Abstract
Study Objectives:
This study challenged on a bench-test the efficacy of auto-titrating positive airway pressure (APAP) devices for obstructive sleep disordered breathing treatment and evaluated the accuracy of the device reports.
Methods:
Our bench consisted of an active lung simulator and a Starling resistor. Eleven commercially available APAP devices were evaluated on their reactions to single-type SDB sequences (obstructive apnea and hypopnea, central apnea, and snoring), and to a long general breathing scenario (5.75 h) simulating various SDB during four sleep cycles and to a short scenario (95 min) simulating one sleep cycle.
Results:
In the single-type sequence of 30-minute repetitive obstructive apneas, only 5 devices normalized the airflow (> 70% of baseline breathing amplitude). Similarly, normalized breathing was recorded with 8 devices only for a 20-min obstructive hypopnea sequence. Five devices increased the pressure in response to snoring. Only 4 devices maintained a constant minimum pressure when subjected to repeated central apneas with an open upper airway. In the long general breathing scenario, the pressure responses and the treatment efficacy differed among devices: only 5 devices obtained a residual obstructive AHI < 5/h. During the short general breathing scenario, only 2 devices reached the same treatment efficacy (p < 0.001), and 3 devices underestimated the AHI by > 10% (p < 0.001). The long scenario led to more consistent device reports.
Conclusion:
Large differences between APAP devices in the treatment efficacy and the accuracy of report were evidenced in the current study.
Citation:
Zhu K, Roisman G, Aouf S, Escourrou P. All APAPs are not equivalent for the treatment of sleep disordered breathing: a bench evaluation of eleven commercially available devices. J Clin Sleep Med 2015;11(7):725–734.
Keywords: auto-titrating continuous positive airway pressure, obstructive sleep apnea, bench test, central sleep apnea, device report
Obstructive sleep apnea syndrome is caused by repetitive closure of the upper airway during sleep that leads to episodes of arterial oxygen desaturation and interrupted sleep. Continuous positive airway pressure (CPAP) delivered via a nasal mask is an effective treatment for obstructive sleep apnea (OSA).1 It is the reference treatment for patients with moderate-to-severe OSA2,3 and has been shown to improve nocturnal and diurnal symptoms of OSA, objective and subjective measures of daytime somnolence, quality of life, and also been demonstrated to reduce driving accidents.4–6 When hypertension coexists with OSA, CPAP may reduce blood pressure.7 As with many therapies for chronic conditions, compliance is a major issue. It ranges in the literature from 20% to 83%.8–12
As opening airway pressure may vary during the night with position, sleep stage, drug or alcohol use, attempts to improve compliance and treatment efficacy have included the use of auto-titrating CPAP (APAP). These devices are designed to vary and achieve the necessary pressure to maintain airway patency throughout the sleep. Their mechanism of action proposes that the reduction in mean pressure minimizes side effects of CPAP, improving tolerance and increasing associated usage.13
BRIEF SUMMARY
Current Knowledge/Study Rationale: Auto-titrating positive airway pressure devices are designed to adjust the therapeutic pressure to maintain the upper airway patency and treat the obstructive sleep disordered breathing. The efficacy of treatment is questioned and clinical evaluations are curtailed by the variability of disease in patients.
Study Impact: All APAPs performed differently when subjected to simulated sleep disordered breathing patterns on a bench-test. Large differences exist in the treatment efficacy and accuracy of the device report data between APAP devices.
But studies to date have not identified a statistically significant difference between APAP and fixed CPAP devices in compliance or in Epworth Sleepiness scores.14 Patruno et al.15 favored fixed pressure over APAP for reducing cardiovascular risk, although data on blood pressure outcomes were limited.
The clinical efficacy of APAP has also been questioned by some studies showing a large residual apnea-hypopnea index (AHI) with some devices.16 Reports of residual events obtained by the devices have also been questioned by some authors.17–22 Moreover, FDA approval for introducing a new APAP device to the market does not guarantee its effectiveness and safety, as manufacturers may gain entry to the market by “510(k) premarket notification,” which relies on a “substantial equivalence” to an existing device, or by demonstrating safety and effectiveness with limited clinical studies.23 Since clinical studies are curtailed by the variability between patients and study conditions, an overall picture of their results is not clear. Bench studies are advantageous over clinical ones as they allow evaluating devices in standardized and quite reproducible conditions.24,25
As many APAP devices are now released on the market, we wished to evaluate their functioning and the validity of their reports that are often used by physicians as measures of efficacy. Eleven devices were evaluated on a new bench using patient-simulated events and disease scenarios close to the actual observations in patients.
METHODS
Materials
The bench model is mainly composed of an active lung simulator ASL5000 (IngMar Medical, Pittsburgh, USA) and a Starling resistor (Figure 1).25,26 It is able to reproduce normal and disordered breathing patterns, e.g., obstructive and central apneas and hypopneas.
Figure 1. Principle of the bench model.
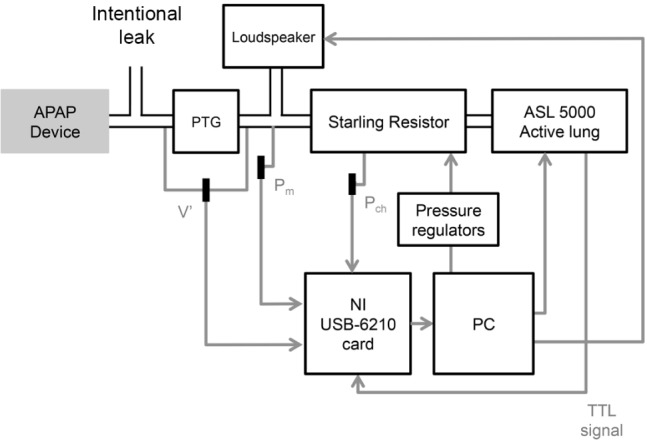
PTG, pneumotachograph; V', measured mask flow; Pm, measured mask pressure; Pch, measured chamber pressure of the Starling resistor; TTL, transistor-transistor logic; Intentional leak, intentional leak of nasal mask, of which the airflow was calibrated to 24 L/min at 10 cm H2O.
The Starling resistor within a cylindrical transparent chamber (180 mm long, 28 mm internal diameter) consisted of a compliant rubber tube (120 mm long between two 15-mm external diameter connectors at each side of the cylinder). The chamber was connected to a pressure control system (MFCS-4C-70 and MFCS-NEG-4C-70, Fluigent, Villejuif, France), which supplied continuous positive and negative pressures around the tube inside the chamber (Pch). The Pch regulated the opening state of the rubber tube that represented the pharynx, and this pressure was monitored by a manometer (MECOSMARTD-06, Mesureur, Chilly-Mazarin, France). The upper airway obstruction and snoring were triggered and synchronized to the breathing via a transistor-transistor logic (TTL) signal sent by the ASL5000 at the beginning of breathing cycles, in order to mimic the pathophysiology of OSA. During obstructive apneas, the critical closing pressure and the full opening pressure measured at the mask were 6 and 11 cm H2O, respectively.
The APAP device was connected to a calibrated leak port (24 L/min at 10 cm H2O) built in the patient circuit,25,26 which presented a standardized intentional leak at the mask.27 A linear pneumotachograph (series 4700A, Hans Rudolph, Shawnee, USA) was connected downstream to the leak port. The mask pressure and airflow were measured by PA-1 flow instrumentation (series 1110A, Hans Rudolph). A wireless speaker (UE984-000298, Logitech) was placed in a hermetic chamber connected to the mask to generate snoring.
All data were transferred to a PC via a NI USB-6210 card (National Instruments, Austin, USA), and a LabView (National Instruments) program was developed for data acquisition and instrument control. All the recorded signals were sampled at 20 Hz for further analysis.
Bench Model Principles
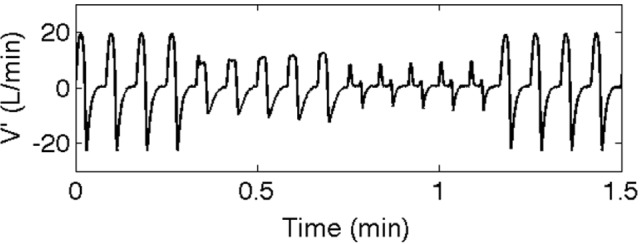
The breathing flow patterns resulted from the interactions of the ASL5000 with the Starling resistor.26 The following settings were applied to the lung model: uncompensated residual capacity = 0.5 L, compliance = 80 mL/cm H2O, resistance = 5 cm H2O/L/s, and inspiratory flow amplitude of normal breathing = 20 L/min. To maintain the inspiratory efforts during obstructive sleep disordered breathing (SDB) events, the ASL5000 was switched to flow pump mode and produced normal breathing flow. The lung was set as passive during central apneas (central apneas in this paper refer to the ones without cardiac oscillation if not specified). All central apneas occurred with an open upper airway. For obstructive apnea, the pressure inside the chamber of the Starling resistor (Pch) was set at 9 cm H2O. By modifying the settings of the lung simulator and the Pch, different waveforms of airflow could be achieved (Figure 2). All the SDB patterns were produced at 4 cm H2O airway pressure as minimal default value of APAP devices. For normal breathing and central apneas, the Pch was −8 cm H2O and the upper airway was fully opened.
Figure 2. Airflow waveforms of the obstructive hypopnea.
The snoring sound was extracted from a patient sleep recording. The high-frequency elements were filtered out and its peak power was at 46 Hz.
The presence of cardiac oscillations on the airflow may be considered as an indicator of open upper airway in central apneas and may be used in some APAP algorithms.28 The cardiac oscillations were simulated by the active lung as 1-Hz sinusoidal airflow of 2 L/min (10% of baseline amplitude).
The opening of the upper airway at the resumption breathing after the obstructive apneas might result in a so-called “obstructive pressure peak” at mask.29 To produce this signal, the upper airway was opened with a 0.5-sec delay with regard to the TTL signal, i.e., the flow pump started breathing prior to the opening of the upper airway.
Devices under Study
Eleven APAP devices were included in the study: iCH Auto (Apex, New Taipei City, Taiwan), RESmart Auto (BMC, Beijing, China), iSleep20i (Breas, Mölnlycke, Sweden), Floton Auto (Curative, Beijing, China), SleepCube Auto (Devilbiss, Somerset, USA), ICON+ (Fisher & Paykel, Auckland, New Zealand), PR1 Remstar Auto P-Flex (Philips Respironics, Murrysville, USA), S9 AutoSet (Resmed, Sydney, Australia), DreamStar Auto (Sefam, Viller-lès-Nancy, France), Transcend Auto (Somnetics, New Brighton, USA), and SOMNOBalance-e (Weinmann, Hamburg, Germany). These devices were numbered from D1 to D11. Treatment reports were extracted through the corresponding software of each device.
The minimum and maximum pressures of the devices were set at 4 and 20 cm H2O, respectively. Pressure ramp and comfort mode were disabled.
Test Protocols
Single-Type SDB Event Sequences
Five flow sequences of single-type SDB events were developed. Brief descriptions of these sequences are summarized in Table 1. Illustrations of these sequences are shown in Figures 2–4.
Table 1.
Sequence of single-type SDB events.
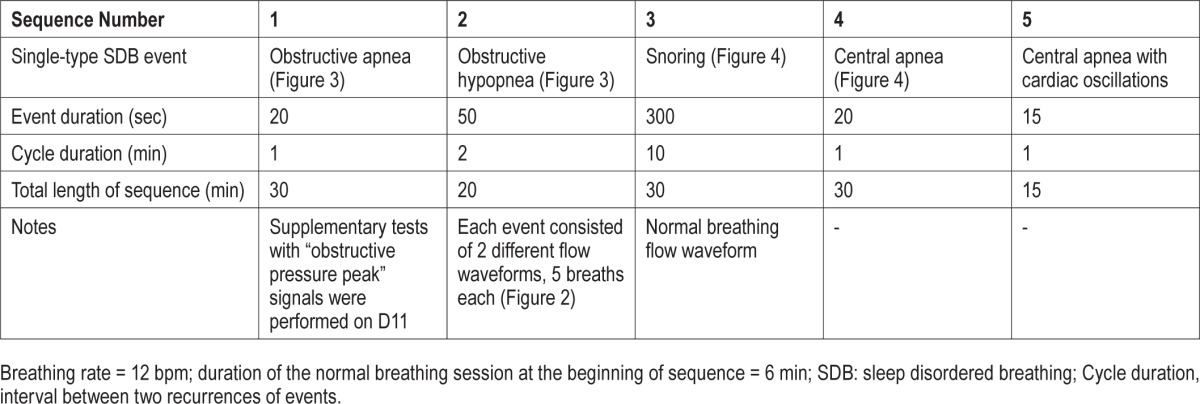
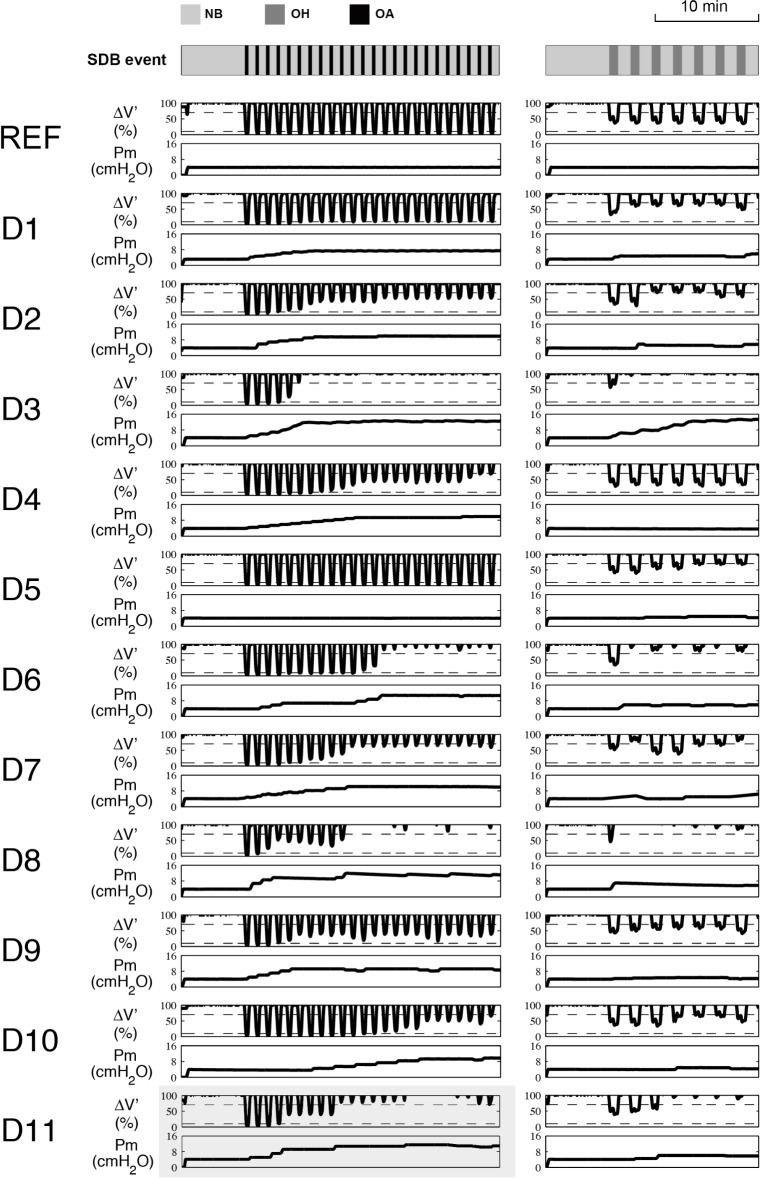
Figure 3. Illustration of single-type SDB event sequences and results: obstructive apnea (left column) and hypopnea (right column).
The SDB events and the sequences are indicated in the top line, in which the bars represent the apneas or hypopneas, with a width proportional to the duration of the event. The dashed lines in the panels of ΔV' represent 10% and 70% of baseline flow amplitude. Curves in gray panel at the bottom: “obstructive pressure peak” signals were simulated at the resumption breathing after the apnea. Of note, without this “obstructive pressure peak” signal, pressure of D11 did not change and remained at initial value. ΔV', airflow amplitude, expressed in percentage of the amplitude of normal breathing airflow. Pm, mask pressure; NB, normal breathing; OH, obstructive hypopnea; OA, obstructive apnea; REF, reference test, carried out with a constant positive pressure = 4 cm H2O; D1, iCH Auto; D2, RESmart Auto; D3, iSleep20i; D4, Floton Auto; D5, SleepCube Auto; D6, ICON+; D7, PR1 Remstar Auto; D8, S9 AutoSet; D9, DreamStar Auto; D10, Transcend Auto; D11, SOMNOBalance-e. For apnea, D3, D6, D7, D8, D10, and D11 (with “obstructive pressure peaks”) were able to normalize the breathing flow; hypopneas still remained in D1, D2, D4, and D9; apnea remained unchanged in D5. For hypopnea, D1, D2, D3, D5, D6, D7, D8, and D11 normalized the airflow, hypopneas remained in D4, D9, and D10.
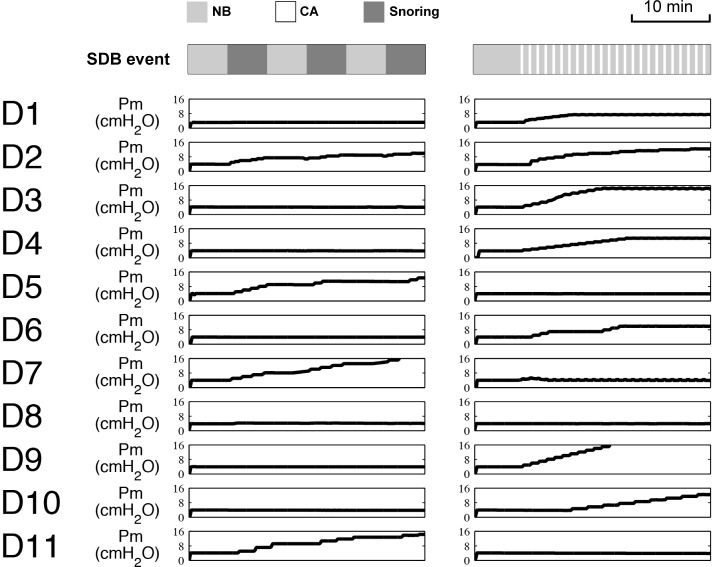
Figure 4. Illustration of single-type SDB event sequences and results: snoring (left column) and central apnea without cardiac oscillations (right column).
The SDB events and the sequences are indicated in the top line, in which the bars represent the snoring or central apnea, with a width proportional to the duration of the event. Since the tests of central apnea with cardiac oscillations showed the same results as those without oscillations, they are not shown in this figure. Pm, mask pressure; NB, normal breathing; CA, central apnea; D1, iCH Auto; D2, RESmart Auto; D3, iSleep20i; D4, Floton Auto; D5, SleepCube Auto; D6, ICON+; D7, PR1 Remstar Auto; D8, S9 AutoSet; D9, DreamStar Auto; D10, Transcend Auto; D11, SOMNOBalance-e. During snoring, D2, D5, D7, D8, and D11 increased the pressure. In central apneas, D5, D7, D8, and D11 did not increase the pressure.
General Scenarios
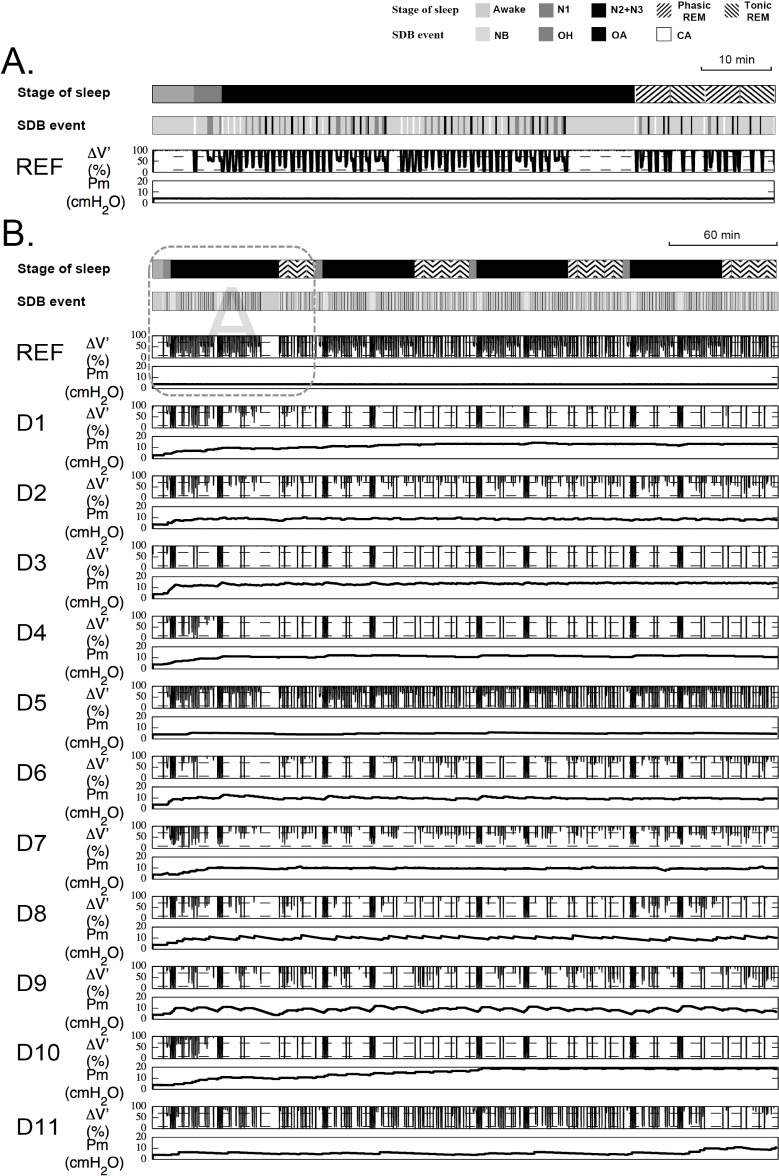
In addition to repetitive single-type SDB events, we developed 2 breathing scenarios, which included a distribution of mixed SDB events to simulate clinical and complex conditions (Figure 5). The long scenario lasted 5.75 h, including a 6-min normal breathing session, which corresponded to awake state of patient, and 4 complete sleep cycles each lasting about 1.4 h. The breathing rate and the frequency of SDB events were adapted to the sleep stages as observed in sleep disorders. The duration of the events also varied. For example, the first sleep cycle consisted of a 4-min “N1 sleep stage” at 12 bpm breathing rate with few events, a 60-min “N2+N3 sleep stages” at 12 bpm with numerous events of all types including central apneas, and a 20-min “REM sleep stage” with variable breathing rate (Figure 5A). Most SDB events were set up in the N2+N3 stages. A 10-min normal breathing session was placed at the end of N2+N3 part in order to verify if the absence of SDB events could prompt a gradual decrease in pressure. The 20-min REM sleep was composed of 4 alternated 5-min sessions of “phasic” and “tonic” REM, where the breathing rate varied from 10 to 15 bpm in “phasic” REM and remained steady at 12 bpm in “tonic” REM with predominantly obstructive SDB events. For the entire scenario, the total AHI set on the bench was 51.4/h, of which 75% of events were obstructive (obstructive AHI = 38.6/h) and 25% were central. Of note, snoring, “obstructive pressure peak” signals, and cardiac oscillations were not simulated in this scenario. For the first sleep cycle part in the general scenario (the first 95-min session), the total AHI was equal to 44.8/h, of which 73% of events were obstructive (obstructive AHI = 32.8/h). The short scenario lasted 95 min, which corresponded to the first sleep cycle of the long scenario.
Figure 5. Illustration of the general scenarios and results.
(A) Short general scenario, which corresponded to the first sleep cycle in the long general scenario (the framed part in B). (B) long general scenario with 4 sleep cycles. In both two panels, the simulated stages of sleep are shown in the first line. The SDB events and the scenario are indicated in the second line, in which the bars indicate corresponding SDB events. The width of bars is proportional to the duration of the event. The dashed lines in the ΔV' panels represent 10% and 70% of baseline flow amplitude. Of note, snoring, cardiac oscillations and “obstructive pressure peak” signal were not simulated in either scenario. NB, normal breathing; OH, obstructive hypopnea; OA, obstructive apnea; CA, central apnea; ΔV', airflow amplitude, expressed in percentage of the amplitude of normal breathing airflow; Pm, mask pressure; REF, the resultant flow amplitude and mask pressure of the reference test, which was carried out with a constant positive pressure = 4 cm H2O; D1, iCH Auto; D2, RESmart Auto; D3, iSleep20i; D4, Floton Auto; D5, SleepCube Auto; D6, ICON+; D7, PR1 Remstar Auto; D8, S9 AutoSet; D9, DreamStar Auto; D10, Transcend Auto; D11, SOMNOBalance-e. All devices decreased their pressure after a 10-min normal breathing session except D3. D9 decreased its pressure most rapidly during the 10-min normal breathing session.
Methodology
For reproducibility, tests of single-type SDB events and of the long scenario were repeated twice. A third test was executed if the coefficient of variation of the first 2 tests was > 10%. Tests of the short scenario were repeated 3 times for each device. For each sequence or scenario, a baseline reference test was completed with a fixed CPAP = 4 cm H2O.
Data Analysis
For the obstructive apnea and hypopnea sequences, mask pressure (Pm) and airflow-derived peak-to-peak flow amplitude (ΔV', derived by calculating the upper and lower envelops of the flow curve) were recorded and calculated. Pm curves were uniquely presented for the snoring and central apnea sequences. Regarding the general scenarios, the mean/median pressure and P90/95 were calculated from the Pm. Residual AHI was scored by analyzing the flow curve. Precisely, the residual events were scored by considering both the amplitude reduction and the corresponding duration, i.e., ΔV' ≤ 10% of normal baseline: apnea; 10% < ΔV' ≤ 70%: hypopnea, with a duration ≥ 10 seconds.26,30 All the analyses mentioned above were performed with MATLAB (MathWorks Inc., Natick, USA).
The differences in treatment efficacy (residual AHI) and in therapy pressure between devices and between bench-assessed and device-reported data were investigated by repeated measures analysis of variance (rANOVA) with these 2 factors. Further rANOVA was conducted for each device to compare the bench-assessed and device-reported AHI if the global difference was found significant (Medcalc Software, Mariakerke, Belgium).
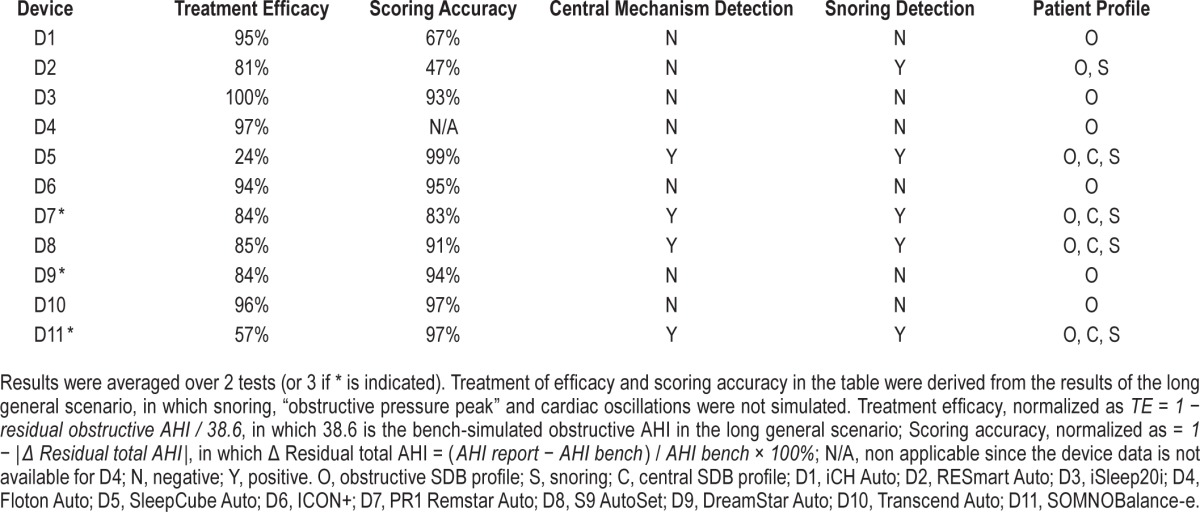
For an overview, each device was scored based on its treatment efficacy and accuracy of device-reported residual AHI. Also, devices were classified according to specific clinical profile, such as treatment of snoring, apneas of obstructive and central mechanisms. The following results were normalized and chosen as criteria: (1) the percentage of normalized obstructive events for the long general scenario (denoted as treatment efficacy, normalized as TE = 1 − residual obstructive AHI / 38.6); (2) the consistency in residual AHI between bench and device (denoted as scoring accuracy, normalized as = 1 − |Δ Residual total AHI|, in which Δ Residual total AHI = (AHI report − AHI bench) / AHI bench × 100%); (3) reactions to snoring, and (4) reactions to central apneas (graded as Yes or No).
RESULTS
Single-Type SDB Event Sequences
Obstructive Apnea Sequence
According to the resultant flow, in percentage of the normal baseline amplitude, at the end of the sequence, the devices fell into 3 categories: (A) resultant flow > 70%: D3, D6, D7, D8, and D10—especially D3 and D8—fully normalized the breathing flow; (B) 10% < resultant flow ≤ 70%, i.e., hypopneas still remained: D1, D2, D4, and D9; (C) resultant flow ≤ 10%: D5 and D11 (Figure 3).
The time to reach the maximum pressure varied from device to device. In category A, D8 reached the maximum pressure most rapidly, at 14.8 min, i.e., before the middle of the sequence, D10 increased its pressure most slowly and the airflow was normalized only at the end of the sequence. D3 reached the highest pressure (13.5 cm H2O) among all the devices. Two devices in category C did not change their pressure during the entire tests (D5 and D11). Of note, D11 performed differently when the “obstructive pressure peak” signal was presented: the ΔV' was enhanced to 70.2% and its pressure reached at 11.4 cm H2O with a delay of 20.1 minutes (Figure 3).
Obstructive Hypopnea Sequence
Similarly to the obstructive apnea test, the devices fell into 2 categories according to the resultant flow at the end of the 20-min sequence: (A) resultant flow > 70%: D1, D2, D3, D5, D6, D7, D8, and D11—of which D3 and D11 fully normalized the breathing flow; (B) resultant flow ≤ 70%: D4, D9, and D10, of which D4 did not change its pressure during the tests (Figure 3). In category A, D2, D6, D8, and D9 reached the maximum pressure before the middle of the sequence; of these, D8 increased its pressure most rapidly. D3 recorded the highest pressure (12.6 cm H2O) among the devices.
Snoring Sequence
Devices were divided into 2 categories according to the pressure change when snoring was presented. (A) D2, D5, D7, D8, and D11 increased the pressure; (B) D1, D3, D4, D6, D9, and D10 kept their pressure at the initial value (Figure 4).
Central Apnea Sequence with/without Cardiac Oscillations
Devices fell into 2 categories according to the pressure change during central apneas: (A) D5, D7, D8, and D11 kept the same EPAP during the test; (B) D1, D2, D3, D4, D6, D9, and D10 increased their pressure. In category B, D1, D4, and D6 limited their maximum pressures around 10 cm H2O. The Pm curves are shown on Figure 4.
For central apneas with cardiac oscillations, all the devices reacted in the same way as for the central apneas without cardiac oscillation.
General Scenarios
All devices decreased their pressure after a 10-min normal breathing session in the first sleep cycle except D3 (Figure 5B). D9 decreased its pressure most rapidly by 4.8 cm H2O during the 10-min normal breathing session (Figure 5B).
In the long scenario, bench-measured mean/median treatment pressures and P90/95 differed between devices (p < 0.001, Figure 6A, 6B). D1, D3, D4, and D10 had a mean treatment pressure > 10 cm H2O (Figure 6A). D10 showed the highest P90 = 19.5 cm H2O (Figure 6B). The residual obstructive AHI on the bench that revealed the efficacy of treatment also differed significantly between devices (p < 0.001): D1, D3, D4, D6, and D10 obtained a residual obstructive AHI < 5/h, among which D3 totally eliminated the obstructive SDB events (Figure 6C). The Pm and flow curves are shown in Figure 5. For all devices, the differences between bench-assessed and device-reported AHI and pressure data were not significant.
Figure 6. Comparison between bench-measured and device-reported results of the long general scenario.
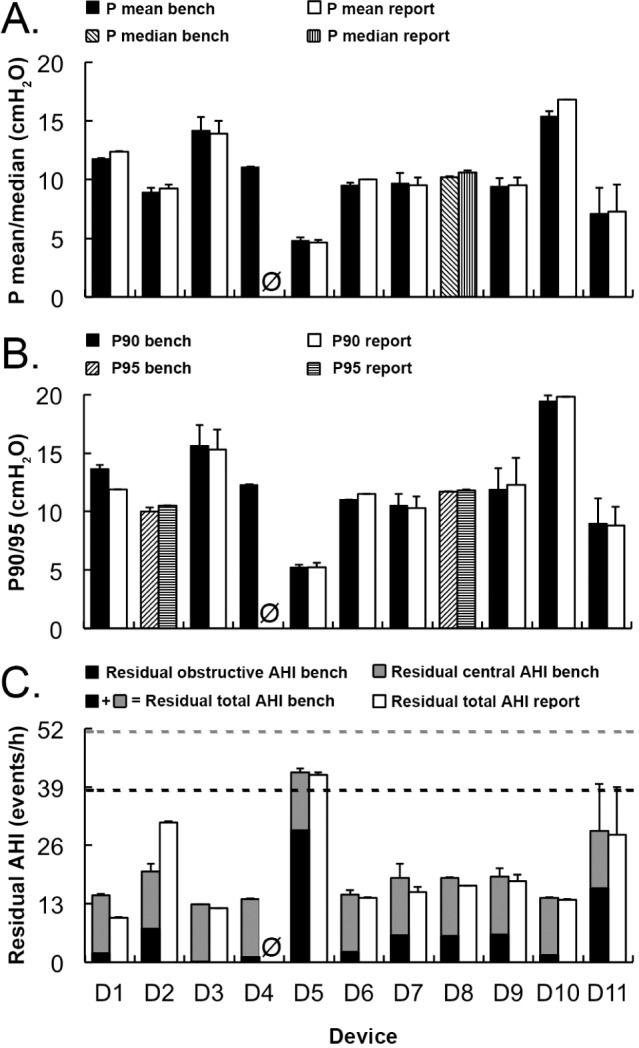
(A) Mean (median for D8) pressure, (B) P90 (P95 for D2 and D8), and (C) residual AHI. Results were averaged over 2 tests (or 3 if * is indicated) and the standard deviations were presented. Ø: device-reported data were not available for D4. In C, two horizontal dashed lines represent bench-simulated total AHI (51.4/h) and obstructive AHI (38.6/h). Treatment efficacy of each device can be revealed from the gap between the “residual obstructive AHI bench” (black) and the “simulated obstructive AHI” (lower dashed line). Repeated measures analysis of variance showed that bench-measured mean/median treatment pressures and P90/95 were different between devices (p < 0.001), and the bench-assessed residual obstructive AHI also differed significantly between devices (p < 0.001). No difference found between bench-assessed and device-reported data. D1, iCH Auto; D2, RESmart Auto; D3, iSleep20i; D4, Floton Auto; D5, SleepCube Auto; D6, ICON+; D7, PR1 Remstar Auto; D8, S9 AutoSet; D9, DreamStar Auto; D10, Transcend Auto; D11, SOMNOBalance-e. The device-reported AHI for D5 is calculated as the sum of AHI and non-responding event index (NRI) shown on reports.
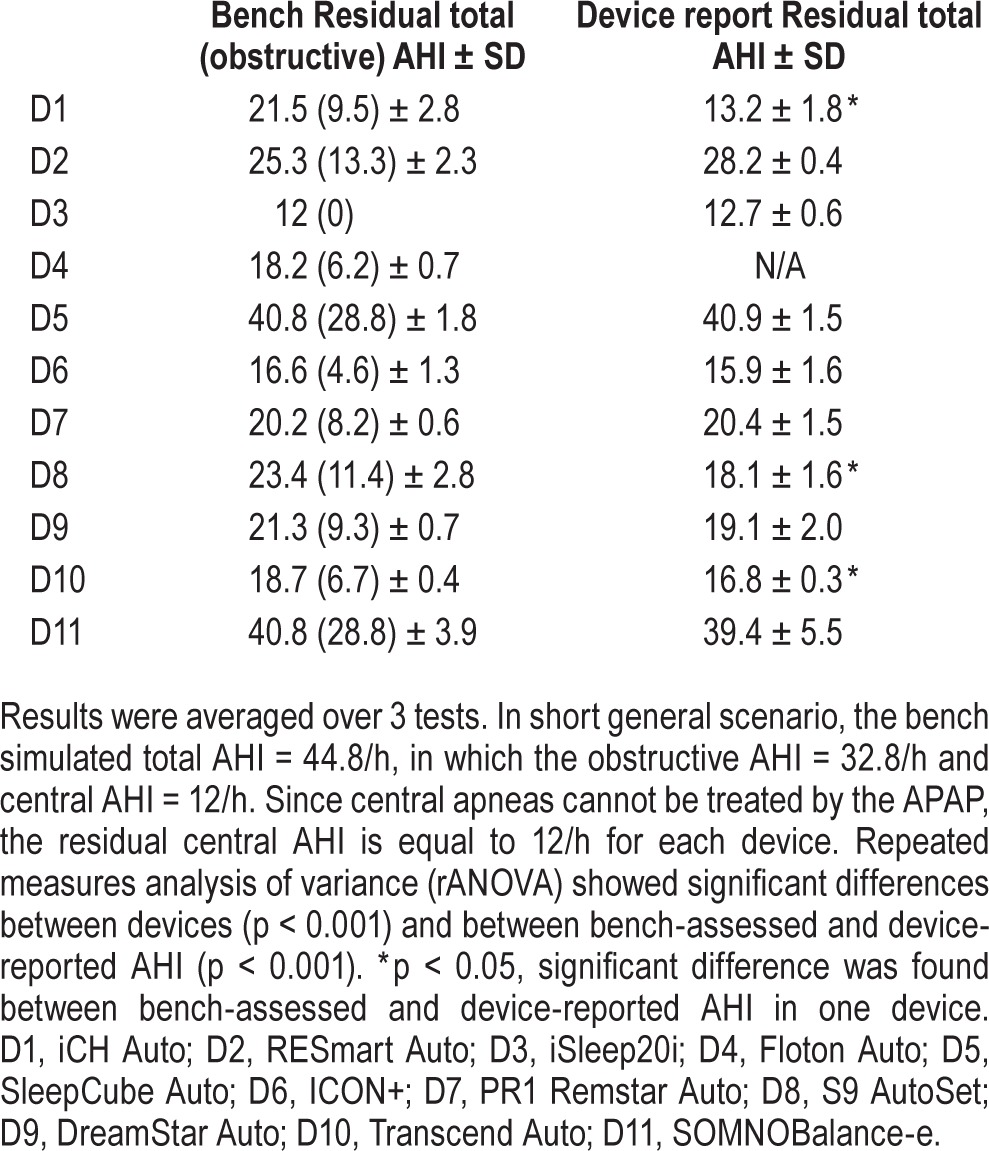
In the short scenario, significant differences were found in mean/median pressure and in P90/95 (p < 0.001 for each). D3 and D6 had a mean pressure > 10 cm H2O. Device-reported mean/median pressure data were different from measured pressure (p < 0.001). D1 overestimated the mean therapy pressure by > 10% (p = 0.01). Residual obstructive AHI differed between devices (p < 0.001, Table 2): only D3 and D6 obtained a residual obstructive AHI < 5/h. For D3, the residual obstructive AHI = 0 (Table 2). Device-reported AHI were different to bench-assessed ones (p < 0.001). D1, D8, and D10 underestimated the AHI by 39%, 23%, and 11%, respectively (p < 0.05 for each).
Table 2.
Bench-assessed and device-reported AHI in short general scenario.
DISCUSSION
This study is the most extensive evaluation of APAP devices to date using a new closed-loop respiratory bench model taking into account not only the mechanical properties of human upper airway, but also the lung characteristics, such as compliance and resistance. With this bench test, eleven currently marketed APAP devices were challenged by three different protocols: short sequences of constant repetitive single-type SDB events, as well as by two general breathing scenarios including a variety of events to approach actual clinical conditions. The devices were investigated on both the performance and on the accuracy of the device reports. The main findings were as follows: (1) most devices responded to simulated obstructive apneas (except D5 and D11) and obstructive hypopneas (except D4), but their reaction time and their treatment efficacy considerably differed. D11 only responded to the obstructive apneas when “obstructive pressure peak” signals were added; (2) 5 devices raised the pressure when subjected to the snoring sound (D2, D5, D7, D8, D11); (3) when central apneas were simulated, only 4 devices did not rise the pressure (D5, D7, D8, D11); (4) For the long scenario, efficacy varied between devices: only 5 devices obtained a residual obstructive AHI < 5/h (D1, D3, D4, D6, D10); (5) For the short scenario, significant differences were found in therapy pressure and in efficacy between devices and between bench-assessed and device-reported data: only 2 devices obtained a residual obstructive AHI < 5/h (D3, D6) whereas 3 devices underestimated the AHI by > 10% (D1, D8, D10).
Regarding the long scenario, only 5 of 11 devices (D1, D3, D4, D6, and D10) showed effectiveness, i.e., the residual obstructive AHI < 5/h, owing to their higher therapy pressure (Figure 6A, 6B). Noteworthy, their prompt responses in pressure were linked to the inability to differentiate between central and obstructive apneas (Figure 5). Also, only D3 did not decrease the pressure when the normal breathing resumed. However, when the pressure dropped too fast, the treatment that resumed after the normal breathing session was insufficient (e.g., D9, Figure 5). These differences between devices in residual AHI were probably due to the inconsistencies between the definitions of SDB events in airflow amplitude in comparison to the recommendations regarding the flow amplitude thresholds.30 The treatment was not always efficient for the short scenario. Some devices resulted in a high amount of residual obstructive SDB events even when their pressure increased, as they reached the equilibrium with a significant lag time (e.g., D1, D4, and D10).
Device D5 did not respond to any simulated apnea. Such an apnea with the flow amplitude lower than 5% was considered as a non-obstructive SDB event according to the manufacturer's definition.31 Also, the “obstructive pressure peak” signal, which was considered by D11 as a surrogate for obstructive apnea, was only reported in 67% of cases, while no sensitivity or specificity was indicated,29 and the clinical application of this method remained questionable. Other techniques of upper airway patency evaluation were applied by some devices, such as forced oscillation technique32 for D8 and pulse pressure method for D7. For D9, the upper airway patency identification relied on the detection of cardiac oscillations in airflow at mask. However, D9 raised the pressure during central apneas despite the presence of simulated “cardiac” oscillations. A potential explanation could be a misdetection of amplitude or frequency of these physiological oscillations. Of note, the sensitivity of cardiac oscillation was reported as only 60% for central apnea diagnosis.28 As a “trivial” solution, D9 allows users to set a maximum pressure for apneas in order to prevent a high pressure level during central apneas. It is noteworthy that the APAP devices showed better performance and treatment effectiveness for obstructive hypopnea than for apnea, especially for D5 and D11. Hence, these devices may be better adapted to mild obstructive SDB patients.
The reported results may bear a considerable significance due to the current clinical practice, which relies on unattended auto-titrating methods to set up constant pressure in patients as a way to save the cost of in-lab titration. Auto-titration could be used to select an effective EPAP or an appropriate EPAP range,14,33 in order to shorten the lag time for reaching the pressure equilibrium for APAP treatment and to avoid unnecessary pressure variations that could induce microarousals in patients,34,35 or ineffective adjustment of pressure which might be observed in patients with high number of alternation between sleep and wake periods.36
Concerning the outcomes of treatment, the poor performances of some devices may explain the observation of a poorer control of blood pressure with APAP, which was associated with a higher residual AHI.15 More recent studies have also underlined a less beneficial effect of APAP on autonomic nervous system activation measurements such as heart rate variability37,38 or pulse wave amplitude.39 The observed differences in residual AHI between bench values and device-reported ones bear considerable clinical implications, as the current follow-up of patient often rely on device-reported residual AHI which may be very different from actual patient values.17–21,39 Table 3 is intended to provide a general overview on the performance of each device and a classification according to patients' SDB profiles. D1, D3, D4, D6, and D10 showed a treatment efficacy > 90% (Table 3). In addition, D3, D5, D6, D8, D9, D10, and D11 showed an accuracy of device-reported AHI > 90% (Table 3). However, the inability of central-mechanism detection should be highlighted for the following devices: D1, D2, D3, D4, D6, D9, and D10. These devices should be used with cautions in patients with coexisting central SDB events.
Table 3.
Scoring and classification of APAP devices.
Limitation of the Study
On the current bench, the obstructive SDB patterns were characterized by the mechanical properties of the upper airway. Compared to the clinical trials, the variety of specific airflow patterns was limited, and the critical closing pressure for the upper airway (6 cm H2O) was positive as observed, particularly in severe obstructive patients. Also, the reported device performance only relies on the simulated patient's condition, i.e., the general scenarios, which were created to more closely simulate clinical variations within sleep-stage distribution.
CONCLUSIONS
This study using reproducible and standardized SDB events evidenced large differences between all APAP devices in performance and treatment efficacy. Both bench studies and clinical evaluations are necessary to test the devices in full range of patients' spectrum of diseases and should be implemented in the registration of devices.
DISCLOSURE STATEMENT
This was not an industry supported study. This research was supported by a CIFRE grant to K. Zhu, from the French Ministry of Higher Education and Research. The authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- AHI
apnea-hypopnea index
- APAP
auto-titrating positive airway pressure
- OSA
obstructive sleep apnea
- CPAP
continuous positive airway pressure
- SDB
sleep-disordered breathing
REFERENCES
- 1.Sullivan CE, Issa FG, Berthon-Jones M, McCauley VB, Costas LJ. Home treatment of obstructive sleep apnoea with continuous positive airway pressure applied through a nose-mask. Bull Eur Physiopathol Respir. 1984;20:49–54. [PubMed] [Google Scholar]
- 2.Giles TL, Lasserson TJ, Smith B, White J, Wright JJ, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006;(1):CD001106. doi: 10.1002/14651858.CD001106.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Scottish Intercollegiate Guidelines Network. Edinburgh: Scottish Intercollegiate Guidelines Network; 2003. Management of obstructive sleep apnoea/hypopnoea syndrome in adults. [Google Scholar]
- 4.Engleman HM, Martin SE, Kingshott RN, Mackay TW, Deary IJ, Douglas NJ. Randomised placebo controlled trial of daytime function after continuous positive airway pressure (CPAP) therapy for the sleep apnoea/hypopnoea syndrome. Thorax. 1998;53:341–5. doi: 10.1136/thx.53.5.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jenkinson C, Davies RJ, Mullins R, Stradling JR. Comparison of therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised prospective parallel trial. Lancet. 1999;353:2100–5. doi: 10.1016/S0140-6736(98)10532-9. [DOI] [PubMed] [Google Scholar]
- 6.George CF. Reduction in motor vehicle collisions following treatment of sleep apnoea with nasal CPAP. Thorax. 2001;56:508–12. doi: 10.1136/thorax.56.7.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pepperell JC, Ramdassingh-Dow S, Crosthwaite N, et al. Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Lancet. 2002;359:204–10. doi: 10.1016/S0140-6736(02)07445-7. [DOI] [PubMed] [Google Scholar]
- 8.Hoffstein V, Viner S, Mateika S, Conway J. Treatment of obstructive sleep apnea with nasal continuous positive airway pressure. Patient compliance, perception of benefits, and side effects. Am Rev Respir Dis. 1992;145:841–5. doi: 10.1164/ajrccm/145.4_Pt_1.841. [DOI] [PubMed] [Google Scholar]
- 9.Nino-Murcia G, McCann CC, Bliwise DL, Guilleminault C, Dement WC. Compliance and side effects in sleep apnea patients treated with nasal continuous positive airway pressure. West J Med. 1989;150:165–9. [PMC free article] [PubMed] [Google Scholar]
- 10.Rolfe I, Olson LG, Saunders NA. Long-term acceptance of continuous positive airway pressure in obstructive sleep apnea. Am Rev Respir Dis. 1991;144:1130–3. doi: 10.1164/ajrccm/144.5.1130. [DOI] [PubMed] [Google Scholar]
- 11.Waldhorn RE, Herrick TW, Nguyen MC, O'Donnell AE, Sodero J, Potolicchio SJ. Long-term compliance with nasal continuous positive airway pressure therapy of obstructive sleep apnea. Chest. 1990;97:33–8. doi: 10.1378/chest.97.1.33. [DOI] [PubMed] [Google Scholar]
- 12.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy. Proc Am Thorac Soc. 2008;5:173–8. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006;(4):CD005308. doi: 10.1002/14651858.CD005308.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith I, Lasserson TJ. Pressure modification for improving usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2009;(4):CD003531. doi: 10.1002/14651858.CD003531.pub3. [DOI] [PubMed] [Google Scholar]
- 15.Patruno V, Aiolfi S, Costantino G, et al. Fixed and autoadjusting continuous positive airway pressure treatments are not similar in reducing cardiovascular risk factors in patients with obstructive sleep apnea. Chest. 2007;131:1393–9. doi: 10.1378/chest.06-2192. [DOI] [PubMed] [Google Scholar]
- 16.Meurice JC, Cornette A, Philip-Joet F, et al. Evaluation of autoCPAP devices in home treatment of sleep apnea/hypopnea syndrome. Sleep Med. 2007:695–703. doi: 10.1016/j.sleep.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 17.Desai H, Patel A, Patel P, Grant BJB, Mador MJ. Accuracy of autotitrating CPAP to estimate the residual Apnea-Hypopnea Index in patients with obstructive sleep apnea on treatment with autotitrating CPAP. Sleep Breath. 2009;13:383–90. doi: 10.1007/s11325-009-0258-2. [DOI] [PubMed] [Google Scholar]
- 18.Denotti AL, Wong KKH, Dungan GC, 2nd, Gilholme JW, Marshall NS, Grunstein RR. Residual sleep-disordered breathing during autotitrating continuous positive airway pressure therapy. Eur Respir J. 2012;39:1391–7. doi: 10.1183/09031936.00093811. [DOI] [PubMed] [Google Scholar]
- 19.Ikeda Y, Kasai T, Kawana F, et al. Comparison between the apnea-hypopnea indices determined by the REMstar Auto M series and those determined by standard in-laboratory polysomnography in patients with obstructive sleep apnea. Intern Med. 2012;51:2877–85. doi: 10.2169/internalmedicine.51.8249. [DOI] [PubMed] [Google Scholar]
- 20.Cilli A, Uzun R, Bilge U. The accuracy of autotitrating CPAP-determined residual apnea-hypopnea index. Sleep Breath. 2013;17:189–93. doi: 10.1007/s11325-012-0670-x. [DOI] [PubMed] [Google Scholar]
- 21.Ueno K, Kasai T, Brewer G, et al. Evaluation of the apnea-hypopnea index determined by the S8 Auto-CPAP, a continuous positive airway pressure device, in patients with obstructive sleep apnea-hypopnea syndrome. J Clin Sleep Med. 2010;6:146–51. [PMC free article] [PubMed] [Google Scholar]
- 22.Berry RB, Kushida CA, Kryger MH, Soto-Calderon H, Staley B, Kuna ST. Respiratory event detection by a positive airway pressure device. Sleep. 2012;35:361–7. doi: 10.5665/sleep.1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The 510(k) Program: Evaluating Substantial Equivalence in Premarket Notifications [510(k)] - Guidance for Industry and Food and Drug Administration Staff [Internet] [Date last accessed: December 19, 2014]. Available from: http://www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/ucm404770.htm Document issued on: July 28, 2014.
- 24.Farré R, Montserrat JM, Rigau J, Trepat X, Pinto P, Navajas D. Response of automatic continuous positive airway pressure devices to different sleep breathing patterns: a bench study. Am J Respir Crit Care Med. 2002;166:469–73. doi: 10.1164/rccm.2111050. [DOI] [PubMed] [Google Scholar]
- 25.Abdenbi F, Chambille B, Escourrou P. Bench testing of auto-adjusting positive airway pressure devices. Eur Respir J. 2004;24:649–58. doi: 10.1183/09031936.04.00133703. [DOI] [PubMed] [Google Scholar]
- 26.Zhu K, Kharboutly H, Ma J, Bouzit M, Escourrou P. Bench test evaluation of adaptive servoventilation devices for sleep apnea treatment. J Clin Sleep Med. 2013;9:861–71. doi: 10.5664/jcsm.2982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. ISO 17510-1: 2007 Sleep apnoea breathing therapy - Part 1: Sleep apnoea breathing therapy equipment.
- 28.Ayappa I, Norman RG, Rapoport DM. Cardiogenic oscillations on the airflow signal during continuous positive airway pressure as a marker of central apnea. Chest. 1999;116:660–6. doi: 10.1378/chest.116.3.660. [DOI] [PubMed] [Google Scholar]
- 29.Ruhle KH, Domanski U, Nilius G. Obstructive pressure peak: a new method for differentiation of obstructive and central apneas under auto-CPAP therapy. Sleep Breath. 2013;17:111–5. doi: 10.1007/s11325-012-0657-7. [DOI] [PubMed] [Google Scholar]
- 30.Iber C, Ancoli-Israel S, Chesson AL, Quan SF. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. [Google Scholar]
- 31.DeVilbiss Healthcare. Clinical overview: DeVilbiss IntelliPAP AutoAdjust [Internet] [Date last accessed: June 30, 2014]. Available from: http://www.devilbisshealthcare.com/files/LT-2089_RevC_FINAL_050814_Web.pdf. Last update: 2010.
- 32.Armitstead JP, Richards GN, Wimms A, Benjafield AV. Central sleep apnea detection and the enhanced AutoSet algorithm [Internet] [Date last accessed: June 30, 2014]. Available from: http://www.resmed.com/fr/assets/documents/product/s9_series/1013916_s9-autoset_white-paper.pdf. Last update: 2010.
- 33.Morgenthaler TI, Aurora RN, Brown T, et al. Practice parameters for the use of autotitrating continuous positive airway pressure devices for titrating pressures and treating adult patients with obstructive sleep apnea syndrome: an update for 2007. An American Academy of Sleep Medicine report. Sleep. 2008;31:141–7. doi: 10.1093/sleep/31.1.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fuchs FS, Wiest GH, Frank M, et al. Auto-CPAP therapy for obstructive sleep apnea: induction of microarousals by automatic variations of CPAP pressure? Sleep. 2002;25:514–8. [PubMed] [Google Scholar]
- 35.Marrone O, Insalaco G, Salvaggio A, Bonsignore G. Role of different nocturnal monitorings in the evaluation of CPAP titration by autoCPAP devices. Respir Med. 2005;99:313–20. doi: 10.1016/j.rmed.2004.07.018. [DOI] [PubMed] [Google Scholar]
- 36.Lévy P, Pépin JL. Autoadjusting continuous positive airway pressure: what can we expect? Am J Respir Crit Care Med. 2001;163:1295–6. doi: 10.1164/ajrccm.163.6.ed1801f. [DOI] [PubMed] [Google Scholar]
- 37.Patruno V, Tobaldini E, Bianchi AM, et al. Acute effects of autoadjusting and fixed continuous positive airway pressure treatments on cardiorespiratory coupling in obese patients with obstructive sleep apnea. Eur J Intern Med. 2014;25:164–8. doi: 10.1016/j.ejim.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 38.Karasulu L, Epöztürk PÖ, Sökücü SN, Dalar L, Altın S. Improving heart rate variability in sleep apnea patients: differences in treatment with auto-titrating positive airway pressure (APAP) versus conventional CPAP. Lung. 2010;188:315–20. doi: 10.1007/s00408-010-9237-4. [DOI] [PubMed] [Google Scholar]
- 39.Bakker JP, Campbell AJ, Neill AM. Pulse wave analysis in a pilot randomised controlled trial of auto-adjusting and continuous positive airway pressure for obstructive sleep apnoea. Sleep Breath. 2011;15:325–32. doi: 10.1007/s11325-010-0385-9. [DOI] [PubMed] [Google Scholar]