Abstract
Effective care coordination is a key quality and safety strategy for populations with chronic conditions, including children with medical complexity (CMC). However, gaps remain in parent report of the need for care coordination help and receipt of care coordination help. New models must close this gap while maintaining family-centered focus. A three-armed randomized controlled trial conducted in an established medical home utilized an advanced practice registered nurse intervention based on Presler’s model of clinic-based care coordination. The model supported families of CMC across settings using telephone only or telephone and video telehealth care coordination. Effectiveness was evaluated from many perspectives and this paper reports on a subset of outcomes that includes family-centered care (FCC), need for care coordination help and adequacy of care coordination help received. FCC at baseline and end of study showed no significant difference between groups. Median FCC scores of 18.0–20.0 across all groups indicated high FCC within the medical home. No significant differences were found in the need for care coordination help within or between groups and over time. No significant difference was found in the adequacy of help received between groups at baseline. However, this indicator increased significantly over time for both intervention groups. These findings suggest that in an established medical home with high levels of FCC, families of CMC have unmet needs for care coordination help that are addressed by the APRN telehealth care coordination model.
Keywords: Care coordination, Children with medical complexity, Family-centered care, Advance practice registered nurse, Telehealth, Medical home
Introduction
The recommended approach for primary care of all children is the medical home [1]. Care coordination is an essential component of this model [2, 3] and a key quality and safety strategy for populations with chronic conditions [4–7]. The Maternal Child Health Bureau defines care coordination as, “a process that links children with special health care needs and their families to services and resources in a coordinated effort to maximize the potential of children and provide them with optimal health care” [8]. Children with medical complexity (CMC) [9] have chronic conditions involving multiple body systems, multiple service providers, rely intermittently or chronically on life-sustaining technology and high health resource utilization [9, 10]. CMC represent <1 % of the total population of children [11, 12], but their health care expenditures accounted for nearly one-third of pediatric health care costs in a Canadian province [12] and four times the cost of non-CMC in a panel of US children [13]. Life expectancy of CMC is increasing due to improved health care interventions [14] and their medical and social complexity can intensify coordination needs across settings and over time [15]. The purpose of this paper is to present preliminary evidence for supplementing a medical home for CMC with an advanced practice registered nurse (ARPN) model of telehealth care coordination.
The primary care provider (PCP), historically a physician, directs coordination of a child’s care [16] which encompasses proactive and comprehensive care for acute and chronic conditions, communication between medical home, family, other providers and community resources, and measurement and improvement of health and quality of life outcomes [17, 18]. Coordinating care across diverse providers and services has shown improved clinical, social and emotional outcomes [4, 7] and reduced costs [19–21] for CMC. Care coordination requires a broad range of competencies and the American Association of Pediatricians highlights the importance of identifying “competencies, job descriptions, and functions in the physician-led team” [18] providing care for the child and their family in and outside the medical home. A team approach with active involvement of families and children, and a non-physician care coordinator assuming responsibility for the broad range of tasks has been recommended [22].
APRNs are licensed providers building on competencies of registered nurses (RN) via graduate-level course work and clinical experience [23]. APRN depth and breadth of knowledge, synthesis of data, and complexity of skills results in role autonomy as an independent practitioner who can assess, diagnosis, and manage patient populations with autonomous pharmacologic and non-pharmacologic interventions [23]. Unique scope of practice, critical thinking and problem-solving orientation provides a framework to address health and psychosocial contexts [24–26], making the APRN ideally suited for a high-intensity family-centered care (FCC) coordination role [27, 28]. Activities of APRN care coordinators described elsewhere include acute and chronic condition management, care coordination with providers, parental education and support, care coordination with community resources and discharge planning [29]. Health care teams with APRNs coordinating care for CMC have demonstrated improved outcomes and lower costs, particularly through a reduction in hospital length of stay [30–34].
The use of telehealth for care coordination is increasing. Telehealth is “any electronic medium to mediate or augment clinical consultations; it can be simultaneous (for example, telephone or videoconference) or store and forward (an email with an attached message)” [35]. Tele-health facilitates clinic-home and clinician-consumer communication and the use of telehealth to support management of chronic health conditions outside clinic visits is expanding [36]. Telephone and video telehealth care management of adults showed improved health outcomes, increased patient satisfaction and reduced costs [37–40], and care coordination for CMC delivered via telephone telehealth showed similar results [31, 32, 34].
FCC is a preferred approach to partnering with families within the pediatric medical home [3, 21]. The National Quality Forum (NQF) identified FCC as a practice standard for care coordination [41] and this element is a core outcome endorsed by the Maternal and Child Health Bureau and measured by the NS-CSHCN [42]. FCC coordination recognizes the family as partner and primary decision-maker in all aspects of a child’s care [43]. It is proactive, based on developmental needs of the child and family, and includes educating all persons involved with the child on planned and emergency transitions of care [28]. The intensity and type of FCC coordination needed by CMC is related to the complexity of their physical and psychosocial conditions [15, 44]. Families report their greatest challenge as the stress of coordinating multiple providers [45] and the lack of communication between services and providers [46]. Effectiveness measures of FCC coordination should include broader measurement of care coordination need.
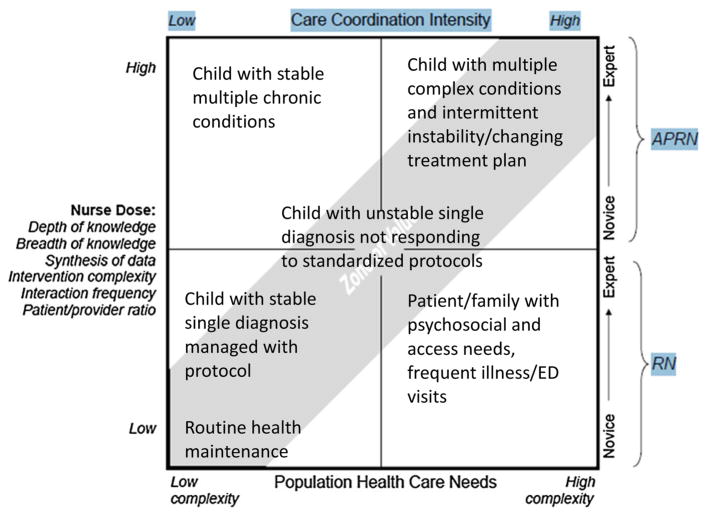
This paper reports only on FCC outcomes from a 4-year three-arm randomized controlled trial testing effectiveness of a medical home based care coordination model for CMC, delivered by an APRN via telehealth. An APRN care coordinator role was selected because advanced scope of practice, and clinical autonomy align with the complex health and care coordination needs of CMC (Fig. 1) [15, 23]. We hypothesized that the need for care coordination help would not differ between study groups, but FCC and adequacy of care coordination help received would increase for intervention groups.
Fig. 1.
Zone of value© for matching nurse scope of practice with population health care. From: Looman et al. [15]
Methods
Setting and Subjects
Institutional Review Boards approved this study. The setting was a large, urban, general pediatrics clinic affiliated with a non-profit children’s hospital. The clinic serves approximately 800 CMC who are enrolled in a state certified medical home conforming to American Academy of Pediatrics (AAP) guidelines [47]. All CMC enrolled in the medical home were screened for eligibility criteria which included age, parental language and condition severity. A 2 year age minimum excluded neonates who resolve conditions with age and a 15 year age maximum avoided transition to adult services. English speaking parent/ guardian eliminated variability in data collection. Meeting four of five CSHCN Screener [48] criteria ensured a study cohort reflecting the CMC definition. Parents of the 375 eligible children received recruitment information by mail or during clinic visits. Interested parents met with study staff who explained the study protocol and participation risks and benefits. Written informed consent to participate was provided by 172 families. Nine subjects withdrew prior to randomization. This paper reports on 163 randomized subjects.
Study Design
TeleFamilies is a 4-year three-arm randomized controlled trial testing effectiveness of increasing levels of telehealth technology and care coordination, delivered by a clinic-based APRN, on healthcare service utilization (HCSU) and secondary satisfaction, FCC and quality of life outcomes. The study has 80 % power to detect a mean difference in the primary outcome (HCSU). Study participation was 30 months. Upon completion of a 6-month baseline period, subjects were randomized to one of three care coordination groups: standard (control) group (n = 55); APRN intervention via telephone group (n = 54) or APRN intervention via telephone and interactive video group (n = 54). Randomization was stratified by age (2–5, 6–12 and 13–15 years).
The clinic in which the study was conducted utilized a medical home model of care coordination [16], with the PCP managing and coordinating overall care. A typical clinic visit included PCP review of the electronic medical record (EMR), parent history of recent clinical encounters, assessment, diagnosis and adjustment of the plan of care. After the clinic visit, the PCP directed clinic staff (RNs, LPNs, schedulers, medical assistants and referral coordinators) to follow-up on orders for procedures, treatment changes, referrals to sub-specialists, and community resources. Between clinic visits, questions from families and external entries were routed to available staff rather than a single contact familiar with the child and family. An off-site triage service handled after-hours/weekend concerns. All subjects in the control group received this model of care coordination.
Intervention
For both intervention groups, the model of PCP managing and coordinating overall care remained unchanged, along with the after-hours/weekend off-site triage service. What differed for intervention subjects was assignment of a single clinic-based APRN care coordinator who provided a consistent point of contact that supported cumulative knowledge of the child’s clinical and psychosocial course, and who worked collaboratively with each child’s PCP before, during, after and between clinic visits. Before clinic visits, the APRN summarized clinical and psychosocial needs addressed since the last clinic visit and provided PCP and family with a common understanding of interim needs and treatments without extensive medical record review. During clinic visits, the APRN advocated patient/families preferences in the plan of care. After and between clinic visits, the APRN followed-up on all coordination needs. The use of a single APRN ensured fidelity of the intervention.
Care coordination activities with parents were conducted primarily via telehealth and included acute and chronic condition management, and support, education and follow-up. Parents of subjects in the telephone intervention group used telephone telehealth to conduct these activities, while parents of subjects in the video intervention group used telephone and interactive clinic-home video. Video visits utilized a HIPAA-compliant, web-based platform (Virtual Interactive Families©, Cedar Falls, IA) and occurred whenever the APRN or parent felt video would enhance communication, diagnosis and/or treatment. Examples include skin, respiratory and acute injury assessments, and observing/teaching parents and home health nurses during treatments (i.e. wound care). The APRN also met with families during PCP clinic visits to maintain the coordination relationship and address needs, and during hospitalizations to assess the current plan of care and make adjustments for discharge transition. Examples include medication/treatment changes, feeding plan or equipment changes, and intensity of home care services.
Care coordination activities with the interdisciplinary medical home team were conducted in-person and via EMR communication. The APRN was a consistent single point of contact for coordinating care with other providers, payers and community resources (schools, home care, equipment/supply vendors and community services) and care coordination activities were conducted via telephone or mail. The APRN provided care coordination in other service delivery settings which included individual education plan (IEP) meetings, visits to home care agencies and equipment suppliers and communicating plan of care changes with schools and home care agencies.
Measures
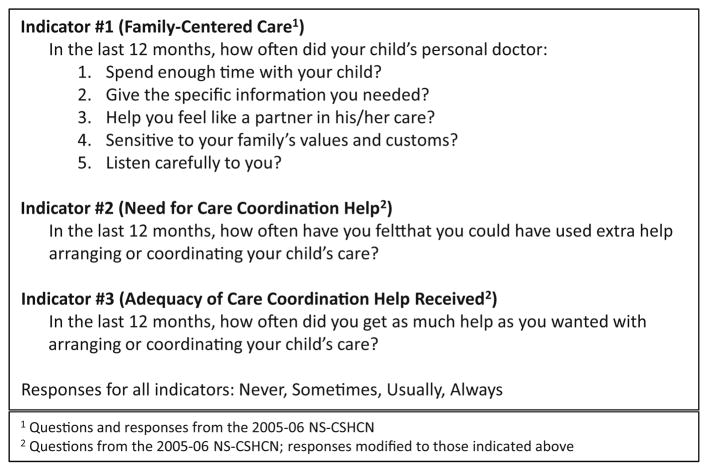
Effectiveness of the care coordination model was measured using three outcome indicators: 5-item FCC subset, need for care coordination help, and adequacy of care coordination help received. All three indicators were taken from the 2005–2006 NS-CSHCN [49], and appear in Fig. 2. Validity and reliability of all indicators has been reported [50, 51]. Because the 5-item FCC [49] subset does not measure the effect of non-physician care coordinators, two additional indicators were included: family need for care coordination help and adequacy of care coordination help received [49]. The need for care coordination help is our relabeling of ‘could of used extra help arranging or coordinating care’ and responses of usually or always was categorized as needing help. Adequacy of care coordination help received is our relabeling of ‘getting as much help as wanted arranging or coordinating care’ and responses of usually or always was categorized as adequacy of help received.
Fig. 2.
Indicators of family-centered care coordination effectiveness
Data Collection
Study data were collected by self-report from the parent or legal guardian of children enrolled in the study, using a paper survey booklet that contained five standard validated surveys and a subset of questions from the 2005–2006 NS-CSHCN [49]. Demographic data was abstracted from the child’s EMR. Only the subset from the NS-CSHCN is reported in this paper. Future papers will report findings from the standard surveys.
The survey booklet and an addressed, stamped return envelope were distributed by mail at three distinct data collection points: completion of baseline period; completion of first randomization year; completion of second randomization year/end of study. Over the 30 month study, 14 subjects withdrew (control = 7, telephone = 4, video = 3) and one subject died (control).
Data Analysis
Demographic data were compared for differences between groups at baseline. FCC coordination effectiveness was tested using data collected for the three outcome indicators (FCC, need for care coordination help, and adequacy of care coordination help received). The null hypothesis for each outcome indicator stated no change within group across time, and no change between groups across time. Descriptive and inferential statistical analysis was conducted with SAS V9.3 (SAS Institute Inc., Cary, NC).
Analysis of variance (ANOVA) and analysis of covariance (ANCOVA) tested for differences in the 5-item FCC subset at baseline and post-baseline, respectively. Pairwise comparisons (with Tukey–Kramer multiple comparison adjustments) were made if the overall ANOVA or ANCOVA was statistically significant. Fisher’s exact test compared the need for and adequacy of care coordination between the three groups, at baseline, year one and year two. McNemar’s test assessed changes in need for and adequacy of care coordination help within each group, at baseline versus year one and baseline versus year two. A generalized estimating equations (GEEs) model, tested need for and adequacy of care coordination between the groups over time. GEEs allow for modeling repeated measures data and baseline, year one and year two data were included. A P value <0.05 is considered statistically significant and rejects the null hypothesis.
Results
Subjects in the video group used telephone telehealth for the majority of their care coordination interactions with the APRN; on average, video telehealth was used only once by each subject. Demographic information of subjects appears in Table 1 and demographic information of survey respondents (parent/guardian) appears in Table 2. The average age of children enrolled in the study was 7.2 years. The only difference between subject and survey respondent groups at baseline was parent report of health severity. This difference could result from non-response bias of the control group.
Table 1.
Demographics of telefamilies subjects
| Control | Telephone | Video | P value* | |
|---|---|---|---|---|
| Data obtained from medical recorda | ||||
| Gender | ||||
| Male (female) | 31 (24) | 33 (21) | 26 (28) | 0.4085 |
| Age at start of intervention, mean (SD) | 7.1 (4.3) | 7.0 (3.9) | 7.6 (4.3) | 0.7265 |
| 2–5 years | 23 | 23 | 23 | |
| 6–12 years | 24 | 23 | 22 | |
| 13–15 years | 8 | 8 | 9 | |
| Primary insurance | 0.3630 | |||
| Private | 31 | 30 | 24 | |
| Public | 23 | 24 | 30 | |
| Uninsured/self pay | 1 | 0 | 0 | |
| Condition complexityb | 1.0000 | |||
| Single complex chronic condition | 7 | 7 | 7 | |
| Multiple complex chronic conditions | 48 | 47 | 47 | |
| Neurologic impairment | 0.7003 | |||
| Yes (no) | 47 (8) | 46 (8) | 43 (11) | |
| Need for life-sustaining technology assistanceb | ||||
| Yes (no) | 25 (30) | 22 (32) | 29 (25) | 0.4109 |
| Data obtained from baseline surveyc | ||||
| Race | 0.0871 | |||
| White | 30 | 33 | 35 | |
| Black or African American | 2 | 8 | 10 | |
| Asian | 4 | 1 | 3 | |
| Multiracial | 1 | 8 | 4 | |
| Ethnic background | 0.9066 | |||
| Hispanic (non-Hispanic) | 4 (33) | 7 (43) | 8 (44) | |
| Parent report of health problem severity | 0.0280 | |||
| Minor | 2 | 8 | 9 | |
| Moderate | 16 | 26 | 23 | |
| Severe | 14 | 16 | 20 | |
| Don’t know | 5 | 0 | 0 | |
| Parent report of health care needs stability | 0.9476 | |||
| Change all the time | 11 | 17 | 16 | |
| Change once in a while | 15 | 20 | 20 | |
| Are usually stable | 10 | 13 | 14 | |
| Don’t know | 1 | 0 | 2 | |
P values are from Fisher’s exact tests for categorical variables and ANOVA for age
Based on information obtained from subject electronic medical record (control = 55, telephone = 54, video = 54)
Based on information obtained from completed baseline survey (control = 37, telephone = 50, video = 52)
Table 2.
Demographic of telefamilies survey respondents
| Control | Telephone | Video | P value* | |
|---|---|---|---|---|
| Relationship to child | 0.6290 | |||
| Parent/legal guardian | 37 | 48 | 51 | |
| Foster | 0 | 2 | 1 | |
| Race | 0.2907 | |||
| White | 31 | 36 | 36 | |
| Black or African American | 2 | 8 | 10 | |
| Asian | 3 | 1 | 2 | |
| Multiracial | 1 | 5 | 4 | |
| Ethnic background | 0.9223 | |||
| Hispanic (non-Hispanic) | 2 | 4 | 5 | |
| Non-Hispanic | 35 | 46 | 46 | |
| Missing | 0 | 0 | 1 | |
| Age | 0.2618 | |||
| 18–34 years | 17 | 24 | 16 | |
| 35–54 years | 20 | 24 | 34 | |
| 55–64 years | 0 | 2 | 2 | |
| Marital status | 0.1969 | |||
| Married/partnered | 27 | 31 | 28 | |
| Single parent | 10 | 19 | 24 | |
| Household size | 0.6098 | |||
| 2–4 Household members | 23 | 36 | 36 | |
| 5+ Household members | 14 | 14 | 14 | |
| Household’s annual income | 0.0663 | |||
| < $22,000 per year | 5 | 12 | 19 | |
| $22,001–$50,000 per year | 16 | 18 | 22 | |
| $50,001–$88,000 per year | 6 | 12 | 4 | |
| > $88,000 per year | 10 | 7 | 7 | |
| Missing | 0 | 1 | 0 |
P values are from Fisher’s exact tests
Based on information obtained from completed baseline survey (control = 37, telephone = 50, video = 52)
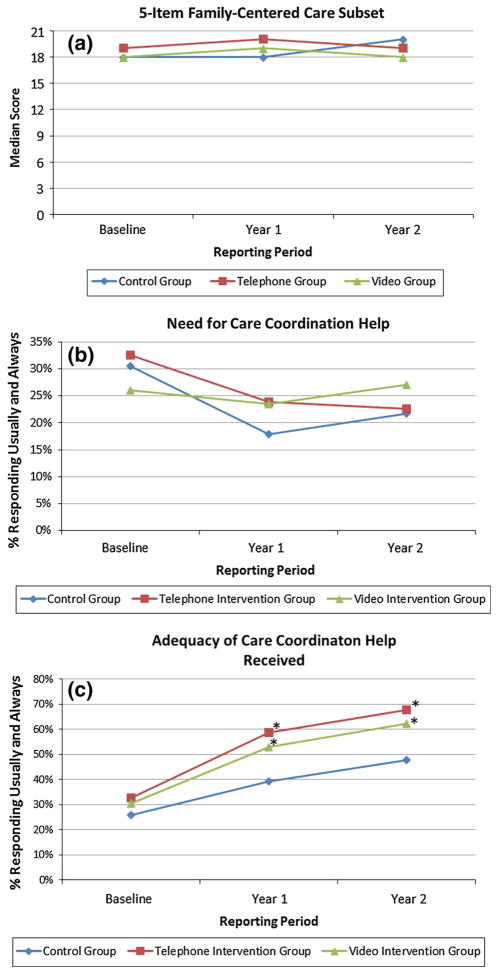
The first indicator of FCC coordination effectiveness used parent report of the 5-item FCC subset. For all groups, a median FCC score of 18.0–20.0 (of a maximum score of 20.0) across the 30 month study period indicated high levels of parent/guardian satisfaction and reflects the strength of the established medical home (Fig. 3). Comparison between-groups at baseline and post-baseline yielded no significant findings.
Fig. 3.
Change over time for outcome indicators of family-centered care coordination *McNemar’s test; P value <0.05 considered statistically significant
The second indicator of FCC coordination effectiveness used parent report of the need for care coordination help. Approximately 25 % of parents reported needing additional help coordinating their child’s care over the 30 month study period (Fig. 3). No significant differences were found in the need for care coordination help within or between groups at each data collection point or over time. TeleFamilies subjects have high levels of condition complexity and technology assistance that could explain an ongoing and unchanging need for care coordination help.
The third indicator of FCC coordination effectiveness used parent report of the adequacy of care coordination help received. At baseline, there was no significant difference in the adequacy of help received between groups, with approximately 30 % of respondents in each group reporting adequate care coordination help (Fig. 3). At both year one and year two data collection points, adequacy in care coordination help received within both APRN intervention groups, as compared to baseline increased significantly (P < 0.05). This help was described by parents (Table 3) at study end and included the benefit of having a single contact person that knows ‘their child’s story,’ understanding and learning how to best manage their child’s condition, reduced stress and the ability to return to work, and the benefit of telehealth in reducing clinic visits. Adequacy of care coordination help received between groups over time yielded conflicting results, with the GEE model finding no significant change. This could be explained by the similar and significant increases in adequacy of care coordination for both intervention groups.
Table 3.
Comments collected from intervention group parents at end of study
| Healthcare doesn’t have to be a maze if you have someone to help |
| One contact is so much easier. I could get answers right away |
| I realized just how complicated our situation is at times, and how one contact person helps |
| By not having to go into the clinic as often, my child did not get sick from office germs |
| How much help is actually needed (made aware) and how important coordination is |
| It is easier to do a videochat and show the nurse what’s wrong with your child instead of trying to explain it over the phone |
| The APRN showed me a website where I can find information and answers to questions. I learned to ask more questions and not be afraid to tell the doctors or nurses if I don’t understand something. Basically I learned how to speak up more for my child |
| I think telemedicine is a great idea and time saver for families! |
| Immediate care was so helpful. Convenience of just opening a screen and accessing competent and friendly help instead of taking my child out in bad weather |
| It changed our lives, and allowed me to work somewhat and know all I need to do is call the APRN when something came up |
| It helped to take some of the stress away and it was nice to have someone that knew your child on a personal level |
| It made my life easier to have one person to contact regarding my child who knows everything about my child and our family |
Discussion
FCC is a fundamental component of the pediatric medical home [21, 47] and a NQF practice standard for care coordination [41]. This paper reports preliminary evidence on the effectiveness of the APRN care coordinator role for CMC, using three FCC outcome indicators. To the best of our knowledge, this is the first report of care coordination effectiveness using these indicators. Our findings demonstrate that in a medical home with high levels of FCC, families of CMC have unmet care coordination needs that are addressed by the APRN care coordinator role (Fig. 3). These findings align with reports from community-based complex care clinics showing significant increases in parental perception of care coordination when delivered by a pediatric nurse practitioner [34, 52]. These findings are further illustrated in the Value Model [15] which advocates matching care coordinator skillset (RN vs. APRN) to patient/family needs as complexity escalates (Fig. 1).
The 5-item FCC subset used by this study is an established measurement framework for FCC [53]. We propose that this subset alone is not a robust measure of FCC coordination for CMC because it does not measure the effect of non-PCP care coordinator roles. The 2009–2010 NS-CSHCN found 64 % of parents responding positively to the 5-item FCC subset but<20 % reporting adequacy of care coordination help received [42]. Our baseline findings found a similar gap, with high levels of FCC as measured by the 5-item FCC subset (79 %) and low adequacy of care coordination help received (30 %) for all groups. At study end, the 5-item FCC subset did not significantly change for any group but adequacy of care coordination help received increased significantly for intervention subjects. These findings provide preliminary evidence that our outcome indicators differentiate a typical medical home model of care coordination from one incorporating an APRN care coordinator working collaboratively within the medical home. Future studies should incorporate these FCC outcome indicators.
The inclusion of coordinated care as a required element for accountable care organizations under the Affordable Care Act [54] is changing the reimbursement model of care coordination. The transition from fee-for-service to total-cost-of-care highlights the importance of clinic productivity over reimbursable cost. APRN care coordinator use of telehealth to manage acute and chronic illness complaints has the potential to change clinic productivity and addresses the fundamental importance of this model, “reduction in care fragmentation and inefficiency within and across health systems.” [18] For control group subjects, illness calls to the clinic automatically resulted in a clinic visit and if none where available emergency department diversion. For intervention group subjects, the APRN managed acute and chronic illness complaints with telehealth. This freed PCPs to manage additional patients, especially those with higher acuity. While not reported in this paper, examination of costs deferred through better care coordination rather than simply costs incurred are needed.
The total-cost-of-care transition has also resulted in multiple demonstration projects to meet the Triple Aim [55] using care coordination interventions [56]. The organization in which this research was conducted is an emerging accountable care organization and recognized the benefit of the APRN care coordinator role for CMC. The APRN was employed by the clinic but subsidized by the research project, and upon study completion, assisted with development and implementation of the ACOs new care coordination program targeting high utilization CMC. In this program, caseload is determined by care coordination need with the APRN coordinating the most complex CMC, and RNs coordinate the remainder. Social workers and bilingual service coordinators support access to medical and community resources and administrative staff help with indirect service activities. This model differs from the one reported by this paper by utilizing a team of personnel to match care coordination need. Future studies should incorporate a model where care coordination need determines the skill level of care coordinator assignment.
This study has limitations that affect generalizability of results. The study was conducted in a medical home that provides access to an integrated EMR and a variety of sub-specialists. The medical home supported the APRN care coordination intervention with EMR documentation enhancements, office space and integration of the telehealth technology. Other organizations may not be able to provide this support. A single APRN with 30 years of experience provided all care coordination services to intervention subjects, ranging from diagnosis and treatment to copying and faxing forms. While this model ensured research fidelity, it is not economically sustainable and a less-experienced APRN could yield different results. PCPs in the medical home embraced the care coordination intervention and integrated the APRN into the co-management of TeleFamilies subjects. An APRN who is less integrated in the medical home could yield different results. Seventy percent of subjects in the intervention groups but only 40 % of subjects in the control group returned surveys at all three data collection points. Our findings could reflect non-response bias of the control group.
Conclusion
This paper reported on a subset of TeleFamilies findings using FCC coordination outcome measures to demonstrate the effectiveness of the APRN care coordinator role. Our findings provide evidence that families of CMC enrolled in a well-established pediatric medical home have unmet care coordination needs, and care coordination provided by an APRN via telehealth significantly address these needs. Evaluation of FCC coordination for CMC should encompass not only the measures reported in this paper, but health care service utilization, child and family quality of life and child functional status. TeleFamilies is collecting this data and future papers will report these outcome measurements. Further study of the APRN care coordinator role for CMC in other settings is needed to strengthen evidence of effectiveness. Results of these studies should inform practice improvement efforts and shape health policy to support sustainable models of care coordination that serve the needs of families with CMC.
Acknowledgments
Funded in part by National Institutes of Health, National Institute of Nursing Research R01NR010883, Stanley M. Finkelstein, Principal Investigator.
Contributor Information
Rhonda G. Cady, Email: rhondagcady@gillettechildrens.com, University of Minnesota, 420 Delaware Street SE, MMC 609, Minneapolis, MN 55455, USA. Gillette Children’s Specialty Healthcare, St. Paul, Minnesota, USA
Mary Erickson, Children’s Hospitals and Clinics of Minnesota, Minneapolis, MN, USA.
Scott Lunos, University of Minnesota, 420 Delaware Street SE, MMC 609, Minneapolis, MN 55455, USA.
Stanley M. Finkelstein, University of Minnesota, 420 Delaware Street SE, MMC 609, Minneapolis, MN 55455, USA
Wendy Looman, University of Minnesota, 420 Delaware Street SE, MMC 609, Minneapolis, MN 55455, USA.
Margaret Celebreeze, University of Minnesota, 420 Delaware Street SE, MMC 609, Minneapolis, MN 55455, USA.
Ann Garwick, University of Minnesota, 420 Delaware Street SE, MMC 609, Minneapolis, MN 55455, USA.
References
- 1.Patient-centered primary care collaborative. [Accessed 26 Feb 2014];Joint principles of the patient-centered medical home. 2013 http://www.pcpcc.org/about/medical-home.
- 2.NAPNAP. [Accessed 11 Feb 2014];NAPNAP position statement on pediatric health care/medical home: Key issues on delivery, reimbursement, and leadership. 2009 http://www.napnap.org/PNPResources/Practice/PositionStatements.aspx.
- 3.American Academy of Pediatrics Council on Children with Disabilities. Care coordination in the medical home: Integrating health and related systems of care for children with special health care needs. Pediatrics. 2005;116(5):1238–1244. doi: 10.1542/peds.2005-2070. [DOI] [PubMed] [Google Scholar]
- 4.Meyers D, Peikes D, Genevro J, Peterson G, Taylor EF, Lake T, et al. The roles of patient-centered medical homes and accountable care organizations in coordinating patient care. Rockville: Agency for Helathcare Research and Quality; 2010. [Google Scholar]
- 5.McDonald KM, Sundaram V, Bravata DM, Lewis R, Lin N, Kraft SA, et al. Closing the quality gap: A critical analysis of quality improvement strategies (Vol. 7: care coordination) Rockville: Agency for Healthcare Research and Quality; 2007. [PubMed] [Google Scholar]
- 6.Institute of medicine (US) committee on quality of health care in america. Crossing the quality chasm: A new health system for the 21st century. Washington: National Academy Press; 2001. [PubMed] [Google Scholar]
- 7.Wise PH, Huffman LC, Brat G. A critical analysis of care coordination strategies for children with special health care needs. Technical review no. 14. (Prepared by the Stanford University—UCSF Evidence-based Practice Center under Contract No. 290-02-0017.) Rockville, MD: Agency for Healthcare Research and Quality; 2007. AHRQ Publication No. 07-0054. [PubMed] [Google Scholar]
- 8.Ziring PR, Brazdziunas D, Cooley WC, Kastner TA, Kummer ME, de Gonzalez PL, et al. American academy of pediatrics. Committee on children with disabilities. Care coordination: Integrating health and related systems of care for children with special health care needs. Pediatrics. 1999;104(4 Pt 1):978–981. [PubMed] [Google Scholar]
- 9.Cohen E, Kuo D, Agrawal R, Berry J, Bhagat S, Simon T, et al. Children with medical complexity: An emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529–538. doi: 10.1542/peds.2010-0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berry JG, Agarwal RK, Cohen E, Kuo DZ. The landscape of medical care for children with medical complexity. Alexandria: Children’s Hospital Association; 2013. [Google Scholar]
- 11.Neff JM, Sharp VL, Muldoon J, Graham J, Myers K. Profile of medical charges for children by health status group and severity level in a Washington State Health Plan. Health Services Research. 2004;39(1):73–89. doi: 10.1111/j.1475-6773.2004.00216.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics. 2012;130(6):e1463–e1470. doi: 10.1542/peds.2012-0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newacheck PW, Inkelas M, Kim SE. Health services use and health care expenditures for children with disabilities. Pediatrics. 2004;114(1):79–85. doi: 10.1542/peds.114.1.79. [DOI] [PubMed] [Google Scholar]
- 14.Tennant PW, Pearce MS, Bythell M, Rankin J. 20-year survival of children born with congenital anomalies: A population-based study. The Lancet. 2010;375(9715):649–656. doi: 10.1016/S0140-6736(09)61922-X. [DOI] [PubMed] [Google Scholar]
- 15.Looman WS, Presler E, Erickson MM, Garwick AW, Cady RG, Kelly AM, et al. Care coordination for children with complex special health care needs: The value of the advanced practice nurse’s enhanced scope of knowledge and practice. Journal of Pediatric Health Care. 2013;27(4):293–303. doi: 10.1016/j.pedhc.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Academy of Pediatrics. [Accessed 11 Feb 2014];2013 http://www.medicalhomeinfo.org/
- 17.McAllister JW, Presler E, Cooley WC. Practice-based care coordination: A medical home essential. Pediatrics. 2007;120(3):e723–e733. doi: 10.1542/peds.2006-1684. [DOI] [PubMed] [Google Scholar]
- 18.Council on Children with Disabilities and Medical Home Implementation Project Advisory Committee. Patient-and family-centered care coordination: a framework for integrating care for children and youth across multiple systems. Pediatrics. 2014;133(5):e1451–e1460. doi: 10.1542/peds.2014-0318. [DOI] [PubMed] [Google Scholar]
- 19.Bodenheimer T, Berry-Millett R. Care management of patients with complex health care needs. 19. Robert Wood Johnson Foundation; 2009. Research synthesis report. [PubMed] [Google Scholar]
- 20.McDonald KM, Schultz E, Albin L, Pineda N, Lonhart J, Sundaram V, et al. Care coordination measures atlas. Rockville: Agency for Healthcare Research and Quality; 2011. [Google Scholar]
- 21.Antonelli RC, McAllister JW, Popp J. [Accessed 11 Feb 2014];Making care coordination a critical component of the pediatric health system: A multidisciplinary framework. 2009 http://www.commonwealthfund.org/Publications/Fund-Reports/2009/May/Making-Care-Coordination-a-Critical-Component-of-the-Pediatric-Health-System.aspx.
- 22.Stille CJ, Antonelli RC. Coordination of care for children with special health care needs. Current Opinion in Pediatrics. 2004;16(6):700–705. doi: 10.1097/01.mop.0000144442.68016.92. [DOI] [PubMed] [Google Scholar]
- 23.APRN Consensus Model and Endorsing Organizations. [Accessed 11 Feb 2014];2008 http://www.nursingworld.org/consensusmodel.
- 24.US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Professions, Division Of Nursing. Specialty Areas: Adult, Family, Gerontological, Pediatric, and Women’s Health. 2002. Nurse Practitioner Primary Care Competencies; pp. 1–51. HRSA 00-0532(P) [Google Scholar]
- 25.NP Competencies-National Organization of Nurse Practitioner Faculties (NONPF) [Accessed 11 Feb 2014];2012 http://www.nonpf.org/?page=14.c.
- 26.Safriet BJ. Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine, editor. The Future of Nursing: Leading Change, Advancing Health. The National Academies Press; 2011. Federal options for maximizing the value of advanced practice nurses in providing quality, cost-effective health care. [Google Scholar]
- 27.Lindeke LL, Anderson SE, Chesney ML, O’Conner-Von S. Family-centered health care/medical home: APN roles in shaping new care models. Journal of Pediatric Health Care. 2010;24(6):413–416. doi: 10.1016/j.pedhc.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 28.Lindeke LL, Leonard BJ, Presler B, Garwick A. Family-centered care coordination for children with special needs across multiple settings. Journal of Pediatric Health Care. 2002;16(6):290–297. [PubMed] [Google Scholar]
- 29.Cady RG, Kelly AM, Finkelstein SM, Looman WS, Garwick AW. Attributes of advanced practice registered nurse care coordination for children with medical complexity. Journal of Pediatric Health Care. 2014;28(4):305–312. doi: 10.1016/j.pedhc.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gordon J, Colby H, Bartelt T, Jablonski D, Krauthoefer M, Havens P. A tertiary care primary care partnership model for medically complex and fragile children and youth with special health care needs. Archives of Pediatrics and Adolescent Medicine. 2007;161(10):937–944. doi: 10.1001/archpedi.161.10.937. [DOI] [PubMed] [Google Scholar]
- 31.Cady RG, Finkelstein SM, Kelly A. A telehealth nursing intervention reduces hospitalizations in children with complex health conditions. Journal of Telemedicine and Tele-care. 2009;15(6):317–320. doi: 10.1258/jtt.2009.090105. [DOI] [PubMed] [Google Scholar]
- 32.Farmer JE, Clark MJ, Drewel EH, Swenson TM, Ge B. Consultative care coordination through the medical home for CSHCN: A randomized controlled trial. Maternal and Child Health Journal. 2011;15(7):1110–1118. doi: 10.1007/s10995-010-0658-8. [DOI] [PubMed] [Google Scholar]
- 33.Palfrey JS, Sofis LA, Davidson EJ, Liu J, Freeman L, Ganz ML. The pediatric alliance for coordinated care: Evaluation of a medical home model. Pediatrics. 2004;113(5 Suppl):1507–1516. [PubMed] [Google Scholar]
- 34.Petitgout JM, Pelzer DE, McConkey SA, Hanrahan K. Development of a hospital-based care coordination program for children with special health care needs. Journal of Pediatric Health Care. 2013;27(6):419–425. doi: 10.1016/j.pedhc.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 35.Wyatt JC, Liu JL. Basic concepts in medical informatics. Journal of Epidemiology and Community Health. 2002;56(11):808–812. doi: 10.1136/jech.56.11.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koch S. Home telehealth—Current state and future trends. International Journal Of Medical Informatics. 2006;75(8):565–576. doi: 10.1016/j.ijmedinf.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 37.Finkelstein SM, Speedie SM, Potthoff S. Home telehealth improves clinical outcomes at lower cost for home healthcare. Telemedicine Journal and e-Health. 2006;12(2):128–136. doi: 10.1089/tmj.2006.12.128. [DOI] [PubMed] [Google Scholar]
- 38.Jia H, Chuang H, Wu SS, Wang X, Chumbler NR. Long-term effect of home telehealth services on preventable hospitalization use. Journal of Rehabilitation Research and Development. 2009;46(5):557–566. doi: 10.1682/jrrd.2008.09.0133. [DOI] [PubMed] [Google Scholar]
- 39.Jerant AF, Azari R, Martinez C, Nesbitt TS. A randomized trial of telenursing to reduce hospitalization for heart failure: Patient-centered outcomes and nursing indicators. Home Health Care Services Quarterly. 2003;22(1):1–20. doi: 10.1300/J027v22n01_01. [DOI] [PubMed] [Google Scholar]
- 40.Baker LC, Johnson SJ, Macaulay D, Birnbaum H. Integrated telehealth and care management program for Medicare beneficiaries with chronic disease linked to savings. Health Affairs. 2011;30(9):1689–1697. doi: 10.1377/hlthaff.2011.0216. [DOI] [PubMed] [Google Scholar]
- 41.National Quality Forum (NQF) Preferred practices and performance measures for measuring and reporting care coordination: A consensus report. Washington: National Quality Forum; 2010. [Google Scholar]
- 42. [Accessed 11 Feb 2014];National Survey of Children with Special Health Care Needs–Data Resource Center. 2012 http://www.childhealthdata.org/learn/NS-CSHCN.
- 43.Presler B. Care coordination for children with special health care needs. Orthopaedic Nursing. 1998;17(2 Suppl):45–51. [PubMed] [Google Scholar]
- 44.Kelly A, Golnik A, Cady R. A medical home center: Specializing in the care of children with special health care needs of high intensity. Maternal and Child Health Journal. 2008;12(5):633–640. doi: 10.1007/s10995-007-0271-7. [DOI] [PubMed] [Google Scholar]
- 45.Kelly A, Call K, Staub B, Donald B, Wisner C, Nelson A, et al. Children with complex chronic medical conditions and special needs privately insured through an HMO. Families Systems and Health. 2002;20(3):279–289. [Google Scholar]
- 46.Lutenbacher M, Karp S, Ajero G, Howe D, Williams M. Crossing community sectors: challenges faced by families of children with special health care needs. Journal of Family Nursing. 2005;11(2):162–182. doi: 10.1177/1074840705276132. [DOI] [PubMed] [Google Scholar]
- 47.American Academy of Pediatrics. Medical home initiatives for children with special needs project advisory committee. Policy statement: The medical home. Pediatrics. 2002;110(1 Pt 1):184–186. [Google Scholar]
- 48.Bethell CD, Read D, Stein R, Blumberg SJ, Wells N, Newacheck PW. Identifying children with special health care needs: Development and evaluation of a short screening instrument. Ambulatory Pediatrics. 2002;2(1):38–47. doi: 10.1367/1539-4409(2002)002<0038:icwshc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 49.US Department of Health and Human Services (USDHHS) Health Resources and Services Administration, Maternal and Child Health Bureau. [Accessed 11 Feb 2014];National Survey of Children with Special Health Care Needs 2005–2006. 2008 http://mchb.hrsa.gov/cshcn05/
- 50.Bethell CD, Read D, Brockwood K American Academy of P. Using existing population-based data sets to measure the American Academy of Pediatrics definition of medical home for all children and children with special health care needs. Pediatrics. 2004;113(5 Suppl):1529–1537. [PubMed] [Google Scholar]
- 51.Drummond A, Looman WS, Phillips A. Coping among parents of children with special health care needs with and without a health care home. Journal of Pediatric Health Care. 2012;26(4):266–275. doi: 10.1016/j.pedhc.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 52.Cohen E, Lacombe-Duncan A, Spalding K, MacInnis J, Nicholas D, Narayanan U, et al. Integrated complex care coordination for children with medical complexity: A mixed-methods evaluation of tertiary care-community collaboration. BMC Health Services Research. 2012;12(1):366. doi: 10.1186/1472-6963-12-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.US Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. The national survey of children with special health care needs chartbook 2009–2010. Rockville: Department of Health and Human Services; 2013. [Google Scholar]
- 54.Office of the Legislative Counsel US house of representatives. [accessed 8-8-13 from 2010]; [Accessed 11 Feb 2014];Compilation of patient protection and affordable care act. http://www.hhs.gov/healthcare/rights/law/index.html.
- 55.Institute for Healthcare Improvement: The IHI triple aim. [Accessed 5 Sept 2014];2014 http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx.
- 56.Accountable Care Organizations (ACO)—centers for medicare and medicaid services. [Accessed 5 Sept 2014];2013 http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ACO/index.html?redirect=/ACO.