Abstract
Objective:
Insomnia is common following exposure to trauma and can occur independently or as a feature of posttraumatic stress disorder (PTSD). However, there is limited research identifying risk factors associated with the development of insomnia following exposure to a traumatic event. The goal of this study was to evaluate the role of specific trauma types in the risk for insomnia in a community sample of urban African Americans young adults.
Methods:
A sample of 554 nonclinical, urban, young adult African Americans was recruited for a larger study from which 465 participants were utilized for this study based on their completion of all study self-report measures. Participants were initially screened by phone to determine whether they provisionally met study criteria. Once selected, participants underwent informed consent and then completed a battery of self-report measures that included the Life Events Checklist, the PTSD Checklist, the Insomnia Severity Index, and the Fear of Sleep Index.
Results:
Of the seven trauma categories that were endorsed by at least 20% of the sample, results from logistic regression models indicated that sexual trauma, physical assault, accidents, natural disasters, and sudden violent death predicted insomnia independent of sex. However, PTSD symptom severity and nocturnal fears differentially influenced the relationship between trauma type and risk for insomnia.
Conclusions:
Exposure to specific types of trauma increases the odds of insomnia twofold to threefold. Additionally, PTSD symptom severity and nocturnal fears contribute differentially to the relationship between trauma exposure and insomnia suggesting the possibility of multiple underlying pathways.
Citation:
Hall Brown TS, Akeeb A, Mellman TA. The role of trauma type in the risk for insomnia. J Clin Sleep Med 2015;11(7):735–739.
Keywords: insomnia, PTSD, sleep disturbance, trauma
Insomnia, defined as difficulty initiating or maintaining sleep or nonrestorative sleep of at least 1 mo in duration,1 is associated with multiple adverse outcomes. These include increased risk for the metabolic syndrome, all-cause mortality,2,3 mood and anxiety disorders, reduced productivity, accidents, and greater use of medical services.4–6 A better understanding of factors contributing to insomnia could aid its prevention, which would have implications for improving function, quality of life, and long-term health.
Insomnia symptoms are common following exposure to trauma.7 They can manifest independently or as a feature of posttraumatic stress disorder (PTSD)7; however, there is limited research identifying risk factors associated with its development in this context. Retrospective studies have suggested connections between specific types of trauma and insomnia but have not directly compared whether certain trauma types are more engendering of insomnia than others.8,9 For example, Bader and colleagues8 studied a clinical sample of adults with primary insomnia and found that 46% of the patients reported a moderate to severe adverse experience during childhood, which included physical, sexual, and emotional abuse, and neglect. This subgroup exhibited a greater number of awakenings and more nocturnal movements during sleep recordings than those with limited or no adverse childhood experiences. In addition, Noll and colleagues9 found that children and adolescents who were sexually abused endorsed greater rates of insomnia symptoms, sleep avoidance, and nightmares compared with their nontrauma-exposed peers even after controlling for PTSD and depression. Previous studies by our group also support the association between insomnia and PTSD and the additional contribution of nocturnal fears.10 Specifically, we found that PTSD symptom severity and nocturnal fears were correlated in urban young adults exposed to trauma and that they both independently predicted the presence of insomnia. However, like other studies we did not investigate whether specific trauma types were more engendering of insomnia.
BRIEF SUMMARY
Current Knowledge/Study Rationale: Insomnia symptoms are common following exposure to trauma, however, there is limited research identifying risk factors associated with its development in this context. The goal of this study was to evaluate associations of insomnia with specific types of trauma in a community sample of urban African Americans exposed to a broad range of trauma types.
Study Impact: Results suggest exposure to specific types of trauma confer increased risk for insomnia and that PTSD and nocturnal fears differentially contribute to this relationship. These results point to the utility of sleep specific treatment strategies that can be used independently or in conjunction with empirically supported trauma treatments dependent on the type of trauma exposure.
The goal of this study was to evaluate associations of insomnia with specific types of trauma in a community sample of urban African Americans exposed to a broad range of trauma types. We also evaluated whether these associations were accounted for by PTSD and sleep fears. Based on the findings of previous studies8,9 we hypothesized that out of the seven trauma types analyzed in our study, sexual trauma and physical assault would be associated with a high risk for insomnia. Determination of specific high-risk trauma categories and understanding whether they are independent of PTSD and trauma-related sleep fears could serve to identify individuals at greatest risk for developing insomnia and inform the type of interventions that would be most effective for preventing or treating insomnia in the context of trauma.
METHOD
Participants
A sample of 554 nonclinical, urban, young adult African Americans was recruited for a study examining the relationship between PTSD, sleep, and nocturnal blood pressure. These participants were recruited using fliers posted in neighborhoods surrounding the Howard University Medical Center as well as other District of Columbia neighborhoods in which population demographics were consistent with study recruitment goals and through referrals from previous participants. For this study, data from 465 participants were utilized based on their completion of all study self-report measures. There were no significant demographic differences between those with complete versus incomplete data. The average age of the sample was 22 years (standard deviation [SD] = 3.68, range 18–35), 57% were female, and 81% had at least some college education.
Measures
A battery of self-report measures was administered to each participant during the first phase of the parent study, followed by clinical interviews and laboratory studies of a subgroup that are not included in the current report. A demographic questionnaire obtained age, sex, and race. Additional self-report measures included the following:
The Insomnia Severity Index (ISI) assessed the amount of difficulty falling asleep, staying asleep, and waking early, satisfaction with sleep, effect of insomnia on daily functioning, degree to which others notice, and the amount of distress caused by lack of sleep for a 2-w period using a five-point Likert scale rating. The internal consistency for this measure in our sample was α = 0.87, and a score of 11 or higher has been established as optimal for detecting clinically significant sleep difficulties in a community sample and is used in this study as the threshold for identifying the prevalence of mild to severe insomnia.11 We also utilized a more restricted range of scores (a cutoff score of greater than 15) to examine the prediction of moderate to severe insomnia. Using this more stringent cutoff score increased the specificity of the measure from 87.7% to 98.3% in a community sample.11
The Life Events Checklist (LEC) was administered to evaluate exposure to traumatic events over the course of a respondent's lifetime.12 The LEC lists 16 events that are associated with the development of PTSD and an additional item that allows the respondent to report any other “stressful” event that was not captured by the first 16 items. Respondents endorse each trauma exposure as occurring before or after the age of 16 y. For this study several categories were combined to enable analyses. Sexual assault, sexual abuse, and unwanted sexual experience were combined to form the category “sexual trauma.” Assault with a weapon and physical assault were combined to form the category “physical assault” and transportation accidents and serious accidents at work, home, or during a recreational activity were combined to form the category “accidents.”
The Posttraumatic Stress Disorder Checklist (PCL) was utilized to assess the severity of posttraumatic stress symptoms.13 The PCL is a measure that uses a five-point Likert scale where higher scores represent increased symptom severity. The internal consistency for the PCL for this sample was α = 0.92. We used a score of 44 (94% sensitivity and 86% specificity) as a threshold for probable PTSD based on the clinical cutoff score established for civilian populations.14 Sleep items were deleted from the overall score when the PCL score was analyzed in relation to insomnia.
The Fear of Sleep Inventory (FOSI)15,16 assesses sleep related fears that are commonly associated with trauma including vigilant behaviors, fear of loss of vigilance, and dread of nightmares. It features a five-point Likert scale format that is anchored by 0 “not at all” and 4 “nearly every night” where higher scores indicate greater nocturnal fears. The FOSI has demonstrated good reliability and modest correlations16 with sleep quality (Pittsburgh Sleep Quality Index; r = 0.39), PTSD severity (PCL; r = 0.68), and insomnia severity (ISI; r = 0.32–0.47). The internal consistency for the FOSI in our sample was α = 0.93.
Procedures
Approval for this study was obtained through the Howard University Institutional Review Board. Participants were initially screened by phone to determine whether they provisionally met study criteria, which included good health (i.e., the absence of any chronic medical condition), consistent use of medication, limited caffeine use (i.e., fewer than three cups of coffee a day or its equivalent), and absence of recent shift work, alcohol or drug dependence, and severe chronic mental illness other than PTSD. Once selected for the parent study, participants underwent procedures for informed consent and then completed the battery of self-report measures in a private room located in the Clinical Research Unit of Howard University.
Analytic Strategy
Sample characteristics were assessed using descriptive statistics. Basic checks for normality were conducted for all variables. Frequency counts were examined for each specific trauma type from the LEC to identify those trauma types where at least 20% of the sample endorsed exposure, which yielded seven trauma categories for subsequent analyses. Chi-square analyses were calculated to inform subsequent logistic regression models by determining which of the retained trauma categories were associated with insomnia. Logistic regression analyses were then conducted to determine which trauma categories conferred the greatest risk for both mild to severe insomnia and moderate to severe insomnia while holding sex constant. These regression models were then run again with the inclusion of PTSD symptoms severity scores and FOSI scores to determine whether these associations were accounted for by PTSD severity and/or nocturnal fears.
RESULTS
Insomnia
The average score on the ISI was 9.1 (SD = 6.1) with 40% (n = 185) of the sample screening positively for mild to severe insomnia (ISI score > 10) and 16% (n = 75) screening positively for moderate to severe insomnia (ISI > 15). Overall, insomnia was more prevalent among females (45%) than males (33%) (Chi-square [1, 455] = 6.57, p = 0.01). There were no significant differences in insomnia prevalence for any other of the demographic variables (i.e., age, or highest education). Therefore, sex was included as a covariate in subsequent analyses.
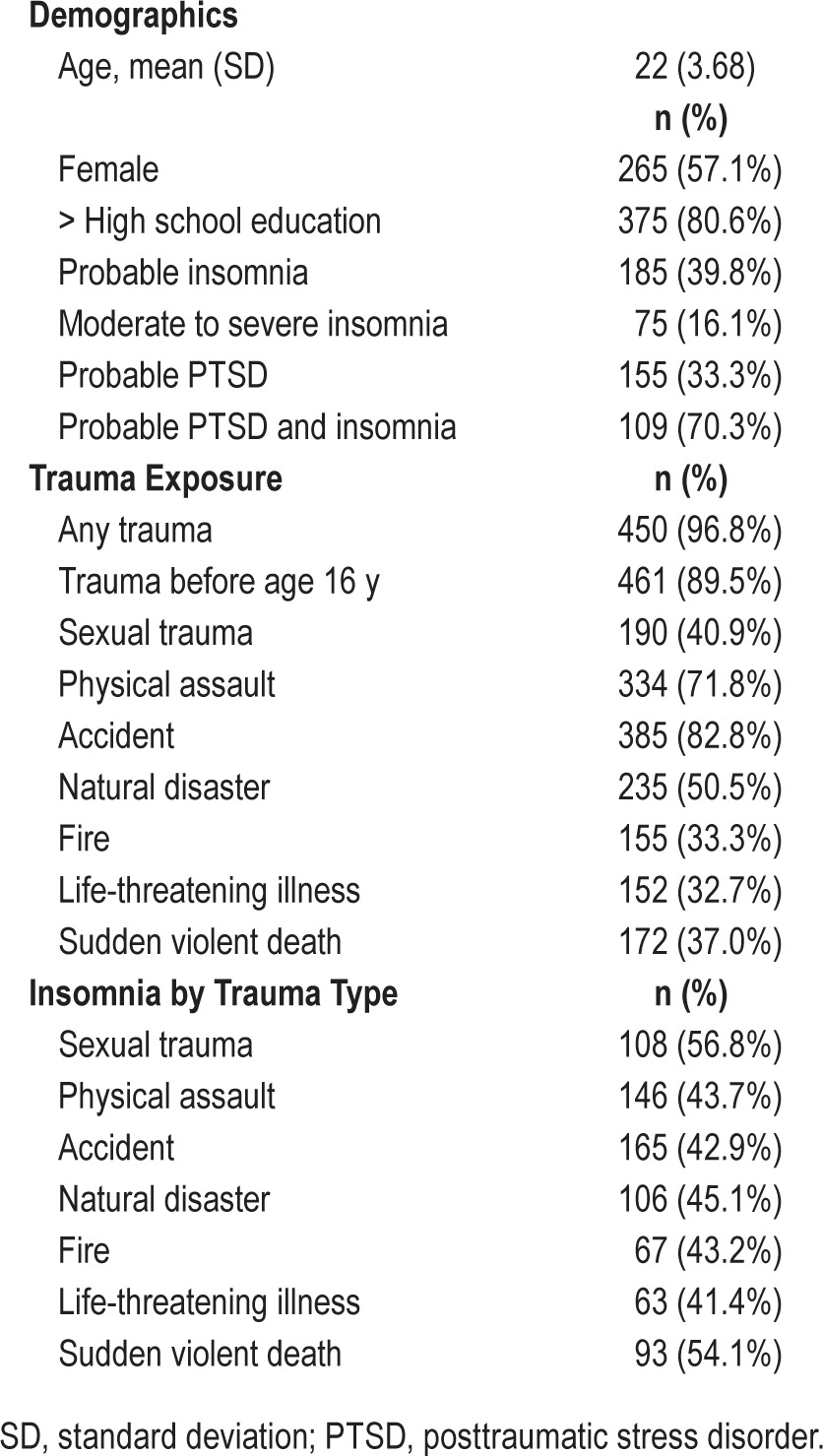
Trauma and PTSD
Ninety-seven percent (n = 450) of the sample endorsed exposure to at least one trauma (probable Diagnostic and Statistical Manual of Mental Disorders, 4th Edition criterion A event) during their lifetime, with 90% (n = 417) endorsing exposure to at least one traumatic experience before the age of 16 y (see Table 1). Differences also existed by sex with more females endorsing exposure to sexual trauma (Chi-square [1, 464] = 57.28, p < 0.001), physical assault (Chi-square [1, 464] = 13.04, p < 0.001), and accidents (Chi-square [1, 464] = 6.67, p < 0.05) as compared with males. The average number of trauma categories endorsed was 4.8 (SD = 2.6). The most commonly experienced types of traumas included transportation accidents (83%), physical assaults (72%), natural disasters (51%), and sexual traumas (41%). Thirty-three percent of the total sample (n = 155) met criteria for probable PTSD from the PCL, with 70% (n = 109) of those who met criteria for probable PTSD also meeting criteria for insomnia (see Table 1). Trauma exposed participants had an average PCL score of 37.6 (SD = 15.5).
Table 1.
Sample characteristics (n = 465).
Specific Trauma Type and Risk for Insomnia
Of the seven trauma categories that were endorsed by at least 20% of the sample, insomnia was significantly associated with sexual trauma (Chi-square [1, 465] = 39.38, p < 0.001), physical assault (Chi-square [1, 465] = 7.50, p < 0.01), accidents (Chi-square [1,465] = 8.72, p < 0.01), natural disasters (Chi-square [1, 465] = 5.43, p < 0.05), and exposure to sudden violent death (Chi-square [1, 465] = 22.71, p < 0.001) compared to never having been exposed to these types of traumas. The remaining included trauma categories, fire/explosions and life threatening illness/injury, were not significantly associated with insomnia.
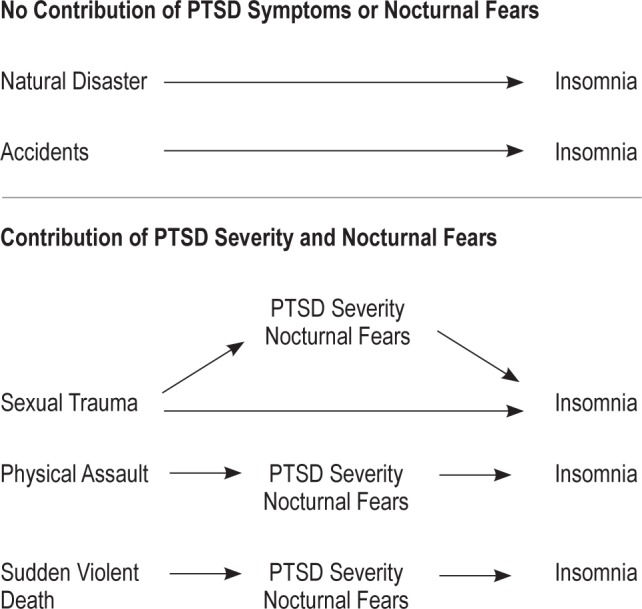
Results from logistic regression models indicated that sexual trauma, physical assault, accidents, natural disasters, and sudden violent death predicted mild to severe insomnia independent of sex with estimated odds ratios of 3.3, 2.1, 2.4, 1.5, and 2.5 respectively. However, only sexual trauma, physical assault, and sudden violent death predicted moderate to severe insomnia with estimated odds ratios of 2.9, 3.3, and 2.4, respectively (see Table 2). Based on an established association between PTSD symptoms and insomnia in the literature as well as a previously identified relationship between nocturnal fears and insomnia by our group, PCL score and FOSI score were added to the models to determine whether they accounted for the increased odds of insomnia associated with the previously identified trauma categories. Given the high correlation between these two variables (r = 0.625, p < 0.001), they were entered into each model simultaneously. Results indicated that the increased odds for mild to severe insomnia associated with physical assault and sudden violent death were completely accounted for by PCL score and FOSI score. The estimated odds ratio was attenuated for sexual trauma with the inclusion of PCL and FOSI scores, dropping to an estimated odds ratio of 2.1. The risk of mild to severe insomnia for accidents and natural disasters was not influenced by either PCL score or FOSI, maintaining approximately the same odds ratios as their initial models (see Table 2 and Figure 1). When the same analyses were conducted to predict the odds of moderate to severe insomnia the increased odds associated with sexual trauma, physical assault, and sudden violent death were completely accounted for by PCL score and FOSI score (see Table 2).
Table 2.
Estimated odds ratio for insomnia based on specific trauma type.
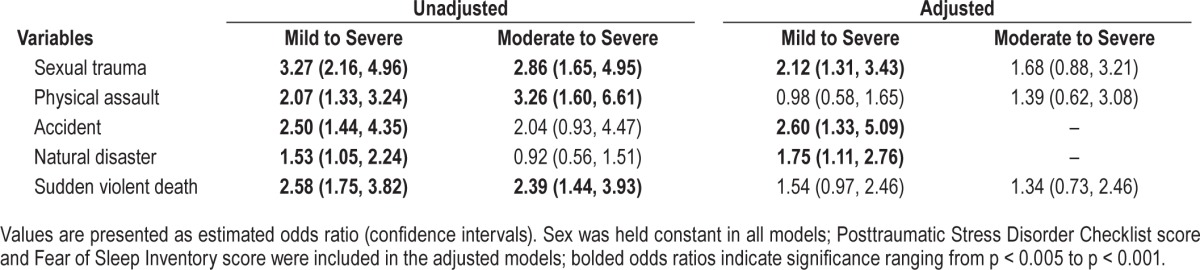
Figure 1. Contribution of posttraumatic stress disorder (PTSD) symptoms and nocturnal fears to the relationship of mild to severe insomnia and trauma type.
DISCUSSION
Results of this study are consistent with prior epidemiologically derived studies that indicated a high prevalence of inadequate or disturbed sleep in African American populations.17–19 Endorsement of self-report measures show that the rates of mild to severe insomnia were higher than the rates for probable PTSD in this highly trauma exposed population; however, when more stringent criteria were used to only include moderate to severe insomnia symptoms, the rates of insomnia drop to 16%. Given that even mild forms of insomnia have been linked to adverse health outcomes20 these findings have implications for public health, including the health disparities that disproportionately burden African Americans.
Our data also indicate that exposure to specific types of trauma increases the odds of insomnia twofold to threefold over never having been exposed. This finding is consistent with previous data that link sexual trauma, physical assault, and exposure to natural disasters7,8,21 with sleep disturbance and extends the extant PTSD and sleep literature by revealing additional trauma categories that may more commonly occur in urban environments (i.e., traffic accidents in more densely populated areas and exposure to sudden violent death). Additionally, our data suggest that sexual trauma, physical assault, and sudden violent death are trauma types that convey increased susceptibility to more severe levels of insomnia. Individuals who experience these high-risk traumas may be more fearful of their environment and perceive a loss of control or security, leading to increased risk for disturbances of sleep. Identification of specific trauma types that are more engendering of insomnia has important clinical implications for assessment and diagnosis. Specifically, these findings underscore the importance of (1) assessing for insomnia in individuals exposed to sexual traumas, physical assault, accidents, natural disasters, and sudden violent deaths over and above the typical trauma focused assessment, and (2) identifying clinically significant levels of sleep disturbance that occur with or independently of PTSD.
The varying influence of PTSD symptom severity and trauma-related sleep fears on the risk of insomnia related to individual trauma types suggests multiple pathways for this relationship and may help explain why insomnia often persists upon completion of trauma-focused treatments for PTSD.22 It would be worthwhile to replicate these findings with evaluation of alternate pathways that take into account temporal relationships among insomnia, PTSD, and sleep fears. Treatment implications of the results of such studies should also be evaluated. For example, insomnia associated with exposure to natural disasters and accidents may benefit from treatments that specifically target sleep disturbance. Sleep symptoms associated with sexual trauma may be more likely to be influenced by PTSD-focused treatments in most cases but could also benefit from adjunctive sleep-focused strategies in cases with persistent sleep problems. Insomnia symptoms associated with physical assault or exposure to sudden violent death may respond to trauma-focused therapies but investigation of the need for further emphasis on sleep disturbance is warranted.
There are several limitations to consider in interpreting our findings. First, this study relied on self-report data for both PTSD and insomnia symptoms. Future studies might utilize objective measures of sleep, or incorporate clinical interviews to better characterize symptoms and strengthen confidence in diagnoses. Additionally, it would be beneficial to evaluate other types of sleep disturbances (i.e., nightmares, short sleep duration, etc) to provide a more comprehensive understanding of the relationship between sleep and trauma. Second, low rates of endorsement of certain trauma types preclude inferences regarding their relevance to insomnia. Future studies might over sample for these particular traumas to determine whether an association with insomnia exists. Finally, given the retrospective nature of these data, prospective research designs could be used to further examine factors associated with this relationship that were not considered in the current models.
In summary, this study replicates previous findings and extends the extant literature by providing data related to the role of specific trauma types in the risk for insomnia following exposure to trauma. These results reveal that mild to severe insomnia is more common than PTSD in urban, African American young adults and that rates for insomnia differ based on the type of trauma exposure. Additionally, PTSD symptom severity and nocturnal fears contribute to the relationship between trauma exposure and insomnia in some categories but do not explain the entire relationship in most instances. Replication and extension of these results could point to the necessity for sleep specific treatment strategies that can be used independently or in conjunction with empirically supported trauma treatments dependent on the type of trauma exposure. For example, in the case of exposure to natural disasters and accidents, primary insomnia treatment may often be indicated. In the case of sexual trauma, physical assault, and exposure to sudden violent death, adjunct treatments used in combination with empirically supported trauma focused therapies might prove most effective. However, further research is necessary to formally test these potential implications.
DISCLOSURE STATEMENT
This was not an industry supported study. This research was, in part, supported by NHLBI grant 5R01HL087995 to Dr. Mellman, NCATS grant UL1RR031975 for the Georgetown Howard Universities Center for Clinical and Translational Science, and NCATS grant KL2 RR 025006 for the Johns Hopkins Institute for Clinical and Translational Research (ICTR). The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors acknowledge Duaa Altee, Latesha McLaughlin, and Janeese Brown-low for their technical assistance with this project.
ABBREVIATIONS
- FOSI
Fear of Sleep Inventory
- ISI
Insomnia Severity Index
- LEC
Life Events Checklist
- PCL
Posttraumatic Stress Disorder Checklist
- PTSD
posttraumatic stress disorder
- SD
standard deviation
REFERENCES
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th edition. Washington, DC: American Psychiatric Association; 1994. text revision. [Google Scholar]
- 2.Chien K, Chen P, Hsu H, et al. Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: report from a community-based cohort. Sleep. 2012;33:177–84. doi: 10.1093/sleep/33.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Troxel WM, Buysse DJ, Matthews KA, et al. Sleep Symptoms predict the development of metabolic syndrome. Sleep. 2010;33:1633–40. doi: 10.1093/sleep/33.12.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basta M, Chrousos GP, Vela-Bueno A, Vgontzas AN. Chronic insomnia and stress system. Sleep Med Clin. 2007;2:279–91. doi: 10.1016/j.jsmc.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daley MM, Morin CM, LeBlanc MM, Grégoire JP, Savard JJ, Baillargeon LL. Insomnia and its relationship to health-care utilization, work absenteeism, productivity and accidents. Sleep Med. 2009;10:427–38. doi: 10.1016/j.sleep.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Kuppermann M, Lubeck DP, Mazonson PD, Stewart AL, Buesching DP, Fifer SK. Sleep problems and their correlates in a working population. J Gen Intern Med. 1995;10:25–32. doi: 10.1007/BF02599573. [DOI] [PubMed] [Google Scholar]
- 7.Ohayon M, Shapiro C. Sleep disturbances and psychiatric disorders associated with posttraumatic stress disorder in the general population. Comp Psychiatry. 2000;41:469–78. doi: 10.1053/comp.2000.16568. [DOI] [PubMed] [Google Scholar]
- 8.Bader K, Schafer V, Schenkel M, Nissen L, Schwander J. Adverse childhood experiences associated with sleep in primary insomnia. Eur Sleep Res Soc. 2009;16:285–96. doi: 10.1111/j.1365-2869.2007.00608.x. [DOI] [PubMed] [Google Scholar]
- 9.Noll JG, Trickett PK, Susman EJ, Putnam FW. Sleep disturbances and childhood sexual abuse. J Pediatr Psychol. 2006;31:469–80. doi: 10.1093/jpepsy/jsj040. [DOI] [PubMed] [Google Scholar]
- 10.Hall Brown T, Mellman TA. The influence of PTSD, sleep fears, and neighborhood stress on insomnia and short sleep duration in urban, young adult, African Americans. Behav Sleep Med. 2014;12:198–206. doi: 10.1080/15402002.2013.784704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morin CM., Belleville G, Belanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–8. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–41. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- 13.Weathers FW, Frank W, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the clinician-administered posttraumatic stress disorder scale. Psychological Assessment. 1999;11:124–33. [Google Scholar]
- 14.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (pcl) Behav Res Ther. 1996;34:669–73. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 15.Huntley ED, Hall Brown TS, Kobayashi I, Mellman TA. Validation of the Fear of Sleep Inventory (FOSI) in an urban young adult African American sample. J Trauma Stress. 2014;27:103–7. doi: 10.1002/jts.21882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeViva JC, Zayfert C, Pigeon WR. Trauma in a sleep context: implications for insomnia related to PTSD. In: Zayfert C, editor. The Role of Fear of Sleep in Trauma-Related Insomnia: Biological and Psychological Perspectives; Symposium conducted at: annual meeting of the International Society of Traumatic Stress Studies (ISTSS); November 4-7; Hollywood, CA. 2006. (chair) [Google Scholar]
- 17.Feredinand Z, Pandey A, Murray-Bachmann R, et al. Race/ethnicity, sleep duration, and diabetes mellitus: analysis of the National Health Interview Survey. Am J Med. 2012;125:162–7. doi: 10.1016/j.amjmed.2011.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30:1096–103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kripke DF, Jean-Louis G, Elliott JA, et al. Ethnicity, sleep, mood, and illumination in postmenopausal women. BMC Psychiatry. 2004;4:8. doi: 10.1186/1471-244X-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall Brown T, Mellman TA, Alfano CA, Weems CF. Sleep fears, sleep disturbance, and PTSD symptoms in minority youth exposed to Hurricane Katrina. J Trauma Stress. 2011;24:575–80. doi: 10.1002/jts.20680. [DOI] [PubMed] [Google Scholar]
- 21.Troxel WM, Buysse DJ, Matthews KA, et al. Sleep symptoms predict the development of the metabolic syndrome. Sleep. 2010;33:1633–40. doi: 10.1093/sleep/33.12.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zayfert C, DeViva JC. Residual insomnia following cognitive behavioral therapy for PTSD. J Trauma Stress. 2004;17:69–73. doi: 10.1023/B:JOTS.0000014679.31799.e7. [DOI] [PubMed] [Google Scholar]


