beats/min, respiratory frequency, 20 breaths/min and oxygen saturation, 96 % on room air. Head and neck examination results were normal without nuchal rigidity. Chest examination was normal. Cardiac examination revealed a regular rhythm, no gallop or murmur. Abdomen was not tender, with normal bowel sounds without hepatosplenomegaly. Extremities revealed no pitting edema. There was no evidence of any skin rash.
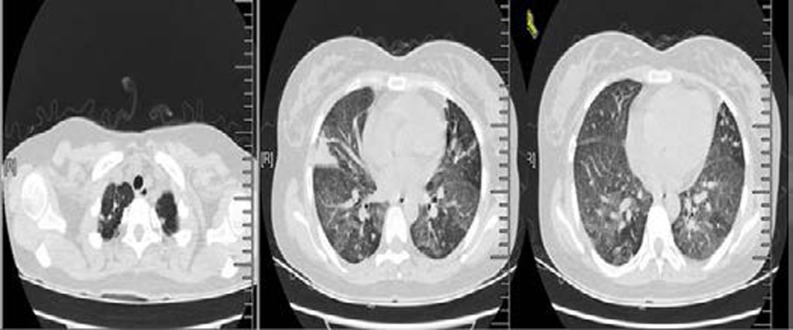
Laboratory test presented that white blood cell count were 5570 cells/µL with 80.4% neutrophils, hemoglobin level was 10.4 g/dL, and platelet count was 315,000 cell/µL. CRP was 18.2 mg/l. Electrolytes, renal and liver function tests were normal. ESR was 32 mm/h. Rapid HIV screening was negative. ECG showed sinus tachycardia. Chest CT scan (Fig 1) showed consolidation and effusion in the middle lobe of the right lung and hyperplasia and calcified lesions in the bilateral upper lobes of the lung. According to these results the community acquired pneumonia (CAP) and secondary tuberculosis diagnosis was made.
Fig 1.
consolidation and effusion in the middle lobe of the right lung and calcified lesions in double upper lobe hyperplasia
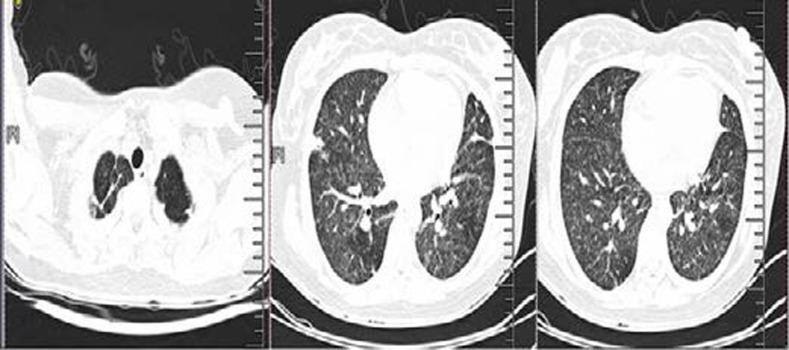
The patient was treated with Azithromycin and Cefuroxime. However, she developed severe shortness of breath and the temperature reaching 40°C, respiratory frequency 26 breaths/min, oxygen saturation 90% in room air. Arterial blood gas analysis revealed PH 7.43, PaO2 59.3mmHg and PaCO2 32mmHg. She got serious. Five days later, the other chest CT scan (Fig 2) showed randomly distributed, innumerable tiny, military nodules throughout the lungs. The branchofiberoscope test was performed. The bronchoalveolar lavage fluid (BALF) did not find acid-fast bacilli. But the fluorescence quantitative PCR of BALF was positive for Mycobacterium tuberculosis and M. tuberculosis was cultured on Day 29 from BALF. Thus, the diagnosis was revised to Military tuberculosis.
Fig 2.
Diffuse miliary pattern in the lung
Discussion
It is well established that genital tuberculosis is one of the most common causes of female infertility2. In female genital tuberculosis patients, it affects the fallopian tubes and the endometrium and may cause infertility, the incidence of infertility in genital tuberculosis worldwide varies from 44 to 74%3. Involvement of the endometrium is observed in 50–60% of the genital tuberculosis patients4. In China we have no true prevalence. However, it is difficult to predict the accurate prevalence of genital tuberculosis because it often tends to exist without any clinical signs or symptoms.
Military tuberculosis is due to hematogenous spread of tubercle bacilli. It is often the consequence of primary infection in children, in adults it may be due to either recent infection or reactivation of old disseminated foci5, when their immune function is lower, such as longtime using immunosuppressive agents (e.g., glucocorticoid, anti-cancer drugs, etc), immunocompromised persons (e.g., patients with HIV infection), combined with chronic disease or the elderly and so on. Military tuberculosis has showed relatively specific images, so most of the time a high index of suspicion is required for the images to diagnose military tuberculosis.
During pregnancy, the maternal immune system shows a relative bias toward T helper type 2 immunity. These alterations lead to impaired cell-mediated immunity with increased susceptibility to certain infections such as tuberculosis6. In addition to the change of immune system during pregnancy, after IVF-ET the patient took dydrogesterone orally everyday to protect the fetus. Dydrogesterone is a kind of progesterone which affects the cellular immune function just like glucocorticoids7. Our patient didn't have any signs and symptoms of genital tuberculosis and she had no history of prior pulmonary infection. However, the first chest CT scan showed the hyperplasia and calcified lesions in the bilateral upper lobes of the lung. Actually she had had the Mycobacterium tuberculosis infection before, that may have been the reason for her bilateral tubal occlusion and the latent foci was reactive and disseminated when she got pregnant.
Conclusion
More than 5 million new cases of tuberculosis (all forms, both pulmonary and extrapulmonary) were reported to the World Health Organization (WHO) in 2005, >90% of cases were reported from developing countries2. China is the most populous developing country in the world, so prevention and control of tuberculosis is very important. With the development of assisted reproductive technology, more and more patients with infertility get pregnant by IVF-ET. Thus, before IVF-ET operation, clinicians should exclude tuberculosis for the infertility patients especially with bilateraltubal occlusion in order to avoid tuberculosis disseminate during pregnancy.
Follow up
The patient was transferred to the specialised hospital and started on four-drug chemotherapy with isoniazid, rifampin, pyrazinamide, and ethambutol. Unfortunately, after two weeks the patient had an abortion. One month later clinical symptoms had completely disappeared.
References
- 1.World Health Organization, author. Guidelines for the programmatic management of drug-resistant tuberculosis. Geneva: 2006. [PubMed] [Google Scholar]
- 2.Sutherland A. The changing pattern of tuberculosis of the female genital tract: a thirty year survey. Arch Gynecol Obstet. 1983;234:95–101. doi: 10.1007/BF00207681. [DOI] [PubMed] [Google Scholar]
- 3.Tripathy SN, Tripathy SN. Infertility and pregnancy outcome in female genital tuberculosis. Fertil Steril. 2002;76:159–163. doi: 10.1016/s0020-7292(01)00525-2. [DOI] [PubMed] [Google Scholar]
- 4.Gurgan T, Demirol A. Tuberculosis in assisted reproduction and infertility. Int Congr Ser. 2004;1266:287–294. [Google Scholar]
- 5.Harrison's PRINCIPLES OF INTERNAL MEDICINE. Seventeenth Edition. Chapter 158. [Google Scholar]
- 6.Yip L, MeCluskey J, Sinclair R. Immunological aspects of pregnancy. Clin Dermatol. 2006;24:84–87. doi: 10.1016/j.clindermatol.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 7.Song Xiangf, Sun Xiang, Wang Hui. Regulatory effect of estrogen and progesterone on the growth of T cells. Chinese Journal of Celluar and Molecular Immunology. 2005;21:249–250. [Google Scholar]