Abstract
Study Objectives:
To document the time course of perceived stress among women through the period of a natural disaster, to determine the effect of sleep quality on this time course, and to identify risk factors that predict higher levels of perceived stress.
Design:
Longitudinal study from 2006–2012.
Setting:
Community-based family planning clinics in southeast Texas.
Participants:
There were 296 women aged 18–31 y who experienced Hurricane Ike, September 2008.
Measurements and Results:
Cohen Perceived Stress Scale (PSS) was administered every 2 mo from 6 mo before to 12 mo after Hurricane Ike. Sleep quality was assessed 1 mo after Hurricane Ike using the Pittsburg Sleep Quality Index (PSQI). Good sleep was defined as a PSQI summary score < 5, and poor sleep as a score ≥ 5. Hurricane Ike stressors (e.g., property damage, subjective stressors) and pre-Ike lifetime major life events and emotional health (e.g., emotional dysregulation, self-control) were also assessed.
Results:
Over the entire period of 18 mo (6 mo before and 12 mo after the hurricane), perceived stress was significantly higher among poor sleepers compared to good sleepers, and only good sleepers showed a significant decrease in perceived stress after Hurricane Ike. In addition, a higher level of perceived stress was positively associated with greater Ike damage among poor sleepers, whereas this correlation was not observed among good sleepers. In the final multivariate longitudinal model, Ike-related subjective stressors as well as baseline major life events and emotional dysregulation among poor sleepers predicted higher levels of perceived stress over time; among good sleepers, additional factors such as lower levels of self-control and having a history of a psychiatric disorder also predicted higher levels of perceived stress.
Conclusions:
Sleep quality after Hurricane Ike, an intense natural disaster producing substantial damage, impacted changes in perceived stress over time. Our findings suggest the possibility that providing victims of disasters with effective interventions to improve sleep quality could help to reduce their perceived stress over time.
Citation:
Wu ZH, Stevens RG, Tennen H, North CS, Grady JJ, Holzer C. Sleep quality among low-income young women in southeast texas predicts changes in perceived stress through hurricane Ike. SLEEP 2015;38(7):1121–1128.
Keywords: natural disaster, sleep quality, stress, women
INTRODUCTION
Poor sleep is one of the most prevalent, yet underaddressed, health concerns in the modern world.1,2 Perceived stress is also an important aspect of coping that has received increasing interest as a potential health threat.3–5 Sleep quality and perceived stress are undoubtedly related,6,7 but it is unclear whether poor sleep causes stress or vice versa. Data suggest that sleep problems correlate with past traumatic life event experiences.8 A recent review reported that sleep problems commonly occur among people exposed to trauma, particularly those who develop posttraumatic stress disorders (PTSD).9 However, cross-sectional data supporting this conclusion provides only limited information regarding the secondary versus central nature of sleep in the genesis of PTSD. Predisaster information can help determine whether sleep problems are caused by such traumatic experiences. Thus, we aimed to examine whether predisaster major life events and emotional health, as well as disaster-related factors like the degree of damage experienced, would predict sleep quality immediately post disaster.
The extent to which poor sleep increases stress versus stress compromising sleep quality is not clear. When challenged by untoward events, such as natural disasters, people's reactions differ.10–12 Natural disasters are often followed by emotional distress, as well as injuries and illnesses, in affected populations.10,11 However, the typical absence of data collected before disasters has rarely permitted prospective study of the course of stress symptoms through a disaster period.10,11
The eye of Hurricane Ike made landfall at Galveston, Texas on September 13, 2008 as a strong, 600-mile-wide Category 2 storm. This storm was one of the most destructive in Texas state history, with a 20-foot storm surge pushing a wall of water across a wide area and flooding that extended far inland. As many as 4 million people in the region were without power for several weeks.
Reported consequences of Hurricane Ike included short-term and long-term mental and physical health problems,13–15 but as in previous disaster research, these reports did not obtain in-depth data before and after the storm. We examined the effect of sleep quality on the time course of perceived stress from 6 mo before through 1 y after Hurricane Ike among 296 low-income women living in the Galveston area.
METHODS
Study Design and Sampling
The data for the current analysis originated from a larger longitudinal study of stress and substance use in young women conducted from November 2006 through January 2012 in southeast Texas. Participants were patients attending one of six University of Texas Medical Branch (UTMB) community-based family planning clinics serving primarily low-income women with an average annual income of $7,000. Inclusion criteria were: (1) female; (2) not pregnant; (3) aged 18 y or older; (4) non-Hispanic white, non-Hispanic black, or Hispanic; (5) able to speak English or Spanish; and (6) able to consent. This study was approved by the UTMB Institutional Review Board.
Formal written consent was obtained in English or Spanish and was renewed annually throughout the study. Participants completed face-to-face interviews at the baseline, as well as 12 mo and 24 mo post-Ike. In addition, four bimonthly telephone interviews were conducted between the annual interviews. Participants were reimbursed for their time and travel costs. Of 1,363 women invited to participate, 886 accepted and provided consent. Hurricane Ike struck the geographical study area at approximately the midpoint of the original longitudinal study.
For the purposes of this investigation, the original 24-mo study data were restructured according to the Hurricane Ike timeline. Because participant availability was limited at this point in the study, a subgroup of 403 women from the study was subsequently requested to answer additional Ike-related questions. These women were interviewed starting 1 mo after Hurricane Ike. Participants in the post-Ike subgroup did not differ from the larger sample in age, education, employment status, or race. However, more women in the post-Ike subgroup had a steady boyfriend (36%) or were married (23%) as compared with the total study population (33% and 19%, respectively); whereas fewer women in the post-Ike subgroup were cohabitating (19%) or did not have a steady partner (23%) compared to the total study population (20% and 28%, respectively) (P < 0.05). Of these post-Ike study participants, 88 were recruited after September 2008 and were excluded due to lack of data collected before Hurricane Ike. An additional 19 participants were excluded because of missing sleep information. A total of 296 women with complete sleep measures and pre-Ike and post-Ike stress measures were retained. In comparing subject participating in the analysis (n = 296) with those who were excluded from analysis (n = 107), no significant differences were found in age, race, education, marital status, employment status, or psychiatric diagnosis.
Measures and Instruments
Timeline of Hurricane Ike
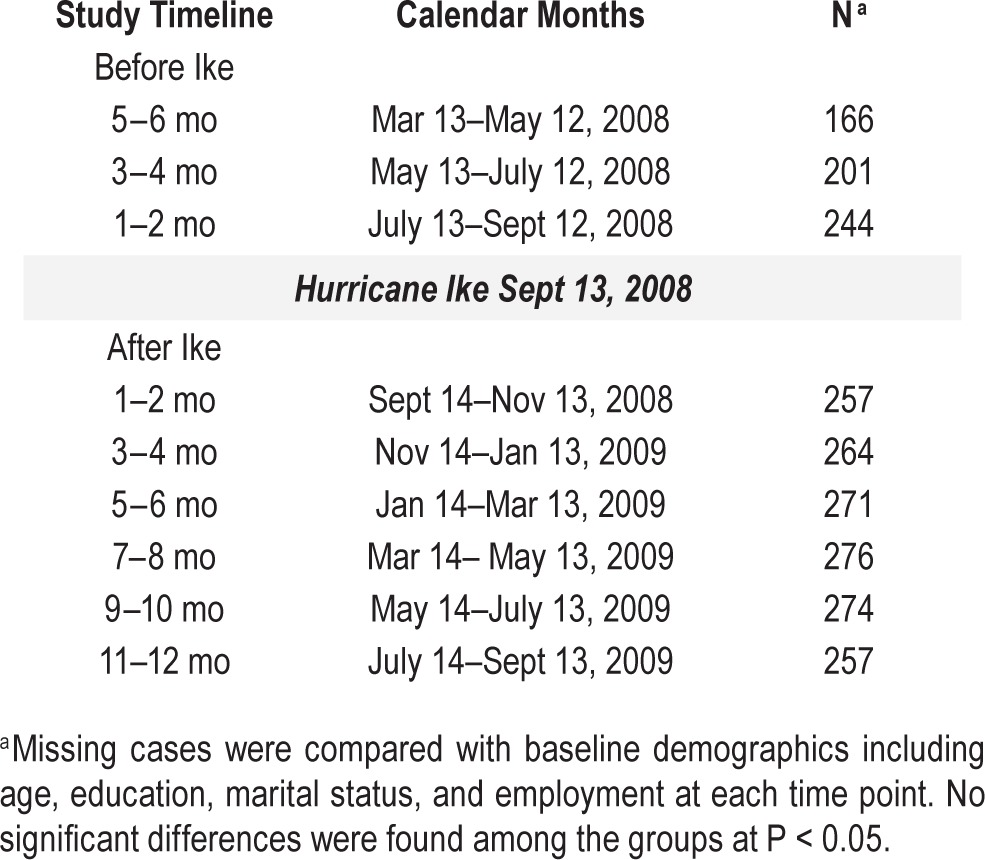
Each of the 296 women's interview dates were assigned to a timeline according to the time period in which they were conducted. Time periods included 3–4 mo and 1–2 mo prior to Hurricane Ike and six additional time periods after Ike (see Table 1).
Table 1.
Study timeline and calendar months for a study of young, low-income women in the southeast Texas (n = 296).
Cohen Perceived Stress Scale (PSS)
This 10-item scale measures the degree to which life situations are appraised as stressful during the last 30 days using a five-point Likert scale.16 Summary score ranges from 0 (no stress) to 40 (high stress), and the mean for women in the United States in the normative samples was about 16.1.3 For this study, the PSS was administered at baseline and every 2 mo for the duration of the study. Cronbach α at baseline was 0.84.
Sleep Quality
The quality of sleep was assessed using the Pittsburgh Sleep Quality Index (PSQI), which measures the quality and patterns of sleep in seven domains during the past month (e.g., subjective sleep quality, use of sleep medication) on a 0 to 3 scale.17 An overall score of 5 or greater indicates poor sleep. In the current study, the PSQI was administered 30 days after Hurricane Ike.
Hurricane Ike Stressors
Selected items from the Disaster Supplement Questionnaire18 were administered to the post-Ike subgroup. Two sets of questions were selected for analysis. The first set of questions involved tangible stressors including six categories of damage (i.e., property/houses, external structure, furniture, appliances, motor vehicles and sentimental possessions [e.g., pets, family photo albums or family videos]) that were rated on a five-point scale of “none,” “slight damage,” “moderate damage,” “severe damage,” and “total destruction. For analysis, responses were combined to indicate either “none to minimum damage” (= 0) or “more severe damage” (= 1). The second set of questions were related to subjective stressors that included family arguments, embarrassment or humiliation, feeling isolated, and fear of crime. Summary indicators of both stressors were created separately by summing corresponding items with higher scores indicative of more stressful exposures.
Hurricane Ike Assistance Applied for
The Disaster Supplement Questionnaire18 asked participants to indicate the agencies to which they had applied for assistance after Hurricane Ike. The agencies listed included the Federal Emergency Management Agency, state local police, other parts of state and local government, the National Guard and armed forces, other parts of the federal government, the Red Cross, other relief agencies, insurance companies, and the American public. A summary index was created representing any Ike assistance applied for, which served as a proxy for any assistance needed.
Other Covariates
At baseline, demographic information was obtained including age, race, marital status, employment, and education. Lifetime psychiatric disorders of major depression, generalized anxiety disorder, substance use disorder, and posttraumatic stress disorder were assessed at baseline using the Composite International Diagnostic Interview—World Health Organization version (WHO CIDI 2.1).19 In addition, standard instruments assessing major life events,20 emotional dysregulation,21 and self-control22 were completed at baseline.
Statistical Analyses
Descriptive statistics were used to compare demographic characteristics of the study sample as stratified according to sleep quality. Cross-tabulation was performed for categorical variables and t tests were used for continuous variables. When baseline life events, emotional health, and Ike stressor variables were used to predict sleep quality, the SAS logistic procedure (SAS version 9.4, SAS Institute, Cary, NC)23 was used. Perceived stress over time as the outcome variable was analyzed using a repeated measures generalized linear mixed model (SAS MIXED procedure, SAS version 9.4, SAS Institute),23 and an autoregressive process AR(1) was used to model the covariance structure. These models produce unbiased marginal estimates of effect when missing observations can be assumed to be missing at random.24 We tested the main effect of sleep status after Ike against perceived stress over time, as well as the main effect of stress over the period of time from 6 mo before to 12 mo after Hurricane Ike. Then, using the grouping factor “sleep quality,” we investigated whether there was a group × time interaction to determine whether the relationship between sleep quality and perceived stress changed over time. We tested differences in the mean stress level at each post-Ike time point and compared this to the 2 mo immediately before the disaster. We also tested the interaction between sleep quality and the primary exposure (i.e., Ike stressors) on perceived stress over time. A significant interaction would indicate that the relationship between sleep quality and perceived stress differed depending on the extent of Ike stressors. If a significant interaction was detected, the final multivariate model was analyzed separately according to sleep quality. These models use Ike stressor summary variables and risk factors assessed at baseline interviews to predict the time course of stress.
RESULTS
Overall, the mean score of the PSQI was 4.2 (standard deviation [SD] = 3.3), with 39% having a total summary score of PSQI ≥ 5, and thus classified as poor sleepers shortly after Hurricane Ike (Table 2). As expected, a significant association was detected between the post-Ike PSQI and overall sleep quality from the baseline pre-Ike questionnaire (P < 0.01). However, there were no significant differences in sleep quality between any of the baseline demographic variables.
Table 2.
Baseline background characteristics and Hurricane Ike sleep quality description of low-income women from the southeast Texas (n = 296).
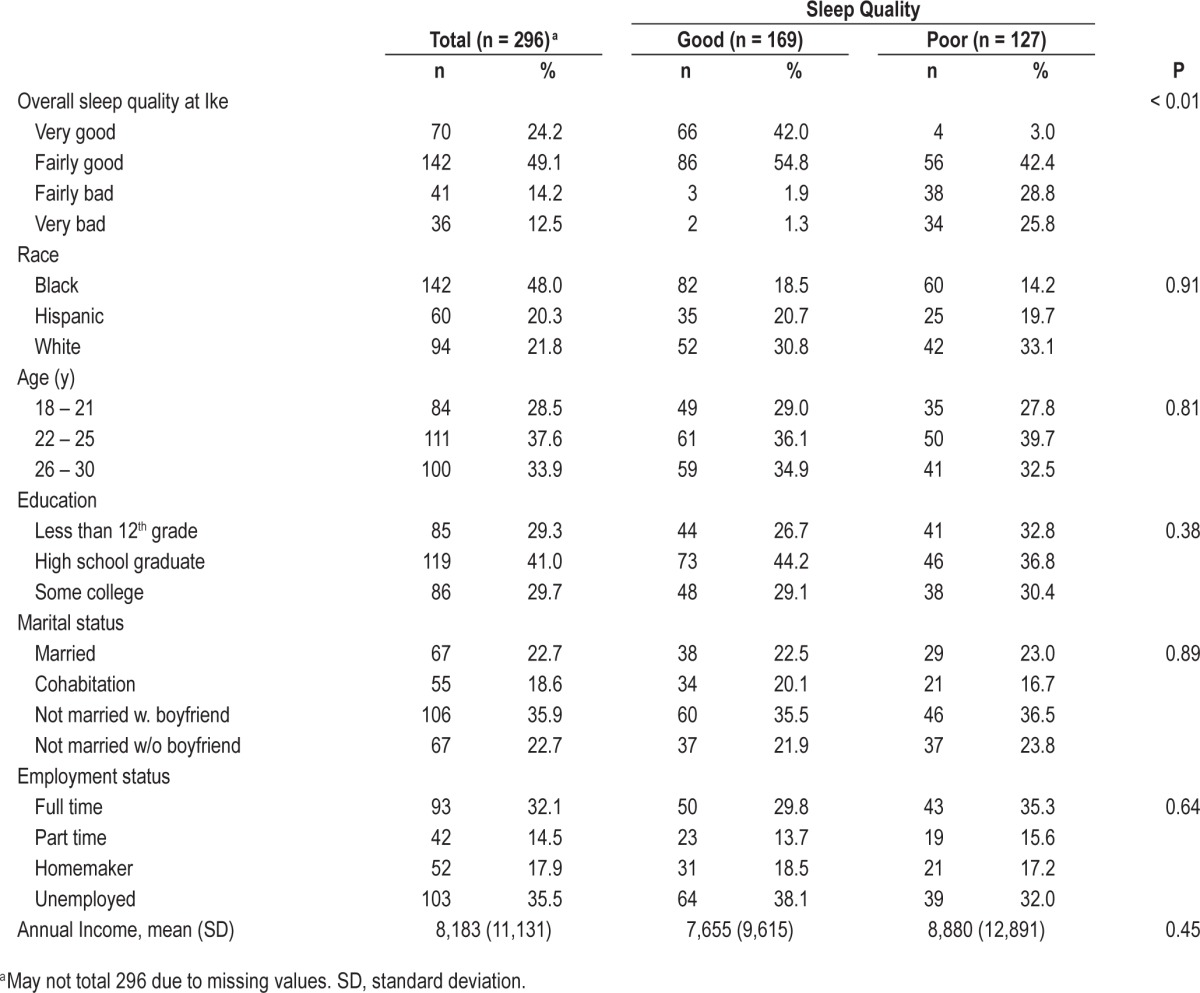
Figure 1 depicts a significant interaction between sleep quality and time period, indicating that the difference in perceived stress between good and poor sleepers followed a different pattern after Hurricane Ike than before (Den DF = 1824, F = 2.33, P = 0.018). Over the 18-mo study period, average perceived stress scores among good sleepers, as determined shortly after Ike, ranged from 16.9 (SD = 9.3) 6 mo before Ike to 12.8 (SD = 8.0) 1 y after Ike; and the scores began to decline after Ike, being significantly lower from 3–4 mo (average 2.56 points lower, P < 0.001) through 12 mo (average 2.68 points lower, P < 0.003) after Ike. In contrast, the range of perceived stress scores for poor sleepers was 20.2 (SD = 8.4) before Ike to 16.7 (SD = 9.3) after Ike. The scores for poor sleepers remained high after Ike compared to before (P > 0.05), with the single exception of 5–6 mo post-Ike (average 2.3 points lower, P = 0.005). In addition, the main effect of sleep quality on stress was significant (estimate = 1.89, P < 0.05), indicating that poor sleepers were almost twice as likely to experience higher levels of perceived stress as good sleepers.
Figure 1.
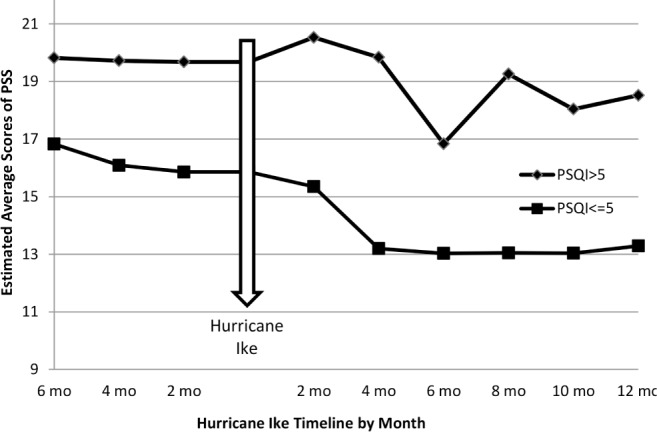
Estimated average scores of Perceived Stress Scale (PSS) by the Pittsburgh Sleep Quality Index (PSQI).
Table 3 shows the bivariate distribution of sleep quality with baseline (pre-Ike) measurements of major life events, emotional dysregulation, and self-control, and Ike-related experiences including stressors (tangible and subjective) and assistance applied for. All these factors were significantly associated with sleep quality (P < 0.05).
Table 3.
Bivariate statistical estimates to describe the relationshipa between sleep quality and baseline experiences and Hurricane Ike stressors.
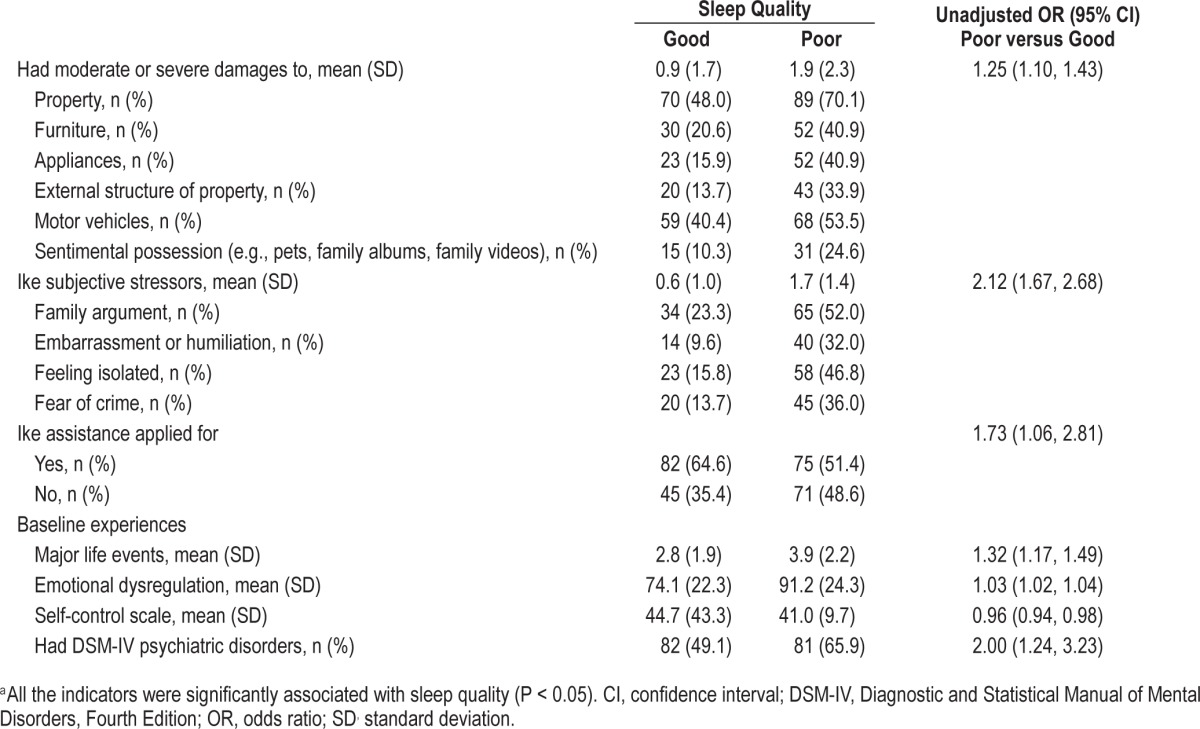
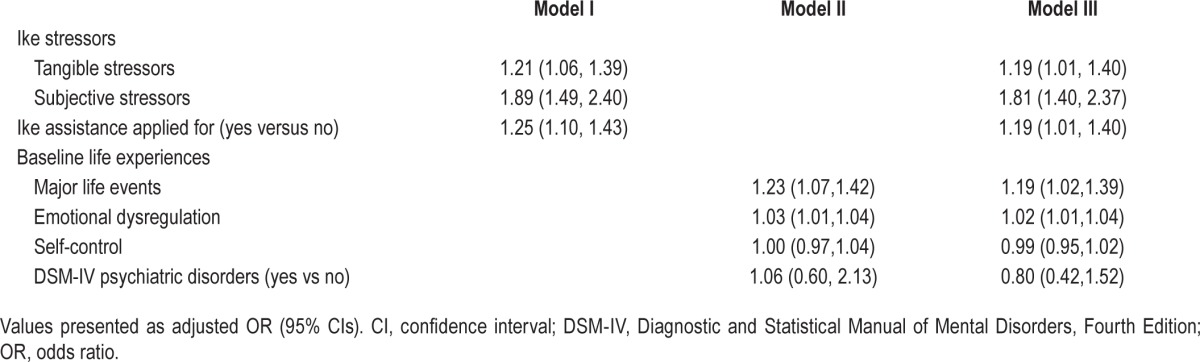
Table 4 shows adjusted odds ratios (ORs) for the effects of both pre-Ike and post-Ike stressors and emotional health on sleep quality in three models, all of which control for the demographic variables. Model I included baseline life experiences, Model II included Ike stressors, and Model III included both. In Model III, baseline reports of lifetime major life events (OR = 1.19, 95% confidence interval [CI]: 1.02, 1.39) and emotional dysregulation (OR = 1.02, 95% CI: 1.01, 1.04) were both significant predictors of poor sleep after Hurricane Ike, as were the post-Ike tangible stressors (OR = 1.19, 95% CI: 1.01, 1.40) and subjective stressors (OR = 1.81, 95% CI: 1.40, 2.37).
Table 4.
Adjusted odds ratios to predict poor sleep after Hurricane Ike by baseline life experiences and Ike stressors.
We then assessed the interaction of sleep quality and Ike tangible stressors on perceived stress over time. After controlling for main effects as well as the interaction of sleep quality and the Ike time period (Figure 1), the interaction was statistically significant (P < 0.05), as indicated in Figure 2. Among poor sleepers, levels of perceived stress increased as the number of Ike tangible stressors increased. In contrast, among the good sleepers, levels of perceived stress did not show significant changes associated with number of Ike tangible stressors, except for a slight increase correlated with reported experience of one Ike stressor.
Figure 2.
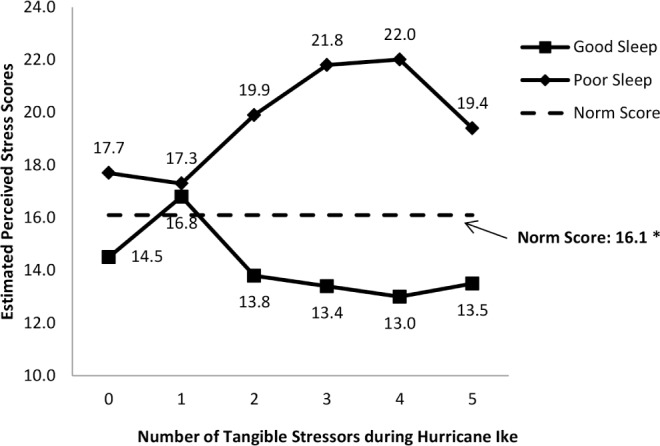
Estimated perceived stress scores by number of Hurricane Ike tangible stressors and sleep status. *The norm score from Cohen S, Janicki-Deverts D. Who's stressed? Distribution of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol 2012;42:1320–34.
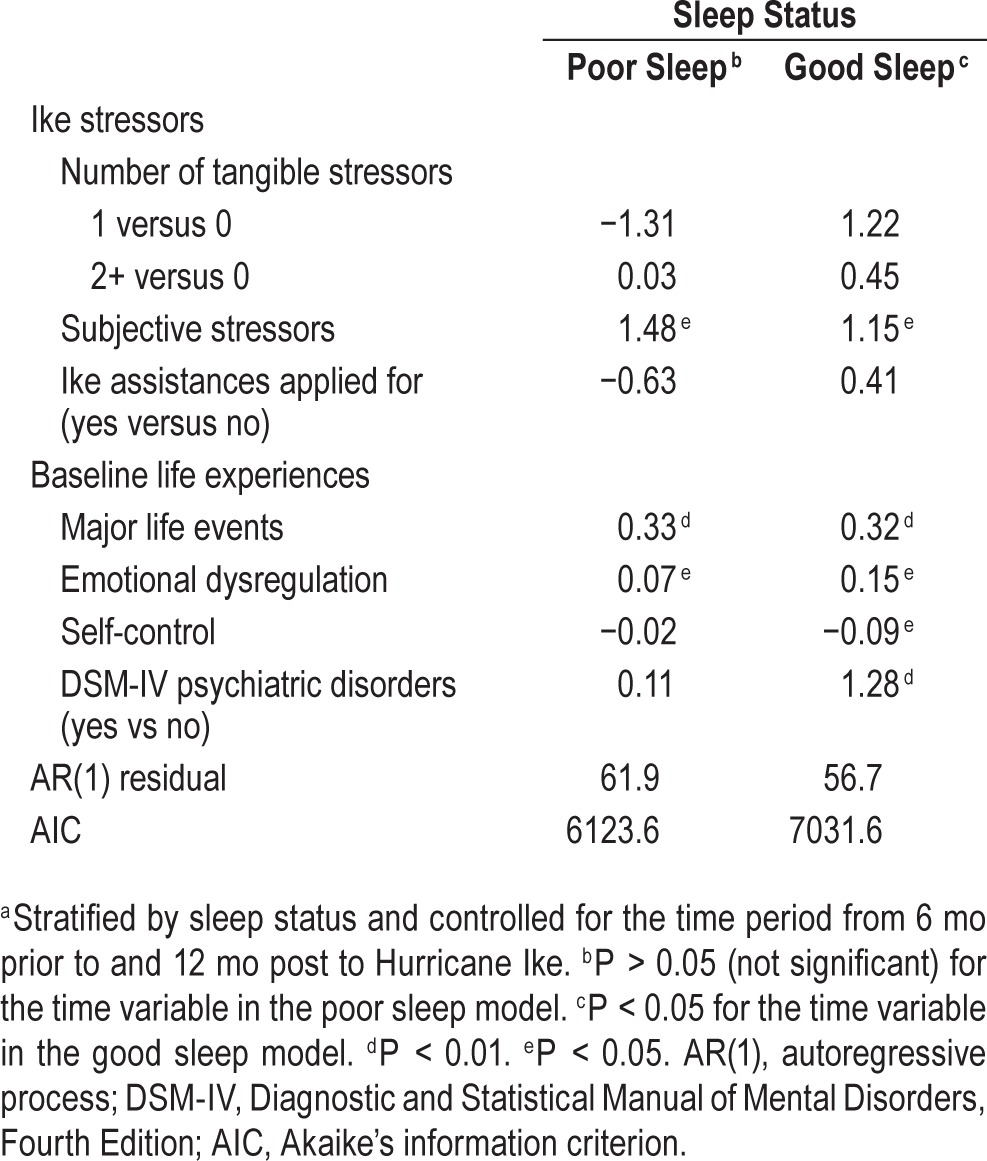
Because of the interactions between sleep quality and Ike stressors, we analyzed the effect of these stressors on perceived stress separately for good sleepers and poor sleepers (Table 5). Among both good sleepers and poor sleepers, baseline emotional dysregulation and more major life events before Ike were associated with higher levels of perceived post-Ike stress. For example, among poor sleepers, a one-unit increase in subjective stress increased the perceived stress score by 1.48 (P < 0.05). Among the good sleepers, lower self-control and diagnosis of any psychiatric disorder at baseline were both associated with greater perceived stress over time. For example, a one-unit increase in self-control reduced the score of perceived stress by 0.09 (P < 0.05).
Table 5.
Multivariate stratified longitudinal modelsa to predict perceived stress over time by baseline life experiences and Ike stressors.
DISCUSSION
In a sample of young, low-income women in southeast Texas who experienced Hurricane Ike in 2008, sleep quality was assessed once after Ike using the PSQI. About 39% of women were classified as poor sleepers. In a cross-sectional study of low-income young women from the same family planning program, Kachikis and Breitkopf7 found that 44% of participants reported their sleep quality as less than “good,” and sleep quality, assessed with a single question, was inversely associated with perceived stress. Sleep quality, including short sleep, varies among women according to demographic characteristics such as age, education level, employment status, and number of children. Mindell et al.25 examined sleep quality among a large sample of mothers of young children in 14 countries and correlated poor sleep with lower educational level, lower income, and having a younger child. They reported that 59% of subjects in the United States were poor sleepers. In addition, Patel et al.26 found that poor sleep (also using one question) was associated with poverty, and that African-American and Latino residents in greater Philadelphia were more likely to report poor sleep than Whites. Our results are consistent with those previously reported in women.
We found that both baseline experiences (lifetime major life events, emotional dysregulation) and subjective Ike stressors predicted sleep quality in both unadjusted bivariate analyses (Table 3) and adjusted multivariate analyses (Table 4). Thus, obtaining such predisaster information in this population may be valuable for disaster preparedness. It also indicates that the effect of the disaster itself on sleep quality may be independent of predisaster factors. Incorporating both predisaster and disaster-related experiences may benefit recovery efforts.
In our study, sleep quality was related to the time course of perceived stress as measured at many time points beginning before Ike through 1 y after. Good sleepers fared considerably better than poor sleepers. Prather et al.27 used the PSQI to categorize 289 women as “good” or “poor” sleepers and found that sleep quality was inversely associated with perceived stress level. In another cross-sectional study of African American women, poorer sleep quality on the PSQI was correlated with higher perceived stress.28 However, these studies lacked longitudinal data to determine changes in stress and sleep quality over time. A substantial body of literature has examined stressful experiences and sleep quality in relation to traumatic events, including natural disasters.10,11,29 Disasters generate a wide range of stressors on individuals and their communities over time. In addition, adverse outcomes may accrue or become apparent over time.10,11,30 However, after examining 225 samples of ≥ 85,000 individuals who experienced 132 distinct disasters between 1981 and 2004, Norris and associates10,11 noted that only 10 samples (4.4%) included data obtained before the disaster. They concluded that “studies using pre-post design were much less likely to find severe (or very severe) effects than were studies using after-only designs.”11 To our knowledge, our study is one of the few with a reasonable sample size that describes a longitudinal time course over the period of a natural disaster with measures collected before the disaster.
It is interesting to note that perceived stress decreased after Hurricane Ike among good sleepers. McMillen et al.31 explored the concept of “perceived benefit” after a disaster, in which people who believe they have somehow benefitted from the disaster show greater recovery after the event than those who perceived no benefit. The perceived benefits included “community became closer,” “enhanced closeness,” and “personal growth.” The effect is greater with more severe disaster exposure. Perceived benefit may also interact with sleep quality. Hamilton et al.32 found that higher quality sleep buffers the relationship between stress and negative affect and the relationship between pain and both positive and negative affect. These investigators suggested that high-quality sleep acts as a biobehavioral resource that reduces allostatic load. This buffering may exert its effect by modulating negative affect in response to stressful encounters, or by maximizing the use of effective coping strategies.
Our study also identified multiple risk factors to predict higher levels of perceived stress for both poor and good sleepers. First, subjective stressors experienced during Hurricane Ike (e.g., family arguments, embarrassment or humiliation, feeling isolated, fear of crime) were associated with higher levels of stress. Second, major life events and emotional dysregulation assessed at baseline were also associated with higher perceived stress. Awareness of these factors may help disaster aid workers refine and focus psychosocial relief efforts for victims of natural disasters.
A primary limitation of this study was that sleep quality was assessed only once shortly after the hurricane, therefore poor sleep in some women may have simply been related to greater property damage and hardship. However, sleep quality was associated with perceived stress even after controlling for hurricane-related stressors and damages. In addition, both major life events and emotional dysregulation at baseline predicted poor sleep after Ike. This suggests that sleep quality was not simply an acute state reflecting the trauma of Ike. Sleep quality, even after the hurricane, seems to primarily reflect womens' long-term experiences. Because our sample included only women of lower socioeconomic status, generalizations to men and to more economically stable individuals must be approached with caution.
Although sleep quality was assessed only once after Hurricane Ike, it was clearly associated with perceived stress even before Ike. It is salient to consider whether sleep problems intensified perceived stress or whether stress caused the sleep problems. If it is the former, then measures to improve sleep quality in low-income women are warranted as stress prevention interventions. If it is the latter, however, efforts to cope more effectively with stressful experiences would be beneficial for mitigating disaster-related sleep problems. This distinction is important because although education about improving sleep quality is clear and often feasible (e.g., dark, quiet bedroom; dim lights in the evening; early lights out), interventions to reduce stress among low-income women are more difficult and frequently involve factors beyond a woman's control (e.g., violence, food insecurity); however, interventions can help women develop improved skills to better cope with adversity.
In summary, our findings provide new insights that could be used to design multilevel, individualized, or targeted strategies for disaster preparedness and interventions, potentially including initial sleep quality screening. Conventional, traditional preparedness measures may be sufficient for low-income women with good sleep habits and without any predisaster emotional needs. However, additional targeted inventions could be useful for good sleepers who may have experienced more major life events and those with greater emotional needs (i.e., higher levels of emotional dysregulation and lower levels of self-control). For poor sleepers, a systematic, comprehensive preparedness and intervention is recommended.
DISCLOSURE STATEMENT
This was not an industry supported study. Funding was provided by the National Institutes of Health, National Institute on Drug Abuse, DA020058 and DA021814 and National Institute on Alcohol Abuse and Alcoholism, P30 AA019358. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Margarita Morgardo, Arely Duran, Didi Rivas, Diane Rosaly, Sultana Nasrin, and Ebony Green (UTMB) for data collection; and Yimei Han (UTMB) for data management and analysis. These individuals were funded as part of the research team by Dr. Wu's NIH grants. We also thank the UTMB Department of Obstetrics and Gynecology and Maternal Child Health Regional Program, where Dr. Wu was a faculty member (2000–2010), for their support of the study. We also thank for Zhuo Wang and Yu-Bo Wang, Department of Statistics, University of Connecticut for their contributions to data management and preliminary data analyses and Laura L. Mallary for her editorial assistance. Authorship responsibility: Dr. Wu had full access to all the data in the study, took full responsibility for the integrity of the data and the accuracy of the data analysis, and had final responsibility for the decision to submit for publication; Study concept and design: Drs. Wu, Holzer, Grady, and North; Acquisition of data: Drs. Wu, Holzer, and Grady; Analysis and interpretation of data: Drs. Wu, Grady, Stevens, Tennen, and Holzer; Drafting of the manuscript: Drs. Wu, Stevens, Tennen, Holzer, and North; Critical revision of the manuscript for important intellectual content: Wu, Stevens, Tennen, Holzer, and North; Statistical analysis: Drs. Wu and Grady; Obtained funding: Drs. Wu, Holzer, and Grady; Administrative, technical, or material support: Drs. Wu, Holzer, and Grady; Study supervision: Drs. Wu and Holzer. The study was conducted at the University of Texas Medical Branch, Galveston, TX. The study was approved by the University of Texas Medical Branch Institutional Review Board on human subject research (#03-238) and appropriate informed consent was obtained from study participants.
REFERENCES
- 1.Buysse DJ. Insomnia. JAMA. 2013;309:706–16. doi: 10.1001/jama.2013.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldstein AN, Walker MP. The role of sleep in emtional brain function. Annu Rev Clin Psychol. 2014;10:679–708. doi: 10.1146/annurev-clinpsy-032813-153716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen S, Janicki-Deverts D. Who's stressed? Distribution of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol. 2012;42:1320–34. [Google Scholar]
- 4.Lockley SF, RG . Sleep: a very short introduction. New York: Oxford University Press; 2012. [Google Scholar]
- 5.Ferrie JE, Kumari M, Salo P, Singh-Manoux A, Kivimäki M. Sleep epidemiology—a rapidly growing field. Int J Epidemiol. 2011;40:1431–7. doi: 10.1093/ije/dyr203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Reeth O, Weibel L, Spiegel K, Leproult R, Dugovic C, Maccari C. Interactions between stress and sleep: from basic research to clinical situations. Sleep Med Rev. 2000;3:201–19. [Google Scholar]
- 7.Kachikis AB, Breitkopf CR. Predictors of sleep characteristics among women in southeast Texas. Womens Health Issues. 2012;22:e99–109. doi: 10.1016/j.whi.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lavie P. Sleep disturbances in the wake of traumatic events. N Engl J Med. 2001;345:1825–32. doi: 10.1056/NEJMra012893. [DOI] [PubMed] [Google Scholar]
- 9.Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. J Anxiety Disord. 2010;24:1–15. doi: 10.1016/j.janxdis.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981-2001. Psychiatry. 2002;65:207–39. doi: 10.1521/psyc.65.3.207.20173. [DOI] [PubMed] [Google Scholar]
- 11.Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: Part II. Summary and implications of the disaster mental health research. Psychiatry. 2002;65:240–60. doi: 10.1521/psyc.65.3.240.20169. [DOI] [PubMed] [Google Scholar]
- 12.Norris FH, Tracy M, Galea S. Looking for resilience: understanding the longitudinal trajectories of responses to stress. Soc Sci Med. 2009;68:2190–8. doi: 10.1016/j.socscimed.2009.03.043. [DOI] [PubMed] [Google Scholar]
- 13.Norris FH, Sherrieb K, Galea S. Prevalence and consequences of disaster-related illness and injury from Hurricane Ike. Rehabil Psychol. 2010;55:221–30. doi: 10.1037/a0020195. [DOI] [PubMed] [Google Scholar]
- 14.Pietrzak RH, Southwick SM, Tracy M, Galea S, Norris FH. Posttraumatic stress disorder, depression, and perceived needs for psychological care in older persons affected by Hurricane Ike. J Affect Disord. 2012;138:96–103. doi: 10.1016/j.jad.2011.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perry M, Banerjee D, Slentz M, et al. Hurricane Ike rapid needs assessment-Houston, Texas, September 2008. MMWR. 2009;58:1066–71. [PubMed] [Google Scholar]
- 16.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 17.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 18.North CS, Pfefferbaum B. The diagnostic interview schedule/disaster supplement questionnaire. St. Louis, MO: Washington University; 2002. [Google Scholar]
- 19.Kessler RC, Abelson J, Demler O, et al. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI) Int J Methods Psychiatr Res. 2004;13:122–39. doi: 10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turner RJ, Lloyd DA. The stress process and the social distribution of depression. J Health Soc Behav. 1999;40:374–404. [PubMed] [Google Scholar]
- 21.Gratz K, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26:41–54. [Google Scholar]
- 22.Tangney JP, Baumeister RF, Boone AL. High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. J Pers. 2004;72:271–324. doi: 10.1111/j.0022-3506.2004.00263.x. [DOI] [PubMed] [Google Scholar]
- 23.SAS Institute, Inc. SAS/STAT 9.4: User's Guide. Cary, NC: SAS Institute, Inc; 2014. [Google Scholar]
- 24.Fitzmaurice G, Laird N, Ware J. Applied longitudinal analysis. Hoboken, NJ: John Wiley & Sons; 2004. [Google Scholar]
- 25.Mindell JA, Sadeh A, Kown R, Goh DY. Cross-cultural comparison of maternal sleep. Sleep. 2013;36:1699–706. doi: 10.5665/sleep.3132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patel N, Grandner M, Xie D, Branas C, Gooneratne N. “Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010;10:475. doi: 10.1186/1471-2458-10-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prather AA, Bogdan R, Hariri AR. Impact of sleep quality on amygdala reactivity, negative affect, and perceived stress. Psychosom Med. 2013;75:350–8. doi: 10.1097/PSY.0b013e31828ef15b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bidulescu A, Din-Dzietham R, Coverson DL, et al. Interaction of sleep quality and psychosocial stress on obesity in African Americans: the Cardiovascular Health Epidemiology Study (CHES) BMC Public Health. 2010;10:581. doi: 10.1186/1471-2458-10-581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bryant RA, Creamer M, O'Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. 2010;33:69. doi: 10.1093/sleep/33.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.North CS, Oliver J. Analysis of the longitudinal course of PTSD in 716 survivors of 10 disasters. Soc Psychiatry Psychiatr Epidemiol. 2013;48:1189–97. doi: 10.1007/s00127-012-0639-x. [DOI] [PubMed] [Google Scholar]
- 31.McMillen JC, Smith EM, Fisher RH. Perceived benefit and mental health after three types of disaster. J Consult Clin Psychol. 1997;65:733–9. doi: 10.1037//0022-006x.65.5.733. [DOI] [PubMed] [Google Scholar]
- 32.Hamilton NA, Catley D, Karlson C. Sleep and the affective response to stress and pain. Health Psychol. 2007;26:288–95. doi: 10.1037/0278-6133.26.3.288. [DOI] [PubMed] [Google Scholar]


