Abstract
Background
Malaria is the leading cause of morbidity and mortality in Uganda particularly among children under 5 years of age.
Objectives
The study assessed the knowledge and practices on malaria prevention in 2 rural communities in Wakiso District, Uganda with emphasis on the various prevention methods.
Methods
The study was a cross-sectional survey carried out among 376 households using both quantitative and qualitative methods. Log-binomial regression, chi square and Spearman's rank order correlation were used to test for associations.
Results
The majority of participants (64.6%) had low knowledge on malaria prevention methods, with untreated mosquito nets (81.7%), mosquito coils (36.9%) and insecticide treated nets (29.6%) being the most known methods. Knowledge on malaria prevention methods was associated with age (χ2 = 32.1; p < 0.01), employment status (χ2 = 18.1; p < 0.01), education (χ2 = 20.3; p = 0.01), income (χ2 = 14.5; p = 0.01) and having heard a malaria message in the previous 12 months (χ2 = 92.3; p < 0.01). Households that had at least one mosquito net were 45.5% and net ownership increased with household income. Only 0.5% of the houses had undergone indoor residual spraying in the previous 12 months, while 2.1% had complete mosquito proofing in windows and ventilators to prevent mosquito entry.
Conclusion
There is potential to improve practices on malaria prevention by targeting other methods beyond mosquito nets such as installing proofing in windows and ventilators. The integrated approach to malaria prevention which advocates the use of several malaria prevention methods in a holistic manner should be explored for this purpose.
Keywords: Malaria, prevention, knowledge, practices, integrated approach, Uganda
Introduction
Malaria is a significant public health challenge particularly in sub-Saharan Africa. In 2012, there were an estimated 207 million cases of the disease worldwide with most (80%) being in Africa1. In Uganda, malaria is the leading cause of morbidity and mortality especially among children under five years of age. An estimated 8–13 million cases occur per year and account for approximately 30–50% of outpatient care, 15–20% of health facility admissions and 9–14% of inpatient deaths in the country2. Uganda ranks fourth among the highest malaria burdened countries in the WHO African region based on the estimated number of cases3. In addition to its impact on health, the burden of malaria in the country has also social and economic dimensions. The social dimension includes hindrances to usual social participation due to the disease. The economic costs can be direct including seeking treatment or preventive measures, or indirect ones such as low productivity due to absenteeism from school / work and time lost caring for the sick4.
The current global malaria control core interventions are use of long lasting insecticidal nets (LLINs), indoor residual spraying (IRS), preventive chemotherapy including intermittent preventive treatment among pregnant women, and prompt diagnosis and treatment1. These strategies are also being used in the control of malaria in Uganda2. The use of insecticide treated nets (ITNs) has significantly increased in recent years. Households that own at least one ITN are estimated at 60%, while 45% of Ugandans have access to an ITN5. The Ministry of Health has previously provided free ITNs especially for children under five years of age and pregnant women with over three million nets being distributed since 20066.
However, the disease still causes a great burden to the country's health system7. In addition to the use of ITNs and IRS, other measures can be implemented at household level to reduce mosquitoes that transmit the disease. These measures include installing screens in windows, ventilators, and eaves to prevent entry of mosquitoes; eliminating mosquito breeding sites notably stagnant water for instance through filling with soil; larviciding; and reducing vegetation near houses where mosquitoes habour8,9,10. Several challenges have been identified while seeking health care for malaria (and other illnesses) in Uganda. The challenges include travelling long distances to health facilities and regular stock out of drugs11.
The success of malaria control interventions requires high utilisation of global and national interventions12. However, inadequate knowledge is a main challenge for the appropriate use of these interventions at individual and community levels13. Indeed, knowledge on malaria prevention methods is likely to influence practices by households in the control of the disease. It is therefore important to establish communities' knowledge and practices on malaria control particularly in rural areas which face a high burden of the disease2,14.
This study assessed the knowledge and practices on malaria prevention in two rural communities in Wakiso district, Uganda with emphasis on the various prevention strategies that can be used. The study was carried out as a baseline survey before implementation of a pilot project that promoted the integrated approach to malaria prevention which advocates the use of several malaria prevention methods in a holistic manner at households15.
Methods
Study design and setting
This was a cross-sectional survey carried out in 2011. The study involved 376 households from 2 villages in rural Uganda. The villages were Mayanzi in Entebbe Municipality and Lukose in Ssisa sub-county both in Wakiso District. Wakiso District is located in the central region of the country with a population of 1,315,300 (data from Uganda Bureau of Statistics) and encircles Kampala, the capital city. The villages and households involved in the study were randomly selected using available local data. The lists of households obtained from the village chairpersons were used to systematically select the households involved in the study. The systematic sampling interval used for each village was obtained based on the number of households therein and required sample size. A structured questionnaire and observational checklist were used to collect quantitative data, while 10 key informant interviews provided qualitative data. The key informants were community health workers (CHWs), village leaders, and health practitioners in the study area selected based on their availability and nature of their work.
Data collection and measurements
The questionnaire, which was piloted and translated into the local language, gathered information on malaria prevention and control including participants' knowledge and household practices. The observational checklist assessed the environmental conditions at households that are associated with occurrence of malaria. Use of the checklist included observing the presence of mosquito breeding sites and mosquito proofing in windows, ventilators and open eaves. From the households selected, only one member per household, preferably the household head participated in the study. In situations where the household head was not available or unwilling to take part, any other adult present was included.
The participants provided information on their knowledge on malaria prevention, the methods that were being used by their households to prevent the occurrence of malaria, and their health seeking behaviour when a child under 5 years of age in their household had malaria. The question regarding knowledge on malaria prevention methods had 7 possible responses plus any other mentioned by the participants. The 7 methods regarding knowledge were use of untreated mosquito nets, ITNs, mosquito coils, spraying houses with insecticides, taking preventive medicine, mosquito repellents and draining mosquito breeding sites. Knowledge on malaria prevention was therefore assessed by the number of malaria prevention methods mentioned by the participants, with each method contributing a score of 1 to form an assessment score. Participants with an assessment score of 0 were categorized as having no knowledge; 1 – 3 low knowledge; 4 – 6 medium knowledge and above 6 high knowledge.
The knowledge assessment scores were converted into percentages using the number of participants in each category as the numerator and total number of participants involved in the study as the denominator. Practices on malaria prevention were assessed by the individual methods being used by households to prevent malaria and related risk factors which were obtained from the questionnaire and observational checklist. The practices and risk factors obtained from the questionnaire were use of mosquito nets (treated and untreated), IRS and time of closing windows while those observed were mosquito proofing in windows and ventilators, presence of stagnant water and presence of overgrown vegetation. Key informants provided in-depth data on community knowledge and practices on malaria prevention which was used to supplement the quantitative data.
Data analysis
Quantitative data was entered in SPSS version 17 and transferred to STATA version 12 statistical software for analysis. At univariate level, categorical variables were summarized using frequencies and percentages while continuous ones are presented using mean and inter-quartile range. The chi-square test was used to identify potential factors that may be associated with knowledge on malaria prevention methods among the participants. Since use of LLINs is the most advocated method for malaria prevention globally and nationally, factors associated with ownership of mosquito nets, and the relationship between number of nets owned with household size were identified. For bivariate and multivariate analysis, log-binomial regression model was used to estimate the crude and adjusted prevalence rate ratios at 95% confidence intervals for the factors associated with ownership of mosquito nets. Covariates that were significant at p <0.1 at bivariate level and those with biological plausibility were included in multivariable analysis. Spearman's rank order correlation was run to assess the relationship between number of mosquito nets in households and household size.
From the transcribed qualitative data, summaries were generated highlighting the emerging issues. Coding of the data was then done for all the transcribed work. The coded data was then used to identify the key emerging themes from the qualitative data which was guided by the summaries initially generated. After the themes were identified, the transcribed data was reread to ensure that all coded data was correctly assigned to respective themes.
Ethical considerations
Approval to conduct the research was obtained from the Makerere University School of Public Health Higher Degrees, Research and Ethics Committee. The study was also registered at the Uganda National Council for Science and Technology. The local leaders of the study area were duly informed about the study and permission obtained from them before collecting data. Written informed consent was obtained from participants before they took part in the study.
Results
Socio-demographic characteristics of participants
Majority of participants had gone to school, with 45.2% having attained primary school education as their highest level of education and 39.1% with secondary school education. Nearly half of the participants (49.2%) had an average household monthly income between 20 – 60 US dollars (USD) with only 5.9% earning more than 100 USD. Over half of the participants (50.5%) had household size between 4 – 6 members while most were female (67.6%). The largest number of participants (33.8%) was in the age category of 25 – 34 years (Table 1).
Table 1.
Socio-demographic characteristics of participants
| Variable | Frequency (N = 376) | Percentage (%) |
| Age | ||
| 18–24 | 80 | 21.3 |
| 25–34 | 127 | 33.8 |
| 35–44 | 76 | 20.2 |
| > 44 | 93 | 24.7 |
| Gender | ||
| Male | 122 | 32.4 |
| Female | 254 | 67.6 |
| Religion | ||
| Catholic | 148 | 39.4 |
| Anglican | 116 | 30.9 |
| Muslim | 64 | 17.0 |
| Pentecostal | 39 | 10.4 |
| Other | 9 | 2.4 |
| Occupation | ||
| Farmer | 121 | 32.2 |
| Business | 93 | 24.7 |
| Housewife | 88 | 23.4 |
| Others | 74 | 19.7 |
| Highest level of education | ||
| None | 51 | 13.6 |
| Primary | 170 | 45.2 |
| Secondary | 147 | 39.1 |
| Tertiary / university | 8 | 2.1 |
| Average household monthly income | ||
| (US dollars) | ||
| <20 | 123 | 32.7 |
| 20 –60 | 185 | 49.2 |
| 60 –100 | 46 | 12.2 |
| > 100 | 22 | 5.9 |
| Household size | ||
| 1 –3 | 117 | 31.1 |
| 4 –6 | 190 | 50.5 |
| ≥7 | 69 | 18.4 |
Knowledge on malaria prevention
Majority of participants (89.6%) were aware of malaria being transmitted through mosquito bites. However, other transmission routes of the disease given were cold / changing weather (11.7%), drinking un-boiled water (10.1%) and eating maize (6.9%). Over half of the participants (56.1%) had heard or seen messages about malaria in the previous 12 months. The main source of malaria information was radio (70.6%) while others were health facilities (9.5%), community leaders (5.2%) and television (4.3%).
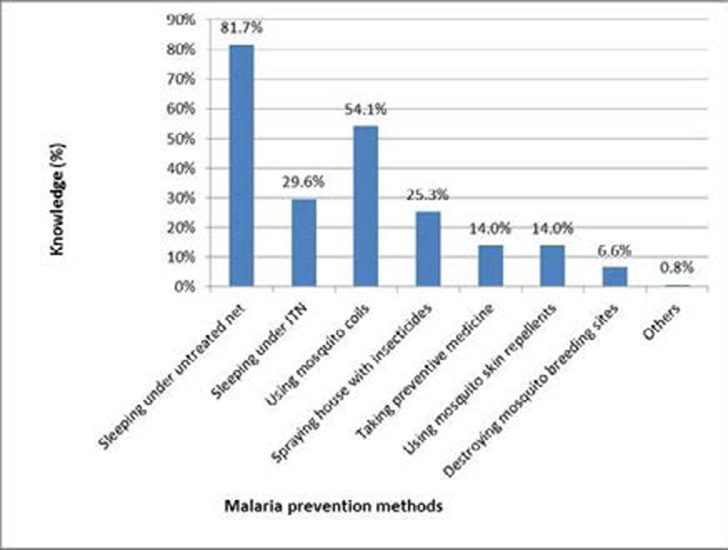
Majority of participants (67.6%) were aware of ways to avoid getting malaria. The most prominent methods were: sleeping under mosquito nets including untreated (81.7%) and insecticide treated ones (29.6%), using mosquito coils (36.9%) and spraying houses with insecticides (17.3%) (Figure 1).
Figure 1.
Knowledge on individual malaria prevention methods
From the assessment score, the majority of participants (64.6%) had low knowledge on malaria prevention methods, with the rest having no (32.5%) or medium (2.9%) knowledge. None of the participants had high knowledge on malaria prevention methods. The factors found to be associated with knowledge on malaria prevention methods were age (χ2 = 32.1; p < 0.01), employment status (χ2 = 18.1; p < 0.01), education (χ2 = 20.3; p = 0.01), income (χ2 = 14.5; p = 0.01) and having heard malaria message in the previous 12 months (χ2 = 92.3; p < 0.01) (Table 2).
Table 2.
Factors associated with knowledge on malaria prevention methods
| Variable | Category | No Knowledge (score 0) n (%) |
Low Knowledge (score 1–3) n (%) |
Medium Knowledge (score 4 – 6) n (%) |
Chi square (χ2) |
P value |
| Age | 18 –24 | 16(20.0) | 62(77.5) | 2(2.5) | 32.1 | 0.00* |
| 25–34 | 26(20.5) | 96(75.6) | 5(3.9) | |||
| 35–44 | 35(46.1) | 40(52.6) | 1(1.3) | |||
| 45+ | 45(48.4) | 45(48.4) | 3(3.2) | |||
| Gender | Male | 45(36.9) | 74(60.7) | 3(2.46) | 1.7 | 0.43 |
| Female | 77(30.3) | 169(66.5) | 8(64.6) | |||
| Employment | Unemployed | 10(13.5) | 59(79.7) | 5(6.8) | 18.1 | 0.00* |
| status | Employed | 112(37.1) | 184(60.9) | 6(2.0) | ||
| Highest level of | None | 22(43.1) | 28(54.9) | 1(1.9) | 20.3 | 0.01* |
| education | Primary | 47(27.7) | 120(70.6) | 3(1.8) | ||
| Secondary | 40(34.5) | 72(62.1) | 4(3.5) | |||
| (ordinary level) |
||||||
| Secondary (advanced) level |
10(32.3) | 20(64.5) | 1(3.2) | |||
| Tertiary / university | 3(37.5) | 3(37.5) | 2(25.0) | |||
| Average | < 20 | 54(43.9) | 65(52.9) | 4(3.3) | 14.5 | 0.01* |
| household | 20 . 60 | 55(29.7) | 126(68.1) | 4(2.16) | ||
| monthly income | > 60 | 13(19.1) | 52(76.5) | 3(4.4) | ||
| (US dollars) | ||||||
| Household size | 1 –3 | 32(27.4) | 80(68.4) | 5(4.3) | 5.3 | 0.26 |
| 4 –6 | 70(36.8) | 117(61.6) | 3(1.58) | |||
| ≥7 | 20(29.0) | 46(66.7) | 3(4.4) | |||
| Heard malaria | Yes | 26(12.3) | 174(82.5) | 11(5.2) | 92.3 | 0.00* |
| message in | No | 96(58.2) | 69(41.8) | 0(0.0) | ||
| previous 12 months |
Statistically significant at p < 0.05
The key informants revealed that although the community was aware of malaria prevention methods such as sleeping under mosquito nets, many families could not afford to implement these measures in their households:
“Basing on the income of people in this village, very few can afford to prevent malaria because they do not have money to buy mosquito nets or screens for their windows and ventilators even when they know such practices would help their families”. Village leader.
Practices on malaria prevention
Households that had at least one mosquito net for use in the prevention of malaria were 45.5%, with the mean number of nets being 2.11 (inter quartile range, IQR 1–3) compared to the mean household size of 4.69 (IQR 3–6). The proportion of population who slept under a mosquito net the night before the survey was 28.4% compared to 43.3% among children under 5 years of age. There was a positive correlation between household size and number of mosquito nets owned (Spearman's correlation coefficient = 0.405, p <0.01). Participants aged 35–44 years were less likely to report having a mosquito net in their household compared to those aged 18–24 years (Adjusted Prevalence Rate Ratio — APRR 0.7, Confidence Interval – CI 0.51 – 0.92). Similarly, participants aged 45 or older were less likely to report having a mosquito net in their household compared to those aged 18–24 years (APRR 0.4, CI 0.27– 0.66). Participants who were employed were more likely to report having a mosquito net in their households compared to those who were unemployed (APRR 1.2, CI 1.01 – 1.53). Participants whose households had an average monthly income between 20 – 60 US dollars were more likely to report having a mosquito net in their households compared to those earning less than 20 dollars (APRR 1.5, CI 1.05 – 2.03). Similarly, participants whose households had an average monthly income above 60 US dollars were more likely to report having a mosquito net in their households compared to those earning less than 20 dollars (APRR 2.1, CI 1.47 – 2.91) (Table 3).
Table 3.
Factors associated with ownership of mosquito nets in households
| Variable | Category | Ownership | Crude PRR^ | Adjusted PRR | p-value | |
| net | (95% CI^^) | (95% CI) | ||||
| N=376 | ||||||
| No | Yes | |||||
| n=205 | n=171 | |||||
| Gender | Male | 78 | 44 | Ref | Ref | |
| Female | 127 | 127 | 1.4(1.06–1.81)* | 1.3(0.99–1.62) | 0.06 | |
| Age | 18–24 | 34 | 46 | Ref | Ref | |
| 25–34 | 52 | 75 | 1.0(0.81–1.30) | 1.0(0.79 –1.22) | 0.89 | |
| 35–44 | 48 | 28 | 0.6(0.45–0.91)* | 0.7(0.51 –0.92)* | 0.01 | |
| 45+ | 71 | 22 | 0.4(0.27–0.62)* | 0.4(0.27 –0.66)* | 0.00 | |
| Highest level | None | 32 | 19 | Ref | Ref | |
| of educational | Primary | 94 | 76 | 1.2(0.81–1.78) | 0.9(0.67 –1.26) | 0.61 |
| Ordinary level | 56 | 60 | 1.4(0.93–2.07) | 1.0(0.71 –1.31) | 0.84 | |
| Advanced level and | 23 | 16 | 0.8(0.52 –1.22) | 0.29 | ||
| tertiary | 1.1(0.66–1.85) | |||||
| Employment | Unemployed | 127 | 82 | Ref | Ref | |
| status | Employed | 78 | 89 | 1.4(1.09–1.69)* | 1.2(1.01 – 1.53)* | 0.04 |
| Average | < 20 | 87 | 36 | Ref | Ref | |
| monthly household | 20 –60 | 93 | 92 | 1.7(1.25–2.32)* | 1.5(1.05–2.03)* | 0.03 |
| income (US dollars) | > 60 | 25 | 43 | 2.2(1.55–3.00)* | 2.1(1.47 –2.91)* | 0.00 |
PRR - Prevalence rate ratio
CI - Confidence Interval
Statistically significant at 95% confidence interval
Key informant interviews revealed that the communities had previously received support from the Government in form of ITNs. However, these were not sufficient as noted below:
“We received mosquito nets from Government. However, they were given to only households with children under 5 years and pregnant women but still, not all households that had children or pregnant women received these nets”. Health worker.
Although it was generally appreciated that use of ITNs played a big role in the prevention of malaria, some of the challenges faced by the community in using them were poverty and large family size:
“Most families in this village have many members therefore based on this fact, they cannot buy insecticide treated nets for each person in the family.” Village leader.
“Due to poverty, many households cannot afford to buy mosquito nets and mainly use those that were provided by the government. Some families cannot even afford to buy drugs when members have malaria in addition to not being able to buy screening for their windows and ventilators to prevent mosquitoes entering their houses.” Health worker.
Only 0.5% of the participants' houses had undergone IRS in the previous 12 months and this had been done by household members. Only 2.1% houses had complete mosquito proofing in windows and ventilators to prevent mosquito entry. Stagnating water was found around 17.6% of the houses while vessels that could potentially hold water for mosquito breeding were found in 37.2% households (Table 4). In addition to the stagnant water in compounds, it was established that numerous persistent pools of water in the community existed that could be used by mosquitoes for breeding: “There are very many mosquito breeding places in this area especially those resulting from excavation of clay for brick making. These breeding sites greatly contribute to the many cases of malaria in our community.” CHW.
Table 4.
Malaria prevention practices and risk factors at households
| Variable | N = 376 | Percentage (%) |
| Presence of at least one mosquito net | 171 | 45.5 |
| Used indoor residual spraying in previous 12 months | 2 | 0.5 |
| Presence of mosquito proofing in windows and | 8 | 2.1 |
| ventilators | ||
| Presence of stagnant water in compound | 66 | 17.6 |
| Presence of vessels around house that can potentially | 140 | 37.2 |
| hold water for mosquito breeding | ||
| Time of closing windows on houses | ||
| Before 6 pm | 146 | 38.8 |
| After 6 pm | 178 | 47.3 |
| Not applicable | 52 | 13.8 |
| Presence of overgrown vegetation within 5 meters of | 161 | 42.8 |
| house |
In 42.8% of households, overgrown vegetation was found within 5 meters of house. Among households that opened the windows on their houses (86.2%), nearly half (47.3%) closed them after 6.00pm (Table 4).
Health seeking practices
Among the participants, 30.6% had children under 5 years in their households who had had a fever 2 weeks prior to data collection. Among these, 85.2% sought treatment from various sources, the main ones being Government health facilities (59.1%), community health workers (33.7%) and private facilities (21.4%). Treatment was first sought mainly from government facilities (53.1%). Only 29.6% of the households sought treatment for the sick children on the very day the fever began. The rest sought treatment 1 – 3 days (61.2%) or more than 3 days (9.2%) after onset of the fever. Among those who did not seek treatment, the main reasons given were the child not being very ill (23.5%), having no money (23.5%), and waiting for the child's parent (11.8%). Most participants (62.2%) had travelled between 1 — 4 kilometers to seek treatment when children in their household were sick.
The rest travelled less than 1 kilometer (23.5%) or more than 5 kilometers (9.2%). The long distances that the community had to travel to seek healthcare was a significant challenge:
“One of the main challenges we face in seeking health services is the distance we have to cover to get to health facilities. Due to having few Government health facilities, people have to travel very long distances to get treatment. Families therefore spend a lot of money on transportation alone.” Village leader.
Majority of participants 62.5% were aware of the existence of community health workers in form of village health teams (VHTs) in their respective areas who distributed malaria medicines. However, among these, 62.7% did not know whether the VHTs had malaria medicine available at the time while only 9.7% confirmed existence of the medicine. The number of VHTs distributing malaria medicine in the community was found to be insufficient:
“We have only 4 Government trained VHTs for the whole village. However, it is only 2 of these volunteers who were given malaria drugs for use by children when sick. Due to the many malaria cases among children, this medicine is usually used up in a short time leaving no medicine with these community health workers for long periods”. Village leader.
Discussion
The study established that knowledge on malaria prevention methods was low. However, participants were specifically highly aware of sleeping under mosquito nets to prevent malaria. High knowledge on mosquito nets can be attributed to the Ministry of Health's extensive campaign on increasing awareness and use of ITNs in recent years, including free distribution to vulnerable groups of children and pregnant women as established by this study. However, beyond the ITNs provided by the Government, many families could not afford to buy such nets which directly relates to the low income levels in rural areas in Uganda as established by this and other studies16,17. Poverty not only affected use of malaria prevention methods in this study but also health seeking behaviours which has been documented in other studies18,19. Since poverty remains high in rural areas of Uganda, the Government's strategy of free distribution of ITNs is likely to greatly benefit such communities. However, some studies conducted in other parts of Africa have shown misuse of received nets including being used for fishing20,21. Therefore, an all-encompassing approach including health education and targeting other malaria prevention methods is recommended.
Knowledge on malaria prevention methods was associated with age, employment status, education, income and having heard malaria message in the previous 12 months. People who are educated are expected to have had more exposure to malaria prevention methods compared to those who are not22. Since education is a contributing factor to employment hence income23, the association of these factors to knowledge on malaria is justified. The strong association between knowledge on malaria and having heard malaria message is an indication that increased publicity could contribute towards improving malaria prevention practices in Uganda and beyond24.
With less than half of the households owning at least one mosquito net, this most advocated method of malaria prevention was being underutilized. However, it is possible that some participants may have under reported the nets their households had in anticipation of being given ITNs if they had a few or none. It was evident in this study that households gave priority to children under 5 years of age regarding sleeping under mosquito nets, a category most affected by malaria1. Indeed, 43.3% of children under 5 years of age slept under a mosquito net the night before the survey compared to 28.4% among the general population. The estimated number of households owning at least one ITN nationally is 60%, with an average of 1.3 ITNs5. The positive correlation between household size and number of nets owned (Spearman's correlation coefficient = 0.405, p <0.001) could be attributed to households with more children having received more nets from the Government.
However, with the mean number of nets being 2 compared to the mean household size of 5, the available nets among households were clearly insufficient for the members. Ownership of nets increased with household income as established by other studies25,26. This finding is logical as nets are costly and may not be affordable by families with low income. Indeed, participants who were employed and had an income were more likely to own a net in their household as established by this study. The negative association between ownership of nets and participants who were above 34 years could be due to such households having fewer children hence receiving less free nets from the Government. Indeed, nets were provided to households with children under 5 years and/or pregnant women. The current universal coverage campaign by the Ministry of Health where one net is to be given to every two people in a household is likely to benefit all age groups. In this campaign, an estimated 21 million LLINs are to be distributed countrywide27.
Besides mosquito nets, there was low knowledge and utilization of other malaria prevention methods including IRS which is a key national and global strategy7,12. Wakiso district in central Uganda where this study was conducted was not among the areas where IRS was implemented by the Government which targeted mainly the northern region of the country6. In addition, the use of IRS has been found to have several challenges elsewhere including insecticide smell, mess left by the sprayers, inconvenience of removing household items from houses before spraying, increased prevalence of other insects, perceived ineffectiveness and side effects28,29,30. Installing proofing in windows and ventilators of houses was also underutilized as has been found in a related study31. Although proofing of windows, ventilators and open eaves has historically been used to prevent entry of mosquitoes in houses, the method has been ignored in many communities32. In addition to promotion of use of ITNs and IRS, advocating the use of other malaria prevention methods is important in reducing the burden of the disease in endemic countries. Indeed, the integrated approach to malaria prevention promoted in the study community after conducting this survey had immediate benefits such as reduced presence of mosquitoes in houses15. It is planned that the long term public health impact of the integrated approach in the study community will be assessed more than 2 years after implementing the project.
This study re-emphasizes the high utilisation of Government health facilities and community health workers in rural communities for the treatment of malaria among children under 5 years of age. However, the challenges of accessing these services established in this study included long distance to facilities, insufficient number of VHTs and stock-out of drugs among them. Similar challenges affecting utilisation of health services have been found in other studies carried out in Uganda and beyond33,34. These health system challenges greatly affect health outcomes particularly in rural communities which are most at need of health services11. Therefore to improve the health of rural populations, concerned authorities such as ministries responsible for health need to address these challenges.
Limitations
A major limitation of this study was some of the malaria prevention practices such as use of mosquito nets and IRS were reported as they could not be observed. Nevertheless, for the malaria prevention methods that could be seen including mosquito proofing in windows and ventilators, these were observed with guidance of an observational checklist which is indeed a strength of the study. Another limitation is that the study was conducted in only 2 villages where the pilot project was to be implemented hence a relatively small sample size. This may have affected some statistical tests, and the results may not be generalised to a wider geographical area. Nevertheless, the qualitative data suitably supplemented the quantitative one and the findings can be used to inform future studies.
Conclusion
Besides mosquito nets, knowledge and practices on other malaria prevention methods was low in this study. There is potential to improve practices of malaria prevention by targeting other methods beyond ITNs, such as installing proofing in windows and ventilators. The integrated approach to malaria prevention which advocates the use of several malaria prevention methods in a holistic manner should be explored for this purpose.
Acknowledgements
We thank the Welsh Government under the Wales4Africa Health Links Grant Scheme 2011–12 for funding the malaria project. This investigation also received financial support from TDR, the Special Programme for Research and Training in Tropical Diseases, co-sponsored by UNICEF, UNDP, the World Bank and WHO. Our appreciation also goes to the entire project team (UK and Uganda), village leaders, mobilizers, local authorities, research assistants and community for their contribution towards the study.
Competing interests
The authors declare that they have no competing interests.
References
- 1.WHO, author. World Malaria Report 2013. Geneva: 2013. [Google Scholar]
- 2.UBOS - Uganda Bureau of Statistics, author. Uganda Malaria Indicator Survey 2009. Kampala, Uganda: 2010. [Google Scholar]
- 3.WHO, author. World Malaria Report 2012. Geneva: 2012. [Google Scholar]
- 4.Orem JN, Kirigia JM, Azairwe R, Kasirye I, Walker O. Impact of malaria morbidity on gross domestic product in Uganda. Int Arch Med. 2012;5(1):12. doi: 10.1186/1755-7682-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UBOS - Uganda Bureau of Statistics, author. Uganda Demographic and Health Survey 2011. UBOS and Calverton, Maryland: ICF International Inc.; 2012. [Google Scholar]
- 6.Yeka A, Gasasira A, Mpimbaza A, Achan J, Nankabirwa J, Nsobya S, et al. Malaria in Uganda: challenges to control on the long road to elimination: I. Epidemiology and current control efforts. Acta Trop. 2012;121(3):184–195. doi: 10.1016/j.actatropica.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.MOH - Ministry of Health, Uganda, author. Health Sector Strategic Plan III 2010/11–2014/15. Kampala, Uganda: 2010. [Google Scholar]
- 8.Walker K, Lynch M. Contributions of Anopheles larval control to malaria suppression in tropical Africa: review of achievements and potential. Med Vet Entomol. 2007;21(1):2–21. doi: 10.1111/j.1365-2915.2007.00674.x. [DOI] [PubMed] [Google Scholar]
- 9.CDC, author. Anopheles mosquitoes. Division of parasitic diseases. 2008. [5th August 2009]. http://www.cdc.gov/malaria/biology/mosquito/
- 10.Ng'ang'a PN, Shililu J, Jayasinghe G, Kimani V, Kabutha C, Kabuage L, Kabiru E, Githure J, Mutero C. Malaria vector control practices in an irrigated rice agro-ecosystem in central Kenya and implications for malaria control. Malar J. 2008;7:146. doi: 10.1186/1475-2875-7-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kiwanuka S, Ekirapa E, Peterson S, Okui O, Rahman MH, Peters D, et al. Access to and utilization of health services for the poor in Uganda: a systematic review of available evidence. Trans R Soc Trop Med Hyg. 2008;102(11):1067–1074. doi: 10.1016/j.trstmh.2008.04.023. [DOI] [PubMed] [Google Scholar]
- 12.WHO, author. Indoor residual spraying. Use of indoor residual spraying for scaling up global malaria control and elimination. Global Malaria Programme; 2006. [Google Scholar]
- 13.Gobena T, Berhane Y, Worku A. Women's knowledge and perceptions of malaria and use of malaria vector control interventions in Kersa, Eastern Ethiopia. Glob Health Action. 2013;6:20461. doi: 10.3402/gha.v6i0.20461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keiser J, Utzinger J, Caldas de Castro M, Smith TA, Tanner M, Singer BH. Urbanization in sub-saharan Africa and implication for malaria control. Am J Trop Med Hyg. 2004;71(2 Suppl):118–127. [PubMed] [Google Scholar]
- 15.Musoke D, Karani G, Ssempebwa JC, Musoke MB. Integrated approach to malaria prevention at household level in Uganda: experiences from a pilot project. Malar J. 2013;12:327. doi: 10.1186/1475-2875-12-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mbonye AK, Neema S, Magnussen P. Preventing malaria in pregnancy: a study of perceptions and policy implications in Mukono district, Uganda. Health Policy Plan. 2006;21(1):17–26. doi: 10.1093/heapol/czj002. [DOI] [PubMed] [Google Scholar]
- 17.Welch K, Fuster M. Barriers in access to insecticide-treated bednets for malaria prevention: an analysis of Cambodian DHS data. J Vector Borne Dis. 2012;49(1):1–7. [PubMed] [Google Scholar]
- 18.Tumwesigire S, Watson S. Health seeking behavior by families of children suspected to have malaria in Kabale: Uganda. Health Sci. 2002;2(3):94–98. [PMC free article] [PubMed] [Google Scholar]
- 19.Das A, Das Gupta RK, Friedman J, Pradhan MM, Mohapatra CC, Sandhibigraha D. Community perceptions on malaria and care-seeking practices in endemic Indian settings: policy implications for the malaria control programme. Malar J. 2013;12:39. doi: 10.1186/1475-2875-12-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Minakawa N, Dida GO, Sonye GO, Futami K, Kaneko S. Unforeseen misuses of bed nets in fishing villages along Lake Victoria. Malar J. 2008;7:165. doi: 10.1186/1475-2875-7-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hopkin M. The big push. Nature. 2008;451:1047–1049. doi: 10.1038/4511047a. [DOI] [PubMed] [Google Scholar]
- 22.Akinleye SO, Ajayi IO. Knowledge of malaria and preventive measures among pregnant women attending antenatal clinics in a rural local government area in Southwestern Nigeria. World Health Popul. 2011;12(3):13–22. doi: 10.12927/whp.2011.22172. [DOI] [PubMed] [Google Scholar]
- 23.Gregorio JD, Lee J. Education and Income Inequality: New Evidence From Cross-Country Data. Review of Income and Wealth. 2002;48:395–416. [Google Scholar]
- 24.Rhee M, Sissoko M, Perry S, Dicko A, McFarland W, Doumbo O. Malaria prevention practices in Mopti region, Mali. East Afr Med J. 2005;82(8):396–402. doi: 10.4314/eamj.v82i8.9323. [DOI] [PubMed] [Google Scholar]
- 25.Kaliyaperumal K, Mengistie E, Dagnew Z, Deboch B. Examining household possession and willingness to pay for the retreatment of ITNs with insecticides among local residences in a malaria endemic area. East Afr J Public Health. 2010;7(4):305–310. doi: 10.4314/eajph.v7i4.64748. [DOI] [PubMed] [Google Scholar]
- 26.Biswas AK, Hutin YJ, Ramakrishnan R, Patra B, Gupte MD. Increased financial accessibility and targeted education messages could increase ownership and use of mosquito nets in Purulia District, West Bengal, India. Trans R Soc Trop Med Hyg. 2010;104(6):423–428. doi: 10.1016/j.trstmh.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 27.MOH - Ministry of Health, Uganda, author. Distribution of long lasting treated mosquito nets. Kampala, Uganda: 2014. [25th January 2014]. http://health.go.ug/mohweb/?p=1350. [Google Scholar]
- 28.Rodriguez AD, Penilla RP, Rodriguez MH, Hemingway J, Trejo A, Hernandez-Avila JE. Acceptability and perceived side effects of insecticide indoor residual spraying under different resistance management strategies. Salud Publica Mex. 2006;48:317–324. doi: 10.1590/s0036-36342006000400006. [DOI] [PubMed] [Google Scholar]
- 29.Govere J, Durrheim D, la Grange K, Mabuza A, Booman M. Community knowledge and perceptions about malaria and practices influencing malaria control in Mpumalanga Province, South Africa. S Afr Med J. 2000;90(6):611–616. [PubMed] [Google Scholar]
- 30.Kaufman MR, Rweyemamu D, Koenker H, Macha J. “My children and I will no longer suffer from malaria": a qualitative study of the acceptance and rejection of indoor residual spraying to prevent malaria in Tanzania. Malar J. 2012;11:220. doi: 10.1186/1475-2875-11-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Musoke D, Musoke MB, Nsubuga W. Factors associated with prevention of malaria and other diseases transmitted by mosquitoes at household level in Wakiso district, Uganda. Journal of Environmental Health Research. 2013;13(1):59–67. [Google Scholar]
- 32.Lindsay SW, Emerson PM, Charlwood JD. Reducing malaria transmission by mosquito-proofing homes. Trends Parasitol. 2002;18(11):510–514. doi: 10.1016/s1471-4922(02)02382-6. [DOI] [PubMed] [Google Scholar]
- 33.Kiguli J, Ekirapa-Kiracho E, Okui O, Mutebi A, Macgregor H, Pariyo GW. Increasing access to quality health care for the poor: Community perceptions on quality care in Uganda. Patient Prefer Adherence. 2009;3:77–85. doi: 10.2147/ppa.s4091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Smith N, Obala A, Simiyu C, Menya D, Khwa-Otsyula B, O'Meara WP. Accessibility, availability and affordability of anti-malarials in a rural district in Kenya after implementation of a national subsidy scheme. Malar J. 2011;10:316. doi: 10.1186/1475-2875-10-316. [DOI] [PMC free article] [PubMed] [Google Scholar]