Abstract
Study Objectives:
There is limited knowledge about the prospective relationship between major work characteristics (psychosocial, physical, scheduling) and disturbed sleep. The current study sought to provide such knowledge.
Design:
Prospective cohort, with measurements on two occasions (T1 and T2) separated by two years.
Setting:
Naturalistic study, Sweden.
Participants:
There were 4,827 participants forming a representative sample of the working population.
Measurements and Results:
Questionnaire data on work factors obtained on two occasions were analyzed with structural equation modeling. Competing models were compared in order to investigate temporal relationships. A reciprocal model was found to fit the data best. Sleep disturbances at T2 were predicted by higher work demands at T1 and by lower perceived stress at T1. In addition, sleep disturbances at T1 predicted subsequent higher perception of stress, higher work demands, lower degree of control, and less social support at work at T2. A cross-sectional mediation analysis showed that (higher) perceived stress mediated the relationship between (higher) work demands and sleep disturbances; however, no such association was found longitudinally.
Conclusions:
Higher work demands predicted disturbed sleep, whereas physical work characteristics, shift work, and overtime did not. In addition, disturbed sleep predicted subsequent higher work demands, perceived stress, less social support, and lower degree of control. The results suggest that remedial interventions against sleep disturbances should focus on psychosocial factors, and that such remedial interventions may improve the psychosocial work situation in the long run.
Citation:
Åkerstedt T, Garefelt J, Richter A, Westerlund H, Magnusson LL, Sverke M, Kecklund G. Work and sleep—a prospective study of psychosocial work factors, physical work factors, and work scheduling. SLEEP 2015;38(7):1129–1136.
Keywords: control, cross-lagged, demand, long hours, longitudinal, physical work factors, shift work, sleep, stress, support
INTRODUCTION
Complaints of disturbed sleep are common,1,2 and a major factor is stress at work or in private life.3–5 Stress typically involves increased physiological and psychological arousal in response to external demands,6 and increased arousal is associated with disturbed sleep.7 Thus, a clear link can be expected between work stress and subsequent sleep disturbances, and has indeed been demonstrated in several prospective studies. Ribet and Derriennic8 were the first to show such a link, using the stress indicator “having to hurry.” Using a more established work stress indicator, the demand/control/support model,9 de Lange et al.10 showed that a change from low to high job strain (i.e., going from high influence and low work demands to low influence and high work demands) was associated with increased sleep problems and fatigue between two measurement occasions. Two other studies have shown similar results regarding strain.11,12 In another study, Magnusson Hanson et al.13 used structural equation modeling and found no significant link between work demands and subsequent sleep problems. When studying changes in working conditions between two points in time, Akerstedt et al.14 found that increased work demands, as well as preoccupation with work, predicted new cases of disturbed sleep. It should be noted that the focus of the studies cited above was external demands that could lead to a stress reaction, not the experience of stress itself. Social support at work9 may protect against stress and disturbed sleep,15,16 possibly because it provides a buffer to high work demands and/or low degree of control.9 However, no clear relation was observed between demands at work and sleep in an earlier prospective study.13
Work schedules may also influence sleep. Sleep complaints have been found in several prospective studies of night-shift workers.8,17,18 Some evidence of prospective negative effects on sleep has also been reported in association with overtime and long working weeks.8,19 Other aspects of work scheduling do not seem to have been addressed. Another work-related factor that may affect sleep is the physical demands of the work task, such as awkward work positions or heavy lifting or carrying. However, Ribet and Derriennic8 found no prospective evidence of this, and no other studies could be found in the literature. The direct physical environment at work, such as loud noise or extreme temperatures or lighting conditions, may also be assumed to affect sleep quality, but the only previous study on this issue revealed no effects of extreme temperatures or noise in the workplace.8 It is clear that there is a need for more research into physical work factors and their effects on sleep.
Although the study by Ribet and Derriennic8 revealed important information regarding work characteristics and sleep disturbances, the study had several limitations. For instance, it did not measure exposure at both time points, nor did it control for sleep disturbances at the start. Furthermore, the sample only included individuals from 37 to 52 y of age and was not a representative national sample. The current study sought to improve on the approach by Ribet and Derriennic by investigating the prospective relation between a variety of work environment factors (stress, demands, control, support, physical work load, physical work environment, and work scheduling) and disturbed sleep in a representative national sample with two waves of measurements. Because impaired sleep may affect emotional responses,20 reverse relations also were investigated; that is, how sleep disturbances relate to subsequent perceptions of work factors. In addition, the current study also introduces a measure of the perception of stress as a complement to work demands and as a possible mediator of a potential relation between work demands and sleep disturbances.
METHODS
Design and Participants
The study is based on the Swedish Longitudinal Occupational Survey of Health, SLOSH. This is a nationally representative longitudinal study with follow-ups every second year (from 2006). It has its origin in the Swedish Work Environment Survey (SWES, www.scb.se), which in turn is based on nationally representative samples of the working population. Earlier waves from this cohort have been studied by Magnusson Hansson et al.13 regarding demands at work and their effects on sleep. The Regional Research Ethics Board in Stockholm approved the current study.
In the current study, we used data from the second wave in 2008 (T1) and the third wave in 2010 (T2). In the 2008 wave of SLOSH, all eligible participants from SWES 2003 or 2005 were invited to participate (n = 15,147). A total of 11,441 individuals replied, of which 9,756 were gainfully employed. In that group, 6,580 people responded and were also gainfully employed in 2010 (Figure 1). As this study was focused on work characteristics, we used data only from those gainfully employed at both T1 and T2 (n = 6,580), thereby excluding individuals on sick leave or parental leave, or who were retired or unemployed at T1 or T2. The dropout rate between T1 and T2 was 28% (n = 2,311). The number of respondents for which valid data were available for all variables investigated in this study at T1 was 5,489, but 662 of these individuals had missing values at T2, resulting in an internal dropout rate of 12.1%. The final sample thus consisted of 4,827 participants. Of these, 2,655 were females and 2,171 were males. There were 1,979 participants who had a university education (the remainder had a shorter education) (see Table 1 where these values are presented as proportions in column 1).
Figure 1.
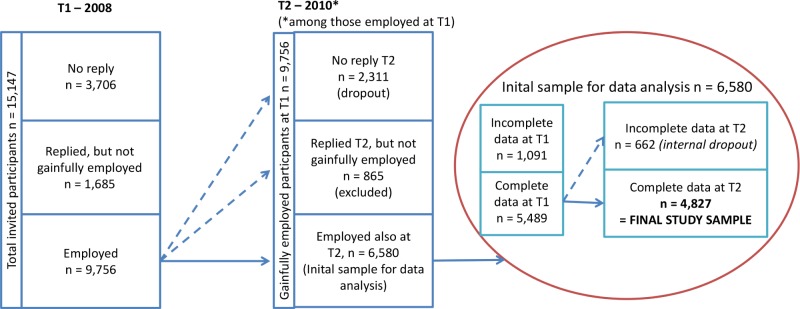
Illustration of dropout. See text.
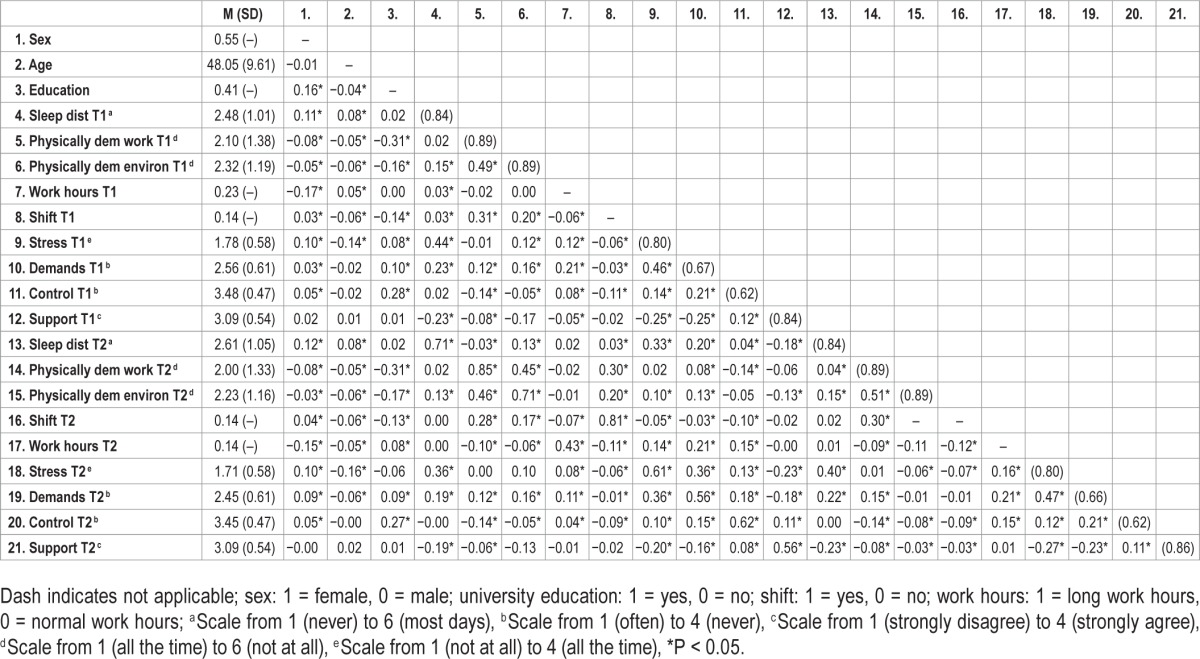
Table 1.
Means, standard deviations, reliability (Cronbach α in parentheses), and intercorrelations (n = 4,827).
An analysis was conducted to investigate whether dropout (nonresponse) at T2 could be predicted by demographic, work environment, or sleep disturbance variables at T1 (Figure 1). Logistic regression analysis indicated that overall nonresponse dropout at T2 could be predicted (χ2(12) = 276.35, P < 0.001). Dropout was lower for women than for men (odds ratio [OR] = 0.74, P < 0.001), and among individuals with at least 3 y of education at university level, compared to the rest (OR 0.85, P < 0.001). Younger employees (age in years, OR = 0.96, P < 0.001) and those having physically demanding work tasks (OR = 1.08, P < 0.001) had a higher tendency to drop out at T2. Another logistic regression analysis was performed to investigate whether internal dropout at T2 (due to missing values) could be predicted by the same variables. The results showed that overall internal dropout at T2 could be predicted (χ2(12) = 64.48, P < 0.05). Further investigations of the results showed that the internal dropout rate was higher for women than for men (OR = 1.24, P < 0.05). Older employees (OR = 1.03, P < 0.001) and those with demanding physical work (OR = 1.11, P < 0.01), as well as those working shifts (OR = 1.29, P < 0.05) had a higher tendency for missing values at T2. Moreover, individuals reporting a higher degree of control at T1 were more likely to have missing values at T2 (OR = 1.25, P < 0.05).
Questionnaire
Information regarding sex, age, and socioeconomic position (SEP) were obtained from national register data at T1. SEP was defined by educational level (≥ 3 y of university education versus all other forms of education). For the other constructs investigated, items were selected as indicators based on reliability and confirmatory factor analyses. Items with a factor loading below 0.4 were removed in order to obtain a reasonable model fit.21 Table 1 shows the correlations between the variables at T1 and T2, and between T1 and T2.
Psychosocial Variables
Four items representing disturbed sleep were selected from the 14-item Karolinska Sleep Questionnaire (KSQ)14,22–24 (Cronbach α > 0.70). The scale differentiates patients with insomnia from healthy individuals,23 and correlates with perceived stress, anxiety, depression, and burnout (r > 0.40).24 The items included are: difficulties falling asleep, restless sleep, repeated awakenings, and premature awakening. The responses range from “never” to “most days of the week” (values from 1 through 6 being assigned). Cronbach α was 0.84 at both T1 and T2 in the current study, and the correlation between time points was r = 0.71.
Work demands were measured using the Swedish version of the Demand-Control-Support Questionnaire.9 This scale has been extensively psychometrically investigated25,26 and used to predict health outcomes of psychosocial work factors.27,28 The three items that were selected (considering factor loadings) were: Do you have to work very intensively? Does your work demand too much effort? Do you have enough time to do everything? (reverse coded). The items excluded were: Do you have to work very fast? and Does your work often involve conflicting demands? The response alternatives range from 1: Hardly ever/never, to 4:Yes, often. Cronbach α was 0.67 at T1 and 0.66 at T2, and the test-retest reliability between T1 and T2 was r = 0.56. Higher values on this scale indicate higher perceived work demands.
Control at work9 was measured as an index of three questions (based on factor loadings from the Demand-Control-Support Questionnaire (Do you have to do the same thing over and over again? Do you have a choice in deciding how you do your work? Do you have a choice in deciding what you do at work?). The following items were excluded: Does your work require a high level of skill or expertise? Does your work require ingenuity? Do you have the possibility of learning new things through your work? High values indicate a high degree of control. The response alternatives were the same as for the work demands. Cronbach α was 0.62 at both T1 and T2 and the test-retest reliability between T1 and T2 was r = 0.62.
Social support at work9 was measured as an index of five statements (There is a calm and pleasant atmosphere where I work; There is a good spirit of unity; My colleagues are there for me; People understand that I can have a bad day; I get on well with my colleagues). The following item was removed: I get on well with my superiors. Response alternatives ranged from 1: Strongly disagree, to 4: Strongly agree. Cronbach α was 0.84 at T1 and 0.86 at T2 and the test-retest reliability between T1 and T2 was r = 0.56. It should be emphasized that this scale focuses only on support at work, in contrast to many other social support scales.
The Physical Work Environment, Scheduling, and Work Hours
“Shift work” refers to any type of scheduling system that includes non-daytime work; that is, night work, three-shift work, two-shift work, day-oriented roster work, permanent morning work (starting before 07:00), or permanent afternoon work (starting after 12:00). A total of 676 individuals had shift work (see Table 1 for the proportion of shift workers in column 1), and among these, 196 had some form of night shifts included (65 of these had permanent nights). “Long working hours” (overtime work) was defined as usually working ≥ 46 h per week (using 36–45 h/w as a reference). A total of 1,110 individuals worked long hours (> 46 h/w).
Physically demanding work tasks were measured as an index of three questions (Is your work such that you have to use bent, twisted or otherwise unsuitable positions? Do you have to lift at least 15 kilos several times a day? Does your work sometimes involve heavy physical labor; that is, do you physically exert yourself more than when walking and standing and moving around in a normal way?). Response alternatives ranged from 1: No, not at all to 6: Almost all the time. Cronbach α was 0.89 for both T1 and T2 and the test-retest reliability between T1 and T2 was r = 0.85.
Physically demanding work environment was measured using three questions on exposure to poor or excessively bright light, noise, and excessive heat, cold, or draught. These questions have been constructed and used by Statistics Sweden since the late 1980s in their surveys of the working environment in Sweden. Validation and “calibration” against objectively measured work environment factors were carried out before using the questions in surveys.29 The six response alternatives range from 1: No, not at all to 6: Almost all the time. Cronbach α was 0.89 for both T1 and T2 and the test-retest correlation between T1 and T2 was r = 0.71.
Although the current study was focused on work factors, it was considered of interest to also investigate whether a more generic stress scale could serve as a complement to the traditional work demand scale. However, the available generic stress scales30–32 include items (for example, “angry,” “forgotten to do something,” “not in control”) that do not represent the original notion of an arousal response to demands, which constitutes the original concept of stress.6 Generic perceived stress, as measured in this study, was an index of three questions on feelings during the last three months, reasonably in line with the original concept (I have days when I feel wound up all the time; I have days when I feel very pressured all the time; I have days when I feel stressed all the time). Response alternatives ranged from 1: Not at all, to 4: Almost all the time. A 3-mo period was chosen since this should provide a better indication than “the present moment” or “the last few days.” Cronbach α was 0.80 at T1 and T2. As this was the first time this scale was used, we also computed correlations that may be useful psychometrically. It can be seen from Table 1 that the stress rating at T1 correlated (r = 0.61) with the same variable at T2, (r = 0.47; P < 0.001) with the work demand index at T1. The stress rating also correlated with “difficulties relaxing in the evening” at T1 (r = 0.61; P < 0.001), and with “often tense” at T1 (r = 0.58; P < 0.001). The latter two items were derived from other parts of the questionnaire (response range 1–5). The new stress index was called “Perceived Stress.”
Statistical Analysis
In order to test the relationships, structural equation modeling was applied using IBM SPSS Amos 20.0 (IBM SPSS, Rochester, NY). The maximum likelihood method was selected as the estimation procedure. In order to ensure that the data were normally distributed, they were screened for kurtosis and skewness; we found no kurtosis values greater than 10 or skewness values greater than 3.33 Moreover, none of the variables was highly correlated (defined as r > 0.8534) and r did not exceed 0.70 in the current study (except for correlations over time for four variables), thus reducing the risk of multicollinarity.33 In order to test the associations between sleep disturbances and the work environment indicators, four different cross-lagged models were fitted.
A stability model including the autoregressions of all variables (Model 1).
A causal model including eight paths between the work environment indicators at T1 and sleep disturbance at T2, in addition to the autoregressions (Model 2).
A reversed causal model including eight paths, between sleep disturbance at T1 and the work environment indicators at T2, in addition to the autoregressions (Model 3).
A reciprocal model including all the paths in the previous models (Model 4).
To set the scale of the latent variables, one factor loading per latent variable was fixed. The model fit was evaluated using the comparative fit index (CFI),35 the nonformed fit index (NNFI36), and the root mean square error of approximation (RMSEA37) to complement the chi-square fit statistic. The following approximate cutoff criteria were used to evaluate the model fit: for the CFI, values close to or above 0.97,36 for the NNFI, values greater than 0.95,33 and for the RMSEA, values below 0.06.38 The chi-square difference test was used to compare different nested models.39
The four models were systematically evaluated by comparing the baseline model (Model 1) to the more complex models (Models 2, 3, 4) using the chi-square difference test. A lack of statistically significant difference in chi-square values would indicate that the baseline model explains the data as well as the more complex model with additional paths.40 The other fit indices were also used to choose the best-fitting model.
In order to correct for systematic method variance associated with each indicator, the item-specific measurement errors were allowed to correlate over time.39 Moreover, constructs were allowed to correlate within time points in all models in order to account for contemporary relations. Measurement-specific errors were allowed to correlate to improve the model fit. The effects of sex, age, and SEP on the T1 variables under investigation were adjusted for in all models.
In order to further investigate the relation between sleep disturbances, demands at work and perceived stress, mediation analysis was applied. First, cross-sectional mediation was investigated, where the indirect effect of work demands, through perceived stress, on sleep disturbance was tested using the Sobel test.41 The potential power problems associated with the Sobel test were considered small due to the large sample size.41 In order to investigate longitudinal mediation with two waves, a procedure proposed by Taris and Kompier42 was employed. The cross-lagged relationship between T1 work demands and T2 perceived stress was investigated together with the cross-lagged relationship between T1 perceived stress and T2 sleep disturbance. Only conclusions on partial (as opposed to full) mediation can be drawn from studies with only two waves.42,43 In order to estimate the magnitude of the indirect effects, the two cross-lagged relationships (i.e., T1 work demands → T2 perceived stress and T1 perceived stress → T2 sleep disturbance) were multiplied. Again, a Sobel test was conducted to formally investigate the indirect effect.
RESULTS
Table 1 provides descriptive statistics, reliabilities, and intercorrelations between all the variables studied. In accordance with expectations, sleep disturbances were associated with perceived stress, work demands, and support, within, as well as over, time. Overall, the variables were rather stable over the two-year time period, apart from working hours, which had a stability of 0.41 (see Figure 2).
Figure 2.
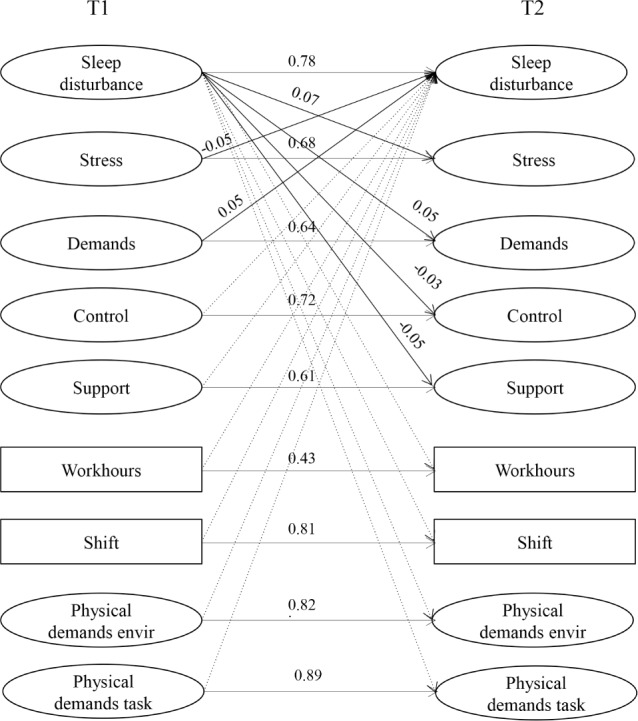
Structural model (reciprocal): standardized coefficients. Nonsignificant paths represented by dotted lines, all coefficients in the model are significant (P < 0.05). Other models not presented.
Table 2 gives the fit statistics for the cross-lagged models. All models exhibited significant chi-square values, which could be expected due to the large sample size; however, the additional fit indices indicated acceptable fits to data for all four models. Comparisons between the stability model (Model 1) and the other three models revealed that Models 3 and 4 gave a significantly lower value of chi-square, thus indicating a better fit. The reciprocal model (Model 4), however, showed the greatest decrease in chi-square (Δχ2 = 60.33, df = 14, P < 0.05) and this model was thus identified as the model giving the best fit.
Table 2.
Results of the test of the structural models: cross-lagged effects (n = 4,827).
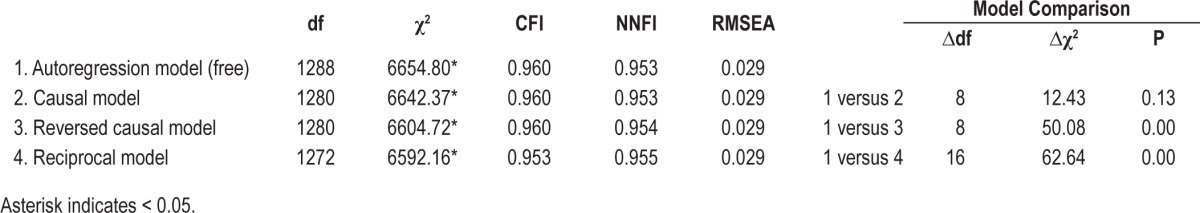
Figure 2 shows the significant standardized path estimates for the reciprocal model, and it can be seen that higher work demands at T1 were related to higher levels of sleep disturbance at T2, while perceived stress at T1 was associated with lower levels of sleep disturbances at T2, after adjusting for sex, age, and SEP. Moreover, sleep disturbances at T1 were related to higher perceived stress and work demands, as well as a lower degree of control and support at work at T2, after adjusting for sex, age, and SEP.
Because the negative beta coefficient for perceived stress and disturbed sleep was unexpected, we also carried out structural equation modeling using only perceived stress or work demands in combination with disturbed sleep. The results of this were as expected. Stress at T1 predicted subsequent sleep disturbances (β = 0.06, P < 0.05) and vice versa (β = 0.13, P < 0.05). A similar pattern was found with regard to demands at work. Demands at T1 predicted subsequent sleep disturbances (β = 0.03, P < 0.05), and vice versa (β = 0.04, P < 0.05).
Because perceived stress was seen as a complement to work demands, and assumed to be related to disturbed sleep, a mediation model (demands-stress-sleep disturbances) was applied. No mediation could be detected in the longitudinal analysis; demands were positively related to perceived stress (β = 0.05, P < 0.05), but perceived stress was not related to subsequent sleep disturbances (β = 0.001, P > 0.05). The indirect effect was not significant (z = 0.057, P > 0.05). However, mediation was found in the cross-sectional analysis. Demands were positively related to perceived stress (β = 0.29, P < 0.05) and perceived stress was positively related to sleep disturbances (β = 0.60, P < 0.05). The indirect effect was significant (z = 15.1, P < 0.05). In addition, work demands had an effect on sleep disturbance (β = 0.27, P < 0.05).
DISCUSSION
The reciprocal model showed the best fit to the data. Our main hypothesis, of a forward “causal” pathway between work demands and sleep disturbances, was partly confirmed by the significant relationship between work demands at T1 and sleep disturbances at T2. Perceived stress showed an unexpected negative relation to disturbed sleep. No significant relationships were seen for control at work, social support, physical work factors, work schedules, or working hours. The reciprocal model also showed significant paths between sleep disturbances at T1 and work demands, stress, control at work, and social support at T2, indicating the presence of reversed causal paths.
The results regarding work demands are in line with those from several other prospective studies,8,10,13,14 although the effect found in the current study was modest. However, an important and new observation is that the prospective relation between work demands and disturbed sleep persisted in an analysis containing variables representing the physical aspects of work, shift work, overtime, and social support at work. It is important to take the 2-y time lag into account when interpreting the results. It is possible that other time lags may have yielded stronger (or weaker) relationships. There is, however, no indication of the optimal time lag for the variables used in the current study, or for the variables used in most other observational studies. This is clearly an important topic for future research.
The unexpected negative association between perceived stress at T1 and sleep disturbances at T2 appeared despite a significant bivariate positive correlation between the two variables over time and a strong cross-sectional correlation. Both correlations were stronger than those between work demands and sleep disturbances. Furthermore, the cross-sectional mediation of perceived stress between demands and sleep disturbance was significant. When the structural equation modeling was restricted to perceived stress only, the path from T1 to T2 was significant and the coefficient positive (as was that of work demands). These observations suggest that the negative coefficient for perceived stress in the main analysis was due to suppression effects or, possibly, that stress at T1 might perhaps have encouraged a change of lifestyle. In terms of psychometrics, the perceived stress index showed high internal consistency and test-retest reliability. It was also correlated with work demands, as well as with the item “tension,” which suggests construct validity.
As in our previous studies,13,14 control at work was not significantly related to subsequent sleep disturbances. The dropout rate among those with a low degree of control was higher, but this cannot explain the results because the correlation between control at T1 and disturbed sleep at T2 was r = 0.04, and the cross-sectional correlations at T1 and T2 were r = 0.02 and r = 0.04, respectively. Thus, the relation was very small at both points in time, and actually increased at T2, which would not have been the case if dropout had affected the results (i.e., reduced the correlation). Possibly the reduced reliability could have contributed to the lack of effects. The finding that (poor) social support failed to predict later sleep disturbances was unexpected, considering previous findings14,44,45; however, it is in line with findings reported by Magnusson Hansson et al.13 The cross-sectional correlation with disturbed sleep was significant, and it may be that social support is important when support and sleep are measured closer together in time.
Regarding the effects of work scheduling, the lack of a significant association between shift work and disturbed sleep differs from our previous findings.14 However, we only adjusted for one physical work environment variable—heavy work—in our previous study, whereas more aspects of the physical working environment were included in the current study. Furthermore, in a previous prospective study in a representative sample on the effects of starting or ending shift work we found that mainly difficulties in falling asleep were influenced by these changes.18 It could thus be that the lack of effect in the current study is the result of including other indicators of disturbed sleep in the index, such as restless sleep, frequent awakenings, and premature final awakening. Indeed, workers on the night shift tend not to report more disturbed sleep than day workers.23 The reason for the lack of reports of disturbed sleep could be that shift workers do not consider their sleep to be disturbed because there is a clear external cause (the temporal displacement of sleep). The dropout frequency was also higher among shift workers, but it is unlikely that this will have affected the results because the correlation between shift work at T1 and disturbed sleep at T2 was low (r = 0.03), and the cross-sectional correlations between shift work and disturbed sleep were also low (r = 0.03 at T1 and r = 0.02 at T2).
The lack of any significant association between long hours of work and disturbed sleep is in contrast to the findings of previous studies,8,19,46 but very few individuals with long working weeks were included in the current study, compared to the studies cited. Thus, the range of variation may have been restricted. Also, as with shift workers, those with long working hours may not regard their sleep as being disturbed, but rather curtailed by external factors. However, this requires further investigation.
The physical workload variables were not prospectively related to disturbed sleep. There are few data to compare our findings with, but we have previously found heavy physical work load to be associated with disturbed sleep in a cross-sectional study,22 but not in a longitudinal one.14 The dropout rate was higher among individuals with higher physical workload, but this is unlikely to have affected the results of the current study because the correlation between physical workload at T1 and disturbed sleep at T2 was low (r = 0.03, as were the cross-sectional correlations (r = 0.02 and r = 0.03 at T1 and T2, respectively). Furthermore, the analyses concerning physical working environment variables did not suggest a higher risk of subsequent sleep disturbances. Because this association has not been studied previously, caution should be exercised when drawing conclusions.
The second major finding of this study was that disturbed sleep at T1 predicted several psychosocial variables at T2. Both perceived stress and work demands were higher with prior sleep disturbance. Neither Magnusson Hanson et al.13 nor de Lange et al.10 found any similar reversed effects on demands. One reason for this, at least in the study by de Lange et al., may have been that the sample was relatively young. Our findings with respect to stress agree with recent experimental results showing that disturbed sleep increases responses to stressors,20 and that sleep loss reduces the control of the prefrontal cortex over the amygdala, leading to increased emotional reactivity.47 It is also a common observation that sleep loss causes sleepiness/fatigue and impaired performance,48 and these may in turn lead to demands at work being seen as more difficult to handle than would otherwise be the case. It is also likely that a similar mechanism could apply to social support and control at work. Magnusson Hansson et al.13 also reported an association between sleep disturbances and later social support, whereas no significant paths were observed between disturbed sleep and control or work demands. These issues are important in understanding the relationship between sleep and working life, and there is a need for further research in these areas. Furthermore, it is noteworthy that disturbed sleep showed no reverse causality pattern with physical work factors.
A limitation of the current study is that more waves may be needed to gain a better understanding of the prospective links. Thus, the present results are merely suggestive. Another limitation is that no detailed information was available on changes in disturbed sleep (or in predictors) within the 2-y interval studied. For example, major life events may occur, such as divorce, bereavement, etc. There is also a moderate day-to-day covariation between self-reported stress and sleep in normal sleepers,49 but no knowledge is available on the amount or duration of demands or stress exposure that causes more chronic sleep disturbances. Day-to-day variation in sleep quality seems to be relatively high in patients with insomnia, but considerably smaller in normal sleepers.50 Also, the correlation between sleep quality at T1 and T2 was high in the current study, suggesting considerable stability. Clearly, there is a need to study the relation between disturbed sleep and its causes, using shorter intervals between measurements. Another potential problem may be that the questions on work-related exposure asked about the respondents' “work situation,” which was probably interpreted as meaning at the present time, in contrast to the questions on self-reported stress, which referred to the past 3 months. The reason for the choice of 3 months was that there was a need for an anchor similar in time to what may be meant by the “present work” concept. This still resulted in some lack of clarity with respect to timing, which may have influenced the results.
A weakness of the study is the loss of some items with low factor loadings in order to improve model fit.21 The result may have been more unreliable scales, but Cronbach α values were still acceptable. There may also have been a reporting bias, that is, a dispositional tendency of an individual to report both psychosocial adversity and more health symptoms. This phenomenon is probably present in most studies on psychosocial factors and health, and may affect the associations between such variables. However, a certain amount of consistency across predictors would then be expected. In the current case, control at work did not show any significant relation to disturbed sleep, which would have been expected had the subjectivity bias been strong. The “healthy worker effect” is another factor that must be taken into consideration because our sample only included gainfully employed individuals. Length of employment may have been of importance in the current context, but this information was not available for analysis.
In summary, the current study has shown that high work demands predict self-reporting of disturbed sleep 2 y later, but also that disturbed sleep predicts increased levels of perceived stress, work demands, (lack of) work control, and (lack of) social support 2 y later. Physical work factors and work scheduling seem to have no prospective relation to sleep disturbance. The results imply that remedial interventions to alleviate sleep disturbances should focus on psychosocial factors, and that interventions to improve sleep may be important in reducing stress and negative views of work, and perhaps life in general.
DISCLOSURE STATEMENT
This was not an industry supported study. This work was supported by the Swedish Council for Working Life and Social Research, the Insurance Company Alecta AB, and Stockholm Stress Center, Stockholm University and Karolinska institutet. Torbjörn Åkerstedt has had speaking assignments with Astra Zeneca. The other authors have indicated no financial conflicts of interest.
Footnotes
A commentary on this article appears in this issue on page 1007.
REFERENCES
- 1.Walsh JK, Coulouvrat C, Hajak G, et al. Nighttime insomnia symptoms and perceived health in the America Insomnia Survey (AIS) Sleep. 2011;34:997–1011. doi: 10.5665/SLEEP.1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ohayon MM, Bader G. Prevalence and correlates of insomnia in the Swedish population aged 19-75 years. Sleep Med. 2010;11:980–6. doi: 10.1016/j.sleep.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Burgard SA, Ailshire JA. Putting work to bed: stressful experiences on the job and sleep quality. J Health Soc Behav. 2009;50:476–92. doi: 10.1177/002214650905000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nylen L, Melin B, Laflamme L. Interference between work and outside-work demands relative to health: unwinding possibilities among full-time and part-time employees. Int J Behav Med. 2007;14:229–36. doi: 10.1007/BF03002997. [DOI] [PubMed] [Google Scholar]
- 5.Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation survey. I. Sleep. 1999;22:S347–53. [PubMed] [Google Scholar]
- 6.Selye H. The stress of life. New York: McGraw Hill; 1956. [Google Scholar]
- 7.Riemann D, Spiegelhalder K, Feige B, et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14:19–31. doi: 10.1016/j.smrv.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Ribet C, Derriennic F. Age, working conditions, and sleep disorders: a longitudinal analysis in the French cohort E.S.T.E.V. Sleep. 1999;22:491–504. [PubMed] [Google Scholar]
- 9.Theorell T, Perski A, Akerstedt T, et al. Changes in job strain in relation to changes in physiological state. Scand J Work Environ Health. 1988;14:189–96. doi: 10.5271/sjweh.1932. [DOI] [PubMed] [Google Scholar]
- 10.de Lange AH, Kompier MA, Taris TW, et al. A hard day's night: a longitudinal study on the relationships among job demands and job control, sleep quality and fatigue. J Sleep Res. 2009;18:374–83. doi: 10.1111/j.1365-2869.2009.00735.x. [DOI] [PubMed] [Google Scholar]
- 11.Ota A, Masue T, Yasuda N, et al. Psychosocial job characteristics and insomnia: a prospective cohort study using the Demand-Control-Support (DCS) and Effort-Reward Imbalance (ERI) job stress models. Sleep Med. 2009;10:1112–7. doi: 10.1016/j.sleep.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 12.Edmé J-L, Facq J, Frimat P, Vezina M. Relationship between psychosocial factors at work and incidence of perceived health problems in the GERICOTS cohort. Revue d'Epidémiologie et de Santé Publique. 2011;59:295–304. doi: 10.1016/j.respe.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Magnusson Hanson LL, Akerstedt T, Naswall K, Leineweber C, Theorell T, Westerlund H. Cross-lagged relationships between workplace demands, control, support and sleep problems. Sleep. 2011;34:1403–10. doi: 10.5665/SLEEP.1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akerstedt T, Nordin M, Alfredsson L, Westerholm P, Kecklund G. Predicting changes in sleep complaints from baseline values and changes in work demands, work control, and work preoccupation--the WOLF-project. Sleep Med. 2012;13:73–80. doi: 10.1016/j.sleep.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 15.Wahlstedt KGI, Edling C. Organizational changes at a postal sorting terminal—their effects upon work satisfaction, psychosomatic complaints and sick leave. Work Stress. 1997;11:279–91. [Google Scholar]
- 16.Nordin M, Westerholm P, Alfredsson L, Akerstedt T. Social support and sleep. Longitudinal relationships from the WOLF-Study. Psychology. 2012;3:1223–30. [Google Scholar]
- 17.Niedhammer I, Lert F, Marne M-J. Effects of shift work on sleep among french nurses. J Occup Med. 1994;36:667–74. [PubMed] [Google Scholar]
- 18.Akerstedt T, Nordin M, Alfredsson L, Westerholm P, Kecklund G. Sleep and sleepiness: impact of entering or leaving shiftwork - a prospective study. Chronobiol Int. 2010;27:98–96. doi: 10.3109/07420528.2010.489423. [DOI] [PubMed] [Google Scholar]
- 19.Virtanen M, Ferrie JE, Gimeno D, et al. Long working hours and sleep disturbances: the Whitehall II prospective cohort study. Sleep. 2009;32:737–45. doi: 10.1093/sleep/32.6.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Minkel JD, McNealy K, Gianaros PJ, et al. Sleep quality and neural circuit function supporting emotion regulation. Biol Mood Anxiety Disord. 2012;2:22. doi: 10.1186/2045-5380-2-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelloway EK. Saint Mary's University, Canada SAGE Publication Inc.; 1998. Using LISREL for Structural Equation Modeling. A researchers guide. [Google Scholar]
- 22.Åkerstedt T, Knutsson A, Westerholm P, Theorell T, Alfredsson L, Kecklund G. Sleep disturbances, work stress and work hours. A cross-sectional study. J Psychosom Res. 2002;53:741–8. doi: 10.1016/s0022-3999(02)00333-1. [DOI] [PubMed] [Google Scholar]
- 23.Akerstedt T, Ingre M, Broman JE, Kecklund G. Disturbed sleep in shift workers, day workers, and insomniacs. Chronobiology international. 2008;25:333–48. doi: 10.1080/07420520802113922. [DOI] [PubMed] [Google Scholar]
- 24.Nordin M, Akerstedt T, Nordin S. Psychometric evaluation and normative data for the Karolinska Sleep Questionnaire. Sleep Biol Rhythms. 2013;11:216–26. [Google Scholar]
- 25.Fransson E, Nyberg S, Heikkilä K, et al. Comparison of alternative versions of the job demand-control scales in 17 European cohort studies: the IPD-Work consortium. BMC Public Health. 2012;12:62. doi: 10.1186/1471-2458-12-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chungkham HS, Ingre M, Karasek R, Westerlund H, Theorell T. Factor structure and longitudinal measurement invariance of the demand control support model: an evidence from the Swedish Longitudinal Occupational Survey of Health (SLOSH) PLoS One. 2013;8:e70541. doi: 10.1371/journal.pone.0070541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kivimäki M, Nyberg ST, Batty GD, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet. 2012;380:1491–7. doi: 10.1016/S0140-6736(12)60994-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Magnusson Hanson LL, Madsen IEH, Westerlund H, Theorell T, Burr H, Rugulies R. Antidepressant use and associations with psychosocial work characteristics. A comparative study of Swedish and Danish gainfully employed. J Affect Disord. 2013;149:38–45. doi: 10.1016/j.jad.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 29.Wikman A. Att utveckla sociala indikatorer: en surveyansats belyst med exempel arbetsmiljö. Stockholm: Statisktiska Centralbyrån; 1991. [Google Scholar]
- 30.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 31.Carlson LE, Thomas BC. Development of the Calgary Symptoms of Stress Inventory (C-SOSI) Int J Behav Med. 2007;14:249–56. doi: 10.1007/BF03003000. [DOI] [PubMed] [Google Scholar]
- 32.Brantley PJ, Waggoner CD, Jones GN, Rappaport NB. A Daily Stress Inventory: development, reliability, and validity. J Behav Med. 1987;10:61–74. doi: 10.1007/BF00845128. [DOI] [PubMed] [Google Scholar]
- 33.Weston R, Gore PA. A brief guide to structural equation modeling. Couns Psychol. 2006;34:719–51. [Google Scholar]
- 34.Kline RB. Principles and practice of structural equation modeling. 2nd ed. New York: Guilford; 2005. [Google Scholar]
- 35.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–46. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 36.Hu L-T, Bentler PM. Evaluating model fit. In: Hoyle RH, editor. Structural equation modeling: concept, issues, and applications. Thousand Oaks CA: Sage; 1995. pp. 76–99. [Google Scholar]
- 37.Steiger JH. Structural Model Evaluation and Modification - an Interval Estimation Approach. Multivar Behav Res. 1990;25:173–80. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- 38.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 39.Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- 40.Kline RB. Principles and practice of structural equation modeling. New York: The Guilford Press; 1998. [Google Scholar]
- 41.Sobel ME. Asymptotic intervals for indirect effects in structural equation models. In: Leinhart S, editor. Sociological methodology. Washington, DC: American Sociological Association; 1982. pp. 290–312. [Google Scholar]
- 42.Taris TW, Kompier MA. Games researchers play--extreme-groups analysis and mediation analysis in longitudinal occupational health research. Scand J Work, Environ Health. 2006;32:463–72. doi: 10.5271/sjweh.1051. [DOI] [PubMed] [Google Scholar]
- 43.Cole DA, Maxwell SE. Testing mediational models with longitudinal data: questions and tips in the use of structural equation modeling. J Abnorm Psychol. 2003;112:558–77. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- 44.Sinokki M, Ahola K, Hinkka K, et al. The association of social support at work and in private life with sleeping problems in the Finnish health 2000 study. J Occup Environ Med. 2010;52:54–61. doi: 10.1097/JOM.0b013e3181c5c373. [DOI] [PubMed] [Google Scholar]
- 45.Nordin M, Knutsson A, Sundbom E. Is disturbed sleep a mediator in the association between social support and myocardial infarction? J Health Psychol. 2008;13:55–64. doi: 10.1177/1359105307084312. [DOI] [PubMed] [Google Scholar]
- 46.Nakashima M, Morikawa Y, Sakurai M, et al. Association between long working hours and sleep problems in white-collar workers. J Sleep Res. 2011;20:110–6. doi: 10.1111/j.1365-2869.2010.00852.x. [DOI] [PubMed] [Google Scholar]
- 47.Yoo SS, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep--a prefrontal amygdala disconnect. Curr Biol. 2007;17:R877–8. doi: 10.1016/j.cub.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 48.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 49.Åkerstedt T, Orsini N, Petersen H, Axelsson J, Lekander M, Kecklund G. Predicting sleep quality from stress and prior sleep - A study of dayto-day covariation across six weeks. Sleep Med. 2012;13:674–9. doi: 10.1016/j.sleep.2011.12.013. [DOI] [PubMed] [Google Scholar]
- 50.Buysse DJ, Cheng Y, Germain A, et al. Night-to-night sleep variability in older adults with and without chronic insomnia. Sleep Med. 2010;11:56–64. doi: 10.1016/j.sleep.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]


